Abstract
Background.
Electroconvulsive therapy (ECT) is highly effective for treatment-resistant depression (TRD), and previous studies have demonstrated short-term improvements in quality of life (QoL) after ECT. However, long-term QoL after ECT has not been studied, and the baseline patient characteristics that predict long-term QoL remain unknown.
Methods.
Seventy-nine subjects with unipolar or bipolar TRD were enrolled in this prospective longitudinal observational study. Physical, psychological, social, and environmental QoL domains were measured with the abbreviated World Health Organization Quality of Life scale (WHOQOL-BREF) at baseline and every 6 months for up to 2 years after ECT. Baseline sociodemographic and clinical features were tested for association with long-term QoL.
Results.
Long-term follow-up data were available from 49 participants. Relative to baseline, average psychological and physical QoL improved during the follow-up period (Hedges’ effect size: 0.27–0.83). About 40–50% of individuals experienced clinically meaningful improvement. Subjects with better initial antidepressant response with ECT reported better QoL over the subsequent two years. Long-term QoL improved most among individuals who were married, those without disability status, and those with psychotic features or shorter depressive episodes at baseline.
Limitations.
Participants were from a single US academic center and mainly of European ancestry, so findings may not generalize to other settings or ethnicities. The observational design does not allow causal inferences.
Conclusions.
Long-term psychological and physical QoL outcomes vary widely after ECT. Individuals with the best outcomes are those who respond well to ECT initially, married people, and those with a less chronic course of illness.
Keywords: Treatment-Resistant Depression, Quality of life, long-term (24months) Quality of Life, predictors for quality of life, Electroconvulsive Therapy, Minimum Clinically Important Difference
Introduction
Depressive disorders are the single largest contributor to non-fatal health loss globally, as measured by years lost to disability (WHO, Disease Burden, 2017). Although currently available psychosocial and pharmacological treatments are effective for the majority of individuals, many patients develop treatment resistant depression (TRD), which does not respond to these first-line therapies. For example, 33% of participants in the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study did not recover after a series of up to four antidepressant trials (Rush et al., 2006). In addition, long-term outcomes of TRD are typically poor. A systematic review reported that TRD is associated with poor social function, persistent symptoms, increased mortality, and a recovery rate of less than 40% over 10 years (Fekadu et al., 2009).
Traditionally studies of TRD have focused on the severity of depressive symptoms as the primary clinical outcome of interest, but recent studies have emphasized the importance of quality of life (QoL). Measuring QoL is an essential component for clinical trials in mental illness as the assessment takes into account patients’ rights, autonomy, and opinions (Barneveld et al., 2014; Mas-Expósito et al., 2011; Oliveira et al., 2016; Rubio et al., 2014). Reviews of health-related QoL have highlighted the profound effects that TRD has on physical, psychological, and social functioning, as well as life satisfaction and well-being (Johnston et al., 2019; Rosenquist et al., 2006). We recently reported that persons with TRD had profound impairments in physical and psychological QoL as measured with the abbreviated World Health Organization Quality of Life instrument (WHOQOL-BREF, (Lex et al., 2019)). Furthermore, we found that QoL domain scores were not strongly associated with traditional measures of depressive symptoms or functional impairment, suggesting that QoL should be understood as a distinct outcome for individuals with TRD (Lex et al., 2019).
Patients with severe TRD often consider electroconvulsive therapy (ECT), which is effective for about two-thirds of depressed patients (Haq et al., 2015). Antunes and Fleck used the WHOQOL-BREF to investigate the immediate effects of ECT on a cohort of psychiatric inpatients, many of whom had TRD, and found improvements across QoL domains (Antunes & Fleck, 2009). A recent meta-analysis of studies that used the Medical Outcomes Study Short Form 36 (SF-36) to measure health-related QoL showed similar improvements across multiple domains immediately following the ECT series (Giacobbe et al., 2018). Thus, cross-sectional studies have clearly revealed the severe impact of TRD on QoL, and short-term studies have demonstrated marked improvements in QoL immediately following ECT.
In contrast to short-term outcomes, less is known about QoL trajectories beyond 6 months among persons with TRD. An analysis of data from the STAR*D trial showed that 68% of participants who did not reach remission (i.e., those with TRD) experienced “severely impaired” QoL at 1-year follow-up, compared to 13% of subjects who reached remission (IsHak et al., 2015). Similarly, a study of depressed subjects treated naturalistically with antidepressant medication found poorer health-related QoL at 1–2 years among participants with more persistent depressive symptoms (Saragoussi et al., 2018). To our knowledge, no published studies have reported long-term QoL outcomes among TRD patients after ECT.
The current study had two objectives. First, we aimed to describe physical, psychological, social, and environmental QoL outcomes for a TRD cohort over the 2-year period following an index ECT series. We hypothesized that psychological and physical QoL would be superior for those with a better acute response to ECT. Second, we aimed to identify baseline patient characteristics that predicted long-term QoL outcomes. Robust individual-level predictors would be clinically useful for patients and clinicians considering ECT and the prospect for long-term improvements in QoL following this intervention.
Materials and Methods
Study design
The Michigan Biomarkers for Refractory Depression (Bluebird) study was conducted at the University of Michigan, Ann Arbor, between 2011 and 2016. The study was approved by the University of Michigan Institutional Review Board. All subjects provided written informed consent. Baseline QoL data from 79 subjects were previously reported (Lex et al., 2019). One subject did not proceed to ECT for logistical reasons and is excluded from this analysis. Here we describe longitudinal QoL outcomes for the 78 subjects who received at least one ECT treatment, focusing on the 49 participants who provided follow-up QoL data.
The longitudinal study design has been described in detail (Mickey et al., 2018). Briefly, participants were recruited from adult inpatients and outpatients who were referred to the ECT Program at the University of Michigan. Eligible participants had a medication-resistant, moderate-to-severe depressive episode (DSM-IV/5 major depressive disorder or bipolar disorder) for at least 2 months. Medication resistance was defined by failure of at least one medication trial of adequate dose and duration within the current episode; all participants had a lifetime history of multiple medication failures. Following the baseline assessment, ECT was delivered as clinically indicated. Clinical response to ECT was characterized with the Clinical Global Impression - Improvement (CGI-I) scale (Guy, 1976). Follow-up assessments were conducted by mail using paper questionnaires 6, 12, 18, and 24 months (± 1 month) after the start of the ECT index series.
Quality of life instrument
The WHOQOL-BREF scale (WHOQOL Group, 1998) is a self-report questionnaire that assesses four QoL domains: physical, psychological, social relationships, and environmental. The WHOQOL-BREF is an internationally normed, cross-culturally validated, multilingual instrument. Skevington and colleagues demonstrated good-to-excellent psychometric properties of the WHOQOL-BREF in a large sample of healthy individuals and those with physical and mental illnesses (Skevington et al., 2004). Each domain may be scored using a 4–20 scale or a 0–100 scale; higher values represent a better QoL. In this paper we use the 0–100 scale, which may be obtained from the 4–20 scale using the following formula: (x–4) / 0.16. The questionnaire also includes two items on overall QoL and satisfaction with health (range 1–5).
The minimum clinically important difference (MCID) in a clinical scale represents the smallest change that is considered meaningful for the patient. Although statistically significant changes may occur after an intervention, such changes may have little clinical significance (Cook, 2008). No consensus yet exists regarding MCIDs for the WHOQOL-BREF domains, so we sought a working estimate to aid interpretation of our results. A systematic review of health-related QoL measures found that the MCID usually falls near 0.5 standard deviation (SD) (Norman et al., 2003). Based on normative values of the SD for the WHOQOL-BREF (Skevington et al., 2004) the 0.5-SD rule results in MCID estimates of 9, 9, 10, and 8 for physical, psychological, social, and environmental domains (using the 0–100 scale). Similarly, based on our previously reported SD values for the current sample of TRD patients (Lex et al., 2019), MCIDs would be 7, 7, 10, and 8, respectively. A recent study of the WHOQOL-BREF used two methods to estimate MCIDs in lung cancer patients (de Mol et al., 2018). A conservative method yielded estimates of 13, 12, 17, and 11, while the 0.5-SD method yielded estimates of 10, 8, 8, and 7, respectively. Based on all of these considerations, we adopted 10 points as a simple MCID estimate for each domain.
Data analysis
The data was analyzed using SPSS version 25.0 (Everitt et al., 2004) and R statistical software (version 3.2.4, R Core Team, 2019). Demographic data were presented in frequency tables and differences were calculated with chi-square tests for categorical data and t-tests for continuous data. Follow-up data were compared with baseline data using paired t-tests and linear mixed models (“lme4” package, version 1.1–12, “lmer” function, (Bates et al., 2015). Linear mixed models were also used to test baseline sociodemographic variables as predictors of long-term QoL. The outcome variable of each model was QoL score (physical, psychological, social, or environmental) and subject intercept was the random effect. As fixed-effect predictors, we entered terms for QoL score at baseline, acute ECT response, and the predictor of interest. P-values were obtained from fitted models using Wald χ2 tests (“car” package, version 2.1–2, “Anova” function, (Fox and Weisberg, 2019).
To characterize the type and intensity of treatment received during follow-up, questionnaires were used to gather information on the treatments that had been used during the most recent 6-month interval. Data was summarized into four categories: number of psychotherapy visits; total number of medication trials; number of medication trials that were adequate in dose and duration; and use of ECT. Medication trials were classified as adequate or inadequate using the Antidepressant Treatment History Form - Short Form (Sackeim et al, 2019). Averages of the number of psychotherapy visits, total number of medication trials, and number of adequate medication trials were calculated across time for each subject. Use of ECT at any time during follow-up was coded as a binary variable. To examine whether treatment intensity was associated with longitudinal QoL outcomes after ECT, we used linear mixed models with subject intercept as the random effect. Fixed-effect predictors were baseline QoL score, acute ECT response, average number of psychotherapy visits, average number of medication trials, average number of adequate medication trials, and use of ECT during follow-up.
Results
Participant characteristics
Of 78 subjects with baseline QoL data, 29 were lost to follow-up. To examine whether subjects who dropped out differed systematically from those with follow-up data, we compared the two groups on demographic characteristics and baseline clinical features. Baseline QoL scores were similar between the two groups (all p > 0.05, two-sample t tests). Participants with follow-up data were more likely to receive a diagnosis of specific phobia at baseline (p = 0.01, Fisher exact test). Otherwise, the 49 participants with at least one follow-up assessment did not differ from those lost to follow-up (all p > 0.05, Tables 1 and S1), suggesting that the 49 subjects with follow-up data were representative of the entire sample (details in Supplemental Results).
Table 1:
Baseline sociodemographic characteristics for participants with and without follow-up quality of life measures
| With Follow-up | Without Follow-up | All | |
|---|---|---|---|
| (n = 49) | (n = 29) | (n = 78) | |
| Female | 35 | 15 | 50 |
| Age, mean | 48.46 | 50.71 | 49.30 |
| Age, SD | 15.19 | 14.46 | 14.87 |
| Marital Status | |||
| divorced | 12 | 1 | 13 |
| married | 19 | 15 | 34 |
| single | 12 | 6 | 18 |
| unmarried partners | 3 | 3 | 6 |
| widowed | 2 | 4 | 6 |
| other | 1 | 0 | 1 |
| Annual Household Income a | |||
| less than $25,000 | 13 | 11 | 24 |
| $25,000 – 50,000 | 13 | 7 | 20 |
| $50,001 – 75,000 | 9 | 5 | 14 |
| more than $75,000 | 12 | 5 | 17 |
| Years of Education, mean | 15.92 | 15.41 | 15.73 |
| Years of Education, SD | 3.09 | 2.56 | 2.90 |
| Self-reported Race | |||
| white or Caucasian | 46 | 27 | 73 |
| Asian | 1 | 0 | 1 |
| black or African American | 1 | 1 | 2 |
| other | 1 | 1 | 2 |
| Employment Status | |||
| disability | 20 | 14 | 34 |
| full-time | 4 | 3 | 7 |
| not employed | 9 | 3 | 12 |
| part-time | 5 | 0 | 5 |
| retired | 6 | 7 | 13 |
| student or homemaker | 5 | 2 | 7 |
3 missing values
p > 0.05 for all group comparisons
Longitudinal change in QoL after ECT
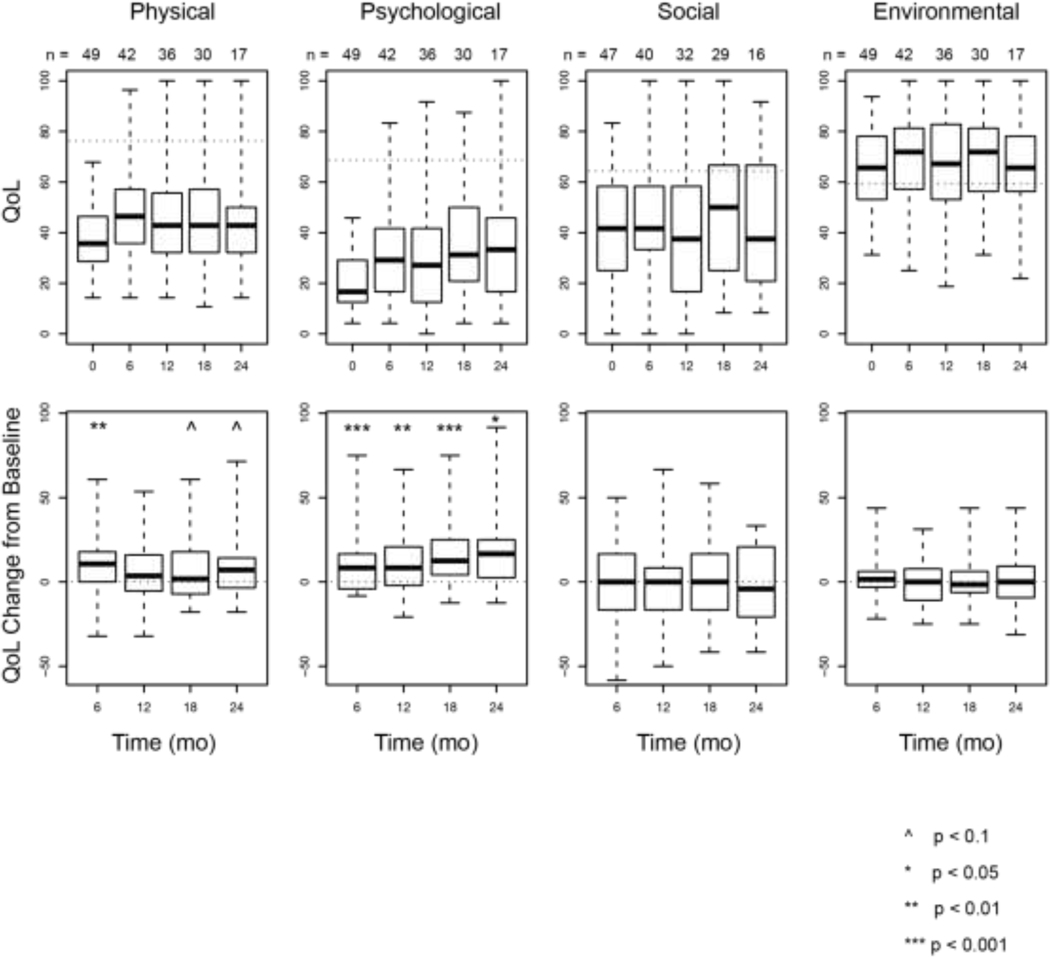
The distributions of QoL scores at baseline and follow-up time points are shown in Figure 1 and Table S2. Participants reported increases in physical QoL 6–24 months after ECT relative to baseline (p = 0.02, χ2 = 11.4, df = 4, linear mixed model). The mean change ranged 6–12 points across the four follow-up assessments (effect size, 0.27–0.50). Subjects also reported improved psychological QoL (p = 0.000001, χ2 = 33.0, df = 4, linear mixed model) with a mean change of 11–17 points (effect size, 0.58–0.83). On average, social and environmental QoL did not change (all p > 0.4, linear mixed models).
Fig. 1.
Distributions of QoL scores over time. The top row shows boxplots of physical, psychological, social, and environmental QoL, respectively.
We determined the proportion of subjects who experienced clinically meaningful QoL changes at follow-up, based on a minimal clinically important difference (MCID) of 10 points (see Methods). The proportion of subjects who reported at least 10 points of improvement in psychological QoL ranged 39–57% across the four follow-up assessments. Similarly, 37–52% reported at least 10-point improvement in physical QoL (see Figure S1).
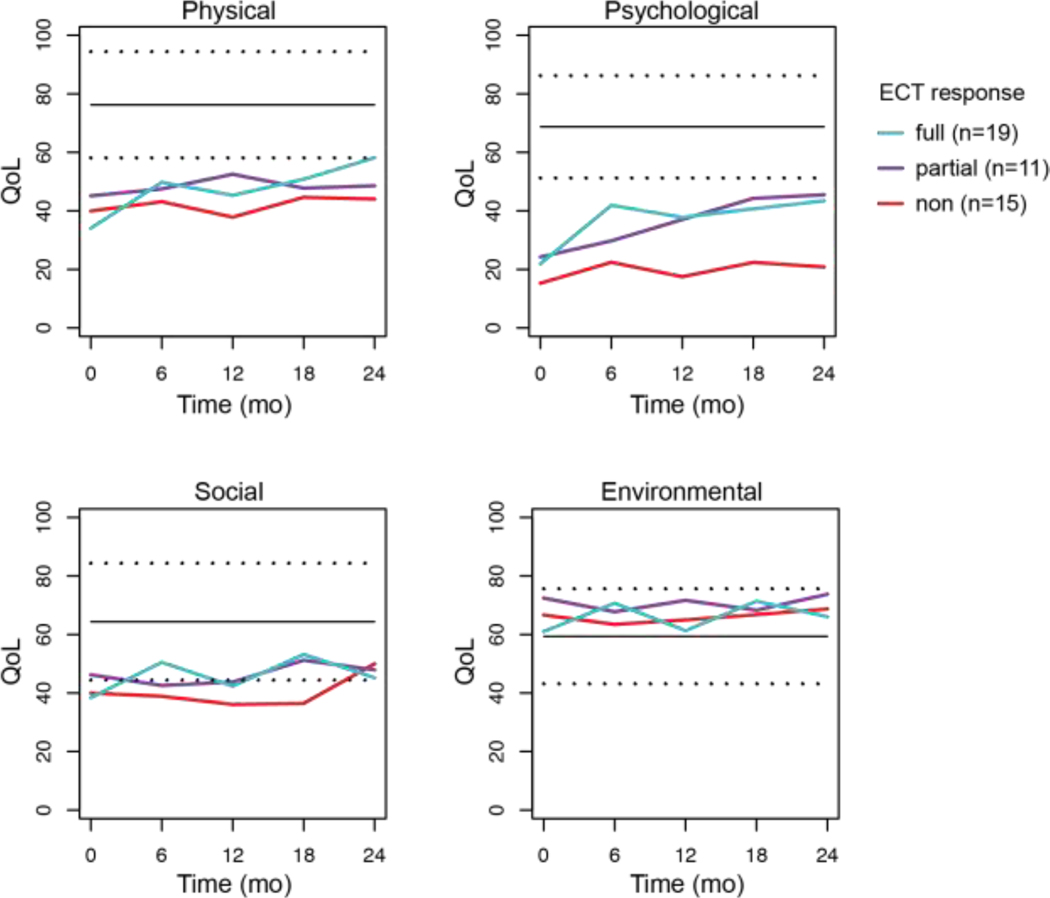
Longitudinal QoL versus acute response to ECT
We hypothesized that subjects who initially responded well to ECT would report better QoL over the subsequent 2 years than subjects who responded poorly. Of the 49 participants with follow-up data, 45 completed the ECT series: 19 were classified as full responders, 11 as partial responders, and 15 as non-responders. We examined longitudinal QoL stratified by level of acute ECT response for the 45 completers, while controlling for baseline QoL (Figure 2 and Table S3). As expected, psychological QoL after ECT was significantly higher among those with better acute response to ECT (χ2 = 5.1, df = 1, p = 0.024, linear mixed model). Participants with better ECT response also reported higher social QoL (χ2 = 4.5, df = 1, p = 0.034), and similar trends were observed for physical QoL (χ2 = 3.7, df = 1, p = 0.055) and environmental QoL (χ2 = 2.8, df = 1, p = 0.092).
Fig. 2.
Average physical, psychological, social, and environmental QoL for three ECT response groups at baseline (0 mo) and longitudinally after ECT.
Association of naturalistic treatment with longitudinal QoL
Subjects received treatment as clinically indicated during the follow-up period, including psychotherapy, medications, and ECT. We hypothesized that more intense treatment might be associated with better psychological and physical QoL. To the contrary, we found that QoL in these domains was not associated with the number of psychotherapy visits, total number of medication trials, number of adequate medication trials, or use of ECT during follow-up (p > 0.05, linear mixed models). These results suggest that analyses of long-term QoL were not confounded by differences in the intensity of treatment during follow-up (see Supplemental Results for details).
Baseline predictors of longitudinal QoL
Exploratory analyses tested baseline sociodemographic and clinical features as predictors of long-term QoL after ECT. Neither age nor sex significantly affected change in QoL over time (p > 0.05, Tables S4 and S5).
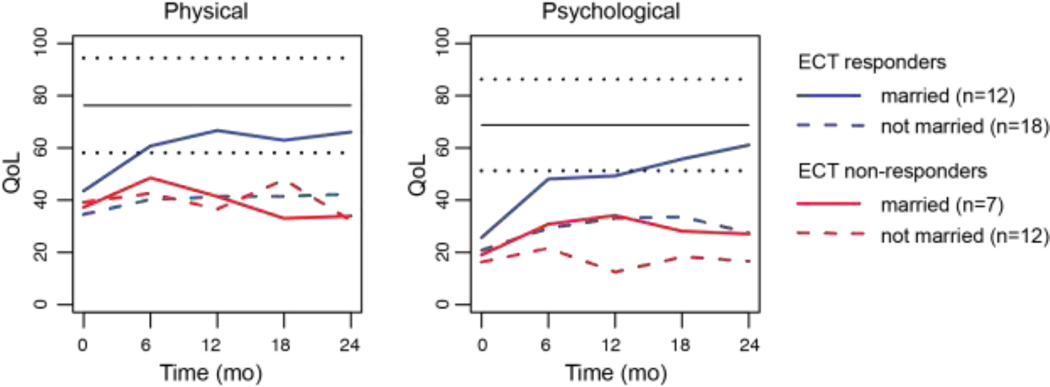
After controlling for baseline QoL and acute ECT response, longitudinal QoL in the physical and psychological domains was superior among subjects who were married (p = 0.03 and p = 0.006, respectively; Figure 3). Physical and psychological QoL was also better among those who did not have disability status (i.e., receiving disability income), those with psychotic features at baseline, and those with shorter index episodes (p < 0.05). Details are provided in the Supplemental Results and Figures S2-S4.
Fig. 3.
Longitudinal QoL for ECT responders and non-responders, sorted by marital status. The panels show mean values for physical and psychological QoL.
Discussion
We found that average long-term psychological and physical QoL improved in this cohort of subjects with TRD during the 2-year period following ECT, while social and environmental QoL remained stable. These statistically significant QoL improvements were clinically meaningful for about 40–50% of participants. As expected, subjects with a better antidepressant response to ECT reported better QoL over the subsequent 2 years than subjects who did not respond acutely. Exploratory analyses suggested that QoL improved most among subjects who were married, those who did not have disability status, those with shorter index episodes, and those with psychotic features at baseline.
Several previous studies have documented clinically significant QoL improvements within the first 5–6 months following an index series of ECT treatments. Antunes and Fleck used the WHOQOL-BREF to investigate the immediate effects of ECT on a cohort of psychiatric inpatients, many of whom had TRD, and found improvements across QoL domains with effect sizes of 0.7 to 1.2 (Antunes & Fleck, 2009). Similarly, a recent meta-analysis of 4 studies that used the Medical Outcomes Study Short Form 36 (SF-36) to measure health-related QoL showed similar improvements (effect sizes 0.5 to 1.3) across multiple domains immediately following the ECT series (Giacobbe et al., 2018). Few studies have reported changes in QoL beyond the immediate post-ECT time point. Two prior studies by McCall et al. followed patients for 24 weeks after an ECT series, during continuation pharmacotherapy or continuation ECT, and found sustained QoL improvements using the SF-36 (McCall et al., 2011, 2018). Our findings complement previous studies by reporting QoL among TRD patients more than 6 months beyond the index series of ECT treatments. We found improvements in long-term psychological and physical QoL (effect sizes 0.58–0.83 and 0.27–0.50, respectively) that were smaller but overlapping with previous short-term studies. This suggests that, on average, the effects of ECT on QoL may diminish beyond 6 months. On the other hand, 40–50% of individuals in our study continued to experience clinically meaningful QoL improvements, suggesting that many patients garnered long-lasting benefits.
Our study also complements a handful of previous longitudinal studies not involving ECT that reported QoL of TRD patients beyond 6 months. An analysis of STAR*D data using the Q-LES-Q instrument over 1 year found that no more than 30% of individuals with major depressive disorder achieved QoL in the normal range after sequenced antidepressant treatment, and QoL was poorer among more treatment-resistant subjects (IsHak et al., 2015). A large European study of MDD patients treated with antidepressant medication measured QoL over 2 years using the Medical Outcomes Study Short Form 12 (SF-12) and EuroQol Five Dimensions questionnaire (Saragoussi et al., 2018). They found that QoL generally decreased over time, despite antidepressant treatment, especially among more treatment-resistant patients. A 5-year study of TRD patients directly compared those treated with vagus nerve stimulation (VNS) to those receiving treatment as usual (Conway et al., 2018). QoL measured with the QLES-Q improved in both groups, but more improvement was found in the VNS group. Because of differences in study design and patient characteristics, it is difficult to directly compare these previously published results to our findings with ECT patients. But a general theme that emerges is that treatment resistance is associated with very poor QoL, and that continued declines in QoL may occur without interventions such as ECT or VNS.
Beyond describing QoL trajectories after ECT, we also discovered individual characteristics that predicted those trajectories. First, we found that, as hypothesized, better acute response to ECT predicted better long-term QoL outcomes. That finding is consistent with the report of McCall and colleagues, who found that remission immediately following ECT predicted sustained QoL improvement at 5–6 months (McCall et al., 2011). In addition, our exploratory analyses revealed baseline demographic and clinical features that predicted QoL outcomes. Four variables were identified -- marital status, disability status, psychotic features, and episode duration -- that were predictive even after accounting for acute ECT response. Some characteristics, such as married status, appeared as powerful as acute ECT response in predicting long-term QoL. Interestingly, a longitudinal study of individuals with relapsing-remitting multiple sclerosis reported parallel findings to ours: QoL over 2-year follow-up was better among patients who were married, those who were employed, and those with shorter disease duration (Baumstarck et al., 2015). Social support may buffer individuals from stress and reduce the chance of relapse of depression. The quality of an interpersonal relationship in receiving social support is important. Although being married predicted worse outcomes in (late-life) depressed persons, subjective social support predicted better improvements in depression (George LK et al., 1989; Park & Unützer, 2014). Because prognosis of long-term outcomes is of interest to TRD patients and clinicians who are considering ECT, the individual characteristics we identified here deserve further study, starting with replication in an independent sample.
Strengths of the current study include the collection of long-term (>6 months) QoL data from individuals with TRD, which has rarely been done, deep clinical phenotyping of the sample, and use of a validated, internationally-normed, cross-cultural QoL instrument. Limitations include the sample size (n=49), which may have prevented us from detecting moderate-sized effects, and the drop-out rate (38%), which could have altered the findings through attrition bias. Because our sample was recruited from a single academic medical center in the US mid-west region and was largely Caucasian, this sample may not be representative of people with TRD in other parts of the world.
Our study has revealed highly variable long-term QoL outcomes among patients with TRD. A better understanding of these diverse trajectories, and the underlying reasons for these trajectories, will be crucial to improve the care of individuals with treatment-resistant mood disorders. If patients at risk of poor long-term outcomes can be identified early on, then personalized interventions might be developed to optimize QoL. Future TRD studies should therefore closely monitor QoL longitudinally while also probing more deeply for individual characteristics that might be targeted to enhance patient satisfaction and well-being.
Supplementary Material
Highlights.
We present QoL-data 6, 12, 18, 24 months after ECT
Exploratory analyses showed that physical and psychological QoL were superior among subjects who were married, did not have disability status, had psychotic features, or had shorter index episodes at baseline.
A clinically meaningful improvement in physical and psychological QoL was observed in about 40--50% of patients during follow-up.
Acknowledgements
We thank Adam F. Sitzmann and Clara Grayhack for assistance with data collection, and the University of Michigan ECT Program for enthusiastically supporting this study.
Funding Resources
This work was supported by the National Institute of Mental Health [NIMH K23 MH 092648), the National Center for Advancing Translational Sciences (NCATS 2UL1 TR 000433), the Taubman Medical Research Institute and the University of Michigan Depression Center.
List of abbreviations:
- CBT
cognitive behavioral therapy
- ECT
electroconvulsive therapy
- MCID
minimum clinically important difference
- MDD
Major Depressive Disorder
- MS
Multiple Sclerosis
- Q-LES-Q
Quality Of Life Enjoyment And Satisfaction Questionnaire
- QoL
quality of life
- SF-36
36-Item Short Form Health Survey
- TRD
treatment-resistant depression
- WHOQOL-BREF
World Health Organization Quality of Life Scale, Brief Version
Footnotes
Disclosure Statement
No author has any financial conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Antunes PB, & Fleck MP (2009). Clinical outcomes and quality of life in patients submitted to electroconvulsive therapy. The Journal of ECT, 25(3), 182–185. 10.1097/YCT.0b013e318190b2a9 [DOI] [PubMed] [Google Scholar]
- Barneveld PS, Swaab H, Fagel S, van Engeland H, & de Sonneville LMJ (2014). Quality of life: A case-controlled long-term follow-up study, comparing young high-functioning adults with autism spectrum disorders with adults with other psychiatric disorders diagnosed in childhood. Comprehensive Psychiatry, 55(2), 302–310. 10.1016/j.comppsych.2013.08.001 [DOI] [PubMed] [Google Scholar]
- Bates D, Mächler M, Bolker B, & Walker S (2015). Fitting Linear Mixed-Effects Models Using lme4. Journal of Statistical Software, 67(1), 1–48. 10.18637/jss.v067.i01 [DOI] [Google Scholar]
- Baumstarck K, Pelletier J, Boucekine M, Auquier P, & MusiQoL study group. (2015). Predictors of quality of life in patients with relapsing-remitting multiple sclerosis: A 2-year longitudinal study. Revue Neurologique, 171(2), 173–180. 10.1016/j.neurol.2014.09.005 [DOI] [PubMed] [Google Scholar]
- Conway CR, Kumar A, Xiong W, Bunker M, Aaronson ST, & Rush AJ (2018). Chronic Vagus Nerve Stimulation Significantly Improves Quality of Life in Treatment-Resistant Major Depression. The Journal of Clinical Psychiatry, 79(5). 10.4088/JCP.18m12178 [DOI] [PubMed] [Google Scholar]
- Cook CE (2008). Clinimetrics Corner: The Minimal Clinically Important Change Score (MCID): A Necessary Pretense. The Journal of Manual & Manipulative Therapy, 16(4), E82–E83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Mol et al. (2018). Satisfactory results of a psychometric analysis and calculation of minimal clinically important differences of the World Health Organization qualit... - PubMed—NCBI. https://www.ncbi.nlm.nih.gov/pubmed/30477456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Everitt PD of B I of P B, Landau S, Everitt BS, Landau SSSSSSL, & Everitt D of B and S CB (2004). A Handbook of Statistical Analyses Using SPSS. Taylor & Francis. [Google Scholar]
- Fekadu A, Wooderson SC, Markopoulo K, Donaldson C, Papadopoulos A, & Cleare AJ (2009). What happens to patients with treatment-resistant depression? A systematic review of medium to long term outcome studies. Journal of Affective Disorders, 116(1–2), 4–11. 10.1016/j.jad.2008.10.014 [DOI] [PubMed] [Google Scholar]
- Foxand Weisberg. (2019). An {R} Companion to Applied Regression, Third Edition. Thousand Oaks CA: Sage. Thousand Oaks CA: Sage. https://socialsciences.mcmaster.ca/jfox/Books/Companion/ [Google Scholar]
- George LK et al. (1989). Social support and the outcome of major depression. - PubMed—NCBI. https://www.ncbi.nlm.nih.gov/pubmed/2590779 [DOI] [PubMed] [Google Scholar]
- Giacobbe P, Rakita U, Penner-Goeke K, Feffer K, Flint AJ, Kennedy SH, & Downar J (2018). Improvements in Health-Related Quality of Life With Electroconvulsive Therapy: A Meta-analysis. The Journal of ECT, 34(2), 87–94. 10.1097/YCT.0000000000000486 [DOI] [PubMed] [Google Scholar]
- Haq AU, Sitzmann AF, Goldman ML, Maixner DF, & Mickey BJ (2015). Response of depression to electroconvulsive therapy: A meta-analysis of clinical predictors. The Journal of Clinical Psychiatry, 76(10), 1374–1384. 10.4088/JCP.14r09528 [DOI] [PubMed] [Google Scholar]
- IsHak WW, Mirocha J, James D, Tobia G, Vilhauer J, Fakhry H, Pi S, Hanson E, Nashawati R, Peselow ED, & Cohen RM (2015). Quality of life in major depressive disorder before/after multiple steps of treatment and one-year follow-up. Acta Psychiatrica Scandinavica, 131(1), 51–60. 10.1111/acps.12301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston KM, Powell LC, Anderson IM, Szabo S, & Cline S (2019). The burden of treatment-resistant depression: A systematic review of the economic and quality of life literature. Journal of Affective Disorders, 242, 195–210. 10.1016/j.jad.2018.06.045 [DOI] [PubMed] [Google Scholar]
- Lex H, Ginsburg Y, Sitzmann AF, Grayhack C, Maixner DF, & Mickey BJ (2019). Quality of life across domains among individuals with treatment-resistant depression. Journal of Affective Disorders, 243, 401–407. 10.1016/j.jad.2018.09.062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mas-Expósito L, Amador-Campos JA, Gómez-Benito J, & Lalucat-Jo L (2011). The World Health Organization Quality of Life Scale Brief Version: A validation study in patients with schizophrenia. Quality of Life Research, 20(7), 1079–1089. [DOI] [PubMed] [Google Scholar]
- McCall WV, Lisanby SH, Rosenquist PB, Dooley M, Husain MM, Knapp RG, Petrides G, Rudorfer MV, Young RC, McClintock SM, Mueller M, Prudic J, Greenberg RM, Weiner RD, Bailine SH, Youssef NA, McCloud L, Kellner CH, & CORE/PRIDE Work Group. (2018). Effects of continuation electroconvulsive therapy on quality of life in elderly depressed patients: A randomized clinical trial. Journal of Psychiatric Research, 97, 65–69. 10.1016/j.jpsychires.2017.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCall WV, Rosenquist PB, Kimball J, Haskett R, Isenberg K, Prudic J, Lasater B, & Sackeim HA (2011). Health-related quality of life in a clinical trial of ECT followed by continuation pharmacotherapy: Effects immediately after ECT and at 24 weeks. The Journal of ECT, 27(2), 97–102. 10.1097/YCT.0b013e318205c7d7 [DOI] [PubMed] [Google Scholar]
- Mickey BJ, Ginsburg Y, Sitzmann AF, Grayhack C, Sen S, Kirschbaum C, Maixner DF, & Abelson JL (2018). Cortisol trajectory, melancholia, and response to electroconvulsive therapy. Journal of Psychiatric Research, 103, 46–53. 10.1016/j.jpsychires.2018.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman GR, Sloan JA, & Wyrwich KW (2003). Interpretation of changes in health-related quality of life: The remarkable universality of half a standard deviation. Medical Care, 41(5), 582–592. 10.1097/01.MLR.0000062554.74615.4C [DOI] [PubMed] [Google Scholar]
- Oliveira SEH, Carvalho H, & Esteves F (2016). Toward an understanding of the quality of life construct: Validity and reliability of the WHOQOL-Bref in a psychiatric sample. Psychiatry Research, 244, 37–44. 10.1016/j.psychres.2016.07.007 [DOI] [PubMed] [Google Scholar]
- Park& Unützer. (2014). Hundred Forty Eight More Days With Depression: The Association Between Marital Conflict and Depression-Free Days—PubMed. https://pubmed.ncbi.nlm.nih.gov/24700495-hundred-forty-eight-more-days-with-depression-the-association-between-marital-conflict-and-depression-free-days/?from_term=marital+discord+model+of+depression+and+quality+of+life+long+term&from_pos=3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team. (2019). A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/. https://www.r-project.org/ [Google Scholar]
- Rosenquist PB, Brenes GB, Arnold EM, Kimball J, & McCall V (2006). Health-related quality of life and the practice of electroconvulsive therapy. The Journal of ECT, 22(1), 18–24. [DOI] [PubMed] [Google Scholar]
- Rubio JM, Olfson M, Pérez-Fuentes G, Garcia-Toro M, Wang S, & Blanco C (2014). Effect of first episode axis I disorders on quality of life. The Journal of Nervous and Mental Disease, 202(4), 271–274. 10.1097/NMD.0000000000000117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rush AJ, Trivedi MH, Wisniewski SR, Nierenberg AA, Stewart JW, Warden D, Niederehe G, Thase ME, Lavori PW, Lebowitz BD, McGrath PJ, Rosenbaum JF, Sackeim HA, Kupfer DJ, Luther J, & Fava M (2006). Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: A STAR*D report. The American Journal of Psychiatry, 163(11), 1905–1917. 10.1176/ajp.2006.163.11.1905 [DOI] [PubMed] [Google Scholar]
- Sackeim. (2019). The assessment of resistance to antidepressant treatment: Rationale for the Antidepressant Treatment History Form: Short Form (ATHF-SF) - PubMed—NCBI. https://www.ncbi.nlm.nih.gov/pubmed/30974339 [DOI] [PubMed] [Google Scholar]
- Saragoussi D, Christensen MC, Hammer-Helmich L, Rive B, Touya M, & Haro JM (2018). Long-term follow-up on health-related quality of life in major depressive disorder: A 2-year European cohort study. Neuropsychiatric Disease and Treatment, 14, 1339–1350. 10.2147/NDT.S159276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skevington SM, Lotfy M, O’Connell KA, & WHOQOL Group. (2004). The World Health Organization’s WHOQOL-BREF quality of life assessment: Psychometric properties and results of the international field trial. A report from the WHOQOL group. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 13(2), 299–310. [DOI] [PubMed] [Google Scholar]
- WHO. (2017). WHO | Disease burden and mortality estimates. https://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html
- WHOQOL Group. (1998). Development of the World Health Organization WHOQOL-BREF quality of life assessment. The WHOQOL Group. Psychological Medicine, 28(3), 551–558. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.