Abstract
Background:
Telemedicine-delivered buprenorphine (tele-buprenorphine) can potentially increase access to buprenorphine for patients with opioid use disorder (OUD), especially during the COVID-19 pandemic, but we know little about use in clinical care.
Methods:
This study was a retrospective national cohort study of veterans diagnosed with opioid use disorder (OUD) receiving buprenorphine treatment from the Veterans Health Administration (VHA) in fiscal years 2012–2019. The study examined trends in use of tele-buprenorphine and compared demographic and clinical characteristics in patients who received tele-buprenorphine versus those who received in-person treatment only.
Results:
Utilization of tele-buprenorphine increased from 2.29% of buprenorphine patients in FY2012 (n=187) to 7.96% (n=1352) in FY2019 in VHA veterans nationally. Compared to patients receiving only in-person care, tele-buprenorphine patients were less likely to be male (AOR=0.85, 95% CI: 0.73–0.98) or Black (AOR=0.54, 95% CI:0.45–0.65). Tele-buprenorphine patients were more likely to be treated in community-based outpatient clinics rather than large medical centers (AOR=2.91, 95% CI: 2.67–3.17) and to live in rural areas (AOR=2.13, 95% CI:1.92–2.35). The median days supplied of buprenorphine treatment was 722 (interquartile range: 322–1459) among the tele-buprenorphine patients compared to 295 (interquartile range: 67–854) among patients who received treatment in-person.
Conclusions:
Use of telemedicine to deliver buprenorphine treatment in VHA increased 3.5-fold between 2012 and 2019, though overall use remained low prior to COVID-19. Tele-buprenorphine is a promising modality especially when treatment access is limited; however, we must continue to understand how practitioners and patient are using telemedicine and how these patients’ outcomes compare to those using in-person care.
Keywords: Buprenorphine, Telemedicine, Telehealth, Opioid use disorder
1. Introduction
Opioid use disorder (OUD) is a debilitating illness associated with serious harms, including overdose and suicide (Bohnert et al., 2012; Ilgen et al., 2010; Larney et al., 2015; Park et al., 2016; Wilcox et al., 2004). The most effective treatment for OUD is pharmacotherapy with the medications buprenorphine and methadone (Mattick et al., 2014; Nielsen et al., 2017). Unlike methadone, buprenorphine can be prescribed by DEA-waivered clinicians in an office-based setting and thus has been a focus of recent expansion efforts (Collins et al., 2018; Wyse et al., 2018). Overall, pharmacotherapy remains greatly underused with less than a third of patients diagnosed with OUD receiving treatment in recent years (Lembke and Chen, 2016; Morgan et al., 2017; Saloner and Karthikeyan, 2015). Telemedicine, defined as synchronous videoconferencing between providers and patients in separate locations, is a treatment modality that can increase access and accessibility of treatment for chronic illnesses (Hill et al., 2010), but has been particularly underused (Grubbs et al., 2015) and understudied in substance use disorder treatment (Lin et al., 2019). With the recent COVID-19 pandemic, there has been an unprecedented shift to telemedicine-delivered treatment across health care systems, with specific policy changes, including lifting restrictions under the Ryan Haight Online Pharmacy Consumer Protection Act of 2008, which has removed barriers to telemedicine-delivered buprenorphine (tele-buprenorphine; Lin et al., 2020). Given this shift in care, it is even more important for those in the field to understand potential impacts of tele-buprenorphine on patient utilization and outcomes.
We know little about tele-buprenorphine treatment, including the types of patients who are more likely to receive telemedicine-delivered versus in-person care and how treatment modality impacts their treatment utilization and patient outcomes. A few studies have examined tele-buprenorphine care within a single clinic (Weintraub et al., 2018; Zheng et al., 2017) or through a series of cases (Brunet et al., 2020) and found similar substance-related outcomes in tele-buprenorphine patients compared to in-person (Zheng et al., 2017). The largest study to date examined telemedicine-delivered OUD treatment from providers located in large clinics to patients located in rural clinics in Ontario, Canada (Eibl et al., 2017). That study found greater retention among patients receiving telemedicine-delivered pharmacotherapy, though many of the patients were receiving tele-methadone treatment. No prior data exist that describe the clinical characteristics of patients who received tele-buprenorphine and how tele-buprenorphine patients compared with patients who received in-person care with respect to both patients’ characteristics and treatment utilization.
To understand recent trends in the use of this new delivery modality and compare patients who received tele-buprenorphine versus patients who received buprenorphine through usual in-person visits, we examined demographic and clinical characteristics of these two groups using data from fiscal years (FY) 2012 through 2019 of patients with OUD treated in the U.S. Veterans Health Administration (VHA). VHA is the largest addiction treatment provider in the United States (Wyse et al., 2018). Specifically, the aims of the study were to: 1) examine trends in utilization of tele-buprenorphine over time, 2) compare characteristics of patients who received tele-buprenorphine versus traditional in-person treatment, and 3) compare treatment utilization including length of buprenorphine treatment and utilization of adjunctive psychosocial treatments in patients who received tele-buprenorphine versus in-person treatment.
2. Methods
2.1. Study design and data source
The study obtained patient data from the VHA Corporate Data Warehouse (CDW). The VHA CDW is a national repository of electronic medical records, including diagnoses, treatment utilization, and pharmacy fills from all VHA patients across the United States. The Ann Arbor Veterans Affairs Institutional Review Board approved the study protocols.
2.2. Sample
We examined the cohort of all veterans nationally who had at least one VHA inpatient or outpatient encounter at any VHA facility with a diagnosis of OUD in fiscal year (FY) 2012 through FY 2018 (i.e., October 1, 2011, through September 30, 2018). The study included patients only if they had filled at least one buprenorphine prescription after OUD diagnosis. We examined treatment utilization for the one year period after, ending in September 30, 2019. The study assessed diagnoses of OUD using the International Classification of Disease (ICD-9 and ICD-10) diagnosis codes (Appendix Table 1).
2.3. Measures
Receipt of buprenorphine was defined as any VHA pharmacy fill of oral buprenorphine medication. We calculated the total days supply of buprenorphine by summing across buprenorphine prescriptions for each patient and counted nonoverlapping days of buprenorphine fills from FY2012 to FY2019. Similar to prior studies (Lin et al., In press; Manhapra et al., 2017; Oliva et al., 2012), we examined clinic “stop codes” in CDW data, which indicate the clinical setting or type of services received during a specific encounter with VHA providers, to determine receipt of psychotherapy visits for OUD treatment.
We defined tele-buprenorphine for OUD by first including veterans who were diagnosed with OUD who received at least one buprenorphine fill within one year after diagnosis of OUD (covering FY 2012 through FY 2019). Among those veterans, we identified individuals who received telemedicine-delivered buprenorphine treatment, defined by: 1) an outpatient telehealth visit identified using secondary stop codes (Appendix Table 2); 2) received during a visit for treatment of OUD; and 3) the name of the buprenorphine prescriber was the same as the clinician who provided the telehealth visit and occurred on the same date. Patients with any tele-buprenorphine visits during the study period were compared with patients who received buprenorphine only via in-person visits.
2.4. Covariates
Demographic characteristics that the study examined included patients’ age, sex, race, Hispanic ethnicity, rural/urban residence, and homelessness. We determined rural/urban status using patient zip code and defined by Rural-Urban Commuting Areas (RUCAs) geographic taxonomy (“USDA ERS - Documentation. 2010 Rural-Urban Commuting Area (RUCA) Codes,” n.d.). The study team determined homelessness by utilization of homeless veteran services (see Appendix Table 3).
Patients receiving the majority of their care at a VHA medical center (VAMC; typically a major facility including a range of specialty services) versus VHA community-based outpatient clinics (CBOCs) are much more likely to receive buprenorphine treatment (Lin et al., In press), so we included a variable indicating whether the patient received >50% of their care in a VA medical center versus a CBOC. The research team identified additional psychiatric and substance use disorder diagnoses via ICD codes from inpatient and outpatient clinical encounters in the 12 months prior to the patient’s first OUD diagnosis. Comorbid mental health diagnoses included psychotic disorders, PTSD, other anxiety disorders, depression, bipolar disorder, alcohol use disorder, stimulant use disorder, cannabis use disorder and other substance use disorder (see Appendix Table 4). The study included number of Elixhauser Comorbid conditions (in addition to OUD) to indicate overall burden of comorbid medical conditions (van Walraven et al., 2009).
2.5. Statistical analysis
We examined trends over time in the percentage of patients who received tele-buprenorphine treatment among all patients who received buprenorphine in that fiscal year. Patients could appear in multiple years in these trend analyses. We also examined the percentage of patients who received telemedicine-delivered psychotherapy among patients who received any buprenorphine treatment in each fiscal year and examined clinic locations where tele-buprenorphine was prescribed.
We then compared the characteristics of patients who received any tele-buprenorphine across the study period with patients who only received buprenorphine in-person. Using χ2 tests, the research team compared two groups’ baseline patient demographic and clinical characteristics. Multivariable logistic regression was then used to examine differences in the demographic and clinical characteristics in patients adjusting for all covariates and also adjusting for year of OUD diagnosis. Finally, we described both in-person and telemedicine-delivered treatment utilization in this cohort, including differences in days supplied of buprenorphine and also examined telemedicine and in-person delivered psychotherapy for OUD. We chose to focus on these treatment characteristics descriptively without adjusting for covariates. Given that use of tele-buprenorphine is quite new, at least pre-COVID-19, a substantial selection effect is likely contributing to which patients’ clinicians were selecting for tele-buprenorphine treatment.
3. Results
3.1. Patients with OUD receiving tele-buprenorphine
A total of 33,616 unique veterans with a diagnosis of OUD received buprenorphine treatment in the VHA from FY2012 to FY2019. Among these patients, a total of 2,718 patients with OUD received any telemedicine-delivered buprenorphine treatment compared to 30,898 patients who received only in-person delivered buprenorphine. Utilization of tele-buprenorphine increased 3.5-fold over the study period, from 2.29% of buprenorphine patients in FY 2012 (n=187) to 7.96% (n=1352) in FY 2019 (see Figure 1). Concurrent to increases in tele-buprenorphine, increases also occurred in telemedicine-delivered individual psychotherapy for patients receiving tele-buprenorphine, while telemedicine-delivered group psychotherapy remained relatively flat during this time period (see Figure 2). Clinic settings where tele-buprenorphine was prescribed include: substance use disorder clinics (78.0% of all tele-buprenorphine encounters), mental health and PTSD clinics (21.1%), primary care (0.3%) and other clinics (0.7%).
Figure 1.
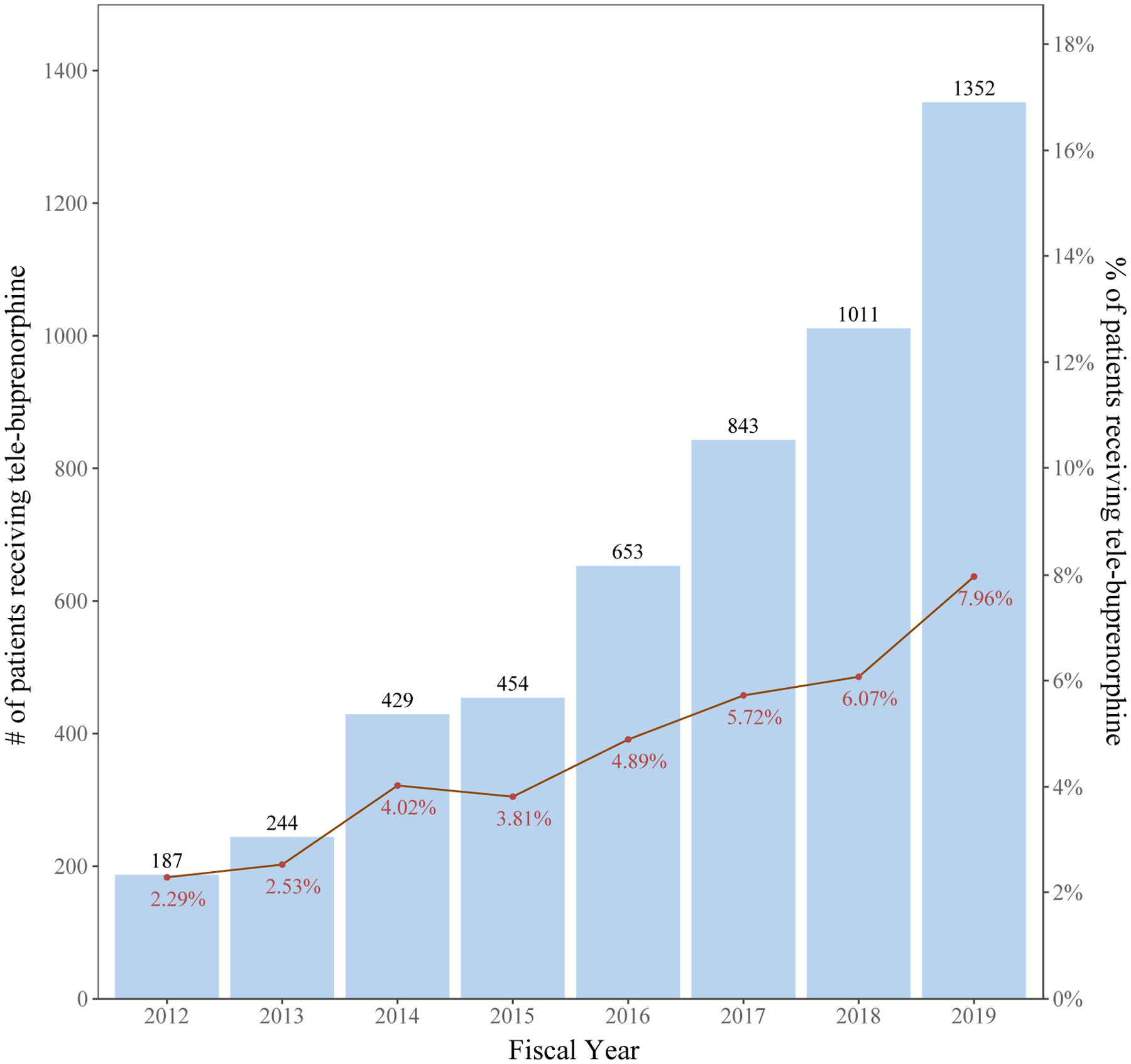
Trends in patients receiving tele-buprenorphine for opioid use disorder in the VHA.
Figure 2.
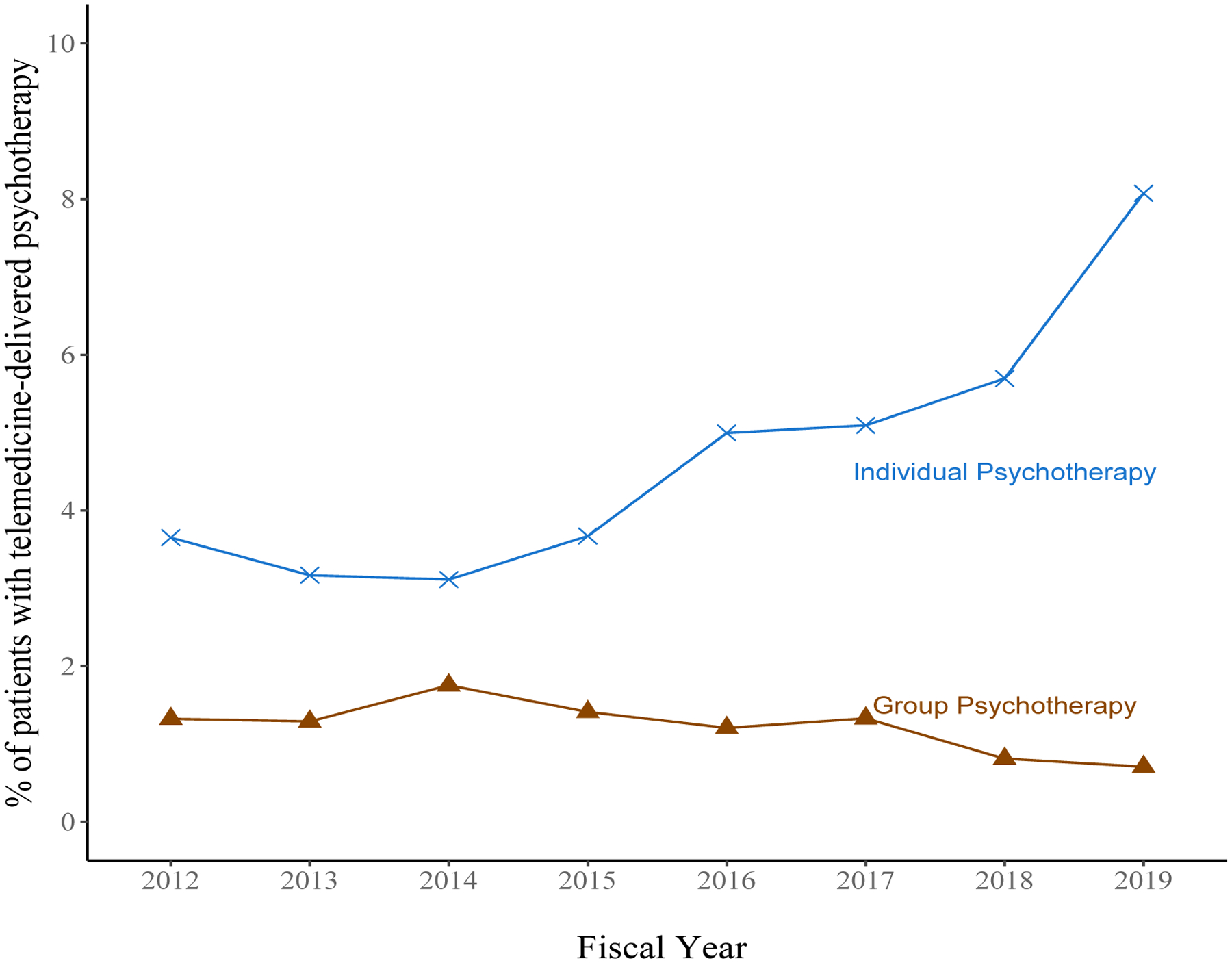
Trends in percentage of patients receiving telemedicine-delivered psychotherapy among patients receiving buprenorphine in each fiscal year.
3.2. Patients’ characteristics associated with telemedicine treatment
When comparing tele-buprenorphine to in-person buprenorphine patients, tele-buprenorphine patients had a higher proportion of patients in younger age groups, higher proportion of females, and a higher proportion of patients who were White (see Table 1). Tele-buprenorphine patients were also more likely to live in rural areas and were more likely to receive their care primarily in a CBOC compared to in-person patients. Tele-buprenorphine patients also had a higher prevalence of depressive disorders and anxiety disorders but lower prevalence of psychotic disorder, alcohol use disorder, stimulant use disorder, and cannabis use disorder compared to patients seen in-person.
Table 1.
Characteristics of patients receiving tele-buprenorphine compared with patients who received in-person buprenorphine (FY2012–2019).
| Patient characteristics | Received telemedicine for OUD % (n)/mean (N = 2,718) | In-person treatment only % (n)/mean (N = 30,898) | Total % (n) (N = 33,616) | X2 | p-value |
|---|---|---|---|---|---|
| Age | 33.80 | <0.0001 | |||
| 18–29 | 2.17% (59) | 2.49% (769) | 2.46% (828) | ||
| 30–50 | 54.56% (1483) | 48.82% (15084) | 49.28% (16567) | ||
| 51–64 | 26.75% (727) | 29.42% (9089) | 29.20% (9816) | ||
| ≥65 | 16.52% (449) | 19.28% (5956) | 19.05% (6405) | ||
| Female | 8.94% (243) | 7.29% (2251) | 7.42% (2494) | 9.96 | 0.0016 |
| Race | |||||
| White | 87.05% (2366) | 80.47% (24864) | 81.00% (27230) | 146.30 | <0.0001 |
| Black | 5.41% (147) | 13.02% (4024) | 12.41% (4171) | ||
| Other/Multi-race | 2.80% (76) | 1.72% (530) | 1.80% (606) | ||
| Unknown | 4.75% (129) | 4.79% (1480) | 4.79% (1609) | ||
| Ethnicity | |||||
| Hispanic | 4.60% (125) | 5.51% (1701) | 5.43% (1826) | 6.11 | 0.047 |
| Non-Hispanic | 92.13% (2504) | 91.73% (28342) | 91.76% (30846) | ||
| Other/Unknown | 3.27% (89) | 2.77% (855) | 2.81% (944) | ||
| Homeless | 15.34% (417) | 18.82% (5814) | 18.54% (6231) | 19.97 | <0.0001 |
| Care location | |||||
| VAMC | 38.45% (1045) | 66.75% (20624) | 64.46% (21669) | 883.85 | <0.0001 |
| CBOC | 49.30% (1340) | 27.48% (8491) | 29.25% (9831) | ||
| Other/Unknown | 12.25% (333) | 5.77% (1783) | 6.29% (2116) | ||
| Residence | |||||
| Urban | 75.97% (2065) | 86.84% (26833) | 85.97% (28898) | 310.94 | <0.0001 |
| Rural | 21.60% (587) | 10.42% (3219) | 11.32% (3806) | ||
| Other/Unknown | 2.43% (66) | 2.74% (846) | 2.71% (912) | ||
| Depressive Disorder | 57.58% (1565) | 52.80% (16313) | 53.18% (17878) | 22.95 | <0.0001 |
| Bipolar Disorder | 10.01% (272) | 9.68% (2992) | 9.71% (3264) | 0.29 | 0.5846 |
| PTSD | 34.51% (938) | 33.99% (10501) | 34.03% (11,439) | 0.30 | 0.5799 |
| Other Anxiety disorder | 34.18% (929) | 31.31% (9673) | 31.54% (10602) | 9.55 | 0.0020 |
| Psychotic disorder | 3.90% (106) | 5.33% (1648) | 5.22% (1,754) | 10.38 | 0.0013 |
| Alcohol use disorder | 30.94% (841) | 34.02% (10512) | 33.77% (11353) | 10.59 | 0.0011 |
| Stimulant Use disorder | 15.49% (421) | 22.06% (6815) | 21.53% (7236) | 63.78 | <.0001 |
| Cannabis use disorder | 10.56% (287) | 14.20% (4389) | 13.91% (4676) | 27.72 | <0.0001 |
| Other Substance Use Disorder | 34.18% (929) | 35.62% (11007) | 35.51% (11936) | 2.27 | 0.1315 |
| Number of Elixhauser comorbid conditions | |||||
| 0 | 19.5% (530) | 20.25% (6258) | 20.19% (6788) | 8.46 | 0.0146 |
| 1 | 26.01% (707) | 23.54% (7273) | 23.74% (7980) | ||
| ≥2 | 54.49% (1481) | 56.21% (17367) | 56.07% (18848) |
In analyses adjusted for all covariates in Table 1, tele-buprenorphine patients were significantly less likely than patients receiving only in-person care to be male or to be Black. Also, compared to patients who received only in-person care, tele-buprenorphine patients were more likely to be treated in a CBOC, more likely to live in a rural area, and more likely to have depressive disorder, and less likely to have stimulant use disorder and cannabis use disorder (see Table 2).
Table 2.
Logistic regression examining patient characteristics associated with tele-buprenorphine compared to in-person buprenorphine treatment.
| Characteristic | AOR comparing tele-health to in-person visit | |
|---|---|---|
| Age | 18–29 | ref |
| 30–50 | 1.18 (0.90,1.56) | |
| 51–64 | 1.11 (0.83,1.47) | |
| 65 & over | 1.05 (0.78,1.41) | |
| Male | 0.85 (0.73,0.98) | |
| Race | White | ref |
| Black | 0.54 (0.45,0.65) | |
| Other/Multi-race | 1.44 (1.12,1.86) | |
| Unknown | 0.88 (0.71,1.09) | |
| Ethnicity | Hispanic | ref |
| Non-Hispanic | 1.13 (0.93,1.37) | |
| Other/Unknown | 1.38 (1.01,1.86) | |
| Homeless | Yes | 0.95 (0.85,1.07) |
| Care location | VAMC | ref |
| CBOC | 2.91 (2.67,3.17) | |
| Other/Unknown | 3.78 (3.30,4.33) | |
| Residence | Urban | ref |
| Rural | 2.12 (1.92,2.35) | |
| Other/Unknown | 1.12 (0.86,1.45) | |
| Depressive Disorder | 1.25 (1.12,1.39) | |
| Bipolar Disorder | 1.12 (0.97,1.28) | |
| PTSD | 0.95 (0.87,1.03) | |
| Other Anxiety disorder | 1.03 (0.94,1.13) | |
| Psychotic disorder | 0.83 (0.68,1.02) | |
| Alcohol use disorder | 1.00 (0.90,1.10) | |
| Stimulant Use disorder | 0.81 (0.72,0.91) | |
| Cannabis use disorder | 0.75 (0.66,0.86) | |
| Other Substance use disorders | 1.03 (0.94,1.13) | |
| Number of Elixhauser Comorbid Conditions | 0 | ref |
| 1 | 1.05 (0.92,1.20) | |
| ≥2 | 0.99 (0.85,1.16) | |
| Diagnosis year. | 2011 | ref |
| 2012 | 1.04 (0.92,1.18) | |
| 2013 | 0.92 (0.80,1.06) | |
| 2014 | 1.03 (0.89,1.19) | |
| 2015 | 0.97 (0.83,1.13) | |
| 2016 | 0.89 (0.76,1.04) | |
| 2017 | 0.87 (0.74,1.03) | |
| 2018 | 0.97 (0.80, 1.16) | |
3.3. OUD treatment utilization in patients using telemedicine versus in-person treatment
Last, we examined utilization of treatments comparing patients who received tele-buprenorphine versus those who only received buprenorphine treatment in-person. Patients who received tele-buprenorphine received a median of 39 (interquartile range [IQR]: 19, 70) buprenorphine treatment visits with 4 (IQR: 2, 13) of those being telemedicine visits. These frequencies are compared to a total of 20 (IQR: 6, 48) buprenorphine visits for patients who received in-person treatment. The median days supplied of buprenorphine treatment was 722 (IQR: 322, 1459) among the tele-buprenorphine patients compared to 295 (IQR: 67, 854) among patients who received only treatment in-person. Among patients who received tele-buprenorphine, the average number of psychotherapy treatment visits for OUD was 18 (IQR: 6, 40) with 1 (IQR: 0, 3) of those being telemedicine visits compared to 15 (IQR: 4, 39) psychotherapy treatment visits for those who received in-person treatment. Among patients receiving tele-buprenorphine, 2,374 (87.3%) received treatment from a clinician in a VAMC while they were in a VHA clinic (Clinical Video Telehealth [CVT]) and 315 received tele-buprenorphine while they were located at home (VA Video Connect [VVC]).
4. Discussion
This study of veterans receiving OUD treatment in the VHA found substantial increases in use of tele-buprenorphine treatment from FY 2012 to FY2019, with 7.96% receiving any tele-buprenorphine visits among all patients receiving buprenorphine in FY2019. Patients who received tele-buprenorphine, as expected, were more likely to live in rural areas. However, in many other respects, patients who received tele-buprenorphine were similar to patients receiving in-person treatment with a high prevalence of comorbid physical and mental health conditions, as well as substance use disorders.
The few studies that have compared tele-buprenorphine patients to patients receiving traditional in-person care have found that retention in buprenorphine treatment was similar (Zheng et al., 2017). This current analysis adds to those prior results by showing patients receiving tele-buprenorphine are more likely to live in rural areas but the vast majority of tele-buprenorphine patients did not live in a rural area. This study also broadens the evidence-base by including multiple years of data from the largest national health care system delivering buprenorphine care in the United States. Similar to a prior study of mostly patients receiving telemedicine-delivered methadone (Eibl et al., 2017), these results also indicate that patients receiving tele-buprenorphine stayed in treatment for longer than patients receiving in-person treatment. Retention in buprenorphine treatment is a critical outcome because longer retention is associated with numerous positive clinical outcomes including decreased mortality (Morgan et al., 2017; Norton et al., 2017; Sordo et al., 2017). Because tele-buprenorphine is a fairly new approach and relative outcomes are not well established, only more stable patients may be referred, so patients who stayed longer in treatment were more likely to receive tele-buprenorphine. However, telemedicine-delivered buprenorphine may also help patients stay in treatment longer due to increased accessibility of care. Randomized controlled trials should examine the impact of telemedicine care on treatment utilization and retention as well as substance-related outcomes. In addition, this was also the first study that examined real-world use of tele-buprenorphine in a large health care system that used different models of tele-buprenorphine; given that for many patients, telemedicine visits were a minority of total buprenorphine visits, future work should examine clinical decision-making around when telemedicine is used versus in-person, and how this affects patient retention.
These results are among the first to examine telemedicine-delivery of psychotherapy for substance use disorder treatment in real-world clinical settings throughout the United States. A few prior studies have piloted telemedicine-delivery of psychotherapy in patients receiving medications for OUD; those findings indicate patients find this modality of therapy delivery to be generally acceptable (King et al., 2014, 2009). Here, we saw an increasing trend in telemedicine-delivered individual therapy for patients who received tele-buprenorphine along with relative stability in the lower levels of telemedicine-delivered group psychotherapy. In many ways, telemedicine-delivered psychotherapy is just as crucial for patients with substance use disorders given the lack of access to evidence-based forms of psychotherapy treatments for substance use disorders and comorbid mental health conditions in many parts of the United States. Also, the majority of patients with OUD have additional mental health and SUD conditions (Lin et al., 2020a), where psychotherapy may be a key treatment option. However, psychotherapy treatment often requires frequent treatment visits, commonly weekly therapy sessions, which is particularly challenging for the SUD treatment populations, where transportation barriers and competing demands are common. Telemedicine-delivery of psychotherapy, especially to patients at home, may minimize the barriers (e.g., transportation) and burdens (e.g., time away from work and family responsibilities) of office-based treatment, thus increasing reach and accessibility of existing empirically based psychotherapy treatment for substance use disorders. Future research should seek to understand overall effectiveness of telemedicine-delivered psychotherapy and which patients may benefit from this modality.
This study also identified important differences between tele-buprenorphine patients and patients who received only in-person care. Tele-buprenorphine patients were significantly less likely to be Black even after controlling for other sociodemographic differences. Several recent studies examining telemedicine use broadly post-COVID-19 have also begun to find differences in race, ethnicity, and other demographic characteristics, and suggest that numerous contributors, including differences at the patient, healthc are system, and community levels, are at play (Chunara et al., 2021; Eberly et al., 2020). Specifically, research should determine whether Black veterans are more likely to be treated in facilities with a low propensity to deliver tele-buprenorphine and/or whether Black veterans are less likely to be offered and/or engage in tele-buprenorphine than White veterans treated within the same facility. It will be crucial to continue to investigate contributors to any disparities in treatment use and to consider additional interventions to address disparities that may persist with the transition to virtual care. In addition to demographic differences, comorbid mental health disorders were highly prevalent, with comorbid depression even more prevalent in patients who received tele-buprenorphine. Unfortunately, recent data have also shown that patients with depression and comorbid substance use disorders are less likely to receive high quality depression treatment (Coughlin et al., 2020). Thus, it may be particularly important to consider how to address these comorbid conditions within telemedicine models, incorporating both medication and psychotherapy treatment. Telemedicine hub models, in which clinicians with different backgrounds located in a hub site who can treat patients located in distant clinics or their homes in different locations, are promising (Brunet et al., 2020). Although, ideally, clinics would be able to deliver the array of mental health and substance use disorder medication and psychotherapy treatments via telehealth, a range of delivery models likely will be needed to meet patients’ needs.
Examining telemedicine delivery of treatment for vulnerable patients, including those with OUD is particularly important in the current context of the COVID-19 pandemic. Much of chronic care management has shifted dramatically from in-person care to both telemedicine and telephone-delivered treatment. For buprenorphine treatment, major changes have taken place in federal guidelines from the DEA and SAMHSA to lower barriers to tele-buprenorphine due to specific concerns about decreasing access to treatment in this patient population due to social distancing (Lin et al., 2020b). The impact of these changes in federal guidelines not only on the uptake of tele-buprenorphine but also on retention in care and other patient outcomes will be important to study. In addition, all prior studies to date of tele-buprenorphine examined care delivery of clinicians located at one clinic location to patients at a rural clinic, but much of the shift since COVID-19 has occurred toward tele-buprenorphine to patients at home. Data from this study are the first to include patients receiving tele-buprenorphine in an at-home setting in light of recent VHA efforts to expand telemedicine treatment to veterans at home. However, future studies should assess patients’ experiences and outcomes, especially because other concurrent changes are likely, including reduced ability to obtain urine toxicology to monitor for relapse and increased psychosocial stressors for patients due to COVID-19. Findings that tele-buprenorphine is associated with improved patient outcomes would suggest the federal guidelines lowering barriers to tele-buprenorphine, currently in effect during the public health emergency, should become permanent. Alternatively, if the quality of care and outcomes of treatment are significantly worse for tele-buprenorphine compared to in-person care, identifying novel strategies to overcome the differences in care (e.g., remote monitoring tools) would be a critical next step.
This study hads several important limitations. The study used VHA administrative data focusing on veterans with OUD. Although this is an important population with similar prevalence of OUD compared to the non-veteran population in the United States (Rhee and Rosenheck, 2019), some veterans obtain medications and other treatments outside of the VHA, which these data did not capture. Some of this care outside the VHA may include receipt of tele-buprenorphine, but this is likely to be infrequent given the progress the VHA has made on telehealth in general and low uptake of telemedicine-delivered OUD care in the community (Huskamp, Haiden A. et al., 2018). As noted, patients who are offered tele-buprenorphine may differ in important clinical ways from those offered in-person buprenorphine treatment, and that may affect their ongoing engagement in care. Ideally, clinical trials in which OUD patients are randomly assigned to telemedicine versus in-person care only would allow for comparison of treatment engagement and outcomes without these potential confounds. Finally, the population of veterans with OUD is predominantly male, which may limit generalizability of these findings.
Especially with the recent, rapid implementation of telemedicine services in response to the COVID-19 pandemic, a pressing need exists to understand how telemedicine can be utilized to deliver buprenorphine treatment for the vulnerable population of patients with OUD and also how this form of care delivery impacts patients’ outcomes. Although efficacy of telemedicine is generally compared to in-person care, ongoing access barriers to in-person treatment— particularly in the era of the COVID-19 pandemic—may mean that telemedicine actually increases engagement and utilization of buprenorphine, a life-saving treatment. Tremendous interest exists in understanding what telemedicine delivery of treatment looks like for this patient population, especially related to possible treatment disparities and unintended consequences with respect to retention in care. This large, multiple-year study from the pre-COVID-19 era provides some reassurance about delivery of buprenorphine treatment via telemedicine and can serve as an important comparison of utilization prior to loosening telemedicine barriers since COVID-19. However, a tremendous need remains for additional studies to understand variation in different tele-buprenorphine models and barriers and facilitators to implementing these models, and approaches to complex patients with OUD.
Supplementary Material
Highlights.
Tele-buprenorphine (tele-bup) use increased but use still remained low as of 2019
Tele-bup and in-person buprenorphine patients had largely similar characteristics
Tele-bup patients received more days of buprenorphine but there may be confounders
Future studies are needed on effectiveness and on COVID-19 impacts on tele-bup
Funding:
LAL was supported by a Career Development Award (CDA 18-008) from the US Department of Veterans Affairs Health Services Research & Development Service and CDC R49 CE003085. LNC was supported by a NIAAA Research Career Development Award (K23 AA028232). John Piette was supported by VA HSR&D Senior Research Career Scientist award and John Fortney was supported by VA HSR&D Research Career Scientist award. LAL and ASBB receive funding from SAMHSA for a project titled “Telehealth for Medications for Opioid Use Disorders”
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bohnert ASB, Ilgen MA, Ignacio RV, McCarthy JF, Valenstein M, Blow FC, 2012. Risk of death from accidental overdose associated with psychiatric and substance use disorders. Am J Psychiatry 169, 64–70. 10.1176/appi.ajp.2011.10101476 [DOI] [PubMed] [Google Scholar]
- Brunet N, Moore DT, Lendvai Wischik D, Mattocks KM, Rosen MI, 2020. Increasing buprenorphine access for veterans with opioid use disorder in rural clinics using telemedicine. Subst Abus 1–8. 10.1080/08897077.2020.1728466 [DOI] [PubMed] [Google Scholar]
- Chunara R, Zhao Y, Chen J, Lawrence K, Testa PA, Nov O, Mann DM, 2021. Telemedicine and healthcare disparities: a cohort study in a large healthcare system in New York City during COVID-19. J Am Med Inform Assoc 28, 33–41. 10.1093/jamia/ocaa217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins FS, Koroshetz WJ, Volkow ND, 2018. Helping to End Addiction Over the Long-term: The Research Plan for the NIH HEAL Initiative. JAMA 320, 129–130. 10.1001/jama.2018.8826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coughlin LN, Pfeiffer P, Ganoczy D, Lin LA, 2020. Quality of Outpatient Depression Treatment in Patients With Comorbid Substance Use Disorder. Am J Psychiatry appiajp202020040454. 10.1176/appi.ajp.2020.20040454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eberly LA, Kallan MJ, Julien HM, Haynes N, Khatana SAM, Nathan AS, Snider C, Chokshi NP, Eneanya ND, Takvorian SU, Anastos-Wallen R, Chaiyachati K, Ambrose M, O’Quinn R, Seigerman M, Goldberg LR, Leri D, Choi K, Gitelman Y, Kolansky DM, Cappola TP, Ferrari VA, Hanson CW, Deleener ME, Adusumalli S, 2020. Patient Characteristics Associated With Telemedicine Access for Primary and Specialty Ambulatory Care During the COVID-19 Pandemic. JAMA Netw Open 3, e2031640. 10.1001/jamanetworkopen.2020.31640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eibl JK, Gauthier G, Pellegrini D, Daiter J, Varenbut M, Hogenbirk JC, Marsh DC, 2017. The effectiveness of telemedicine-delivered opioid agonist therapy in a supervised clinical setting. Drug Alcohol Depend 176, 133–138. 10.1016/j.drugalcdep.2017.01.048 [DOI] [PubMed] [Google Scholar]
- Grubbs KM, Fortney JC, Dean T, Williams JS, Godleski L, 2015. A Comparison of Mental Health Diagnoses Treated via Interactive Video and Face to Face in the Veterans Healthcare Administration. Telemed J E Health 21, 564–566. 10.1089/tmj.2014.0152 [DOI] [PubMed] [Google Scholar]
- Hill RD, Luptak MK, Rupper RW, Bair B, Peterson C, Dailey N, Hicken BL, 2010. Review of Veterans Health Administration telemedicine interventions. Am J Manag Care 16, e302–310. [PubMed] [Google Scholar]
- Huskamp Haiden A., Busch Alisa B., Souza Jeffrey, Uscher-Pines Lori, Rose Sherri, Wilcock Andrew, Landon Bruce E., Mehrotra Ateev, 2018. How Is Telemedicine Being Used In Opioid And Other Substance Use Disorder Treatment? | Health Affairs. Health Affairs 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ilgen MA, Bohnert ASB, Ignacio RV, McCarthy JF, Valenstein MM, Kim HM, Blow FC, 2010. Psychiatric diagnoses and risk of suicide in veterans. Arch. Gen. Psychiatry 67, 1152–1158. 10.1001/archgenpsychiatry.2010.129 [DOI] [PubMed] [Google Scholar]
- King VL, Brooner RK, Peirce JM, Kolodner K, Kidorf MS, 2014. A randomized trial of web-based videoconferencing for substance abuse counseling. J Subst Abuse Treat 46. 10.1016/j.jsat.2013.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King VL, Stoller KB, Kidorf M, Kindbom K, Hursh S, Brady T, Brooner RK, 2009. Assessing the effectiveness of an Internet-based videoconferencing platform for delivering intensified substance abuse counseling. J Subst Abuse Treat 36, 331–338. 10.1016/j.jsat.2008.06.011 [DOI] [PubMed] [Google Scholar]
- Larney S, Bohnert ASB, Ganoczy D, Ilgen MA, Hickman M, Blow FC, Degenhardt L, 2015. Mortality among older adults with opioid use disorders in the Veteran’s Health Administration, 2000–2011. Drug Alcohol Depend 147, 32–37. 10.1016/j.drugalcdep.2014.12.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lembke A, Chen JH, 2016. Use of Opioid Agonist Therapy for Medicare Patients in 2013. JAMA Psychiatry 73, 990–992. 10.1001/jamapsychiatry.2016.1390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin LA, Bohnert ASB, Blow FC, Gordon AJ, Ignacio RV, Kim HM, Ilgen MA, 2020. Polysubstance use and association with opioid use disorder treatment in the US Veterans Health Administration. Addiction. 10.1111/add.15116 [DOI] [PubMed] [Google Scholar]
- Lin LA, Casteel D, Shigekawa E, Weyrich MS, Roby DH, McMenamin SB, 2019. Telemedicine-delivered treatment interventions for substance use disorders: A systematic review. J Subst Abuse Treat 101, 38–49. 10.1016/j.jsat.2019.03.007 [DOI] [PubMed] [Google Scholar]
- Lin LA, Fernandez AC, Bonar EE, 2020b. Telehealth for substance using populations in the age of COVID-19: Recommendations to enhance adoption. JAMA Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manhapra A, Petrakis I, Rosenheck R, 2017. Three-year retention in buprenorphine treatment for opioid use disorder nationally in the Veterans Health Administration. Am J Addict 26, 572–580. 10.1111/ajad.12553 [DOI] [PubMed] [Google Scholar]
- Mattick RP, Breen C, Kimber J, Davoli M, 2014. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev CD002207. 10.1002/14651858.CD002207.pub4 [DOI] [PubMed] [Google Scholar]
- Morgan JR, Schackman BR, Leff JA, Linas BP, Walley AY, 2017. Injectable naltrexone, oral naltrexone, and buprenorphine utilization and discontinuation among individuals treated for opioid use disorder in a United States commercially insured population. J Subst Abuse Treat. 10.1016/j.jsat.2017.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen S, Larance B, Lintzeris N, 2017. Opioid Agonist Treatment for Patients With Dependence on Prescription Opioids. JAMA 317, 967–968. 10.1001/jama.2017.0001 [DOI] [PubMed] [Google Scholar]
- Norton BL, Beitin A, Glenn M, DeLuca J, Litwin AH, Cunningham CO, 2017. Retention in buprenorphine treatment is associated with improved HCV care outcomes. J Subst Abuse Treat 75, 38–42. 10.1016/j.jsat.2017.01.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliva EM, Harris AHS, Trafton JA, Gordon AJ, 2012. Receipt of opioid agonist treatment in the Veterans Health Administration: facility and patient factors. Drug Alcohol Depend 122, 241–246. 10.1016/j.drugalcdep.2011.10.004 [DOI] [PubMed] [Google Scholar]
- Park TW, Lin LA, Hosanagar A, Kogowski A, Paige K, Bohnert ASB, 2016. Understanding Risk Factors for Opioid Overdose in Clinical Populations to Inform Treatment and Policy. J Addict Med 10, 369–381. 10.1097/ADM.0000000000000245 [DOI] [PubMed] [Google Scholar]
- Rhee TG, Rosenheck RA, 2019. Comparison of opioid use disorder among male veterans and non-veterans: Disorder rates, socio-demographics, co-morbidities, and quality of life. Am J Addict. 10.1111/ajad.12861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saloner B, Karthikeyan S, 2015. Changes in Substance Abuse Treatment Use Among Individuals With Opioid Use Disorders in the United States, 2004–2013. JAMA 314, 1515–1517. 10.1001/jama.2015.10345 [DOI] [PubMed] [Google Scholar]
- Sordo L, Barrio G, Bravo MJ, Indave BI, Degenhardt L, Wiessing L, Ferri M, Pastor-Barriuso R, 2017. Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies. BMJ 357, j1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- USDA ERS - Documentation. 2010. Rural-Urban Commuting Area (RUCA) Codes [WWW Document], n.d. URL https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/documentation/ (accessed 4.21.19).
- van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ, 2009. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care 47, 626–633. 10.1097/MLR.0b013e31819432e5 [DOI] [PubMed] [Google Scholar]
- Weintraub E, Greenblatt AD, Chang J, Himelhoch S, Welsh CJ, 2018. Expanding access to buprenorphine treatment in rural areas with the use of telemedicine. The American Journal on Addictions 0. 10.1111/ajad.12805 [DOI] [PubMed] [Google Scholar]
- Wilcox HC, Conner KR, Caine ED, 2004. Association of alcohol and drug use disorders and completed suicide: an empirical review of cohort studies. Drug Alcohol Depend 76 Suppl, S11–19. 10.1016/j.drugalcdep.2004.08.003 [DOI] [PubMed] [Google Scholar]
- Wyse JJ, Gordon AJ, Dobscha SK, Morasco BJ, Tiffany E, Drexler K, Sandbrink F, Lovejoy TI, 2018. Medications for Opioid Use Disorder in the Department of Veterans Affairs (VA) Health Care System: Historical Perspective, Lessons Learned and Next Steps. Subst Abus 0. 10.1080/08897077.2018.1452327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng W, Nickasch M, Lander L, Wen S, Xiao M, Marshalek P, Dix E, Sullivan C, 2017. Treatment Outcome Comparison Between Telepsychiatry and Face-to-face Buprenorphine Medication-assisted Treatment for Opioid Use Disorder: A 2-Year Retrospective Data Analysis. J Addict Med 11, 138–144. 10.1097/ADM.0000000000000287 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


