Abstract
Background
Patient engagement in care is a priority and a key component of clinical practice. Different approaches to care have been introduced to foster patient engagement. There is a lack of a recent review on tools for assessing the main concepts and dimensions related to patient engagement in care.
Objective
Our scoping review sought to map and summarize recently validated tools for assessing various concepts and dimensions of patient engagement in care.
Search Strategy
A scoping review of recent peer‐reviewed articles describing tools that assess preferences in and experience with patient engagement in care was conducted in four databases (Ovid Medline, Ovid EMBASE, Cochrane Database of Systematic Reviews, CINAHL‐EBSCO). We adopted a broad definition based on the main concepts of patient engagement in care: patient‐centredness, empowerment, shared decision‐making and partnership in care.
Main Results
Of 2161 articles found, 16, each describing a different tool, were included and analysed. Shared decision‐making and patient‐centredness are the two main concepts evaluated, often simultaneously in most of the tools. Only four scales measure patient‐centredness, empowerment and shared decision‐making at the same time, but no tool measures the core dimensions of partnership in care. Most of the tools did not include patients in their development or validation or just consulted them during the validation phase.
Discussion and Conclusion
There is no tool coconstructed with patients from development to validation, which can be used to assess the main concepts and dimensions of patient engagement in care at the same time.
Patient and Public Contribution
This manuscript was prepared with a patient expert who is one of the authors. Vincent Dumez, who is a patient expert and codirector of the Center of Excellence on Partnership with Patients and the Public, has contributed to the preparation of the manuscript.
Keywords: clinical care, healthcare professionals, patient engagement, patients, scoping review, validated tools
1. INTRODUCTION
Patient engagement in health policies, healthcare planning and improvement and direct care is recognized as a cornerstone of quality and safety. 1 Engaging patients in care has become a priority and a key component of clinical practice in many countries around the world. 2 Evidence suggests that engaging patients can help (re)shape their care and treatment in ways that fit their needs and preferences, ultimately resulting in improved outcomes. 3 , 4 , 5 , 6 Over the last few decades, various approaches to care have been introduced in clinical practice to foster the integration of patient engagement into the delivery of healthcare.
In the 1990s, the patient‐centred care approach gradually replaced the medical paternalism that has dominated healthcare for decades. 7 The patient‐centred care model involves integrating patients' needs and preferences into the delivery of care, ‘moving away from a logic of “care to patients” towards one of “care for patients”’. 7 Patient‐centred care is based on a patient‐oriented perspective of care that includes what patients consider important for their life project. 7
In the last two decades, collaborative approaches have emerged, moving towards a logic of ‘care with patients’. For example, shared decision‐making encourages patients to take part in decisions on their care, 8 , 9 while self‐management or patient education approaches seek to strengthen patients' knowledge and skills to better empower them in their care process. 10 , 11 More recently, the ‘partnership in care’ approach has considered patients as full‐fledged members of healthcare teams. 12 This new model builds on aspects of each care approach, including the integration of patient needs and preferences into care delivery, the participation of patients in care decisions, the coconstruction of a care plan with them and the development of patients' capacities to manage their own care. 13 A previous empirical study on patient partnership from the patients‐as‐partners perspective was able to define partnership in care as the proactive efforts by patients to fill the gap between their preferences or expectations in the care relationship and what they experience during a consultation with a healthcare professional (HCP). 12
All these approaches to care are part of a continuum of engagement, from consultation to partnership in care, that reflects the increasingly important role played by patients in their own care. 1
As patient engagement in care has become a clinical standard in healthcare settings, a growing number of scales have been developed in recent decades for effective quality improvement. Previous reviews have identified, synthesized and appraised the tools used to assess some dimensions of care/approaches to care. A recent systematic review by Philipps et al. 14 focuses on studies published between 2005 and 2014 that described tools for assessing patient participation in healthcare. Their review only includes tools that measure approaches related to self‐management and decision‐making, without including tools that assess patient‐centred care. Conversely, a review by Ree et al. 15 synthetizes information on patient‐centred care tools, with a special focus on how patients are involved in the care. Lastly, a review by Jerofke‐Owen et al. 16 identifies and appraises tools that measure self‐reported patients' preferences in engagement, without considering tools that assess patient experience in engagement or HCPs' preferences in and experience with engaging patients. However, as patient engagement is part of the care relationship between patients and HCPs, it is important to identify the various tools used to assess both patients' and HCPs' preferences and experience in this area. In addition, the literature lacks a broad review of the recently validated scales used to assess the central dimensions on which the different approaches to care (from consultation to partnership in care) are based and that coexist in clinical practices.
The objective of this scoping review was therefore to map and summarize recently validated tools that assess patient engagement in care. To this end, several specific objectives were pursued: (1) to identify tools used to assess both patients' and HCPs' preferences in and/or experiences with patient engagement in care; (2) to summarize the evidence on recently validated tools that assess various concepts and dimensions of patient engagement in care; and (3) to report on various characteristics of scale development and validation (patient involvement, reliability of the scales).
2. METHODS
2.1. Conceptual framework
In this review, we adopted a broad definition of patient engagement in care that reflects the continuum of such engagement and the coexistence of different approaches to enhancing it. The definitions proposed here are based on Castro et al.'s 17 conceptual analysis of the main concepts related to patient engagement in care: patient‐centred care, empowerment and shared decision‐making. These concepts refer to different approaches to patient engagement in care, and together, they form the higher concept of partnership in care. According to Pomey et al., 18 the concept of partnership in care is an approach that considers the patient as ‘a caregiver of herself and, as such, a genuine member of the treatment team, endowed with competencies and limitations just like any other member of the team’. We believe that the concept of partnership can be summarized by all the dimensions on which each approach to care is based, 7 including individualized care, empathy, interpersonal trust, communication, experiential knowledge and self‐care. A summary of these concepts' definitions and dimensions is presented in Table 1.
Table 1.
Definitions of the main concepts related to patient engagement in care, adapted from Castro et al. 17
| Concept | Partnership in care main dimensions: Individualized care, empathy, interpersonal trust, communication, experiential knowledge and self‐care 7 | ||
|---|---|---|---|
| Patient centredness | Shared decision‐making | Empowerment | |
| Definition | ‘Biopsychosocial approach and attitude that aims to deliver care that is respectful and individualized. It implies the individual participation of the patient and is built on a relationship of mutual trust, sensitivity, empathy and shared knowledge’ 17 | ‘Patient's rights and opportunities to influence and engage in the decision‐making about his care through a dialogue attuned to his preferences, potential and a combination of his experiential and the professional's expert knowledge’ 17 | ‘Process that enables patients to exert more influence over their individual health by increasing their capacities to gain more control over issues they themselves define as important’ 17 |
| Main dimensions |
‐ Person‐centred care/climate ‐ Individualized care (considering needs, values and preferences) ‐ Empathy ‐ Therapeutic alliance ‐ Interpersonal trust |
‐ Shared decision‐making ‐ Patient–provider communication ‐ Experiential knowledge |
‐ Self‐care/self‐management ‐ Patient education ‐ Patient enablement ‐ Patient activation ‐ Experiential knowledge |
We used the continuum of patient involvement in research 18 to identify the level of patient involvement in tool development and validation. We considered three levels of involvement: (1) consultation of patients, which refers to asking for patients' input during the validation of the tool; (2) collaboration with patients, which corresponds to involving them in the selection and wording of items; and (3) partnership, which refers to coconstructing the tool with patients, from its development to its validation.
2.2. Review approach
We conducted a scoping review to map recent evidence on validated scales for assessing patient engagement in care. 19 We chose to conduct a narrative synthesis of the literature to describe the major characteristics of the tools, including the measurement objective, the concepts and dimensions assessed, the clinical context of utilisation and the development and validation characteristics of the tools. We followed the PRISMA extension for scoping reviews to apply a systematic approach when conducting the review and reporting the results. 20
2.3. Searches and screening
We searched for articles published between 2014 and 2021 in four major health and social science databases: Ovid MEDLINE, Ovid EMBASE, the Cochrane database of systematic reviews and EBSCO‐CINAHL. We decided to search for articles published starting from 2014 since a previous systematic review by Philipps et al. 14 searched for articles published from 2005 to 2013 that described tools for measuring patient participation in care. As Philips et al. 14 adopted a rather broad definition of patient engagement in care (shared decision‐making, self‐care and patients having self‐knowledge), we wanted to ensure that our review would not duplicate any previous reviews on this topic. The initial search was conducted on 19 January 2021. The search terms used are presented in Table 2. These correspond to the six major concepts searched for, related to patient, engagement, assessment, scale, clinical care and validation. Our search strategy was limited to published and peer‐reviewed literature and we did not conduct any searches in the grey literature. The search strategies developed for Ovid MEDLINE are available in File S1. The search strategies developed for the three other databases are available upon request. Two reviewers (N. C. and J. P.) independently screened articles based on their titles and abstracts. A pilot round was conducted with 50 references to verify the authors' (N. C. and J. P.) agreement on the inclusion and exclusion criteria before performing a full screening of the rest of the articles.
Table 2.
Search terms
| Patient | Engagement | Assessment | Scale | Clinical | Validation |
|---|---|---|---|---|---|
| Patient | Engagement | Assessment | Scale | Clinical care | Validation |
| User | Involvement | Measurement | Tool | Care | Psychometry |
| Client | Participation | Evaluation | Survey | Clinical level | Reliability |
| Centred care | Questionnaire | Validity | |||
| Shared decision‐making | Factor analysis | ||||
| Empowerment | |||||
| Self‐management | |||||
| Patient education | |||||
| Partnership | |||||
| Activation | |||||
| Enablement |
2.4. Inclusion and exclusion criteria
We included both original and review articles describing the development and validation of scales assessing patient engagement in adult inpatient or outpatient care. The inclusion and exclusion criteria are detailed in Table 3.
Table 3.
Inclusion and exclusion criteria
| Inclusion criteria | Exclusion criteria |
|---|---|
| Original or review articles describing the development and validation of scales assessing patient engagement in care | Published in a language other than English or French |
| Studies describing tools used in adult inpatient or outpatient care (all clinical settings) | Studies describing tools developed to be used with specific chronic or acute disease patients |
| Studies published between 2014 and 2021 | Studies describing tools used in paediatric care with children or adolescents |
| The reviewers could not access the full text (the authors were contacted, but did not respond) |
2.5. Extraction methods
Data from the included articles were charted on an extraction grid (File S2) according to the following categories: (1) the general presentation of the scales (e.g., first author, year of publication, title of the article and journal of publication), (2) the specific characteristics of the scales (e.g., name of the scale; measurement objective; patients', family members' or health professionals' perspective; preferences in or experience with patient engagement; context of utilisation; number of items; and scale measurement) and (3) the methodological aspects of tool development and validation (e.g., level of patient involvement in tool development or validation and reliability of the scale).
Furthermore, the extraction grid included Castro et al.'s 17 three main concepts related to patient engagement in care: (1) patient‐centred care, (2) empowerment and (3) shared decision‐making. One author (J. P.) classified each tool's main factors/dimensions or items according to the corresponding concepts, and a second author (N. C.) reviewed each component attribution.
3. RESULTS
3.1. Search results
Our initial search yielded a total of 2161 articles. After removing duplicates, a total of 2002 articles were screened. This process resulted in a total of 71 full‐text articles to be assessed for eligibility. One of them, a review of surveys for measuring patient‐centred care in the hospital setting, 21 included two tools published after 2014: the Family Inventory of Needs 22 and the Person‐Centred Climate Questionnaire‐Family Version (PCQ‐F). 23 Consequently, we have added the two articles corresponding to the development and validation of these tools to assess them against our full eligibility criteria. Following reviews of 73 full‐text articles, 16 articles fulfilled the inclusion criteria. The PRISMA flow diagram is shown in Figure 1.
Figure 1.
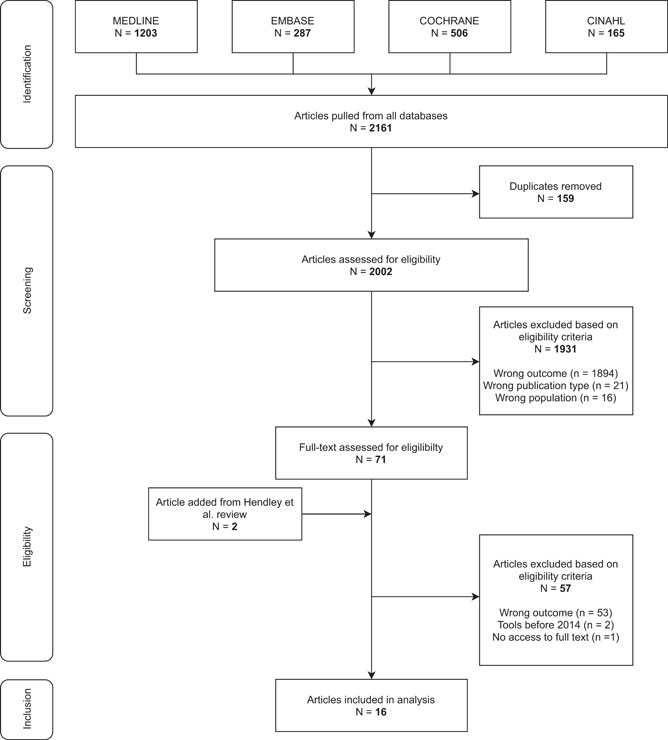
Flowchart of the study selection process
3.2. Study characteristics
We identified a total of 16 articles, representing 16 different tools, based on the eligibility criteria for assessing patient engagement in care. All the findings are presented in Tables 4 and 5. The data extraction table containing all the information that we extracted from the tools can also be accessed from File S2. The included studies were published between 2015 and 2020, and all use a quantitative design based on psychometric data analysis to describe the development and validation of tools assessing patient engagement in care. The studies were from eight different countries around the world: the United States (n = 5), China (n = 2), Denmark (n = 2), Italy (n = 2), Sweden (n = 2), Belgium (n = 1), the Netherlands (n = 1) and Taiwan (n = 1). The included studies were published in 12 different journals, some of which were represented more than once: the Journal of Advanced Nursing (n = 2), the Journal of Nursing Care Quality (n = 2), the Journal of Nursing Management (n = 2) and Patient Education & Counseling (n = 2). The scales contain between 9 and 55 items, most of which are rated on a five‐point Likert scale (56%, n = 9).
Table 4.
Tools included in the scoping review assessing the concepts and dimensions related to patient engagement in care (2014–2021)
| Author and year of publication Name of the scale | Perspective and preferences in or experience with care measured | Patient involvement in tool development | Patient involvement in tool validation | Concepts assessed |
|---|---|---|---|---|
| Berg et al. (2020) 24 | Patients' perspective, experience of engagement | No | Yes | Patient‐centredness, shared decision‐making |
| Patient Participation Questionnaire | ||||
| Casu et al. (2019) 25 | Patients' perspective, experience of engagement | Not reported | Not reported | Patient‐centredness, shared decision‐making |
| Patient–Professional Interaction Questionnaire | ||||
| Cramm and Nieboer (2018) 26 | Patients' perspective, experience of engagement | Yes | No | Patient‐centredness, shared decision‐making |
| 36‐Item patient‐centred primary care instrument | ||||
| Fridberg et al. (2020) 27 | Patients' perspective, Experience of engagement | No | Yes | Patient‐centredness, shared decision‐making, empowerment |
| Generic Person‐Centred Care Questionnaire | ||||
| Greene et al. (2017) 28 | Health professionals' perspective, experience of engagement | Not reported | Not reported | Patient‐centredness, empowerment |
| No name | ||||
| Gremigni et al. (2016) 29 | Health professionals' perspective, experience of engagement | No | No | Patient‐centredness, shared decision‐making |
| Provider–Patient Relationship Questionnaire | ||||
| Huang et al. (2018) 30 | Health professionals' perspective, experience of engagement | No | No | Patient‐centredness, shared decision‐making, empowerment |
| Five‐Dimension Patient‐Centred Innovation Questionnaire | ||||
| Jerofke and Weiss (2016) 31 | Patients' perspective, experience of engagement | No | Yes | Patient‐centredness, shared decision‐making |
| Patient Perceptions of Patient‐Empowering Nurse Behaviours Scale | ||||
| Lindhal et al. (2015) 23 | Family members' perspective, experience of engagement | Not reported | Not reported | Patient‐centredness |
| Person‐Centred Climate Questionnaire‐Family Version | ||||
| Malfait et al. (2016) 32 | Health professionals' perspective, both experience and preferences for engagement | No | Yes | Shared decision‐making |
| Patient Participation Culture Tool for Healthcare Workers | ||||
| Riegel et al. (2018) 33 | Patients' perspective, experience of engagement | No | No | Empowerment |
| Self‐care of chronic illness inventory (SC‐CII or Sky) | ||||
| Stichler and Pelletier (2020) 34 | Patients' perspective, experience of engagement | Yes | No | Shared decision‐making, empowerment |
| Patient Empowerment, Engagement, and Activation Survey | ||||
| Wang et al. (2019) 35 | Patients' perspective, experience of engagement | No | No | Shared decision‐making, empowerment |
| Inpatients' Involvement in Medication Safety Scale | ||||
| Wu et al. (2020) 36 | Patients' perspective, experience of engagement | No | Yes | Patient‐centredness, shared decision‐making, empowerment |
| Patient Engagement in Health Care Questionnaire | ||||
| Yen et al. (2020) 37 | Patients and family members' perspective, preferences for engagement | Yes | No | Patient‐centredness, shared decision‐making, empowerment |
| WeCares | ||||
| Zachariae et al. (2015) 38 | Health professionals' perspective, experience of engagement | No | No | Patient‐centredness, shared decision‐making |
| Student and physician self‐efficacy in patient‐centredness |
Table 5.
Characteristics of the tools included in the scoping review, including context of utilisation, number of items, scale measurement and index of reliability
| Authors, year and name of the scale | Journal | Context of utilisation | Number of items | Scale measurement | Index of reliability |
|---|---|---|---|---|---|
| Berg et al. (2020) 24 | European Journal of Cardiovascular Nursing | Any ward within the departments of cardiology, thoracic surgery and heart and lung transplantation | 16 Items | 4‐Point numeric rating scales | Cronbach's α = .89 |
| Patient Participation Questionnaire | |||||
| Casu et al. (2019) 25 | Patient Education & Counseling | Hospital settings | 16 Items | 5‐Point scale | Cronbach's α = .95 |
| Patient–Professional Interaction Questionnaire | |||||
| Cramm et al. (2018) 26 | BMC Family Practice | Primary care setting (patients with multimorbidity) | 36 Items | 5‐Point scale | Cronbach's α = .89 |
| 36‐Item patient‐centred primary care instrument | |||||
| Fridberg et al. (2020) 27 | BMC Health Services Research | In‐ and outpatient care units | 18 Items | 4‐Point rating scale | Person separation index = 0.85 |
| Generic Person‐Centred Care Questionnaire | |||||
| Greene et al. (2017) 28 | Healthcare | Primary care—Fairview Health Services | 9 Items | 1–5 Scale | Cronbach's α = .73 |
| No name | |||||
| Gremigni et al. (2016) 29 | Patient Education & Counseling | Hospital settings | 16 Items | 5‐Point scale | Cronbach's α = .90 |
| Provider–Patient Relationship Questionnaire | |||||
| Huang et al. (2018) 30 | Journal of Nursing Management | Hospital settings—clinical services | 55 Items | 5‐Point Likert scale | Cronbach's α = .94 |
| Five‐Dimension Patient‐Centred Innovation Questionnaire | |||||
| Jerofke et al. (2016) 31 | Journal of Advanced Nursing | Clinical settings | 42 Items (22 Items in short form) | 11‐Point Likert scale | Cronbach's α = .98 (long from), .97 (short form) |
| Patient Perceptions of Patient‐Empowering Nurse Behaviours Scale | |||||
| Lindhal et al. (2015) 23 | Scandinavian Journal of Caring Sciences | Emergency department | 17 Items | 6‐Point Likert‐type scale | Cronbach's α = .93 |
| Person‐Centred Climate Questionnaire‐Family Version | |||||
| Malfait et al. (2016) 32 | International Journal of Nursing Studies | General and university hospital wards | 52 Items | 4‐Point Likert scale | Cronbach's α = .92 |
| Patient Participation Culture Tool for Healthcare Workers | |||||
| Riegel et al. (2018) 33 | Journal of Advanced Nursing | Inpatient and outpatient settings (patients with chronic illness) | 20 Items | 5‐Point ordinal response scale | Reliability index for multidimensional scales = 0.71 |
| Self‐care of chronic illness inventory | |||||
| Stichler et al. (2020) 34 | Journal of Nursing Care Quality | Acute care and specialty hospitals (behavioural health and women and newborns) | 21 Items | 5‐Point Likert‐like response set | Cronbach's α = .88 |
| Patient Empowerment, Engagement, and Activation Survey | |||||
| Wang et al. (2019) 35 | Journal of Nursing Management | Inpatients from a tertiary hospital—clinical nursing | 23 Items | Not reported (only for content validity: Likert 5‐grade score) | Cronbach's α = .916 |
| Inpatients' Involvement in Medication Safety Scale | |||||
| Wu et al. (2020) 36 | Journal of Nursing Care Quality | General hospitals | 33 Items | 5‐Point Likert scale | Cronbach's α = .928 |
| Patient Engagement in Health Care Questionnaire | |||||
| Yen et al. (2020) 37 | Joint Commission Journal on Quality & Patient Safety | Intensive care units | 13 Items | 4‐Point Likert scale and 5‐point Likert scale | Cronbach α for each subscale = .7116–.866 |
| WeCares | |||||
| Zachariae et al. (2015) 38 | BMC Medical Education | Medical school and hospitals | 27 Items | 5‐Point Likert scale | Cronbach's α = .92 and .94 for medical students (different sample); .95 for physicians |
| Student and physician self‐efficacy in patient‐centredness |
3.3. Perspectives on patient engagement as measured by the tools
Nearly all tools measure experience in patient engagement (88%, n = 14), most of which comes from the patients' perspective (56%, n = 9). 24 , 25 , 26 , 27 , 31 , 33 , 34 , 35 , 36 Tools that inquire about health professionals' perspectives are also mostly based on their own experience in engaging patients (25%, n = 4), 28 , 29 , 32 , 38 but one tool, PaCT‐HCW, 32 evaluates both preferences in and experience with patient engagement. Finally, two tools assess how family members perceived engagement in care: the PCQ‐F tool 23 measures their experience with engagement and the WeCares tool 37 evaluates their preferences.
3.4. Concepts and dimensions assessed with the tools
We categorized the dimensions assessed in each tool into the main concepts of engagement, which include patient centredness, empowerment and shared decision‐making. The results reveal that the two main concepts evaluated in the included scales are shared decision‐making (81%, n = 13) 24 , 25 , 26 , 27 , 29 , 30 , 32 , 34 , 35 , 36 , 37 , 38 and patient centredness (75%, n = 12), 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 36 , 37 , 38 while empowerment is present in 50% (n = 8) of the included tools. 27 , 28 , 30 , 33 , 34 , 35 , 36 , 37
Nine tools evaluate two concepts simultaneously. 24 , 25 , 26 , 28 , 29 , 31 , 34 , 35 , 38 Of these, six evaluate (37%) both patient‐centredness and shared decision‐making. These tools, including the Patient–Professional Interaction Questionnaire, 25 the Provider–Patient Relationship Questionnaire, 29 the Patient Participation Questionnaire, 24 the Patient‐Centred Primary Care instrument, 26 the Patient Perceptions of Patient‐Empowering Nurse Behaviours Scale 31 and the Student and physician self‐efficacy in patient‐centeredness, 38 assess common dimensions of patient‐centredness (empathy/human approach, individualized care/patients' preferences, trust and information exchange) and shared decision‐making (patient involvement in care decisions, patients encouraged to ask questions and effective communication). Three of these tools measure the patient experience of engagement from the patient's perspective 24 , 25 , 26 and two from the HCP's point of view. 29 , 38 Four tools have been developed to be used in inpatient care, 24 , 25 , 29 , 38 while one has been validated in primary care settings. 26 The three main concepts of patient engagement in care are evaluated in four of the scales (25%): the Generic Person‐Centred Care Questionnaire, 27 the Five‐Dimension Patient‐Centred Innovation Questionnaire, 30 the Patient Engagement in Health Care Questionnaire 36 and the WeCares survey. 37 Three of them measure the patient experience of engagement, 27 , 30 , 36 three assess the patient and/or the family perspective 27 , 36 , 37 and one evaluates the point of view of the HCPs. 30 Three tools have been validated in inpatient care settings 30 , 36 , 37 and one is a generic tool that can be used in both inpatient and outpatient care. 27 Finally, three scales (18%) only evaluate a single concept. 23 , 32 , 33
Figure 2 shows the number of tools assessing one or several concepts of patient engagement in care.
Figure 2.
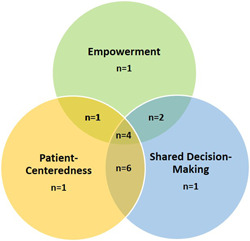
Venn diagram presenting the number of tools assessing one or several concepts of patient engagement in care
3.5. Involvement of patients in tool development or validation
A total of eight tools (50%) did not include patients in their development or validation or did not report having involved patients, and eight were partly developed with patients. For five of them (31%), the involvement of patients consisted mostly of consulting them to validate the tool, including with respect to face or content validity. 24 , 27 , 31 , 32 , 36 Three tools (19%) were developed in collaboration with patients for item development through focus groups or in‐depth interviews or by including patients in expert panels. 26 , 34 , 37 Nevertheless, none of the tools were coconstructed in partnership with patients from item development to the validation phase.
Table 4 presents details on perspectives on patient engagement as measured by the tools, the concepts and dimensions assessed and patient involvement in tool development and validation.
3.6. Context of utilisation of the tools
Most of the tools (75%, n = 12) have been validated in inpatient care, 23 , 24 , 25 , 29 , 30 , 31 , 32 , 34 , 35 , 36 , 37 , 38 while a few (13%, n = 2) were developed for use in outpatient care. 26 , 28 Only two tools have been validated in both inpatient and outpatient clinical settings. 27 , 33 Figure 2 shows information on the context of utilisation of the tools included in our scoping review.
3.7. Psychometric properties of the validated tools
Lastly, in terms of psychometric properties, the reported reliability indices of the tools (Cronbach's α, the reliability index for multidimensional scales and the person separation index) were between 0.71 and 0.98. Based on these coefficients, we consider the reliability of the tools to be moderate to excellent. 14
Table 5 presents information on various characteristics of the tools, including the context of their use, the number of items, the measurement scale and psychometric properties (index of reliability).
4. DISCUSSION
To the best of our knowledge, this is the first systematic scoping review to have identified and summarized recently validated tools assessing various concepts and dimensions of patient engagement in care from both the patients' and HCPs' perspectives. Unlike the systematic review by Jerofke and Weiss, 31 which identified instruments measuring patient preferences regarding engagement in healthcare, our broad review included scales that assessed preferences in or experience with patient engagement from the patients' and HCPs' perspectives.
This scoping review identified and summarized 16 studies that reported on the development and validation of 16 tools assessing patient engagement in care. Nearly all of these tools measure experience with patient engagement and a few measure preferences in patient engagement or both preferences in and experience with engagement simultaneously. The results also show that most of the tools were validated in inpatient care settings and did not involve patients in their development or only consulted them during the validation phase. We identified four important findings concerning the development and validation of the tools included in our scoping review. First, a few tools simultaneously measure some dimensions related to all of the concepts of patient engagement. Second, tools that assess preferences regarding patient engagement in care are relatively scarce. Third, our scoping review has also shown that no tool has been developed in coconstruction with patients, from development to validation. Lastly, very few of the tools were generic, meaning that they could be used in various contexts of care.
4.1. Dimensions measured in tools assessing patient engagement in care
Most of the tools assess dimensions related to one or two concepts of patient engagement (patient centredness or empowerment or shared decision‐making), and only a few tools simultaneously measure some dimensions related to all of the concepts of patient engagement. 27 , 30 , 36 , 37 Furthermore, we found that no tool simultaneously assesses the core dimensions of the partnership in care presented in our conceptual framework (individualized care, empathy, interpersonal trust, communication, experiential knowledge and self‐care). 7
Tools assessing preferences regarding patient engagement in care are relatively scarce. Two out of 16 scales only or partly measured preferences in engagement: One from the HCPs' point of view and the other from both the patients' and family members' perspective. Only one tool, PaCT‐HCW, 32 evaluates both preferences in and experience with patient engagement, but only from the HCPs' point of view. The assessment of patient engagement in care should consider both preferences in and experience with such engagement. From our previous empirical work, which consisted of understanding how patients perceived the partnership in care, we have shown that partnership can be understood as the fit between patients' preferences or expectations for engagement in their care and their experience with such engagement with their HCP. 12 Consequently, measurement of partnership in care could be achieved using a tool capable of assessing the congruence between patients' needs or preferences in their relationship with their HCPs and their perceptions of those interactions.
4.2. Context of tool development, validation and utilization
Our scoping review has also shown that no tool has been developed in coconstruction with patients, from development to validation. For only three tools, patients collaborated in the tool's development, in terms of item selection, through expert panels or focus groups or through in‐depth interviews. There is a consensus that patients should be more actively involved in research to ensure that studies focus on issues that are relevant to them. 39 , 40 It seems particularly important to co‐construct tools with patients when the tools are designed for them. Furthermore, developing a tool to assess patient engagement in care requires a bottom‐up or coconstruction approach with patients and HCPs 41 to identify important dimensions of patient engagement based on the patients' conceptions of being engaged in care and the HCPs' perspectives of engaging patients.
Lastly, very few of the tools were generic. Most of the tools were validated in specific hospital settings, and only two tools were validated in both inpatient and outpatient settings. As most of the tools were not generic, they cannot be used in various contexts of care, in inpatient or outpatient clinical settings, or with patients who have various chronic or acute diseases. As patient engagement in care has become a clinical standard in healthcare settings, it would be important to develop a generic tool that can be used to measure patient engagement in various clinical contexts. This could help monitor the situation and improve patient–HCP relationships, which is one of the core dimensions of quality. 42
4.3. Strengths and limitations
The main strengths of this scoping review are its broad search strategy, which was based on a broad conceptual framework. This allowed us to include various tools assessing the various concepts related to patient engagement in care, and their identification of the levels of patient involvement in tool development and validation. We also used systematic methods to conduct our scoping review, as two reviewers independently screened articles and extracted data, 43 and we complied with the PRISMA extension for scoping reviews. 20 Lastly, we mapped our findings with the broad conceptual framework used to develop our search strategies.
There are two main limitations to our scoping review that may have limited our ability to identify all the relevant tools. First, we only searched for articles published in English or French, which could have led to missing publications in other languages. However, this bias appears to be limited since there is no evidence of systematic bias from using only English‐language articles in systematic reviews. 44 Second, we decided to limit our search to articles published starting from 2014 because a previous systematic review by Phillips et al. 14 covered articles published from 2003 to 2014 on tools for measuring patient participation in care. Philipps et al.'s 14 conceptual framework on patient engagement was not strictly identical to the one that we adopted for our scoping review. However, in their systematic review, Phillips et al. 14 included two of the three main concepts of patient engagement (shared decision‐making and self‐care) that we included in our own conceptual framework. For this reason, we may have missed some relevant tools measuring patient‐centred care by applying this limit.
4.4. Conclusion and implications for clinical practice and research
A growing number of tools have been developed and validated in recent years for assessing patient engagement in care. This scoping review offers a broad identification and description of various tools assessing central concepts in the various approaches to care (patient centredness, empowerment and shared decision‐making) that coexist in clinical practices and settings. No tool offers an exhaustive assessment of the various concepts and dimensions related to both preferences in and experience with engagement in care. However, four tools stand out because they measure the three major concepts of patient engagement in care (patient centredness, empowerment and shared decision‐making). 27 , 30 , 36 , 37 Three of them, and the most recently developed, have involved patients in their tool development or validation. 27 , 36 , 37 Involving patients in the development and validation of tools that assess the quality of care can contribute to uncovering complementary aspects of quality that are not necessarily considered as important by researchers or HCPs. Engaging patients in healthcare research is largely encouraged as it adds value, quality and appropriateness to the research process and outputs. 45 This practice is even more essential when developing a tool that specifically seeks to measure the key dimensions of patient engagement in care. Lastly, the tools that were found in this scoping review only assess preferences in or experience with engagement in care. Nevertheless, measurement of engagement should focus on both patients' preferences in and experience with engagement as a means to appropriately identify the gap between their expectations and experience with their HCPs. A tool measuring this gap in patient engagement could help HCPs to improve the way they interact with patients during consultations, thus improving the quality of care.
The partnership in care approach, which builds on and integrates various approaches to care and dimensions of patient engagement, has started to be applied in clinical practices and different clinical settings. We therefore argue that there is a need for an exhaustive tool that (1) assesses the core dimensions of the partnership in care, (2) measures both preferences in and experiences with engagement, (3) evaluates patients', family members' and HCPs' perspectives to improve partnership practices between patients and their HCPs and (4) has been developed in partnership with patients.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
Nathalie Clavel is the first author of this manuscript. All authors contributed to at least some component of the scoping review and/or manuscript. Nathalie Clavel shaped all aspects of the study design with feedback from Jesseca Paquette and Marie‐Pascale Pomey. Nathalie Clavel and Jesseca Paquette screened independently the titles and abstracts of articles found in the databases and extracted data from full‐text articles. Nathalie Clavel and Jesseca Paquette wrote the manuscript and Vincent Dumez, Claudio Del Grande, Djahanchah Philip (Sacha) Ghadiri, Marie‐Pascale Pomey and Louise Normandin gave substantial suggestions and feedback. All authors have read and approved the final manuscript.
Supporting information
ACKNOWLEDGEMENTS
The authors wish to thank Jim Kroening for his contribution to the editing of this manuscript and Eleonora Bogdanova for her help throughout the scoping review. This study was funded by the research chair held by Dr. Marie‐Pascale Pomey, ‘Chair of Evaluation of State‐of‐the‐Art Technology and Methods‐Citizen and Patient Engagement in the Transformation of Organizations and Health Systems’, at the Hospital Research Center (CRCHUM), University of Montreal.
Clavel N, Paquette J, Dumez V, et al. Patient engagement in care: a scoping review of recently validated tools assessing patients' and healthcare professionals' preferences and experience. Health Expect. 2021;24:1924‐1935. 10.1111/hex.13344
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available in the Supporting Information Material of this article.
REFERENCES
- 1. Carman KL, Dardess P, Maurer M, et al. Patient and family engagement: a framework for understanding the elements and developing interventions and policies. Health Aff. 2013;32(2):223‐231. [DOI] [PubMed] [Google Scholar]
- 2. Armstrong MJ, Mullins CD, Gronseth GS, Gagliardi AR. Impact of patient involvement on clinical practice guideline development: a parallel group study. Implement Sci. 2018;13(1):55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self‐management of chronic disease in primary care. JAMA. 2002;288(19):2469‐2475. [DOI] [PubMed] [Google Scholar]
- 4. Crawford MJ, Rutter D, Manley C, et al. Systematic review of involving patients in the planning and development of health care. BMJ. 2002;325(7375):1263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Trotti A, Colevas AD, Setser A, Basch E. Patient‐reported outcomes and the evolution of adverse event reporting in oncology. J Clin Oncol. 2007;25(32):5121‐5127. [DOI] [PubMed] [Google Scholar]
- 6. Hibbard JH, Greene J, Tusler M. Improving the outcomes of disease management by tailoring care to the patient's level of activation. Am J Manag Care. 2009;15(6):353‐360. [PubMed] [Google Scholar]
- 7. Dumez V, Pomey MP. From medical paternalism to care partnerships: a logical evolution over several decades. In: Macmillan P, ed. Patient Engagement: How Patient‐Provider Partnerships Transform Healthcare Organizations. Palgrave Macmillan; 2019:9‐16. [Google Scholar]
- 8. Gravel K, Légaré F, Graham ID. Barriers and facilitators to implementing shared decision‐making in clinical practice: a systematic review of health professionals' perceptions. Implement Sci. 2006;1:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Elwyn G, Frosch D, Thomson R, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27(10):1361‐1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Foster G, Taylor SJ, Eldridge SE, Ramsay J, Griffiths CJ. Self‐management education programmes by lay leaders for people with chronic conditions. Cochrane Database Syst Rev. 2007;(4):Cd005108. [DOI] [PubMed] [Google Scholar]
- 11. Grady PA, Gough LL. Self‐management: a comprehensive approach to management of chronic conditions. Am J Public Health. 2014;104(8):e25‐e31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pomey M, Ghadiri DP, Karazivan P, Fernandez N, Clavel N. Patients as partners: a qualitative study of patients' engagement in their health care. PLoS One. 2015;10(4):e0122499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Karazivan P, Dumez V, Flora L, et al. The patient‐as‐partner approach in health care: a conceptual framework for a necessary transition. Acad Med. 2015;90(4):437‐441. [DOI] [PubMed] [Google Scholar]
- 14. Phillips NM, Street M, Haesler E. A systematic review of reliable and valid tools for the measurement of patient participation in healthcare. BMJ Qual Saf. 2016;25(2):110‐117. [DOI] [PubMed] [Google Scholar]
- 15. Ree E, Wiig S, Manser T, Storm M. How is patient involvement measured in patient centeredness scales for health professionals? A systematic review of their measurement properties and content. BMC Health Serv Res. 2019;19(1):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jerofke‐Owen T, Garnier‐Villarreal M, Fial A, Tobiano G. Systematic review of psychometric properties of instruments measuring patient preferences for engagement in health care. J Adv Nurs. 2020;76(8):1988‐2004. [DOI] [PubMed] [Google Scholar]
- 17. Castro EM, Van Regenmortel T, Vanhaecht K, Sermeus W, Van Hecke A. Patient empowerment, patient participation and patient‐centeredness in hospital care: a concept analysis based on a literature review. Patient Educ Couns. 2016;99(12):1923‐1939. [DOI] [PubMed] [Google Scholar]
- 18. Pomey M, Flora L, Karazivan P, et al. Le “Montreal Model”: enjeux du partenariat relationnel entre patients et professionnels de la santé. Sante Publique. 2015;HS(S1):41‐50. [PubMed] [Google Scholar]
- 19. Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA‐ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467‐473. [DOI] [PubMed] [Google Scholar]
- 21. Handley SC, Bell S, Nembhard IM. A systematic review of surveys for measuring patient‐centered care in the hospital setting. Med Care. 2021;59(3):228‐237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Catlin A, Ford M, Maloney C. Determining family needs on an oncology hospital unit using interview, art, and survey. Clin Nurs Res. 2016;25(2):209‐231. [DOI] [PubMed] [Google Scholar]
- 23. Lindahl J, Elmqvist C, Thulesius H, Edvardsson D. Psychometric evaluation of the Swedish language Person‐centred Climate Questionnaire‐family version. Scand J Caring Sci. 2015;29(4):859‐864. [DOI] [PubMed] [Google Scholar]
- 24. Berg SK, Færch J, Cromhout PF, et al. Questionnaire measuring patient participation in health care: scale development and psychometric evaluation. Eur J Cardiovasc Nurs. 2020;19(7):600‐608. [DOI] [PubMed] [Google Scholar]
- 25. Casu G, Gremigni P, Sommaruga M. The Patient‐Professional Interaction Questionnaire (PPIQ) to assess patient centered care from the patient's perspective. Patient Educ Couns. 2019;102(1):126‐133. [DOI] [PubMed] [Google Scholar]
- 26. Cramm JM, Nieboer AP. Validation of an instrument for the assessment of patient‐centred care among patients with multimorbidity in the primary care setting: the 36‐item patient‐centred primary care instrument. BMC Fam Pract. 2018;19(1):143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Fridberg H, Wallin L, Wallengren C, Kottorp A, Forsman H, Tistad M. Development and evaluation of the measurement properties of a generic questionnaire measuring patient perceptions of person‐centred care. BMC Health Serv Res. 2020;20(1):960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Greene J, Sacks RM, Hibbard JH, Overton V. How much do clinicians support patient self‐management? The development of a measure to assess clinician self‐management support. Healthc (Amst). 2017;5(1‐2):34‐39. [DOI] [PubMed] [Google Scholar]
- 29. Gremigni P, Casu G, Sommaruga M. Dealing with patients in healthcare: a self‐assessment tool. Patient Educ Couns. 2016;99(6):1046‐1053. [DOI] [PubMed] [Google Scholar]
- 30. Huang C‐Y, Weng R‐H, Wu T‐C, et al. Developing and testing the patient‐centred innovation questionnaire for hospital nurses. J Nurs Manag. 2018;26(2):227‐237. [DOI] [PubMed] [Google Scholar]
- 31. Jerofke T, Weiss M. Development and psychometric analysis of the Patient Perceptions of Patient‐Empowering Nurse Behaviours Scale (PPPNBS). J Adv Nurs. 2016;72(11):2923‐2936. [DOI] [PubMed] [Google Scholar]
- 32. Malfait S, Eeckloo K, Van Daele J, Van Hecke A. The Patient Participation Culture Tool for healthcare workers (PaCT‐HCW) on general hospital wards: a development and psychometric validation study. Int J Nurs Stud. 2016;61:187‐197. [DOI] [PubMed] [Google Scholar]
- 33. Riegel B, Barbaranelli C, Sethares KA, et al. Development and initial testing of the self‐care of chronic illness inventory. J Adv Nurs. 2018;74(10):2465‐2476. [DOI] [PubMed] [Google Scholar]
- 34. Stichler JF, Pelletier LR. Psychometric testing of a patient empowerment, engagement, and activation survey. J Nurs Care Qual. 2020;35(4):E49‐E57. [DOI] [PubMed] [Google Scholar]
- 35. Wang B‐H, Zhang J‐H, Zhang J, Zhu Q, Yan Q‐Y. The development and psychometric testing of Inpatients' Involvement in Medication Safety Scale (IIMSS). J Nurs Manag. 2019;27(8):1648‐1654. [DOI] [PubMed] [Google Scholar]
- 36. Wu Q, Ye X, Wu Y, Zhao L. Development and psychometric evaluation of the patient engagement in Health Care Questionnaire. J Nurs Care Qual. 2020;35(3):E35‐E40. [DOI] [PubMed] [Google Scholar]
- 37. Yen PY, Lehmann LS, Snyder J, et al. Development and validation of WeCares, a survey instrument to assess hospitalized patients' and family members' “Willingness to Engage in Your Care and Safety”. Jt Comm J Qual Patient Saf. 2020;46(10):565‐572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Zachariae R, O'Connor M, Lassesen B, et al. The self‐efficacy in patient‐centeredness questionnaire—a new measure of medical student and physician confidence in exhibiting patient‐centered behaviors. BMC Med Educ. 2015;15:150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Domecq JP, Prutsky G, Elraiyah T. Patient engagement in research: a systematic review. BMC Health Serv Res. 2014;14:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Boivin A, L'espérance A, Gauvin FP, et al. Patient and public engagement in research and health system decision making: a systematic review of evaluation tools. Health Expect. 2018;21:1075‐1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Graffigna G, Barello S, Bonanomi A, Lozza E. Measuring patient engagement: development and psychometric properties of the Patient Health Engagement (PHE) Scale. Front Psychol. 2015;6:274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Elwyn G, Lloyd A, Joseph‐Williams N, et al. Option grids: shared decision making made easier. Patient Educ Couns. 2013;90(2):207‐212. [DOI] [PubMed] [Google Scholar]
- 43. Peters MDJ, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. JBI Evidence Implementation. 2015;13(3):141‐146. [DOI] [PubMed] [Google Scholar]
- 44. Morrison A, Polisena J, Husereau D, et al. The effect of English‐language restriction on systematic review‐based meta‐analyses: a systematic review of empirical studies. Int J Technol Assess Health Care. 2012;28(2):138‐144. [DOI] [PubMed] [Google Scholar]
- 45. Martineau JT, Minyaoui A, Boivin A. Partnering with patients in healthcare research: a scoping review of ethical issues, challenges, and recommendations for practice. BMC Med Ethics. 2020;21(1):34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available in the Supporting Information Material of this article.


