Abstract
Cerebral fat embolism is a rare and potentially fatal condition that may occur following a long bone fracture. Its characterized by respiratory, neurological, and mucocutaneous signs. Isolated severe brain syndrome remains exceptional. We report a 21-year-old male patient admitted for the cerebral manifestation of a fat embolism syndrome due to a fracture of long bone after a traffic accident injury. Neurological deterioration after a free interval was seen with generalized tonic-clonic seizures. MRI of the brain was indicated which showed numerous multifocal hyperintensities involving the deep white matter of both hemispheres producing a “starfield” appearance. This pattern of cytotoxic cerebral edema, with lesions in the white matter rather than the grey matter, is indicative of the subacute stage of fat embolism. The patient was treated with comprehensive support in the intensive care unit, he returned to normal neurological function and was discharged after 3 weeks of hospitalization.
Keywords: Cerebral fat embolism, MRI, long bone fracture
Introduction
Fat embolism syndrome is a rare and potentially lethal complication of long bone fractures.it occurs only in 0.9%-2.2% of long-bone fractures. Neurologic symptoms can be transient and widely variable. On magnetic resonance imaging (MRI), a cerebral fat embolism can demonstrate a “starfield” pattern due to the presence of multiple microemboli infarcts in the whole brain. We aimed to report a case of isolated cerebral fat embolism. Although this patient had severe neurological symptoms, the outcome was favorable.
Case presentation
A 20-year-old male fractured his right femur in a traffic injury (Fig. 1). Upon admission to our institution, the patient was well oriented, normotensive, and eupnoeic without a direct blow to his head. The bone fractures were firstly fixed. At 36 h post-trauma, the patient present a neurological deterioration with generalized tonic-clonic seizures. Glasgow coma score was 6, pupils were isocoric, isocyclic, and reactive. No lateralizing motor deficit was found. The patient was intubated and respiration was supported by mechanical ventilation. An initial CT of the head was unremarkable for intracranial abnormalities.
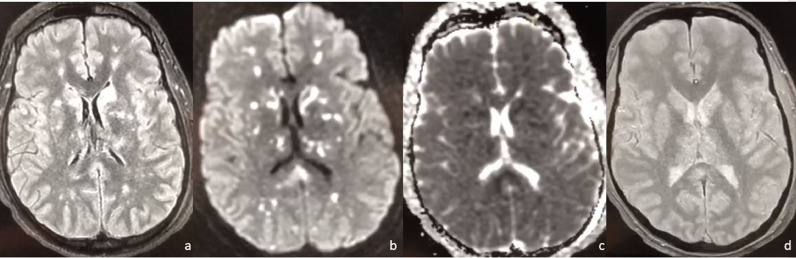
Fig. 1.
X-ray showed multi fragmented right femur fracture
Laboratory tests were normal. An echocardiogram showed normal ventricular function without any thrombus. Bilateral lower limb vascular color doppler ultrasound did not show any thrombus signs. Brain magnetic resonance imaging (MRI) demonstrated multiple hyperintense abnormalities on both T2-weighted images and diffusion in the cerebral white matter. However, there was not any micro bleeding on the susceptibility-weighted imaging sequences of brain MRI (Fig. 2). Combined with the patient's typical clinical manifestation and imaging studies, we diagnosed the patient with cerebral fat embolism syndrome. The patient was treated with methylprednisolone injection and low molecular weight heparin calcium, appropriate antibiotics, and dehydrating drugs. After 3 weeks of follow-up, the patients’ neurological symptoms and signs had disappeared.
Fig. 2.
Axial FLAIR (A) magnetic resonance imaging sequence shows the presence of numerous multifocal hyperintensities involving the deep white matter of both hemispheres (arrow), which correspond to multiple tiny foci of diffusion restrictions on DWI (B) with low signal on ADC map (C). These findings realize the “starfield” pattern suggestive of cerebral fat embolism syndrome. In the same patient, the T2* GRE (D) sequences appear relatively normal
Discussion
CFE is a fatal complication secondary to long bone fractures rarely observed in daily practice. Long bone fractures are recognized to be important risk factors for FES, especially femur fracture, followed by tibia fracture [1].
The present patient had a right multi fragmented femur fracture due to traffic injury.
After a long bone fracture, fat particles enter the systemic circulation, then enter the arterial system through pulmonary blood vessels and the heart. The fat particles then enter the brain, causing Cerebral fat embolism [2]. the pathological mechanisms of brain damage caused by fat particles mainly include microembolism, vasogenic edema, and microhemorrhage.
Most of the cerebral fat embolism was reported 24-72 hour after long bone fractures. In the present case, the clinical symptoms appeared 36 hour after the event.
Neurological symptoms can be transient and widely varied from diffuse encephalopathy to focal deficits [3].
The histopathological changes in adipose particles in brain tissue injury underlie the cerebral fat embolism imaging findings.
CT has limited value in the diagnosis of cerebral fat embolism. Previous studies have reported that cerebral fat embolism lesions are diffuse and multifocal because of the small embolized blood vessels, and so ahead CT is often negative [4].
Ct may be positive in the case of relatively high levels of bleeding with edema; however, in the case of our patient, no characteristic changes were detected in his head CT.
The MRI has a diagnostic value. In the acute phase, diffuse signal anomalies showed in the range of blurred or nodular contours of white matter in hyposignal in T1-weighted sequences, a hyper signal in T2-weighted sequences, and diffusion. These lesions correspond to pale infarctions producing a “starfield” appearance [5]. They are mainly located in the subcortical and periventricular white matter, corpus callosum, central gray nuclei, brain stem, and cerebellar hemispheres early on the onset of neurological manifestations. The evolution is towards the persistence of T2-weighted hypersignals of white matter related to demyelinating lesions or lacunae, partial resolution, or total resolution with the disappearance of the initial lesions. Cortical or cortico-subcortical atrophy may be observed in the longer term [6].
Our patient underwent a head MRI that revealed multiple abnormal signals in bilateral hemispheres. Those abnormal signals were high signals on T2WI, FLAIR, and DWI. This distribution was following the typical imaging findings of cerebral fat embolism previously reported in English literature.
The majority of reported cases found that cerebral dysfunction associated with fat cerebral embolism tends to be reversible [7].
The outcome of patients with fat cerebral embolism who receive supportive care is generally complete resolution of neurological lesions with a mortality of less than 10% [8].
The diagnosis of cerebral fat embolism is primarily clinical, MRI must be performed early, to confirm the diagnosis and evaluate the severity of the lesion.
Footnotes
Competing Interests: The authors declare that they have no conflict of interest.
Funding: This study was not funded.
References
- 1.Mueller F, Pfeifer C, Kinner B, Englert C, Nerlich M, Neumann C. Post-traumatic fulminant paradoxical fat embolism syndrome in conjunction with asymptomatic atrial septal defect: a case report and review of the literature. J Med Case Rep. 2011;5:142. doi: 10.1186/1752-1947-5-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Suh SI, Seol HY, Seo WK, Keun-Sik Hong, Sun U Kwon, et al. Cerebral fat embolism: susceptibility-weighted magnetic resonance imaging. Arch Neurol. 2009;66:1170. doi: 10.1001/archneurol.2009.173. [DOI] [PubMed] [Google Scholar]
- 3.Simon AD, Ulmer JL, Strottmann JM. Contrast-enhanced MR imaging of cerebral fat embolism: case report and review of the literature. AJNR Am J Neuroradiol. 2003;24:97–101. [PMC free article] [PubMed] [Google Scholar]
- 4.Wang Y, Si Z, Han J, Cao S. Imaging findings of cerebral fat embolism syndrome: a case report. J Int Med Res. 2020;48 doi: 10.1177/0300060520950559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rutman AM, Rapp EJ, Hippe DS, Baoanh BS, Mossa-Basha Mahmud MD, et al. T2*-weighted and diffusion magnetic resonance imaging differentiation of cerebral fat embolism from diffuse axonal injury. J Comput Assist Tomogr. 2017;41:877–883. doi: 10.1097/RCT.0000000000000635. [DOI] [PubMed] [Google Scholar]
- 6.Han YT, Tang J, Gao ZQ, et al. Clinical features and neuroimaging findings in patients with cerebral fat embolism. Chin Med J. 2016;129:874–876. doi: 10.4103/0366-6999.178963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tsai IT, Hsu CJ, Chen YH, Fong YC, Hsu HC, Tsai CH. Fat embolism syndrome in long bone fracture: clinical experience in a tertiary referral center in Taiwan. J Chin Med Assoc. 2010;73:407–410. doi: 10.1016/S1726-4901(10)70088-5. [DOI] [PubMed] [Google Scholar]
- 8.Duran L, Kayhan S, Kati C, Akdemir HU, Balci K, Yavuz Y. Cerebral fat embolism syndrome after long bone fracture due to gunshot injury. Indian J Crit Care Med. 2014;18:167–169. doi: 10.4103/0972-5229.128707. [DOI] [PMC free article] [PubMed] [Google Scholar]