Abstract
Introduction:
Depression is a prevalent condition for which screening rates remain low and disparities in screening exist. This study examines the impacts of a medical assistant screening protocol on the rates of depression screening, overall and by sociodemographic groups, in a primary care setting.
Methods:
Between September 2016 and August 2018, a quasi-experimental study of adult primary care visits was conducted at an urban academic clinic to ascertain the change in the rates of completion of the Patient Health Questionnaire-2 after the implementation of a medical assistant protocol (intervention) versus that of physician-only screening (control arm). Analyses were conducted between April 2019 and April 2020 and used interrupted time-series models with generalized estimating equations.
Results:
A total of 45,157 visits by 21,377 unique patients were included. Overall, screening increased from 18% (physician-only screening) to 57% (medical assistant protocol) (p<0.0001). Screening increased for all measured demographics. With physician screening, depression screening was less likely to occur at visits by women (than at visits by men; OR=0.91, 95% CI=0.85, 0.98) and at visits by Black/African American patients (than at visits by White; OR=0.91, 95% CI=0.84, 0.99). However, with the medical assistant protocol, depression screening was more likely to occur at visits by women (than at visits by men; OR=1.07, 95% CI=1.0002, 1.14) and at visits by Black/African American patients (than at visits by White; OR=1.11, 95% CI=1.02, 1.20). In addition, age-related disparities were mitigated for visits by patients aged 40–64 and ≥65 years (e.g., age ≥65 years: physician, OR=0.66, 95% CI=0.59, 0.73; medical assistant protocol, OR=0.78, 95% CI=0.71, 0.85), compared with visits by patients aged 18–39 years.
Conclusions:
Implementation of a medical assistant protocol in a primary care setting may significantly increase depression screening rates while mitigating or removing sociodemographic disparities.
INTRODUCTION
Depression affects an estimated 8.1% of U.S. adults1,2 and is the leading cause of disability worldwide.1 Depression is associated with decreased life expectancy—up to 14 years for men and 10 years for women—as well as with many adverse health events and behaviors, including coronary artery disease, diabetes, and poor adherence to medical treatment.3–6 Screening for depression is the first step toward initiating treatment, and when screening is done, patients can experience improved treatment response and remission rates.7
In 2009 and again in 2016, the U.S. Preventive Services Task Force issued guidelines recommending universal screening of adults, including pregnant and postpartum women, and adolescents for symptoms of depression.7 Despite this recommendation, recent studies have found that as few as 4.2% of all primary care patients have ever been screened for depression.8
Moreover, research has shown that there are significant disparities in depression screening rates by patient demographics. Multiple studies have found that racial minorities, specifically African American, Latinx, and Asian patients, are significantly less likely to be screened for depression than their White counterparts.8–10 In addition, adults aged ≥65 years are up to half as likely to be screened as adults aged 45–64 years.8
Although there are a number of studies showing disparities in depression screening rates, there is scant guidance about how to eliminate these disparities. There is evidence from previous research that depression screening rates may be similar by race and sex using the Collaborative Care Model, an established model of systematic nurse care management supported by telephonic psychiatry consultation.11,12 However, the study did not examine screening rates before implementation, and it is unknown whether the Collaborative Care Model affected disparities.13 This study seeks to evaluate the potential for a systematic medical assistant (MA)-led screening to reduce disparities in rates of depression screening alongside a Primary Care–Behavioral Health model of integrated care.14 This article reports a quasi-experimental study of depression screening rates before and after the change in hospital policy. The analysis evaluates 2 hypotheses: (1) that an MA protocol for depression screening would increase rates overall and (2) that this protocol would reduce differences in screening rates by age, sex, and race, compared with physician-only depression screening.
METHODS
Study Sample
The study cohort consisted of patients at an adult internal medicine and an internal medicine/pediatrics practice at an urban academic medical center who were seen for primary care visits between 2016 and 2018. The 2 practices share staff, but the providers do not cross over between practices. Patients were considered eligible if they were aged ≥18 years and had not received depression screening within the year before the visit. Patients who had previously screened positive for depression, who had a recorded history of depression, or who were screened for depression within the last 12 months were excluded from the study.
In February 2016, the practice instituted population-wide depression screening for patients during routine clinic visits, alongside the Primary Care–Behavioral Health model implemented in the clinic. This model is a widely adopted approach that incorporates behavioral health providers, with colocated clinics and flexible scheduling, into primary care teams with the aim of both extending and supporting the services of primary care providers in the treatment of behavioral health conditions.14
Initially, only physicians were able to perform depression screening (the control group). At the practice, there were about 40 attending physicians and an average of 112 resident physicians and 4.5 MAs, with an MA-to-physician full-time equivalent ratio of 1:3. From November 2016 to August 2017, a pilot study was conducted in which MAs performed depression screening during clinic visit triage for 3 physicians. Because preliminary analysis revealed higher screening in the pilot group (40% vs 20%), hospital policy was changed to allow MAs to perform screening (the intervention). In September 2017, MAs assumed responsibility for screening all eligible patients practice-wide using a standardized protocol; no additional organization-level incentives to change clinical practice were offered, and there was no increase in MAs during the study period.
Measures
Throughout the study period, a passive alert (Best Practice Advisory [BPA]) was active in the Epic electronic health record (EHR) to remind physicians and MAs whether a patient was due for depression screening.15 The BPA was visible under the Planning window with equal prominence in both the physician and MA EHR user contexts. Although the BPA configuration was the same for both MAs and MDs, to access the BPAs, MAs had the additional step of navigating from the Rooming window—where they most frequently completed their work—to the Planning tab. By contrast, the primary care physician workflow initially defaults to the Planning window. Patients were due for screening if they had not received depression screening within the previous 12 months, did not have a current diagnosis of depression or bipolar disorder, or did not have a previous positive depression screening. The BPA included a link to a smart flow sheet for the Patient Health Questionnaire (PHQ)-2, a validated and widely used screening tool consisting of 2 questions.16 Originally, physicians were responsible for completing this screening through the BPA. Under the new policy, an MA verbally administered the PHQ-2 and entered the patient’s responses into the BPA. MAs were provided training in how to administer the PHQ-2, along with in-clinic support and posted reminders. It became an expectation of the MA role to complete this screening, and in September 2017, it became 1 of several metrics assessed when considering their job performance. If the patient screened positive (Score≥3), the MA would then provide the patient with a paper version of the PHQ-9 to complete the remaining 7 questions while waiting to see their physician, and a critical BPA was flagged in the patient’s EHR.17 The physicians were responsible for reviewing the PHQ-9 with the patient and entering the responses to the remaining questions into the EHR. If MAs were unable to complete depression screening, physicians were expected to administer depression screening.
Data were extracted from the EHR for visits 1 year before (September 2016–August 2017) and 10 years after (September 2017–August 2018) implementation of the MA screening protocol. All visits to the 3 physicians who participated in the pilot phase were excluded. The data had 4 levels: (1) clinical department, (2) physician, (3) patient, and (4) visit. Visits were classified by physician type (attending or resident) and specialty department (internal medicine or internal medicine/pediatrics). At the patient level, visits were classified by patient sex, age (18–39, 40–64, and ≥65 years), race (Asian, Black/African American, White, and other), and insurance type (Medicaid or other). Patients could have had multiple visits during the study period with different physicians. The outcome was whether depression screening was completed during the visit. Visit date was treated in 3 ways: (1) a binary indicator (pre/post) of whether the visit was before or after the implementation of the MA screening protocol, (2) years since study inception (September 2016), and (3) years since the beginning of intervention (September 2017).
Statistical Analysis
The sample and screening rates in each study group were described using frequencies and percentages. Chi-square tests were used to assess unadjusted pre–post changes in rates by demographic groups. To account for study design, an interrupted time-series analysis was conducted to examine the impact of an MA depression screening protocol. The unit of analysis was the patient visit, and the period of analysis was days. Differences in screening were analyzed using interrupted time-series generalized estimating equation logistic regression models. Bivariate analyses included study design variables and 1 patient characteristic, and multivariate analyses included study design variables and all patient characteristics.18 Interactions between each patient characteristic (age, sex, race, insurance) and the policy change were modeled accounting for temporal trends within each study period. Multiple visits per patient were modeled using repeated measures that assumed an autoregressive covariance model structure. Statistical significance was determined using 2-sided tests with a=0.05. Analyses were performed between April 2019 and April 2020 using SAS, version 9.4. This project was formally determined to be a quality improvement—not human subjects research—and was therefore not overseen by the University of Chicago Biological Sciences Division IRB.
RESULTS
Between September 2016 and August 2018, there were a total of 45,147 visits by 21,377 unique patients who were due for depression screening (Table 1). Of these, 27,987 (62%) visits were by women. Visits among adults aged 40–64 years and ≥65 years constituted about 40% of visits each. Majority of the visits were by Black/African American (66%) and White patients (27%). Only 4,792 (11%) of the visits were by patients insured through Medicaid. Half of the visits were to attending physicians (22,149, 49%). About 60% of the visits (26,498) occurred before the implementation of the MA screening protocol.
Table 1.
Characteristics of Primary Care Clinic Visits for Patients Due for Depression Screening, September 2016–August 2018
| Characteristics | All visits (N=45,147), n (%) | Physician only (n=26,498), n (%) | Medical assistant protocol (n=18,649), n (%) |
|---|---|---|---|
| Sex | |||
| Female | 27,987 (62) | 16,612 (63) | 11,375 (61) |
| Male | 17,160 (38) | 9,886 (37) | 7,274 (39) |
| Age, years | |||
| 18–39 | 7,364 (16) | 3,980 (15) | 3,384 (18) |
| 40–64 | 18,383 (41) | 10,789 (41) | 7,594 (41) |
| ≥65 | 19,400 (43) | 11,729 (44) | 7,671 (41) |
| Race | |||
| Asian | 1,771 (4) | 941 (4) | 830 (4) |
| Black/African American | 29,573 (66) | 17,782 (67) | 11,791 (63) |
| Other | 1,029 (2) | 553 (2) | 476 (3) |
| White | 12,026 (27) | 6,811 (26) | 5,215 (28) |
| Unknown | 748 (2) | 411 (2) | 337 (2) |
| Insurance | |||
| Medicaid | 4,792 (11) | 3,074 (12) | 1,718 (9) |
| Other | 40,281 (89) | 23,391 (88) | 16,890 (91) |
| Unknown | 74 (0) | 33 (0) | 41 (0) |
| Physician type | |||
| Attending | 22,149 (49) | 13,311 (50) | 8,838 (47) |
| Resident | 22,998 (51) | 13,187 (50) | 9,811 (53) |
| Specialty | |||
| Internal medicine | 42,203 (93) | 25,013 (94) | 17,190 (92) |
| Internal medicine and pediatrics | 2,944 (7) | 1,485 (6) | 1,459 (8) |
Note: Percentages may not total 100 owing to rounding.
Overall, depression screening rates increased from 18% of visits with physician-only screening to 57% after the implementation of the MA screening protocol (p<0.0001) (Table 2). Screening rates increased across all the measured demographics, notably from 15% to 54% of visits by adults aged ≥65 years, from 14% to 53% of visits by Medicaid patients, and from 17% to 57% of visits by Black/African American patients (all p<0.0001) (Figure 1).
Table 2.
Unadjusted Screening Rates Pre- and Post-Policy Change, Overall and by Patient Characteristics (N=45,147 Visits)
| Physician only (n=26,498) | Medical assistant protocol (n=18,649) | |||
|---|---|---|---|---|
| Characteristics | n Visits | n Screened (%) | n Visits | n Screened (%) |
| Overall | 26,498 | 4,777 (18) | 18,649 | 10,704 (57) |
| Sex | ||||
| Female | 16,612 | 2,886 (17) | 11,375 | 6,603 (58) |
| Male | 9,886 | 1,891 (19) | 7,274 | 4,101 (56) |
| Age, years | ||||
| 18–39 | 3,980 | 902 (23) | 3,384 | 2,073 (61) |
| 40–64 | 10,789 | 2,106 (20) | 7,594 | 4,461 (59) |
| ≥65 | 11,729 | 1,769 (15) | 7,671 | 4,170 (54) |
| Race | ||||
| Asian | 941 | 250 (27) | 830 | 532 (64) |
| Black/African American | 17,782 | 2,952 (17) | 11,791 | 6,751 (57) |
| Other | 553 | 116 (21) | 476 | 279 (59) |
| White | 6,811 | 1,366 (20) | 5,215 | 2,937 (56) |
| Insurance | ||||
| Medicaid | 3,074 | 427 (14) | 1,718 | 911 (53) |
| Other | 23,391 | 4,349 (19) | 16,890 | 9,768 (58) |
| Physician type | ||||
| Attending | 13,311 | 2,550 (19) | 8,838 | 5,236 (59) |
| Resident | 13,187 | 2,227 (17) | 9,811 | 5,468 (56) |
| Specialty | ||||
| Internal medicine | 25,013 | 4,132 (17) | 17,190 | 9,579 (56) |
| Internal medicine and pediatrics | 1,485 | 645 (43) | 1,459 | 1,125 (77) |
Note: Percentages may not total to 100 owing to rounding. All pre–post changes p<0.0001.
Figure 1.
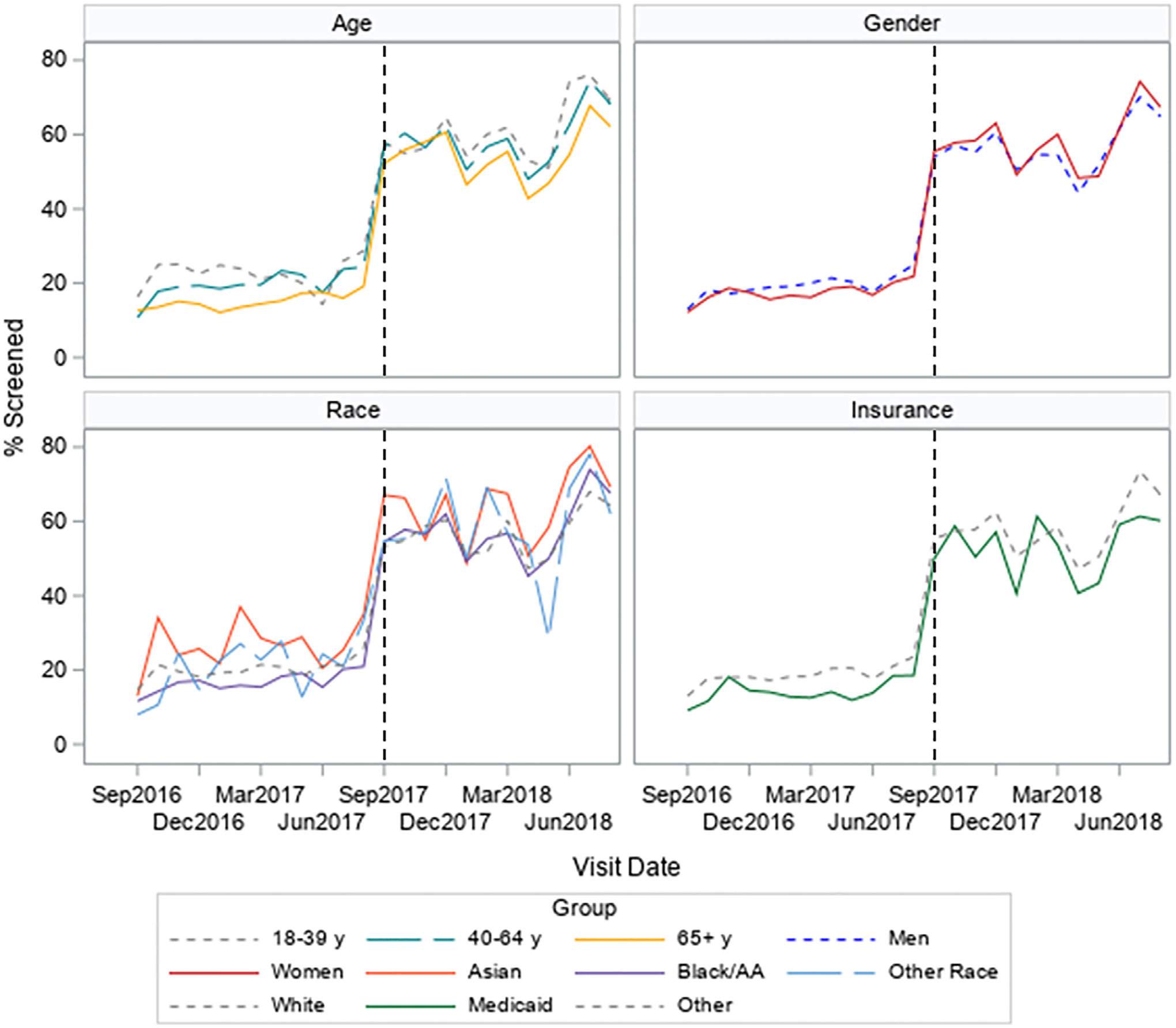
Unadjusted monthly mean depression screening rates by patient characteristics for physician screening (September 2016‒August 2017; n=26,498 visits) and medical assistant screening (September 2017‒August 2018; n=18,649 visits).
AA, African American; Dec, December; Jun, June; Mar, March; Sep, September; y, year.
After the implementation of the MA screening protocol, demographic differences in depression screening rates were inverted or reduced. With physician-only screening, screening for depression was less likely performed at visits for women than for men (OR=0.91, 95% CI=0.85, 0.98) (Table 3); however, with the MA screening protocol, depression screening was slightly more likely for visits by women than for men (OR=1.07, 95% CI=1.0002, 1.14). Similarly, with physician-only screening, depression screening was less likely at visits by Black/African American adults than by White adults (OR=0.91, 95% CI=0.84, 0.99); however, with MA screening, visits by Black/African American patients were more likely to include screening than visits by White patients (OR=1.11, 95% CI=1.02, 1.20).
Table 3.
Adjusted Interrupted Time-Series Model for Depression Screening by Patient Characteristics, Pre- and Post-Policy Change (N=45,147 Visits)
| Physician only (n=26,498 visits) | Medical assistant protocol (n=18,649 visits) | |||||||
|---|---|---|---|---|---|---|---|---|
| Bivariate | Multivariate | Bivariate | Multivariate | |||||
| Characteristics | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value |
| Sex | ||||||||
| Male | ref | ref | ref | ref | ||||
| Female | 0.89 (0.83, 0.95) | <0.001 | 0.91 (0.85, 0.98) | 0.01 | 1.07 (0.998,1.14) | 0.06 | 1.07 (1.0002, 1.14) | 0.049 |
| Age, years | ||||||||
| 18–39 | ref | ref | ref | ref | ||||
| 40–64 | 0.85 (0.77, 0.93) | <0.001 | 0.88 (0.80, 0.97) | 0.01 | 0.93 (0.75, 1.01) | 0.08 | 0.91 (0.83, 0.998) | 0.045 |
| ≥65 | 0.89 (0.83, 0.95) | <0.001 | 0.66 (0.59, 0.73) | <0.0001 | 0.79 (0.72, 0.86) | <0.001 | 0.78 (0.71, 0.85) | <0.001 |
| Race | ||||||||
| White | ref | ref | ref | ref | ||||
| Asian | 0.82 (0.76, 0.89) | <0.001 | 1.31 (1.11, 1.55) | 0.001 | 1.32 (1.12, 1.55) | <0.001 | 1.28 (1.09, 1.50) | 0.003 |
| Black/African American | 0.82 (0.76, 0.89) | <0.001 | 0.91 (0.84, 0.99) | 0.02 | 1.07 (0.99,1.15) | 0.08 | 1.11 (1.02,1.20) | 0.01 |
| Other | 1.04 (0.83, 1.30) | 0.75 | 1.00 (0.80, 1.26) | 1.00 | 1.10 (0.89, 1.36) | 0.36 | 1.06 (0.87, 1.31) | 0.56 |
| Insurance | ||||||||
| Other | ref | ref | ref | ref | ||||
| Medicaid | 0.72 (0.64, 0.80) | <0.001 | 0.73 (0.65, 0.81) | <0.0001 | 0.85 (0.77, 0.95) | 0.003 | 0.81 (0.73, 0.90) | 0.0001 |
Note: Boldface indicates statistical significance (p<0.05).
This statistical significance was based on Wald tests from interrupted time-series generalized estimating equation logistic regression models. Adjusted for physician type and specialty department with repeated effects for repeat patient visits, patients were cross-classified by 228 physicians, and physicians were nested within 2 specialty departments.
Differences by age and insurance type improved to a lesser degree. Compared with visits by adults aged 18–39 years, under physician-only screening, visits by adults aged 40–64 years had 12% lower odds (OR=0.88, 95% CI=0.80, 0.97), and visits by patients aged ≥65 years had 34% lower odds (OR=0.66, 95% CI=0.59, 0.73) of screening. These numbers improved to ORs of 0.91 (95% CI=0.83, 0.998) and 0.78 (95% CI=0.71, 0.85), respectively. Likewise, patients insured through Medicaid had 27% lower odds of being screened during their visits with physician-only screening (OR=0.73, 95% CI=0.65, 0.81) than patients with other insurance plans, and with the MA screening protocol, the difference was smaller but remained present (OR=0.81, 95% CI=0.73, 0.90).
Some associations between patient demographics and depression screening rates did not change. For example, before and after the MA screening protocol, visits by Asians were more likely to include screening than visits by Whites (OR=1.31, 95% CI=1.11, 1.55 and OR=1.28, 95% CI=1.09, 1.50, respectively).
DISCUSSION
In this 2-year study, a protocol for MAs to conduct depression screening during visit triage increased screening rates by 3-fold in a primary care clinic. Increases were observed across all the measured demographics, including a 3.6-fold increase among visits by adults aged ≥65 years and a 3.4-fold increase among visits by Black/African American patients. Differences in visit screening rates by sex, age, race, and insurance type also decreased after the implementation of the MA screening protocol, although some differences remained, particularly for patients aged ≥65 years and for those with Medicaid insurance.
Allowing MAs to conduct depression screening led to a near 40% increase in the rate of depression screening across the practice, in addition to the elimination and mitigation of several sociodemographic disparities in depression screening. Improvements in overall screening rates bolster the odds that patients with depression are identified, potentially increasing access to treatment and improving outcomes, including the rates of treatment response and remission.7 The amelioration of sociodemographic disparities in screening rates allows for improved diagnosis and treatment of underserved populations and is an important step toward achieving healthcare equity. Previous studies have described the effectiveness of MA-driven protocols in improving care outcomes among minority and low-income populations.19,20 To date, however, there have been few studies that explicitly utilize an MA-driven protocol in an effort to reduce healthcare disparities.
Consistent with the literature, before the implementation of the MA screening protocol, Black/African American patients were less likely to be screened for depression than White patients,8,21 a disparity that was inverted with MA-led screening. Systematic underscreening for depression among Black/African American patients may be due to perpetuation of the notion that Blacks/African Americans experience less depression. Although studies suggest that lifetime prevalence is lower for Blacks/African Americans than for Whites, the 12-month prevalence is similar, and persistence of symptoms is significantly higher for Blacks/African Americans than for Whites.22 In addition, Black/ African American patients with depression may present differently from White patients, decreasing the sensitivity of unstandardized clinician-based diagnoses, especially when there is cultural discordance.23–25 Therefore, race-based analyses of depression screening rates, such as that done in this study, are essential to uncovering the disparities that could otherwise perpetuate through the depression care cascade. From these results, adoption of a systematic MA screening protocol appears to be a promising method for eradicating such disparities in a primary care setting.
The analysis also found that women were less likely to be screened for depression under physician-only screening, a difference that was removed with the MA screening protocol. Previous studies on sex disparities in depression screening showed mixed results, with some indicating that men were less likely to be screened and others finding that women were less likely to be screened.8–10,26 However, women constitute a population that is particularly vulnerable to depression. Women are >1.5 times as likely as men to develop depression, with 1 in 5 women reporting experiencing an episode during their lifetime.27 Ensuring that women are screened for depression is critical to its detection and initiation of treatment.
This study also found that older patients and those with Medicaid were less likely to be screened for depression, both before and after intervention, despite an overall increase in screening rates. Medical complexity may contribute to these disparities in screening. Older patients tend to be less physically healthy than their younger counterparts28 and, similar to those insured through Medicaid, frequently carry multiple medical diagnoses that require more intensive and longer-term follow-up.29,30 This increase in both the number and severity of health issues presents a dilemma to the primary care provider, who has a limited amount of time to spend in a patient encounter. Screening for new health conditions, such as major depressive disorder (which if found can increase the visit length), may be eschewed in favor of dedicating more time to more readily apparent health concerns or chronic disease management. In addition, providers may rely on the clinical detection of common signs or symptoms of depression before considering administering screening. However, because depression has a different presentation in older age,31 many cases will be missed. Although older adults may be screened for depression at lower rates, the rates of depression among this population are actually higher and have been found to increase with age.32 After the implementation of MA screening, differences in screening rates for the oldest patients and those insured through Medicaid persisted but became less pronounced. Further research is needed to identify the remaining barriers to equitable screening in these populations.
Although overall screening rates surged with the implementation of the MA protocol, about 40% of patients remained unscreened. Discomfort with engaging patients in the discussion of mental health topics such as depression may remain an impediment to achieving higher screening rates. Time limitations and misguided concerns that inquiring about mental health issues may trigger mental health issues might be additional reasons why providers and MAs fail to perform mental health screening.33,34 Although the systematization of the MA protocol sought to overcome these barriers, it is likely that some remain. Enhanced provider/MA education and feedback, including provider report cards,15 and additional systematic interventions, such as previsit telephonic or computer-based screening or waiting room prework, may be beneficial in further reducing the barriers to screening and improving overall screening rates.
Limitations
This study has several limitations. It is a single-center study performed at an academic teaching hospital in an urban setting where most patients are Black/African American and female. As such, results may not be generalizable to other healthcare settings. Depression screening was only captured when providers entered information through the EHR BPA; therefore, instances when screening was done but not recorded or recorded elsewhere in the EHR may have been missed in the analysis. However, a retrospective chart review of visits in which screening did not occur found that the majority of these patients received no assessment of their mental state through PHQ-2 or otherwise. Data on other patient characteristics, such as ethnicity, ZIP code, and health status, were not available for analysis.
CONCLUSIONS
This study found that an MA protocol led to a 3-fold increase in depression screening rates and reductions in disparities in depression screening among different demographic groups. Using nonphysician staff in primary care clinics to complete depression screening is an important strategy to increase screening rates and mitigate the disparities in depression screening. Future investigation should focus on analyzing screening rates by other demographics, including ethnicity and ZIP code, analyzing the impact of such a protocol on achieving screening equity among these groups, as well as analyzing the impact of depression screening on treatment rates and patient outcomes.
ACKNOWLEDGMENTS
The entities providing funding to this study had no role in study design; collection, analysis, interpretation of data; writing of the report; or the decision to submit the report for publication.
This work was supported through funds from the University of Chicago Medicine Innovation Grant Program. NL and EMS received support from Agency for Healthcare Research and Quality U18 HS26151.
Footnotes
A poster of this study was presented at the Academy Health 12th Annual Conference on the Science of Dissemination and Implementation at Arlington, VA in December 2019.
No financial disclosures were reported by the authors of this study.
REFERENCES
- 1.WHO. Depression and other common mental disorders: global health estimates. Geneva, Switzerland: WHO. https://apps.who.int/iris/bit-stream/handle/10665/254610/WHO-MSD-MER-2017.2-eng.pdf. Published 2017. Accessed July 31, 2020. [Google Scholar]
- 2.Brody DJ, Pratt LA, Hughes JP. Prevalence of depression among adults aged 20 and over: United States, 2013–2016. NCHS Data Brief. 2018(303):1–8. https://www.cdc.gov/nchs/data/databriefs/db303.pdf. Accessed July 31, 2020. [PubMed] [Google Scholar]
- 3.Laursen TM, Musliner KL, Benros ME, Vestergaard M, Munk-Olsen T. Mortality and life expectancy in persons with severe unipolar depression. J Affect Disord. 2016;193:203–207. 10.1016/j.jad.2015.12.067. [DOI] [PubMed] [Google Scholar]
- 4.Lett HS, Blumenthal JA, Babyak MA, et al. Depression as a risk factor for coronary artery disease: evidence, mechanisms, and treatment. Psychosom Med. 2004;66(3):305–315. 10.1097/01.psy.0000126207.43307.c0. [DOI] [PubMed] [Google Scholar]
- 5.Knol MJ, Twisk JW, Beekman AT, Heine RJ, Snoek FJ, Pouwer F. Depression as a risk factor for the onset of type 2 diabetes mellitus. A meta-analysis. Diabetologia. 2006;49(5):837–845. 10.1007/s00125-006-0159-x. [DOI] [PubMed] [Google Scholar]
- 6.DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160(14):2101–2107. 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]
- 7.Siu AL. U.S. Preventive Services Task Force (USPSTF), Bibbins-Domingo K et al. Screening for depression in adults: US Preventive Services Task Force recommendation statement. JAMA. 2016;315(4):380–387. 10.1001/jama.2015.18392. [DOI] [PubMed] [Google Scholar]
- 8.Akincigil A, Matthews EB. National rates and patterns of depression screening in primary care: results from 2012 and 2013. Psychiatr Serv. 2017;68(7):660–666. 10.1176/appi.ps.201600096. [DOI] [PubMed] [Google Scholar]
- 9.Kato E, Borsky AE, Zuvekas SH, Soni A, Ngo-Metzger Q. Missed opportunities for depression screening and treatment in the United States. J Am Board Fam Med. 2018;31(3):389–397. 10.3122/jabfm.2018.03.170406. [DOI] [PubMed] [Google Scholar]
- 10.Hahm HC, Cook BL, Ault-Brutus A, Alegría M. Intersection of race-ethnicity and gender in depression care: screening, access, and minimally adequate treatment. Psychiatr Serv. 2015;66(3):258–264. 10.1176/appi.ps.201400116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brown AF, Vassar SD, Connor KI, Vickrey BG. Collaborative care management reduces disparities in dementia care quality for caregivers with less education. J Am Geriatr Soc. 2013;61(2):243–251. 10.1111/jgs.12079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chin MH, Cook S, Drum ML, et al. Improving diabetes care in Mid-west community health centers with the health disparities collaborative [published correction appears in Diabetes Care. 2004;27(8):2099]. Diabetes Care. 2004;27(1):2–8. 10.2337/diacare.27.1.2. [DOI] [PubMed] [Google Scholar]
- 13.Thompson H, Faig W, Gupta N, et al. Collaborative care for depression of adults and adolescents: measuring the effectiveness of screening and treatment uptake. Psychiatr Serv. 2019;70(7):604–607. 10.1176/appi.ps.201800257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reiter JT, Dobmeyer AC, Hunter CL. The primary care behavioral health (PCBH) model: an overview and operational definition. J Clin Psychol Med Settings. 2018;25(2):109–126. 10.1007/s10880-017-9531-x. [DOI] [PubMed] [Google Scholar]
- 15.Yin I, Wan W, Staab EM, Vinci L, Laiteerapong N. Use of report cards to increase primary care physician depression screening. J Gen Intern Med. Online July 23, 2020 In press. 10.1007/s11606-020-06065-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41 (11):1284–1292. 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 17.Ell K, Unützer J, Aranda M, Sanchez K, Lee PJ. Routine PHQ-9 depression screening in home health care: depression, prevalence, clinical and treatment characteristics and screening implementation. Home Health Care Serv Q. 2005;24(4):1–19. 10.1300/J027v24n04_01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kontopantelis E, Doran T, Springate DA, Buchan I, Reeves D. Regression based quasi-experimental approach when randomisation is not an option: interrupted time series analysis. BMJ. 2015;350:h2750. 10.1136/bmj.h2750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Willard-Grace R, Chen EH, Hessler D, et al. Health coaching by medical assistants to improve control of diabetes, hypertension, and hyperlipidemia in low-income patients: a randomized controlled trial. Ann Fam Med. 2015;13(2):130–138. 10.1370/afm.1768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nelson K, Pitaro M, Tzellas A, Lum A. Practice profile. Transforming the role of medical assistants in chronic disease management. Health Aff (Millwood). 2010;29(5):963–965. 10.1377/hlthaff.2010.0129. [DOI] [PubMed] [Google Scholar]
- 21.Stockdale SE, Lagomasino IT, Siddique J, McGuire T, Miranda J. Racial and ethnic disparities in detection and treatment of depression and anxiety among psychiatric and primary health care visits, 1995–2005. Med Care. 2008;46(7):668–677. 10.1097/MLR.0b013e3181789496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Williams DR, Gonz alez HM, Neighbors H, et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: results from the National Survey of American Life. Arch Gen Psychiatry. 2007;64(3):305–315. 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]
- 23.Bailey RK, Mokonogho J, Kumar A. Racial and ethnic differences in depression: current perspectives. Neuropsychiatr Dis Treat. 2019;15:603–609. 10.2147/NDT.S128584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Whaley AL. Ethnicity/race, paranoia, and psychiatric diagnoses: clinician bias versus sociocultural differences. J Psychopathol Behav Assess. 1997;19(1):1–20. 10.1007/BF02263226. [DOI] [Google Scholar]
- 25.Baker FM. Diagnosing depression in African Americans. Community Ment Health J. 2001;37(1):31–38. 10.1023/a:1026540321366. [DOI] [PubMed] [Google Scholar]
- 26.Jones LE, Doebbeling CC. Depression screening disparities among veterans with diabetes compared with the general veteran population. Diabetes Care. 2007;30(9):2216–2221. 10.2337/dc07-0350. [DOI] [PubMed] [Google Scholar]
- 27.Kessler RC, McGonagle KA, Swartz M, Blazer DG, Nelson CB. Sex and depression in the National Comorbidity Survey. I: lifetime prevalence, chronicity and recurrence. J Affect Disord. 1993;29(2–3):85–96. 10.1016/0165-0327(93)90026-g. [DOI] [PubMed] [Google Scholar]
- 28.Hopman WM, Harrison MB, Coo H, Friedberg E, Buchanan M, Van-DenKerkhof EG. Associations between chronic disease, age and physical and mental health status. Chronic Dis Can. 2009;29(3):108–116. 10.24095/hpcdp.29.3.03. [DOI] [PubMed] [Google Scholar]
- 29.Salisbury C, Johnson L, Purdy S, Valderas JM, Montgomery AA. Epidemiology and impact of multimorbidity in primary care: a retrospective cohort study. Br J Gen Pract. 2011;61(582):e12–e21. 10.3399/bjgp11X548929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chapel JM, Ritchey MD, Zhang D, Wang G. Prevalence and medical costs of chronic diseases among adult Medicaid beneficiaries. Am J Prev Med. 2017;53(6S2):S143–S154. 10.1016/j.amepre.2017.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rodda J, Walker Z, Carter J. Depression in older adults. BMJ. 2011;343:d5219. 10.1136/bmj.d5219. [DOI] [PubMed] [Google Scholar]
- 32.Kok RM, Reynolds CF 3rd. Management of depression in older adults: a review. JAMA. 2017;317(20):2114–2122. 10.1001/jama.2017.5706. [DOI] [PubMed] [Google Scholar]
- 33.Hart S, Morris R. Screening for depression after stroke: an exploration of professionals’ compliance with guidelines. Clin Rehabil. 2008;22 (1):60–70. 10.1177/0269215507079841. [DOI] [PubMed] [Google Scholar]
- 34.Hammond MF. Doctors’ and nurses’ observations on the Geriatric Depression Rating Scale. Age Ageing. 2004;33(2):189–192. 10.1093/ageing/afh037. [DOI] [PubMed] [Google Scholar]


