Abstract
Background:
There is no consensus on the preferred time to remove urethral catheter post caesarean section.
Aim:
To compare rate of significant bacteriuria and urinary retention following 8-h (study) and 24-h urethral catheter removal (control) post elective caesarean section.
Methods:
A randomized controlled trial of eligible participants that underwent elective caesarean section under spinal anaesthesia between March 2019 and November 2019 was conducted. Participants (150 in each arm) were randomly assigned (1:1 ratio) to either 8-h or 24-h group. Primary outcome measures included rates of significant bacteriuria 48-h post-operatively and acute urine retention 6-h post urethral catheter removal. Analysis was by Intention-to-treat. (www.pactr.org:PACTR202105874744483)
Results:
There were 150 participants randomized into each arm and data collection was complete. Significant bacteriuria was less in 8-h group (3% versus 6.0%; risk ratio (RR): 0.85 CI: 0.60 to 5.66; p = 0.274), though not significant. Acute urinary retention requiring repeat catheterisation was significantly higher in 8-h group (11(7.3%) versus 0(0.0%); RR: 0.07; CI: 0.87 to 0.97; p = 0.001). Mean time until first voiding was slightly higher in 8-h group (211.4 ± 14.3 min versus 190.0 ± 18.3 min; mean difference (MD): 21.36; CI: −24.36 to 67.08; p = 0.203); but patient in this group had a lower mean time until ambulation (770.0 ± 26.1 min versus 809 ± 26.2 min; MD: −38.8; CI: −111.6 to 34.0; p = 0.300). The 8-h group were significantly more satisfied (82/150 (54.7%) versus 54/150 (36.0%); p = 0.001)
Conclusions:
An 8-h group was associated with significant clinical satisfaction and acute urine retention compared to 24-h removal. The timing of urethral catheter removal did not affect rate of significant bacteriuria and other outcomes
Keywords: acute urine retention, caesarean section, hospital stay, post-operative satisfaction, urethral catheter removal
Introduction
caesarean delivery has some preventable morbidities, including micturition difficulties and urinary tract infections.1,2 The incidence of significant bacteriuria associated with indwelling catheterization has been estimated to be 3%–8% per day of urethral catheter in situ 3 with up to 85% of indwelling urethral catheters being colonized with bacteria within 48 h of use, which can lead to bacteriuria.1,4 The advocacy for elective caesarean delivery under spinal anaesthesia rather than general anaesthesia revolves around reduced morbidity and mortality risks associated with spinal anaesthesia. 5 - 7 Spinal anaesthesia may, however, affect the lower urinary tract innervation8,9 and leading to a delay in the time of first voiding and ultimately urinary retention with prevalence ranging from 0.05% to 14.1%, following vaginal delivery, and between 3.3% and 24.1% after caesarean delivery. 4
Zanfini et al. 8 showed that up to 80% of urinary bladder function is regained 8 h following spinal anaesthesia. This urodynamic study may portend a better safety profile for the 8-h group; however, this has not been popularized clinically. 8 Interventions like non-urethral catheterization,3,4 immediate removal, 7 2-h removal, 10 6-h removal,11,12 and 24-h removal1,7 after caesarean section are flawed with urine retention morbidity. Immediate or very early removal of urethral catheter may increase the risk of urine retention necessitating the need for recatheterization.4,10,12 There is currently no consensus on the specific time for removal of urinary catheter post caesarean section. 12 The more the duration of urethral catheter in the urinary bladder, the higher the significant bacteriuria rate and the less incidence of urinary retention following caesarean section under spinal anaesthesia.1,5,7,13,14 It is therefore necessary to find a balance in the duration of urethral catheterization, which will combine the advantage of reduced bacteriuria rate and lessen the incidence of urinary retention.
Removing the urethral catheter earlier may reduce the incidence of significant bacteriuria, encourage early ambulation, and may shorten the hospital stay post caesarean delivery.3,4,6,7,10 The policy of 8-h urethral catheter removal post surgery may encourage post-operative patients to get off the hospital bed and micturate by themselves, thus achieving early mobilization which discourages the formation of deep venous thrombosis. 10 There is lack of evidence on the use of 8-h urethral catheter removal post caesarean section. In addition, the peculiar findings of Zanfini et al on 8-h urethral catheter removal in which almost 80% of patients who had caesarean section under spinal anaesthesia achieving urinary bladder function has not been investigated clinically in randomized clinical trials.4,8 Based on our literature search, there is no randomized clinical trial, meta-analysis or systematic review on 8-h urethral catheter removal.
Furthermore, a previous systematic review by Li et al that involved 1084 pregnant women has argued that routine use of indwelling catheter for caesarean section in hemodynamically stable women is unnecessary and could be harmful, and they recommended more trials. 4
In addition, Abdel-Aleem et al in their Cochrane review of 16 studies involving 1065 women concluded that there is insufficient evidence to assess the routine use of indwelling bladder catheters in women undergoing caesarean section. They emphasized the need for more rigorous RCTs, with adequate sample sizes, standardized criteria for the diagnosis of UTI and other outcome measures. 15
This study compared the rate of significant bacteriuria, urine retention, mean time at first voiding, time until ambulation post elective caesarean section and the satisfaction following 8-h versus 24-h urethral catheter removal.
Methods
Study site
This randomized controlled trial was conducted at the Departments of Obstetrics, Gynaecology and Perinatology, and the Medical Microbiology of the Obafemi Awolowo University Teaching Hospitals Complex (OAUTHC), Ilé-Ife, Nigeria.
Study design
The study was a randomized controlled trial.
Study population
All eligible pregnant women slated for elective caesarean delivery under spinal anaesthesia were approached for consent and enrolment upon admission into the antenatal wards of both arms of the hospital after educating them on the purpose of the study. The study was conducted between March 2019 and November 2019.
Eligibility criteria
We recruited 300 consenting and eligible pregnant women slated for elective caesarean delivery under spinal anaesthesia for the study. The eligibility criteria were elective caesarean delivery between 34 weeks and 40 weeks, spinal anaesthesia and absence of pre-operative significant bacteriuria or UTI. Patients with intra-operative bladder injury and those that required conversion to general anaesthesia were excluded.
Primary outcome measures
The primary outcome measures included the rates of significant bacteriuria 48 h post-operatively and acute urine retention 6-h post urethral catheter removal. The secondary outcome measures were the mean time at first voiding post urethral catheter removal, mean time until ambulation post-operatively, the duration of hospital stay and satisfaction among participants.
Definition of terms
Significant bacteriuria was defined as the presence of at least 105 colony forming unit/mL of urine in a sample of mid-stream clean catch urine collected from the subjects pre-operatively or on day 2 post caesarean delivery following urine culture.1,16,17
Urinary tract infection. This was defined as the presence of significant bacteriuria with symptoms or signs that are not due to other identifiable causes, with at least one of the following: urinary frequency, urgency, fever, suprapubic tenderness, or costovertebral angle pain or tenderness.1,18
Postpartum urinary retention was defined as the inability to void 6 h after urethral catheter removal that will require recatheterization to obtain relief. 4
Time until first voiding was defined as the first micturition observed after urethral catheter removal in both groups.
Time until ambulation was defined as the first time of getting off hospital bed and taking a walk after completion of skin closure.
Length of hospital stay was defined as the period starting from the completion of skin incision to hospital discharge.
Satisfaction was defined as participant’s preference to have same timing of urethral catheter removal used for her if she is offered repeat surgery in her next delivery and/or participants that agreed to recommend the same timing of urethra catheter removal in her index delivery to a friend.
Sample size estimation
To identify an 80% reduction in significant bacteriuria following the two urethral catheter removal time using a 11.2% for 24-h-urethral removal group (based on previously published work by Onile et al. on a prospective randomized clinical trial of urethral catheter removal following elective caesarean section, 7 with a power of 80%, 150 women (agreeing a two-tailed alpha error of 0.05, 1:1 enrolment ratio and 10% attrition rate) would be required in each group.
Recruitment, randomization, allocation, concealment and blinding
This was a single blinded study. Blinding of the patients and the surgeons was not possible in this study, because the intervention (catheter removal) is an open one that is known to everybody. However, the outcome assessors and the medical laboratory scientist were not aware of the specific timing as the urine sample bottles were coded. Allocation concealment was, however, done.
Self-directed personnel who was not part of the study performed the randomization study by the random use of permutation blocks (blocks of 4, allocation ratio 1:1) with software accessible online at http://www.randomization.com. Concealment of allocation was done by means of consecutively numbered opaque wrapped papers in brown envelopes. The brown envelopes were stored and unsealed in the theatre room by an independent observer who was a staff of the hospital. Each of the brown envelope enclosed either a paper revealing a ‘Eight Hour group’ (EHR),” that is, the intervention consisted removal of urethral catheter 8 h post completion of skin closure post operatively or a paper revealing a “Twenty-four-hour group” (THR) in which urethral catheter was removed 24 h post completion of skin closure post operatively. In both groups, the obstetrician, the nurse or research assistants removed the urethral catheter at the designated time.
Study procedure
Urethral catheterization was performed on the theatre table after spinal anaesthesia had been administered to the participant. All other aspects of obstetrics were managed according to the standard practice of the hospital. Following delivery, the women and their babies were cared for according to the routine practice and early breastfeeding was encouraged. The participants were aware of which intervention that was administered to them, as the two intervention methods differed by timing of urethral catheter removal.
The catheter was removed at exactly 8 h after the last stitch of skin closure and 24 h after the last stitch of skin closure. The clean catch urine specimen (10 mL) was obtained from each participant by the 48th hour after the last stitch of skin closure. The urine samples were delivered to the Medical Microbiology laboratory without delay, while samples collected at night were refrigerated at 4°C till morning for assay. The fresh urine sample was macroscopically examined for its colour, turbidity, or cloudiness, while the microscopic examination of the urine sample assayed for the presence of pus cells, red blood cells, casts, epithelial cells and white blood cells per high power field.
The urine samples were cultured on CLED (Cysteine-Lactose-Electrolyte-Deficient) Agar, while the urine specimens that were not cultured within 2 h of submission were stored at 4°C. The agar plates were incubated at 37°C for 24 to 48 h; colony counts of 105 or more of pure isolates were considered as significant bacteriuria. Antibiotic susceptibility testing was done on colonies deemed to be significant. The caesarean deliveries were performed by either the Consultants or Senior Registrars as the lead Surgeon. The rest of the caesarean deliveries were completed as per standard protocol, following which the researcher or research assistant was informed immediately post-operative for randomization and data collection. Post-operatively, the vital signs were monitored closely and nil per oris was maintained until review.
All the participants in both groups received intravenous Cefuroxime 750 mg 8-hourly for 24 h post-operatively. Patients were encouraged to get off from bed once they regain sensation in their lower limbs. The 8-h group and 24-h groups had their urethral catheters removed 8 h and 24 h after the last stitch of skin closure. Patients were discharged on day 3 post-operatively across board based on institutional protocol. Those with significant bacteriuria were followed up for 10 days enquiring about urinary symptoms for the diagnosis of UTI.
Statistical analysis
Statistical analysis was done using the IBM SPSS package version 22 (Chicago, Illinois, USA). Tests of normality were done using Kolmogorov–Smirnov and Shapiro–Wilk Test. Risk ratios (RRs), mean difference, and 95% confidence intervals (CIs) were calculated. A p value of <0.05 was considered statistically significant. Analysis was by the ‘intention to treat’ principle.
Ethical consideration
Institution Research Approval was obtained from the Ethics and Research Board of the Institution (IRB/IEC/0004553). The trial was prospectively registered with National Postgraduate Medical College of Nigeria website (https://npmcn.edu.ng) for the purpose of Final fellowship Examination for the award of Fellow of the Medical College of Obstetrics and Gynaecology (FMCOG). I was, however, not aware of subsequent registration with WHO approved trial site; hence, the retrospective registration with the Pan African Clinical Trial Registry (www.pactr.org; PACTR202105874744483). However, all protocols and methodology remain the same during the dissertation defence and during this publication.
Results
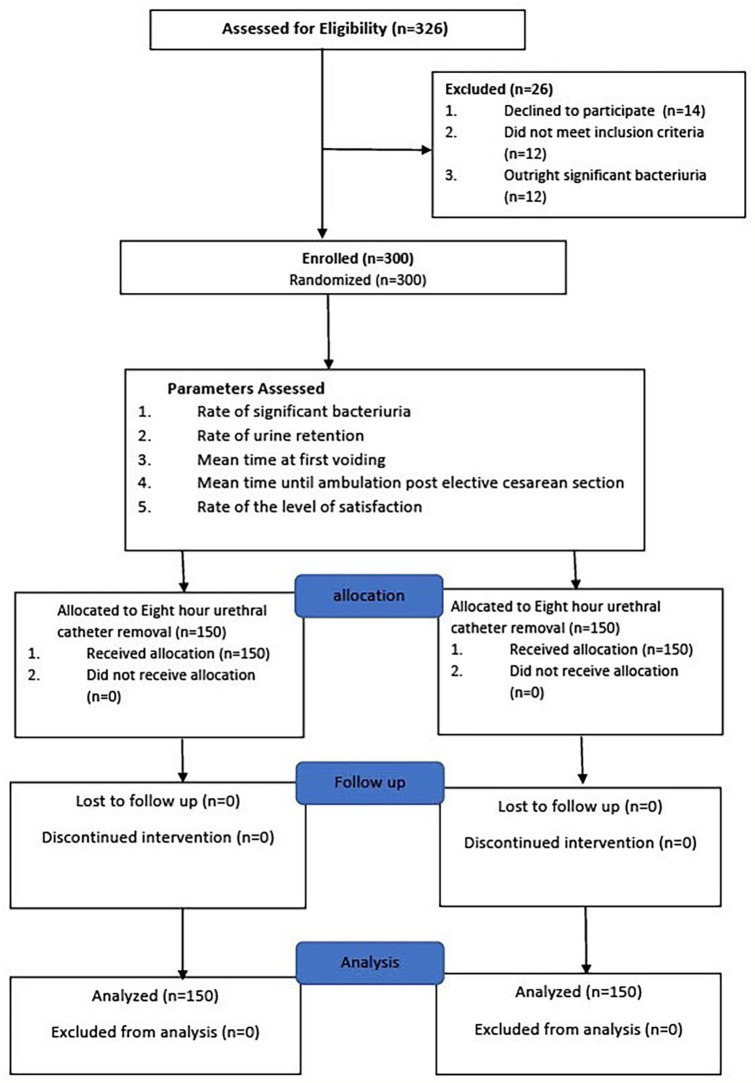
During the study period, among the 326 women who were screened for eligibility, 12 had outright significant bacteriuria and were excluded, while 14 declined participations, leaving 300 for study inclusion. A flow diagram depicting the participants flow through the study is shown in Figure 1. The demographic characteristics of the participants were as depicted in Table 1. The mean age, parity, and gestational age at delivery of both participants were similar (p = 0.38; 0.30; 0.10), respectively, as shown in Table 1.
Figure 1.
Participants’ flow chart.
Table 1.
Baseline demographic and clinical characteristics of the participants.
| Parameter | EHR (N = 150) frequency (%) | THR (N = 150) frequency (%) | p value |
|---|---|---|---|
| Maternal age (mean ± SD) | 31.79 ± 5.29 | 30.86 ± 4.63 | 0.38 |
| Maternal GA (mean ± SD) | 38.29 ± 1.61 | 37.84 ± 2.50 | 0.20 |
| Parity (mean ± SD) | 1.75 ± 1.24 | 1.71 ± 1.27 | 0.10 |
| Educational level | |||
| 1. None | 0 (0) | 5 (100.0) | 0.32 |
| 2. Primary | 1 (20.0) | 4 (80.0) | |
| 3. Secondary | 61 (56.5) | 47 (43.5) | |
| 4. Tertiary | 88 (48.4) | 94 (51.6) | |
| Satisfaction | |||
| Prefers same timing of catheter removal in Repeat surgery | |||
| 1. Yes | 82 (54.7) | 54 (36.0) | 0.001 |
| 2. No | 68 (45.3) | 96 (34.0) | |
| Will recommend same timing of catheter removal to friends | |||
| 1. Yes | 82 (54.7) | 54 (36.0) | 0.001 |
| 2. No | 68 (45.3) | 96 (34.0) | |
| Urethral catheter disturbed free movement in the ward | |||
| 1. Yes | 20 (13.3) | 85 (56.7) | 0.011 |
| 2. No | 130 (86.7) | 65 (43.3) | |
EHR: eight hour urethral catheter removal post surgery; THR: twenty four hour urethral catheter removal post surgery; GA: gestational age; SD: standard deviation.
More participants were significantly satisfied in the EHR group compared to the THR group (p < 0.05), while the educational attainment of both participants was similar (p > 0.05) as shown in Table 1.
There were no urinary frequency, urgency, fever, or dysuria; hence, no UTI was recorded among participants in this study. There were fewer participants who had significant bacteriuria in the 8-h group compared to the 24-h group (five women (3.3%) versus nine women (6.0%)); (RR: 0.85; 95% CI: 0.06 to 5.66). Participants with asymptomatic bacteriuria in this study were followed up with phone calls every 2 days for 10 days to report any symptom(s) of UTI. None of the women subsequently progressed from asymptomatic bacteriuria to the development of UTI.
There were 11(7.3%) participants that needed re-catheterization in the 8-h group due to urine retention, but none in the 24-h group (p = 0.001). The mean time until first voiding post urethral catheter removal was not significantly higher in the 8-h group compared to 24-h group (211.4 ± 14.3 min versus 190.0 ± 18.3 min; MD: 21.36; 95% CI: −24.36 to 67.08, p = 0.360). The mean time until ambulation post-operatively in the 8-h group was 770.0 ± 26.1 min compared to 809 ± 26.2 min in the 24-h group (MD: −38.8; 95% CI: −111.6 to 34.0, p = 0.300). The mean duration of hospital stay for the EHR group and THR group were similar (3.5 ± 0.6 days versus 3.5 ± 0.7 days, respectively) with no statistically significant difference in the mean duration of hospital stay for the two groups (MD: −0.03; 95% CI: −0.174 to 0.108, p = 0.640). The mean duration of caesarean delivery was similar in both groups (p = 0.667). All the caesarean deliveries were done under spinal anaesthesia and transverse lower uterine segment incision was made in all eligible participants (see Table 2).
Table 2.
Outcome measures of the pregnant women post urethral catheter removal/surgery.
| Parameter | 8-h (n = 150) | 24-h (n = 150) | RR (95% CI) | p value |
|---|---|---|---|---|
| Bacteriuria | ||||
| 1. Yes | 5(3.3) | 9 (6.0) | ||
| 2. No | 145 (96.7) | 141 (94.0) | 0.85 (0.60 to 5.66) | 0.274 |
| Urine retention | ||||
| 1. Yes | 11(7.3) | 0 (0.0) | ||
| 2. No | 139 (92.7) | 150.0 (100.0) | 0.07 (0.87 to 0.97) | 0.001 |
| Time until first voiding | 190.0 ± 18.3 min | 211.4 ± 14.3 min | a 21.36 (–24.36 to 67.08) | 0.360 |
| Time until ambulation | 770.0 ± 26.1 min | 809.1 ± 26.2 min | a −38.8 (–111.6 to 34.0) | 0.300 |
| Mean duration of hospital stay | 3.5 ± 0.6 days | 3.5 ± 0.7 days | a –0.03 (–0.174 to 0.108) | 0.640 |
| Duration of surgery | 86.0 ± 32.2 min | 84.4 ± 31.6 min | a 1.59 (–5.772 to 8.852) | 0.667 |
Values in this table are expressed as number (percentage) of women. SD: standard deviation; CI: confidence interval.
Mean difference (95% CI).
Sub-analysis of time until first voiding showed similar result in both groups when comparing on time per time voiding rate basis (p = 0.36), see Table 3.
Table 3.
Sub analysis of Time until first voiding after removal of urethral catheter post surgery.
| Time at first voiding post urethral catheter removal (min) | Number of patients | Total | t | ||
|---|---|---|---|---|---|
| n (%) | p value | ||||
| EHR | THR | df | |||
| <60 | 17 (11.3) | 21 (14.0) | 38 (12.7) | 0.919 | 298 |
| 60–179 | 52 (34.7) | 62 (41.3) | 114 (38.0) | 0.36 | |
| 180–359 | 53 (35.3) | 51 (34.0) | 104 (34.7) | ||
| ⩾360 | 28 (18.7) | 16 (10.7) | 44 (14.6) | ||
| Total | 150 (100.0) | 150 (100.0) | 300 (100.0) | ||
EHR: eight hour urethral catheter removal post surgery; THR: twenty four hour urethral catheter removal post surgery.
Discussion
This study revealed that both 8-h and 24-h urethral catheter removal post caesarean section performed under spinal anaesthesia had no detectable UTI. There was, however, non-statistically significant reduction in the incidence of significant bacteriuria among the 8-h group compared to the 24-h group. The morbidity of urinary retention in the 8-h group was, however, significantly higher compared to the 24-h group. This agreed with the urodynamic study by Zanfini et al. 8 who showed that up to 80% of bladder function are recovered by the 8th hour post spinal anaesthesia. This study showed 92.7% recovery with only 7.3% needing to be re-catheterized post surgery.
The participants that needed re-catheterization in this study was greater than figures reported by Chowdhury and Jahan, 3 where three women (4.61%) needed re-catheterization in the uncatheterized group and quite higher than figures quoted by Onile et al. 7 which was just one woman (1.2%) needing recatheterization in the immediate urethral removal group. Basbug et al. 10 reported fewer figures of 4.3% of women in a 2-h urethral catheter removal group and even lesser (1.3%) in their 12-h urethral catheter removal group. The rate found in this study was, however, far less than 44% reported by Kerr-Wilson and McNally 14 in the ‘in-out’ urethral catheter group, though Kerr-Wilson et al utilized epidural analgesia for their surgery, and such may not be strictly comparable to this study.
The rate of significant bacteriuria was lower than the findings by Onyegbule et al. 1 in Nnewi and Onile et al. 7 at Ile-Ife, both in Nigeria, in which nine (11.4%) and 10 (11.2%) respective participants had significant bacteriuria in the 24-h group. Considering the different timings for urethral catheter removal post caesarean section in literature, the incidence of significant bacteriuria 5(3.3 %) in our 8-h group was less than the findings of 8.0% in the 2-h urethral catheter removal group reported by Basbug et al. 10 and also less than the 8.1% found in the immediate urethral catheter removal group of the study by Onile et al. 7
Participants with symptomatic bacteriuria in this study were followed up with phone calls every 2 days for 10 days to obtain report of any symptom(s) of UTI. None of the followed-up participant subsequently progressed to UTI. The possible explanation for this finding may be that all the participants had no significant bacteriuria before the surgery and all had potent antibiotics after the surgery as routine surgical prophylaxis. Furthermore, the asymptomatic presentation of most catheter associated urinary tract infection (CAUTI) may be due to the presence of urethral catheter preventing exposure of the urethral mucosa to microorganisms in the infected urine. 1
The mean time until first voiding 190.0 ± 18.3 min in the 8-h group was similar to the findings (8–11 h) in the uncatheterized participants reported by Ghoreishi, 19 but higher than 6 ± 2 h in the uncatheterized group in a study by Chowdhury and Jahan. 3 A sub-analysis of the time until first voiding after removal of the urethral catheter demonstrated that upon removal of the urethral catheter by the eighth hour, only 17 (11.3%) of the participants in the 8-h arm were able to empty their urinary bladder.
We were not sure whether the delay in voiding upon removal of the urethral catheter in the 8-h arm in this study was due to a transient loss of bladder control following urethral catheterization as Zanfini in his study used immediate urethral catheter removal post surgery. It is possible that the effect of the spinal anaesthesia was still on the urinary bladder since up to 53 out of 150 (35.3%) voided by the 3rd hour post urethral catheter removal in the 8-h group (i.e. by the 12th hour post surgery). On a closer look, there appeared to be a similar hour-to-hour comparison with the 24-h group, especially by the 2nd to 4th hour post removal of urethral catheter in both groups (p = 0.36). We can therefore ask a stricter question, does the urethral catheter itself influence the time at voiding irrespective of the demonstrated spinal anaesthetic effect?
This significant difference in the need for re-catheterization in the 8-h group versus 24-h group calls for some concern in the removal of the urethral catheter post caesarean delivery before 24 h. It may suggest that the effect of spinal anaesthesia on the urinary bladder function may still be significantly inhibitory before 24 h post surgery. Although the participants had opioid analgesia with non-steroidal anti-inflammatory agents (NSAIDs) post-operatively, these may not have removed the post-operative pain entirely; hence, some pain effect on the urinary bladder can also contribute to urine retention. A combined spinal epidural (CSE) block, rather than spinal block alone, in these participants may further reduce the effect of pain on the urinary bladder in the immediate post-operative and thus reduce the incidence of re-catheterization among the EHR group.
The mean time until ambulation (770.0 ± 26.1 min for 8th hour versus 809.1 ± 26.2 min for 24-h group) was higher than findings by Onile et al. 7 who reported 8.72 ± 2.48 h for the immediate catheter removal group and 7.82 ± 1.85 h for the 24-h group. Of note, the authors of the study by Onile et al. used general anaesthesia in their study, which may have led to earlier recovery and thus earlier time at ambulation in the patients. 7 Haider et al. has shown that early removal of urethral catheter helps with better post-op recovery and early ambulation. 20 Participants were advised to assume supine positions for at least 6 h post operatively to avoid post-spinal headache, though some scholars believe that patient can get off the bed once they start moving their limbs. Our patients, however, assumed the 6-h supine position before mobilization, following which they were encouraged to get to the convenience whenever there is an urge to micturate post-urethral catheter removal. This may have affected the time at ambulation in this study. The use of bedpans was kept to the barest minimum in this study.
The mean duration of hospital stay was similar in both groups (3.5 ± 0.6 days for the 8 h group versus 3.5 ± 0.7 days for the 24 h group, RR: −0.03, 95% CI: −0.74 to 0.108) less than findings by Onyegbule et al. 1 where the mean length of hospital stay between the two groups were 7.18 ± 0.73 days and 7.01 ± 0.72 days, respectively; p > 0.05 and was less than the findings by Onile 6.91 ± 1.82 in the 24-h group and 6.82 ± 1.76 days in the test group. The discrepancy in the length of hospital stay may have followed the choice of sutures and technique of skin closure used in these studies. There is also the possibility that the hospital discharge policies were different across these medical centres. The choice of sutures and technique of skin closure were not stated by either Onyegbule et al. 1 study or Onile et al., 7 but subcuticular skin closure with absorbable sutures were used for all participants in this study, thereby eliminating the need of continued hospital stay until removal of stitches.
The presence or absence of urethral catheter post surgery seemed to have little impact on the length of hospital stay. Most participants were discharged on day 3 across board, as this is our institutional policy. Satisfaction was more in the 8-h group. This may follow ability of the participants to move freely around the wards without cause to drag along with them the urine bags due to earlier removal of their urethral catheters.
The strengths of the study was being a randomized controlled trial which utilized block sampling technique. Furthermore, significant bacteriuria was confirmed by medical microbiological identification using at least two coded specimen samples from the same individual. Blinding of the microbiologist was employed during assay of the urine specimen observing standard protocol and quality assurance. Skilled personnel (Senior registrars and Consultants) performed the caesarean section. The limitations of the study were that the present study was a single-centre-based study conducted in an urban, tertiary health facility, and may not be representative of what is obtainable in secondary health care, rural, and multi-centres. It was difficult blinding patients and clinicians in this study. Only elective caesarean deliveries were considered excluding emergencies due to difficulty with getting a ready urine culture result before the enrolment of such participants into the study. All participants had post-operative antibiotics as per standard; this may have affected the ddoverall urine testing for significant bacteriuria.
Participants receiving 8-h catheter removal have significant clinical satisfaction and acute urine retention compared to the 24-h group. The absence of UTI in both groups may have followed the routine use of potent antibiotics pre- and post-surgery. The rate of significant bacteriuria, mean time at first voiding, time at ambulation and the duration of hospital stay were not affected by the timing of urethral catheter removal in both groups. We recommend a multi-centre study design with a larger sample size in future trials and a sub-analysis of the participants who had need for re-catheterization. This sub-analysis may detect possible reason(s) for urine retention necessitating re-catheterization in this sub-group since all participants were exposed to the same spinal anaesthesia, technique of caesarean delivery and post-operative analgesia.
Supplemental Material
Supplemental material, sj-pdf-1-whe-10.1177_17455065211060637 for Eight-hour versus 24-h urethral catheter removal following elective caesarean section for reducing significant bacteriuria: A randomized controlled trial by Emeka Philip Igbodike, Ibraheem Olayemi Awowole, Olufemi O Kuti, Kayode Olusegun Ajenifuja, George Uchenna Eleje, Simeon Olugbade Olateju, Bolatito Opeyemi Olopade, Omotade Adebimpe Ijarotimi, Emmanuel Oladayo Irek, Njideka Theresa Igbodike, Oluwole Ekundayo Ayegbusi, Joseph Ifeanyichukwu Ikechebelu, Boniface Chukwuneme Okpala, Olabisi Morebisi Loto, Akintunde Olusegun Fehintola, Akinyosoye Deji Ajiboye, Olusola Fajobi, Chima Stephene Abuchi, Uchenna Uchenna Onwudiegwu, Olusola Benjamin Fasubaa, Ernest Okechukwu Orji, Olufemiwa Niyi Makinde, Alexander Tuesday Owolabi and Adebanjo Babalola Adeyemi in Women’s Health
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (https://creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-sav-1-whe-10.1177_17455065211060637 for Eight-hour versus 24-h urethral catheter removal following elective caesarean section for reducing significant bacteriuria: A randomized controlled trial by Emeka Philip Igbodike, Ibraheem Olayemi Awowole, Olufemi O Kuti, Kayode Olusegun Ajenifuja, George Uchenna Eleje, Simeon Olugbade Olateju, Bolatito Opeyemi Olopade, Omotade Adebimpe Ijarotimi, Emmanuel Oladayo Irek, Njideka Theresa Igbodike, Oluwole Ekundayo Ayegbusi, Joseph Ifeanyichukwu Ikechebelu, Boniface Chukwuneme Okpala, Olabisi Morebisi Loto, Akintunde Olusegun Fehintola, Akinyosoye Deji Ajiboye, Olusola Fajobi, Chima Stephene Abuchi, Uchenna Uchenna Onwudiegwu, Olusola Benjamin Fasubaa, Ernest Okechukwu Orji, Olufemiwa Niyi Makinde, Alexander Tuesday Owolabi and Adebanjo Babalola Adeyemi in Women’s Health
Acknowledgments
The index work involved colleagues who work in the Department of Obstetrics and Gynaecology Obafemi Awolowo University Teaching Hospitals Complex Ile Ife, Department of Anaesthesia, Obafemi Awolowo University Teaching Hospitals Complex Ile Ife Department of Obstetrics and Gynaecology Obafemi Awolowo University Teaching Hospitals Complex Ile Ife; Department of Medical Microbiology and Parasitology, Obafemi Awolowo University Teaching Hospitals Complex Ile Ife; Department of Community Medicine, Obafemi Awolowo University Teaching Hospitals Complex Ile Ife; and the Effective Care Research Unit, Ophthalmology and Department of Obstetrics and Gynaecology, Nnamdi Azikiwe University, Awka (Nnewi Campus), who kindly participated in the case management and patient follow-up. Many thanks to all who shared and helped to put this work in its final form.
Footnotes
Authors’ contributions: E.P.I. contributed to the project development, data collection manuscript writing, data analysis and manuscript writing/editing. I.O.A., G.U.E., B.C.O., N.T.I. and O.E.A. contributed to manuscript writing/editing, analysis and revision. S.O.O., B.O.O., E.O.I., O.F., A.F., O.A.I., A.D.A., A.C.S., K.O.A., O.K., M.L., J.I.I., U.O., O.B.F., E.O.O., O.N.M., A.T.O. and A.B.A. contributed to analysis, revision and manuscript writing.
All authors contributed to data analysis, drafting or revising the article; gave final approval of the version to be published and agree to be accountable for all aspects of the work.
Additional declarations for articles in life science journals that report the results of studies involving humans and/or animals.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
Ethics approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Bioethics and Research committee of the Obafemi Awolowo University Teaching Hospitals Complex, Ile-Ife with International Code: IRB/IEC/0004553. The study protocol was approved by the hospital ethics committee.
Consent to participate: A written informed consent was obtained from all individual participants included in the study.
Consent for publication: All the participants gave consent for publication.
ORCID iD: Emeka Philip Igbodike  https://orcid.org/0000-0003-4698-6226
https://orcid.org/0000-0003-4698-6226
Availability of data and material: The raw data will be uploaded in SPSS format upon request
Code availability: Statistical Product and Service Solution version 22 was used for all analysis.
Supplemental material: Supplemental material for this article is available online.
References
- 1. Onyegbule OA, Udigwe GO, Ezebialu I, et al. Catheter-associated urinary tract infection following caesarean section in Nnewi, Nigeria: a prospective comparative study. Br Microbiol Res J 2014; 4(9): 1025–1034. [Google Scholar]
- 2. Ajenifuja KO, Oyetunji IO, Orji EO, et al. Postpartum urinary retention in a teaching hospital in southwestern Nigeria. Gynaecol Obstet Res 2013; 39(8): 1308–1313. [DOI] [PubMed] [Google Scholar]
- 3. Chowdhury L, Jahan I. Cesarean section without urethral catheterization. J Armed Forces Med Coll Bangladesh 2016; 11(1): 3–6. [Google Scholar]
- 4. Li L, Wen J, Wang L, et al. Is routine indwelling catheterisation of the bladder for Caesarean section necessary? A systematic review. BJOG 2011; 118(4): 400–409. [DOI] [PubMed] [Google Scholar]
- 5. Meddings J, Rogers MA, Krein SL, et al. Reducing unnecessary urinary catheter use and other strategies to prevent catheter-associated urinary tract infection: an integrative review. BMJ Qual Saf 2013; 23(4): 277–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Karem Ali Hamad Al, Huri A-A. Caesarean section without using bladder catheterization is safe in uncomplicated patients. J Gynecol Obstet 2017; 5(5): 6–59. [Google Scholar]
- 7. Onile T, Kuti O, Orji EO, et al. A prospective randomized clinical trial of urethral catheter removal following elective cesarean delivery. Int J Gynaecol Obstet 2008; 102(3): 267–270. [DOI] [PubMed] [Google Scholar]
- 8. Zanfini BA, Paradisi G, Savone R, et al. Bladder function after spinal anesthesia for cesarean section: an urodynamic evaluation. Eur Rev Med Pharmacol Sci 2012; 16(11): 1525–1529. [PubMed] [Google Scholar]
- 9. Kamphuis ET, Ionescu TI, Kuipers PW, et al. Recovery of storage and emptying functions of the urinary bladder after spinal anesthesia with lidocaine and with bupivacaine in men. Anesthesiology 1998; 88(2): 310–316. [DOI] [PubMed] [Google Scholar]
- 10. Basbug A, Yuksel A, Ellibeş Kaya A. Early versus delayed removal of indwelling catheters in patients after elective cesarean section: a prospective randomized trial. J Matern Fetal Neonatal Med 2018; 33: 68–72. [DOI] [PubMed] [Google Scholar]
- 11. Yaghmaei M, Mokhtari M, Tamizi A, et al. Comparing the outcomes of urinary catheter removal 6 hour and 12 to 24 hours after cesarean delivery. Iran J Obstet Gynecol Infert 2017; 20(9): 1–7. [Google Scholar]
- 12. Menshawy A, Ghanem E, Menshawy E, et al. Early versus delayed removal of indwelling urinary catheter after elective Caesarean delivery: systematic review and meta-analysis of randomized controlled trials. J Matern Fetal Neonatal Med 2019; 33(16): 2818–2825. [DOI] [PubMed] [Google Scholar]
- 13. Taiwo S, Aderounmu A. Catheter associated urinary tract infection: aetiologic agents and antimicrobial susceptibility pattern in Ladoke Akintola University Teaching Hospital, Osogbo, Nigeria. Afr J Biomed Res 2006; 9(3): 141–148. [Google Scholar]
- 14. Kerr-Wilson RH, McNally S. Bladder drainage for caesarean section under epidural analgesia. Br J Obstet Gynaecol 1986; 93(1): 28–30. [DOI] [PubMed] [Google Scholar]
- 15. Abdel-Aleem H, Fathallah Aboelnasr M, Jayousi TM, et al. Indwelling bladder catheterisation as part of intraoperative and postoperative care for caesarean section. Cochrane Database Syst Rev 2014; 4: CD010322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Onu FA, Ajah LO, Ezeonu PO, et al. Profile and microbiological isolates of asymptomatic bacteriuria among pregnant women in Abakaliki, Nigeria. Infect Drug Resist 2015; 8: 231–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Tosin OJ, Mathew AO, Bello FJ, et al. Asymptomatic Bacteriuria among antenatal Women Attending private Hospital in Lagos, Nigeria. Sch J App Med Sci 2014; 2(6D): 3076–3080. [Google Scholar]
- 18. Czajkowski K, Broś-Konopielko M, Teliga-Czajkowska J. Urinary tract infection in women. Prz Menopauzalny 2021; 20(1): 40–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ghoreishi J. Indwelling urinary catheters in cesarean delivery. Int J Gynaecol Obstet 2003; 83(3): 267–270. [DOI] [PubMed] [Google Scholar]
- 20. Haider MZ, Annamaraju P. Bladder catheterization (updated 12 August 2021). Treasure Island, FL: StatPearls Publishing, January 2021, https://www.ncbi.nlm.nih.gov/books/NBK560748/ [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-whe-10.1177_17455065211060637 for Eight-hour versus 24-h urethral catheter removal following elective caesarean section for reducing significant bacteriuria: A randomized controlled trial by Emeka Philip Igbodike, Ibraheem Olayemi Awowole, Olufemi O Kuti, Kayode Olusegun Ajenifuja, George Uchenna Eleje, Simeon Olugbade Olateju, Bolatito Opeyemi Olopade, Omotade Adebimpe Ijarotimi, Emmanuel Oladayo Irek, Njideka Theresa Igbodike, Oluwole Ekundayo Ayegbusi, Joseph Ifeanyichukwu Ikechebelu, Boniface Chukwuneme Okpala, Olabisi Morebisi Loto, Akintunde Olusegun Fehintola, Akinyosoye Deji Ajiboye, Olusola Fajobi, Chima Stephene Abuchi, Uchenna Uchenna Onwudiegwu, Olusola Benjamin Fasubaa, Ernest Okechukwu Orji, Olufemiwa Niyi Makinde, Alexander Tuesday Owolabi and Adebanjo Babalola Adeyemi in Women’s Health
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (https://creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-sav-1-whe-10.1177_17455065211060637 for Eight-hour versus 24-h urethral catheter removal following elective caesarean section for reducing significant bacteriuria: A randomized controlled trial by Emeka Philip Igbodike, Ibraheem Olayemi Awowole, Olufemi O Kuti, Kayode Olusegun Ajenifuja, George Uchenna Eleje, Simeon Olugbade Olateju, Bolatito Opeyemi Olopade, Omotade Adebimpe Ijarotimi, Emmanuel Oladayo Irek, Njideka Theresa Igbodike, Oluwole Ekundayo Ayegbusi, Joseph Ifeanyichukwu Ikechebelu, Boniface Chukwuneme Okpala, Olabisi Morebisi Loto, Akintunde Olusegun Fehintola, Akinyosoye Deji Ajiboye, Olusola Fajobi, Chima Stephene Abuchi, Uchenna Uchenna Onwudiegwu, Olusola Benjamin Fasubaa, Ernest Okechukwu Orji, Olufemiwa Niyi Makinde, Alexander Tuesday Owolabi and Adebanjo Babalola Adeyemi in Women’s Health