Abstract
Background
Although helicopters are presently an integral part of trauma systems in most developed nations, previous reviews and studies to date have raised questions about which groups of traumatically injured people derive the greatest benefit.
Objectives
To determine if helicopter emergency medical services (HEMS) transport, compared with ground emergency medical services (GEMS) transport, is associated with improved morbidity and mortality for adults with major trauma.
Search methods
We ran the most recent search on 29 April 2015. We searched the Cochrane Injuries Group's Specialised Register, The Cochrane Library (Cochrane Central Register of Controlled Trials; CENTRAL), MEDLINE (OvidSP), EMBASE Classic + EMBASE (OvidSP), CINAHL Plus (EBSCOhost), four other sources, and clinical trials registers. We screened reference lists.
Selection criteria
Eligible trials included randomized controlled trials (RCTs) and nonrandomized intervention studies. We also evaluated nonrandomized studies (NRS), including controlled trials and cohort studies. Each study was required to have a GEMS comparison group. An Injury Severity Score (ISS) of at least 15 or an equivalent marker for injury severity was required. We included adults age 16 years or older.
Data collection and analysis
Three review authors independently extracted data and assessed the risk of bias of included studies. We applied the Downs and Black quality assessment tool for NRS. We analyzed the results in a narrative review, and with studies grouped by methodology and injury type. We constructed 'Summary of findings' tables in accordance with the GRADE Working Group criteria.
Main results
This review includes 38 studies, of which 34 studies examined survival following transportation by HEMS compared with GEMS for adults with major trauma. Four studies were of inter‐facility transfer to a higher level trauma center by HEMS compared with GEMS. All studies were NRS; we found no RCTs. The primary outcome was survival at hospital discharge. We calculated unadjusted mortality using data from 282,258 people from 28 of the 38 studies included in the primary analysis. Overall, there was considerable heterogeneity and we could not determine an accurate estimate of overall effect.
Based on the unadjusted mortality data from six trials that focused on traumatic brain injury, there was no decreased risk of death with HEMS. Twenty‐one studies used multivariate regression to adjust for confounding. Results varied, some studies found a benefit of HEMS while others did not. Trauma‐Related Injury Severity Score (TRISS)‐based analysis methods were used in 14 studies; studies showed survival benefits in both the HEMS and GEMS groups as compared with MTOS. We found no studies evaluating the secondary outcome, morbidity, as assessed by quality‐adjusted life years (QALYs) and disability‐adjusted life years (DALYs). Four studies suggested a small to moderate benefit when HEMS was used to transfer people to higher level trauma centers. Road traffic and helicopter crashes are adverse effects which can occur with either method of transport. Data regarding safety were not available in any of the included studies. Overall, the quality of the included studies was very low as assessed by the GRADE Working Group criteria.
Authors' conclusions
Due to the methodological weakness of the available literature, and the considerable heterogeneity of effects and study methodologies, we could not determine an accurate composite estimate of the benefit of HEMS. Although some of the 19 multivariate regression studies indicated improved survival associated with HEMS, others did not. This was also the case for the TRISS‐based studies. All were subject to a low quality of evidence as assessed by the GRADE Working Group criteria due to their nonrandomized design. The question of which elements of HEMS may be beneficial has not been fully answered. The results from this review provide motivation for future work in this area. This includes an ongoing need for diligent reporting of research methods, which is imperative for transparency and to maximize the potential utility of results. Large, multicenter studies are warranted as these will help produce more robust estimates of treatment effects. Future work in this area should also examine the costs and safety of HEMS, since multiple contextual determinants must be considered when evaluating the effects of HEMS for adults with major trauma.
Plain language summary
Helicopter emergency medical services for adults with major trauma
Background
Trauma is a leading cause of death and disability worldwide and, since the 1970s, helicopters have been used to transport people with injuries to hospitals that specialize in trauma care. Helicopters offer several potential advantages, including faster transport, and care from medical staff who are specifically trained in the management of major injuries.
Study characteristics
We searched the medical literature for clinical studies comparing the transport of adults who had major injuries by helicopter ambulance (HEMS) or ground ambulance (GEMS). The evidence is current to April 2015.
Key results
We found 38 studies which included people from 12 countries around the world. Researchers wanted to find out if using a helicopter ambulance was any better than a ground ambulance for improving an injured person's chance of survival, or reducing the severity of long‐term disability. Some of these studies indicated some benefit of HEMS for survival after major trauma, but other studies did not. The studies were of varying sizes and used different methods to determine if more people survived when transported by HEMS versus GEMS. Some studies included helicopter teams that had specialized physicians on board whereas other helicopter crews were staffed by paramedics and nurses. Furthermore, people transported by HEMS or GEMS had varying numbers and types of procedures during travel to the trauma center. The use of some of these procedures, such as the placement of a breathing tube, may have helped improve survival in some of the studies. However, these medical procedures can also be provided during ground ambulance transport. Data regarding safety were not available in any of the included studies. Road traffic and helicopter crashes are adverse effects which can occur with either method of transport.
Quality of the evidence
Overall, the quality of the included studies was low. It is possible that HEMS may be better than GEMS for people with certain characteristics. There are various reasons why HEMS may be better, such as staff having more specialty training in managing major injuries. But more research is required to determine what elements of helicopter transport improve survival. Some studies did not describe the care available to people in the GEMS group. Due to this poor reporting it is impossible to compare the treatments people received.
Conclusions
Based on the current evidence, the added benefits of HEMS compared with GEMS are unclear. The results from future research might help in better allocation of HEMS within a healthcare system, with increased safety and decreased costs.
Summary of findings
Background
Description of the condition
Worldwide, unintentional injuries are responsible for over 3.9 million deaths and over 138 million disability‐adjusted life‐years (DALY) (Chandran 2010). Trauma currently accounts for 12% of the world's burden of disease and annually there are more than five million deaths due to injuries worldwide (CDC 2010; Krug 2002; Murray 1996). By 2020, it is estimated that 1 in 10 people will die from injuries (CDC 2010; Murray 1996).
Description of the intervention
Early reports from the Korean and Vietnam wars suggested a 2% increase in survival for casualties as the time to definitive care improved from five hours to one hour with prompt transport by helicopter to forward‐deployed surgical theaters (Baxt 1983; Baxt 1985; Bledsoe 2006; Cowley 1973; McNabney 1981; Shatz 2004; Taylor 2010). Based on the results of these wartime experiences, civilian helicopters were used for the first time in the 1970s to transport traumatically injured people to trauma centers (Kerr 1999; Wish 2005). In Germany, the Christoph 1 helicopter entered service in 1970, and services rapidly expanded to over seven rescue bases (Seegerer 1976). Today, the use of helicopter emergency medical services (HEMS) for the transportation of people with trauma is common in most developed nations (Butler 2010; Champion 1990; Kruger 2010; Ringburg 2009a). Helicopters are capable of transporting people with major trauma significantly faster than ground units and the speed benefit is more pronounced as the distance from a trauma center increases. Nevertheless, research has questioned which traumatically injured people derive the greatest benefit from the utilization of this limited and resource‐intensive form of transportation (Bledsoe 2005; Bledsoe 2006; Cunningham 1998; DiBartolomeo 2005; Ringburg 2009a).
How the intervention might work
The use of HEMS is largely predicated on the concept of the 'golden hour' (Cowley 1979). Time may play a crucial role in the treatment of adults with major trauma, and delays in management could worsen prognosis. Helicopter transport can decrease transport times and may facilitate earlier, definitive treatment. Several studies have established that timely and advanced trauma care may help improve mortality figures by reversing hypoperfusion to vital organs (Cowley 1979; Sampalis 1999). In one study, the risk of death was found to be significantly increased for every 10‐minute increase in out‐of‐hospital time (Sampalis 1999). However, the origins and scientific evidence for the 'golden hour', while intuitively appealing, have been questioned as has the role of HEMS in the chain of survival for people who are critically injured (Lerner 2001).
Mortality from motor vehicle crashes is reduced when an organized system of trauma care is implemented, of which HEMS is often an important component (Nathans 2000). The risk of death may be reduced by 15% to 20% when care is provided in a trauma center (MacKenzie 2006; MacKenzie 2007). A level I trauma center provides the highest level of surgical and critical care for people with trauma. Level I trauma centers have 24‐hour surgical coverage, including in‐house coverage by orthopedic surgeons, neurosurgeons, plastic surgeons, and other specialists, in addition to an active research program and a commitment to regional trauma education. People with major trauma who require an operation may benefit from management at a level I trauma center, but it is unclear if earlier intervention and rapid assessment alone fully explain the survival benefit (Haas 2009). The mortality benefits resulting from admission to a level I trauma center may be due to the definitive surgical expertise available at these centers (Haut 2006), in addition to the advanced resources for critical care and rehabilitation services (Haut 2009). Furthermore, speed may not be the only contributory effect of HEMS in terms of mortality benefits for adults with major trauma. HEMS crews are typically composed of highly trained personnel, including experienced paramedics, critical care nurses, respiratory therapists, and, in some cases, physicians. Hence, any HEMS‐associated outcome benefit is likely to be the result of some combination of speed, expertise, and the role that HEMS programs have as part of integrated trauma systems (Thomas 2003). Transport of injured people remains a major goal for most HEMS programs (Thomas 2002); beneficial effects of specialized trauma care regarding morbidity and mortality may be mediated by HEMS.
Why it is important to do this review
Results supporting mortality benefits for adults with major trauma transported by HEMS have been inconsistent (Ringburg 2009a; Thomas 2002; Thomas 2004; Thomas 2007), resulting in substantial controversy in both the medical literature and the transportation safety arena. Many HEMS outcome studies have the limitations of small sample sizes, important heterogeneity, and other inadequate statistical methodologies. Some overviews of the literature have pointed to a clear positive effect on survival associated with HEMS transport (Ringburg 2009a), while others have maintained persistent skepticism about the beneficial impact of HEMS (Bledsoe 2006). The use of HEMS is not without potential risk. In addition to the risk to patients, HEMS flight crews have one of the highest mortality risks of all occupations (Baker 2006). For these reasons, a systematic review of the literature is warranted so that structured evidence may be produced to inform and improve clinical interventions, triage decisions, and public policies regarding HEMS. The results from this review may inform the design of subsequent randomized or nonrandomized trials through the identification of relevant subgroups of people with trauma who may benefit from HEMS transport.
Objectives
To determine if helicopter emergency medical services (HEMS) transport, compared with ground emergency medical services (GEMS) transport, is associated with improved morbidity and mortality for adults with major trauma.
Methods
Criteria for considering studies for this review
Types of studies
Eligible trials include randomized controlled trials (RCTs) and nonrandomized intervention studies.
Evidence for benefit or harm of HEMS was not hypothesized to be found with RCTs because HEMS has become a highly integrated component of many trauma systems; therefore, we also evaluated nonrandomized studies (NRS), which is in accordance with guidance from The Cochrane Collaboration for including NRS (Reeves 2011). We excluded case‐control studies as they are susceptible to different types of biases than other observational studies and allocation to groups is by outcome, which introduces further bias. We did not combine evidence from RCTs with that from NRS.
As NRS cover a wide variety of fundamentally different designs, we included only studies utilizing the best available designs. Studies had to include a comparison group consisting of a GEMS group with or without a comparison via a Trauma‐Related Injury Severity Score (TRISS)‐based analysis. TRISS is a logistic regression model that compares outcomes to a large cohort of people in the Major Trauma Outcomes Study (MTOS) (Champion 1990). As first utilized by Baxt in 1983, TRISS‐based comparisons are made with a three‐step process (Baxt 1983). First, the actual mortality of people transported by HEMS is compared with TRISS‐predicted mortality. Second, the mortality of people transported by GEMS is compared with TRISS‐predicted mortality. Third, the null hypothesis that actual survival is no different than TRISS‐predicted survival is tested for the HEMS cohort versus the GEMS cohort. For non‐United States (US) TRISS‐based studies, use of the standardized W statistic was required because the M statistic for non‐US populations may be below the cutoff for nonstandardized TRISS (Schluter 2010). An M statistic of at least 0.88 is considered acceptable for comparing non‐US populations with the MTOS cohort, based on case‐mix and injury severity. A W statistic indicates the number of survivors expected per 100 people treated. We tracked non‐US TRISS‐based studies that did not report the W statistic and examined them in a subgroup analysis. We also included TRISS studies reporting the Z statistic. A Z statistic of at least 1.96 indicates a potential survival benefit when one population is compared with the MTOS cohort (Champion 1990).
We included studies if other techniques, such as regression modeling or stratification, were used to control for confounding. Each included study had to provide a description of how the groups were formed. We excluded any study that did not compare two or more groups of participants. Groups were defined based on time or location differences or by naturally occurring variations in treatment decisions. For example, some studies examined groups with different crew configurations, different equipment, or different capabilities to perform invasive interventions.
We included both prospective and retrospective NRS. If parts of a retrospective study were conducted prospectively, we only included these studies if the study was described in sufficient detail to discern this. Included studies had to describe comparability between the groups assessed. For instance, the Injury Severity Score (ISS) varied between HEMS and GEMS groups in some studies.
There are many potential confounders that may be responsible for any positive or detrimental effect of HEMS. Potential confounders included:
different types of prehospital interventions (i.e. needle thoracentesis, cricothyrotomy, rapid‐sequence endotracheal intubation);
different levels of care at the receiving trauma center (e.g. integrated trauma system versus isolated rural hospital);
varying expertise of HEMS versus GEMS providers (i.e. different crew configurations);
age, gender of participants;
injury stratification (i.e. ISS or other score);
type of traumatic injury (i.e. blunt versus penetrating trauma; isolated traumatic brain injury (TBI) versus other types of trauma);
scene transport versus interfacility transport.
Types of participants
Adults with major trauma and age 16 years or older. We included studies that had less than 10% of children but controlled for age with regression or stratification methods.
We defined major trauma by an ISS of at least 15, which has been shown to be associated with a greater need for trauma care (Baker 1976; Kane 1985). In the event that the ISS was not reported, we considered alternative scoring systems or other definitions for major trauma such as a New Injury Severity Score (NISS) of at least 15 (Osler 1997). Since any individual Abbreviated Injury Scale (AIS) of at least four will result in an ISS of at least 15, this was also used to indicate major trauma if studies only reported AIS (Wyatt 1998). We included participants reported to have sustained 'major trauma', or a similar description that was nearly equivalent to an ISS of at least 15.
Studies of burn patients are not eligible for inclusion in the review.
Types of interventions
Transport of people with major trauma by HEMS compared with transport by GEMS.
Types of outcome measures
Primary outcomes
Survival, as defined by discharge from the hospital.
Survival is the most consequential, most consignable, and least ambiguous variable used to express outcome in HEMS studies (Ringburg 2009a).
Secondary outcomes
Quality‐adjusted life years (QALYs).
Disability‐adjusted life years (DALYs).
Since the focus of this review was the evaluation of the benefits of HEMS in terms of morbidity and mortality, we did not consider economic outcomes. The financial costs and benefits associated with HEMS are complex and sufficiently important to warrant a separate study.
Search methods for identification of studies
In order to reduce publication and retrieval bias, we did not restrict our search by language, date, or publication status.
Electronic searches
We searched the following:
Cochrane Injuries Group Specialised Register (29 April 2015);
Cochrane Central Register of Controlled Trials (CENTRAL) (Issue 4 of 12, 2015);
MEDLINE (OvidSP) (1946 to April week 3 2015);
Embase Classic + Embase (OvidSP) (1947 to 29 April 2015);
CINAHL (EBSCOhost) (1982 to 29 April 2015);
ISI Web of Science: Science Citation Index Expanded (SCI‐EXPANDED) (1970 to April 2015);
ISI Web of Science: Conference Proceedings Citation Index‐Science (CPCI‐S) (1990 to April 2015);
ZETOC (accessed 29 April 2015);
OpenSIGLE (System for Information on Grey Literature in Europe) (opensigle.inist.fr/) (accessed 29 April 2015);
National Library of Medicine's Health Services Research Projects in Progress (HSRProj) (wwwcf.nlm.nih.gov/hsr_project/home_proj.cfm) (accessed 29 April 2015).
We adapted the MEDLINE search strategy, where necessary, for use in other databases. Appendix 1 provides all search strategies.
Searching other resources
We screened reference lists in all relevant material found to identify additional published and unpublished studies and performed handsearches of secondary references.
We searched the following trials registries for published and unpublished studies:
Clinicaltrials.gov (www.clinicaltrials.gov) (accessed 29 April 2015);
Controlled Trials metaRegister (www.controlled‐trials.com) (accessed 29 April 2015);
World Health Organization (WHO) Clinical Trials Registry Platform (ICTRP) (apps.who.int/trialsearch/) (accessed 29 April 2015).
Data collection and analysis
We collated the search results and merged them into a single bibliographic database. We removed duplicates before screening the titles and abstracts.
Selection of studies
Two review authors (SG and RS) examined the electronic search results in order to reject material that did not meet any of the inclusion criteria. Three review authors (SG, CS, and RS) independently screened the remaining titles and abstracts for reports of possibly relevant trials. We marked each study as 'exclude', 'include', or 'uncertain'.
One of the other three review authors cross‐reviewed all titles or abstracts classified as 'exclude' and documented the reasons for exclusion. If a title was not clearly relevant, we retrieved the full‐text version. Reasons for exclusion included studies not pertaining to traumatically injured adults, studies with nonoriginal data, single case reports, lack of a control group or description of a comparison group, or other reasons, based on the rationale described above (see Characteristics of excluded studies table).
We retrieved all titles or abstracts classified as 'include' or 'uncertain' in full and assessed them using the recommendations provided in Chapter 13 of the Cochrane Handbook for Systematic Reviews of Interventions (Reeves 2011).
We resolved disagreements by group consensus (SG, CS, RS, and ST). If further clarification was required, we attempted to contact the authors.
Data extraction and management
Three review authors (SG, CS, and RS) were each assigned one‐third of the included articles and they independently extracted information on study characteristics and the results. We resolved any uncertainty about study inclusion by group consensus. We developed, pilot tested, and used data extraction and study quality forms. Extracted data included: last name and first initial of the first author, publication year, study design, participants, duration of follow‐up, definition of participant population, data for each intervention‐outcome comparison, estimate of effect with confidence intervals (CI) and P values, key conclusions of study authors, and review author's comments. We entered data into Review Manager 5 software (RevMan 2014).
Assessment of risk of bias in included studies
Two review authors (SG and RS) planned to assess risk of bias for included RCTs. We planned to evaluate six domains: sequence generation, allocation concealment, blinding, incomplete outcome data, selective outcome reporting, and other sources of bias. The risk of bias in each category was to be judged as high risk, low risk, and unclear risk according to guidance in Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We intended to resolve any disagreements by group consensus.
For NRS not conducted entirely prospectively, we assessed risk of bias with the Downs and Black quality assessment scale (Downs 1998). This is considered an acceptable tool for evaluating NRS (Deeks 2003). The Downs and Black assessment tool has five items for evaluating risk of bias in NRS and we used all five subscales. The total number of points for each subscale was 11 for reporting bias, 3 for external validity, 7 for internal validity, 6 for internal validity confounding and selection bias, and 5 for power. Thresholds were established to define 'low', 'unclear', and 'high' levels of bias. Scores met the definition for a 'low' risk of bias if the scores were: at least 8/11 for reporting bias, 3/3 for external validity, at least 5/7 for internal validity, at least 5/6 for internal validity confounding and selection bias, and at least 4/5 for power. Studies were at 'high' risk of bias if the scores were: 6/11 or less for reporting bias, 1/3 or less for external validity, 4/7 or less for internal validity, 3/6 or less for internal validity confounding and selection bias, and 2/5 or less for power. Scores between the 'low' and 'high' bias thresholds were scored as 'unclear'.
Measures of treatment effect
For the dichotomous outcome of mortality, we calculated summary risk ratios (RR) or log RRs using the generic inverse‐variance method, but only if the included studies had similar design features. For the continuous secondary outcomes (QALYs and DALYs), we planned to calculate mean differences (MD); however, no studies reporting these outcomes were found.
Unit of analysis issues
The unit of analysis was the individual participant.
Dealing with missing data
We attempted to contact the authors of included studies to request missing data. If the authors did not respond, we considered the data missing.
Assessment of heterogeneity
We explored possible sources of heterogeneity between studies, and constructed a forest plot. We assessed the forest plot visually for heterogeneity by examining overlap of CIs. We calculated an I2 statistic to determine the proportion of variation due to heterogeneity; we considered a value greater than 50% as an indicator of significant statistical heterogeneity and a value greater than 90% as an indicator of considerable heterogeneity. We also calculated a Chi2 statistic for heterogeneity, with a P value < 0.05 suggestive of significant heterogeneity.
Assessment of reporting biases
We generated a funnel plot and examined it visually to assess for potential publication bias. We anticipated difficulty in showing that all relevant studies could be identified because of poor indexing and inconsistent use of design labels by HEMS researchers. We read full papers to determine eligibility of studies that came into question.
Data synthesis
We presented a narrative synthesis of our review by summarizing the design characteristics, risk of bias, and results of the included studies. We commented extensively on how each study design or quality attribute affected the quantitative result. We discussed potential sources of bias in our review, in addition to our methods used to control for these potential biases.
We hypothesized that several factors relating to different study designs may have an important effect on the results from individual studies. We anticipated that some studies may have used a TRISS‐based analysis, which is based on a population from the MTOS, as a control group. The TRISS analysis, which is used extensively in trauma research, is the most commonly used tool for benchmarking trauma outcomes but the coefficients have not been updated since 2010 (Schluter 2010). TRISS is a weighted combination of participant age, ISS, and Revised Trauma Score (RTS), and was developed to predict a person's probability of survival (Ps) after sustaining a traumatic injury. As trauma care may have improved over time, the data from which the original coefficients were derived may not reflect present day survival. Furthermore, TRISS‐based studies may not be wholly representative of all trauma injury populations (Champion 1990). We considered these limitations in all of our interpretations and analyses of TRISS‐based studies. Since 1996, the Trauma Audit and Research Network in the UK has been used to collect and analyze data for people with trauma (Gabbe 2011). The developers of this trauma registry have formulated a case‐mix adjustment model that addresses some of the limitations of the TRISS model (TARN 2011). Like the TRISS, the Ps for each person can be accurately calculated using age, gender, Glasgow Coma Score (GCS), ISS, and an interaction term for age and gender (TARN 2011).
Subgroup analysis and investigation of heterogeneity
Any salutary effect of HEMS is likely to be the result of some combination of speed, crew configuration (i.e. medical expertise), and that HEMS programs are often an integral part of a comprehensive trauma system (Thomas 2003). Therefore, in our narrative review, we described salient aspects of the different studies that may have contributed to a multifactorial outcomes benefit or detriment.
To investigate the effects of the interventions more precisely, we describe the results of studies according to the methods used for analysis: 1. studies that used multivariate regression methods, 2. studies that used TRISS‐based methods, and 3. studies that used other methods for analysis. We specified a priori that we would conduct a subgroup analysis based on ISS.
Sensitivity analysis
We were able to conduct three sensitivity analyses which were specified a priori: interfacility transfers, TBI, and blunt trauma.
Results
Description of studies
See Characteristics of included studies table.
We scored each study according to the five domains of the Downs and Black risk of bias assessment tool (Downs 1998). Domain scores for each study are reported as the numerator in the risk of bias tables, with the denominator representing the maximum score for each domain.
Results of the search
See Figure 2.
2.
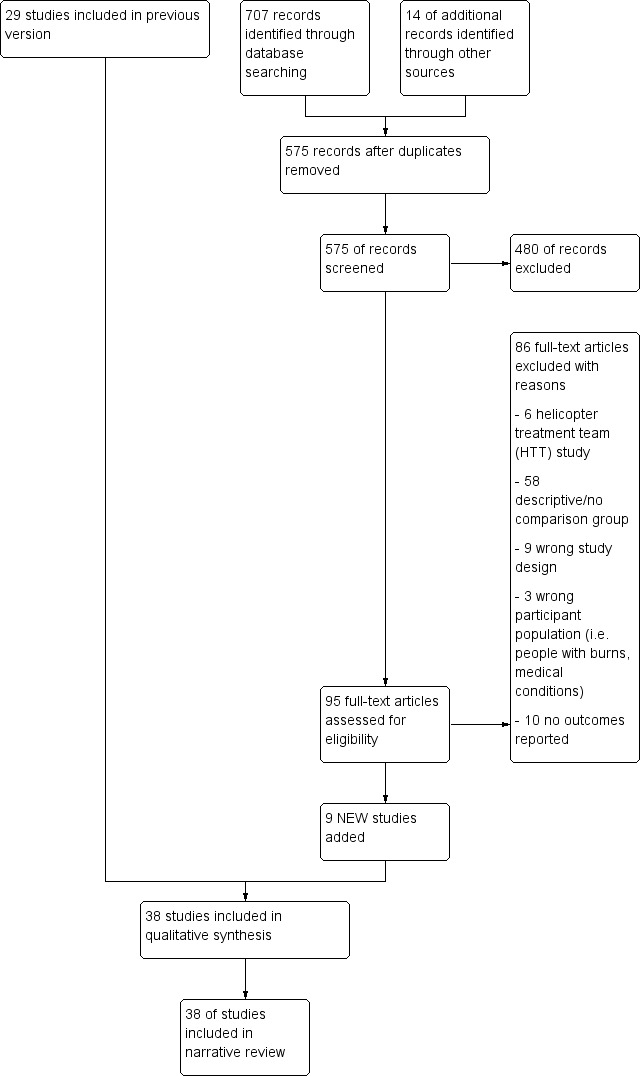
Study flow diagram.
Thirty‐eight studies met the entry criteria for this review.
Included studies
All studies were NRS; we found no RCTS. The methods of analysis used in each study are summarised in Table 2. Nineteen studies included in the primary analysis used logistic regression to control for known confounders (Abe 2014; Andruskow 2013; Braithwaite 1998; Brown 2010; Bulger 2012; Cunningham 1997; Desmettre 2012; Frey 1999; Galvagno 2012; Giannakopoulus 2013; Koury 1998; Newgard 2010; Ryb 2013; Schwartz 1990; Stewart 2011; Sullivent 2011; Talving 2009; Thomas 2002; von Recklinghausen 2011). Eight studies in the primary analysis used TRISS methods (Andruskow 2013; Biewener 2004; Buntman 2002; Frink 2007; Giannakopoulus 2013; Nicholl 1995; Phillips 1999; Schwartz 1990). Two studies did not use TRISS methods or regression but relied on stratification to control for confounding factors (Nardi 1994; Weninger 2005). In Nardi 1994, all participants had an ISS of at least 15, and only data from people transported by HEMS and GEMS to level I centers were used. Weninger 2005 used extensive stratification by physiologic parameters such as blood pressure, heart rate, respiratory rate, oxygen saturation, and AIS to evaluate people transported by HEMS and GEMS.
1. Method of analysis used in the included studies.
| Number | Study Name | Data included in analysis 1.1.1 | Regression used | TRISS‐based method | Other analysis method used |
| 1 | Abe 2014 | X | X | ||
| 2 | Andruskow 2013 | X | X | X | |
| 3 | Bartolacci 1998 | X | X | ||
| 4 | Baxt 1983 | X | X | ||
| 5 | Baxt 1987 | X | X | ||
| 6 | Berlot 2009 | X | X | ||
| 7 | Biewener 2004 | X | X | ||
| 8 | Braithwaite 1998 | X | |||
| 9 | Brown 2010 | X | |||
| 10 | Brown 2011 | X | |||
| 11 | Bulger 2012 | X | X | ||
| 12 | Buntman 2002 | X | X | ||
| 13 | Cunningham 1997 | X | X | ||
| 14 | Davis 2005 | X | X | ||
| 15 | Desmettre 2012 | X | X | ||
| 16 | Di Bartolomeo 2001 | X | X | ||
| 17 | Frey 1999 | X | |||
| 18 | Frink 2007 | X | X | ||
| 19 | Galvagno 2012 | X | X | ||
| 20 | Giannakopoulus 2013 | X | X | X | |
| 21 | Koury 1998 | X | X | ||
| 22 | McVey 2010 | X | |||
| 23 | Mitchell 2007 | X | |||
| 24 | Moylan 1988 | X | |||
| 25 | Nardi 1994 | X | X | ||
| 26 | Newgard 2010 | X | |||
| 27 | Nicholl 1995 | X | X | ||
| 28 | Phillips 1999 | X | X | ||
| 29 | Rose 2012 | X | X | ||
| 30 | Ryb 2013 | X | |||
| 31 | Schiller 1988 | X | X | ||
| 32 | Schwartz 1990 | X | X | ||
| 33 | Stewart 2011 | X | X | ||
| 34 | Sullivent 2011 | X | X | ||
| 35 | Talving 2009 | X | X | ||
| 36 | Thomas 2002 | X | X | ||
| 37 | von Recklinghausen 2011 | X | X | ||
| 38 | Weninger 2005 | X | X |
We evaluated studies examining HEMS versus GEMS for blunt trauma or TBI separately in preplanned sensitivity analyses. Four studies examined outcomes for people sustaining blunt trauma (Bartolacci 1998; Baxt 1983; Desmettre 2012; Thomas 2002). Of the four blunt trauma studies, two used TRISS‐based methods (Bartolacci 1998; Baxt 1983) and two used logistic regression (Desmettre 2012; Thomas 2002). Six studies focused on TBI (Baxt 1987; Berlot 2009; Bulger 2012; Davis 2005; Di Bartolomeo 2001; Schiller 1988). Of these six studies, two were TRISS‐based (Baxt 1987; Di Bartolomeo 2001), two used logistic regression (Bulger 2012; Davis 2005), and two reported unadjusted mortality without stratification (Berlot 2009; Schiller 1988).
Four studies examining the role of people transferred by HEMS versus GEMS met the inclusion criteria for a sensitivity analysis that was planned a priori (Brown 2011; McVey 2010; Mitchell 2007; Moylan 1988). One transfer study used logistic regression (Brown 2011), and two used TRISS‐based methods (McVey 2010; Mitchell 2007). Another transfer study stratified people according to trauma score (Moylan 1988).
Excluded studies
See Characteristics of excluded studies table.
Several HEMS studies examined the effect of physician‐based helicopter treatment teams (HTTs). HTTs, used extensively in European systems in Germany and the Netherlands, rarely transport the person in the helicopter and we excluded these studies since the main objective of this review was to determine the effect of HEMS versus GEMS transport for traumatically injured adults. Only one study examined people with burns, and we excluded this study. Some studies used TRISS to compare the outcomes of people transported by HEMS with the MTOS cohort, but not GEMS, and we excluded these studies since they violated the TRISS methods for comparing HEMS with GEMS as originally described by Baxt 1983. Figure 2 describes additional study exclusions.
Risk of bias in included studies
3.
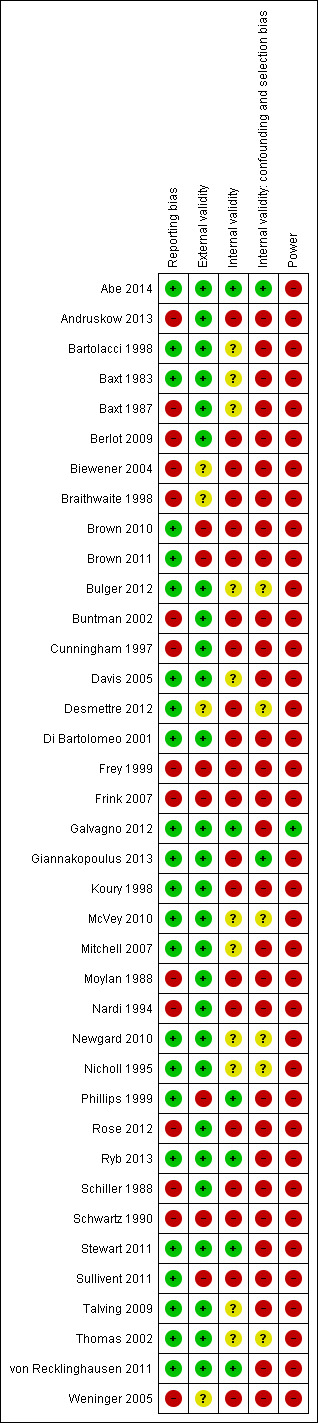
Risk of bias summary: review authors' judgments about each risk of bias item for each included study.
1.
Risk of bias graph: review authors' judgments about each risk of bias item presented as percentages across all included studies. Thirty‐eight studies are included in this review.
We assessed risk of bias with the Downs and Black assessment tool (Downs 1998). The highest possible score for this instrument is 32. The mean overall quality score for all included studies was 15.9 (range 6 to 27). Overall, the majority of studies were of low methodologic quality and no study had an overall 'low' risk of bias. Only two studies included a valid power calculation (Galvagno 2012; Thomas 2002). Thirteen studies (34.2%) had an overall quality score of at least 19 (Abe 2014; Bulger 2012; Davis 2005; Desmettre 2012; Di Bartolomeo 2001; Galvagno 2012; Giannakopoulus 2013; Newgard 2010; Nicholl 1995; Ryb 2013; Stewart 2011; Thomas 2002; von Recklinghausen 2011).
Allocation
All studies had an unclear or high level of selection bias. This was not a surprising finding considering the nature of the included studies; selection bias is an inherent risk of NRS.
One potential source of selection bias was injury severity; not all studies used ISS of at least 15 as an inclusion criterion, and some studies used other measures of injury severity. In Phillips 1999, participants were stratified by probability of survival (Ps) rather than ISS and, therefore, we only included people with a Ps less than 50% in our review. The study by Talving 2009 consisted of a participant population that had an ISS less than 15 in 74% of individuals; we only used data from the subgroup in this study with an ISS of at least 15. In Cunningham 1997, the mean ISS was lower than 15 in the GEMS group, but participants were stratified by ISS and logistic regression was used to adjust for differences in injury severity. Although ISS was not used in Moylan 1988, we included this study because participants were stratified by trauma score, and the mean trauma score was 8.7 for people transported by HEMS and 9.2 for people transported by GEMS (P value not reported).
Most studies attempted to control for confounding. Of the 28 studies in the primary analysis, including the four transfer studies in the prespecified sensitivity analysis, 14 studies (50%) used multivariable logistic regression. Only six studies reported regression diagnostics to ensure that the regression model was specified correctly (Abe 2014; Desmettre 2012; Galvagno 2012; Newgard 2010; Sullivent 2011; Thomas 2002). Four studies used advanced regression techniques including propensity scores (Abe 2014; Davis 2005; Galvagno 2012; Stewart 2011), instrumental variables (Newgard 2010), and techniques to control for clustering by trauma center (Thomas 2002).
Fourteen studies relied on a TRISS‐based analysis to compare both HEMS and GEMS outcomes against the MTOS cohort; however, TRISS‐based statistics were not reported consistently. The validity of TRISS methods has been questioned because the MTOS was established over two decades ago (Champion 1990), and changes in injury prevention and trauma care may preclude valid comparisons over time. Participants in the MTOS might have had a worse prognosis or different injury severity than contemporary trauma participants. To adjust for these potential differences, investigators using TRISS are encouraged to report an M statistic to ensure that severity and case‐mix is comparable (Schluter 2010). Only one study included in this review reported an M statistic (Buntman 2002). Eight TRISS studies were published after 2000 and it is possible that these populations might have differed significantly from the original MTOS cohort (Andruskow 2013; Biewener 2004; Buntman 2002; Di Bartolomeo 2001; Frink 2007; Giannakopoulus 2013; McVey 2010; Mitchell 2007). Di Bartolomeo 2001 attempted to control for case‐mix differences by comparing participants with an Italian MTOS cohort. Four studies reported the W statistic (Bartolacci 1998; Di Bartolomeo 2001; McVey 2010; Mitchell 2007). Five studies reported a Z statistic (Baxt 1983; Biewener 2004; Giannakopoulus 2013; Phillips 1999; Schwartz 1990), and four studies did not formally report any TRISS statistics (Andruskow 2013; Baxt 1987; Frink 2007; Nicholl 1995).
Crew configuration varied widely between studies and this may have had an effect on mortality since people transported by HEMS or GEMS might have been preferentially exposed to potential life‐saving interventions. For example, in one of the earliest and best‐known HEMS studies, Baxt 1983 reported a 52% reduction in mortality for the HEMS group. In this study, the HEMS crews consisted of an acute care physician who could perform advanced airway interventions, while the prehospital interventions authorized for the GEMS group were limited to advanced first aid and placement of an esophageal obturator airway. HEMS and GEMS crew configurations were not described in all studies and fewer than half of all studies included in the primary analysis described the type and frequency of prehospital interventions. The Characteristics of included studies table describes the crew configurations for the studies that provided this information. Sixteen studies included in the primary analysis had physicians as part of the HEMS crew (Abe 2014; Andruskow 2013; Bartolacci 1998; Baxt 1983; Baxt 1987; Berlot 2009; Davis 2005; Desmettre 2012; Di Bartolomeo 2001; Frink 2007; Giannakopoulus 2013; Nardi 1994; Nicholl 1995; Schwartz 1990; Thomas 2002; Weninger 2005). Twelve studies did not describe the crew configuration for HEMS or GEMS (Biewener 2004; Brown 2010; Bulger 2012; Cunningham 1997; Frey 1999; Galvagno 2012; Newgard 2010; Rose 2012; Ryb 2013; Schiller 1988; Stewart 2011; Sullivent 2011). Fourteen studies described the frequency and types of prehospital interventions performed between the HEMS and GEMS groups (Abe 2014; Andruskow 2013; Bartolacci 1998; Berlot 2009; Biewener 2004; Bulger 2012; Davis 2005; Desmettre 2012; Di Bartolomeo 2001; Giannakopoulus 2013; Nardi 1994; Phillips 1999; Schwartz 1990; Weninger 2005), whereas two studies only described the frequency of endotracheal intubation (Stewart 2011; Talving 2009).
Blinding
None of the included studies attempted to blind study participants to the intervention of HEMS versus GEMS. None of the included studies made an attempt to blind those measuring the main outcome of the intervention (HEMS versus GEMS). This resulted in either an 'unclear' or 'high' degree of bias, indicating poor levels of internal validity, for over 90% of the included studies. Detection bias was possible in the majority of included studies due to the retrospective nature of the study designs and because for people with an ISS of at least 15 mortality is more likely. It is also possible that deaths were recorded more frequently in the trauma registries that served as a primary source of data for most of the included studies. Survivors lost to follow‐up might not have been captured in the registries, biasing the results. Furthermore, mortality definitions differed among studies. Thirty‐day mortality may be different from 60‐day mortality, and this outcome is often difficult to assess. Most studies did not provide information on duration of follow‐up.
Incomplete outcome data
We did not include studies with incomplete outcome data in this review; however, attrition bias could not be accurately assessed due to the retrospective nature of the study designs. None of the studies adjusted the analyses for different lengths of follow‐up, and it is possible that not all outcomes were available. Losses to participant follow‐up were not taken into account in any of the included studies and this explains why over 80% of included studies were at high risk of bias in terms of internal validity. For the unadjusted analysis (Analysis 1.1), data were available for 28 of the 38 studies in the primary analysis.
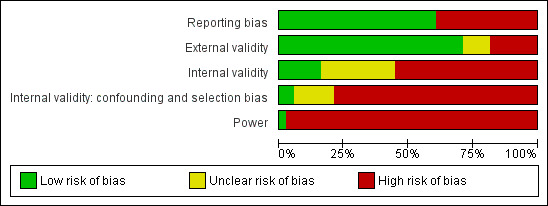
1.1. Analysis.
Comparison 1 Helicopter emergency medical services (HEMS) transport compared with ground emergency medical services (GEMS), Outcome 1 Unadjusted mortality.
Selective reporting
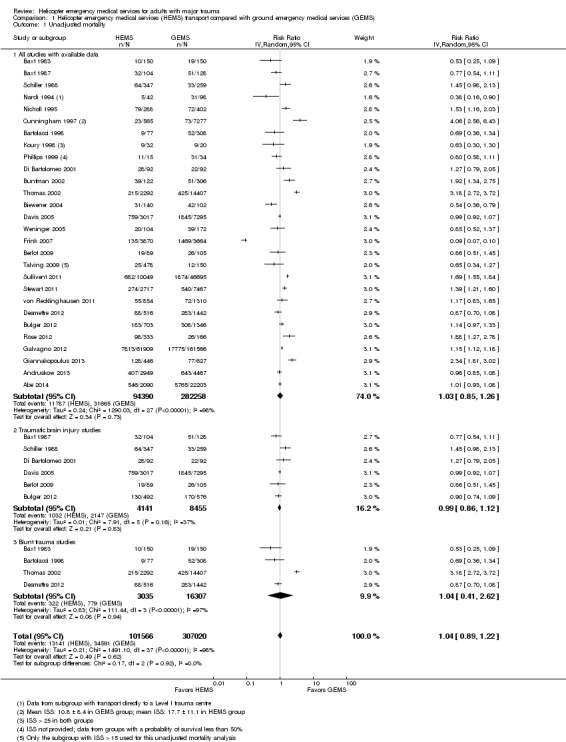
None of the studies fully controlled for all known confounders; 50% of all included studies had a low level of reporting bias and the remaining 50% had a high level of reporting bias. We assessed publication bias with a funnel plot (Figure 4). Trials were seen both to the right and left of the point of no effect, with no trials clustered around the line indicating no difference. There was an empty zone in the lower right quadrant of the plot. Therefore, it is possible that publication bias was present. This result might also be explained by the considerable clinical heterogeneity among the included studies. It is possible that smaller studies with results that were not statistically significant were never published.
4.
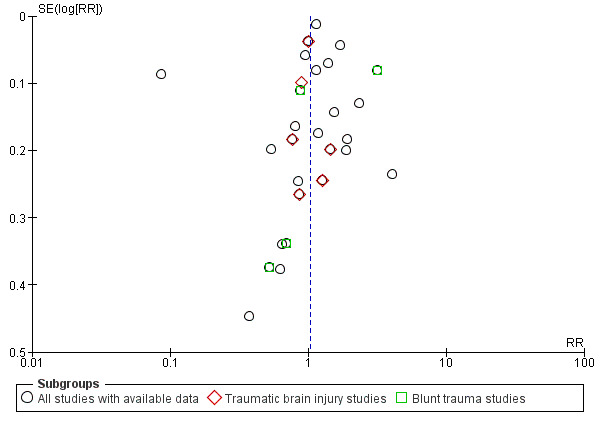
Funnel plot of comparison: helicopter emergency medical services (HEMS) versus ground emergency medical services (GEMS), outcome: 1.1 Overall unadjusted mortality.
Other potential sources of bias
Eleven studies had a minority of children included in the groups; however, the mean age in all of these studies was reported to be greater than 25 years. One study had 74% of people with an ISS less than 15 (Talving 2009); we included only the results from the subgroup with an ISS at least 15.
Effect estimates, and associated CIs in studies using regression techniques, might be inaccurate based on the availability of the data used to specify the regression model. For instance, five studies use the National Trauma Data Bank (USA) (Brown 2010; Brown 2011; Galvagno 2012; Ryb 2013; Sullivent 2011), and this data source is known to have a high proportion of missing data, especially for the physiological variables that the authors included as covariates (Roudsari 2008).
Effects of interventions
See: Table 1
Summary of findings for the main comparison. Helicopter emergency medical services compared with ground emergency medical services for adults with major trauma.
| Helicopter emergency medical services compared with ground emergency medical services for adults with major trauma | ||||||
|
Patient or population: adults (age > 15 years) with major trauma (ISS > 15) Settings: multinational Intervention: transportation to a trauma center by HEMS Comparison: transportation to a trauma center by GEMS | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| GEMS | HEMS | |||||
| Overall unadjusted mortality | Low risk population | RR 1.03 (0.85 to 1.26) | 376,648 | ⊕⊝⊝⊝ very low | Results could not be reliably combined for meta‐analysis due to considerable heterogeneity. The relative effect calculated here reflects unadjusted mortality only for studies that reported data enabling the calculation of a risk ratio. See text and Figure 1 (Analysis 1.1) for details | |
| ‐ | ‐ | |||||
| Medium risk population | ||||||
| ‐ | ‐ | |||||
| High risk population | ||||||
| ‐ | ‐ | |||||
| Quality‐adjusted life years | ‐ | ‐ | ‐ | ‐ | ‐ | No studies examining quality‐adjusted life years as an outcome met the inclusion criteria for this review |
| Disability‐adjusted life years | ‐ | ‐ | ‐ | ‐ | ‐ | No studies examining disability‐adjusted life years as an outcome met the inclusion criteria for this review |
| Adverse events | ‐ | ‐ | ‐ | ‐ | ‐ | None of the 38 included studies reported adverse events (such as GEMS or HEMS crashes) |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; GEMS: ground emergency medical service; HEMS: helicopter emergency medical service; ISS: Injury Severity Score; RR: risk ratio. | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
See Table 1.
Primary outcome measure ‐ Survival (defined as discharge from the hospital)
Twenty‐eight of the included studies had extractable data on unadjusted mortality (Analysis 1.1). Considerable heterogeneity was observed as indicated by an I2 value of 98% and a highly statistically significant Chi2 test for heterogeneity (P value < 0.00001). Combining the results from these unequally sized and heterogeneous studies in a meta‐analysis would be likely to lead to a Yule‐Simpson effect (i.e. Simpson's paradox) and flawed conclusions. For example, when certain groups are combined without accounting for injury severity and other confounders, a correlation may be present. This correlation may disappear when the groups are stratified or when analyzed with regression techniques. Such a phenomenon appears to be evident in Analysis 1.1. Four studies that appeared to show a pronounced benefit for GEMS based on unadjusted mortality had opposite and statistically significant greater odds of survival for people transported by HEMS after adjusting for confounders with multivariable logistic regression (Galvagno 2012; Stewart 2011; Sullivent 2011; Thomas 2002) (Table 3). Another study that appeared to favor GEMS based on unadjusted mortality significantly showed no statistical difference between HEMS and GEMS after adjustment with regression (Cunningham 1997). Similarly, based on the unadjusted mortality from Buntman 2002 and Giannakopoulus 2013, one would infer that GEMS is superior to HEMS. However, after TRISS methods were applied, HEMS was shown to improve survival by 21.43% in Buntman 2002, and Giannakopoulus 2013 calculated 5.4 additional lives per 100 HEMS transports. Alternatively, several studies that appeared to support clearly HEMS based on unadjusted mortality had small sample sizes and the results from these studies might have been biased (Bartolacci 1998; Baxt 1983; Baxt 1987; Koury 1998; Nardi 1994).
2. Studies that utilized multivariate logistic regression to adjust for potential confounders.
| Study | Number of participants | Odds ratio for survival | 95% Confidence interval | P value |
| Abe 2014 | HEMS: 2090 GEMS: 22,203 |
1.23 | 1.02 to 1.49 | (3) |
| Andruskow 2013 | HEMS: 4989 GEMS: 8231 |
1.33 | 1.16 to 1.57 | (3) |
| Braithwaite 1998 | HEMS: 15,938 GEMS: 6473 |
Not reported (1) | Not reported (1) | < 0.01 (2) |
| Brown 2010 | HEMS: 41,987 GEMS: 216,400 |
1.22 | 1.18 to 1.27 | < 0.01 |
| Bulger 2012 | HEMS: 703 GEMS: 1346 |
1.11 | 0.82 to 1.74 | N.S. (3) |
| Cunningham 1997 | HEMS: 1346 GEMS: 17,144 |
Not reported (1) | Not reported (1) | (1) |
| Desmettre 2012 | HEMS: 516 GEMS: 1442 |
1.47 | 1.02 to 2.13 | 0.035 |
| Frey 1999 | HEMS: not reported GEMS: not reported |
1.34 | 0.91 to 1.8 | N.S. (3) |
| Galvagno 2012 | HEMS: 47,637 (7) GEMS: 111,874 (7) HEMS: 14,272 (8) GEMS: 111,874 (8) |
1.16 1.15 |
1.14 to 1.17 1.13 to 1.17 |
< 0.001 < 0.001 (9) |
| Giannakopoulus 2013 | HEMS: 446 GEMS: 627 |
Not reported (1) | Not reported (1) | (1) |
| Koury 1998 | HEMS: 168 GEMS: 104 |
1.6 | 0.77 to 3.34 | 0.24 |
| Newgard 2010 (4) | HEMS: 158 GEMS: 3498 |
1.41 | 0.68 to 2.94 | N.S. (3) |
| Ryb 2013 | HEMS: 29,472 GEMS: 162,950 |
1.78 | 1.65 to 1.92 | (3) |
| Schwartz 1990 | HEMS: 93 GEMS: 33 |
Not reported (1) | Not reported (1) | (1) |
| Stewart 2011 (5) | HEMS: 2739 GEMS: 6473 |
1.49 | 1.19 to 1.89 | 0.001 |
| Sullivent 2011 | HEMS: 10,049 GEMS: 46,695 |
1.64 | 1.45 to 1.87 | < 0.0001 |
| Talving 2009 (6) | HEMS: 1836 GEMS: 1537 |
1.81 | 0.55 to 5.88 | 0.33 |
| Thomas 2002 | HEMS: 2292 GEMS: 14,407 |
1.32 | 1.03 to 1.71 | 0.031 |
| von Recklinghausen 2011 | HEMS: 854 GEMS: 1310 |
1.75 1.87 |
0.86 to 4.2 (10) 0.94 to 3.66 (11) |
N.S. (3) |
GEMS: ground emergency medical service; HEMS: helicopter emergency medical service; N.S.: not significant.
(1) Effect estimate and 95% confidence interval not reported.
(2) Statistically significant effect on survival (in favor of HEMS) when HEMS analyzed as interaction between HEMS and ISS ranges of 16‐60.
(3) P value not reported.
(4) Instrumental variables analysis.
(5) Cox proportional hazards regression, including a propensity score as a confounding covariate.
(6) Adjusted odds ratio for subgroup with ISS > 15.
(7) Data for level I trauma centers.
(8) Data for level II trauma centers.
(9) Results of propensity score matching logistic regression analysis.
(10) ISS 16‐24 group, P value and n not reported.
(11) ISS 25‐75 group, P value and n not reported.
Additionally, it is important to understand that four studies did not provide raw data for calculation of unadjusted mortality, and this may have influenced the overall relative risk of unadjusted mortality (Brown 2010; Frey 1999; Newgard 2010; Schwartz 1990). Three of these studies were regression‐based and all three indicated a statistically significantly improved odds of survival (Brown 2010; Frey 1999; Newgard 2010). Schwartz 1990 used a TRISS analysis to demonstrate an improvement in predicted survival for HEMS but not GEMS, a finding that was contrary to the results from an unadjusted analysis; a similar result was observed in a more recent study by Giannakopoulus 2013. Due to the considerable clinical and methodological heterogeneity found in the included studies, a pooled estimate of effect is not presented.
Subgroup analyses
To investigate the effects of the interventions more precisely, we describe the results of studies according to the methods used for analysis: 1. studies that used multivariate regression methods, 2. studies that used TRISS‐based methods, and 3. studies that used other methods for analysis.
1. Studies that used multivariate regression methods
Nineteen studies used multivariate regression techniques to adjust for known confounders (Abe 2014; Andruskow 2013; Braithwaite 1998; Brown 2010; Bulger 2012; Cunningham 1997; Desmettre 2012; Frey 1999; Galvagno 2012; Giannakopoulus 2013; Koury 1998; Newgard 2010; Ryb 2013; Schwartz 1990; Stewart 2011; Sullivent 2011; Talving 2009; Thomas 2002; von Recklinghausen 2011). Table 3 shows the effect estimates and 95% CIs from these 19 studies (effect estimates and CIs were not available for Cunningham 1997, Giannakopoulus 2013 and Schwartz 1990). The results from three of these studies focused exclusively on people with blunt trauma (Braithwaite 1998; Schwartz 1990; Thomas 2002), and these studies are summarized in the section below 'Sensitivity analysis, blunt trauma'. The results from Andruskow 2013 and Giannakopoulus 2013 are described in the section detailing the results from TRISS‐based studies since this was the primary analysis performed in these studies.
Abe 2014 utilized the Japan Trauma Data Bank (JTDB) to examine retrospectively 2090 HEMS transports and 22,203 GEMS transports between 2004 and 2011. The study used three different logistic regression techniques, adjusting for age, sex, type of trauma, ISS, and prehospital treatments. HEMS were staffed by a physician and nurse and GEMS were staffed by an emergency medical technician (EMT) and firefighter. In all three logistic regression models, HEMS was independently associated with statistically significantly improved survival to hospital discharge when compared with GEMS.
Brown 2010 analyzed 41,987 HEMS transports and 216,400 GEMS transports from the 2007 National Trauma Data Bank. When adjusting for ISS, age, gender, injury mechanism, vital signs, type of trauma center, and urgency of operation, HEMS was associated with a statistically significant greater odds of survival to hospital discharge (odds ratio (OR) 1.22; 95% CI 1.18 to 1.27; P value < 0.01).
Bulger 2012 and researchers from the North American Resuscitation Outcomes Consortium conducted a retrospective analysis from two RCTs that enrolled people with severe TBI or hypovolemic shock. The study analyzed 2049 people in both the shock and TBI cohorts. More people had penetrating trauma in the GEMS group (21.2%) compared with the HEMS group (6%). Mean ISS was higher in HEMS group (30.1) compared with the GEMS group (22.8; P value < 0.0001). Multivariable logistic regression, adjusting for age, mechanism, GCS, hypotension, heart rate, ISS, site of enrolment, and AIS, was used to calculate odds of 24‐hour and 28‐day survival. While the OR for overall survival was 1.11 favoring HEMS, this result was not statistically significant (95% CI 0.82 to 1.51). Nonsignificant results were found independently when the shock and TBI cohorts were analyzed separately. This study had a total number of people of 2049; yet, to detect up to a 5% survival advantage in either the HEMS or GEMS cohort, with 80% power at the 5% significance level, at least 2526 participants would have to be enrolled; a far greater number of participants would have to be enrolled to detect even smaller differences in survival. Of the 703 people transported by HEMS, 60% came from three trauma centers.
Cunningham 1997 found that HEMS was associated with statistically significant survival benefit for people with mid‐range, but not higher, acuity. People with an ISS of 21 to 30 had 56% survival in the HEMS group versus 37.4% survival in the GEMS group. For people with an ISS of 31 to 40, 80% of the HEMS group survived versus 62.8% of the GEMS group. However, for the most severely injured people with a Ps less than 90%, the HEMS group had 66.9% survival and the GEMS group had 81.9% survival.
Desmettre 2012 studied the impact of HEMS versus GEMS on mortality of people with severe blunt trauma. This French study included 1958 participants, of which 74% were transported by GEMS and 26% by HEMS. Although crew configurations both consisted of physicians, HEMS crews were staffed by a team that included an emergency physician from a regional University hospital. Multivariable logistic regression was performed, controlling for several prehospital physiologic and injury‐specific variables. Interaction terms between mode of transport and other independent variables were assessed in the regression model. People treated by HEMS crews were more likely to be treated aggressively with interventions such as endotracheal intubation, administration of fluids, treatment with vasopressors, and blood product transfusion. After adjustment, the risk for survival was greater in the HEMS group (OR 1.47; 95% CI 1.02 to 2.13; P value = 0.035).
Frey 1999 reported in an abstract on 12,233 people involved in motor vehicle crashes admitted to trauma centers in Pennsylvania, PA, USA. There was no difference in survival between transport by HEMS or GEMS (OR 1.34; 95% CI 0.91 to 1.80; P value not reported). Reasons for a lack of statistical significance may be due to residual confounding, transport of people with lower severity trauma, and the fact that this study included only people involved in motor vehicle crashes. Recent advances in vehicle safety may partially explain why no benefit was found when HEMS was compared with GEMS.
Galvagno 2012 used the National Trauma Data Bank to analyze 223,475 people transported by HEMS or GEMS to a level I or level II trauma center. Outcomes were assessed with multiple regression methods. After a propensity score matching was used in a logistic regression, and after outcomes were assessed in an analysis stratified by type of trauma center, people transported by HEMS were statistically significantly more likely to survive to hospital discharge compared with people transported by GEMS. The effect estimate (OR) was more conservative after propensity score matching as compared with two standard logistic regression and an analysis using generalized estimating equations (GEE) to control for clustering by trauma center. The study did not account for crew expertise, distance, time, and prehospital interventions.
A retrospective cohort study by Koury 1998 found no difference in survival in people with an ISS of at least 25 and transported by HEMS (OR 1.6; 95% CI 0.77 to 3.34; P value = 0.24). This study controlled for confounding factors such as age, type of trauma, ISS, hospital length of stay, and length of emergency room stay. This study also included some children (14% to 16.7%) and interfacility transfers, although these factors were adjusted for in the regression model. The relatively small number of participants in Koury et al (n = 272) may explain the wide CI for the effect estimate. Moreover, a higher ISS cutoff was used (≥ 25) and the authors acknowledged that the study was likely to be underpowered to find a difference between HEMS and GEMS.
Newgard 2010 conducted a secondary analysis of a prospective cohort registry study of adults with trauma transported by 146 emergency medical service (EMS) agencies to 51 level I and II trauma centers in North America. A multivariate regression model using instrumental variables was used to study the association of EMS intervals and mortality among people with trauma with field‐based physiologic abnormalities, using distance from a trauma center as the instrument. There was no difference in survival with the use of HEMS (OR 1.41; 95% CI 0.68 to 2.94; P value not reported) in the multivariate model. The primary objective of this study was to test the association of EMS intervals and mortality among people with trauma (e.g. the 'golden hour' concept) and HEMS was only analyzed as one independent variable that might have influenced outcome.
Ryb 2013 used data from 2007 available in the National Trauma Data Bank to examine the effect of HEMS on trauma survival across different subpopulations of people with trauma in relation to injury severity, degree of physiologic derangement, and transport time. The study analyzed 192,422 people with complete data. Using multiple logistic regression models adjusting for ISS, levels of physiologic derangement, and different transport times, HEMS was statistically significantly associated with improved survival (OR 1.78; 95% CI 1.65 to 1.92). When stratified by RTS as a marker of physiologic instability, people transported by HEMS with worse scores had significantly higher adjusted odds of survival. The limitations of the National Trauma Data Bank must be considered when interpreting the results from this study (see Other potential sources of bias).
Stewart 2011 calculated a propensity score based on prehospital variables (age, gender, mechanism of injury, respiratory rate, anatomic triage criteria, intubation, level of prehospital care, and road distance to a trauma center) and hospital variables (RTS on arrival at emergency room, ISS, time from receipt of EMS call to arrival at emergency room, time in minutes from receipt of the first EMS call to time of death). This study included 10,184 people in the state of Oklahoma, USA who were admitted to one level I trauma center or one of two level II trauma centers. The propensity score was used as a single confounding covariate in a Cox multivariable proportional hazards regression model to determine the association between mode of transport and mortality. Overall, people transported by HEMS had a statistically significantly higher HR for survival compared with people transported by GEMS (HR for improved survival 1.49; 95% CI 1.19 to 1.89; P value = 0.001). In the most severely injured people (RTS of 3 or less at the scene), the mode of transport was not associated with improved survival.
Sullivent 2011 used multivariate logistic regression to examine the association between mortality and transportation between HEMS and GEMS. The 2007 National Trauma Data Bank was used for this study, with 148,270 records of people treated at 82 participating trauma centers in the USA. The authors stratified the regression analysis results by three age categories: 18 years and over, 18 to 54 years, and 55 years and over. Overall, HEMS transport conferred a statistically significant mortality benefit (OR 1.64; 95% CI 1.45 to 1.87; P value < 0.0001), although in the age category 55 years and over, there was no difference in survival between HEMS and GEMS (OR 1.08; 95% CI 0.88 to 1.75; P value = 0.42).
Talving 2009 retrospectively examined data for 1836 people transported by HEMS or GEMS in a predominantly urban environment. In the subgroup of people with an ISS of at least 15, there was no difference in survival between people transported by HEMS or GEMS (OR 1.81; 95% CI 0.55 to 5.88; P value = 0.33). An analysis of four high‐risk subgroups was conducted in this study. People with ISS of at least 15, penetrating trauma, a head AIS of at least 4, or systolic blood pressure less than 90 mmHg did not experience a statistically significantly benefit from HEMS transport in a multivariable analysis adjusting for age, vital signs, injury mechanism, and injury severity. The lack of benefit in this study may be due to the geographical location of the HEMS program that was studied. The region serviced by HEMS was predominantly urban and HEMS was used when transport times exceeded 30 minutes. Thirty minutes may not be a clinically important cutoff to justify HEMS use, and patient over‐triage was likely in this study.
von Recklinghausen 2011 compared rural GEMS and HEMS in a retrospective cohort of 2164 participants at one level I trauma center in the northeastern USA. There was no difference in survival among people transported by HEMS or GEMS with ISS scores of 16 to 24 (OR 1.75; 95% CI 0.86 to 4.2). Among people with ISS of 25 to 75, there was also no difference in survival (OR 1.87; 95% CI 0.94 to 3.66). Information about crew expertise and en route interventions was not available. With a low mortality in both the HEMS (6.46%) and GEMS group (5.5%; P value = 0.35), the study was not likely powered to find a statistically significant difference in survival.
2. Studies that used Trauma‐Related Injury Severity Score‐based methods
Fourteen studies used TRISS‐based methods to compare survival for HEMS versus GEMS against the standard of the MTOS cohort (Andruskow 2013; Bartolacci 1998; Baxt 1983; Biewener 2004; Buntman 2002; Frink 2007; Giannakopoulus 2013; Nicholl 1995; Phillips 1999; Schwartz 1990).
In Andruskow 2013, outcomes from physician‐led HEMS and GEMS teams were compared using TRISS methodology. People transported by HEMS had higher ISS compared with people transported by GEMS (26.0 with HEMS versus 23.7 with GEMS; P value < 0.001). The people in the HEMS group were also treated more aggressively with more frequent endotracheal intubation, chest thoracostomy tube placement, and treatment with vasopressors. Predicted mortality according to TRISS was lower in both HEMS and GEMS groups. For people transported to level I trauma centers, the standardized mortality ratio (SMR) was significantly decreased in the HEMS group compared with the GEMS group (0.647 with HEMS versus 0.815 with GEMS; P value = 0.002). The authors performed a multivariable regression analysis and found an improved odds of survival for the HEMS group compared with the GEMS group when 11 confounding variables were included in the regression model (OR for survival in HEMS group: 1.33; 95% CI 1.16 to 1.57). The study reported neither the M or W statistics.
The results from Bartolacci 1998 are discussed in the preceding section ('Studies that used multivariate regression methods'). There was a significant difference between observed and expected survivors for people transported by HEMS (Z = 3.38; P value < 0.0001). The W statistic reported in this study was 11.88, which suggests nearly 12 expected survivors for every 100 people flown; but the M statistic was 0.52, which is less than the acceptable 0.88 threshold for comparing populations (Schluter 2010). The nonsignificant M statistic indicated that there was a higher proportion of people with a low Ps in the HEMS group compared with the MTOS cohort.
Baxt 1983 studied 300 consecutive HEMS and GEMS transports to a level I trauma center over a 30‐month period. Although the actual Z statistic was not reported, a 52% reduction in predicted mortality occurred in the HEMS group (P value < 0.001). Overall, 20.62 people were predicted to die in the HEMS group based on a comparison with the MTOS cohort, but only 10 people died. In the GEMS group, 14.79 people were predicted to die but 19 died. Major improvements in survival were most pronounced for the more seriously injured participant groups. For people with a 24% or less chance of survival, four people transported by HEMS died when 7.03 were predicted to die; in the GEMS group, six people died when 7.03 were predicted to die.
Biewener 2004 assessed the impact of rural HEMS versus urban GEMS in 403 people with trauma in the Dresden region in Germany. The study used TRISS‐based methods only to compare HEMS versus GEMS for people transported directly from the scene to a level I trauma center. No TRISS statistics were reported. In the HEMS groups, the TRISS analysis identified 27 unexpected survivors and four unexpected deaths out of the 140 people transported. In the GEMS group there were 13 unexpected survivors and two unexpected deaths from the people transported. The TRISS evaluation did not identify any differences between the HEMS and GEMS groups in terms of survival. In a multivariate regression model, there was also no difference in survival (OR 0.94; 95% CI 0.38 to 2.34; P value not reported).
Buntman 2002 reported the results from a prospective database analysis of 428 people transported by HEMS and GEMS in South Africa. Survival rates in the HEMS and GEMS groups were compared with TRISS‐predicted survival rates, and people with a Ps less than 65% were more likely to survive if transported by HEMS. Overall, 38.15 people in the HEMS group were expected to die and 39 actually died (Z = 0.223), and 38.96 people in the GEMS group were predicted to die and 51 actually died (Z = 2.939). The difference in the Z statistic between the HEMS and GEMS groups was 1.921 (P value < 0.05) indicating a greater chance for survival in the HEMS group than the GEMS group. It should be noted that the M statistic reported in this study was 0.618 for the HEMS group and 0.867 for the GEMS group; both groups did not meet the threshold for accurate comparison to the MTOS cohort.
Frink 2007 retrospectively evaluated 7534 people transported by HEMS and GEMS in Germany and used a TRISS prediction of survival to demonstrate a survival benefit for people transported by HEMS, though no specific TRISS statistics were reported in this study. Overall mortality was 34.9% in the HEMS group versus 40.1% in the GEMS group (P value < 0.01), but this difference was only found in people with an ISS less than 61.
Giannakopoulus 2013 analyzed 1073 people with an ISS of at least 16 and transported directly from the scene by HEMS or GEMS. HEMS crews consisted of a physician capable of providing advanced airway management and limited surgical interventions. The study did not describe the configuration of the GEMS crew. There was a longer on‐scene time in the HEMS group compared with the GEMS group (27.1 minutes with HEMS versus 20.7 minutes with GEMS, P value < 0.001), and the HEMS population was younger (mean age: 40.5 with HEMS versus 49.3 with GEMS; P value < 0.001). There was no significant difference in the types of injuries. Unadjusted analysis indicated a higher mortality in the HEMS group (28.7% with HEMS versus 12.3% with GEMS, P value < 0.001). However, people in the HEMS group had a significantly higher ISS. The M statistic showed that the population in this study was not comparable to the original TRISS MTOS population, likely because of the higher ISS (> 16) used as an inclusion criteria for this study. The Z statistic showed a positive difference between the observed and the estimated survival for the HEMS group (P value < 0.005) indicating that the actual survival for the HEMS group was higher than predicted by TRISS; there was no difference in the predicted and the actual survival in the GEMS group. When the RTS reached 9 or less, the difference in survival between the groups increased, demonstrating an increased chance of survival for people transported by HEMS. The authors concluded that 5.4 people with multiple traumatic injuries were saved for every 100 HEMS deployments.
Nicholl 1995 compared 337 people transported by HEMS and 466 people transported by GEMS in the UK using the TRISS methodology. The number of HEMS deaths exceeded the MTOS norms by 15.6%, compared with an excess of 2.4% in the GEMS group. No TRISS‐specific statistics were reported and overall mortality for people with an ISS of at least 15 was 51% in the HEMS group and 44% in the GEMS group (not statistically significant, P value not reported). There was no difference in survival between people transported by HEMS compared with GEMS, who had an ISS of 16 to 24 (OR for improved survival 1.25; 95% CI 0.44 to 3.33) or an ISS of 25 to 40 (OR for improved survival 1.11; 95% CI 0.83 to 1.43). In both of these ISS groups, there were fewer than 60 people in each group, thus the wide CIs are likely due to the relatively small number of people within each subgroup.
Phillips 1999 used the TRISS methodology to compare mortality rates of 792 people with trauma transported by HEMS or GEMS in Texas, USA. The Z statistic was not significant for actual versus predicted deaths for HEMS (Z = 0.40) or GEMS (Z = 0.151). The HEMS group sustained 15 deaths compared with a TRISS‐predicted rate of 16.44 deaths; the GEMS group sustained 41 deaths compared with a TRISS‐predicted rate of 39.11 deaths; neither result was statistically significant.
Schwartz 1990 reported on a series of people with blunt trauma transported by HEMS or GEMS to a single level I trauma center in Connecticut, USA, during 1987 and 1988. This study used TRISS methodology, but did not report W, Z, and M statistics. HEMS crews were comprised of highly trained providers, including a physician, nurse, and respiratory therapist, while GEMS crews were comprised of an EMT and paramedic. People transported by HEMS had a Ps of 2.23 standard deviations better than the national norm, while people transported by GEMS had a survival ‐2.69 standard deviations below the national norm. More people in the HEMS group were intubated (42% with HEMS versus 3% with GEMS) and more people in the HEMS group were treated with a pneumatic antishock garment (56% with HEMS versus 30% with GEMS). There was no significant difference in the prehospital times for either HEMS or GEMS once crews had arrived at the scene.
3. Studies using other methods to adjust for confounding
Three additional studies that did not use regression techniques or a TRISS‐based analysis met the inclusion criteria (Nardi 1994; Rose 2012; Weninger 2005).
The results from Nardi 1994 are summarized in the 'Blunt trauma studies' section. This study did not utilize TRISS‐based methods or regression techniques.
In Weninger 2005, people transported by HEMS and by GEMS were similar in age, sex, and injury severity. People in the HEMS group had more frequent administration of intravenous fluids, endotracheal intubation, and chest tube placement than people in the GEMS group. Twenty of 104 (19.2%) people transported by HEMS died (19.2%) versus 39 of 172 (22.7%) people transported by GEMS (P value not reported).
Rose 2012 performed a stratified analysis of 1028 HEMS and 1443 GEMS transports in Alabama, USA. The mode of transport was stratified only by ISS and mean miles to a trauma center. HEMS did not improve survival for people with high ISS (> 30) or in people with lower ISS (< 10) transported from rural areas. The study made no adjustments for crew expertise, prehospital interventions, types of injuries, physiologic data, or other variables. This study was limited by considerable low methodological quality, and did not employ descriptive statistics for between‐group comparisons.
Sensitivity analyses
1. Traumatic brain injury studies
Five studies focused on the role of HEMS versus GEMS transport for TBI (Baxt 1987; Berlot 2009; Davis 2005; Di Bartolomeo 2001; Schiller 1988). These studies analyzed 11,528 people and data were available from all five studies to calculate unadjusted mortality. There was moderate heterogeneity in this subgroup (Chi2 = 6.80; I2 = 41%). Based on the raw mortality data from these five trials, there was no association with improved survival (RR 1.02 in favor of HEMS; 95% CI 0.85 to 1.23).
Davis 2005 studied 10,314 people transported by HEMS or GEMS. They used propensity scores to account for the variability in selection of people undergoing HEMS versus GEMS transport and used a multivariate regression model to adjust for age, sex, mechanism of injury, hypotension, GCS, AIS, and ISS. There was an improved odds of survival for people transported by HEMS after adjustment for potential confounders (OR 1.90; 95% CI 1.60 to 2.25; P value < 0.0001). When stratified by GCS, there was a statistically significant survival benefit observed only for the GCS group with a score of 3 to 8 (OR 1.84; 95% CI 1.51 to 2.23; P value < 0.001).
Di Bartolomeo 2001 utilized a population‐based, prospective cohort design to investigate the effect of two different patterns of prehospital care in the Fiuli‐Venezia Giulia region of Italy. The HEMS group was staffed by a physician and the GEMS group was staffed by a nurse. Significantly more people in the HEMS group received chest tube placement, placement of intravenous lines, and advanced modes of ventilation, including endotracheal intubation. After controlling for transport mode, gender, age, ISS, and RTS, there was no difference in survival between HEMS and GEMS (OR not reported; P value = 0.68). For people requiring urgent neurosurgery, there was no difference in survival between HEMS and GEMS (OR 1.56; 95% CI 0.38 to 6.25; P value not reported).
Schiller 1988 was a retrospective cohort of 606 people in a primarily urban setting in Phoenix, AZ, USA. Unadjusted mortality was statistically significantly higher for HEMS (18%) versus GEMS (13%) (P value < 0.05). All participants in this cohort had blunt trauma and 80% had a TBI. All participants had an ISS between 20 and 39. All participants were transported to a level I trauma center but the study did not describe crew configurations.
Baxt 1987 studied the impact of HEMS versus GEMS for 128 consecutive participants with TBI in San Diego, CA, USA. HEMS crews consisted of an attending physician and nurse, and GEMS crews consisted of EMTs capable of providing only basic life support. Overall unadjusted mortality was 31% in the HEMS group and 40% in the GEMS group (P value < 0.0001). For GCS scores of 5, 6, or 7 the GEMS group had improved mortality; however, for GCS scores of 3 or 4, mortality was statistically significantly lower for the HEMS group (52%) versus the GEMS group (64%) (P value not reported for this subgroup).
Berlot 2009 retrospectively compared HEMS versus GEMS outcomes in 194 people with an AIS‐head of 9 or greater and an ISS of 15 or greater. HEMS crews consisted of two nurses and an anesthesiologist. GEMS crews consisted of a physician capable of providing only basic life support and two nurses trained in emergency care. People in the HEMS group had an unadjusted mortality of 21% versus 25% in the GEMS group (P value < 0.05); 54% of people in the HEMS group survived with only minor neurologic disability compared with 44% of people in the GEMS group (P value < 0.05).
2. Blunt trauma studies
Seven studies consisted of a population of adults with blunt trauma (Bartolacci 1998; Baxt 1983; Braithwaite 1998; Desmettre 2012; Nardi 1994; Schwartz 1990; Thomas 2002). Heterogeneity in this subgroup was considerable (Chi2 = 111.44, I2 = 97%). All studies provided data to estimate unadjusted mortality but due to the heterogeneity, a reliable effect estimate and associated CI, could not be estimated. These data, when considered collectively, suggest an overall benefit of HEMS versus GEMS for adults with major trauma, although meta‐analysis could not be performed to provide a precise estimate of the effect size.
The results from Desmettre 2012 are discussed in the 'Traumatic brain injury studies' section describing studies that used regression to control for confounding variables.
In Bartolacci 1998, people transported by HEMS were treated by an anesthesiologist and a paramedic whereas people transported by GEMS were treated by an acute care physician and a paramedic. All participants were transported to a level I trauma center in Sydney, Australia. Major blunt trauma was defined by the mechanism of injury and an ISS of at least 15. There was a W statistic of 12.18 (95% CI 5.29 to 19.07). This indicated that there were 12 more survivors in the HEMS group than expected for every 100 people transported, based on a comparison with the MTOS cohort.
Thomas 2002 studied 16,699 people with blunt trauma treated in the New England, USA area from 1995 to 1998; 2292 people were treated by HEMS and 14,407 people were treated by GEMS. Although the unadjusted mortality was 9.4% for HEMS versus 2.0% for GEMS, after adjusting for age, sex, transport year, receiving hospital, ISS, mission type, and prehospital level of care, HEMS was associated with a lower odds of death compared with GEMS (OR 0.76; 95% CI 0.59 to 0.98; P value = 0.031). Some HEMS crews consisted of a physician and nurse, while others consisted of paramedics only or nurses only.
Baxt 1983 included 150 people transported by HEMS and 150 people transported by GEMS in the San Diego, CA, USA area who sustained major blunt trauma. The authors employed a TRISS analysis comparing expected versus actual survival based on comparison with the MTOS cohort. In the HEMS group, 20.6 people were predicted to die but only 10 died; in the GEMS group, 14.8 people were expected to die but 19 died. Although the actual Z statistic was not reported, people in the HEMS group were 52% more likely to survive that people in the GEMS group when groups were stratified by injury severity (P value < 0.001).
Braithwaite 1998 performed a retrospective study of 16,699 people with blunt trauma with a categorization of the ISS into five groups: 0 to 15, 16 to 30, 31 to 45, 46 to 60, and greater than 60. There was no beneficial effect on survival for HEMS compared with GEMS. A statistically significant interaction between HEMS transport and mortality was found for the middle ISS group only (16 to 30, 31 to 45, 31 to 45), indicating a possible survival benefit for people with moderate‐to‐severe injuries.
Schwartz 1990 retrospectively analyzed data from an EMS system in Connecticut, USA comparing 126 people with blunt trauma transported by either HEMS or GEMS with TRISS methodology. People transported by HEMS were statistically significantly more likely to survive compared with the MTOS cohort (Z = 2.23) and people transported by GEMS had a lower survival rate than predicated by MTOS (Z = ‐2.69).
Nardi 1994 prospectively collected data on 222 people with blunt trauma, with mean ISS greater than 30, in Italy. People transported directly to a trauma center by HEMS had an unadjusted mortality rate of 12% versus a mortality rate of 32% for people transported directly to a trauma center by GEMS; 14% of people in the HEMS group had a chest tube placed and 81% were intubated, whereas no‐one in the GEMS group had a chest tube placement or intubation. The HEMS crew consisted of an anesthesiologist with at least 10 years' experience and two nurses with intensive care unit (ICU) experience. GEMS crews consisted of two nurses with basic trauma life support training and an occasional emergency room physician who was not allowed to intubate.
3. Interfacility transfer
Four studies that met inclusion criteria focused on the role of HEMS versus GEMS for interfacility transfers to higher levels of trauma care (Brown 2011; McVey 2010; Mitchell 2007; Moylan 1988).
Brown 2011 examined 74,779 people transferred to trauma centers by either HEMS (20%) or GEMS (80%). The authors used multivariate regression to determine whether transport modality was an independent predictor of survival while adjusting for age, gender, mechanism of injury, ISS, hypotension, severe TBI, abnormal respiratory rate, mechanical ventilation, emergent operations, ICU admission, and trauma center designation. HEMS transportation for people with an ISS of at least 15, when used as the modality to transfer people to a higher level of trauma care, was independently associated with statistically significantly improved survival (OR 1.09; 95% CI 1.02 to 1.17; P value = 0.01).
Moylan 1988 examined the effect of HEMS versus GEMS on interhospital transportation to a level I trauma center for 330 severely injured people. People transported by HEMS were more likely to receive blood transfusions (32% with HEMS versus 10.5% with GEMS), be intubated (50% with HEMS versus 25% with GEMS), or have medical antishock trousers (MAST) applied (60.2% with HEMS versus 34.9% with GEMS). People in the HEMS group also received significantly more mean quantities of intravenous fluid (3.34 L per person) than people in the GEMS group (2.1 L per person). For people with a trauma score between 10 and 5, 54 of 101 (53.5%) people in the GEMS group survived compared with 53 of 64 (82.8%) people in the HEMS group. This result was statistically significant favoring HEMS in terms of a survival advantage (P value < 0.001).
Mitchell 2007 compared outcomes for 823 people with an ISS of at least 12 in Nova Scotia, Canada; 84% of people transported by HEMS and 43.5% of people transported by GEMS were transferred from a primary or distant trauma center to the equivalent of a level I trauma center. The authors performed a TRISS‐based regression analysis with reporting of the Z statistic and W score. For the HEMS group, the Z statistic was 2.77 versus a Z statistic of ‐1.97 for the GEMS group. The W score for the HEMS group was 6.40 indicating that there were 6.4 more survivors than expected per 100 people, as compared with the MTOS cohort. In comparison, the W score for the GEMS group was ‐2.40 indicating that there were 2.4 unexpected nonsurvivors per every 100 people. The authors did not describe crew configuration, in‐flight interventions, and stabilizing procedures at the primary and distant trauma centers. Mitchell 2007 did not report anM statistic and, although this study was performed in a North American system, comparability with the original MTOS cohort may not be entirely valid.
In another Canadian study, McVey 2010 compared outcomes of people with trauma transported by HEMS or GEMS, with a mean ISS of at least 20. The authors described this study as a "natural experiment" since some of the people in the GEMS group consisted of people initially designated to be flown by helicopter but who were eventually transported by land due to weather or other aviation‐related reasons. The study performed a TRISS analysis, with calculation of Z statistics and W scores. The majority of HEMS missions in this study were interfacility transfers (79.6%). In the HEMS group, the Z statistic was 3.37 and the W score indicated 5.61 survivors for every 100 people transported. In the GEMS group, the Z statistic was ‐2.71 and the W score indicated that there were two additional unexpected nonsurvivors for every 100 people transported. McVey 2010 did not report anM statistic and, although this study was performed in a North American system, comparability with the original MTOS cohort may not be entirely valid.
Secondary outcome measures
None of the included studies measured QALYs or DALYs.
Adverse events
Data regarding safety were not available in any of the included studies. Road traffic and helicopter crashes are adverse effects which can occur with either method of transport.
Discussion
Summary of main results
This review includes 38 studies, of which 34 studies examined survival following transportation by HEMS compared with GEMS for adults with major trauma. Four studies were of inter‐facility transfer to a higher level trauma center by HEMS compared with GEMS. Most of the available studies did not use methodology that allowed for the ability to assess whether HEMS gave people with trauma who were not in proximity to specialty care the same chance of survival as people for whom care was immediately available (Floccare 2002). Due to the considerable heterogeneity of effects and study methodologies, we could not determine an accurate estimate of composite effect. The quality of evidence, which reflects the extent of confidence that an estimate of effect is correct, was very low as assessed by the GRADE Working Group criteria, thus making comparisons difficult. However, in studies that employed advanced statistical techniques to control for known confounders, the OR, and 95% CI, was statistically significantly in favor of HEMS for improved survival (Table 3). The largest studies that employed advanced regression techniques, and had a lower risk for bias as assessed with the Downs and Black instrument (Figure 3), reported effect estimates in favor of HEMS compared with GEMS in terms of survival (Abe 2014; Andruskow 2013;Brown 2010;Galvagno 2012;Desmettre 2012;Ryb 2013;Stewart 2011;Thomas 2002).
Overall completeness and applicability of evidence
HEMS systems are predominantly located in high‐income countries. Thus, the findings from this review may only be generalizable for a number of settings. This review used a comprehensive search strategy that included non‐English articles. We used a formal protocol that omitted studies known to be more susceptible to bias, and we searched for, and included when appropriate, published abstracts as well as journal articles. We identified nine studies in Europe, 22 studies in the USA, two studies in Canada, and one each in Australia, Japan and South Africa. Seven additional European HEMS studies that we excluded were helicopter treatment team studies. Many European HEMS systems are different from North American systems. For instance, in most European HEMS programs physicians are mandatory crew members, whereas in the USA, most HEMS programs are staffed by critical care nurses and paramedics. Moreover, in Europe the helicopter is used in many systems to transport the treatment team to the scene of the injury, and in countries such as the Netherlands the helicopter is rarely used to transport injured and ill people. Finally, the majority of HEMS studies in this review did not isolate the strict benefit of HEMS. Any salutary effect of HEMS is likely due to some combination of crew expertise, prehospital interventions, and timely access to a high‐level trauma center.
Quality of the evidence
The overall quality of studies in this review was low as assessed by the Downs and Black risk of bias tool and very low according to the GRADE Working Group guidelines for evaluating the impact of healthcare interventions. Most studies had a high risk of bias across all domains. The majority of studies had either an unclear or high risk of bias due to selection bias, confounding, and failure to determine the amount of power required to estimate statistically significant effects. Furthermore, most studies did not report the validity of their measurement methods for assessing outcomes and relied on local or national trauma registries, where the quality of data from these sources is not well known. Not all studies provided data on prehospital interventions and, in some studies, HEMS groups were disproportionally comprised of more highly trained providers, including physicians. It should be noted that the relative effect for mortality calculated for the GRADE analysis reflects unadjusted mortality; it only included studies that reported data that enabled the calculation of a risk ratio.
Potential biases in the review process
Two of the review authors (SG and ST) were the primary author for two of the higher‐quality studies included in this review (Galvagno 2012; Thomas 2002). Nevertheless, these studies were carefully subjected to the risk of bias assessment and the authors did not partake in the risk of bias assessment process. Several of the authors of this review maintain active roles as HEMS administrators and policy advisors (ST, DF, and JH).
It is possible that the studies which analysed data from the National Trauma Data Bank resulted in some patients being counted twice. Data were analyzed from different years (2007 data set was used for Brown 2010; 2007‐2009 data sets used for Galvagno 2012) but there was some overlap with 2007. Data were analyzed differently, and stricter inclusion criteria were used for Galvagno 2012.
Agreements and disagreements with other studies or reviews
Several different reviews have been published on HEMS since the early 2000s (Bledsoe 2006; Butler 2010; Ringburg 2009b; Taylor 2010; Thomas 2002; Thomas 2003; Thomas 2007). Thomas et al published a series of annotated reviews of the HEMS outcomes literature in 2002, 2003, and 2007 (Thomas 2002; Thomas 2003; Thomas 2007). The goal of the 2002 and 2007 reviews was to provide a reference for outcomes‐based literature. Neither of these papers were formal systematic reviews. In 2003, Thomas and Biddinger authored a brief review that highlighted the problems in identifying people who will benefit from HEMS prospectively (Thomas 2003). This study was not a formal systematic review and the goal of the paper was to address studies published since 2001; the brief review discussed only four studies.
Bledsoe 2006 published a meta‐analysis to determine the percentage of people with trauma transported from the scene by helicopter with nonlife‐threatening injuries. The authors included 22 studies in the final analysis, though the study was not, by definition, a meta‐analysis because effects were not pooled. Bledsoe 2006 evaluated five of the studies included in our review (Bartolacci 1998; Baxt 1983; Braithwaite 1998; Cunningham 1997; Phillips 1999). Two of these studies had over 50% of people with an ISS less than 15 (Bartolacci 1998; Cunningham 1997). In our study, we extracted data only from the subgroups of people in these studies with an ISS of at least 15. Furthermore, the studies used TRISS (Bartolacci 1998) and logistic regression (Cunningham 1997) to adjust for severity of injury. Bledsoe 2006 concluded that the majority of people with trauma transported from the scene have nonlife‐threatening injuries; 25.8% of all participants analyzed were discharged within 24 hours after arrival at the trauma center.
Ringburg 2009b performed a literature review in 2009, which reviewed 16 studies. This study was not a systematic review and the authors concluded that HEMS appeared to be beneficial, but only when rigorous statistical methodology was applied. In 2010, Taylor et al conducted a systematic review of the literature to determine the economic costs of HEMS and the relationship of costs to outcomes (Taylor 2010). They employed a limited search strategy and 15 studies met the inclusion criteria. This review also included people without trauma. It highlighted a lack of high‐quality studies. The authors concluded that the "weight of observational evidence" supports an association between HEMS and improved survival in selected people with trauma, but effects could not be pooled due to the considerable differences in the cost and effectiveness of HEMS between studies (Taylor 2010).
One systematic review was conducted by Butler 2010 with the goal of determining whether HEMS is beneficial for people with trauma. There was no meta‐analysis due to the inconsistencies in participant inclusion criteria and outcome measures. Studies were limited to the English language and there was no cutoff for injury severity. The review included studies examining the effect of HTTs. An evidence table evaluated 23 eligible studies. Fourteen studies reported results that demonstrated a survival benefit for HEMS compared with GEMS. Butler et al attributed HEMS benefits to four potential factors: 1. transport of advanced airway skills to the scene, 2. transport of a team experienced in managing people with trauma to the scene, 3. expeditious transport of people from the scene to a hospital, and 4. triage to a definitive trauma center. All studies were moderate to low level evidence as assessed using the Oxford Centre of Evidence Based Medicine guidelines. The authors acknowledged that differences in study design, treatment protocols, triage guidelines, and crew configuration were limiting factors that barred the authors from establishing any resolutions about the role of HEMS for people with trauma. The authors recognized the importance of considering the benefits of a HTT separately from the benefits associated with HEMS transport.
With the exception of the review focused on nonlife‐threatening injuries (Bledsoe 2006), there are no overall disagreements with any of the previous reviews. Our protocol used a comprehensive search strategy that was devised with the help of a methodologist from the Cochrane Injuries Group. In all previous studies, the use of electronic databases was more limited than our comprehensive search strategy. Our strategy was designed to identify as many relevant studies as possible in order to minimize bias and to estimate reliable effects (Reeves 2011). Through the use of strict inclusion criteria, a thorough quality assessment, and a narrative synthesis we are confident that we identified and analyzed all pertinent HEMS studies of adults with major trauma at the time the available literature for this review was assessed as up‐to‐date.
Authors' conclusions
Implications for practice.
Due to the methodological weakness of the available literature, and the considerable heterogeneity of effects and study methodologies, we were unable to determine an accurate composite estimate of the benefit of helicopter emergency medical services (HEMS). The question of which elements of HEMS are most beneficial for people with trauma has not been fully answered, and any HEMS‐associated benefit could be the result of some combination of crew expertise, decreased prehospital time, and the fact that HEMS are an integral part of organized trauma systems in many high‐income countries (Thomas 2003). Moreover, HEMS‐associated benefits may include physician‐adjudicated launching criteria based on severity of injury and mechanism, centrally coordinated launching algorithms with selected HEMS deployment, trauma volumes at receiving trauma centers, and the ability of the helicopter to transport people in areas inaccessible by ground vehicles or prohibitively distant from trauma centers. This review stressed the importance of triage criteria since the benefits of HEMS may be greatest for people with serious but potentially survivable injuries. Ideal dispatch criteria and triage guidelines to ensure the efficient use of helicopters remain elusive.
Implications for research.
The results from this review will motivate future work in this area, including the ongoing need for diligent reporting of research methods, which is imperative for transparency and to maximize the potential utility of results. Given the infeasibility and ethical concerns about performing randomized controlled trial for HEMS, the use of advanced methods for observational research, such as propensity scores and instrumental variables, should be considered the standard for analyzing the data from future HEMS studies. Furthermore, correct specification of logistic regression models is vital since effect estimates will be biased if the assumptions for these models are violated. Other outcomes of interest including morbidity, disability, and health‐related quality of life after HEMS versus ground emergency medical service (GEMS) transport should be also be measured to assess potential HEMS‐associated benefits. Large, multicenter studies are warranted and this will help produce more robust estimates of treatment effects; it is likely that large numbers of participants will be required to quantify outcomes accurately. Finally, the costs and safety of HEMS cannot be ignored, and future studies need to consider multiple contextual determinants if the use of HEMS is to be supported.
What's new
| Date | Event | Description |
|---|---|---|
| 16 June 2015 | New citation required and conclusions have changed | The search has been updated to 29 April 2015. |
| 16 June 2015 | New search has been performed | The results of nine new studies have been added to this systematic review. |
Acknowledgements
We would like to thank Karen Blackhall of the Cochrane Injuries Group for her work on the original search strategy.
Appendices
Appendix 1. Search strategies
Cochrane Injuries Group Specialised Register
((ES or EMS or emergency or emergencies or service* or HEMS or AEMS) AND (helicopter* or rotocraft or rotorwing or rotarywing or helicopter*)) AND ( INREGISTER) [REFERENCE] [STANDARD]
CENTRAL (The Cochrane Library)
#1MeSH descriptor: [Air Ambulances] explode all trees #2(helicopter* near/3 (ES or EMS or emergency or emergencies or service*)):ti,ab,kw (Word variations have been searched) #3(helicopter* or rotorcraft or rotorwing or rotarywing or helicopter* or rotor?craft or rotor?wing or rotary?wing or Helicopter emergency medical service* or HEMS or Air emergency medical service* or AEMS):ti,ab,kw (Word variations have been searched) #4MeSH descriptor: [Emergency Medical Services] explode all trees #5MeSH descriptor: [Transportation of Patients] explode all trees #6#4 or #5 #7(Air* or helicopter* or rotorcraft or rotorwing or rotarywing or rotor?craft or rotor?wing or rotary?wing):ti,ab,kw (Word variations have been searched) #8#6 and #7 #9#1 or #2 or #3 or #8 #10MeSH descriptor: [Wounds and Injuries] explode all trees #11MeSH descriptor: [Fracture Fixation] explode all trees #12MeSH descriptor: [Pelvis] explode all trees and with qualifiers: [Injuries ‐ IN] #13MeSH descriptor: [Pelvic Bones] explode all trees and with qualifiers: [Injuries ‐ IN] #14MeSH descriptor: [Femur Head] explode all trees and with qualifiers: [Injuries ‐ IN] #15((spine* or spinal) near/3 (fracture* or injur* or broke*)):ti,ab,kw (Word variations have been searched) #16((head or crani* or cerebr* or brain* or skull*) near/3 (injur* or trauma* or damag* or wound* or fracture*)):ti,ab,kw (Word variations have been searched) #17((femur* or femoral*) near/3 (fracture* or injur* or trauma* or broke*)):ti,ab,kw (Word variations have been searched) #18((pelvis or pelvic) near/3 (fracture* or injur* or trauma* or broke*)):ti,ab,kw (Word variations have been searched) #19((crush* or burn*) near/3 (injur* or trauma*)):ti,ab,kw (Word variations have been searched) #20#10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 #21#9 and #20
MEDLINE (OvidSP)
1.exp Air Ambulances/ 2.(helicopter* adj3 (ES or EMS or emergency or emergencies or service*)).ab,it. 3.(helicopter* or rotor craft or rotor wing or rotary wing or helicopter* or rotor?craft or rotor?wing or rotary?wing or Helicopter emergency medical service* or HEMS or Air emergency medical service* or AEMS).ab,ti. 4.exp Emergency Medical Services/ 5.exp "Transportation of Patients"/ 6.4 or 5 7.(Air* or helicopter* or rotorcraft or rotorwing or rotarywing or rotor?craft or rotor?wing or rotary?wing).ab,ti. 8.6 and 7 9.1 or 2 or 3 or 8 10.exp "Wounds and Injuries"/ 11.exp Fracture Fixation/ 12.exp Pelvis/in [Injuries] 13.exp Pelvic Bones/in [Injuries] 14.exp Femur Head/in [Injuries] 15.((spine* or spinal) adj3 (fracture* or injury* or broke*)).ti,ab. 16.((head or crani* or cerebr* or brain* or skull*) adj3 (injur* or trauma* or damag* or wound* or fracture*)).ti,ab. 17.((femur* or femoral*) adj3 (fracture* or injur* or trauma* or broke*)).ti,ab. 18.((pelvis or pelvic) adj3 (fracture* or injur* or trauma* or broke*)).ti,ab. 19.((crush* or burn*) adj3 (injur* or trauma*)).ti,ab. 20.10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 21.9 and 20 22.((injur* or wound* or sick or trauma* or patient*) adj3 (transport* or transfer*) adj3 (air* or helicopter* or rotorcraft or rotorwing or rotarywing or rotor?craft or rotor?wing or rotary?wing or sky)).ab,ti. 23.21 or 22 24.clinical trials as topic.sh. 25.randomi?ed.ti,ab. 26.randomized controlled trial.pt. 27.controlled clinical trial.pt. 28.(controlled adj3 (('before and after') or trial* or study or studies or evaluat*)).ab,ti. 29.randomized.ab. 30.placebo.ti,ab. 31.((before adj3 after) or (interrupted adj3 time)).ab,ti. 32.randomly.ab. 33.trial.ti. 34.groups.ti,ab. 35.(observed or observation*).mp. 36.exp device approval/ 37.((compar* or intervention or evaluat*) adj3 (trial* or stud*)).ab,ti. 38.(random* adj3 allocat*).ab,ti. 39.exp prospective studies/ 40.exp follow‐up studies/ 41.exp comparative study/ 42.exp cohort studies/ 43.exp evaluation studies/ 44.exp treatment outcome/ 45.or/24‐44 46.exp animals/ 47.exp humans/ 48.46 not (46 and 47) 49.45 not 48 50.23 and 49
EMBASE Classic + EMBASE (OvidSP)
1. exp Air Ambulances/ 2. (helicopter* adj3 (ES or EMS or emergency or emergencies or service*)).ab,ti. 3. (helicopter* or rotorcraft or rotorwing or rotarywing or helicopter* or rotor?craft or rotor?wing or rotary?wing or Helicopter emergency medical service* or HEMS or Air emergency medical service* or AEMS).ab,ti. 4. exp Emergency Medical Services/ 5. exp "Transportation of Patients"/ 6. 4 or 5 7. (Air* or helicopter* or rotorcraft or rotorwing or rotarywing or rotor?craft or rotor?wing or rotary?wing).ab,ti. 8. 6 and 7 9. 1 or 2 or 3 or 8 10. exp "Wounds and Injuries"/ 11. exp Fracture Fixation/ 12. ((spine* or spinal) adj3 (fracture* or injur* or broke*)).ti,ab. 13. ((head or crani* or cerebr* or brain* or skull*) adj3 (injur* or trauma* or damag* or wound* or fracture*)).ti,ab. 14. ((femur* or femoral*) adj3 (fracture* or injur* or trauma* or broke*)).ti,ab. 15. ((pelvis or pelvic) adj3 (fracture* or injur* or trauma* or broke*)).ti,ab. 16. ((crush* or burn*) adj3 (injur* or trauma*)).ti,ab. 17. ((injur* or wound* or sick or trauma* or patient*) adj3 (transport* or transfer*) adj3 (air* or helicopter* or rotorcraft or rotorwing or rotarywing or rotor?craft or rotor?wing or rotary?wing or sky)).ab,ti. 18. exp pelvis/ 19. (fracture* or injur* or trauma* or broke*).ti,ab. 20. 18 and 19 21. 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 20 22. 9 and 21
CINAHL Plus (EBSCOhost)
S29S17 AND S28 S28S18 or S19 or S20 or S21 or S22 or S23 or S24 or S25 or S26 or S27 S27MH quantitative studies S26TX random* N3 allocat* S25(MH "Random Assignment") S24TX placebo* S23(MH "Placebos") S22TX randomi?ed N3 control* N3 trial* S21TI ( (singl* N3 blind*) or (doubl* N3 blind*) or (trebl* N3 blind*) or (tripl* N3 blind*) ) or TI ( (singl* N3 mask*) or (doubl* N3 mask*) or (trebl* N3 mask*) or (tripl* N3 mask*) ) or AB ( (singl* N3 blind*) or (doubl* N3 blind*) or (trebl* N3 blind*) ) or AB ( (singl* N3 mask*) or (doubl* N3 mask*) or (trebl* N3 mask*) or (tripl* N3 mask*) ) S20TX clinical N3 trial* S19PT clinical trial* S18(MH "Clinical Trials") S17S15 OR S16 S16TX ((injur* or wound* or sick or trauma* or patient*) N3 (transport* or transfer*) N3 (air* or helicopter* or rotorcraft or rotorwing or rotarywing or rotor?craft or rotor?wing or rotary?wing or sky)) S15S7 AND S14 S14S8 OR S9 OR S10 OR S11 OR S12 OR S13 S13TX ((crush* or burn*) N3 (injur* or trauma*)) S12TX ((pelvis or pelvic) N3 (fracture* or injur* or trauma* or broke*)) S11TX ((femur* or femoral*) N3 (fracture* or injur* or trauma* or broke*)) S10TX ((head or crani* or cerebr* or brain* or skull*) N3 (injur* or trauma* or damag* or wound* or fracture*)) S9TX ((spine* or spinal) N3 (fracture* or injur* or broke*)) S8(MH "Wounds and Injuries+") OR (MH "Fracture Fixation") OR (MH "Pelvis/IN") OR (MH "Pelvic Bones/IN") OR (MH "Femur Head/IN") S7S2 OR S3 OR S4 OR S6 S6S1 AND S5 S5TX (Air* or helicopter* or rotorcraft or rotorwing or rotarywing or rotor?craft or rotor?wing or rotary?wing) S4TX (helicopter* or rotorcraft or rotorwing or rotarywing or helicopter* or rotor?craft or rotor?wing or rotary?wing or Helicopter emergency medical service* or HEMS or Air emergency medical service* or AEMS) S3TX (helicopter* N3 (ES or EMS or emergency or emergencies or service*)) S2(MH "Aeromedical Transport") S1(MH "Emergency Medical Services+") OR (MH "Transportation of Patients+")
ISI Web of Science: Science Citation Index Expanded (SCI‐EXPANDED) & Conference Proceedings Citation Index‐Science (CPCI‐S) ((ES or EMS or emergency or emergencies or service* or HEMS or AEMS) AND (helicopter* or rotocraft or rotorwing or rotarywing or helicopter*))
OpenSIGLE (System for Information on Grey Literature in Europe) & ZETOC
helicopter AND emergency
National Library of Medicine's Health Services Research Projects in Progress (HSRProj)
helicopter emergency
Data and analyses
Comparison 1. Helicopter emergency medical services (HEMS) transport compared with ground emergency medical services (GEMS).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Unadjusted mortality | 28 | 408586 | Risk Ratio (IV, Random, 95% CI) | 1.04 [0.89, 1.22] |
| 1.1 All studies with available data | 28 | 376648 | Risk Ratio (IV, Random, 95% CI) | 1.03 [0.85, 1.26] |
| 1.2 Traumatic brain injury studies | 6 | 12596 | Risk Ratio (IV, Random, 95% CI) | 0.99 [0.86, 1.12] |
| 1.3 Blunt trauma studies | 4 | 19342 | Risk Ratio (IV, Random, 95% CI) | 1.04 [0.41, 2.62] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Abe 2014.
| Methods | Retrospective, multicenter, observational trial | |
| Participants | Adults (age > 15 years) included in the Japan Trauma Data Bank, from 2004 to 2011, with an ISS > 15 | |
| Interventions | HEMS vs. GEMS. HEMS crews consisted of physician and nurse. GEMS crews consisted of EMT and firefighter | |
| Outcomes | Primary: survival to discharge from the hospital. Secondary: survival to discharge from the emergency room | |
| Notes | 3 different regression models used: unconditional logistic regression, logistic regression with propensity score matching, and a conditional logistic regression model. All 3 models indicated a statistically significant positive association with HEMS and improved survival | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | Low risk | 11/11 |
| External validity | Low risk | 3/3 |
| Internal validity | Low risk | 5/7 |
| Internal validity: confounding and selection bias | Low risk | 6/6 |
| Power | High risk | 0 |
Andruskow 2013.
| Methods | Retrospective cohort using the TraumaRegister DGU of the German Society for Trauma Surgery, TRISS‐based (W statistic not reported) | |
| Participants | People with trauma treated by HEMS or GEMS between 2007 and 2009 transported to level I or II trauma centers | |
| Interventions | Both HEMS and GEMS staffed by physicians; treatments: intubation, vasopressors, chest thoracostomy tube insertion, cardiopulmonary resuscitation, sedation, administration of intravenous fluids | |
| Outcomes | Survival, incidence of multiple organ dysfunction, duration of mechanical ventilation, ICU length of stay, overall hospital length of stay | |
| Notes | Inclusion criteria included ISS > 9, but mean ISS was 26 in HEMS and 23.7 in GEMS. Multivariate regression used with hospital mortality as dependent variable. Confounders in model: ISS < age, unconsciousness, shock, hypotension, intubation, sex, type of injury, mechanism of injury, level of care at the target hospital, daytime | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | High risk | 7/11 |
| External validity | Low risk | 3/3 |
| Internal validity | High risk | 3/7 |
| Internal validity: confounding and selection bias | High risk | 3/6 |
| Power | High risk | 0/5 |
Bartolacci 1998.
| Methods | Retrospective cohort, TRISS‐based (W statistic reported) | |
| Participants | Blunt trauma only, ISS > 15, New South Wales, Australia | |
| Interventions | HEMS vs. GEMS transport to a trauma center | |
| Outcomes | Mortality | |
| Notes | HEMS crews: physicians (anesthesiologist), GEMS crews: paramedics | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | Low risk | 8/11 |
| External validity | Low risk | 3/3 |
| Internal validity | Unclear risk | 4/7 |
| Internal validity: confounding and selection bias | High risk | 3/6 |
| Power | High risk | 0/5 |
Baxt 1983.
| Methods | Retrospective cohort, ground comparison group only | |
| Participants | People with blunt trauma only in San Diego, USA, over a 30‐month period | |
| Interventions | HEMS vs. GEMS transport to a trauma center | |
| Outcomes | Mortality | |
| Notes | HEMS crews: physician and nurse, GEMS crews: paramedic and EMT | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | Low risk | 8/11 |
| External validity | Low risk | 3/3 |
| Internal validity | Unclear risk | 4/7 |
| Internal validity: confounding and selection bias | High risk | 3/6 |
| Power | High risk | 0/5 |
Baxt 1987.
| Methods | Retrospective cohort, TRISS‐based (W, Z, M statistics not reported) | |
| Participants | People with traumatic brain injury in California, USA | |
| Interventions | HEMS vs. GEMS transport to a single level I trauma center | |
| Outcomes | Mortality | |
| Notes | HEMS crews administered medications and provided advanced life support; GEMS crews rendered mostly basic life support (10% of GEMS units were staffed by a paramedic) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | High risk | 5/11 |
| External validity | Low risk | 3/3 |
| Internal validity | Unclear risk | 4/7 |
| Internal validity: confounding and selection bias | High risk | 2/6 |
| Power | High risk | 0/5 |
Berlot 2009.
| Methods | Retrospective cohort, ground comparison group only | |
| Participants | People with traumatic brain injury in the Fruli‐Venezia Giulia region, Italy, 2002‐2007 | |
| Interventions | HEMS vs. GEMS transport to 1 of 2 specialty hospitals for traumatic brain injury | |
| Outcomes | Mortality | |
| Notes | HEMS crews had advanced‐life support‐capable physicians and 2 nurses, GEMS crews had a nonadvanced life support physician and 2 nurses; people transported by HEMS were treated more aggressively | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | High risk | 7/11 |
| External validity | Low risk | 3/3 |
| Internal validity | High risk | 4/7 |
| Internal validity: confounding and selection bias | High risk | 1/6 |
| Power | High risk | 0/5 |
Biewener 2004.
| Methods | Retrospective cohort, TRISS (W, Z, M statistics not reported) | |
| Participants | People with polytrauma in Germany between January 1998‐December 1999 | |
| Interventions | HEMS vs. GEMS transfer to a local hospital vs. trauma center | |
| Outcomes | Mortality | |
| Notes | 4 pathways: HEMS to trauma center, GEMS to trauma center, GEMS to local hospital, GEMS followed by late interhospital transfer to a trauma center | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | High risk | 7/11 |
| External validity | Unclear risk | 2/3 |
| Internal validity | High risk | 4/7 |
| Internal validity: confounding and selection bias | High risk | 2/6 |
| Power | High risk | 0/5 |
Braithwaite 1998.
| Methods | Retrospective cohort, ground comparison group only | |
| Participants | Trauma patients in the Pennsylvania Trauma Outcome study, 1978‐1995, USA | |
| Interventions | HEMS versus GEMS transport to trauma centres | |
| Outcomes | Mortality | |
| Notes | Not all hospitals were level I trauma centres, types of injuries not described | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | High risk | 5/11 |
| External validity | Unclear risk | 2/3 |
| Internal validity | High risk | 4/7 |
| Internal validity: confounding and selection bias | High risk | 3/6 |
| Power | High risk | 0/5 |
Brown 2010.
| Methods | Retrospective cohort, ground comparison group only | |
| Participants | People with trauma in the 2007 NTDB, USA | |
| Interventions | HEMS vs. GEMS transport to trauma centers | |
| Outcomes | Mortality | |
| Notes | Higher baseline ISS in HEMS group compared with GEMS group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | Low risk | 8/11 |
| External validity | High risk | 0/3 |
| Internal validity | High risk | 3/7 |
| Internal validity: confounding and selection bias | High risk | 2/6 |
| Power | High risk | 0/5 |
Brown 2011.
| Methods | Retrospective cohort, ground comparison group only | |
| Participants | People with trauma in the 2007 NTDB, USA | |
| Interventions | HEMS vs. GEMS interfacility transfer to higher level trauma centers | |
| Outcomes | Mortality | |
| Notes | Crew configurations unknown | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | Low risk | 8/11 |
| External validity | High risk | 1/3 |
| Internal validity | High risk | 4/7 |
| Internal validity: confounding and selection bias | High risk | 2/6 |
| Power | High risk | 0/5 |
Bulger 2012.
| Methods | Retrospective cohort, based on prospectively collected data; multiple logistic regression | |
| Participants | 2049 participants, of whom 811 were in a shock cohort, and 1238 in a traumatic brain injury cohort; 10 regions in the USA and Canada representing 114 EMS agencies | |
| Interventions | HEMS vs. GEMS transport to a trauma center | |
| Outcomes | Mortality | |
| Notes | Overall, people transported by HEMS were more likely to have an advanced airway (80.8% vs. 36.1%) received more intravenous fluids, and had more total out‐of‐hospital time (76.1 vs. 43.5 minutes). Crew configurations unknown | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | Low risk | 10/11 |
| External validity | Low risk | 3/3 |
| Internal validity | Unclear risk | 4/7 |
| Internal validity: confounding and selection bias | Unclear risk | 4/6 |
| Power | High risk | 0/5 |
Buntman 2002.
| Methods | Retrospective cohort, TRISS‐based (Z and M statistic reported) | |
| Participants | People with trauma admitted to 1 of 2 trauma centers in Johannesburg, South Africa, September 1999‐January 2000 | |
| Interventions | HEMS vs. GEMS transport to a trauma center | |
| Outcomes | Mortality | |
| Notes | Crew configurations and types of injuries not described | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | High risk | 6/11 |
| External validity | Low risk | 3/3 |
| Internal validity | High risk | 3/7 |
| Internal validity: confounding and selection bias | High risk | 2/6 |
| Power | High risk | 0/5 |
Cunningham 1997.
| Methods | Retrospective cohort, ground comparison group only | |
| Participants | People with trauma in North Carolina, USA, 1987‐1993 | |
| Interventions | HEMS vs. GEMS transport to level I or level II trauma centers | |
| Outcomes | Mortality | |
| Notes | Crew configurations not described | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | High risk | 6/11 |
| External validity | Low risk | 3/3 |
| Internal validity | High risk | 3/7 |
| Internal validity: confounding and selection bias | High risk | 2/6 |
| Power | High risk | 0/5 |
Davis 2005.
| Methods | Retrospective cohort, ground comparison group only | |
| Participants | People with traumatic brain injury in the San Diego area, California, USA, 1987‐2003 | |
| Interventions | HEMS vs. GEMS transport to level I or level II trauma centers | |
| Outcomes | Mortality | |
| Notes | GEMS crews could not intubated, but HEMS crews could; HEMS crews: nurse, paramedic, physician, GEMS crews: 2 paramedics | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | Low risk | 11/11 |
| External validity | Low risk | 3/3 |
| Internal validity | Unclear risk | 5/7 |
| Internal validity: confounding and selection bias | High risk | 3/6 |
| Power | High risk | 0/5 |
Desmettre 2012.
| Methods | Retrospective cohort, 2703 participants with severe blunt trauma, multiple logistic regression (with exam for effect modification) | |
| Participants | 2703 adults with severe blunt trauma, in France | |
| Interventions | HEMS vs. GEMS transport; 6 life‐saving interventions examined: intubation, colloid/hypertonic saline solution infusion, continuous catecholamine infusion, pneumothorax aspiration or chest tube insertion, blood product administration, > 1000 mL crystalloid infusion | |
| Outcomes | Survival at 30 days or at ICU discharge | |
| Notes | People transported by HEMS were more frequently intubated, received more fluids, vasopressors, and blood products. Same crew configuration (physician‐based). Blunt trauma only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | Low risk | 9/11 |
| External validity | Unclear risk | 2/3 |
| Internal validity | High risk | 4/7 |
| Internal validity: confounding and selection bias | Unclear risk | 4/6 |
| Power | High risk | 0/5 |
Di Bartolomeo 2001.
| Methods | Retrospective cohort, TRISS‐based (W, Z, M statistics not reported) | |
| Participants | People with traumatic brain injury in the Fruli‐Venezia Giulia region of Italy, March 1998‐February 1999 | |
| Interventions | HEMS with physician vs. GEMS with nurse, transport to a specialty hospital for traumatic brain injury | |
| Outcomes | Mortality | |
| Notes | People transported by HEMS received advanced ventilation including endotracheal intubation (64/92 people), chest tubes (4/92), and intravenous lines (92/92); people transported by GEMS only received bag‐mask ventilation, no chest tubes, and 74/92 had intravenous lines placed | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | Low risk | 10/11 |
| External validity | Low risk | 3/3 |
| Internal validity | High risk | 4/7 |
| Internal validity: confounding and selection bias | High risk | 3/6 |
| Power | High risk | 0/5 |
Frey 1999.
| Methods | Retrospective cohort, ground comparison group only | |
| Participants | 12,244 people involved in motor vehicle crash admitted to trauma centers in Pennsylvania, USA | |
| Interventions | HEMS vs. GEMS transport to trauma centers | |
| Outcomes | Mortality | |
| Notes | Crew configurations and types of injuries not described; levels of trauma centers not described | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | High risk | 4/11 |
| External validity | High risk | 0/3 |
| Internal validity | High risk | 1/7 |
| Internal validity: confounding and selection bias | High risk | 1/6 |
| Power | High risk | 0/5 |
Frink 2007.
| Methods | Retrospective cohort, TRISS‐based (W, Z, M statistics not reported) | |
| Participants | People with polytrauma admitted to trauma centers in Germany, Switzerland, Austria, Netherlands, 1993‐2003 | |
| Interventions | HEMS vs. GEMS transport to trauma centers | |
| Outcomes | Mortality | |
| Notes | Both HEMS and GEMS had physician crews; participants were admitted to different types (level) of trauma centers | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | High risk | 5/11 |
| External validity | High risk | 0/3 |
| Internal validity | High risk | 3/7 |
| Internal validity: confounding and selection bias | High risk | 2/6 |
| Power | High risk | 0/5 |
Galvagno 2012.
| Methods | NTDB from USA used. Multiple imputation, multiple logistic regression (including generalized estimating equations and propensity score matching) | |
| Participants | Adults age > 15 years, ISS > 15, transported to level I or II trauma centers in the USA | |
| Interventions | HEMS vs. GEMS transportation | |
| Outcomes | Survival to hospital discharge | |
| Notes | No information on time, distance, crew configuration. High proportion of missing data in NTDB; high proportion of data missing transportation mode (data not analyzed). Largest observational study done to date (total of 61,909 people in HEMS group and 161,566 people in GEMS group) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | Low risk | 11/11 |
| External validity | Low risk | 3/3 |
| Internal validity | Low risk | 5/7 |
| Internal validity: confounding and selection bias | High risk | 3/6 |
| Power | Low risk | 5/5 |
Giannakopoulus 2013.
| Methods | Retrospective cohort of 1073 participants | |
| Participants | Adults with trauma with ISS > 16 in the Netherlands (single level I trauma center), 1 July 2004‐1 July 2010 | |
| Interventions | HEMS vs. GEMS. HEMS crews performed advanced procedures such as rapid sequence intubation, chest tubes, airway management, and limited surgical interventions. GEMS crews not described. HEMS crews were led by a physician | |
| Outcomes | Mortality, need for ICU admission, hospital length of stay | |
| Notes | Longer on‐scene time was reported in the HEMS group (27.1 vs. 20.7 minutes, P value < 0.001) Participants were younger in the HEMS group (40.5 vs. 49.3 years, P value < 0.0001) No significant differences in types of injuries Z statistic was higher in HEMS group (3.13, P value < 0.005) vs. GEMS group (‐0.183, P value > 0.1) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | Low risk | 9/11 |
| External validity | Low risk | 3/3 |
| Internal validity | High risk | 4/7 |
| Internal validity: confounding and selection bias | Low risk | 4/6 |
| Power | High risk | 0 |
Koury 1998.
| Methods | Retrospective cohort, ground comparison group only | |
| Participants | People with trauma in Kentucky, USA, 1990‐1994 | |
| Interventions | HEMS vs. GEMS transported to a single trauma center (level I) | |
| Outcomes | Mortality | |
| Notes | HEMS crews: nurse and paramedic, GEMS crews: paramedic only; ISS higher in HEMS group (22.3 vs. 15.9) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | Low risk | 9/11 |
| External validity | Low risk | 2/3 |
| Internal validity | High risk | 4/7 |
| Internal validity: confounding and selection bias | High risk | 3/6 |
| Power | High risk | 0/5 |
McVey 2010.
| Methods | Retrospective cohort, TRISS‐based, W and Z statistic reported | |
| Participants | People with trauma in Nova Scotia, Canada, 1997‐2003 | |
| Interventions | HEMS vs. GEMS interfacility transport to a level I trauma center | |
| Outcomes | Mortality | |
| Notes | 79.6% of HEMS were interfacility transfers; 41.6% of all GEMS were interfacility transfers; 90% of all participants with trauma had blunt trauma | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | Low risk | 8/11 |
| External validity | Low risk | 3/3 |
| Internal validity | Unclear risk | 4/7 |
| Internal validity: confounding and selection bias | Unclear risk | 3/6 |
| Power | High risk | 0/5 |
Mitchell 2007.
| Methods | Retrospective cohort, TRISS‐based, W and Z score reported | |
| Participants | People with trauma with an ISS > 12 in Novia Scotia, Canada, 1998‐2002 | |
| Interventions | HEMS vs. GEMS transfer to a level I trauma center | |
| Outcomes | Mortality | |
| Notes | 84% of all HEMS were interfacility transfers; 43.5% of all GEMS were interfacility transfers; quality score: 18 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | Low risk | 8/11 |
| External validity | Low risk | 3/3 |
| Internal validity | Unclear risk | 4/7 |
| Internal validity: confounding and selection bias | High risk | 3/6 |
| Power | High risk | 0/5 |
Moylan 1988.
| Methods | Retrospective cohort, ground comparison group only | |
| Participants | People with polytrauma in North Carolina, USA, 1985‐1986 | |
| Interventions | HEMS vs. GEMS interfacility transfer to a level I trauma center | |
| Outcomes | Mortality | |
| Notes | Types of injuries not described | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | High risk | 6/11 |
| External validity | Low risk | 3/3 |
| Internal validity | High risk | 2/7 |
| Internal validity: confounding and selection bias | High risk | 3/6 |
| Power | High risk | 0/5 |
Nardi 1994.
| Methods | Prospective 7‐month cohort, 2 ground comparison groups (GEMS to regional center, GEMS to level I trauma center) | |
| Participants | People with trauma in 3 Italian provinces, 7‐month period | |
| Interventions | HEMS vs. GEMS transport to a trauma center (all HEMS went to a level I trauma center) | |
| Outcomes | Mortality | |
| Notes | HEMS crews: anesthesiologist and 2 ICU nurses, GEMS crews: 2 nurses with basic trauma life support training and 1 emergency physician who could not intubate; HEMS only operated in daytime | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | High risk | 4/11 |
| External validity | Low risk | 2/3 |
| Internal validity | High risk | 1/7 |
| Internal validity: confounding and selection bias | High risk | 0/7 |
| Power | High risk | 0/5 |
Newgard 2010.
| Methods | Secondary analysis of a prospective cohort of people with trauma, instrumental variables analysis | |
| Participants | People with trauma from 10 sites across North America, 2005‐2007 | |
| Interventions | HEMS vs. GEMS transport to level I and II trauma centers | |
| Outcomes | Mortality | |
| Notes | Unknown crew configurations | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | Low risk | 9/11 |
| External validity | Low risk | 2/3 |
| Internal validity | Unclear risk | 4/7 |
| Internal validity: confounding and selection bias | Unclear risk | 4/6 |
| Power | High risk | 0/5 |
Nicholl 1995.
| Methods | Retrospective cohort, TRISS‐based (W, Z, M statistics not reported) | |
| Participants | People with trauma in Greater London area, UK, 1991‐1993 | |
| Interventions | HEMS vs. GEMS transport to a trauma center | |
| Outcomes | Mortality | |
| Notes | Type of injuries not described; HEMS crews: physician, GEMS crews: did not always have a physician | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | Low risk | 9/11 |
| External validity | Low risk | 3/3 |
| Internal validity | Unclear risk | 4/7 |
| Internal validity: confounding and selection bias | Unclear risk | 4/6 |
| Power | High risk | 0/5 |
Phillips 1999.
| Methods | Retrospective cohort, ground comparison group only | |
| Participants | People with trauma in San Antonio, TX, USA, October 1995‐September 1996 | |
| Interventions | HEMS vs. GEMS transport to a single level I trauma center | |
| Outcomes | Mortality | |
| Notes | HEMS crews: nurse and paramedic, GEMS crews: 2 paramedics | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | Low risk | 9/11 |
| External validity | High risk | 1/3 |
| Internal validity | Low risk | 5/7 |
| Internal validity: confounding and selection bias | High risk | 3/6 |
| Power | High risk | 0/5 |
Rose 2012.
| Methods | Retrospective cohort | |
| Participants | 499 people with an ISS > 20 over a 2 year period (January 2007‐December 2008) at a level 1 trauma center in Alabama, USA | |
| Interventions | HEMS vs. GEMS transport | |
| Outcomes | Mortality | |
| Notes | No adjustment, stratified analysis by transport time and injury severity. Total participants were 2471, but only 499 could be included in this review due to the ISS cutoff that the authors used (11‐20) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | High risk | 4/11 |
| External validity | Low risk | 3/3 |
| Internal validity | High risk | 4/7 |
| Internal validity: confounding and selection bias | High risk | 2/6 |
| Power | High risk | 0/5 |
Ryb 2013.
| Methods | 2007 NTDB data used (USA). Multiple logistic regression, controlling for ISS, RTS, and transport time | |
| Participants | Adults in the 2007 NTDB with ISS ≥ 16 | |
| Interventions | HEMS vs. GEMS (transport times analyzed) | |
| Outcomes | Mortality | |
| Notes | Large proportion of missing data for transport times. No information on crew expertise or interventions. Adjusted odds of survival lower for transport times > 60 minutes and for people with RTS ≥ 6 at time of emergency room admission (people who demonstrated less severity of injury) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | Low risk | 8/11 |
| External validity | Low risk | 3/3 |
| Internal validity | Low risk | 6/7 |
| Internal validity: confounding and selection bias | High risk | 2/6 |
| Power | High risk | 0/5 |
Schiller 1988.
| Methods | Retrospective cohort, ground comparison group only | |
| Participants | People with traumatic brain injury in Arizona, USA, 1983‐1986 | |
| Interventions | HEMS vs. GEMS transport to a single level I trauma center | |
| Outcomes | Mortality | |
| Notes | Unclear if GEMS had advanced life support capabilities; blunt traumatic brain injuries only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | High risk | 6/11 |
| External validity | Low risk | 3/3 |
| Internal validity | High risk | 2/7 |
| Internal validity: confounding and selection bias | High risk | 2/6 |
| Power | High risk | 0/5 |
Schwartz 1990.
| Methods | Retrospective cohort, TRISS‐based (W, Z, M statistics not reported) | |
| Participants | People with blunt trauma in Connecticut, USA, July 1987‐June 1988 | |
| Interventions | HEMS vs. GEMS transport to a single level I trauma center | |
| Outcomes | Mortality | |
| Notes | HEMS crews: physician, nurse, respiratory therapist, GEMS crews: paramedic and EMT; no definition for 'severe blunt trauma' | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | High risk | 3/11 |
| External validity | High risk | 1/3 |
| Internal validity | High risk | 1/7 |
| Internal validity: confounding and selection bias | High risk | 3/6 |
| Power | High risk | 0/5 |
Stewart 2011.
| Methods | Retrospective cohort | |
| Participants | 10,184 people with blunt or penetrating trauma admitted to trauma centers in the state of Oklahoma, USA, January 2005‐December 2008 | |
| Interventions | HEMS vs. GEMS transport to a single level I trauma center or transport to 1 of 2 level II trauma centers; % intubated was also tabulated | |
| Outcomes | 24‐hour and 2‐week mortality | |
| Notes | Propensity score analysis: the propensity score was used as a confounding covariate in a Cox proportional hazards model (hazard ratios calculated) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | Low risk | 9/11 |
| External validity | Low risk | 3/3 |
| Internal validity | Low risk | 5/7 |
| Internal validity: confounding and selection bias | High risk | 2/6 |
| Power | High risk | 2/5 |
Sullivent 2011.
| Methods | Retrospective cohort, ground comparison only | |
| Participants | People with trauma in the 2007 NTDB, USA | |
| Interventions | HEMS vs. GEMS transport to 82 different trauma centers | |
| Outcomes | Mortality | |
| Notes | Crew configuration not described; type of trauma center (level) not described; type of injuries not described | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | Low risk | 8/11 |
| External validity | High risk | 0/3 |
| Internal validity | High risk | 2/7 |
| Internal validity: confounding and selection bias | High risk | 2/6 |
| Power | High risk | 0/5 |
Talving 2009.
| Methods | Retrospective cohort, ground comparison only (ground group with > 30 minutes transport time) | |
| Participants | People with trauma in the Los Angeles area, CA, USA, 1998‐2007 | |
| Interventions | HEMS vs. GEMS transport to a single level I trauma center | |
| Outcomes | Mortality | |
| Notes | HEMS crews: paramedic and nurse, GEMS crews: 2 paramedics | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | Low risk | 8/11 |
| External validity | Low risk | 3/3 |
| Internal validity | Unclear risk | 4/7 |
| Internal validity: confounding and selection bias | High risk | 3/6 |
| Power | High risk | 0/5 |
Thomas 2002.
| Methods | Retrospective cohort, ground comparison group only | |
| Participants | People with blunt trauma only, in New England, USA, 1995‐1998 | |
| Interventions | HEMS vs. GEMS transport to 1 of 5 level I trauma centers | |
| Outcomes | Mortality | |
| Notes | HEMS crews: all had a nurse, some had a physician, GEMS crews: paramedics and nurses | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | Low risk | 9/11 |
| External validity | Low risk | 3/3 |
| Internal validity | Unclear risk | 4/7 |
| Internal validity: confounding and selection bias | Unclear risk | 3/6 |
| Power | High risk | 0/5 |
von Recklinghausen 2011.
| Methods | Retrospective cohort, multiple logistic regression and descriptive statistics | |
| Participants | 2164 adults (mean age in HEMS group 36.5 years, mean age in GEMS group 47.9 years) transported by HEMS or GEMS January 2003‐December 2008, USA | |
| Interventions | HEMS vs. GEMS transport to a rural level 1 trauma center | |
| Outcomes | Mortality, ICU length of stay, total time in the emergency room, total hospital length of stay, ventilator days, participants discharged to rehabilitation | |
| Notes | Smaller number of participants with higher ISS likely included as evidenced by large confidence intervals in stratified analysis. Interventions and crew expertise not described | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | Low risk | 9/11 |
| External validity | Low risk | 3/3 |
| Internal validity | Low risk | 6/7 |
| Internal validity: confounding and selection bias | High risk | 3/6 |
| Power | High risk | 0/5 |
Weninger 2005.
| Methods | Retrospective cohort, ground comparison group only | |
| Participants | People with trauma in Germany | |
| Interventions | HEMS vs. GEMS transport to a single level I trauma center | |
| Outcomes | Mortality | |
| Notes | Types of injuries not described; both HEMS and GEMS staffed by physicians but different prehospital interventions performed between the groups | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Reporting bias | High risk | 6/11 |
| External validity | Unclear risk | 2/3 |
| Internal validity | High risk | 1/7 |
| Internal validity: confounding and selection bias | High risk | 2/6 |
| Power | High risk | 0/5 |
Note: Domain scores for each study are reported as the numerator in the 'Risk of bias' tables, with the denominator representing the maximum score for each domain.
EMS: emergency medical service; EMT: emergency medical technician; GEMS: ground emergency medical service; HEMS: helicopter emergency medical service; ICU: intensive care unit; ISS: Injury Severity Score; NTDB: National Trauma Data Bank; RTS: Revised Trauma Score; TRISS: Trauma‐Related Injury Severity Score.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Abbott 1998 | Wrong study design (case‐control) |
| Anderson 1987 | No comparison group |
| Baack 1991 | No outcomes reported |
| Badiali 1989 | No comparison group |
| Baxt 1985 | No comparison group |
| Boyd 1988 | No comparison group |
| Burney 1992 | Quote: "The purpose of this study was to compare the severity of illness or injury and outcomes of patients transported by physician/nurse and nurse/nurse crews" |
| Cameron 1993 | No comparison group |
| Cannell 1993 | Descriptive study |
| Carrel 1994 | No comparison group |
| Chappell 2002 | Wrong study design (before/after study; "natural experiment") |
| Chipp 2010 | No comparison group |
| Cleveland 1976 | Descriptive study |
| Cocanour 1997 | No comparison group |
| Cudnik 2008 | No comparison between HEMS and GEMS |
| Cummings 2000 | No outcomes reported for an ISS >15 group (mortality was not stratified by ISS). Mortality was a secondary outcome, and not reported for HEMS vs. GEMS groups. |
| Dardis 2000 | No comparison group |
| de Jongh 2012 | Helicopter treatment team (people not transported by HEMS), case‐control study |
| De Wing 2000 | Wrong study design (case‐control study); burns |
| Di Bartolomeo 2005 | Only included people with traumatic cardiac arrest |
| Dreyfuss 1979 | Descriptive study |
| Falcone 1998 | No comparison group |
| Fischer 1984 | No comparison group |
| Frankema 2004 | Helicopter treatment team (participants not transported by HEMS) |
| Franschman 2012 | Helicopter treatment team (participants not transported by HEMS) |
| Gerhardt 2000 | Descriptive study |
| Hallock 1985 | People with burn |
| Hoogerwerf 2013 | Letter to the editor |
| Hubner 1999 | Helicopter treatment team (participants not transported by HEMS) |
| Irola 2006 | Helicopter treatment team (participants not transported by HEMS) |
| Jacobs 1999 | No comparison group |
| Jenkinson 2006 | Descriptive study |
| Karanicolas 2006 | Outcome reporting unclear (the primary analysis was a comparison of HEMS vs. GEMS interfacility transport times). It is unclear how many pediatric patients were included (standard deviation was large) and how many patients had an ISS < 15 (large standard deviations). |
| Kidher 2012 | No comparison group |
| Kruesathit 2012 | Descriptive study, does not describe HEMS care |
| Kurola 2002 | No comparison group |
| Lossius 2002 | Helicopter treatment team (participants not transported by HEMS); also included people with medical conditions (mixed participant population) |
| Mackenzie 1979 | No outcomes data (only participants transported by HEMS and those who died reported) |
| Mann 2002 | Wrong type of study design (before/after study) |
| Margolis 2009 | Descriptive study, no comparison group |
| Massarutti 2006 | No comparison group |
| Matsumoto 2006 | No comparison group |
| McCowan 2007 | No comparison group (urban vs. rural HEMS) |
| McCoy 2013 | No comparison group |
| Melton 2007 | No comparison group |
| Michel 1994 | No comparison group |
| Moen 2008 | Patient transfer study, not specifically of HEMS |
| Munford 1994 | Wrong design (editorial) |
| Nielsen 2002 | No comparison group (also included children) |
| Norton 1996 | No comparison group |
| Nutbeam 2011 | No comparison group |
| Palarcik 1991 | Descriptive study |
| Papa 1993 | No comparison group |
| Powell 1997 | No comparison group |
| Purkiss 1994 | No comparison group (examined thoracotomy data by HEMS) |
| Ringburg 2005 | No comparison group (dealt with protocol adherence for helicopter dispatch) |
| Ringburg 2007 | Helicopter treatment team (participants not transported by HEMS) |
| Ringburg 2009 | Helicopter treatment team (participants not transported by HEMS) |
| Roberts 1970 | Descriptive study |
| Rouse 1992 | No outcomes reported (outcome was mission time). ISS was not specified, and the study population was comprised of patients with "compound lower limb fracture." |
| Salimi 2009 | No comparison group |
| Sampalis 1993 | No comparison group (GEMS only) |
| Schiller 2009 | No comparison group (before/after study; 1 vs. 2 helicopters in EMS system) |
| Schipper 2006 | Wrong design (editorial; brief narrative review of previous studies) |
| Schwab 1985 | No comparison group |
| Shatney 2002 | No comparison group |
| Shepherd 2008 | No comparison group |
| Sihler 2002 | No comparison group (descriptive cohort of people who were "twice transferred" by HEMS) |
| Skogvoll 2000 | No comparison group |
| Slater 2002 | No outcomes reported |
| Snooks 1996 | Comparison of 3 different regional HEMS services |
| Spencer‐Jones 1993 | Descriptive study |
| Struck 2007 | Wrong design (questionnaire) |
| Taylor 2010 | Wrong design (systematic review) |
| Taylor 2011 | No outcomes reported (only examined costs) |
| Thomas 2000 | Descriptive study |
| Treat 1980 | No comparison group |
| Urdaneta 1984 | No comparison group |
| Urdaneta 1987 | No comparison group |
| Veenema 1995 | Not a HEMS study |
| Walcott 2011 | No comparison group |
| Williams 2003 | No comparison group |
| Wills 2000 | No comparison group |
| Wirtz 2002 | Examined HEMS crew configuration: nurse/nurse vs. paramedic/nurse |
| Yoon 2011 | Descriptive study |
| Young 1998 | No comparison group (scene vs. transfer of HEMS only) |
EMS: emergency medical service; GEMS: ground emergency medical service; HEMS: helicopter emergency medical service.
Differences between protocol and review
In the protocol for this review, we intended to include people with burns. After further deliberation, we decided to exclude these types of injuries. Only one study of people with burns would have met the inclusion criteria for this review (Hallock 1985).
The original protocol stated that Trauma‐Related Injury Severity Score (TRISS)‐based studies would be included even if a GEMS comparison group was not specified. Three studies did not have a GEMS comparison group and we excluded them. The approach to TRISS studies should have been described in more detail in the original protocol. Briefly, analysis of HEMS versus GEMS TRISS‐based studies relies on a three‐step process as originally described by Baxt et al (Baxt 1983). In this version of the review, we describe the TRISS‐study selection process in more detail.
Originally, we planned to use 30‐day mortality as the primary outcome of interest. The vast majority of studies only reported survival at discharge, and so we decided to use survival at hospital discharge instead.
In the protocol for this review, we intended to have a subgroup analysis based on Injury Severity Score. In the review, we have created three subgroups: 1. studies that used multivariate regression methods, 2. studies that used TRISS‐based methods, and 3. studies that used other methods for analysis.
Contributions of authors
DB ran the search for studies and screened some of the search results.
SG, ST, CS, DF, EH, JH, and PP conducted the review and contributed to the final manuscript.
Sources of support
Internal sources
No sources of support supplied
External sources
-
National Institutes of Health, USA.
Dr. Galvagno is supported by a T‐32 training grant administered by the National Institutes of Health.
Declarations of interest
SG was supported by a National Institutes of Health T‐32 Ruth Kirschstein Institutional Training Grant at the time this review was initiated.
DB, DF, CS, RS: None known.
ST: Competing interests include grant support from nonprofit organizations with an interest in furthering HEMS outcomes research, and medical directorship support for the past 20 years, from nonprofit and for‐profit HEMS services.
JH: Dr. Hirshon is partially funded through a contract with the Maryland Institute of Emergency Medicine Services Systems (MIEMSS). MIEMSS is the Maryland State Agency that supervises all helicopter EMS use. This contract is to assist with MIEMSS' data management and analysis, but does not directly relate to this work.
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
Abe 2014 {published data only}
- Abe T, Takahashi O, Saitoh D, Tokuda Y. Association between helicopter with physician versus ground emergency medical services and survival of adults with major trauma in Japan. Critical Care 2014;18:R146 (1‐8). [DOI] [PMC free article] [PubMed] [Google Scholar]
Andruskow 2013 {published data only}
- Andruskow H, Lefering R, Frink M, Mommsen P, Zeckey C, Rahe K, et al. Survival benefit of helicopter emergency medical services compared to ground emergency medical services in traumatized patients. Critical Care 2013;17:R124. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bartolacci 1998 {published data only}
- Bartolacci RA, Munford BJ, Lee A, McDougall PA. Air medical scene response to blunt trauma: effect on early survival. Medical Journal of Australia 1998;169:612‐6. [DOI] [PubMed] [Google Scholar]
Baxt 1983 {published data only}
- Baxt WG, Moody P. The impact of a rotorcraft aeromedical emergency care service on trauma mortality. JAMA 1983;249(22):3047‐51. [PubMed] [Google Scholar]
Baxt 1987 {published data only}
- Baxt WG, Moody P. The impact of advanced prehospital emergency care on the mortality of severely brain‐injured patients. Journal of Trauma: Injury, Infection, and Critical Care 1987;27(4):365‐9. [DOI] [PubMed] [Google Scholar]
Berlot 2009 {published data only}
- Berlot G, LaFata C, Bacer B, Biancardi B, Viviani M, Lucangelo U, et al. Influence of prehospital treatment on the outcome of patients with severe blunt traumatic brain injury: a single‐centre study. European Journal of Emergency Medicine 2009;16:312‐7. [DOI] [PubMed] [Google Scholar]
Biewener 2004 {published data only}
- Biewener A, Aschenbrenner U, Rammelt S, Grass R, Zwipp H. Impact of helicopter transport and hospital level on mortality of polytrauma patients. Journal of Trauma: Injury, Infection, and Critical Care 2004;56:94‐8. [DOI] [PubMed] [Google Scholar]
Braithwaite 1998 {published data only}
- Braithwaite CE, Rosko M, McDowell R, Gallagher J, Proenca J, Spott MA. A critical analysis of on‐scene helicopter transport on survival in a statewide trauma system. J Trauma 1998;45(1):140‐146. [DOI] [PubMed] [Google Scholar]
Brown 2010 {published data only}
- Brown JB, Stassen NA, Bankey PE, Sangosanya AT, Cheng JD, Gestring ML. Helicopters and the civilian trauma system: national utilization patterns demonstrate improved outcomes after traumatic injury. Journal of Trauma: Injury, Infection, and Critical Care 2010;69:1030‐6. [DOI] [PubMed] [Google Scholar]
Brown 2011 {published data only}
- Brown JB, Stassen NA, Bankey PE, Sangosanya AT, Cheng JD, Gestring ML. Helicopters improve survival in seriously injured patients requiring interfacility transfer for definitive care. Journal of Trauma: Injury, Infection, and Critical Care 2011;70:310‐4. [DOI] [PubMed] [Google Scholar]
Bulger 2012 {published data only}
- Bulger EM, Guffey D, Guyette FX, MacDonald RD, Brasel K, Kerby JD, et al. Impact of prehospital mode of transport after severe injury: a multicenter evaluation from the Resuscitation Outcomes Consortium. Journal of Trauma and Acute Care Surgery 2011;72(3):567‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]
Buntman 2002 {published data only}
- Buntman AJ, Yeomans KA. The effect of air medical transport on survival after trauma in Johannesburg, South Africa. South African Medical Journal 2002;92:807‐11. [PubMed] [Google Scholar]
Cunningham 1997 {published data only}
- Cunningham P, Rutledge R, Baker C, Clancy TV. A comparison of the association of helicopter and ground ambulance transport with the outcome of injury in trauma patients transported from the scene. Journal of Trauma: Injury, Infection, and Critical Care 1997;43(6):940‐6. [DOI] [PubMed] [Google Scholar]
Davis 2005 {published data only}
- Davis DP, Peay J, Serrano JA, Buono C, Vilke GM, Sise MJ, et al. The impact of aeromedical response to patients with moderate to severe traumatic brain injury. Annals of Emergency Medicine 2005;46:115‐22. [DOI] [PubMed] [Google Scholar]
Desmettre 2012 {published data only}
- Desmettre T, Yeguiayan JM, Coadou H, Jaquot C, Raux M, Vivien B, et al. Impact of emergency medical helicopter transport directly to a university hospital trauma center on mortality of severe blunt trauma patients until discharge. Critical Care 2012;16:R170. [DOI] [PMC free article] [PubMed] [Google Scholar]
Di Bartolomeo 2001 {published data only}
- Bartolomeo S, Sanson G, Nardi G, Scian F, Michelutto V, Lattuada L. Effects of 2 patterns of prehospital care on the outcome of patients with severe head injury. Archives of Surgery 2001;136:1293‐300. [DOI] [PubMed] [Google Scholar]
Frey 1999 {published data only}
- Frey C, Dula D, Escalante M. Outcomes associated with helicopter and ambulance transport of motor vehicle accident victims to trauma centers. American Journal of Epidemiology 1999;149(11):79. [Google Scholar]
Frink 2007 {published data only}
- Frink M, Probst C, Hildebrand F, Richter M, Hausmanninger C, Wiese B, et al. The influence of transportation mode on mortality in polytraumatized patients. An analysis based on the German Trauma Registry [German] [Einfluss des Transportmittels auf die Letalität bei polytraumatisierten Patienten]. Unfallchirug 2007;110:334‐40. [DOI] [PubMed] [Google Scholar]
Galvagno 2012 {published data only}
- Galvagno SM, Haut ER, Zafar SN, Millin MG, Efron DT, Koenig GJ, et al. Association between helicopter vs ground emergency medical services and survival for adults with major trauma. JAMA 2012;307(15):1602‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Giannakopoulus 2013 {published data only}
- Giannakopoulos GF, Kolodzinskyi MN, Christiaans HMT, Boer C, Lange‐de Klerk ESM, Zuidema WP, et al. Helicopter emergency medical services save lives: outcome in a cohort of 1073 polytraumatized patients. European Journal of Emergency Medicine 2013;20:79‐85. [DOI] [PubMed] [Google Scholar]
Koury 1998 {published data only}
- Koury SI, Moorer L, Stone K, Stapczynski JS, Thomas SH. Air vs ground transport and outcome in trauma patients requiring urgent operative interventions. Prehospital Emergency Medical Care 1998;2:289‐92. [DOI] [PubMed] [Google Scholar]
McVey 2010 {published data only}
- McVey J, Petrie DA, Tallon JM. Air versus ground transport of the major trauma patient: a natural experiment. Prehospital Emergency Care 2010;14:45‐50. [DOI] [PubMed] [Google Scholar]
Mitchell 2007 {published data only}
- Mitchell AD, Tallon JM, Sealy B. Air versus ground transport of major trauma patients to a tertiary trauma centre: a province‐wide comparison using TRISS analysis. Canadian Journal of Surgery 2007;50(2):129‐33. [PMC free article] [PubMed] [Google Scholar]
Moylan 1988 {published data only}
- Moylan JA, Fitzpatrick KT, Beyers J, Georgiade GS. Factors improving survival in multisystem trauma patients. Annals of Surgery 1988;207(6):679‐83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nardi 1994 {published data only}
- Nardi G, Massarutti D, Muzzi R, Kette F, Demonte A, Carnelos GA, et al. Impact of emergency medical helicopter service on mortality for trauma in north‐east Italy. European Journal of Emergency Medicine 1994;1:69‐77. [PubMed] [Google Scholar]
Newgard 2010 {published data only}
- Newgard CD, Schmicker RH, Hedges JR, Trickett JP, Davis DP, Bulger EM, et al. Emergency medical services intervals and survival in trauma: assessment of the "Golden Hour" in a North American prospective cohort. Annals of Emergency Medicine 2010;55:235‐46. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nicholl 1995 {published data only}
- Nicholl JP, Brazier JE, Snooks HA. Effects of London helicopter emergency medical service on survival after trauma. BMJ 1995;311:217‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Phillips 1999 {published data only}
- Phillips RT, Conaway C, Mullarkey D, Owen JL. One year's trauma mortality experience at Brooke Army Medical Center: is aeromedical transportation of trauma patients necessary?. Military Medicine 1999;164(5):361‐5. [PubMed] [Google Scholar]
Rose 2012 {published data only}
- Rose MK, Cummings GR, Rodning CB, Brevard SB, Gonzalez RP. Is helicopter evacuation effective in rural trauma transport?. American Surgeon 2012;78(7):794‐7. [PubMed] [Google Scholar]
Ryb 2013 {published data only}
- Ryb GE, Dischinger P, Cooper C, Kufera JA. Does helicopter transport improve outcomes independently of emergency medical system time?. Journal of Trauma and Acute Care Surgery 2013;74:149‐56. [DOI] [PubMed] [Google Scholar]
Schiller 1988 {published data only}
- Schiller WR, Knox R, Zinnecker H, Jeevanandam M, Sayre M, Burke J, et al. Effect of helicopter transport of trauma victims on survival in an urban trauma center. Journal of Trauma: Injury, Infection, and Critical Care 1988;28(8):1127‐33. [DOI] [PubMed] [Google Scholar]
Schwartz 1990 {published data only}
- Schwartz RJ, Lenworth MG, Juda RJ. A comparison of ground paramedics and aeromedical treatment of severe blunt trauma patients. Connecticut Medicine 1990;54(12):660‐2. [PubMed] [Google Scholar]
Stewart 2011 {published data only}
- Stewart KE, Cowan LD, Thompson DM, Sacra JC, Albrecht R. Association of direct helicopter versus ground transport and in‐hospital mortality in trauma patients: a propensity score analysis. Academic Emergency Medicine 2011;18:1208‐16. [DOI] [PubMed] [Google Scholar]
Sullivent 2011 {published data only}
- Sullivent EE, Faul M, Wald MW. Reduced mortality in injured adults transported by helicopter emergency medical services. Prehospital Emergency Care 2011;15:295‐302. [DOI] [PubMed] [Google Scholar]
Talving 2009 {published data only}
- Talving P, Teixeira PGR, Barmparas G, DuBose J, Inaba K, Lam L, et al. Helicopter evacuation of trauma victims in Los Angeles: does it improve survival?. World Journal of Surgery 2009;33:2469‐76. [DOI] [PubMed] [Google Scholar]
Thomas 2002 {published data only}
- Thomas SH, Harrison TH, Buras WR, Ahmed W, Cheema F, Wedel SK. Helicopter transport and blunt trauma mortality: a multicenter trial. Journal of Trauma: Injury, Infection, and Critical Care 2002;52:136‐45. [DOI] [PubMed] [Google Scholar]
von Recklinghausen 2011 {published data only}
- Recklinghausen FM. Comparing rural ground and air emergency medical services. Journal of Trauma Nursing 2011;18(4):241‐5. [DOI] [PubMed] [Google Scholar]
Weninger 2005 {published data only}
- Weninger P, Trimmel H, Herzer G, Nau T, Aldrian S, Vecsei V. Prehospital trauma care provided by HEMS or ground EMS: does it make a difference? [German]. Notfall & Rettungsmedizin 2005;8(3):171‐81. [Google Scholar]
References to studies excluded from this review
Abbott 1998 {published data only}
- Abbott D, Brauer K, Hutton K, Rosen P. Aggressive out‐of‐hospital treatment regimen for severe closed head injury in patients undergoing air medical transport. Air Medical Journal 1998;17(3):94‐100. [DOI] [PubMed] [Google Scholar]
Anderson 1987 {published data only}
- Anderson TE, Rose WD, Leicht MJ. Physician‐staffed helicopter scene response from a rural trauma center. Annals of Emergency Medicine 1987;16(1):58‐61. [DOI] [PubMed] [Google Scholar]
Baack 1991 {published data only}
- Baack BR, Smoot EC, Kucan JO, Riseman L, Noak JF. Helicopter transport of the patient with acute burns. Journal of Burn Care & Rehabilitation 1991;12(3):229‐33. [DOI] [PubMed] [Google Scholar]
Badiali 1989 {published data only}
- Badiali S, Cancellieri F, Fiandri MT, Gordini G, Loreti E, Pasini T. The impact of trauma care of EMS helicopter in the Bolonga area (Italy). Urgences Médicales 1989;8:23‐7. [Google Scholar]
Baxt 1985 {published data only}
- Baxt WG, Moody P, Cleveland HC, Fischer RP, Kyes FN, Leicht MJ, et al. Hospital‐based rotorcraft aeromedical emergency care services and trauma mortality: a multicenter study. Annals of Emergency Medicine 1985;14(9):859‐64. [DOI] [PubMed] [Google Scholar]
Boyd 1988 {published data only}
- Boyd CR, Corse KM. Outcome evaluation of trauma patients transported by a rural hospital‐based helicopter EMS program. Hospital Aviation 1988;7(7):14‐8. [Google Scholar]
Burney 1992 {published data only}
- Burney RE, Passini L, Hubert D, Maio R. Comparison of aeromedical crew performance by patient safety and outcome. Annals of Emergency Medicine 1992;21(4):375‐8. [DOI] [PubMed] [Google Scholar]
Cameron 1993 {published data only}
- Cameron PA, Flett K, Kaan E, Atkin C, Dziukas L. Helicopter retrieval of primary trauma patients by a paramedic helicopter service. Australian and New Zealand Journal of Surgery 1993;63:790‐7. [DOI] [PubMed] [Google Scholar]
Cannell 1993 {published data only}
- Cannell H, Silvester C, O'Regan MB. Early management of multiply injured patients with maxillofacial injuries transferred to hospital by helicopter. British Journal of Oral Maxillofacial Surgery 1993;31:207‐212. [DOI] [PubMed] [Google Scholar]
Carrel 1994 {published data only}
- Carrel M, Moeschler O, Ravussin P, Favre JB, Boulard G. Medicalisation prehospitaliere heliportee et agressions cerebrales secondarires d'origine systemique chez les traumatises craniocerebraux graves. Annales Françaises d'Anesthésie et de Réanimation 1994;13:326‐35. [DOI] [PubMed] [Google Scholar]
Chappell 2002 {published data only}
- Chappell VL, Mileski WJ, Wolf SE, Gore DC. Impact of discontinuing a hospital‐based air ambulance service on trauma patient outcomes. Journal of Trauma 2002;52:486‐91. [DOI] [PubMed] [Google Scholar]
Chipp 2010 {published data only}
- Chipp E, Warner RM, McGill DJ, Moiemen NS. Air ambulance transfer of adult patients to a UK regional burns centre: who needs to fly?. Burns 2010;36:1201‐7. [DOI] [PubMed] [Google Scholar]
Cleveland 1976 {published data only}
- Cleveland HC, Bigelow DB, Dracon D, Dusty F. A civilian air emergency service: a report of its development, technical aspects, and experience. Journal of Trauma 1976;16(6):452‐63. [PubMed] [Google Scholar]
Cocanour 1997 {published data only}
- Cocanour CS, Fischer RP, Caesar U. Are scene flights for penetrating trauma justified?. Journal of Trauma 1997;43(1):83‐8. [DOI] [PubMed] [Google Scholar]
Cudnik 2008 {published data only}
- Cudnik MT, Newgard CD, Wang H, Bangs C, Herrington R. Distance impacts mortality in trauma patients with an intubation attempt. Prehospital Emergency Care 2008;12:459‐66. [DOI] [PubMed] [Google Scholar]
Cummings 2000 {published data only}
- Cummings G, O'Keefe G. Scene disposition and mode of transport following rural trauma: a prospective cohort study comparing patient costs. Journal of Emergency Medicine 2000;18(3):349‐54. [DOI] [PubMed] [Google Scholar]
Dardis 2000 {published data only}
- Dardis R, Roberts G, Phillips J. A cost‐benefit evaluation of helicopter transfers to the Beaumont neurosurgical unit. Irish Medical Journal 2000;93(2):50‐1. [PubMed] [Google Scholar]
de Jongh 2012 {published data only}
- Jongh MAC, Stel HF, Schrijvers AJP, Leenen LPH, Verhofstad MHJ. The effect of helicopter emergency medical services on trauma patient mortality in the Netherlands. Injury 2012;43:1362‐7. [DOI] [PubMed] [Google Scholar]
De Wing 2000 {published data only}
- Wing MD, Curry T, Stephenson E, Palmieri T, Greenhalgh DG. Cost‐effective use of helicopters for the transportation of patients with burn injuries. Journal of Burn Care & Rehabilitation 2000;21(6):535‐40. [DOI] [PubMed] [Google Scholar]
Di Bartolomeo 2005 {published data only}
- Bartolomeo S, Sanson G, Nardi G, Michelutto V, Scian F. HEMS vs. ground‐BLS care in traumatic cardiac arrest. Prehospital Emergency Care 2005;9:79‐84. [DOI] [PubMed] [Google Scholar]
Dreyfuss 1979 {published data only}
- Dreyfuss UY, Faktor JH, Charnilas JZ. Aeromedical evacuation in Israel ‐ a study of 884 cases. Aviation, Space, and Environmental Medicine 1979;50(9):958‐60. [PubMed] [Google Scholar]
Falcone 1998 {published data only}
- Falcone RE, Herron H, Werman H, Bonta M. Air medical transport of the injured patient: scene versus referring hospital. Air Medical Journal 1998;17(4):161‐5. [DOI] [PubMed] [Google Scholar]
Fischer 1984 {published data only}
- Fischer RP, Flynn TC, Miller PW, Duke JH. Urban helicopter response to the scene of injury. Journal of Trauma 1984;24(11):946‐51. [DOI] [PubMed] [Google Scholar]
Frankema 2004 {published data only}
- Frankema SPG, Ringburg AN, Steyerberg EW, Edwards MJR, Schipper IB, Vugt AB. Beneficial effect of helicopter emergency medical services on survival of severely injured patients. British Journal of Surgery 2004;91:1520‐6. [DOI] [PubMed] [Google Scholar]
Franschman 2012 {published data only}
- Franschman G, Verburg N, Brens‐Heldens V, Andriessen TMJC, Naalt J, Peerdeman SM, et al. Effects of physician‐based emergency medical services dispatch in severe traumatic brain injury on prehospital run time. Injury 2012;43:1838‐42. [DOI] [PubMed] [Google Scholar]
Gerhardt 2000 {published data only}
- Gerhardt RT, Stewart T, Lorenzo RA, Gourley EJ, Schreiber MA, McGhee JS. US Army air ambulance operations in El Paso, Texas: a descriptive study and system review. Prehospital Emergency Medicine 2000;4:136‐43. [DOI] [PubMed] [Google Scholar]
Hallock 1985 {published data only}
- Hallock GG, Okunski WJ. The role of the helicopter in management of the burned patient. Journal of Burn Care & Rehabilitation 1985;6(3):233‐5. [DOI] [PubMed] [Google Scholar]
Hoogerwerf 2013 {published data only}
- Hoogerwerf N, Valk JP, Houmes RJ, Christiaans HM, Geeraedts LMG, Schober P, et al. Benefit of helicopter emergency medical services on trauma patient mortality in the Netherlands. Injury 2013;44:274‐6. [DOI] [PubMed] [Google Scholar]
Hubner 1999 {published data only}
- Hubner BL. Evaluation of the Immediate Effects of Preclinical Treatment of Severely Injured Trauma Patients by Helicopter Trauma Team in the Netherlands [thesis]. Amstelveen, Netherlands: Vrije Universiteit, 1999. [Google Scholar]
Irola 2006 {published data only}
- Irola TT, Laaksonen MI, Vahlberg TJ, Palve HK. Effect of physician‐staffed helicopter emergency medical service on blunt trauma patient survival and prehospital care. European Journal of Emergency Medicine 2006;13:335‐9. [DOI] [PubMed] [Google Scholar]
Jacobs 1999 {published data only}
- Jacobs LM, Gabram SGA, Sztajnkrycer MD, Robinson KJ, Libby MCN. Helicopter air medical transport: ten‐year outcomes for trauma patients in a New England program. Connecticut Medicine 1999;63(11):677‐82. [PubMed] [Google Scholar]
Jenkinson 2006 {published data only}
- Jenkinson E, Currie A, Bleetman A. The impact of a new regional air ambulance service on a large general hospital. Emergency Medicine Journal 2006;23:368‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Karanicolas 2006 {published data only}
- Karanicolas PJ, Bhatia P, Williamson J, Malthaner RA, Parry NG, Girotti MJ, et al. The fastest route between two points is not always a straight line: an analysis of air and land transfer of nonpenetrating trauma patients. Journal of Trauma 2006;61:396‐403. [DOI] [PubMed] [Google Scholar]
Kidher 2012 {published data only}
- Kidher E, Krasopoulos G, Coats T, Charitous A, Magee P, Uppal R, et al. The effect of prehospital time related variables on mortality following severe thoracic trauma. Injury 2012;43(9):1389‐92. [DOI] [PubMed] [Google Scholar]
Kruesathit 2012 {published data only}
- Kruesathit O, Laopaiboon M, Chadbunchachai W. Capability of emergency medical service response teams at Kohn Kaen, Thailand. Research Journal of Medical Sciences 2012;6(5):232‐7. [Google Scholar]
Kurola 2002 {published data only}
- Kurola J, Wangel M, Uusaro A, Ruokonen E. Paramedic helicopter emergency service in rural Finland ‐ do benefits justify the cost. Acta Anaesthesiologica Scandinavica 2002;46:779‐84. [DOI] [PubMed] [Google Scholar]
Lossius 2002 {published data only}
- Lossius HM, Soreide E, Hotvedt R, Hapnes A, Eilesen OV, Forde OH, et al. Prehospital advanced life support provided by specially trained physicians: is there a benefit in terms of life years gained?. Acta Anaesthesiologica Scandinavica 2002;46:771‐78. [DOI] [PubMed] [Google Scholar]
Mackenzie 1979 {published data only}
- Mackenzie CF, Shin B, Fisher R, Cowley RA. Two‐year mortality in 760 patients transported by helicopter direct from the road accident scene. American Surgeon 1979;45(2):101‐8. [PubMed] [Google Scholar]
Mann 2002 {published data only}
- Mann NC, Pinkney KA, Price DD, Rowland D, Arthur M, Hedges JR, et al. Injury mortality following the loss of air medical support for rural interhospital transport. Academic Emergency Medicine 2002;9(7):694‐8. [DOI] [PubMed] [Google Scholar]
Margolis 2009 {published data only}
- Margolis SA, Ypinazar VA. Aeromedical retrieval for critical clinical conditions: 12 years of experience with the Royal Flying Doctor Service, Queensland, Australia. Journal of Emergency Medicine 2009;36(4):363‐8. [DOI] [PubMed] [Google Scholar]
Massarutti 2006 {published data only}
- Massarutti D, Trillo G, Berlot G, Tomasini A, Bacer B, D'Orlando L, et al. Simple thoracostomy in prehospital trauma management is safe and effective: a 2‐year experience by helicopter emergency medical crews. European Journal of Emergency Medicine 2006;13:276‐80. [DOI] [PubMed] [Google Scholar]
Matsumoto 2006 {published data only}
- Matsumoto H, Mashiko K, Hara Y, Sakamoto Y, Kutsukata N, Takei K, et al. Effectiveness of a "doctor‐helicopter" system in Japan. Israel Medical Association Journal 2006;8:8‐11. [PubMed] [Google Scholar]
McCowan 2007 {published data only}
- McCowan CL, Swanson ER, Thomas F, Handrahan DL. Outcomes of blunt trauma victims transported by HEMS from rural and urban scenes. Prehospital Emergency Care 2007;11:383‐8. [DOI] [PubMed] [Google Scholar]
McCoy 2013 {published data only}
- McCoy CE, Menchine M, Sampson S, Anderson C, Kahn C. Emergency medical services out‐of‐hospital scene and transport times and their association with mortality in trauma patients presenting to an urban level 1 trauma center. Annals of Emergency Medicine 2013;61(2):167‐74. [DOI] [PubMed] [Google Scholar]
Melton 2007 {published data only}
- Melton JTK, Jain S, Kendrick B, Deo SD. Helicopter emergency ambulance service (HEAS) transfer: an analysis of trauma patient case‐mix, injury severity and outcome. Annals of the Royal College of Surgeons of England 2007;89:513‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Michel 1994 {published data only}
- Michel BC, Hout BA. Is het inzetten van helikopters met een traumateam bij ernstig gewonde ongevalsslachtoffers in Nederland kosteneffectif?. Nederlands Tijdschrift voor Geneeskunde 1994;138(46):2110‐5. [PubMed] [Google Scholar]
Moen 2008 {published data only}
- Moen KG, Klepstad P, Skandsen T, Fredriksli OA, Vik A. Direct transport versus interhospital transfer of patients with severe head injury in Norway. European Journal of Emergency Medicine 2008;15:249‐55. [DOI] [PubMed] [Google Scholar]
Munford 1994 {published data only}
- Munford B, Manning R. Paramedic helicopter retrieval of trauma patients. Australian and New Zealand Journal of Surgery 1994;64:640‐1. [DOI] [PubMed] [Google Scholar]
Nielsen 2002 {published data only}
- Nielsen EW, Ulvick A, Carlsen AW, Rannestad B. When is an anesthesiologist needed in a helicopter emergency medical service in northern Norway. Acta Anaesthesiologica Scandinavica 2002;46:785‐8. [DOI] [PubMed] [Google Scholar]
Norton 1996 {published data only}
- Norton R, Wortman E, Eastes L, Daya M, Hedges J, Hoyt J. Appropriate helicopter transport of urban trauma patients. Journal of Trauma 1996;41(5):886‐91. [DOI] [PubMed] [Google Scholar]
Nutbeam 2011 {published data only}
- Nutbeam T, Leaman A, Oakley P. Transporting major trauma patients from the margins of a UK trauma system. Emergency Medicine Journal 2011;29(3):182‐3. [DOI] [PubMed] [Google Scholar]
Palarcik 1991 {published data only}
- Palarcik J. Rozbor souboru ranenych prevezenych k hopspitalizaci do Vyzkumneho ustavu traumatologie a specialni chirurgie v Brne v obdobi. Cas Led Ces 1991;130:22‐3. [PubMed] [Google Scholar]
Papa 1993 {published data only}
- Papa G, Gulotta G, Costa P, Agro C, Biondo L, Mularo A, et al. Esperienza di primo soccorso con eliambulanza nei traumatizzati cranici. Minerva Anestesiologica 1993;59:787‐90. [PubMed] [Google Scholar]
Powell 1997 {published data only}
- Powell DG, Hutton K, King JK, Mark L, McLellan HM, McNab J, et al. The impact of a helicopter emergency medical services program on potential morbidity and mortality. Air Medical Journal 1997;16(2):48‐50. [DOI] [PubMed] [Google Scholar]
Purkiss 1994 {published data only}
- Purkiss SF, Williams M, Cross FW, Graham TR, Wood A. Efficacy of urgent thoracotomy for trauma in patients attended by a helicopter emergency medical service. Journal of the Royal College of Surgeons of Edinburgh 1994;39:289‐91. [PubMed] [Google Scholar]
Ringburg 2005 {published data only}
- Ringburg A, Frissen IN, Spanjersberg WR, Jel G, Frankema SPG, Schipper IB. Physician‐staffed HEMS dispatch in the Netherlands: adequate deployment or minimal utilization?. Air Medical Journal 2005;24(6):248‐51. [DOI] [PubMed] [Google Scholar]
Ringburg 2007 {published data only}
- Ringburg AN, Spanjersberg WR, Frankema SPG, Steyerberg EW, Patka P, Schipper IB. Helicopter emergency medical services (HEMS): impact on on‐scene times. Journal of Trauma 2007;63:258‐62. [DOI] [PubMed] [Google Scholar]
Ringburg 2009 {published data only}
- Ringburg AN, Polinder S, Meulman TJ, Steyerberg EW, Lieshout EMM, Patka P, et al. Cost‐effectiveness and quality‐of‐life analysis of physician‐staffed helicopter emergency medical services. British Journal of Surgery 2009;96:1365‐70. [DOI] [PubMed] [Google Scholar]
Roberts 1970 {published data only}
- Roberts S, Bailey C, Vendermade JR, Marable SA. An airborne intensive care unit. Annals of Surgery 1970;172(3):325‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rouse 1992 {published data only}
- Rouse A. The effect of the Cornwall and Isles of Scilly helicopter ambulance unit on the ambulance services' ability to deliver acutely traumatized patients to hospital. Archives of Emergency Medicine 1992;9:113‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Salimi 2009 {published data only}
- Salimi J, Khaji A, Kashayar P, Bande MK. Helicopter emergency medical system in a region lacking trauma coordination (experience from Tehran). Emergency Medical Journal 2009;26:361‐4. [DOI] [PubMed] [Google Scholar]
Sampalis 1993 {published data only}
- Sampalis JS, Lavoie A, Williams JI, Mulder DS, Kalina M. Impact of on‐site care, prehospital time, and level of in‐hospital care on survival in severely injured patients. Journal of Trauma 1993;34(2):252‐61. [DOI] [PubMed] [Google Scholar]
Schiller 2009 {published data only}
- Schiller J, McCormack JE, Tarsia V, Shapiro MJ, Singer AJ, Thode HC, et al. The effect of a second helicopter on trauma‐related mortality in a county‐based trauma system. Prehospital Emergency Care 2009;13:437‐43. [DOI] [PubMed] [Google Scholar]
Schipper 2006 {published data only}
- Schipper I. Een nachtelijke traumahelikoter geen wezenlijke verbetering van acute hulpverlening. Nederlands Tijdschrift voor Geneeskunde 2006;150(30):1700‐1. [PubMed] [Google Scholar]
Schwab 1985 {published data only}
- Schwab CW, Peclet M, Zackowski SW, Holmes EM, Forrester JC, Hensleigh CN. The impact of an air ambulance system on an established trauma center. Journal of Trauma 1985;25(7):580‐6. [DOI] [PubMed] [Google Scholar]
Shatney 2002 {published data only}
- Shatney CH, Homan SJ, Sherck JP, Ho CC. The utility of helicopter transport of trauma patients from the injury scene in an urban trauma center. Journal of Trauma 2002;53:817‐22. [DOI] [PubMed] [Google Scholar]
Shepherd 2008 {published data only}
- Shepherd MV, Trethewy CE, Kennedy J, Davis L. Helicopter use in rural trauma. Emergency Medicine Australasia 2008;20:494‐9. [DOI] [PubMed] [Google Scholar]
Sihler 2002 {published data only}
- Sihler KC, Hansen AR, Torner JC, Kealey GP, Morgan LJ, Zwerling C. Characteristics of twice‐transferred, rural trauma patients. Prehospital Emergency Care 2002;6:330‐5. [DOI] [PubMed] [Google Scholar]
Skogvoll 2000 {published data only}
- Skogvoll E, Bjelland E, Thorarinsson B. Helicopter emergency medical service in out‐of‐hospital cardiac arrest ‐ a 10‐year population‐based study. Acta Anaesthesiologica Scandinavica 2000;44:972‐9. [DOI] [PubMed] [Google Scholar]
Slater 2002 {published data only}
- Slater H, O'Mara MS, Goldfarb IW. Helicopter transportation of burn patients. Burns 2002;28:70‐2. [DOI] [PubMed] [Google Scholar]
Snooks 1996 {published data only}
- Snooks HA, Nicholl JP, Brazier JE, Lees‐Mlanga S. The costs and benefits of helicopter emergency ambulance services in England and Wales. Journal of Public Health Medicine 1996;18(1):67‐77. [DOI] [PubMed] [Google Scholar]
Spencer‐Jones 1993 {published data only}
- Spencer‐Jones R, Thomas P, Stevens DB. Helicopter transfer of trauma patients: the Isle of Man experience. Injury 1993;24(7):447‐50. [DOI] [PubMed] [Google Scholar]
Struck 2007 {published data only}
- Struck MF, Hilbert P, Hofmann GO, Laubach W, Stuttmann R. Prahospitale prasenz der berufsgenossenschaftlichen unfallkliniken. Notfall & Rettungsmed 2007;10:362‐6. [Google Scholar]
Taylor 2010 {published data only}
- Taylor CB, Stevenson M, Jan S, Middleton PM, Fitzharris M, Myburgh JA. A systematic review of the costs and benefits of helicopter emergency medical services. Injury 2010;41:10‐20. [DOI] [PubMed] [Google Scholar]
Taylor 2011 {published data only}
- Taylor CB, Stevenson M, Jan S, Liu B, Tall G, Middleton PM, et al. An investigation into the cost, coverage and activities of helicopter emergency medical services in the state of New South Wales, Australia. Injury 2011;42(10):1088‐94. [DOI] [PubMed] [Google Scholar]
Thomas 2000 {published data only}
- Thomas SH, Harrison T, Wedel SK, Thomas DP. Helicopter emergency medical services roles in disaster operations. Prehospital Emergency Care 2000;4:338‐44. [DOI] [PubMed] [Google Scholar]
Treat 1980 {published data only}
- Treat RC, Sirinek KR, Levine BA, Pruitt BA. Air evacuation of thermally injured patients: principles of treatment and results. Journal of Trauma 1980;20(4):275‐9. [DOI] [PubMed] [Google Scholar]
Urdaneta 1984 {published data only}
- Urdaneta LF, Sandberg MK, Cram AE, Vargish T, Jochimsen PR, Scott DH, et al. Evaluation of an emergency air transport service as a component of a rural EMS system. American Surgeon 1984;50(4):183‐8. [PubMed] [Google Scholar]
Urdaneta 1987 {published data only}
- Urdaneta LF, Miller BK, Ringenberg BJ, Cram AE, Scott DH. Role of an emergency helicopter transport service in rural trauma. Archives of Surgery 1987;122:992‐6. [DOI] [PubMed] [Google Scholar]
Veenema 1995 {published data only}
- Veenema KR, Rodewald LE. Stabilization of rural multiple‐trauma patients at level 3 emergency departments before transfer to a level 1 regional trauma center. Annals of Emergency Medicine 1995;25(2):175‐81. [DOI] [PubMed] [Google Scholar]
Walcott 2011 {published data only}
- Walcott BP, Coumans JV, Mian MK, Nahed BV, Kahle KT. Interfacility helicopter ambulance transport of neurosurgical patients: observations, utilization, and outcomes from a quaternary level care hospital. PLoS One 2011;6(10):e26216. [DOI] [PMC free article] [PubMed] [Google Scholar]
Williams 2003 {published data only}
- Williams ME, Harries WJ. The effects of air ambulance admissions on orthopaedic trauma services in a single hospital. Injury 2003;34:13‐5. [DOI] [PubMed] [Google Scholar]
Wills 2000 {published data only}
- Wills VL, Eno L, Walker C, Gani JS. Use of an ambulance‐based helicopter retrieval service. Australian and New Zealand Journal of Surgery 2000;70:506‐10. [DOI] [PubMed] [Google Scholar]
Wirtz 2002 {published data only}
- Wirtz MH, Cayten CG, Kohrs DA, Atwater R, Larsen EA. Paramedic versus nurse crews in the helicopter transport of trauma patients. Air Medical Journal 2002;21:17‐21. [DOI] [PubMed] [Google Scholar]
Yoon 2011 {published data only}
- Yoon YH, Moon SW, Lee SW, Choi SH, Cho HJ, Kim JY. Helicopter emergency medical services: a report on the current status in a metropolitan area of South Korea. European Journal of Emergency Medicine 2011;18:176‐8. [DOI] [PubMed] [Google Scholar]
Young 1998 {published data only}
- Young JS, Bassam D, Cephas GA, Brady WJ, Butler K, Pomphrey M. Interhospital versus direct scene transfer of major trauma patients in a rural trauma system. American Surgeon 1998;64(1):88‐92. [PubMed] [Google Scholar]
Additional references
Baker 1976
- Baker SP, O'Neill B. The injury severity score: an update. Journal of Trauma 1976;16(11):882‐5. [DOI] [PubMed] [Google Scholar]
Baker 2006
- Baker SP, Grabowski JG, Dodd RS, Shanahan DF, Lamb MW, Li G. EMS helicopter crashes: what influences fatal outcome?. Annals of Emergency Medicine 2006;47:351‐6. [DOI] [PubMed] [Google Scholar]
Bledsoe 2005
- Bledsoe BE, Smith MG. Medical helicopter accidents in the United States: a 10‐year review. Journal of Trauma 2004;56(6):1325‐8. [DOI] [PubMed] [Google Scholar]
Bledsoe 2006
- Bledsoe BE, Wesley AK, Eckstein M, Dunn TM, O'Keefe MF. Helicopter scene transport of trauma patients with non life‐threatening injuries: a meta‐analysis. Journal of Trauma 2006;60(6):1257‐65. [DOI] [PubMed] [Google Scholar]
Butler 2010
- Butler DP, Anwar I, Willett K. Is it the H or the EMS in HEMS that has an impact on trauma patient mortality? A systematic review of the evidence. Emergency Medicine Journal 2010;27:692‐701. [DOI] [PubMed] [Google Scholar]
CDC 2010
- Centers for Disease Control and Prevention. 10 leading causes of death, United States. 1999‐2006, all races, both sexes, 2010. webappa.cdc.gov/sasweb/ncipc/leadcaus10.html (accessed 8 July 2015).
Champion 1990
- Champion HR, Copes WS, Sacco WJ, Lawnick MM, Keast SL, Bain LW, et al. The Major Trauma Outcome Study: establishing national norms for trauma care. Journal of Trauma 1990;30(11):1356‐65. [PubMed] [Google Scholar]
Chandran 2010
- Chandran A, Hyder AA, Peek‐Asa C. The global burden of unintentional injuries and an agenda for progress. Epidemiologic Reviews 2010;32(1):110‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cowley 1973
- Cowley R, Hudson F, Scanlan E, Gill W, Lally RJ, Long W, et al. An economical and proved helicopter program for transporting the emergency critically ill and injured patient in Maryland. Journal of Trauma 1973;13(12):1029‐38. [DOI] [PubMed] [Google Scholar]
Cowley 1979
- Cowley RA, Mergner WJ, Fisher RS, Jones RT, Trump BF. The subcellular pathology of shock in trauma patients: studies using the immediate autopsy. American Journal of Surgery 1979;45(4):255‐69. [PubMed] [Google Scholar]
Cunningham 1998
- Cunningham P, Rutledge R, Baker CC, Clancy TV. A comparison of the association of helicopter and ground ambulance transport with the outcome of injury in trauma patients transported from the scene. Journal of Trauma 1997;43(6):940‐6. [DOI] [PubMed] [Google Scholar]
Deeks 2003
- Deeks JJ, Dinnes J, D'Amico R, Sowden AJ, Sakarovitch C, Song F, et al. Evaluating non‐randomised intervention studies. Health Technology Assessment 2003;7(27):139. [DOI] [PubMed] [Google Scholar]
DiBartolomeo 2005
- DiBartolomeo S, Sanson G, Nardi G, Michelutto V, Scian F. HEMS vs Ground‐BLS care in traumatic cardiac arrest. Prehospital Emergency Care 2005;9:79‐84. [DOI] [PubMed] [Google Scholar]
Downs 1998
- Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non‐randomised studies of health care interventions. Journal of Epidemiology and Community Health 1998;52:377‐84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Floccare 2002
- Floccare DJ, Hankins DG. Chapter 50: air services. In: Kuehl AE editor(s). Prehospital Systems and Medical Oversight. 3rd Edition. Lenexa, KS, USA: National Association of EMS Physicians, 2002:567‐75. [Google Scholar]
Gabbe 2011
- Gabbe BJ, Lecky FE, Bouamra O, Woodford M, Jenks T, Coats TJ, et al. The effect of an organized trauma system on mortality in major trauma involving serious head injury: a comparison of the United Kingdom and Victoria, Australia. Annals of Surgery 2011;253:138‐43. [DOI] [PubMed] [Google Scholar]
Haas 2009
- Haas B, Jurkovich GJ, Wang J, Rivara FP, MacKenzie EJ, Nathens AB. Survival advantage in trauma centres: expeditious intervention or experience?. Journal of the American College of Surgeons 2009;208(1):28‐36. [DOI] [PubMed] [Google Scholar]
Haut 2006
- Haut ER, Chang DC, Efron D, Cornwell 3rd EE. Injured patients have lower mortality when treated by "full‐time" trauma surgeons vs. surgeons who cover trauma "part‐time". Journal of Trauma 2006;61(2):272‐9. [DOI] [PubMed] [Google Scholar]
Haut 2009
- Haut ER, Chang DC, Hayanga AJ, Efron DT, Haider AH, Cornwell 3rd EE. System‐based and surgeon‐based influences on trauma mortality. Archives of Surgery 2009;8:759‐64. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Altman DG, Sterne JAC. Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Kane 1985
- Kane G, Engelhardt R, Celentano J, Koenig W, Yamanaka J, McKinney P, et al. Empirical development and evaluation of prehospital trauma triage instruments. Journal of Trauma 1985;25(6):482‐9. [DOI] [PubMed] [Google Scholar]
Kerr 1999
- Kerr WA, Kerns TJ, Bissell RA. Differences in mortality rates among trauma patients transported by helicopter and ambulance in Maryland. Prehospital and Disaster Medicine 1999;14(3):159‐64. [PubMed] [Google Scholar]
Krug 2002
- Krug EG, Dhalberg LL, Mercy JA, Zwi AB, Lozano R (editors). World report on violence and health. World Health Organization 2002:1‐19.
Kruger 2010
- Kruger AJ, Skogvoll E, Castren M, Kurola J, Lossius HM, the ScanDoc Phase 1a Study Group. Scandinavian pre‐hospital physician‐manned emergency medical services ‐ same concept across borders?. Resuscitation 2010;81:427‐33. [DOI] [PubMed] [Google Scholar]
Lerner 2001
- Lerner EB, Moscati RM. The golden hour: scientific fact or medical urban legend. Academic Emergency Medicine 2001;8(7):758‐60. [DOI] [PubMed] [Google Scholar]
MacKenzie 2006
- MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, et al. A national evaluation of the effect of trauma‐centre care on mortality. New England Journal of Medicine 2006;354(4):366‐78. [DOI] [PubMed] [Google Scholar]
MacKenzie 2007
- MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, et al. The National Study on Costs and Outcomes of Trauma. Journal of Trauma 2007;63:S54‐67. [DOI] [PubMed] [Google Scholar]
McNabney 1981
- McNabney WK. Vietnam in context. Annals of Emergency Medicine 1981;10(12):659‐61. [DOI] [PubMed] [Google Scholar]
Murray 1996
- Murray CJ, Lopez A. The global burden of disease: I. A comprehensive assessment of mortality and disability from diseases, and injuries and risk factors in 1990 and projected to 2020. Cambridge, MA, USA: Harvard University Press, 1996. [Google Scholar]
Nathans 2000
- Nathens AB, Jurkovich GJ, Rivara FP, Maier RV. Effectiveness of state trauma systems in reducing injury‐related mortality: a national evaluation. Journal of Trauma 2000;48(1):25‐30. [DOI] [PubMed] [Google Scholar]
Osler 1997
- Osler T, Baker SP, Long W. A modification of the injury severity score that improves accuracy and simplifies scoring. Journal of Trauma 1997;43(6):922‐5. [DOI] [PubMed] [Google Scholar]
Reeves 2011
- Reeves BC, Deeks JJ, Higgins JPT, Wells G. Chapter 13: Including non‐randomised studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Ringburg 2009a
- Ringburg AN, Polinder S, Meulman TJ, Styerberg WE, Lieshout EM, Patka P, et al. Cost‐effectiveness and quality‐of‐life analysis of physician‐staffed helicopter emergency medical services. British Journal of Surgery 2009;96(11):1365‐70. [DOI] [PubMed] [Google Scholar]
Ringburg 2009b
- Ringburg AN, Thomas SH, Steyerberg EW, Lieshout EMM, Patka P, Schipper IB. Lives saved by helicopter emergency medical services: an overview of literature. Air Medical Journal 2009;28(6):298‐302. [DOI] [PubMed] [Google Scholar]
Roudsari 2008
- Roudsari B, Field C, Caetano R. Clustered and missing data in the US National Trauma Data Bank: implications for analysis. Injury Prevention 2008;14:96‐100. [DOI] [PubMed] [Google Scholar]
Sampalis 1999
- Sampalis JS, Denis R, Lavoie A, Frechette P, Boukas S, Nikolis A, et al. Trauma care regionalization: a process‐outcome evaluation. Journal of Trauma 1999;46(4):565‐79. [DOI] [PubMed] [Google Scholar]
Schluter 2010
- Schluter PJ, Nathens A, Neal ML, Gobel S, Cameron CM, Davey TM, et al. Trauma and Injury Severity Score (TRISS) coefficients 2009 revision. Journal of Trauma 2010;68(4):761‐70. [DOI] [PubMed] [Google Scholar]
Seegerer 1976
- Seegerer K. 10 years of the Munich Emergency Medical Service: organization and technic. MMW Muenchener medizinische Wochenschrift 1976;118(18):573‐8. [PubMed] [Google Scholar]
Shatz 2004
- Shatz DV, Delgado J. Civilian use of rotor wing medical transport has had its opponents. Journal of Trauma 2004;56(6):1325‐8. [DOI] [PubMed] [Google Scholar]
TARN 2011
- The Trauma Audit and Research Network. Ps09: an improved approach to outcome predictions. www.tarn.ac.uk/Content.aspx?c=1894 (accessed 24 March 2011).
Thomas 2003
- Thomas SH, Biddinger PD. Helicopter trauma transport: an overview of recent outcomes and triage literature. Current Opinions in Anaesthesiology 2003;16(2):153‐8. [DOI] [PubMed] [Google Scholar]
Thomas 2004
- Thomas SH. Helicopter emergency medical services transport outcomes literature: annotated review of articles published 2000‐2003. Prehospital Emergency Care 2004;8(3):322‐33. [DOI] [PubMed] [Google Scholar]
Thomas 2007
- Thomas SH. Helicopter emergency medical services transport outcomes literature: annotated review of articles published 2004‐2006. Prehospital Emergency Care 2007;11:477‐88. [DOI] [PubMed] [Google Scholar]
Wish 2005
- Wish JR, Long WB, Edlich RF. Better trauma care. How Maryland does it. Journal of Long‐Term Effects of Medical Implants 2005;15(1):79‐89. [DOI] [PubMed] [Google Scholar]
Wyatt 1998
- Wyatt JP, Beard D, Busuttil A. Quantifying injury and predicting outcome after trauma. Forensic Science International 1998;95(1):57‐66. [DOI] [PubMed] [Google Scholar]


