Abstract
Poorly ventilated indoor spaces pose a risk for airborne transmission of SARS-CoV-2. We measured carbon dioxide levels in a multiple areas in an acute care hospital to assess the adequacy of ventilation. Carbon dioxide levels remained below 800 parts per million in most areas but exceeded this level in a small conference room with 8 occupants, an office with 3 occupants, and a bathroom with 2 occupants. Measuring carbon dioxide levels could provide a simple means for healthcare facilities to assess the adequacy of ventilation.
Key words: COVID-19, Aerosol, Transmission
Poorly ventilated indoor spaces pose a risk for airborne transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and other respiratory viruses.1, 2, 3 One rapid and simple method to assess the adequacy of ventilation in occupied indoor settings is monitoring of carbon dioxide levels.1 , 2 The concentration of carbon dioxide in outdoor air is approximately 400 parts per million (ppm) versus approximately 40,000 ppm in exhaled breath.4 Thus, carbon dioxide levels rise in occupied spaces that are inadequately ventilated. Carbon dioxide monitoring has been used to identify measures to improve ventilation in settings such as schools and dental offices.4 , 5 For example, Wargocki and Da Silva5 used carbon dioxide sensors in classrooms to provide real-time visual feedback on air quality that was used to indicate when windows should be opened to improve ventilation.
In comparison to residential and commercial buildings, the risk for airborne transmission of SARS-CoV-2 may be relatively low in healthcare facilities due to requirements for increased ventilation in areas involving or affecting patient care.6 In 2 recent studies on COVID-19 wards, carbon dioxide levels were consistently below 800 ppm.7 , 8 However, other investigators have reported elevated carbon dioxide levels in hospitals, particularly in settings with increased room occupancy.9 Moreover, SARS-CoV-2 transmission in healthcare facilities often occurs in ancillary care and outpatient areas that might have suboptimal ventilation,10 and exposures frequently occur in areas such as breakrooms.11 Therefore, we monitored carbon dioxide levels in a wide range of settings in an acute care hospital to assess ventilation.
Methods
The assessment was approved by the Cleveland VA Medical Center's Infection Control Committee as a quality improvement project. The hospital engineering department maintains ventilation requirements throughout the facility in accordance with American Institute of Architects and American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE) recommendations.6 A minimum of 2 air changes of outdoor air per hour are maintained in clinical areas.
Using an IAQ-MAX COW Monitor and Data Logger (CO2Meter, Inc), carbon dioxide levels were continuously monitored and recorded every minute over 12 hours from 7 AM to 5 PM in the main lobby, cafeteria, physical therapy, and emergency department. The peak number of people present in these locations during monitoring was recorded. All measurements were taken during weekdays.
Using an Indoor Air Quality Carbon Dioxide Meter Model #CO240 (EXTECH Instruments), additional readings were obtained over 10-60-minute periods in inpatient rooms (N = 5), outpatient clinic rooms (N = 5), large (N = 1) and small (N = 1) conference rooms, breakrooms (N = 2), offices (N = 5), elevators (N = 2), and bathrooms (N = 4). Carbon dioxide levels were recorded every 5 seconds. The readings in conference rooms were recorded during routine educational conferences. The readings in the elevators were recorded during routine elevator operation. For the remaining sites, only study staff were present in the rooms. For the office measurements, the door was kept open for 8 minutes and then closed. For inpatient and clinic rooms, breakrooms, and bathrooms, the doors were kept closed.
Based on recommendations from the Centers for Disease Control and Prevention (CDC), carbon dioxide readings above 800 ppm were considered an indicator of suboptimal ventilation requiring intervention.1 If available, the expected air changes per hour (ACH) based on design specifications were recorded for the areas or rooms where carbon dioxide readings were taken.
Results
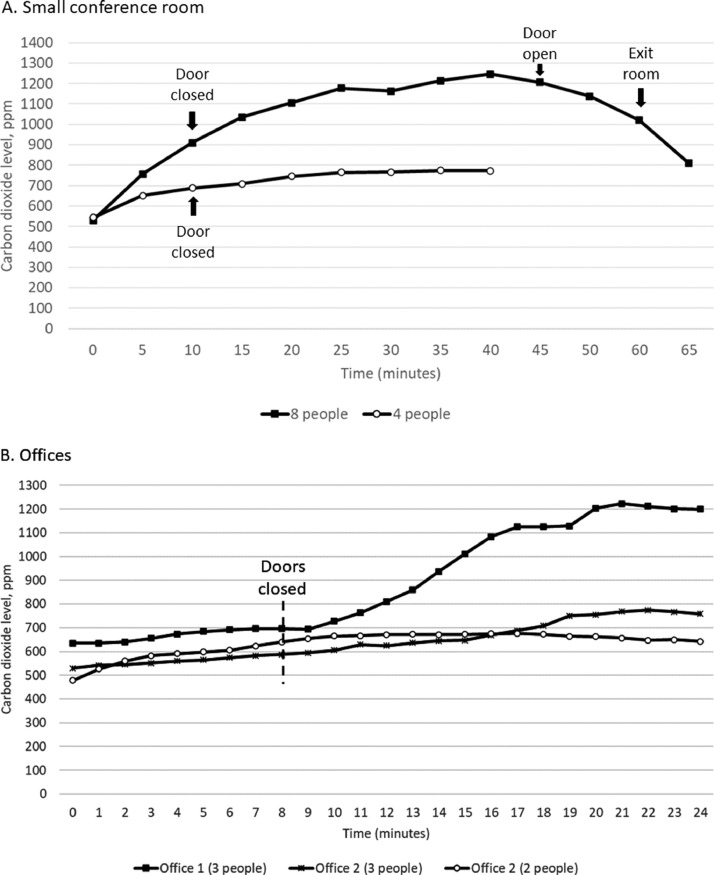
Table 1 shows the peak carbon dioxide levels, peak number of people present, and duration of monitoring for all the test sites. Peak carbon dioxide levels were below 800 ppm for all sites except a small conference room that was overcrowded during a meeting (Fig 1 A), in 1 of 5 offices tested when 3 occupants were present (Fig 1B), and in 1 of 4 bathrooms. In the small conference room (31 m3), the carbon dioxide level rose gradually and peaked at 1,246 ppm during a meeting that included 8 total participants; the meeting room normally seats 6 people. In the conference room, the carbon dioxide level rose above 800 ppm when the door was open; the carbon dioxide level continued to rise when the door was closed and decreased when the door was later opened (Fig 1A). In the same small conference room, the carbon dioxide level peaked at 774 ppm during a meeting with 4 total participants. It was possible to maintain ≥1.8 meters between all individuals with 4 occupants in the conference room, but not when 8 occupants were present (ie, ≥0.9 meters between all individuals).
Table 1.
Carbon dioxide levels in different areas in an acute care hospital
| Location (volume m3) | Peak carbon dioxide level (ppm) | Peak # people present | Time period monitored |
|---|---|---|---|
| Main lobby | 577 | 75 | 12 h (7 AM-5 PM) |
| Cafeteria | 756 | 68 | 12 h (7 AM-5 PM) |
| Physical therapy | 552 | 14 | 12 h (7AM-5 PM) |
| Emergency department* | 701 | 20 | 12 h (7AM-5 PM) |
| Elevators (N = 2) (8.5 m3) | 638 | 1 to 6 | 20 min |
| Large conference room (55.5 m3) | 638 | 37 | 60 min |
| Small conference room (31 m3) with overcrowding | 1246 | 8 | 60 min |
| Small conference room (31 m3) without overcrowding | 774 | 4 | 60 min |
| Breakrooms (N = 2) (52 m3) | ≤628 | 3 | 20 min |
| Office #1 (38.5 m3) | 1226 | 3 | 24 min |
| Offices (N = 4) (24.8 m3) | ≤788 | 3 | 24 min |
| Inpatient rooms (N = 5) (43 m3)† | ≤567 | 2 | 20 min |
| Outpatient clinic rooms (N = 5) (24 m3)‡ | ≤709 | 3 | 20 min |
| Bathrooms in patient care area (N = 3) | ≤636 | 2 | 10 min |
| Bathroom in patient care area (N = 1) | 908 | 2 | 10 min |
≥12 air changes per hour (ACH).
9 ACH.
6 ACH.
Fig 1.
Carbon dioxide levels in a small conference room (A) and in 2 offices (B) in an acute care hospital. The occupants entered the rooms at time 0. ppm, parts per million.
In the 5 offices tested, the carbon dioxide level remained below 800 ppm when the door was open with 2 or 3 people present (Fig 1B shows data for 2 offices). When 3 people were present, the carbon dioxide level rose in all offices after the door was closed, but only exceeded 800 ppm in 1 of the offices. This office routinely has 3 co-workers present and the door is usually closed; the 3 co-workers maintain ≥1.8 meters between individuals.
In 3 bathrooms, the carbon dioxide levels remained below 800 ppm when 2 people were present. However, in a fourth bathroom the carbon dioxide level rose to 908 ppm with 2 people present and spaced ≥1.8 meters apart. In inpatient rooms and in outpatient clinic rooms with 6-9 ACH, carbon dioxide levels remained less than 800 ppm when 2-3 people were present.
Discussion
Our findings suggest that ventilation in most areas of our hospital may be adequate to minimize the risk for airborne transmission of respiratory viruses.1 , 2 Carbon dioxide levels remained consistently below 800 ppm in most areas, including in the main lobby and cafeteria when more than 50 people were present. However, our results also highlight the fact that ventilation may be suboptimal in some areas or under certain conditions such as when a conference room or office is overcrowded or when doors are closed.
Our results also suggest that ventilation may vary considerably in locations such as offices, bathrooms, and conference rooms. Carbon dioxide levels rose above 800 ppm in 1 of 5 offices, 1 of 4 bathrooms, and 1 of 2 conference rooms tested. These findings suggest that measuring carbon dioxide levels in different areas with varying levels of occupancy may provide information that can be used to improve ventilation and/or adjust the maximum recommended occupancy. As noted previously, real-time feedback on carbon dioxide levels in school classrooms has been used to indicate when windows should be opened to improve air quality.5 The CDC has recommended that adjunctive measures such as portable air cleaners or upper room germicidal irradiation be considered in areas of buildings with suboptimal ventilation.1
In addition to ensuring adequate ventilation, wearing face masks and maintaining physical distancing of ≥1.8 meters are essential measures to minimize the risk for SARS-CoV-2 transmission in healthcare facilities.1 It is notable that in the overcrowded conference room where carbon dioxide levels rose above 800 ppm, it was not possible for the meeting participants to maintain appropriate physical distancing. Thus, efforts to ensure adequate spacing may have prevented the elevation of carbon dioxide above 800 ppm. However, carbon dioxide levels rose above 800 ppm in 1 office and 1 bathroom despite adequate physical distancing of ≥1.8 meters between occupants.
Our study has some limitations. Only a small number of offices and conference rooms were tested. Carbon dioxide levels in areas such as patient rooms and breakrooms were only assessed when 2-3 people were present. It is plausible that carbon dioxide levels might rise above 800 ppm if these areas are overcrowded. Many of the carbon dioxide measurements were collected over relatively short periods of 10-60 minutes. However, preliminary experiments demonstrated that carbon dioxide levels typically plateaued in hospital offices and conference rooms within 15 minutes when the number of occupants was stable. Elevated carbon dioxide levels have not been directly linked to SARS-CoV-2 transmission risk. However, poorly ventilated indoor spaces are generally considered high-risk areas.1, 2, 3 Although carbon dioxide levels below 800 ppm were considered an indicator of adequate ventilation based on CDC recommendations,1 others have suggested that levels should be below 700 ppm to minimize risk for airborne transmission of SARS-CoV-2.2 Finally, there is evidence that transmission of SARS-CoV-2 may occur in areas of healthcare facilities with adequate ventilation.12 For example, Chow et al.12 reported frequent transmission of SARS-CoV-2 from patients with unsuspected COVID-19 to roommates, particularly if aerosol-generating procedures were performed. Thus, adequate ventilation based on carbon dioxide measurements should not provide complete reassurance that airborne transmission will not occur.
Conclusion
Carbon dioxide measurements in healthcare facilities could provide a simple method to assess the adequacy of ventilation. Monitoring carbon dioxide levels is safe as the carbon dioxide is produced through natural respiration by personnel and patients. The concentration of carbon dioxide can be easily and rapidly measured with inexpensive carbon dioxide meters. Additional studies are needed to determine if interventions to improve ventilation based on carbon dioxide monitoring are effective in reducing transmission of SARS-CoV-2 and other respiratory viruses.
Footnotes
Funding/support: This work was supported by a Merit Review grant (CX001848) from the Department of Veterans Affairs to C.J.D.
Conflict of interest: C.J.D has received research grants from Clorox, Pfizer, and PDI. All other authors report no conflicts of interest relevant to this article.
References
- 1.Centers for Disease Control and Prevention. Ventilation in buildings. 2021. Accessed September 6, 2021. https://www.cdc.gov/coronavirus/2019-ncov/community/ventilation.html
- 2.Wang CC, Prather KA, Sznitman J, et al. Airborne transmission of respiratory viruses. Science. 2021;373:eabd9149. doi: 10.1126/science.abd9149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jones LD, Chan ER, Zabarsky TF, et al. Transmission of SARS-CoV-2 on a patient transport van. Clin Infect Dis. 2021:ciab347. doi: 10.1093/cid/ciab347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang Q, Marzouk T, Cirligeanu R, Malmstrom H, Eliav E, Ren YF. Ventilation assessment by carbon dioxide levels in dental treatment rooms. J Den Res. 2021;100:810–816. doi: 10.1177/00220345211014441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wargocki P, Da Silva NA. Use of visual CO2 feedback as a retrofit solution for improving classroom air quality. Indoor Air. 2015;25:105–114. doi: 10.1111/ina.12119. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Guidelines for environmental infection control in health-care facilities (2003). Appendix B: Air. Accessed September 6, 2021. https://www.cdc.gov/infectioncontrol/guidelines/environmental/appendix/air.html
- 7.Vosoughi M, Karami C, Dargahi A, et al. Investigation of SARS-CoV-2 in hospital indoor air of COVID-19 patients' ward with impinger method. Environ Sci Pollut Res Int. 2021;28:50480–50488. doi: 10.1007/s11356-021-14260-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kenarkoohi A, Noorimotlagh Z, Falahi S, et al. Hospital indoor air quality monitoring for the detection of SARS-CoV-2 (COVID-19) virus. Sci Total Environ. 2020;748 doi: 10.1016/j.scitotenv.2020.141324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Laurent MR, Frans J. Monitors to improve indoor air carbon dioxide concentrations in the hospital: a randomized crossover trial. Sci Total Environ. 2021 Oct 30 doi: 10.1016/j.scitotenv.2021.151349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jinadatha C, Jones LD, Choi H, et al. Transmission of SARS-CoV-2 in inpatient and outpatient settings in a Veterans Affairs health care system. Open Forum Infect Dis. 2021;8:ofab328. doi: 10.1093/ofid/ofab328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zabarsky TF, Bhullar D, Silva SY, et al. What are the sources of exposure in healthcare personnel with coronavirus disease 2019 infection? Am J Infect Control. 2021;49:392–395. doi: 10.1016/j.ajic.2020.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chow K, Aslam A, McClure T, et al. Risk of healthcare-associated transmission of SARS-CoV-2 in hospitalized cancer patients. Clin Infect Dis. 2021:ciab670. doi: 10.1093/cid/ciab670. [DOI] [PMC free article] [PubMed] [Google Scholar]