Abstract
Objective
The aim of this study was to compare the diagnostic performances of digital tomosynthesis (DTS) and conventional radiography in detecting osteonecrosis of the femoral head (ONFH) using computed tomography (CT), as the reference standard and evaluate the diagnostic reproducibility of DTS.
Materials and Methods
Forty-five patients (24 male and 21 female; age range, 25–77 years) with clinically suspected ONFH underwent anteroposterior radiography, DTS, and CT. Two musculoskeletal radiologists independently evaluated the presence and type of ONFH. The diagnostic performance of radiography and DTS in detecting the presence of ONFH and determining the types of ONFH were evaluated. The interobserver and intraobserver reliabilities of each imaging modality were analyzed using Cohen's kappa.
Results
DTS had higher sensitivity (89.4%–100% vs. 74.5%–76.6%) and specificity (97.3%–100% vs. 78.4%–83.8%) for ONFH detection than radiography. DTS showed higher performance than radiography in identifying the subtypes of ONFH with statistical significance in one reader (type 1, 100% vs. 30.8%, p = 0.004; type II, 97.1% vs. 73.5%, p = 0.008). The interobserver agreement was excellent for DTS and moderate for radiography (kappa of 0.86 vs. 0.57, respectively). The intraobserver agreement for DTS was higher than that of radiography (kappa of 0.96 vs. 0.69, respectively).
Conclusion
DTS showed higher diagnostic performance and reproducibility than radiography in detecting ONFH. DTS may be used as a first-line diagnostic modality instead of radiography for patients suspected of having ONFH.
Keywords: Digital tomosynthesis, Osteonecrosis, Femoral head, Reproducibility, Agreement
INTRODUCTION
Osteonecrosis of the femoral head (ONFH) is relatively common and primarily affects patients in the third to fifth decades of life [1]. Ischemic death of the bone and marrow cells is the end result of ONFH; however, its exact pathogenesis is not fully understood [1,2]. Among the various etiologies of ONFH, the most common causes are idiopathic origin, trauma, corticosteroid use, and alcoholism [3]. ONFH is usually asymptomatic during the early stages, and deep groin pain is the most common clinical symptom in symptomatic patients. Early diagnosis is important because treatment is based on the disease stage, and ONFH often leads to femoral head collapse if left untreated [4,5]. In the absence of specific physical or laboratory findings that allow a definitive diagnosis of ONFH, imaging is essential.
Radiography is the initial imaging assessment performed for patients with clinically suspected ONFH [2,3]. It is the least expensive imaging modality, and it is widely available. However, it is insensitive to early changes in ONFH, which usually requires additional radiological assessment. Multidetector computed tomography (CT) is superior to radiography for detecting articular collapse of the femoral head, its location, and combined secondary degenerative joint disease [6,7]. Nevertheless, it is less sensitive than magnetic resonance imaging (MRI) and has the disadvantage of radiation exposure. MRI is the most sensitive and specific radiologic modality for detecting ONFH [2,3,5,8,9]. However, considering the cost of examination, prolonged acquisition time, limited availability, and the difficulty performing it in patients with claustrophobia, the usefulness of MRI as a regular screening test is restricted.
Digital tomosynthesis (DTS) is a recently developed imaging modality that uses standard X-ray equipment with digital flat panel detectors to create images from a series of projection radiographs obtained at different angles [10,11,12]. It has been shown to be useful for imaging various body parts, including the breast [13,14], chest [15], head and neck [16], and musculoskeletal system [17,18,19].
Few studies have reported the potential role of DTS as a tool for detecting ONFH. The aim of this study was to compare the diagnostic performance of DTS in detecting ONFH with that of conventional radiography using CT as the reference standard and evaluate the diagnostic reproducibility of DTS.
MATERIALS AND METHODS
Participants
This retrospective study was approved by our Institutional Review Board, and the requirement for informed consent was waived. A total of 45 patients (24 male and 21 female; age range, 25–77 years) who underwent DTS, radiography, and CT for the evaluation of ONFH between December 2012 and September 2018 were consecutively enrolled in this study. All patients were older than 18 years, and they were examined using the three techniques within a week.
Radiography
Digital radiographic examination (Discovery XR656; GE Healthcare) was performed for each patient, including the anteroposterior (AP) view of the pelvis and two lateral views of the bilateral hip joints. This system can be used for both conventional and DTS imaging. The tube voltage was 75 kV, and the variable tube current (mA) was adjusted by automatic exposure control (AEC) depending on the patient.
Digital Tomosynthesis
Pelvic DTS was performed in an X-ray room with DTS equipment (Discovery XR656 with VolumeRAD option; GE Healthcare). Each DTS examination was performed with the patient in a supine position on the table, and the source-to-image distance was 100 cm for the central projection. The examinations were performed using a tube voltage of 80 kV, a total filtration of 2.7 Al, and an anti-scatter grid (grid ratio 10:1, strip density 70 lines/cm). The dose ratio was 8:1. Low-dose projection images were obtained with a minimum of 1.6 mA per projection. The scout image was an AP pelvic projection image collected using the AEC.
During the DTS examination, the detector was fixed, and the X-ray tube was moved using a continuous sweeping motion along a straight line in the caudocranial direction. With an angular movement between −20° and +20°, a mean of 60 low-dose projection radiographs were obtained. The reconstructions had a thickness of 2 mm. The scan duration was approximately 11 seconds.
The registered dose-area product (DAP), field size, and tube angle were obtained from the Digital Imaging and Communications in Medicine header of each projection radiograph. The effective doses were calculated for each patient using the following formula: E = EDAP × DAP (mSv). EDAP is the conversion factor, which is 0.29 mSv/Gycm2, and it was obtained from the Swedish Radiation Protection Authority as described by Göthlin and Geijer [20].
CT Acquisition
Multidetector CT images were acquired with variable CT scanners (Sensation 16; Siemens, SOMATOM Definition Flash; Siemens, Brilliance 64; Philips). The acquisition parameters were 120 kV and 100–483 mA, depending on the patient's body habitus. Axial 3-mm-thick sections were obtained to reconstruct 3-mm thick coronal, sagittal, and axial sections. Dual-energy CT (DECT) was performed using a Siemens SOMATOM Definition Flash CT scanner for eight patients who underwent internal fixation or a hip arthroplasty. For the DECT protocol, tube voltages of 140 and 100 kV were used with tube currents of 483 mA and 250 mA, respectively. The dose-length product was assessed, and effective doses were calculated using a κ coefficient of 0.015 [21].
Image Analysis
Two musculoskeletal radiologists, both with more than 10 years of experience, independently analyzed the radiography, DTS, and CT images. Both readers were blinded to the previous radiologic reports and clinical information. The images were anonymized and randomized before the interpretation. The interval between the image analyses for each modality was at least 2 weeks to avoid recall bias.
The presence or absence of ONFH was identified for each femoral head using images from different modalities. If ONFH was present, it was classified into two types: one with a reactive interface showing linear sclerosis without fracture or collapse (type I) and the other with a crescent sign or collapse (type II). After a washout period of four weeks, reader A interpreted the images from each modality to allow the assessment of the intraobserver agreement. Discrepancies related to CT interpretation were resolved by consensus, which was reached four weeks after the second imaging interpretation of reader A. If a pelvic MR image obtained within one month from our hospital or another hospital was available, it was also referred to when the readers reached the final consensus.
Statistical Analysis
The sensitivity, specificity, positive and negative predictive values, and accuracy for each reader and each imaging technique for ONFH detection were calculated using CT as the reference standard. The sensitivities, specificities, and accuracies of the imaging modalities were compared using McNemar's test. The interobserver and intraobserver agreements for each imaging method, including the subtyping of the ONFH, were assessed using Cohen's kappa (κ) test. The κ values were interpreted as follows: slight agreement, κ < 0.20; fair agreement, κ = 0.20–0.39; moderate agreement, κ = 0.40–0.59; substantial agreement, κ = 0.60–0.79; or excellent agreement, κ ≥ 0.80.
All calculations were performed using IBM SPSS Statistics for Windows (version 24.0; IBM Corp.), with a p value of < 0.05 indicating significance.
RESULTS
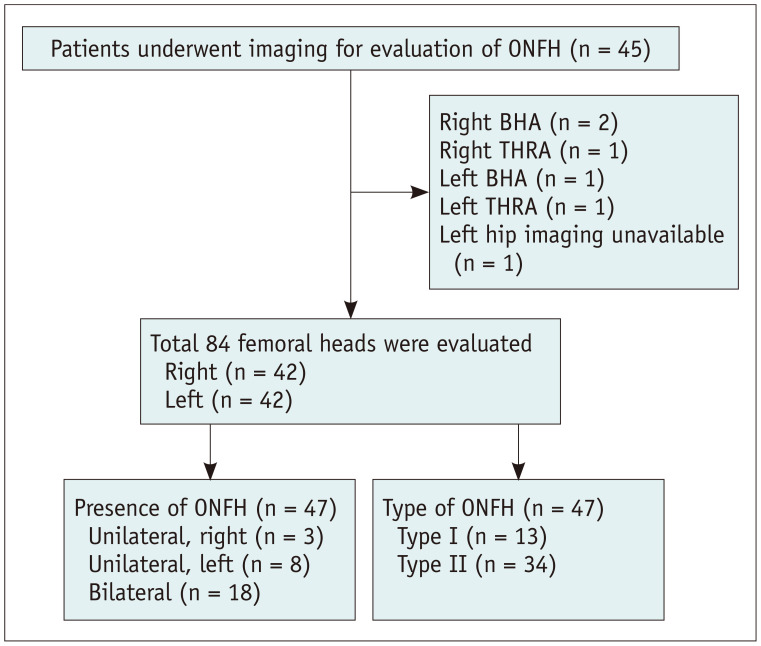
Forty-five consecutive patients (24 male, 21 female) with a mean age ± standard deviation (SD) of 52.1 ± 14.9 years (range, 25–77 years) were included in the study (Fig. 1). The patient demographics are provided in Table 1. Two patients underwent right bipolar hip arthroplasty (BHA), one patient underwent right total hip replacement arthroplasty (THRA), one patient underwent left BHA, and one patient underwent left THRA. In one patient, only images of the right femoral head were obtained. A total of 42 right and left femoral heads were included in the study. Twenty-nine patients had ONFH, including 11 with unilateral ONFH (3 right and 8 left) and 18 with bilateral ONFH. Of the 47 cases of ONFH, 13 were type I and 34 were type II. Pelvic MRI was performed in 10 patients within one month, and MR images obtained from other hospitals were available for five patients.
Fig. 1. Flow diagram for patient inclusion and exclusion.
BHA = bipolar hemiarthroplasty, ONFH = osteonecrosis of the femoral head, THRA = total hip replacement arthroplasty
Table 1. Patient Characteristics.
| Variables | Data | ||
|---|---|---|---|
| Sex | |||
| Male | 24 (53) | ||
| Female | 21 (47) | ||
| Age, years | 52.1 ± 14.9 | ||
| Etiology | |||
| Idiopathic | 12 | ||
| Rheumatoid arthritis | 9 | ||
| SLE | 7 | ||
| Trauma | 7 | ||
| Osteoarthritis | 5 | ||
| Alcoholism | 3 | ||
| Polymyositis | 1 | ||
| Systemic sclerosis | 1 | ||
| Presence of ONFH* | 47 (56) | ||
| Unilateral | 11 | ||
| Right | 3 | ||
| Left | 8 | ||
| Bilateral | 18 | ||
| Type of ONFH* | |||
| Type I | 13 (28) | ||
| Type II | 34 (72) | ||
*Data are number of patients or hips with the percentage in parenthesis, except for age for which mean ± standard deviation is presented. ONFH = osteonecrosis of the femoral head, SLE = systemic lupus erythematosus
The sensitivity of DTS for ONFH detection was significantly higher than that of radiography for both readers, as shown in Table 2 (89.4%–100% vs. 74.5%–76.6%, respectively). The specificity of DTS was also higher than that of radiography, although the result was not statistically significant for reader A (reader A: 97.3% vs. 83.8%, p = 0.063; reader B: 100% vs. 78.4%, p = 0.008). DTS had a higher accuracy than radiography for both readers (94.0%–98.8% vs. 76.8%–76.8%, respectively).
Table 2. Diagnostic Performance of Radiography and DTS for Each Reader in Detecting Osteonecrosis of the Femoral Head.
| Reader A | Reader B | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Accuracy (%) | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Accuracy (%) | |
| Radiography | 76.6 (36/47) | 83.8 (31/37) | 85.7 (36/42) | 73.8 (31/42) | 79.8 (67/84) | 74.5 (35/47) | 78.4 (29/37) | 81.4 (35/43) | 70.7 (29/41) | 76.2 (64/84) |
| DTS | 100 (47/47) | 97.3 (36/37) | 97.9 (47/48) | 100 (36/36) | 98.8 (83/84) | 89.4 (42/47) | 100 (37/37) | 100 (42/42) | 88.1 (37/42) | 94.0 (79/84) |
| p value | < 0.001 | 0.063 | < 0.001 | 0.016 | 0.008 | < 0.001 | ||||
DTS = digital tomosynthesis, NPV = negative predictive value, PPV = positive predictive value
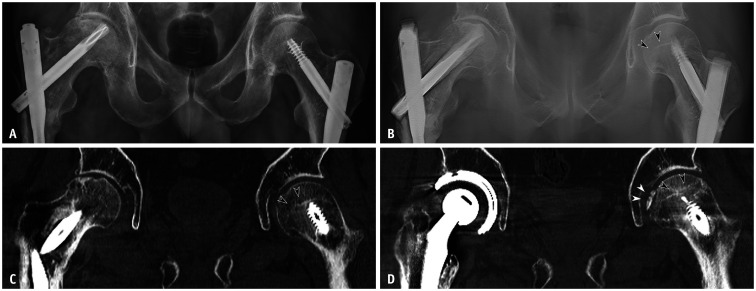
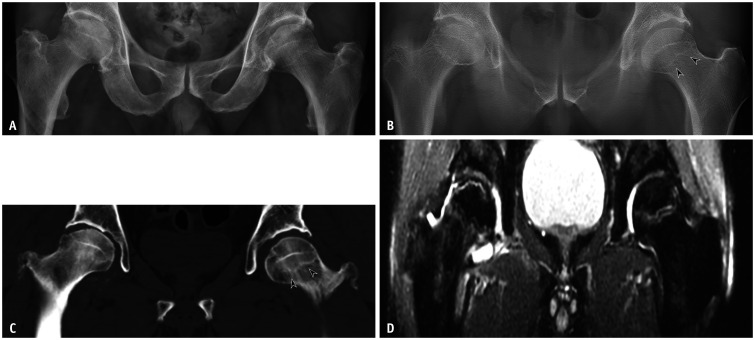
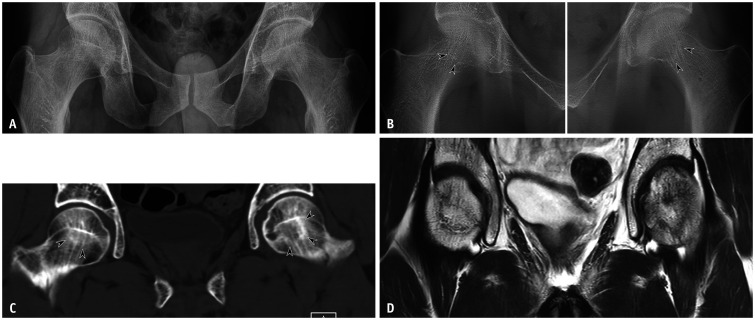
Table 3 shows the performances of radiography and DTS in identifying the subtypes of ONFH (Figs. 2,3,4). For both readers, the performance of DTS was higher than that of radiography for both types I and II, with statistical significance for reader A but not reader B.
Table 3. Performance of Radiography and DTS in Identifying the Type of Osteonecrosis of the Femoral Head.
| Type I (%, n = 13) | Type II (%, n = 34) | ||
|---|---|---|---|
| Reader A | |||
| Radiography | 30.8 (4/13) | 73.5 (25/34) | |
| DTS | 100 (13/13) | 97.1 (33/34) | |
| p value | 0.004 | 0.008 | |
| Reader B | |||
| Radiography | 15.4 (2/13) | 91.2 (31/34) | |
| DTS | 53.8 (7/13) | 100 (34/34) | |
| p value | 0.125 | 0.25 | |
DTS = digital tomosynthesis
Fig. 2. A 62-year-old male with bilateral intramedullary nailing in the femurs.
A. Radiograph with the anteroposterior view shows a collapsed right femoral head and normal left femoral head. B. Digital tomosynthesis image shows similar findings for the right femoral head and linear sclerosis involving the left femoral head without collapse (arrowheads). C. CT images also show linear sclerosis at the left femoral head (arrowheads), suggesting type I osteonecrosis of the femoral head (Association Research Circulation Osseous stage II) at the left femoral head. D. CT images taken two years later show a progression of osteonecrosis at the left femoral head (black arrowheads) with a subchondral fracture (white arrowheads).
Fig. 3. A 62-year-old male with osteonecrosis involving both femoral heads.
A. Radiograph shows type II ONFH on the right femoral head and a normal left femoral head. B. Digital tomosynthesis images show linear sclerosis at the left femoral head (arrowheads). Supplementary Video clip is available. C. CT images also show linear sclerosis at the left femoral head without collapse (arrowheads). D. T2-weighted fat suppressed MR images show the T2 double-line sign at the left femoral head, confirming type I ONFH (Association Research Circulation Osseous stage II). Type II ONFH is also observed at the right femoral head. ONFH = osteonecrosis of the femoral head
Fig. 4. A 36-year-old male with left groin pain.
A. Radiograph shows normal right and left femoral heads. B. Digital tomosynthesis images show subtle linear line at the right and left femoral heads (arrowheads). C. CT images show linear sclerosis involving both femoral heads without a subchondral fracture or collapse (arrowheads). D. T2-weighted MR images show a serpentine dark signal intensity line at both femoral heads, confirming type I osteonecrosis of the femoral head.
The interobserver and intraobserver agreements by modality and location are described in Tables 4 and 5, respectively. The interobserver agreement was moderate for radiography (right 0.56, left 0.57, and total 0.57) and excellent for DTS (right 0.84, left 0.88, and total 0.86). The intraobserver agreement for radiography was lower than that for DTS (total 0.69 vs. 0.96).
Table 4. Interobserver Agreement for Radiography and DTS.
| Modality and Location | Interobserver Agreement | |
|---|---|---|
| Radiography | ||
| Right | 0.56 (0.35–0.77) | |
| Left | 0.57 (0.38–0.77) | |
| Total | 0.57 (0.42–0.71) | |
| DTS | ||
| Right | 0.84 (0.69–0.99) | |
| Left | 0.88 (0.75–1.00) | |
| Total | 0.86 (0.76–0.96) | |
Values are Cohen's kappa with 95% confidence interval in parentheses. DTS = digital tomosynthesis
Table 5. Intraobserver Agreement for Radiography and DTS.
| Modality and Location | Intraobserver Agreement | |
|---|---|---|
| Radiography | ||
| Right | 0.60 (0.40–0.79) | |
| Left | 0.78 (0.62–0.93) | |
| Total | 0.69 (0.56–0.81) | |
| DTS | ||
| Right | 0.96 (0.89–1.00) | |
| Left | 0.96 (0.88–1.00) | |
| Total | 0.96 (0.91–1.00) | |
Values are Cohen's kappa with 95% confidence interval in parentheses. DTS = digital tomosynthesis
The radiation doses for radiography, DTS, and CT were calculated for 14 patients. Among the 14 participants, 10 underwent standard pelvic bone CT, and the other four underwent metal artifact reduction (MAR) CT due to the presence of a prosthetic device. For 10 patients without a prosthetic device, the mean effective doses ± SDs of the radiography, DTS, and CT were 1.35 ± 0.45 mSv, 1.38 ± 0.93 mSv, and 6.36 ± 2.94 mSv, respectively. For the four patients with prosthetic devices, the mean effective doses ± SDs for radiography, DTS and MAR CT were 1.45 ± 0.21 mSv, 1.45 ± 0.57 mSv, and 14.87 ± 0.34 mSv, respectively.
DISCUSSION
DTS is widely used in various imaging fields owing to its high in-plane resolution. For musculoskeletal studies, DTS is useful for analyzing high-contrast structures such as the bones [12]. DTS is superior to radiography for visualizing superimposed anatomical structures because multiple images from various angles are taken while the X-ray tube is swept within a specified range [17,22]. DTS is also beneficial for evaluating regions of interest that contain metallic implements [23].
In our study, DTS was superior to radiography for diagnosing ONFH when using CT as the reference standard. Concordance between the readers was better for DTS than for radiography, and the intraobserver agreement was also higher for DTS than radiography. Ottenin et al. [17] reported that DTS was superior to radiography for detecting fractures in patients with acute wrist trauma and showed a higher sensitivity than radiography; its specificity was comparable to that of radiography regardless of the involvement of the wrist bone. The interobserver kappa value in their study was higher for DTS than for radiography (0.66–0.69 vs. 0.54–0.59). Song et al. [24] evaluated the association of acromiohumeral distance detected with DTS with rotator cuff tears. They reported excellent interobserver and intraobserver agreements of DTS for assessing the acromiohumeral distance (ICC = 0.947–0.983, 0.975–0.987) and the diagnostic reproducibility of DTS.
Currently, the most commonly used systems for the classification of ONFH include those by Ficat and Arlet [25], Steinberg et al. [26], and Association Research Circulation Osseous (ARCO) [27]. We divided the participants with ONFH into type I and type II groups, and they had prevalence of 28% and 72%, respectively. In our study, type II ONFH was advanced, corresponding to Ficat and Arlet stage IIB-IV, Steinberg stage III-VI, or ARCO stage III-IV. For both readers, DTS had a higher sensitivity in diagnosing type I and type II ONFH than radiography, with statistical significance for one reader.
The diagnosis of type I ONFH based on radiography may have been more challenging because it represents an earlier stage of ONFH with only subtle changes such as osteoporosis or cystic changes. On the other hand, DTS provides a set of section planes from multiple projections obtained at various angles, allowing a more sensitive detection of changes that can be missed by radiography taken from a single plane. ONFH is a progressive disease that results in the collapse of the femoral head and destruction of the hip joint. Since it typically affects middle-aged patients who want to maintain high activity levels, it is appropriate to avoid or delay joint replacement as much as possible. Therefore, conservative treatment or reconstruction methods that preserve the femoral head are favored during the precollapse stage, while hip joint replacement surgery is performed in patients with advanced stages and collapsed femoral heads [28]. As shown in our study, DTS can detect minor radiological changes, which can help in the early diagnosis of ONFH and prevent patients from undergoing invasive procedures due to delayed diagnosis.
Regarding the radiation dose, the effective dose for DTS was comparable to that of radiography (AP pelvis and two lateral views of bilateral hip) and much less than that of CT (radiography vs. DTS vs. CT: 1.35 mSv vs. 1.38 mSv vs. 6.37 mSv). In a study by Koyama et al. [29], the effective dose for DTS in the anthropometric phantom hip joint was 0.82 mSv, approximately ten times higher than that of radiography (0.08 mSv). However, they only included the hip AP view radiograph in the calculation; in practice, additional views of the joint are taken depending on the clinical need. Göthlin and Geijer [20] studied hip prosthetic loosening; the effective dose for radiography (AP pelvis and hip cross-lateral view) was 1.1 mSv, and that for DTS was 0.9 mSv. Shim et al. [30] evaluated patients with sacroiliitis and reported that the effective dose for radiography (pelvis and two oblique AP images of bilateral SI joints) was 0.32 mSv and that for DTS was 0.4 mSv.
We used CT as a reference standard for the diagnosis of ONFH, and we acknowledge the limitation of our study in that regard. MRI is the best modality for diagnosing ONFH and has high sensitivity and specificity. However, the high cost and limited availability of MRI equipment restrict its utility as a routine screening tool. In addition, when we reviewed images of 15 patients who underwent pelvic MRI, there was no difference between the results of MRI and CT related to the presence or type of ONFH. Nevertheless, future studies using MRI or bone scintigraphy as reference standards are warranted.
In conclusion, DTS showed higher diagnostic performance and reproducibility than radiography in detecting ONFH. DTS may be used as a first-line diagnostic tool instead of radiography for patients suspected of having ONFH.
Acknowledgments
We thank Yun Jin Kim, Soorack Ryu in the Biostatistical Consulting and Research Lab, Hanyang University for assistance with statistical analysis.
Footnotes
Conflicts of Interest: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Seunghun Lee, Jeong Ah Ryu.
- Data curation: Seunghun Lee, Jeong Ah Ryu.
- Formal analysis: Yeo Ju Kim.
- Investigation: Yeesuk Kim, Jiyoon Bae.
- Methodology: Seunghun Lee, Jeong Ah Ryu.
- Software: Yeo Ju Kim.
- Supervision: Seunghun Lee.
- Validation: Yun Hwa Roh.
- Writing—original draft: Yun Hwa Roh.
- Writing—review & editing: Seunghun Lee, Yun Hwa Roh.
Supplement
The Supplement is available with this article at https://doi.org/10.3348/kjr.2021.0058.
DTS images of the patient are shown in Figure 3. Note the sclerotic line on the left femoral head.
References
- 1.Zalavras CG, Lieberman JR. Osteonecrosis of the femoral head: evaluation and treatment. J Am Acad Orthop Surg. 2014;22:455–464. doi: 10.5435/JAAOS-22-07-455. [DOI] [PubMed] [Google Scholar]
- 2.Murphey MD, Roberts CC, Bencardino JT, Appel M, Arnold E, Chang EY, et al. ACR appropriateness criteria osteonecrosis of the hip. J Am Coll Radiol. 2016;13:147–155. doi: 10.1016/j.jacr.2015.10.033. [DOI] [PubMed] [Google Scholar]
- 3.Murphey MD, Foreman KL, Klassen-Fischer MK, Fox MG, Chung EM, Kransdorf MJ. From the radiologic pathology archives imaging of osteonecrosis: radiologic-pathologic correlation. Radiographics. 2014;34:1003–1028. doi: 10.1148/rg.344140019. [DOI] [PubMed] [Google Scholar]
- 4.Mont MA, Marulanda GA, Jones LC, Saleh KJ, Gordon N, Hungerford DS, et al. Systematic analysis of classification systems for osteonecrosis of the femoral head. J Bone Joint Surg Am. 2006;88 Suppl 3:16–26. doi: 10.2106/JBJS.F.00457. [DOI] [PubMed] [Google Scholar]
- 5.Choi HR, Steinberg ME, Y Cheng E. Osteonecrosis of the femoral head: diagnosis and classification systems. Curr Rev Musculoskelet Med. 2015;8:210–220. doi: 10.1007/s12178-015-9278-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stevens K, Tao C, Lee SU, Salem N, Vandevenne J, Cheng C, et al. Subchondral fractures in osteonecrosis of the femoral head: comparison of radiography, CT, and MR imaging. AJR Am J Roentgenol. 2003;180:363–368. doi: 10.2214/ajr.180.2.1800363. [DOI] [PubMed] [Google Scholar]
- 7.Yeh LR, Chen CK, Huang YL, Pan HB, Yang CF. Diagnostic performance of MR imaging in the assessment of subchondral fractures in avascular necrosis of the femoral head. Skeletal Radiol. 2009;38:559–564. doi: 10.1007/s00256-009-0659-0. [DOI] [PubMed] [Google Scholar]
- 8.Markisz JA, Knowles RJ, Altchek DW, Schneider R, Whalen JP, Cahill PT. Segmental patterns of avascular necrosis of the femoral heads: early detection with MR imaging. Radiology. 1987;162:717–720. doi: 10.1148/radiology.162.3.3809485. [DOI] [PubMed] [Google Scholar]
- 9.Mitchell DG, Rao VM, Dalinka MK, Spritzer CE, Alavi A, Steinberg ME, et al. Femoral head avascular necrosis: correlation of MR imaging, radiographic staging, radionuclide imaging, and clinical findings. Radiology. 1987;162:709–715. doi: 10.1148/radiology.162.3.3809484. [DOI] [PubMed] [Google Scholar]
- 10.Dobbins JT, 3rd, Godfrey DJ. Digital x-ray tomosynthesis: current state of the art and clinical potential. Phys Med Biol. 2003;48:R65–R106. doi: 10.1088/0031-9155/48/19/r01. [DOI] [PubMed] [Google Scholar]
- 11.Machida H, Yuhara T, Tamura M, Ishikawa T, Tate E, Ueno E, et al. Whole-body clinical applications of digital tomosynthesis. Radiographics. 2016;36:735–750. doi: 10.1148/rg.2016150184. [DOI] [PubMed] [Google Scholar]
- 12.Blum A, Noël A, Regent D, Villani N, Gillet R, Gondim Teixeira P. Tomosynthesis in musculoskeletal pathology. Diagn Interv Imaging. 2018;99:423–441. doi: 10.1016/j.diii.2018.05.001. [DOI] [PubMed] [Google Scholar]
- 13.Lei J, Yang P, Zhang L, Wang Y, Yang K. Diagnostic accuracy of digital breast tomosynthesis versus digital mammography for benign and malignant lesions in breasts: a meta-analysis. Eur Radiol. 2014;24:595–602. doi: 10.1007/s00330-013-3012-x. [DOI] [PubMed] [Google Scholar]
- 14.Haas BM, Kalra V, Geisel J, Raghu M, Durand M, Philpotts LE. Comparison of tomosynthesis plus digital mammography and digital mammography alone for breast cancer screening. Radiology. 2013;269:694–700. doi: 10.1148/radiol.13130307. [DOI] [PubMed] [Google Scholar]
- 15.Chou SH, Kicska GA, Pipavath SN, Reddy GP. Digital tomosynthesis of the chest: current and emerging applications. Radiographics. 2014;34:359–372. doi: 10.1148/rg.342135057. [DOI] [PubMed] [Google Scholar]
- 16.Yoo JY, Chung MJ, Choi B, Jung HN, Koo JH, Bae YA, et al. Digital tomosynthesis for PNS evaluation: comparisons of patient exposure and image quality with plain radiography. Korean J Radiol. 2012;13:136–143. doi: 10.3348/kjr.2012.13.2.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ottenin MA, Jacquot A, Grospretre O, Noël A, Lecocq S, Louis M, et al. Evaluation of the diagnostic performance of tomosynthesis in fractures of the wrist. AJR Am J Roentgenol. 2012;198:180–186. doi: 10.2214/AJR.11.6374. [DOI] [PubMed] [Google Scholar]
- 18.Hayashi D, Xu L, Roemer FW, Hunter DJ, Li L, Katur AM, et al. Detection of osteophytes and subchondral cysts in the knee with use of tomosynthesis. Radiology. 2012;263:206–215. doi: 10.1148/radiol.12111649. [DOI] [PubMed] [Google Scholar]
- 19.Ha AS, Lee AY, Hippe DS, Chou SH, Chew FS. Digital tomosynthesis to evaluate fracture healing: prospective comparison with radiography and CT. AJR Am J Roentgenol. 2015;205:136–141. doi: 10.2214/AJR.14.13833. [DOI] [PubMed] [Google Scholar]
- 20.Göthlin JH, Geijer M. The utility of digital linear tomosynthesis imaging of total hip joint arthroplasty with suspicion of loosening: a prospective study in 40 patients. Biomed Res Int. 2013;2013:594631. doi: 10.1155/2013/594631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Christner JA, Kofler JM, McCollough CH. Estimating effective dose for CT using dose-length product compared with using organ doses: consequences of adopting International Commission on Radiological Protection publication 103 or dual-energy scanning. AJR Am J Roentgenol. 2010;194:881–889. doi: 10.2214/AJR.09.3462. [DOI] [PubMed] [Google Scholar]
- 22.Aoki T, Fujii M, Yamashita Y, Takahashi H, Oki H, Hayashida Y, et al. Tomosynthesis of the wrist and hand in patients with rheumatoid arthritis: comparison with radiography and MRI. AJR Am J Roentgenol. 2014;202:386–390. doi: 10.2214/AJR.12.10029. [DOI] [PubMed] [Google Scholar]
- 23.Gillet R, Teixeira P, Bonarelli C, Coudane H, Sirveaux F, Louis M, et al. Comparison of radiographs, tomosynthesis and CT with metal artifact reduction for the detection of hip prosthetic loosening. Eur Radiol. 2019;29:1258–1266. doi: 10.1007/s00330-018-5717-3. [DOI] [PubMed] [Google Scholar]
- 24.Song Y, Lee S, Lee BG, Joo YB, Song SY. The diagnostic reproducibility of tomosynthesis for the correlation between acromiohumeral distance and rotator cuff size or type. Korean J Radiol. 2018;19:417–424. doi: 10.3348/kjr.2018.19.3.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ficat RP. Idiopathic bone necrosis of the femoral head. Early diagnosis and treatment. J Bone Joint Surg Br. 1985;67:3–9. doi: 10.1302/0301-620X.67B1.3155745. [DOI] [PubMed] [Google Scholar]
- 26.Steinberg ME, Hayken GD, Steinberg DR. A quantitative system for staging avascular necrosis. J Bone Joint Surg Br. 1995;77:34–41. [PubMed] [Google Scholar]
- 27.Yoon BH, Mont MA, Koo KH, Chen CH, Cheng EY, Cui Q, et al. The 2019 revised version of association research circulation osseous staging system of osteonecrosis of the femoral head. J Arthroplasty. 2020;35:933–940. doi: 10.1016/j.arth.2019.11.029. [DOI] [PubMed] [Google Scholar]
- 28.Zhao D, Zhang F, Wang B, Liu B, Li L, Kim SY, et al. Guidelines for clinical diagnosis and treatment of osteonecrosis of the femoral head in adults (2019 version) J Orthop Translat. 2020;21:100–110. doi: 10.1016/j.jot.2019.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Koyama S, Aoyama T, Oda N, Yamauchi-Kawaura C. Radiation dose evaluation in tomosynthesis and C-arm cone-beam CT examinations with an anthropomorphic phantom. Med Phys. 2010;37:4298–4306. doi: 10.1118/1.3465045. [DOI] [PubMed] [Google Scholar]
- 30.Shim E, Ha T, Kim BH, Hong SJ, Kang CH, Jeon S, et al. Additive values of pelvic tomosynthesis in comparison to pelvic radiography alone for the diagnosis of sacroiliitis in patients with suspected axial spondyloarthritis. Skeletal Radiol. 2021;50:1197–1207. doi: 10.1007/s00256-020-03626-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
DTS images of the patient are shown in Figure 3. Note the sclerotic line on the left femoral head.