Abstract
Background
Patients are increasingly being asked for feedback about their healthcare and treatment, including safety, despite little evidence to support this trend. This review identifies the strategies used to engage patients in safety during direct care, explores who is engaged and determines the mechanisms that impact effectiveness.
Methods
A systematic review was performed of seven databases (CINAHL, Cochrane, Cochrane‐Central, Embase, ISI Web of Science, Medline, PsycINFO) that included research published between 2010 and 2020 focused on patient engagement interventions to increase safety during direct care and reported using PRISMA. All research designs were eligible; two reviewers applied criteria independently to determine eligibility and quality. A narrative review and realist synthesis were conducted.
Results
Twenty‐six papers reporting on twenty‐seven patient engagement strategies were included and classified as consultation (9), involvement (7) and partnership (11). The definitions of ‘patient engagement’ varied, and we found limited details about participant characteristics or interactions between people utilizing strategies. Collaborative strategy development, a user‐friendly design, proactive messaging and agency sponsorship were identified as mechanisms to improve engagement about safety at the point of direct care.
Conclusions
Agency sponsorship of collaboration between staff and patients is essential in the development and implementation of strategies to keep patients safe during direct care. Insufficient details about participant characteristics and patient–provider interactions limit recommendations for practice change. More needs to be learned about how patients are engaged in discussions about safety, particularly minority groups unable to engage with standard information.
Patient or Public Contribution
Review progress was reported to the CanEngage team, including the consumer steering group, to inform project priorities (PROSPERO CRD42020196453).
Keywords: patient engagement, patient participation, patient safety, point of care, systematic review
1. BACKGROUND
Patients are often the only constant element in their healthcare journey and provide important contextual information for designing safe healthcare services. 1 The fact that patients can retrospectively identify unsafe events that occurred during their care is well established. 2 , 3 , 4 , 5 They also play an active role in their own safety by raising concerns or flagging inconsistencies and inaccuracies during healthcare interactions. 4 Over the past 20 years, interventions that encourage patients to discuss or raise concerns about inaccuracies relevant to their care have been implemented. 6 , 7 , 8 These interventions occurred simultaneously with evaluations of patient involvement in system‐ and service‐level patient safety programmes, such as patient‐led incident reporting systems. 9 The use of patient‐centred tools and strategies to enhance safety has increased despite limited evidence about their effectiveness.
Limited research about the effectiveness of patient engagement, and the depth of engagement needed to promote safe care, is reflective of wider inconsistencies. There are various definitions of patient engagement, involvement and participation in the literature. 10 Carman et al. 10 defined patient engagement as ‘patients, families, their representatives, and health professionals working in active partnership at various levels across the health care system’ (p. 224). The framework of engagement developed by Carman et al. 10 builds upon Arnstein's 11 work and classifies patient engagement across a continuum, ranging from patient consultation through to partnership. This engagement continuum spans three distinct spheres of patient engagement: direct care, organisational design and governance and policy making. In light of the variation in what constitutes patient engagement present in current research and practice, Carman et al.'s 10 definition and framework are used throughout this review. This paper focuses on engagement strategies implemented in the ‘direct care’ sphere of engagement. Carmen et al.'s 10 sphere of direct care aligns with the clinical point of care and refers to the period when clinicians deliver healthcare services or treatments to patients; this can be hospital or community based. 12
With growing recognition of the value of engaging patients in healthcare design and delivery, and the susceptibility that some specific population groups have to adverse events, the need for better data about facilitating engagement is imperative. The literature identifies various system, service and clinical factors that support effective patient engagement such as education about their condition, 13 , 14 empowerment to engage 15 , 16 and the willingness and ability of clinicians and patients to communicate about safety. 17 , 18 , 19 , 20 The extent to which an organisation is committed to patient engagement is a measure in most organisational safety culture surveys, but there is little evidence of the enablers and system prerequisites to facilitate effective engagement. 21 , 22 Evidence of the enablers and system prerequisites for effective engagement have not been synthesized to support the implementation of such interventions. 22 Similarly, evidence about the nature and extent to which patients are engaged in safety is fragmented and lacks information about approaches for diverse populations, such as people from culturally and linguistically diverse (CALD) backgrounds or other communication needs. 8 , 21 , 23 , 24
This systematic review aims to address the knowledge gaps identified above using a realist synthesis 25 to explore the following questions: (1) What interventions have been used to engage patients in safety during direct care and what is the mode of intervention (e.g., video, paper chart, electronic portal) and extent of engagement (e.g., number of opportunities, with whom)? (2) What types of patients and their contexts are described in the interventions? (3) What are the mechanisms that influence the effectiveness of consumer engagement approaches in enhancing safe care and treatment?
2. METHODS
A systematic review and realist synthesis were undertaken and reported in accordance with the Preferred Reporting Items for Systematic Review and Meta‐Analyses (PRISMA) statement. 26
2.1. Prospero registration number: CRD42020196453
Inclusion criteria: Studies published between January 2010 and December 2020 in English were included. All research designs were eligible, including qualitative, quantitative, multi‐ and mixed‐method studies. All studies included participants who were healthcare consumers, patients, family members or other caregivers. Safety outcomes in the clinical encounters described encompassed increased notifications of or the prevention of safety breaches, errors, accidents, incidents, complications and infections. Selected interventions had to use patient engagement designed to minimize harm. Studies that did or did not include a comparator intervention were eligible.
Exclusion criteria: All studies outside the date range or published in a language other than English were excluded. Systematic or other literature reviews were not included, but their reference lists were searched. Studies that focused on methods beyond direct care, for example, to enhance governance or inform improvements to organisational safety for example, adverse event reporting systems or service governance, service planning, self‐management or improving health, such as self‐management for people with chronic conditions, were beyond the scope of the present review. Studies about patient involvement in training medical or nursing staff, patient attitudes towards safety or willingness to participate and studies about participatory research or codesign methods unrelated to safety were not included.
2.2. Study identification
The key concepts of patient engagement and unsafe healthcare were used to generate keywords, synonyms and phrases to inform a comprehensive search strategy (see File S1). The search strategy was applied to seven databases: CINAHL, Cochrane, Cochrane‐Central, Embase, ISI Web of Science, Medline, PsycINFO January 2010 and December 2020. In addition to searching the reference lists of the included studies, hand searches of the following relevant journals were conducted to locate further potentially recently published eligible studies: The Journal of Patient Safety, The British Medical Journal of Quality and Safety, The International Journal for Equity in Healthcare, BMC Health Services Research and The International Journal for Quality in Healthcare.
2.3. Study selection and data extraction
Search results were exported to Endnote (X10) and duplicates were removed. Articles were then extracted to Covidence systematic review management software (Veritas 150 Health Innovation). Two reviewers (J. L. and B. J.) completed the initial title and abstract review, followed by an independent screening by a third reviewer (B. N). The inclusion criteria were then independently applied to full‐text articles by two reviewers (B. N. and R. H.), with disagreements or uncertainty resolved through discussion. The following data were extracted: author, year, country, aims/objectives, setting, number of participants, participant characteristics, inclusion of diverse populations, method of data collection and samples, intervention/method of patient engagement, main findings and what worked (enablers, barriers).
2.4. Assessment of study quality
Due to the heterogeneity of the study types, the Quality Assessment Tool for Diverse Studies, a validated quality appraisal tool, 27 was used. Two reviewers (B. N. and K. J.) independently applied the 13 criteria to the included studies. The κ test was used to determine inter‐rater reliability, and substantial reliability was confirmed (κ = .726). 28
2.5. Data synthesis
Findings were synthesized using a narrative approach and the realist framework to explore which interventions worked, in what conditions and with whom. 25 Realist evaluation was selected because it examines the conditions that facilitate success rather than just information about whether the outcome or intervention ‘worked’. 29
Key findings relevant to the review questions were extracted, including barriers and enablers to implementation. Carman et al.'s 10 engagement framework was used to determine the extent of engagement in the interventions, and engagement strategies are described in relation to the three levels of engagement.
3. RESULTS
The systematic search produced 3029 papers, with 2706 studies excluded and 217 duplicates removed. A total of 82 full texts were reviewed and 55 were excluded (28 included outcomes not related to safety, 14 study designs and 9 intervention types did not fulfil the inclusion criteria, 3 were in nonhealth settings and 1 more recent paper available), leading to 26 included publications describing 27 strategies. Figure 1 shows the search and selection process.
Figure 1.
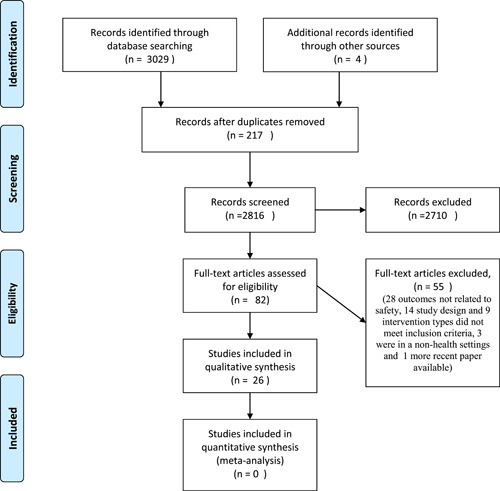
Preferred Reporting Items for Systematic Review and Meta‐Analyses 2009 flow diagram
Characteristics of the included studies: Studies originated from the United States (13), the Netherlands (4), the United Kingdom (3), Canada (2), Vietnam (1), Australia (1), Korea (1) and Norway (1). Seventeen of the twenty‐six studies were focused on inpatient safety, three on specific clinics or treatments and six were focused on treatment between face‐to‐face visits. The studies were conducted in a range of clinical areas including inpatient adult general medical services, 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 inpatient surgical departments, 40 , 41 , 42 adult oncology, 43 outpatient radiology clinics, 44 , 45 adult intensive care, 46 residential aged care facility, 39 inpatient paediatric services, 34 , 45 , 46 , 47 , 48 , 49 , 50 , 51 with two whole of hospital studies 52 , 53 and homecare visits, appointments, discharge and pharmacy community. 32 , 52 , 54
Study quality: A score of 0–3 was assigned in the 13 categories used to assess quality (see File S2). Of the 26 included papers, most achieved high scores (2 or 3) in the categories of statement of aims (23), appropriate study design to address research aims (22) and format of data collection tool to address research aims (23). Fourteen studies contained limited details in the participation data provided (Criteria 9) and eight described involvement of ‘consumers or stakeholders’ (Criteria 12) in the process of study design and conduct.
3.1. Review findings
3.1.1. What interventions have been used to engage patients in safety activities during direct care, and what is the mode of intervention and extent of engagement?
Twenty‐seven patient engagement strategies were reported in twenty‐six publications (Table 1). The engagement activities are described in relation to approaches that were focused on consultation, involvement or partnership relative to the Carman Framework. 10 Evidence from each study of the effectiveness of a strategy in improving safety is presented in Table 1.
Table 1.
Summary of the study findings
| Author | Year | Country/setting | Aims/objectives | Method/sample | Intervention type | Main findings | Enablers | Barriers |
|---|---|---|---|---|---|---|---|---|
| Baker et al. 52 | 2016 | Canada/hospital and community | To evaluate three efforts to engage patients in quality improvement efforts | Case study | PARTNERSHIP | By implementing patient‐informed practices (TCAB), they achieved a 25% decrease in Clostridium difficile and vancomycin‐resistant Enterococci infections. Identified that | *Client‐centred systems at many levels of care and governance. *Opportunities for patients and staff to work together towards tangible goals. *Cultural shift in valuing patients, families and *caregivers as partners. * peer mentors, *multiple participating advisors, *external facilitators for events, *leadership support and role modelling | None identified |
| Transforming care at the bedside (TCAB) project to increase quality of bedside interaction | ||||||||
| Case study | PARTNERSHIP Collaboratively developed a hip surgery post‐op complication kit that encouraged engagement | The FReSH START Toolkit: led to better satisfaction and proactive approach to prevent complications | ||||||
| Bell et al. 53 | 2017 | USA/hospital | To evaluate a new patient reporting tool named OpenNotes focused on safety concerns | 9‐Question survey and designed a FAQs document for patients (n = 2736) | INVOLVEMENT | Giving patients/care partners the opportunity to review online notes can increase safety for the individual and improve practices. Concerns raised in 59 reports (23%), most commonly possible mistakes (21%) | *Access to information provided greater transparency, and did not impact the relationships between providers and service users | Health literacy, cultural differences, demographic factors, cognitive issues and provider‐related factors |
| OpenNotes patient feedback reporting tool | ||||||||
| Bergal et al. 40 | 2010 | USA/hospital | Strategy to improve the safety and quality of care, promote patient education and provide a tool for a cooperative treatment approach | Patients to mark the site of surgery to see if this helped avoid wrong‐site surgery (n = 135) | CONSULTATION | 68.2% Compliance—concluded that patient involvement in surgical site marking is unreliable and may not help in decreasing the chances of wrong‐site surgery. Of the 200 patients who were enroled, 135 made the mark | *Younger participants more ‘compliant’ and engaged in their care. *Asking the patient to mark the site when not sedated/medicated, appropriate timing between education and surgery (not too long before) | *Age and cultural beliefs impacted compliance *difficult to measure impact of study as wrong‐site surgery is uncommon |
| Asking patients to mark on their body where surgery was to occur | ||||||||
| Buning et al. 30 | 2016 | The Netherlands/hospital | To examine the availability and accountability of a web tool for medication coordination (MMa) during medical transitions and across various appointments/points of care | Patients completed the MMa list on existing portal and compared with a list of meds completed by pharmacists, questionnaire (n = 17) | PARTNERSHIP | Discrepancies between the lists were differences in dose and frequency (n = 27) and differences in medications registered (n = 15). *Patients had a more accurate list that the list compiled by the pharmacy practitioner. *Mobile application was feasible and well accepted by the patients | *Skilled tech users more likely to participate—not clear whether they would be more likely to use app. Or take part in research *patients were positive about it controlling data across sites | Patients would have preferred password feature for security |
| Web‐based tool for patients to be part of medication reconciliation at points of transition—for use in various care settings. Patient owns and is responsible for the information rather than a different system at each service/doctor's visit | ||||||||
| Campbell et al. 51 | 2020 | Vietnam/hospital | To measure the effectiveness of visual empowerment tools to improve hand hygiene in Southeast Asia | Observation before and after intervention (n = 73) | PARTNERSHIP | Giving families visual reminder tools and brief education is associated with increased HCW HH. Baseline HH adherence was 46%, and increased to 73% during the implementation period (p < .001) | *Low‐cost tool *empowerment and education of patients rather than education of HCW. *Leaving a visual reminder at the bedside enabled patients to show a reminder rather than confront HCWs | Fear of HCW reaction |
| Visual tool to empower patients to remind healthcare workers to wash their hands and script for use by the research assistant to explain how to use the visual tool | ||||||||
| Cox et al. 47 | 2017 | USA/hospital | To examine the impact of the family‐centred rounds (FCRs) checklist and associated provider training, on performance of FCR elements, family engagement and patient safety | Parent survey, admission data for length of stay and video recording of FCRs (n = 273) | PARTNERSHIP | Using the checklist enhanced engagement and impacted safety of care. Safety findings—measured climate but commented on increased awareness of hand hygiene and open communication during handover re. meds | *The checklist incorporates recommendations for FCRS with non‐English speakers. *Reading back ‘orders’ may be useful to foster safe medication use | *Stress *new diagnosis, *English proficiency impacted research participation. But these are not necessarily barriers for use of FCR |
| Family engagement in rounds—checklist for families to measure 8 elements. Data analysis = qualitative review of video footage, survey of families was conducted re. safety | ||||||||
| de Jong et al. 38 | 2016 | The Netherlands/community | To investigate whether quality of the electronic medication record improves when patients play a vigilant role | Digital questionnaires and patients visit the pharmacist twice for verification consultations (n = 152) | INVOLVEMENT | Forty‐nne percent of participants never logged into their eMAR. Corrections were necessary for approximately 20% of eMARS because the patient started/stopped a medication, changed the timing of medication and changed dosage | *User‐friendly *daily users of the internet were more likely to email | Data collection process was onerous |
| Electronic medication administration record (eMAR) patient communication tool. Module on the pharmacist's website with a personal patient log‐in. Patients can view their prescribed medications (inc. method, dose, freq.) and communicate with the pharmacist regarding errors. Patients were invited to check after every change to prescription | ||||||||
| Duckworth et al. 31 | 2019 | USA/hospital | To assess the effectiveness for engaging patients and family in the three‐step fall prevention process using varied modalities: electronic toolkit, laminated toolkit and bedside display | Randomly selected patients asked what their plan is and nurse checks if there is a plan visible at bedside (n = 1209) | CONSULTATION | Providing three Fall TIPS modalities is effective and flexible approach. Over 80% adherence with protocol. It is possible to have evidence‐based falls programme within current workflow and to engage patients in any of the modalities | *Support from leadership *good communication channels *flexibility in the way sites can automate/implement | *Lack of systemic support, *lack of funding, *limited staff engagement |
| Examining a previously developed intervention adding modalities—a falls prevention kit that is electronic, laminated and a poster | ||||||||
| Dykes et al. 46 | 2017 | USA/hospital | To examine the efficacy of a patient‐centred care and engagement programme implemented in ICUs. To shift the clinical paradigm from providers alone determining ‘What is the matter?’ to discovering ‘What matters to you?’ | Whole of hospital, reported experience/satisfaction and adverse events‐ survey in person before transfer from ICU, phone survey by research staff 45 days postdischarge (random sample) (n = 2105) | PARTNERSHIP | Reduction in adverse events and improved patient and care partner satisfaction. Adverse events decreased 29% 59.0 per 1000 patient days (95% CI: 51.8–67.2) to 41.9 per 1000 patient days (95% CI: 36.3–48.3; p < .001), during the intervention period of 11 months compared to the baseline period (preceding 12 months) | *Patient‐centred care, *staff training, *staff skill/attitude, *partnership with care partners (as the patient is often too ill) | *Portal was most used by white, young privately insured patients, *activating portals is complex |
| Structured patient‐centred care and engagement training programme and web‐based technology including ICU safety checklist, shared care plan and messaging platform. Patients can access the online portal to view health information, participate in the care plan and communicate with providers | ||||||||
| Dykes et al. 55 | 2020 | USA/hospital | To assess whether a fall prevention toolkit that engages patients and families in the fall prevention process throughout hospitalisation is associated with reduced falls and injurious falls | Falls data and injury from falls data per 1000 patient days (n = 37,231) | CONSULTATION | Engaging patients in fall‐prevention was associated with fewer falls among younger patients and substantially fewer fall‐related injuries among older patients. There was a 34% reduction in falls after implementation | *Team approach, *engagement of hospital leadership staff, *continuous engagement | *Timing, *limited engagement of leadership staff |
| Nurses reviewed tailored falls TIPS with the patient at admission and each shift | ||||||||
| Ekstedt et al. 43 | 2014 | Norway/hospital and community | To explore if and how an e‐message service, a single component of practice‐integrated SMSS, affect the continuity of care and safety of patients with breast cancer | Data collected through an online tool WebChoice (n = 200) | PARTNERSHIP | Safety related to messages about information double checking and coordination of care. Ninety‐one dialogues consisting of 284 messages were analysed. Patients were able to clarify, report concerns more easily and ensure accurate transfer of information between services | *Informed patient seen as a buffer against medical mishaps and delays, *giving patients opportunities to check on advice that they had been given, ask specific questions | *Researchers identified that new tools may increase the complexity of interactions |
| Online self‐management support system (SMSS) e‐messaging service. Patients can direct questions to nurses, physicians and social workers | ||||||||
| Garfield et al. 32 | 2020 | UK/primary and secondary healthcare | To identify mechanisms by which patient‐held medication lists could be used to support safety, key supporting features and barriers and facilitators to their use | Two focus groups with patients and carers, 16 interviews with healthcare professionals (n = 16), interviews with people carrying medication lists (n = 60), quantitative features analysis of tools and usability testing of four tools | PARTNERSHIP | Patients and healthcare professionals perceive patient‐held medication lists to have a wide variety of benefits, need a variety of options, useful especially in transitions and emergencies | *Support from healthcare professionals, family/friends *patients recognizing need—trigger event for example, emergency or extra complexity of med schedule *flexibility, *clear purpose of the tool | *Lack of patient awareness that health systems were not linked—assumed that health staff already knew about meds. *Small number of patients were concerned about confidentiality, *bulky paperwork |
| Explored the use of various existing patient‐held medication tools (103 tools). Electronic and paper‐based tools were included | ||||||||
| Gerard et al. 33 | 2017 | USA/hospital | To learn more about patient experiences with reading and providing feedback on their visit notes | Electronic portal for patients to review notes. Two‐hundred and sixty reports | INVOLVEMENT | Access to notes gave patients the opportunity to confirm what they needed to do, gain access to info faster, share info with others, engage with clinicians. Identified the benefit for correcting mistakes and inaccuracies | *Education level, *comfort using technology, *giving patient access to information about their health, *making EHR more open and interactive | *Limited confidence with technology |
| Patients can use the open notes portal to engage with electronic notes. This study examined what they value about that tool as part of a bigger quality improvement project | ||||||||
| Grossman et al. 34 | 2018 | USA/hospitals and medical centres | To provide recommendations on how to most effectively implement advanced features of acute care patient portals | Case studies‐ descriptive exploration of 6 sites that use patient portals (n = 1065) | INVOLVEMENT | Need to adjust current portals to meet stakeholder needs—patients and providers | *Having an ‘invite’ feature could eliminate privacy issues, *consistency in how info is reported, *photographs and bios of care team, *having communication categories for feedback and communication in addition to generic messaging features | *Practitioners fear interruption to workflow *privacy issues re. caregivers viewing info |
| Various interventions across 6 sites | ||||||||
| Heyworth et al. 35 | 2014 | USA/hospital at discharge | To test the use of an online medication reconciliation tool ‘Secure Messaging for Medication Reconciliation Tool’ (SMMRT) among patients to improve patient safety | Patients viewed medications and clarified any inaccuracies through SMMRT and 10 in‐depth interviews (n = 60) | INVOLVEMENT | Sent 51 SMMRT messages to patients and received 34 replies. In 40/51 patients, there was a discrepancy between the discharge summary and medications filled in at the pharmacy. This amounted to 108 clinically important discrepancies total. 68% were medication omissions an 19% were medication duplications. 23 potential Adverse drug events were identified; 43% were potentially life threatening | *Technical support, *easy to use, *rapid access to health info | *No computer access or knowledge of the internet, *patients may have meds prescribed elsewhere that are not part of the study |
| An online portal; patients view their medications in a secure email message and reply using SMMRT's interactive form to verify medication regimes and clarify inaccuracies | ||||||||
| Khan et al. 48 | 2018 | USA/hospital | To determine whether medical errors, family experience and communication processes improved after implementation of an intervention to standardize the structure of healthcare provide–family communication on FCRs | AEs and medical errors were measured using an established tool to determine the number of events per 1000 patient days (n = 3106) | PARTNERSHIP | Although overall errors were unchanged, harmful medical errors decreased and communication processes improved | *Staff training, *collaborative development of tool, *structured communication framework, *iterative development with family involvement, *using plain language, *structural change to accommodate rounds | *Before intervention—family passive at sites that did have bedside rounds, some had rounds without patients present, jargon was used, social issues or limited English often precluded involvement in rounds |
| The intervention consisted of a communication framework for rounds, family engagement and bidirectional communication principles | ||||||||
| Kim et al. 44 | 2017 | Korea/outpatient clinic | Verify the effectiveness of patient involvement in identifying both patients and the location(s) before X‐ray examinations at orthopaedic clinics | Over 1 year, 2013−2014, using comparison of errors before and after intervention. Errors were categorized and analysed. n = 13,617 (Group 1) and n = 12,588 (Group 2) | CONSULTATION | There was a significant reduction in errors. The rate of X‐ray prescription errors declined from 0.58% (Group I, 79/13,617) to 0.08% (Group II, 10/12,588) | *Simple change to practice | *Staff change was problematic—need consistent data collector |
| Staff asking additional questions of patients to confirm the X‐ray site | ||||||||
| Lachman et al. 49 | 2015 | UK/hospital | Testing and introduction of a self‐reporting, real‐time bedside tool | The reporting tool was developed in three stages: (1) tested patient readiness with a questionnaire, (2) designed a patient‐centric process for managing risk with a real‐time daily reporting tool and (3) staff checked the tool each day at the end of their shift (n = 85) | PARTNERSHIP | Thirty events were recorded, the highest proportion almost equally relating to equipment problems and communication issues. During this study period, staff critical incident reporting increased to 2.31 reports per week. Only 3% of incidents reported by patients were reported in the staff reporting process | *Pictorial reporting tool did not require high levels of literacy or English proficiency—children could also use it, *patient engagement throughout and using visual tool, *proactive approach rather than only reactive | *Questionnaire was time‐consuming and reliant on English‐language proficiency, *involving staff in the reporting process leads to fewer reports |
| Daily safety reporting tool and questionnaire | ||||||||
| Lawton et al. 50 | 2016 | UK/hospital | To evaluate the efficacy of the Patient Reporting and Action for a Safe Environment intervention | PMOS 44‐point questionnaire, PIRT = safety reporting tool for patients. Both are validated tools. Average of 25 patients per ward at three‐time points | CONSULTATION | Intervention uptake and retention of wards were 100% and patient participation was high (86%), no significant effect of the intervention on any outcomes at 6 or 12 months. However, for those for which the wards were directly accountable, intervention wards showed improvement compared with control wards | *Hospital ward engagement | *Development and adherence to action plans |
| The ward‐level intervention/data collection comprised two tools: (1) a questionnaire (patient measure of safety (PMOS)) and (2) a proforma for patients to report both safety concerns and positive experiences (patient incident reporting tool) | ||||||||
| Lutjeboer et al. 45 | 2015 | The Netherlands/outpatient clinic | To compare patient safety and patient satisfaction between patients who were subjected to a preprocedural visit to an IR outpatient clinic | Safety checklist and questionnaire (19 questions in Dutch). Control group (n = 188) and experimental group (n = 198) | INVOLVEMENT | The number of process deviations associated with elective IR procedures can be significantly reduced when patients are consulted in an IR outpatient clinic before the procedure. Increase in informed consent for those in the treatment group | *Hospital systems/staff recognizing the role of IRs relating to patient before the intervention. *Recognition of the value of the relationship rather than conducting the procedure only | *Dutch‐speaking participants only. *Barrier relates to research data collection rather than actual intervention |
| Appointment 2–14 days before the scheduled IR procedure, information, screening for risk and consent obtained | ||||||||
| Opsahl et al. 41 | 2017 | USA/hospital | Explore the impact of adding a video educational engagement strategy intervention for patients and families added to the current fall prevention intervention | Staff interview, falls data. A pre/posttest comparison of monthly and quarterly fall rate reports before, during and after video implementation guided the study (n = 2148) | CONSULTATION | Video offers the clinician another component to collaborate with patients and their families, and impact patient education outcomes. Including video engagement for the patient can result in positive trends towards a decrease in the fall rate of hospitalized patients | *Staff education, *engaging patients and families with video, *incorporate evidence‐based preventative strategies in all levels of the healthcare system | *Technology and resources |
| The addition of an educational video for patients in an existing falls prevention strategy to attain better fall rates | ||||||||
| Rochon et al. 42 | 2019 | USA/hospital | To describe the process of implementing and developing a falls prevention programme aimed at decreasing falls and improving patient safety by including patients in their care | Used the plan, do, study, act model implementation period from 10 June 2014 to 31 May 2015 | CONSULTATION | The rate of falls decreased (71%) from 8.06 to 3.18. The average number of falls decreased from 4 to 1.7. The length of stay also decreased, meaning that the cost to the hospital decreased | *Staff commitment, *dedicated falls prevention role, *video monitoring to reduce falls, *cost reduction due to decreased falls | *Communication with patients about their involvement in the project— patients were unaware that they were involved in the falls prevention project |
| ‘Partnering with the Patient’ had 4 parts: (1) Engaging the patient. (2) Communicating fall safety goals. (3) Enquiring about safety concerns. (4) Rewarding patients for not falling during their stay | ||||||||
| Seale et al. 36 | 2015 | AUS/hospital | The purpose of the pilot study was to test hospital patients' acceptance of a new enabling tool designed to increase patient awareness and participation in the prevention of healthcare‐associated infections (HCAIs) | Nineteen questions survey conducted two times: At baseline and after discharge (n = 60) | PARTNERSHIP | Participants more likely to ask a factual question than challenge staff about hand hygiene—more likely to challenge staff when more informed; three patients asked staff about hand washing after the intervention | *Being informed about infection control, *importance of verbally delivering the messages rather than just providing written material | *Baseline survey measured intention—this does not always = behaviour, *need empowerment messages only in languages other than English |
| Empowerment tools, a Flip chart and a brochure with information about HCAI and the role that the patient plays in preventing them | ||||||||
| Silkworth et al. 37 | 2016 | USA/hospital/hospital | Describe a staff‐driven quality improvement initiative to develop a video in partnership with patients and families to prevent falls when hospitalized. Engaging patients and their families in a ‘2‐way conversation’ about how they can participate in meeting a mutual goal rather than by one‐sided education | Data collected via EMR about patient response | CONSULTATION | Falls rates have decreased by 29.4% since the release of the video—other measures were implemented simultaneously—for example, hourly rounds and a broader focus on falls prevention‐ attributable to patient engagement | *Learning style | Not identified |
| Mandatory video about falls to increase interaction between patients and staff about falls | ||||||||
| van Gaal et al. 39 | 2011 | The Netherlands/hospital and aged care | To test SAFE or SORRY programme impact on AEs related to ulcers, UTIs and falls | Patient file review, AE data and weekly inspection of patients' skin. A total of 1081 in the intervention group (n = 1081) and 1120 usual care in hospital (n = 1120). A total of 196 intervention and usual care (nursing home (n = 3045) | CONSULTATION | Implementation of multiple guidelines simultaneously is possible. Patients in the intervention groups developed 43% and 33% fewer adverse events compared to the usual care groups in hospitals and nursing homes, respectively | *Tailored education patient involvement and feedback dealing with multiple potential AEs at the same time, *using an approach with many different elements | *Underreporting |
| Consisted of education, feedback through a computerized registration programme and an implementation plan for every ward | ||||||||
| Watt et al. 54 | 2020 | Canada/primary healthcare | Help prevent medication‐related failures and manage opioid use | Feedback was gathered from services (n = 200), and opioid study patient survey (n = 127) | PARTNERSHIP | The tool enables patients and families to start a conversation about medication. In conjunction with other strategies, researchers noted increased patient education and decreased use of opioids | *Engaged health services. *Further evaluation, *empowered patients, *collaboration | *Limited service/practitioner engagement |
| Patients were empowered to ask 5 specific questions about medication for use, staff training and standardized electronic prescribing |
Note: Baker et al. 52 reported on three strategies; two fulfilled the inclusion criteria for this review.
Consultation: In the context of Carman et al.'s 10 framework, nine strategies summarized in Table 1 conceptualize engagement as consultation. What is distinct in this phase of engagement is that patients were consulted, or invited to provide input, about a specific safety issue/s within parameters of engagement set by health practitioners.
Four strategies involved staff‐initiated engagement about a specific treatment or potential adverse event. Kim et al. 44 describe how direct questioning by staff to patients about the site of their X‐ray at an orthopaedic clinic in Korea led to a significant decrease in X‐ray site errors. Bergal et al. 40 describe a similar strategy implemented to reduce wrong‐site surgery in the United States of America with less definitive findings, primarily due to few incidents of wrong‐site surgery. van Gaal et al. 39 described a programme focused on reducing poor outcomes by staff providing education and opportunity for engagement in three areas (ulcers, urinary tract infections and falls) in 10 wards across four hospitals and aged care facilities in the Netherlands. 39 Rochon and Salazar 42 described a four‐stage falls reduction process implemented in medical/surgical wards in a USA hospital. Although both van Gaal et al. 39 and Rochon and Salazar 42 reported decreased falls and fewer adverse events, limited details about interactions between staff and patients were reported. These two interventions have been classified as consultation due to the focus on patient education and staff‐directed interaction. 39 , 42 One strategy sought to create engagement about a safety event by driving patient‐initiated contributions through a feedback mechanism: the Patient Reporting and Action for a Safe Environment (PRASE) Tool. PRASE was trialled in 33 wards across 5 UK hospitals, which demonstrated a decrease in preventable harm at the ward level. 50
Four strategies described staff adapting existing engagement tools to promote interaction by staff with patients in hospital settings and were relevant to this category due to the focus on patient education and staff‐directed interaction. 31 , 37 , 41 , 55 Silkworth et al. 37 developed a 5‐min video to encourage patients and their families to engage in a ‘2‐way conversation' about falls risks on admission, 37 and Opsahl et al. 41 added a video to an existing falls prevention strategy. Both studies were conducted in acute care hospitals in the United States of America and both reported decreased falls and positive findings about using video to engage patients. Similarly, Duckworth et al. 31 and Dykes et al. 55 evaluated the addition of a multimodal approach (laminated, electronic or bedside display) to present information of a person‐centred falls prevention plan (FallTIPS) in three large hospitals in the United States of America 31 , 54 (see Table 1 for effectiveness data).
Involvement: The involvement phase of engagement 10 indicates that patients were asked about their preferences and concerns, with the opportunity to interact and engage with practitioners about a specific health or treatment issue. This stage of engagement contains strategies devised by staff, offering opportunities for increased ongoing interaction between staff and patients that were not evident in strategies classified as consultation. Six strategies sought to enhance safety by involving patients (Table 1).
Only one strategy in the involvement phase of the continuum was related to face‐to‐face interactions between staff and patients, reporting on a strategy used in an outpatient interventional radiology clinic in the Netherlands. 45 Clinic patients were invited to attend an additional appointment before their interventional radiology visit to discuss their queries and concerns about the procedure, risk and consent, hence the classification as involvement. This strategy enhanced the relationship between the practitioner and the patient, led to increased informed consent and a reduction in deviations from process (Table 1). Two further online strategies were used to facilitate communication between patients and health practitioners 35 , 38 about specific areas of care. de Jong et al. 38 evaluated an online medication reconciliation and Heyworth reported on a similar pilot study of recently discharged patients from a USA veterans' hospital and reported that patients notified staff of medication discrepancies with potential for significant adverse reactions.
Three online feedback strategies provided an opportunity for patients to raise issues and interact with staff about safety concerns across their care experience. All three studies were hospital based and conducted in the United States of America. 32 , 33 , 52 Bell et al. 53 reported on the efficacy of open notes with a feedback tool, 53 Gerard et al. 33 explored patient experiences using electronic notes viewable by patients in a hospital setting 33 and Grossman et al. 34 reported on portals as a mode to engage with patients about safety. All papers reported positive findings in relation to opportunities for patients to raise concerns, although detailed data were not available about the impact of portals on safety outcomes (see Table 1).
Partnership/leadership: Strategies that create a partnership between healthcare providers and patients are at the endpoint of the continuum of engagement. 10 Almost half of the strategies (12) sought to provide patients with the opportunity to raise concerns about their treatment and ‘work’ with practitioners to improve the safety of their care and treatment, often with strategies using person‐centred tools or designed to empower patients to alert practitioners of concerns. 30 , 32 , 36 , 43 , 46 , 47 , 48 , 49 , 51 , 52 , 54 Although all strategies in this classification enhance partnership, only six strategies included patients in the inception, design or evaluation of strategies. 46 , 47 , 48 , 49 , 52 , 54
Of the range of strategies included, six described collaboratively developed tools 46 , 47 , 48 , 49 , 52 , 54 and processes designed to encourage and facilitate patient communication and feedback. All six studies reported positive impacts on patient safety, including decreased adverse events and increased identification of errors that would have resulted in harm (see Table 1). Four of the six strategies were ‘bedside’ tools collaboratively developed with patients designed to enhance quality and included ‘safety’ as one of many goals. 46 , 47 , 48 , 52 Dykes et al. 46 evaluated a suite of strategies implemented in two medical intensive care units in the United States of America. 46 Khan et al. 48 reported on a patient‐centred project implemented in medical paediatric wards at one Canadian and six US teaching hospitals. Transforming care at the bedside (TCAB) is a codesigned bedside checklist designed to enable families to provide real‐time feedback on various quality measures, including safety, implemented the TCAB in 19 units at 6 hospitals in Montreal, Canada. 52 Family‐centred rounds evaluated in four US paediatric hospital sites used a similar approach to the strategies described above, concluding that patient‐centred engagement is effective for identifying patient safety concerns. 47 A bedside safe‐outcomes reporting tool was collaboratively developed to enable patients to measure risk and raise unsafe care issues in an inpatient paediatric renal ward in a United Kingdom. 49 The tool was pictorial for ease of use and patients recorded concerns as issues arose; this led to an increase in critical incident reporting by staff. The Fracture Recovery for Seniors at Home (FReSH START Toolkit) was collaboratively developed by staff, patients and their families and highlighted the value of collaboration with patients and caregivers in preventing complications. 52
Three partnership or leadership strategies sought to empower patients to take responsibility for specific elements in their care as inpatients, although they did not report patient involvement in the design or inception of the strategy. 36 , 51 , 54 Seale et al. 36 report on the use of a flip chart and brochure with the aim of empowering healthcare consumers to take responsibility for safety, and alert staff to hygiene issues in an Australian hospital. Watt et al. 54 report on a Canadian strategy implemented in 200 community and inpatient healthcare settings that encouraged patients to ask five questions. The aim was to decrease medication errors and the paper reported on a study that showed the impact of this intervention on opioid use. Campbell et al. 51 reported on a strategy implemented in paediatric intensive care units in Hanoi, Vietnam. The strategy described was a bedside tool to encourage patients to remind staff to wash their hands (see Table 1 for effectiveness data).
The final three strategies of the 12 in this group were designed to assist patients to highlight issues at various points of direct care. A Norwegian developed online tool enabled improved communication between breast cancer patients and multiple practitioners, including communications about medications, and treatment. 43 The strategy progressed other strategies by providing patients with opportunities to clarify issues at a time of their choosing. Two studies highlighted the benefits of patient‐held medication information. 29 , 31 Garfield et al. 32 evaluated medication reconciliation tools used by people who access primary and secondary healthcare organisations in greater London, UK, and noted the benefits of using patient‐held medication management tools in various formats. Similar conclusions were reached by Buning et al. 30 in their proof‐of‐concept study exploring a mobile application for medication reconciliation in a Netherlands hospital. These three studies reinforced the need for flexibility and benefits of patient‐managed tools that span various healthcare providers and agencies to increase safety when care spans various sites.
3.1.2. What types of patients and contexts are described in the interventions?
The included studies were predominantly conducted in inpatient settings (13 studies) or after discharge from inpatient stay (10); the remainder were conducted in outpatient clinics or community settings, including an aged care facility (4). Twenty‐four studies were conducted in countries classified as ‘developed’ by the United Nations, 25 studies in countries classified as high income and one developing economy. 51 Participants were most often recruited from university or teaching hospitals (22), predominantly city based (17), and in the United States of America (13). Twenty‐five studies recruited male and female participants; one study recruited only women. 43 Participant characteristics and demographic information were reported with varying levels of detail; all studies recruited participants over 16. Information about culture and ethnicity was variable, and only eight papers provided data about culture and language preferences. 31 , 32 , 36 , 46 , 47 , 48 , 50 , 53 No papers reported on any other diverse communication needs.
In 24 papers, engagement approaches were available to all eligible patients. Three papers excluded participants not from dominant language groups for methodological reasons. 36 , 45 , 50 In the remaining papers, participation was open to all; however, people who opted to participate were often identified as well‐educated, 33 insured and 35 , 46 computer literate 35 , 46 and tended to be from the dominant language group.
Safety engagement strategies described were only available in the dominant language in 19 papers. 16 , 30 , 32 , 33 , 35 , 38 , 39 , 41 , 42 , 43 , 44 , 45 , 46 , 51 , 52 , 53 , 54 , 55 Two papers reported constrained resource‐limited adaptation of information to meet diverse needs of patients, identifying the absence of key groups as a study limitation. 36 , 50 Six papers contained commentary about the suitability of tools for CALD communities, noting that more older non‐Caucasian patients accessed the Open‐notes tool than anticipated, 53 the benefits of a visual tool 49 , 51 and highlighting the need for alternative or adapted strategies. 36 , 40 , 47 , 48 , 49
The question of the effectiveness of strategies ‘for whom’ is central to realist synthesis. The included studies are robust; however, they also have insufficient data to determine the extent to which vulnerable or minority groups were represented. The combination of limited socio‐cultural data and a lack of description of how engagement tools were adapted or used means that the effectiveness of strategies for patients from CALD communities or other vulnerable groups is difficult to ascertain.
3.1.3. What are the mechanisms that influence the effectiveness of consumer engagement approaches in enhancing safe care and treatment?
The included studies were examined to articulate common factors identified as influencing the success of strategies to engage healthcare consumers in the delivery of safe care and treatment. Acknowledging the limited data about the inclusion of diverse participant groups (see Q2 and Table 1), four common factors were evident.
Patient–professional collaboration: Strategies across the continuum of engagement reported the value of opportunities for staff and patients to establish communication, 47 form partnerships 37 and emphasized the value of the ‘relationship’. 45 These findings are reflective of the evidence that underpins person/patient‐centred approaches. 56 Some staff participants thought that collaborating with patients about safety could have unintended negative consequences for the practitioner/patient relationship. 41 , 53
Pragmatic and user‐friendly: Ten strategies emphasize the need for simple feedback systems about safety features that are not time consuming, 49 use plain language, 48 not solely reliant on text 49 , 51 and can be incorporated into existing documentation systems, interactions or portals. 29 , 43 Electronic portals and apps need a user‐friendly interface 38 and focus on relevant safety concerns. 34 , 35 Questionnaires were time consuming and not suited to varied communication needs 49 or distressed patients. 50
Promoting confidence and safety proactively: The benefit of increasing patient confidence or empowering patients underpinned the implementation success of the interventions across the continuum of engagement. 30 , 36 , 37 , 49 , 51 , 54 The advantages of a proactive approach to enhance safe care were emphasized, 49 , 51 , 54 , 55 along with the need for cultural awareness and sensitivity. 51
Organisational sponsorship: All papers identify the need for an organisational culture that supports transparency and values health consumer input. Staff training, ongoing commitment of resources including practical adjustment of schedules, 37 , 39 , 41 , 42 , 48 , 51 , 54 staff consistency, 44 systematic/whole of agency approach 48 and management support 31 , 46 , 52 were identified as vital for consumer engagement interventions to be implemented effectively.
4. DISCUSSION
Our findings identified 27 strategies that used interactive technologies, dedicated additional appointments and verbal communication prompts to engage patients in ensuring safe care and treatment during direct care. Multimodal strategies were also used in several studies. Most of the strategies were implemented in inpatient settings. The strategies were predominantly evaluated in locations characterized by a significant cultural shift towards patient partnership. The included papers were largely from America (13), Northern Europe (3) and the United Kingdom (3).
The nature of engagement across the strategies spanned the patient engagement classifications of consultation (nine strategies), involvement (seven strategies) and partnership (twelve strategies). 10 Working in partnership with patients and families is central to devising suitable engagement approaches for specific populations or settings. 10 It was notable that publications provided varied levels of detail in data about the type and degree of patient engagement in strategy development or implementation. In some instances, researchers identified limited inclusion of diverse patients as an issue to address; however, it was difficult for researchers to ascertain whether it was the patient engagement strategy or research data collection tools that precluded engagement. 32 , 38 , 45 While some papers included details about codesigning strategies with patients, 46 , 47 , 48 , 49 , 52 , 54 this aspect of engagement is most often absent, undefined or unreported. Insufficient information about such elements as the patient role in strategy design reflected limited evidence that the strategies described were theoretically informed. Lawton et al. 50 provided a theoretical background to engagement; similarly, the patient‐centred strategies embedded engagement in such approaches. 46 , 47 , 48 However, the theoretical justification for strategy design presented in most papers was on content (e.g, falls prevention or wrong‐site intervention), technical production (e.g., videos 37 ) or staff implementation, 41 , 43 rather than on the nature or details of engagement.
Attributing changes in patient safety outcomes to a particular type of patient engagement was challenging due to the variation in the definition of engagement in the included papers, which is reflected in the wider literature. 10 Lack of consistency in defining ‘engagement’, coupled with limited details about strategy implementation and participant characteristics, created challenges in understanding the types of engagement strategies that work to achieve particular outcomes in particular populations or contexts of care. These shortcomings have been recognized in the literature, with Lawton et al. 50 concluding that the widely used practice of using adverse events reporting data to ascertain the impact of specific engagement strategies is unsuitable. Similarly, Wright et al. 5 highlight the challenges to measuring the impact of patient engagement strategies on safety and call for more detailed analysis of engagement.
Knowledge of intervention effectiveness, acceptability and feasibility is critical in the context of emerging evidence of both increased risk of safety events and barriers to engagement for particular patient groups. The needs of patients from ethnic minority backgrounds 23 , 57 and disability 24 , 58 have been highlighted in recent reviews. 21 There is emerging literature about the advantage of animation‐ or picture‐based communication for various patient groups including people from ethnic minority backgrounds or with disabilities; 59 , 60 yet, only two included papers incorporated visuals to accompany text. 48 , 50 While brief commentary about the effectiveness of specific strategies for people from different ethnic backgrounds and the impact of lower health literacy was made, addressing the needs of diverse participant groups was not a focus of the papers reviewed. Our review therefore identified a need for strategies developed and evaluated with consideration of and input from diverse patient population groups, along with evidence of their effectiveness for people from different ethnic backgrounds, age groups, disability status and other critical patient characteristics.
Patient–professional collaboration, user‐friendly strategies, proactive messaging and agency sponsorship were all recognized as enablers of patient engagement. Findings regarding the facilitators of patient engagement between papers in this review were consistent, confirming recent research seeking to empower patients to raise safety issues within a supportive culture. 15 , 16 , 22 , 61 , 62 The importance of agency sponsorship of a collaborative culture for engagement has long been emphasized in the change management and person‐centred care literature. 63 Staff identified that agency support is required to address the potential impact of engagement on the patient/provider relationship and workload. 34 These concerns are reflective of Park et al.'s 8 systematic review, which found that staff were aware of the importance of engaging in safety, but were not always confident to do so. A comprehensive approach including a culture of transparency, collaboration and support to implement evidence‐based engagement strategies is required. 62 , 64
4.1. Implications
Patient engagement interventions are being deployed across health services to promote patient safety despite vast variations in the definitions and conceptualisation of the concept of patient engagement. Few studies have utilized theory‐informed approaches or robust study designs to evaluate current techniques.
There are implications for health services in the challenges posed to scaling and spreading the adoption of potentially useful patient engagement strategies. There is a danger of unintended harmful impacts for those for whom the intervention may not be suitable. There are resource, financial and ethical implications, given the additional time and technologies required by patients and staff to take part in such interventions. This review reinforces the need for a multifaceted approach to patient engagement, incorporating agency culture, practices and appropriate engagement strategies. 9
Therefore, researchers need to work collaboratively with health services to establish more robust evidence of (a) what the intervention mechanisms are in current strategies and (b) information about (1) the feasibility and acceptability of the strategies for all parties, (2) the end‐users and (3) cost‐effectiveness.
4.2. Strengths and limitations
The capacity to explore varied engagement strategies by using a realist synthesis supported by Carman et al.'s 10 engagement framework provided scaffolding for the review. Use of Carman et al.'s 10 framework was useful in light of the varied definitions of patient engagement evident in the included papers and the broader literature. Similarly, use of realist synthesis enabled comparison across a disparate group of studies of varying quality and synthesis of information to influence practice.
The findings of this review must be understood in the context of the limitations of the included studies. We identified limited geographical diversity in the countries where the research originated and a lack of studies that sought to compare groups, or samples that were sufficiently powered. By including only published material, valuable insight from nonpublished and nonempirical work may have been missed. 65 An additional limitation arises from the wide range of terms used to describe patient engagement in safety and the many different types of journals used to house patient safety research. The lack of evidence regarding the theoretical underpinning of the interventional approaches and their intended impact on patient engagement creates barriers to determining the intervention mechanism/s responsible for identified changes. The diverse purposes of papers included also created challenges, particularly papers that reported on a single element of a bigger project, multiple interventions across several sites or safety outcomes reported among a number of interventions carried out simultaneously. The levels of sensitivity and precision of bibliographic databases vary and can also affect the number of articles returned. We used several databases in addition to manual searching to broaden coverage, but there may have been omissions.
5. CONCLUSION
Despite the growing number of patient‐centred tools and safety engagement strategies, evidence about use and effectiveness is limited. More details about how they are used and with whom are required to enable patients and practitioners to engage effectively. More clarity is needed to consistently define patient engagement along with further research to determine which strategies are effective. Little evidence exists about people from minority or vulnerable backgrounds in patient safety, which needs to be addressed due to acknowledged disparities in healthcare safety and engagement.
CONFLICT OF INTERESTS
The authors declare that there are no conflicts of interest.
AUTHOR CONTRIBUTIONS
Reema Harrison and the CanEngage project team conceived the study. Stephen Mears completed the database search. Two reviewers (Jiadai Li, Benjamin Jones) completed the initial title and abstract review, followed by an independent screening by a third reviewer (Bronwyn Newman). The inclusion criteria were then independently applied to full‐text articles by two reviewers (Bronwyn Newman, Reema Harrison), with disagreements or uncertainty resolved through discussion. Quality was assessed by two reviewers (Bronwyn Newman, Kathryn Joseph). Bronwyn Newman completed writing of the manuscript. Reema Harrison, Holly Seale, Elizabeth Manias, Merrilyn Walton, Ashfaq Chauhan and Kathryn Joseph provided feedback during analysis and reporting and reviewed the manuscript.
Supporting information
Supporting information.
Supporting information.
ACKNOWLEDGEMENTS
The authors would like to acknowledge the support of the CanEngage Project group: Monika Latanik, Dr. Ramesh Walpola, Dr. Éidín Ní Shé, Mrs Thit Tieu, Dr. Allan (Ben) Smith, Dr. Desiree Leone, Professor Afaf Girgis and Professor Carlene Wilson. This study was funded by the National Health and Medical Research Council (NHMRC) Ideas (APP1180925) grant and through Cancer Australia's Supporting people with cancer Grant initiative (CA‐1819/01). The content is solely the responsibility of the grant recipient and does not necessarily represent the official views of Cancer Australia.
Newman B, Joseph K, Chauhan A, et al. Do patient engagement interventions work for all patients? A systematic review and realist synthesis of interventions to enhance patient safety. Health Expect. 2021;24:1905‐1923. 10.1111/hex.13343
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available in the Supporting Information Material of this article.
REFERENCES
- 1. Unruh KT, Pratt W. Patients as actors: the patient's role in detecting, preventing, and recovering from medical errors. Int J Med Inform. 2006;76:S236‐S244. 10.1016/j.ijmedinf.2006.05.021 [DOI] [PubMed] [Google Scholar]
- 2. Weingart SN, Zhu J, Chiappetta L, et al. Hospitalized patients' participation and its impact on quality of care and patient safety. Int J Qual Health Care. 2011;23(3):269‐277. 10.1093/intqhc/mzr002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Walton M. Patient safety—a view from down under. Qual Saf Health Care. 2009;18(6):422‐423. 10.1136/qshc.2009.037044 [DOI] [PubMed] [Google Scholar]
- 4. Adams RJ, Tucker G, Price K, et al. Self‐reported adverse events in health care that cause harm: a population‐based survey. Med J Aust. 2009;190(9):484‐488. 10.5694/j.1326-5377.2009.tb02523.x [DOI] [PubMed] [Google Scholar]
- 5. Wright J, Lawton R, O'hara J, et al. Improving patient safety through the involvement of patients: development and evaluation of novel interventions to engage patients in preventing patient safety incidents and protecting them against unintended harm. Programme Grants Appl Res. 2016;4(15):1–332. 10.3310/pgfar04150 [DOI] [PubMed] [Google Scholar]
- 6. Chaboyer W, Bucknall T, Webster J, et al. The effect of a patient centred care bundle intervention on pressure ulcer incidence (INTACT): a cluster randomised trial. Int J Nurs Stud. 2016;64:63‐71. 10.1016/j.ijnurstu.2016.09.015 [DOI] [PubMed] [Google Scholar]
- 7. Hwang J‐I, Kim SW, Chin HJ. Patient participation in patient safety and its relationships with nurses' patient‐centered care competency, teamwork, and safety climate. Asian Nurs Res. 2019;13(2):130‐136. 10.1016/j.anr.2019.03.001 [DOI] [PubMed] [Google Scholar]
- 8. Park M, Giap TTT. Patient and family engagement as a potential approach for improving patient safety: a systematic review. J Adv Nurs. 2020;76(1):62‐80. 10.1111/jan.14227 [DOI] [PubMed] [Google Scholar]
- 9. O'Hara JK, Lawton RJ. At a crossroads? Key challenges and future opportunities for patient involvement in patient safety. BMJ Qual Saf. 2016;25(8):565‐568. 10.1136/bmjqs-2016-005476 [DOI] [PubMed] [Google Scholar]
- 10. Carman KL, Dardess P, Maurer M, et al. Patient and family engagement: a framework for understanding the elements and developing interventions and policies. Health Aff. 2013;32(2):223‐231. 10.1377/hlthaff.2012.1133 [DOI] [PubMed] [Google Scholar]
- 11. Arnstein SR. A Ladder of citizen participation. J Am Plann Assoc. 2019;85(1):24‐34. 10.1080/01944363.2018.1559388 [DOI] [Google Scholar]
- 12. Schols AMR, Dinant G‐J, Hopstaken R, Price CP, Kusters R, Cals JWL. International definition of a point‐of‐care test in family practice: a modified e‐Delphi procedure. Fam Pract. 2018;35(4):475‐480. 10.1093/fampra/cmx134 [DOI] [PubMed] [Google Scholar]
- 13. An J, Kim SJ, Park S, Moon KT, Park EC. The effects of patient education on patient safety: can we change patient perceptions and attitudes? Lessons from the Armed Forces Capital Hospital in Korea. Int J Qual Health Care. 2017;29(3):392‐398. 10.1093/intqhc/mzx037 [DOI] [PubMed] [Google Scholar]
- 14. Schwappach DLB, Frank O, Buschmann U, Babst R. Effects of an educational patient safety campaign on patients' safety behaviours and adverse events. J Eval Clin Pract. 2013;19(2):285‐291. 10.1111/j.1365-2753.2012.01820.x [DOI] [PubMed] [Google Scholar]
- 15. Grota PG, Eng T, Jenkins CA. Patient motivational dialogue: a novel approach to improve hand hygiene through patient empowerment in ambulatory care. Am J Infect Control. 2020;48(5):573‐574. 10.1016/j.ajic.2019.11.024 [DOI] [PubMed] [Google Scholar]
- 16. Seale HP, Chughtai AAP, Kaur RMPH, Phillipson LP, Novytska Y, Travaglia JP. Empowering patients in the hospital as a new approach to reducing the burden of health care‐associated infections: the attitudes of hospital health care workers. Am J Infect Control. 2015;44(3):263‐268. 10.1016/j.ajic.2015.10.003 [DOI] [PubMed] [Google Scholar]
- 17. Davis R, Murphy MF, Sud A, et al. Patient involvement in blood transfusion safety: patients' and healthcare professionals' perspective. Transfus Med. 2012;22(4):251‐256. 10.1111/j.1365-3148.2012.01149.x [DOI] [PubMed] [Google Scholar]
- 18. Davis RE, Sevdalis N, Pinto A, Darzi A, Vincent CA. Patients' attitudes towards patient involvement in safety interventions: results of two exploratory studies. Health Expect. 2013;16(4):e164‐e176. 10.1111/j.1369-7625.2011.00725.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Pinto A, Vincent C, Darzi A, Davis R. A qualitative exploration of patients' attitudes towards the ‘participate inform notice know’ (pink) patient safety video. Int J Qual Health Care. 2013;25(1):29‐34. 10.1093/intqhc/mzs073 [DOI] [PubMed] [Google Scholar]
- 20. Seale H, Travaglia J, Chughtai AA, Phillipson L, Novytska Y, Kaur R. ‘I don't want to cause any trouble’: the attitudes of hospital patients towards patient empowerment strategies to reduce healthcare‐acquired infections. J Infect Prev. 2015;16(4):167‐173. 10.1177/1757177415588378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sharma AE, Rivadeneira NA, Barr‐Walker J, Stern RJ, Johnson AK, Sarkar U. Patient engagement in health care safety: an overview of mixed‐quality evidence. Health Aff. 2018;37(11):1813‐1820. 10.1377/hlthaff.2018.0716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bombard Y, Baker GR, Orlando E, et al. Engaging patients to improve quality of care: a systematic review. Implement Sci. 2018;13(1):98. 10.1186/s13012-018-0784-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chauhan A, Walton M, Manias E, et al. The safety of health care for ethnic minority patients: a systematic review. Int J Equity Health. 2020;19(1):118. 10.1186/s12939-020-01223-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mimmo L, Harrison R, Hinchcliff R. Patient safety vulnerabilities for children with intellectual disability in hospital: a systematic review and narrative synthesis. BMJ Paediatr Open. 2018;2(1):e000201. 10.1136/bmjpo-2017-000201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Pawson R. The Science of Evaluation: A Realist Manifesto. SAGE; 2013. [Google Scholar]
- 26. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred Reporting Items for Systematic Reviews and Meta‐Analyses: the PRISMA statement. BMJ. 2009;339(7716):332‐336. 10.1136/bmj.b2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Harrison R, Jones B, Gardner P, et al. Quality assessment with diverse studies (QuADS): an appraisal tool for methodological and reporting quality in systematic reviews of mixed‐ or multi‐method studies. BMC Health Serv Res. 2021;21:144. 10.1186/s12913-021-06122-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Gisev N, Bell JS, Chen TF. Interrater agreement and interrater reliability: key concepts, approaches, and applications. Res Soc Adm Pharm. 2013;9(3):330‐338. 10.1016/j.sapharm.2012.04.004 [DOI] [PubMed] [Google Scholar]
- 29. Dalkin SM, Greenhalgh J, Jones D, Cunningham B, Lhussier M. What's in a mechanism? Development of a key concept in realist evaluation. Implement Sci. 2015;10:49. 10.1186/s13012-015-0237-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Buning AW, Klopotowska JE, Duyvendak M, Engelen L, Arts J. Patient empowerment through provision of a mobile application for medication reconciliation: a proof of concept study. BMJ Innov. 2016;2(4):152‐157. 10.1136/bmjinnov-2015-000110 [DOI] [Google Scholar]
- 31. Duckworth M, Adelman J, Belategui K, et al. Assessing the effectiveness of engaging patients and their families in the three‐step fall prevention process across modalities of an evidence‐based fall prevention toolkit: an implementation science study. J Med Internet Res. 2019;21(1):2. 10.2196/10008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Garfield S, Furniss D, Husson F, et al. How can patient‐held lists of medication enhance patient safety? A mixed‐methods study with a focus on user experience. BMJ Qual Saf. 2020;29(9):764‐773. 10.1136/bmjqs-2019-010194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Gerard M, Fossa A, Folcarelli PH, Walker J, Bell SK. What patients value about reading visit notes: a qualitative inquiry of patient experiences with their health information. J Med Internet Res. 2017;19(7):1‐9. 10.2196/jmir.7212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Grossman LV, Choi SW, Collins S, et al. Implementation of acute care patient portals: recommendations on utility and use from six early adopters. J Am Med Inform Assoc. 2018;25(4):370‐379. 10.1093/jamia/ocx074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Heyworth L, Paquin AM, Clark J, et al. Engaging patients in medication reconciliation via a patient portal following hospital discharge. J Am Med Inform Assoc. 2014;21(e1):e157‐e162. 10.1136/amiajnl-2013-001995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Seale H, Chughtai AA, Kaur R, et al. Ask, speak up, and be proactive: Empowering patient infection control to prevent health care‐acquired infections. Am J Infect Control. 2015;43(5):447‐453. 10.1016/j.ajic.2015.01.007 [DOI] [PubMed] [Google Scholar]
- 37. Silkworth AL, Baker J, Ferrara J, Wagner M, Gevaart M, Morin K. Nursing staff develop a video to prevent falls: a quality improvement project. J Nurs Care Qual. 2016;31(1):40‐45. 10.1097/NCQ.0000000000000135 [DOI] [PubMed] [Google Scholar]
- 38. de Jong CC, Ros WJG, van Leeuwen M, Schrijvers G. Exploring the effects of patients taking a vigilant role in collaborating on their e‐medication administration record. Int J Med Inform. 2016;88:18‐24. 10.1016/j.ijmedinf.2016.01.001 [DOI] [PubMed] [Google Scholar]
- 39. van Gaal BG, Schoonhoven L, Mintjes JA, et al. Fewer adverse events as a result of the SAFE or SORRY? programme in hospitals and nursing homes. Part I: primary outcome of a cluster randomised trial. Int J Nurs Stud. 2011;48(9):1040‐1048. 10.1016/j.ijnurstu.2011.02.017 [DOI] [PubMed] [Google Scholar]
- 40. Bergal LM, Schwarzkopf R, Walsh M, Tejwani NC. Patient participation in surgical site marking: can this be an additional tool to help avoid wrong‐site surgery? J Pat Saf. 2010;6(4):221‐225. 10.1097/PTS.0b013e3181fd19ec [DOI] [PubMed] [Google Scholar]
- 41. Opsahl AG, Ebright P, Cangany M, Lowder M, Scott D, Shaner T. Outcomes of adding patient and family engagement education to fall prevention bundled interventions. J Nurs Care Qual. 2017;32(3):252‐258. 10.1097/ncq.0000000000000232 [DOI] [PubMed] [Google Scholar]
- 42. Rochon R, Salazar L. Partnering with the patient to reduce falls in a medical‐surgical unit. Int J Safe Pat Handl Mob. 2019;9(4):135‐142. [Google Scholar]
- 43. Ekstedt M, Borosund E, Svenningsen IK, Ruland CM. Reducing errors through a web‐based self‐management support system. Stud Health Technol Inform. 2014;201:328‐334. [PubMed] [Google Scholar]
- 44. Kim JY, Jung MG, Kwon MH, Noh SO, Kim HJ. Patient involvement in reducing errors during X‐ray imaging in an orthopedic outpatient clinic. J Eval Clin Pract. 2017;23(6):1227‐1231. 10.1111/jep.12764 [DOI] [PubMed] [Google Scholar]
- 45. Lutjeboer J, Burgmans MC, Chung K, van Erkel AR. Impact on patient safety and satisfaction of implementation of an outpatient clinic in interventional radiology (IPSIPOLI‐Study): a quasi‐experimental prospective study. Cardiovasc Intervent Radiol. 2015;14:543‐551. 10.1007/s00270-015-1069-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Dykes PC, Rozenblum R, Dalal A, et al. Prospective evaluation of a multifaceted intervention to improve outcomes in intensive care: the promoting respect and ongoing safety through patient engagement communication and technology study. Crit Care Med. 2017;45(8):e806‐e813. 10.1097/CCM.0000000000002449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Cox ED, Jacobsohn GC, Rajamanickam VP, et al. A family‐centered rounds checklist, family engagement, and patient safety: a randomized trial. Pediatrics. 2017;139(5):12. 10.1542/peds.2016-1688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Khan A, Spector ND, Baird JD, et al. Patient safety after implementation of a coproduced family centered communication programme: multicenter before and after intervention study. BMJ. 2018;363:k4764. 10.1136/bmj.k4764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Lachman P, Linkson L, Evans T, Clausen H, Hothi D. Developing person‐centred analysis of harm in a paediatric hospital: a quality improvement report. BMJ Qual Saf. 2015;24(5):337‐344. 10.1136/bmjqs-2014-003795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Lawton RJ, Sheard L, O'Hara J. Can patient involvement improve patient safety? A cluster randomized control trial of the Patient Reporting and Action for a Safe Environment (PRASE) intervention. Int J Qual Health Care. 2016;28:21. 10.1093/intqhc/mzw104.29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Campbell JI, Pham TT, Le T, et al. A family empowerment strategy is associated with increased healthcare worker hand hygiene in a resource‐limited setting. Infect Control Hosp Epidemiol. 2020;41(2):202‐207. 10.1017/ice.2019.312 [DOI] [PubMed] [Google Scholar]
- 52. Baker GR, Fancott C, Judd M, O'Connor P. Expanding patient engagement in quality improvement and health system redesign. Healthc Manage Forum. 2016;29(5):176‐182. 10.1177/0840470416645601 [DOI] [PubMed] [Google Scholar]
- 53. Bell SK, Gerard M, Fossa A, et al. A patient feedback reporting tool for OpenNotes: implications for patient‐clinician safety and quality partnerships. BMJ Qual Saf. 2017;26(4):312‐322. 10.1136/bmjqs-2016-006020 [DOI] [PubMed] [Google Scholar]
- 54. Watt A, Murray M, Herold D, Hyland S, Hoffman C, Cass M. Empowering patients: 5 questions to ask about your medications. Healthc Q. 2020;22(SP):58‐71. 10.12927/hcq.2020.26046 [DOI] [PubMed] [Google Scholar]
- 55. Dykes PC, Burns Z, Adelman J, et al. Evaluation of a patient‐centered fall‐prevention tool kit to reduce falls and injuries: a nonrandomized controlled trial. JAMA Netw Open. 2020;3(11):e2025889. 10.1001/jamanetworkopen.2020.25889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Håkansson Eklund J, Holmström IK, Kumlin T, et al. “Same same or different?” A review of reviews of person‐centered and patient‐centered care. Patient Educ Couns. 2019;102(1):3‐11. 10.1016/j.pec.2018.08.029 [DOI] [PubMed] [Google Scholar]
- 57. Johnstone M‐J, Kanitsaki O. Engaging patients as safety partners: some considerations for ensuring a culturally and linguistically appropriate approach. Health Policy. 2008;90(1):1‐7. 10.1016/j.healthpol.2008.08.007 [DOI] [PubMed] [Google Scholar]
- 58. Iacono T, Bigby C, Unsworth C, Douglas J, Fitzpatrick P. A systematic review of hospital experiences of people with intellectual disability. BMC Health Serv Res. 2014;14(1):505. 10.1186/s12913-014-0505-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Backman C, Stacey D, Crick M, Cho‐Young D, Marck PB. Use of participatory visual narrative methods to explore older adults' experiences of managing multiple chronic conditions during care transitions. BMC Health Serv Res. 2018;18(1). 10.1186/s12913-018-3292-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. See L‐C, Chang Y‐H, Chuang K‐L, et al. Animation program used to encourage patients or family members to take an active role for eliminating wrong‐site, wrong‐person, wrong‐procedure surgeries: preliminary evaluation. Int J Surg. 2011;9(3):241‐247. 10.1016/j.ijsu.2010.11.018 [DOI] [PubMed] [Google Scholar]
- 61. Elger BM, Esparaz JR, Nierstedt RT, Jennetten RC, Aprahamian CJ, Pearl RH. Engaging the patient and family in the surgical safety process utilizing. J Pediatr Surg. 2020;55(4):597‐601. 10.1016/j.jpedsurg.2019.06.012 [DOI] [PubMed] [Google Scholar]
- 62. Stewart GL, Manges KA, Ward MM. Empowering sustained patient safety the benefits of combining top‐down and bottom‐up approaches. J Nurs Care Qual. 2015;30(3):240‐246. 10.1097/ncq.0000000000000103 [DOI] [PubMed] [Google Scholar]
- 63. Dubrovsky AS, Bishop A, Biron A, et al. “We Should Talk”—moving knowledge into action by learning to engage patients, families, and healthcare staff to communicate for patient safety. Healthc Manage Forum. 2016;29(4):141‐145. 10.1177/0840470416641119 [DOI] [PubMed] [Google Scholar]
- 64. Knowles S, Hays R, Senra H, et al. Empowering people to help speak up about safety in primary care: using codesign to involve patients and professionals in developing new interventions for patients with multimorbidity. Health Expect. 2018;21(2):539‐548. 10.1111/hex.12648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Annie F, Neil M, Gabor S. Publication bias in the social sciences: unlocking the file drawer. Science. 2014;345(6203):1502‐1505. 10.1126/science.1255484 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.
Supporting information.
Data Availability Statement
The data that support the findings of this study are available in the Supporting Information Material of this article.


