Abstract
Iatrogenic non–thrombotic pulmonary embolism is a rare cause of pulmonary embolism. This case demonstrates the unusual imaging findings associated with pulmonary migration of Precipitating Hydrophobic Injectable Liquid, a liquid embolization material most commonly used in interventional neuroradiological procedures. Chest X-ray and CT Pulmonary Angiogram images are shown. The case highlights the importance of a thorough clinical history, including past medical history, when interpreting radiological studies.
Keywords: Iatrogenic, Pulmonary embolism, Interventional Neuroradiology
Introduction
Non–thrombotic pulmonary embolism (NTPE) can represent a significant diagnostic challenge due to its diverse clinical presentation and varied imaging features [1]. Radiology, in the form of chest X-ray and CT, are the mainstay of accurate and timely identification of this potentially fatal condition [2]. This case reports details an unusual case of iatrogenic NTPE with striking imaging features.
Clinical and radiological observations
A 36-year-old patient presented to the Emergency Department with a 3-day history of shortness of breath on exertion. They reported no chest pain, cough, hemoptysis, or fever. No risk factors for pulmonary embolism were identified. Full blood count, urea and electrolytes, and C-reactive protein were normal. An arterial blood gas demonstrated a mild metabolic acidosis. A chest X-ray was initially considered unremarkable (Fig. 1). Review of the patient's past medical history and drug history revealed they had commenced acetazolamide 2 weeks previously for intracranial hypertension and their breathlessness was diagnosed as a side effect of this medication. [3] However, given that breathlessness secondary to acetazolamide rarely requires hospital care in younger patients, a CT Pulmonary Angiogram (CTPA) was performed to rule out an alternative cause that was not clearly appreciable on the chest X-ray, such as early COVID-19. This CTPA showed high attenuation material scattered throughout the subsegmental pulmonary arteries of all lung lobes (Fig. 2, Figure 3). The initial detection of this high attenuation material was challenging due to the lack of a non–contrast CT phase, but appropriate windowing made its presence readily identifiable.
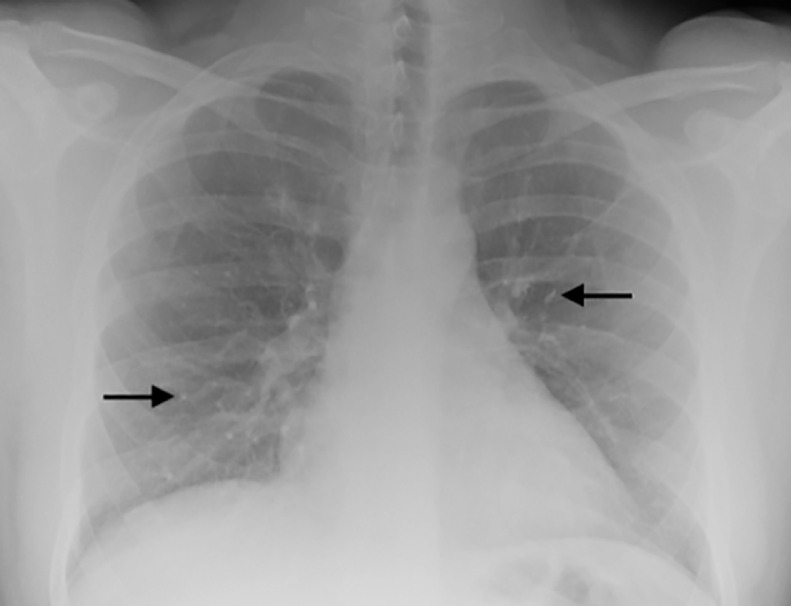
Fig. 1.
PA chest X-ray taken at time of patient's presentation. High attenuation foci, most notably within the right lower zone, were assumed to represent end-on vessels prior to the subsequent CTPA. Two example foci are highlighted by the black arrows.
Fig. 2.
Axial (A) and coronal (B) 30 mm maximum intensity projection slices from the patient's CTPA. The high attenuation embolic material is located in dependent areas. The patient's embolization had occurred with the patient in a supine position. It is likely the distribution of emboli is consistent with immediate migration of material to these locations while the patient remained supine, analogous to migration of vertebral body cement to anterior portions of the pulmonary vasculature in vertebroplasty. The example foci highlighted in Fig. 1 are circled on the coronal (B) image.
Figure 3.
Pulmonary artery reconstruction from the patient's CTPA showing high attenuation embolic material within dependent regions in all lung lobes.
On further review of the patient's past medical history, it was discovered they had undergone embolization of a dural arteriovenous fistula with Precipitating Hydrophobic Injectable Liquid (PHIL) (Micro Vention, CA) 4 months prior to presentation. An additional diagnosis of iatrogenic NTPE was subsequently made and the patient recovered after adjustment of their acetazolamide dose. It is believed the patient's iatrogenic NTPE may have exacerbated their acetazolamide-induced breathlessness. The patient has had no episodes of breathlessness since this presentation.
Discussion
NTPE encompasses embolization due to a wide spectrum of substances, from well-known biological materials such as amniotic fluid, fat, and septic emboli, to foreign bodies, talc, gas, cement, and glue [4]. PHIL is an established treatment option in interventional neuroradiology for the embolization of cerebral and spinal arteriovenous malformations and dural fistulae. It is also increasingly being used in body intervention [5]. Liquid embolic agents such as PHIL have several advantages over traditional coiling and particulate-based embolization techniques: they solidify when injected into the vasculature, providing a superior mould of their target area's geometry compared to coiling; the processes of solidification and occlusion are independent of the patient's physiology, allowing their use in patients with coagulopathies and patients receiving anti–coagulation treatment; and they are considered less likely to fragment and migrate than particulate-based embolic materials. Nevertheless, pulmonary migration remains a recognised but rare complication of embolization with liquid embolic materials [6]. PHIL is comprised of a polymer covalently bonded to an iodine compound (triiodophenol) [7] and so it appears radiopaque on X-ray and CT, presenting a diagnostic quandary if the patient's full past medical history is not known.
Conclusion
Iatrogenic NTPE is a rare condition, with chest X-ray and CTPA being crucial in its diagnosis [2]. This case highlights the possibility of NTPE following the use of liquid embolization material in distant parts of the body. It also demonstrates the importance of a thorough review of patients’ past medical history when interpreting unusual imaging findings.
Patient consent
The patient has provided written, informed consent for publication of their case. Original documents for verification of this statement can be provided upon reasonable request.
Footnotes
Competing Interests: The authors have no conflicts of interest to declare.
References
- 1.Jorens PG, Van Marck E, Snoeckx A, Parizel PM. Nonthrombotic pulmonary embolism. Eur Respir J. 2009;34(2):452–474. doi: 10.1183/09031936.00141708. [DOI] [PubMed] [Google Scholar]
- 2.McCabe BE, Veselis CA, Goykhman I, Hochhold J, Eisenberg D, Son H. Beyond pulmonary embolism; nonthrombotic pulmonary embolism as diagnostic challenges. Curr Probl Diagn Radiol. 2019;48(4):387–392. doi: 10.1067/j.cpradiol.2018.07.007. [DOI] [PubMed] [Google Scholar]
- 3.Venkatesha SL, Umamaheswara Rao GS. Metabolic acidosis and hyperventilation induced by acetazolamide in patients with central nervous system pathology. Anesthesiology. 2000;93(6):1546–1548. doi: 10.1097/00000542-200012000-00035. [DOI] [PubMed] [Google Scholar]
- 4.Bach AG, Restrepo CS, Abbas J, Villanueva A, Dus MJ, Schöpf R, et al. Imaging of nonthrombotic pulmonary embolism: biological materials, nonbiological materials, and foreign bodies. Eur Respir J. 2013;82(3):e120–e141. doi: 10.1016/j.ejrad.2012.09.019. [DOI] [PubMed] [Google Scholar]
- 5.Prashar A, Butt S, Shaida N. Introducing PHIL (precipitating hydrophobic injectable liquid) – a new embolic agent for the body interventional radiologist. Diagn Interv Radiol. 2020;26(2):140. doi: 10.5152/dir.2019.19063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lord J, Britton H, Spain SG, Lewis AL. Advancements in the development on new liquid embolic agents for use in therapeutic embolisation. J Mater Chem B. 2020;8(36):8207–8218. doi: 10.1039/d0tb01576h. [DOI] [PubMed] [Google Scholar]
- 7.Varadharajan S, Ramalingaiah AH, Saini J, Gupta AK, Devi BI, Acharya UV. Precipitating hydrophobic injectable liquid embolization of intracranial vascular shunts: initial experience and technical note. J Neurosurg. 2017;129(5):1217–1222. doi: 10.3171/2017.6.JNS16447. [DOI] [PubMed] [Google Scholar]