Abstract
Background:
Teledentistry is used in many countries to provide oral health services. However, using teledentistry to provide oral health services for older adults is not well documented. This knowledge gap needs to be addressed, especially when accessing a dental clinic is not possible and teledentistry might be the only way for many older adults to receive oral health services.
Types of Studies Reviewed:
Nine databases were searched, and 5,713 studies were screened using established eligibility criteria. Included studies were original research or review articles where the intervention of interest was delivered to an older adult population (age 60 and older) via teledentistry. Authors followed the “Preferred Reporting Items for Systematic reviews and Meta-Analyses” (PRISMA) extension for scoping review criteria.
Results:
Nineteen studies were identified that met the criteria for inclusion. Only one study was from the US. Seven studies had results focusing only on older adult participants, with most of those conducted in elder care facilities. The remainder consisted of studies with mixed-age populations reporting distinct results and/or information for older adults. The included studies used teledentistry, in both synchronous and asynchronous modes, to provide services such as diagnosis, oral hygiene promotion, assessment and referral of oral emergencies, and post-intervention follow-ups.
Practical implications:
The current use of teledentistry comprises a variety of promising applications. This review identifies and describes current uses, promising possibilities, and limitations of teledentistry to improve the oral health of older adults.
Keywords: Teledentistry, older adults, oral health status, telemedicine, telehealth
INTRODUCTION
The older adult population is growing rapidly globally. In the United States (US), the number of adults age 65 and older is expected to increase nearly two-fold over the next four decades from 52 million in 2018 to 95 million by 2060.1 Older adults develop chronic medical and dental conditions as they age and many older Americans have multiple chronic conditions including hypertension, arthritis, dyslipidemias, heart disease, diabetes, and mental health problems like Alzheimer’s disease and other forms of cognitive decline.2
Substantial improvements in preventive and restorative oral health care over the last five decades have helped older adults retain more of their natural dentition. In addition, the proportion and number of older adults has grown significantly. Consequently, the need for oral health services for older adults has grown, requiring comprehensive management of complex oral health conditions, including periodontal diseases, dental caries, root caries, xerostomia, oral mucosal lesions, and oral and pharyngeal cancers. These oral conditions can also be affected or exacerbated by coexisting systemic diseases.3 Access to oral health services is an important concern for many older adults, especially for those who are institutionalized, living in long-term care facilities, or for those living in rural areas.4-6
Telehealth has been defined by the World Health Organization as “The delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies, for the exchange of valid information for diagnosis, treatment, and prevention of disease and injuries, research and evaluation, and for the continuing education of health care providers, in all the interests of advancing the health of individuals and their communities.”7 When telehealth is applied in dental settings, the term teledentistry is generally used. Teledentistry is often directed at providing oral health services to vulnerable populations and facilitating access to specialty care. For example, the Eastman teledentistry program in New York state has successfully demonstrated a sustainable, cost-effective approach to providing oral health services to underserved children.8, 9 Potential benefits of teledentistry include enabling access to oral health services, decreasing cost of care, and reducing oral health disparities. 10, 11, 12,13, 14
The importance of telehealth (including teledentistry) has become more evident as a result of the dramatic impact of the COVID-19 pandemic on clinical care.15 Telehealth holds the promise of reaching many individuals, particularly those with compromised immune systems, underlying medical conditions, or concurrent family responsibilities such as child care, by avoiding unnecessary contact and enabling physical distancing. In recognition of this potential, the Federal Communication Commission (FCC) provided substantial funding for medical providers and health institutions to subsidize telehealth services during the COVID-19 pandemic.16 Oral health providers, by shifting from in-person visits to teledentistry, can eliminate the risk of infection transmission while providing important oral health services such as triaging orofacial problems, providing after-care follow-up, conducting screenings, and promoting oral health, especially to older adults and those home-bound or living in long-term care facilities—populations at high risk of severe complications when contracting COVID-19.
The topic of teledentistry and its application in older adults have not been studied widely. Therefore, we aim to systematically explore and describe the current literature on the various uses of teledentistry in older adults, including its reported effectiveness and limitations. This scoping review will provide opportunities to inform oral health clinicians and researchers regarding potential uses of teledentistry. A scoping review differs from a systematic review. A systematic review’s purpose is to focus on a specific question regarding existing practice by evaluating the literature systematically, resulting in a synthesis of the abstracted information to inform practice and policy.17, 18 A scoping review is an evaluation of the literature using a systematic methodology to determine the “scope” of published information on a topic and to identify and map the available evidence. Therefore, a scoping review serves as a precursor to a systematic review and can be helpful in identifying and analyzing knowledge gaps.17, 18
METHODS
We conducted a scoping review on the topic of teledentistry and geriatric oral health to assess key concepts and knowledge gaps in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR). A protocol was developed a-priori and we followed the preferred PRISMA-ScR reporting methodology to guide this scoping review.19
Review Questions
Two lines of inquiry guided this review:
What are the current uses and limitations of telehealth /teledentistry for the prevention, detection, diagnosis, and treatment of oral conditions, and for delivering oral health services to adults 60 years and older?
What are the differences (if any) between medical and dental settings in delivering oral health services through a teledentistry approach in terms of use, provider type, population served, and modalities used for service delivery (synchronous vs asynchronous)?
Operational Definitions
Telehealth:
A broad variety of technologies and applications to deliver virtual health care and education services via information technologies using, but not limited to, the following modalities: live video (synchronous), store-and-forward (asynchronous), remote patient monitoring (RPM), and mobile health (mHealth). For detailed definitions, please refer to (Supplemental Table 4). The term telehealth is an umbrella term that can be further defined when applied to various healthcare disciplines or specialties, including dentistry. 20
Teledentistry:
Providing oral health care services via telehealth technologies. According to one study, “Teledentistry can be defined as the remote provision of dental care, advice, or treatment through the medium of information technology, rather than through direct personal contact with any patient(s) involved.” 21
Healthcare providers (in this review):
A healthcare practitioner that delivers oral health care (e.g., intervention, education, consultation or any type of service) to improve oral health. They may include dentists, dental hygienists, physicians, physician assistants, nurse practitioners, nurses, or other health professionals meeting this definition.
Study Inclusion Criteria and Search Strategy
We included original research studies and review articles reporting on adults aged 60 and above with no sociodemographic restrictions using targeted oral health interventions and outcomes provided through any type of tele-modalities. Search strategies were developed and conducted in collaboration with a research librarian (AAL) following a comprehensive research methodology to retrieve citations and abstracts from large databases (Supplemental Tables 5-6). Searches were conducted in January 2020 and limited to articles published in English between 1991–2020. EndNote X9 (Clarivate Analytics) was used to manage citations.
Screening
Covidence 22, a web-based application, was used to manage and document the systematic review process. A pilot test on the eligibility criteria was conducted prior to study selection to measure agreement between the reviewers (MOB, DW). Good agreement was demonstrated for title and abstracts and full-text screening (82% and 91%, respectively). The reviewers identified publications independently using the specified and tested eligibility criteria. A third author (SB) reviewed and resolved disagreements. The same screening process was used for the full-text screening. The reference lists of the review articles remaining after the full-text screening stage were compiled independently by two authors (MOB, DW) to identify other articles of potential interest not already retrieved. The articles identified were screened independently (MOB, DW) using the previously defined eligibility criteria. Supplemental Tables 2-3 highlight the eligibility criteria used for screening.
Information Abstraction
Identification and extraction of defined data elements pertaining to oral health status and services was performed by one of the authors (MOB) and reviewed by three authors (DW, SB, BAD). Microsoft Excel was used for collation and storage of collected data. See Supplemental Table 1 for a list of data elements collected.
RESULTS
Search Results and Study Characteristics
5,713 articles were retrieved from the database searches, of which 3,396 were unique articles identified for screening. After title and abstract screening, 359 studies met the inclusion criteria; following full text screening, 19 studies remained and were reviewed for data extraction. Figure 1 shows the PRISMA-ScR inclusion and exclusion flow diagram for this review.
Figure 1:
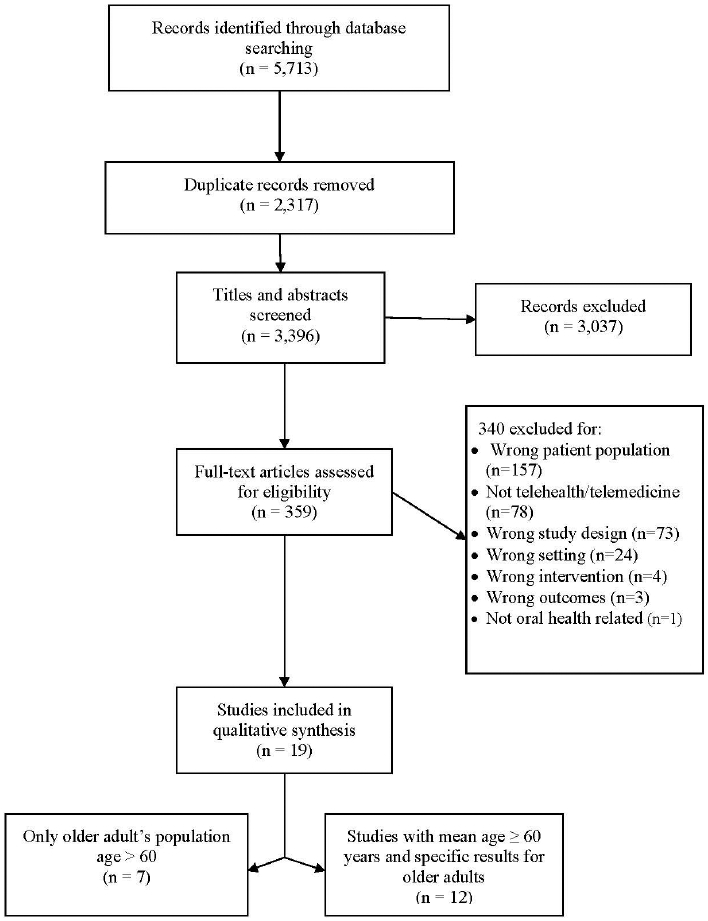
PRISMA-SCr flow diagram
General characteristics of the 19 reviewed studies are described in Table 1. Only one study was from the US. Seven studies focused on a teledentistry approach targeting older adults only. The remaining 13 studies included mixed-age populations, but reported separate results for older adults. Table 2 describes intervention modalities, settings, types of provider, and population description for 19 reviewed studies; Table 3 includes the study limitations, limitations of teledentistry, description of interventions or services provided, and results (success or effectiveness).
Table 1:
General Characteristics of 19 Reviewed Studies
| Author | Country | Study Population | Study Design | Objective(s) | Oral Health Outcome(s) | Relative Secondary Outcome |
|---|---|---|---|---|---|---|
| Alabi, R. O34 | Finland and Brazil | Older adults and other age groups | Observational with mixed retrospective and prospective designs | Use of Artificial Neural Networks along with a web-based-tool to estimate oral tongue squamous cell carcinoma recurrence | Oral cancer screening | N/A |
| Araujo, M. R35 | Portugal | Older adults and other age groups | Randomized Clinical Trial | Explore the effect of using an integrated camera while performing oral hygiene procedure followed up by consultation through text messages on the clinical and behavioral measures of patients with periodontal problems | Dental hygiene and bleeding on marginal probing | Social cognitive determinants of behavior change |
| Buser, R29 | Germany | Older adults only | Non-randomized clinical trial | Use of a purpose-built two-colored chewing gum in conjunction with smartphone application to assess chewing function | Chewing ability | N/A |
| Bradley, M40 | Ireland | Older adults and other age groups | Non-randomized clinical trial | Assess the feasibility of using Teledentistry to process oral medicine referral to a consultant at main hospital (Belfast) using photographs | Triage and management of oral medicine referrals | Acceptability of Teledentistry to both patient and provider (feasibility) |
| Cohen, L. A33 | USA | Older adults and other age groups | Cross-sectional | Examine the pharmacist’s role in managing dental pain from the patient’s perspective. | Tooth pain | N/A |
| Gomes, M. S38 | Brazil | Older adults and other age groups | Non-randomized clinical trial | Screening for a potential malignant lesion among individuals with high risk | Malignant lesions | N/A |
| Lyu, K. X36 | China | Older adults and other age groups | Randomized Clinical Trial | Investigate the practicability and advantage of WeChat mobile app in dental follow-up. | Head and neck tumor-related quality of life, and satisfaction with tele approach | Economic saving, satisfaction using both delivery models |
| Marino, R24 | Australia | Older adults only | Non-randomized clinical trial | Evaluate a Teledentistry model for teleconsultation and diagnosis inside nursing homes | 5-level Likert scale to assess acceptability, an economic evaluation based on general cost data | Screening for oral diseases and lesions, opinions of participants about the tele approach |
| Marino, R25 | Australia | Older adults only | Non-randomized clinical trial | Compare costs /benefits of Teledentistry versus in-person approach following assessments by a dentist at rural nursing homes | Cost saving, effectiveness and feasibility of access through Teledentistry at rural nursing homes | N/A |
| Petcu, R39 | France | Older adults and other age groups | Non-randomized clinical trial | Measure perception of oral teleconsultation among elder patients with cognitive and physical problems | Acceptance of oral teleconsultation service | N/A |
| Queyroux, A26 | France | Older adults only | Cross-sectional study | Assess the precision of Teledentistry for diagnosing dental pathology, assessing rehabilitation status of dental prostheses, and the chewing ability of older adults living in nursing homes | Oral conditions/lesions, chewing ability, dental prostheses rehabilitation | N/A |
| Shah, P31 | India | Older adults and other age groups | Cross-sectional | Assess technology-enabled non-invasive diagnostic screening (TES) utilizing smartphones and other medical devices in conjunction with routine health screenings | Dental conditions | Other medical conditions |
| Skandarajah, A32 | India | Older adults and other age groups | Cross-sectional | Assess an automatic tablet-supported portable microscope as an assistant tool for oral cancer screening | Oral cancer screening | N/A |
| Tomuro, K23 | Japan | Older adults only | Non-randomized clinical trial | Evaluate a telecare program for home-bound elderly in provision of education on oral and general health care. | Oral care knowledge and attitudes, selfcare skills, communication abilities | N/A |
| Tynan, A27 | Australia | Older adults only | Non-randomized clinical trial | Explore the impact and experience of an integrated oral health program using tele approach and oral health therapists | Oral health- related quality of life | N/A |
| Tynan, A28 | Australia | Older adults only | Non-randomized clinical trial | Dismantle barriers related to delivering oral health at nursing homes | Experience of older adults with tele approach at nursing homes, reduction of unnecessary appointments, compliance with oral health care plan | N/A |
| Vaishampayan, S41 | India | Older adults and other age groups | Non-randomized-clinical trial | Assess effectiveness of text messaging (SMS) for postoperative compliance in oral cancer patients, and the efficacy of self-examination for early identification of recurrent lesions | Patient self-examination of oral cancer/oral lesion recurrence | N/A |
| Worsley, D. J30 | UK | Older adults and other age groups | Cross-sectional | Assess government facility services during both in- and out-of-hours urgent dental service, including telephone triage provider and a sole clinical provider | Telephone consultation delivery, suitability of referral, acceptability of service, cost and relevance | N/A |
| Yamazaki, S37 | Japan | Older adults and other age groups | Non-randomized clinical trial | Evaluate systemic management of high-risk dental patients during dental procedures by the remote online hemodynamic monitoring system | Remote hemodynamic monitoring of medically high-risk patients in private dental offices | N/A |
Note: N/A: not applicable
Table 2:
Intervention Modalities, Settings, Types of Provider, and Population Description for 19 Reviewed Studies
| Author | Source | Modality / Type of Application |
Setting (hospital /university/health center/individual provider |
Type of Provider | Population Description |
|---|---|---|---|---|---|
| Alabi, R. O34 | Teledentistry | Asynchronous | Hospital service to the public | Dental provider with the help of artificial intelligence | Older adults and young adults with tongue squamous cell carcinoma |
| Araujo, M. R35 | Teledentistry | Synchronous | Private clinics | Dentist with the aid of dental hygienist | 18 years and above who have more than 20 teeth |
| Buser, R29 | Teledentistry | Asynchronous | Academic setting | Dental provider with the help of artificial intelligence | Older adults |
| Bradley, M40 | Teledentistry | Asynchronous | Community dental clinic | Oral medicine specialist, oral surgeon and general dentists | Mixed ages including older adults, patients with oral mucosal presentation |
| Cohen, L. A33 | Telehealth | Synchronous | Pharmacy | Pharmacist | Mixed ages including older adults, general participants have tooth pain |
| Gomes, M. S38 | Teledentistry | Asynchronous | Academic institution | Dentist | Mixed ages including older adults, high risk smoker patients aged 60-79 |
| Lyu, K. X36 | Telemedicine | Synchronous | Hospital | Physicians | Mixed ages including older adults, patients with tumor treatments |
| Marino, R24 | Teledentistry | Synchronous and Asynchronous | Nursing home | On-site nurse and remote dentist | Older adults living in nursing homes in rural areas Australia |
| Marino, R25 | Teledentistry | Synchronous and Asynchronous | Nursing home | On-site nurse and remote dentist | Older adults living in nursing homes in rural areas Australia |
| Petcu, R39 | Teledentistry | Asynchronous | Long term facilities, two facilities for older adults with severe intellectual - motor -psychotic illnesses | Dentist and nurse aid | Mixed ages including older adults, older adults with cognitive or physical impairment |
| Queyroux, A26 | Teledentistry | Asynchronous | Nursing home | Dentist and nurse aid | Older adults, nursing home residents with oral health complaints (self-reported or reported by caregiver) |
| Shah, P31 | Telehealth | Asynchronous | Primary care clinic | Group of clinicians including dentist | Mixed ages including older adults |
| Skandarajah, A32 | Telemedicine | Asynchronous | University research and primary care clinic | Pathologist | Mixed ages including older adults |
| Tomuro, K23 | Teledentistry | Asynchronous | Nursing home | Dentist | Older adult males, 4 older male adults living in the dwelling center |
| Tynan, A27 | Teledentistry | Synchronous along with integrated service at location | Nursing home | Dentist and oral health therapist | 250 older adults living at rural nursing homes |
| Tynan, A28 | Teledentistry | Synchronous along with integrated service at location | Nursing home | Dentist and oral health therapist | 250 older adults living at rural nursing homes |
| Vaishampayan, S41 | Teledentistry | Asynchronous | Community clinic | Oral oncologist | Mixed ages who had a previous treatment for oral cancer |
| Worsley, D. J30 | Teledentistry | Synchronous | Governmental agency UK NHS | Nurse or dental nurse | Mixed ages including older adults, patients with unscheduled service (without dentist) need made urgent call to triage service |
| Yamazaki, S37 | Telehealth | Synchronous | Dentist practice | Physician | Older adults visiting dental office with a need for medical monitoring |
Table 3.
Study Limitations, Teledentistry Limitations, Interventions/Services Provided, and Results for 19 Reviewed Studies
| Author | Study limitations | Limitations of Teledentistry | Description of Interventions or Services Provided | Results (Success/Effectiveness) |
|---|---|---|---|---|
| Alabi, R. O34 | The tool needed an extra validation from other datasets; based on limited dataset, some predictivity may be absent. | Artificial intelligence learning process required a larger number of cases to predict cases in an accurate way; and required a diverse database to build better results. | A supervised learning method (prognostic estimation) used to estimate recurrence of tongue carcinoma, then a web-based tool created based on neural network to produce prediction model for cancer recurrence. | Online asynchronous prediction tool was able to predict 90% of oral squamous cell carcinoma recurrence, the Azure web-based tool could be used to evaluate cases remotely. |
| Araujo, M. R35 | Possible selection bias, participants recruited through advertisement | Text messaging may not be a favorable method for older adults even though the results showed no significant difference from younger participants. | Intra-oral camera and text messages used to influence the dental hygiene behavior (through dental hygiene consultation), boost frequency of dental hygiene, and decrease bleeding on marginal probing. | Improvement in the interproximal flossing and tooth brushing habit was attained in both intra-oral camera and text messaging groups, a 70% reduction in bleeding on probing. All gained results were sustained after 8 months. The study did not show significant difference between age groups over time. |
| Buser, R29 | Not mentioned | Not mentioned | Patients chewed special gum for specific time, and then a Maximum Voluntary Bite Force (MVBF) measured. Then, gums were evaluated using a smartphone software. | The use of the two-colored chewing gum would provide a fast, simple and inexpensive method for assessment of masticatory performance, which could be used in geriatric wards or in private practices without requiring specialized equipment or trained staff (web-based or smartphone app could aid in diagnosis and assessment process remotely). |
| Bradley, M40 | Small sample size, one assessment with the consultant, asynchronous diagnosis based on photos provided, biopsy was not possible at the point of care | A small percentage of the patients’ video clips were problematic. A more rigorous study using advanced method required with more details. | Consultant provided appropriate diagnosis based on the photographs provided by the remote location | Communicating cases with the consultant was feasible and provided access to the participants. Half of the participants were able to manage their conditions remotely with the help of local dental provider. Only 20 participants required urgent care at hospital. |
| Cohen, L. A33 | Not mentioned | The type of provider was not dental provider (pharmacists); and presence of language barrier | Telephone consultation with a pharmacist regarding pain | Older adults aged 64 and older were least likely to speak to a pharmacist compared with middle-aged groups; similar results also noticed among the younger population aged 21-34 years. |
| Gomes, M. S38 | Not mentioned | Knowledge among Brazilians regarding oral cancer was not yet widespread to use such approach; dentists’ performance and knowledge of technical issues were not adequate. | Oral lesions screening and diagnosis | High sensitivity, specificity and accuracy obtained during lesions screening and diagnosis as compared with the gold-standard. The positive predictive values were between 71% and 100% and the negative predictive values between 93% and 100%. |
| Lyu, K. X36 | Not mentioned | Due to inadequate technology usability, older adults may depend on care providers to implement; also, poor literacy regarding this approach | Follow-up consultation through a WeChat app or phone calls (for head and neck tumor patients) for 6 months | Quality of life head and neck tumor |
| Marino, R24 | Convenience sample of 50 | There were obstacles to implementation largely due to human factors. | Screening patients at nursing homes for oral diseases and pathological conditions | Intra-examiner agreement for screened conditions were excellent (kappa=0.83), and majority of older adults were satisfied with the tele approach. |
| Marino, R25 | Not mentioned | Older adults needed support to use technology. There was a need to increase internet knowledge, and perceived usefulness. | Access to dental care for older adults living in nursing homes | No difference in terms of cost was observed between the two approaches. Tele approach showed potential to solve access issue for the population living in nursing homes. |
| Petcu, R39 | Nurses collected data (data validity depended on nurse’s subjective judgment) | Observational data collection by nurses may lead to human error. Reliability of the data depended on the level of professionalism and engagement of the medical personnel involved in the study. | Teleconsultations of dental problems and measuring patients’ acceptance of tele approach | 92% completed the consultation process, older adults with psychotic problems perceived the service as negative experience while non-psychotic elders had an overall positive experience. |
| Queyroux, A26 | Used same provider to do both assessments which should be blinded. | Not all patients were able to attend the dental clinic. | Patient received 2 examinations. Each patient served as his/her own, individual control. The first assessment consisted of the dentist establishing a diagnosis remotely by reviewing a video recorded in the nursing home. The second examination occurred face-to-face within a maximum of 7 days by the same dentist who made the initial diagnosis. | Sensitivity and specificity of using Teledentistry to diagnose dental pathology was very high. |
| Shah, P31 | Not mentioned | Not mentioned | Tele diagnosis of oral health conditions among other medical problems | A statistically higher prevalence of dental diseases was measured in 65–90-year-old and 40–64-year-old compared with 18-39-year-old. |
| Skandarajah, A32 | Not mentioned | Brush biopsy technique is considered sensitive (sensitivity of 70%). | Screening and diagnosis of oral lesions, performing oral biopsy (using brush) and uploading biopsy images to the server where it can be reviewed by a pathologist later | High agreement reached by 2 pathologists screened the cell scope images derived from patients (both cytology and histology). |
| Tomuro, K23 | Very small sample (4 participants only) | Older technological approach, where internet connection is limited, can be solved by fast internet connection | Distance tutorials given to older male adults and their families, color-coded oral risk assessment, tooth brushing demonstration, text-based education, eating instructions, psychological motivation, reducing the burden on the caregiver | Qualitative changes were observed in the seven evaluation topics, consisted of knowledge of oral care, self-care skill, attitudes toward oral care, communication ability, impact on the community, oral and general health, and diet. |
| Tynan, A27 | Mixed methods | Many barriers were observed; not enough time for the staff to focus on management of the program; and some facilities not properly equipped. | Teledentistry along with integrative approach to improve access to oral health services, and ultimately improve oral health | The intervention helped the facilities meet accreditation standards for oral health, and improved access to oral health services for older adults living in ECFs. No significant difference between intervention and control groups in terms of GOHAI scores. |
| Tynan, A28 | Not mentioned | Associated costs, management issues and need for attendance | Teledentistry along with integrative approach implemented by a visiting oral health therapist to initiate oral health screening and provide oral health promotion. If there was a need for a dentist visit, it conducted through Teledentistry model | Positive feedback received from both residents and staff. Intervention led to increased awareness among residents about their oral health needs. |
| Vaishampayan, S41 | Not mentioned | SMS may not be the favorite method of communication among older adults. | After teaching the MSE method, the participants stimulated through SMS for consistent time to perform MSE | A number of participants reported recurrence of the disease but were normal after confirmatory examination. Education was the only factor associated with both clinical concordance and compliance. |
| Worsley, D. J30 | Cross-sectional | Patient satisfaction issues | During and after-hours telephone triage service | Majority of calls received needed advice and triage only, the rest of calls referred to dentist for urgent treatment. Service utilized mostly by people living in deprived areas. Fewer people over 54 used the service; it was mostly used by people aged 20-44. |
| Yamazaki, S37 | Not mentioned | Advanced technical support needed | Medical condition of older adults monitored through tele approach during dental visit to avoid any serious consequences | Common problems were hypertension, heart disease, and diabetes. |
Of the seven studies comprising only older adults, all took place at elder care facilities (ECF) 23-29. One study attempted to evaluate the feasibility of teledentistry to provide access solutions, including teleconsultation and telediagnosis.24 Another study aimed to provide dental education through a synchronous modality (live audio/video connection). Two studies explored the feasibility and cost of implementing teledentistry in ECFs.24, 25 Another study used mixed methods to examine the impact of Teledentistry, through an integrated oral health program, on older adults' oral health-related quality of life measured by the geriatric oral health assessment index (GOHAI).27 The program employed visiting oral health therapists (an oral health professional dual qualified in dental therapy and dental hygiene in Australia) for screening, education, and referral to a dentist for a remote real-time oral examination if needed.27 A follow-up study measured the impact of teledentistry services on number of avoidable dental visits, staff and residents’ feedback on program experience, compliance with oral health care plan implementation, and potential cost saving.28 The last study evaluated the accuracy of the teledentistry service model in diagnosing oral pathologies, evaluating chewing ability, and assisting with the prosthetic rehabilitation for older adults living in ECFs.26
Twelve studies involved mixed-age populations.30-41 We included these studies after careful examination of the reported methods and results to ensure that information about teledentistry uses, interventions, and limitations specific to older adults' oral health were clearly described. One randomized clinical trial (RCT) investigated the effect of using a remote intra-oral camera (IOC) along with text messaging during and after dental hygiene visits to assess bleeding on probing.35 Another RCT examined the feasibility of conducting a teleconsultation through the “WeChat” messaging application to monitor lesion recurrences in patients with head and neck tumors.36 The extent of patient satisfaction, cost, and time associated with the intervention were reported.36 Two non-RCTs tested the potential use and feasibility of teledentistry to provide triage and referral for suspected oral malignant lesions.38, 40 Another non-RCT examined perception and acceptance of oral teleconsultation among patients with cognitive and physical problems.39
One cross-sectional study examined the screening of oral cancer lesions using a tablet-based mobile microscope;32 while another cross-sectional study applied opportunistic screening of oral health conditions by using a mobile technology, approved by the Food and Drug Administration (FDA), to capture diagnostic oral images.31 The remaining three cross-sectional studies used teledentistry to solve a variety of problems among a population of older adults. The first provided an insight into how urgent dental care triage services in the United Kingdom (UK) offered remote and after-hours consultations, and provided referrals if needed.30 A US study examined the pattern of consultations that people of low economic status sought from pharmacists to manage severe tooth pain.33 Lastly, a Japanese study attempted to use a telemedicine service provided by a physician to monitor and manage dental patients with challenging medical conditions during a dental visit. 37
Interventions and Findings
Table 3 shows a summary of various interventions and reported results of the 19 studies reviewed. The main findings are organized into nine domains as follows:
Oral Health Knowledge, Attitudes, Efficacy:
The self-efficacy related to oral health, oral health knowledge, and attitudes of the older adults showed improvement after delivery of oral health promotion materials using an Interactive learning telecare application.23 Additionally, improvements were observed among older adults living in an ECF, where participants' oral hygiene habits including brushing behavior such as brush grasp, increased power, number of strokes, and brushing frequency improved after intervention delivery. Finally, measured oral health knowledge increased after the tele-demonstration of a color-coded cancer risk assessment tool kit.23
Access to Oral Care:
Accessibility issues were addressed through a variety of methods. An access problem experienced by older adults living at a residential ECF was solved by developing a teleconsultation treatment model. Nurses deployed at the facility delivered oral health prevention intervention under the supervision of a remote dentist. Intra-examiner agreement was high (kappa=0.83) between Teledentistry and face-to-face models.24 In a similar study, the cost of facilitating and implementing teleconsultation was similar to the face-to-face model. Also, cost reductions as a result of reducing avoidable dental visits was similar to the previous “nurse with the guidance of remote dentist” model. 25
Another teledentistry model targeted an underserved population in the UK through a dedicated teleconsultation phone number, with advice and referral provided in an average of 60 seconds. Most callers received advice and a small portion required urgent referral to an emergency service provider. However, older adults used the service to a lesser extent compared to the younger population. The study also reported decreased use of resources (avoiding unnecessary travel and reducing time for services) as result of telephone consultation service.30 Another study described a prototype asynchronous video system that screened and triaged a majority of older adults within a participating community in Ireland. It successfully identified urgent cases needing treatment in a hospital setting (20%), and referred other patients to a remote consultant specialist.40 In one study, older adults with complex medical conditions were monitored during their dental visits using a synchronous telemedicine approach to prevent adverse events. The majority of patients reported feeling safe and relaxed during the dental visit.37
Oral Self-Care:
After a brief demonstration of how to perform an oral self-examination, text messaging was deployed to patients with oral squamous cell carcinoma to maintain proper follow-up and to identify lesion recurrences. About 7% of the recruited patients reported having a recurrence that was subsequently confirmed by a dentist. The remainder of the conditions reported were either mucositis or ulcers.41 In another study,23 patients reported increased healthy oral habits after implementation of a tele-video interactive system about oral hygiene and proper oral care measures.
Diagnosis of Oral Health Conditions:
One study described screening of electronic images for multiple medical problems (including oral health conditions) by medical providers among participants of mixed ages. Many oral health conditions were identified, with oral pathologies being more prevalent among older adults compared to younger participants.31 In another study, oncologists utilized medical visits to perform opportunistic oral health tele-screening using a biopsy device synchronized with an online web-based portal. Specimens from participants were successfully diagnosed by two remote pathologists with high inter-examiner agreement (90%).32 A unique diagnostic method using Artificial Intelligence (AI) was used to predict the recurrence of squamous cell carcinoma of the tongue. High accuracy (92%) in predicting lesion recurrence was attained, using a group of predictive factors for lesion recurrence.34 Lastly, a study relying on synchronous video capture to diagnose oral lesions among dependent elders living in ECFs demonstrated high sensitivity (93.8%) and specificity (94.2%) compared to a face-to-face approach.26
Oral Function Assessment:
A variety of oral functions were assessed using asynchronous and synchronous modalities. For example, in one study synchronous tele-education was used to monitor and improve the technique used by care providers to feed residents in an ECF.23 Other studies examined the possibility of assessing oral functions through teledentistry. One of these studies used asynchronous video recorded by a nurse and evaluated remotely by a dentist. This method enabled assessment of chewing ability with high sensitivity and specificity (85.0% and 82.8%, respectively).26 In the same study, the prevalence of dental functional units was 70.7% and 94.6% of them were captured by using an integrated oral camera and digital video recorder.26 A third study synchronously evaluated chewing efficiency in older adults through an integrated chewing-gum and optoelectronic evaluation using a smartphone application. This method showed high agreement with a more complex gold standard method for classifying dental status and chewing efficiency of older adult participants.29
Oral Health-Related Quality of Life:
A mixed-methods comparative study examined the impact of a Teledentistry model using oral health therapists to deliver oral health screening, education, and referral for older adults living in ECFs. Although the authors didn’t find a significant difference between the intervention and control groups in terms of GOHAI scores, the integrated oral health program utilizing this model demonstrated potential to improve the oral health outcomes of ECFs’ residents.27
Emergency Management:
A US-based research examined a new telehealth method for managing tooth pain among a mixed-age cohort; in this study, low income patients consulted with pharmacists regarding tooth pain management. About 90% of patients followed the pharmacists’ advice. It was noted that older adults were among the least likely group to seek consultation using this model compared to younger age groups.33
Periodontal Care:
In one study, providers motivated adults of all ages by sharing their intra-oral images using text messages; this was an effective way to improve oral health behavior and reduce bleeding on marginal probing in an eight-month randomized trial. Authors reported no significant outcome differences between older adults patients receiving traditional care and those receiving text messaging.35
Teledentistry Acceptance:
Acceptance of teledentistry was reported in several studies and on-site provider acceptance was favorable. Older adults with no cognitive or physical problems generally accepted teledentistry approaches, such as phone calls and text messaging. Older adults with these conditions showed some refusal either before or during the interventions. In one study, when nurses used an intra-oral camera to capture oral images to be transferred to a remote dentist, about 28% of older adults did not fully cooperate and 7% refused the intervention.39 In another study, the majority of older adults participants with no cognitive impairment (94%) were either moderately or strongly satisfied with the remote teleconsultation. A small portion of the participants (16%) reported slight dissatisfaction with the way dentists handled their oral health needs.24
DISCUSSION
Technologies used for teledentistry range from simple text messaging or phone call follow-up to more sophisticated tele-video conferencing utilizing an intra-oral camera or live monitoring device to capture and transmit live images. These telehealth methods could allow programs with limited resources to deliver targeted interventions to older adults. The availability of AI tools may introduce additional opportunities for enhancing risk identification and diagnostic services, particularly in cases of specialty shortage, distance, and patient mobility problems; or as exemplified during the COVID-19 pandemic when social distancing is necessary and older adults are more cautious about going out in public. ECFs can collaborate with academic and research institutions to build tailored AI tools to help deliver precision oral health services.
Studies that examined older adults within ECFs focused on facilitating access to dental expertise for the purpose of diagnosis, consultation and oral health promotion. Teledentistry is an acceptable option to provide access to the proper diagnosis and management of oral health conditions. This is of unique value during times of restricted access to oral health services due to mobility limitations and/or comorbidities among older adults.
Conversely, studies that included a mixed-age population had a broader scope of interventions, including urgent tooth pain management, oral conditions triage and referral, oral health promotion, oral cancer lesion screening and monitoring, treatment follow-up, and other services. As previously mentioned, older adults can embrace technology targeted at modifying health behaviors, screening for lesions, or simply to comply with treatment plans, but using this technology could be problematic for those living with cognitive or physical problems. Tested technologies, which have been tailored specifically to older adults, could effectively remove or reduce such obstacles.
Teledentistry may be limited in applicability when there are technological challenges, such as slow internet speed or unreliable service. These challenges are likely exacerbated in many developing countries and rural areas, where the necessary infrastructure to adopt teledentistry doesn’t exist. Communication infrastructure requires bandwidth and reliability to effectively adopt teledentistry modalities. Another issue reported with adopting teledentistry was the reliance on caregivers among some older adults to communicate and report on their oral health status. However, telehealth can enable HIPAA-covered family members, primary care physicians, language interpreters, or other medical advocates to connect with one another in a virtual visit.
The main limitation of this review is the quality of the studies included, as many were cross-sectional studies with no clear methodology stated, non-RCTs with small sample sizes, or clinical trials that were dependent on self-reports or subjective opinions of participants or their caregivers. An additional limitation was the inclusion of mixed-age study populations, even though we carefully examined studies to include only those with specific results pertaining to older adults. Finally, although the evidence is growing to support the efficacy of Teledentistry in general, there is insufficient evidence to date to support conclusions advocating for cost-effectiveness or demonstrating long-term effectiveness.42 Our review confirms this for similar applications in older adults and suggests a potential limitation for policy decision-making.
CONCLUSION
Routine oral health services are necessary for older adults to maintain their oral health but accessing these services can be challenging in this population due to general health problems, mobility challenges, limited transportation, and present social distancing requirements. The current body of literature provides a promising, albeit incomplete, guide to the use of teledentistry for older adults. There is evidence that telehealth can be used for a variety of dental service types (e.g. medical and dental specialty consultations, oral health promotions, oral health screening and referrals). But some limitations identified, including the paucity of US-based studies, small sample sizes, and non-randomized designs, which require careful attention and consideration. Future larger, high-quality, and well-conducted studies are needed to optimize the use of teledentistry to improve the oral health of older adults. More US-based studies could help to better inform the delivery of teledentistry in the US, as the healthcare systems of different countries vary in terms of policies, workforce, financing, infrastructure, and attitudes of adults toward technology and novel interventions. These are all significant factors that may influence the adoption and implementation of Teledentistry in this country.
Supplementary Material
ACKNOWLEDGEMENT
This manuscript was prepared as a result of a call-for-papers exploring geriatric issues in dentistry by the ADA’s Council on Access, Prevention and Interprofessional Relations’ National Eldercare Advisory Committee (NEAC) in 2019. The authors wish to acknowledge the NEAC for their guidance and comments. Funding for this work was provided by the National Institutes of Health (NIH) Intramural Research Programs of the National Library of Medicine (NLM) and the National Institutes of Dental and Craniofacial Research (NIDCR) through salary support of the authors. This research was also supported in part by Dr Munder Ben-Omran’s appointment to the NLM Research Participation Program, administered by the Oak Ridge Institute for Science and Education (ORISE) through an interagency agreement between the US Department of Energy (DoE) and the NLM.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Munder O. Ben-Omran, National Library of Medicine and National Institute of Dental and Craniofacial Research, National Institutes of Health, Bethesda, MD, USA.
Alicia A. Livinski, National Institutes of Health Library, National Institutes of Health, Bethesda, Maryland, USA.
Dorota T. Kopycka-Kedzierawski, Eastman Institute for Oral Health, University of Rochester, Rochester, New York, USA.
Shahdokht Boroumand, National Institute of Dental and Craniofacial Research, National Institutes of Health, Bethesda, MD, USA.
Demetres Williams, National Institute of Dental and Craniofacial Research, National Institutes of Health, Bethesda, MD, USA.
Darien J. Weatherspoon, National Institute of Dental and Craniofacial Research, National Institutes of Health, Bethesda, MD, USA.
Timothy J. Iafolla, National Institute of Dental and Craniofacial Research, National Institutes of Health, Bethesda, MD, USA.
Paul Fontelo, National Library of Medicine, National Institutes of Health, Bethesda, MD, USA.
Bruce A. Dye, National Institute of Dental and Craniofacial Research, National Institutes of Health, Bethesda, MD, USA.
References
- 1.Mark M, Linda AJ, Kelvin MP. Fact Sheet: Aging in the United States. Washington DC: Population Reference Bureau; 2015. [Google Scholar]
- 2.Center for Disease Control and Prevention Chronic Diseases and Cognitive Decline – A Public Health Issue. Center for Disease Control and Prevention 2020. "https://www.cdc.gov/aging/publications/chronic-diseases-brief.html". 2020. [Google Scholar]
- 3.Tavares M, Lindefjeld Calabi KA, San Martin L. Systemic diseases and oral health. Dent Clin North Am 2014;58(4):797–814. [DOI] [PubMed] [Google Scholar]
- 4.Ghezzi EM, Kobayashi K, Park DY, Srisilapanan P. Oral healthcare systems for an ageing population: concepts and challenges. Int Dent J 2017;67 Suppl 2:26–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Skillman SM, Doescher MP, Mouradian WE, Brunson DK. The challenge to delivering oral health services in rural America. J Public Health Dent 2010;70 Suppl 1:S49–57. [DOI] [PubMed] [Google Scholar]
- 6.Fish-Parcham C, Burroughs M, Tranby EP, Brow AR. Addressing Rural Seniors’ Unmet Needs For Oral Health Care. HEALTH AFFAIRS BLOG: HEALTH AFFAIRS; 2019. [Google Scholar]
- 7.World Health Organization. Telemedicine: opportunities and developments in Member States: report on the second global survey on eHealth. Geneva: World Health Organization; 2010. [Google Scholar]
- 8.McLaren SW, Kopycka-Kedzierawski DT, Nordfelt J. Accuracy of teledentistry examinations at predicting actual treatment modality in a pediatric dentistry clinic. J Telemed Telecare 2017;23(8):710–15. [DOI] [PubMed] [Google Scholar]
- 9.Kopycka-Kedzierawski DT, McLaren SW, Billings RJ. Advancement Of Teledentistry At The University Of Rochester’s Eastman Institute For Oral Health. Health Affairs 2018;37(12):1960–66. [DOI] [PubMed] [Google Scholar]
- 10.Fricton J, Chen H. Using Teledentistry to Improve Access to Dental Care for the Underserved. Dent Clin N Am 2009;53(3):537–48. [DOI] [PubMed] [Google Scholar]
- 11.Madrid Troconis C, Rodriguez J, Puello P. Impact of Teledentistry Programs on Dental Service in Rural Areas: A Systematic Review. International Journal of Applied Engineering Research 2018:14417–23. [Google Scholar]
- 12.Estai M, Bunt S, Kanagasingam Y, Tennant M. Cost savings from a teledentistry model for school dental screening: an Australian health system perspective. Aust Health Rev 2018;42(5):482. [DOI] [PubMed] [Google Scholar]
- 13.Reddy KV. Using teledentistry for providing the specialist access to rural Indians. Indian J Dent Res 2011;22(2):189. [DOI] [PubMed] [Google Scholar]
- 14.Jampani ND, Nutalapati R, Dontula BS, Boyapati R. Applications of teledentistry: A literature review and update. J Int Soc Prev Community Dent 2011;1(2):37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brian Z, Weintraub JA. Oral Health and COVID-19: Increasing the Need for Prevention and Access. Prev Chronic Dis 2020;17:E82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.FCC. FCC Fights COVID-19 with $200M; Adopts Long-Term Connected Care Study. Washington DC; 2020. [Google Scholar]
- 17.Munn Z, Peters MDJ, Stern C, et al. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol 2018;18(1):143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peters MD, Godfrey CM, Khalil H, et al. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc 2015;13(3):141–6. [DOI] [PubMed] [Google Scholar]
- 19.Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med 2018;169(7):467–73. [DOI] [PubMed] [Google Scholar]
- 20.D9995 and D9996 – ADA Guide to Understanding and Documenting Teledentistry Events: American Dental Association 2020. p. 1–10. [Google Scholar]
- 21.Khan SA, Omar H. Teledentistry in practice: literature review. Telemed J E Health 2013;19(7):565–7. [DOI] [PubMed] [Google Scholar]
- 22.Innovation VH. Covidence systematic review software. Melbourne, Australia; 2020. [Google Scholar]
- 23.Tomuro K Development of oral home telecare programme for the home-dwelling elderly: a pilot study. Gerodontology 2004;21(3):177–80. [DOI] [PubMed] [Google Scholar]
- 24.Mariño R, Tonmukayakul U, Marwaha P, et al. Teleconsultation/telediagnosis using teledentistry technology: A pilot feasibility study. IJALS 2014;6(3–4):291–99. [Google Scholar]
- 25.Mariño R, Tonmukayakul U, Manton D, Stranieri A, Clarke K. Cost-analysis of teledentistry in residential aged care facilities. J Telemed Telecare 2016;22(6):326–32. [DOI] [PubMed] [Google Scholar]
- 26.Queyroux A, Saricassapian B, Herzog D, et al. Accuracy of Teledentistry for Diagnosing Dental Pathology Using Direct Examination as a Gold Standard: Results of the Tel-e-dent Study of Older Adults Living in Nursing Homes. J Am Med Dir Assoc 2017;18(6):528–32. [DOI] [PubMed] [Google Scholar]
- 27.Tynan A, Deeth L, McKenzie D. An integrated oral health program for rural residential aged care facilities: a mixed methods comparative study. BMC Health Serv Res 2018;18(1):515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tynan A, Deeth L, McKenzie D, et al. Integrated approach to oral health in aged care facilities using oral health practitioners and teledentistry in rural Queensland. Aust J Rural Health 2018. [DOI] [PubMed] [Google Scholar]
- 29.Buser R, Ziltener V, Samietz S, et al. Validation of a purpose-built chewing gum and smartphone application to evaluate chewing efficiency. J Oral Rehabil 2018;45(11):845–53. [DOI] [PubMed] [Google Scholar]
- 30.Worsley DJ, Marshman Z, Robinson PG, Jones K. Evaluation of the telephone and clinical NHS urgent dental service in Sheffield. Community Dent Health 2016;33(1):9–14. [PubMed] [Google Scholar]
- 31.Shah P, Yauney G, Gupta O, et al. Technology-enabled examinations of cardiac rhythm, optic nerve, oral health, tympanic membrane, gait and coordination evaluated jointly with routine health screenings: an observational study at the 2015 Kumbh Mela in India. BMJ Open 2018;8(4):e018774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Skandarajah A, Sunny SP, Gurpur P, et al. Mobile microscopy as a screening tool for oral cancer in India: A pilot study. PLoS One 2017;12(11):e0188440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cohen LA, Bonito AJ, Akin DR, et al. Role of pharmacists in consulting with the underserved regarding toothache pain. J Am Pharm Assoc (2003) 2009;49(1):38–42. [DOI] [PubMed] [Google Scholar]
- 34.Alabi RO, Elmusrati M, Sawazaki-Calone I, et al. Machine learning application for prediction of locoregional recurrences in early oral tongue cancer: a Web-based prognostic tool. Virchows Archiv 2019;475(4):489–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Araujo MR, Alvarez MJ, Godinho CA, Roberto MS. An eight-month randomized controlled trial on the use of intra-oral cameras and text messages for gingivitis control among adults. Int J Dent Hyg 2019;17(3):202–13. [DOI] [PubMed] [Google Scholar]
- 36.Lyu KX, Zhao J, Wang B, et al. Smartphone application weChat for clinical follow-up of discharged patients with head and neck tumors: A randomized controlled trial. Chin Med J 2016;129(23):2816–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yamazaki S, Kawaai H, Sasaki S, et al. Availability of a remote online hemodynamic monitoring system during treatment in a private dental office for medically high-risk patients. Ther Clin Risk Manag 2008;4(4):721–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gomes MS, Bonan PR, Ferreira VY, et al. Development of a mobile application for oral cancer screening. Technol Health Care 2017;25(2):187–95. [DOI] [PubMed] [Google Scholar]
- 39.Petcu R, Kimble C, Ologeanu-Taddei R, Bourdon I, Giraudeau N. ASSESSING PATIENT'S PERCEPTION OF ORAL TELECONSULTATION. Int J Technol Assess Health Care 2017;33(2):147–54. [DOI] [PubMed] [Google Scholar]
- 40.Bradley M, Black P, Noble S, Thompson R, Lamey PJ. Application of teledentistry in oral medicine in a Community Dental Service, N. Ireland. Br Dent J 2010;209(8):399–404. [DOI] [PubMed] [Google Scholar]
- 41.Vaishampayan S, Malik A, Pawar P, Arya K, Chaturvedi P. Short message service prompted mouth self-examination in oral cancer patients as an alternative to frequent hospital-based surveillance. South Asian J Cancer 2017;6(4):161–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Estai M, Kanagasingam Y, Tennant M, Bunt S. A systematic review of the research evidence for the benefits of teledentistry. J Telemed Telecare. 2018. April;24(3):147–156. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


