Abstract
Many service members experience symptoms of posttraumatic stress disorder (PTSD) after deployment. PTSD can vary widely in its presentation and associated features, such as comorbid conditions. Research has shown that veterans with PTSD and an internalizing personality profile are more likely to experience internalizing comorbidity (e.g., anxiety, depression), whereas veterans with PTSD and an externalizing personality profile are more likely to experience externalizing comorbidity (e.g., substance abuse, aggression). To date, however, this research has been limited by a focus on diagnosable disorders and personality categories. In a nonclinical sample of 224 National Guard/Reserve service members who had served since 2001, we explored whether personality traits (measured continuously) moderated associations of PTSD symptom severity with the severity of internalizing (depression, anxiety) and externalizing (alcohol abuse, aggression) symptoms. Results showed that the association of PTSD with anxiety was stronger when extraversion was lower (corresponding to an internalizing personality profile). Moreover, the association of PTSD with alcohol abuse was stronger when extraversion was high and conscientiousness was low (corresponding to an externalizing personality profile). Surprisingly, this association was also stronger when extraversion was low and conscientiousness was high. Results offer additional insights into prior research on personality and comorbidity.
Keywords: comorbidity, posttraumatic stress, military, war, veterans
INTRODUCTION
The prevalence of posttraumatic stress disorder (PTSD) among veterans of recent operations in Afghanistan and Iraq has been estimated at 14% to 22% (Seal et al., 2009; Tanielian & Jaycox, 2008). Findings from the National Comorbidity Survey Replication revealed that 88% of people diagnosed with PTSD had at least one comorbid diagnosis of an anxiety, depressive, conduct, or substance use disorder, and 59% had at least two diagnoses (Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995). Similarly, data from the National Epidemiologic Survey on Alcohol and Related Conditions (n = 34,653) revealed that, of those with PTSD, 62% were also diagnosed with a mood disorder, 59% were diagnosed with anxiety disorders other than PTSD, and 46% were diagnosed with alcohol abuse or dependence (Pietrzak, Goldstein, Southwick, & Grant, 2011). Thus, veterans with PTSD are likely to have at least one comorbid disorder.
Although PTSD is sometimes presumed to precede comorbid conditions (e.g., Davidson, Kudler, Saunders, & Smith, 1990; Jacobsen, Southwick, & Kosten, 2001), researchers’ understanding of factors contributing to differing patterns of comorbidity across individuals is limited. One factor that has received attention in prior research is personality. The five-factor model (FFM) describes personality in terms of five broad personality traits: conscientiousness, neuroticism, extraversion, openness, and agreeableness (Costa & McCrae, 1992). Conscientiousness refers to self-discipline, organization, and achievement striving. Neuroticism refers to a lack of emotional stability, reduced impulse control, and anxiety. Extraversion refers to sociability, assertiveness, and talkativeness. Openness refers to intellectual curiosity and a preference for novelty and variety. Agreeableness refers to helpfulness, cooperation, and sympathy toward others.
A separate but related model of personality is a three-factor model advocated by Clark and Watson (1999). Two factors are comparable to factors in the FFM: Positive emotionality (PEM) relates to extraversion, and negative emotionality (NEM) relates to neuroticism. The third factor, constraint/disinhibition (CON), does not have a direct relationship with a single trait in the FFM. Instead, various studies have found that CON is positively correlated with both high conscientiousness and low extraversion (see Kotov, Gamez, Schmidt, & Watson, 2010).
Studies have revealed associations of internalizing disorders, such as depression and anxiety, with both high neuroticism and low extraversion (meta-analyses by Kotov et al., 2010; Malouff, Thorsteinsson, & Schutte, 2005). In contrast, externalizing disorders, such as substance abuse or conduct disorders, are linked with higher levels of extraversion and, less strongly, with lower conscientiousness (Kotov et al., 2010; Malouff et al., 2005). Furthermore, a recent meta-analysis by Kotov and colleagues (2010) revealed that the clearest personality correlate of substance abuse disorders was low CON. Given these findings, it appears that personality traits might help explain differential rates of externalizing and internalizing PTSD comorbidities across individuals.
Miller and colleagues (Miller, Greif, & Smith, 2003; Miller, Kaloupek, Dillon, & Keane, 2004) were among the first to examine this issue among service members. Using cluster analyses of a measure of Clark and Watson’s (1999) three-factor model of personality, Miller and colleagues (2003, 2004) obtained three distinct clusters in two separate samples of mostly Vietnam veterans with combat-related PTSD. The first group, termed low pathology, consisted of participants with statistically average scores on NEM, PEM, and CON. The second group, termed internalizers, was characterized by a combination of high NEM (similar to neuroticism) and low PEM (similar to extraversion). The third group, termed externalizers, was characterized by a combination of high NEM (similar to neuroticism) and low CON (similar to a combination of high extraversion and low conscientiousness). In both samples, Miller and colleagues (2003, 2004) found that comorbid depressive and/or anxiety disorders were more common in internalizers than in externalizers, whereas comorbid substance abuse disorders were more common in externalizers than in internalizers. Since these original studies, numerous other groups have obtained similar findings (e.g., Forbes, Elhai, Miller, & Creamer, 2010; Miller et al., 2012; Wolf, Miller, & Brown, 2011; Wolf, Miller, Harrington, & Reardon, 2012).
To date, this research has utilized a categorical approach to both personality and mental health symptoms. Much research on veterans of the recent conflicts in Iraq and Afghanistan, however, has examined both clinical and subclinical levels of PTSD (e.g., Campbell & Renshaw, 2013; Pietrzak, Goldstein, Malley, Johnson, & Southwick, 2009; Renshaw, Rodebaugh, & Rodrigues, 2010). Moreover, most researchers and clinicians view personality traits as continuous in nature (e.g., Krueger & Eaton, 2010; Widiger & Trull, 2007). Thus, examining these issues on a continuous level, without restricting participants to those with clinical levels of PTSD, could add to the existing knowledge base in this area.
To address this issue, we investigated whether personality traits explained symptom comorbidity in modern service members by examining both symptom comorbidity and personality traits on a continuum. We sought to predict differential associations of internalizing symptoms (depression and anxiety) and externalizing symptoms (substance abuse and aggression) with PTSD symptoms based on combinations of personality traits as defined by the FFM of personality. As neuroticism is elevated in individuals with internalizing and externalizing psychopathology, it was not expected to differentiate between comorbidity patterns. Regarding internalizing symptoms, we expected associations with PTSD to strengthen as levels of extraversion decreased. In contrast, with regard to externalizing symptoms, we expected associations with PTSD to strengthen as levels of extraversion increased and levels of conscientiousness decreased (based on general associations of CON with traits from the FFM model).
METHOD
Participants
Participants in the current study were part of a larger study approved by an institutional review board that involved members of the Utah National Guard/Reserves (NG/R) and their spouses. A total of 224 service members who had deployed overseas between 2001 and 2008 completed measures. Of the participants, 74% were affiliated with the Army NG/R, and 19% were affiliated with the Air NG/R (7% did not report their affiliation). Moreover, 97% of the service members were married, 98% were male, and 88% were White. The sample had deployed to Iraq (64%), Afghanistan (20%), and other locations (e.g., Turkey; 16%).
Measures
The Big Five Inventory (John, Donahue, & Kentle, 1991) is a 44-item, Likert-type, self-report measure that assesses the five factors from the FFM: neuroticism (8 items), extraversion (8 items), openness to experience (10 items), agreeableness (9 items), and conscientiousness (9 items). Each item consists of a word or phrase describing a personality characteristic, and respondents indicate how representative the item is of them on a scale from 1 (disagree strongly) to 5 (agree strongly). Items on each subscale are summed for a total score on that subscale. John and colleagues (1991) found that the overall measure and the individual subscales demonstrated good internal consistency, test–retest reliability, and convergent validity with other measures of personality. Internal consistencies for all subscales in our sample were adequate: neuroticism (α = .82), extraversion (α = .86), openness to experience (α = .71), agreeableness (α = .76), and conscientiousness (α = .76).
The PTSD Checklist–Military Version (PCL-M; Weathers, Litz, Herman, Huska, & Keane, 1993) is a 17-item, self-report, Likert-type scale that assesses symptoms of PTSD. Each item represents one criterion for PTSD as described in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (American Psychiatric Association, 1994). Items are answered as to how much the respondent has experienced the symptom in the past month on a scale from 1 (not at all) to 5 (extremely). Higher scores indicate greater symptom intensity. The scale is widely used and has high internal consistency, test–retest reliability, and convergent validity (Pratt, Brief, & Keane, 2006). In our sample, internal consistency was excellent (α = .94).
The Depression Anxiety Stress Scales (Lovibond & Lovibond, 1995) is a 42-item, Likert-type, self-report measure of depression (14 items), anxiety (14 items), and stress (14 items). Participants answer each item in terms of how much it applied over the past week, from 0 (did not apply to me at all) to 3 (applied to me very much, or most of the time). Items are summed within each subscale (depression, anxiety, and stress) for a total score on each. The subscales all have good test–retest reliability, convergent and divergent validity, and internal consistency (Lovibond & Lovibond, 1995). Only the depression and anxiety subscales were used in analyses for this study. In our sample, internal consistency was excellent for both subscales (depression, α = .94; anxiety, α = .92).
The Alcohol, Smoking, and Substance Involvement Screening Test (WHO ASSIST Working Group, 2002) is a self-report questionnaire that assesses misuse of, abuse of, and/or dependency on any of nine substances. Eight questions are used for each of the nine substances. This questionnaire is the product of a 10-year effort by the World Health Organization to develop a reliable, valid, and useful substance use screening device and has been tested in multiple samples from different countries. We used the alcohol subscale, which provided a continuous measure of problematic alcohol use in the past 3 months. In our sample, internal consistency was acceptable (α = .73).
The Aggression Questionnaire (Buss & Perry, 1992) consists of four subscales with a total of 29 items that assess internal experiences of anger and external expressions of aggression. Each question is answered using a 5-point Likert-type scale from 1 (very uncharacteristic of me) to 5 (very characteristic of me). The measure is divided into four subscales. The Aggression Questionnaire and its subscales possess strong reliability and validity (Buss & Perry, 1992). We focused on the two externalizing subscales of the measure in the present study: verbal aggression (5 items), which measures aggressive or hostile verbal actions toward others; and physical aggression (9 items), which assesses physical expressions of aggression toward others. In our sample, these two subscales were strongly correlated with each other (r = .49, p < .001). We thus combined the verbal and physical aggression subscales in order to measure symptoms of overt aggression. Internal consistency for the combined verbal and physical aggression subscales was good (α = .83).
Procedure
All procedures for this study were approved by the University of Utah Institutional Review Board and the Utah NG Judge Advocate General. Participants were recruited during eight voluntary postdeployment workshops for Utah NG/R members held between September 2007 and August 2008. Approximately 490 predominantly married service members attended the workshops, and a total of 271 service members (55%) participated in the study. A total of 47 participants who did not report having been deployed since 2001 were excluded from analyses. All participants provided written informed consent prior to participating. Upon completion of the survey, participants were reimbursed $10.
Data Analysis
Our primary hypotheses explored whether various personality trait levels would moderate the associations of PTSD symptoms with (a) internalizing symptoms (anxiety and depression) and (b) externalizing symptoms (alcohol use and aggression). We used path analysis to accommodate the multiple covarying outcomes and overlapping predictor variables. Anxiety, depression, substance use, and aggression were modeled as covarying, observed, endogenous (outcome) variables. PTSD, neuroticism, extraversion, conscientiousness, and relevant interaction terms were modeled as covarying, exogenous (predictor) variables (see Figure 1). In all analyses, neuroticism was included to control for its influence (as it was expected to be relevant to both types of comorbidity), not as part of any interaction terms.
FIGURE 1.
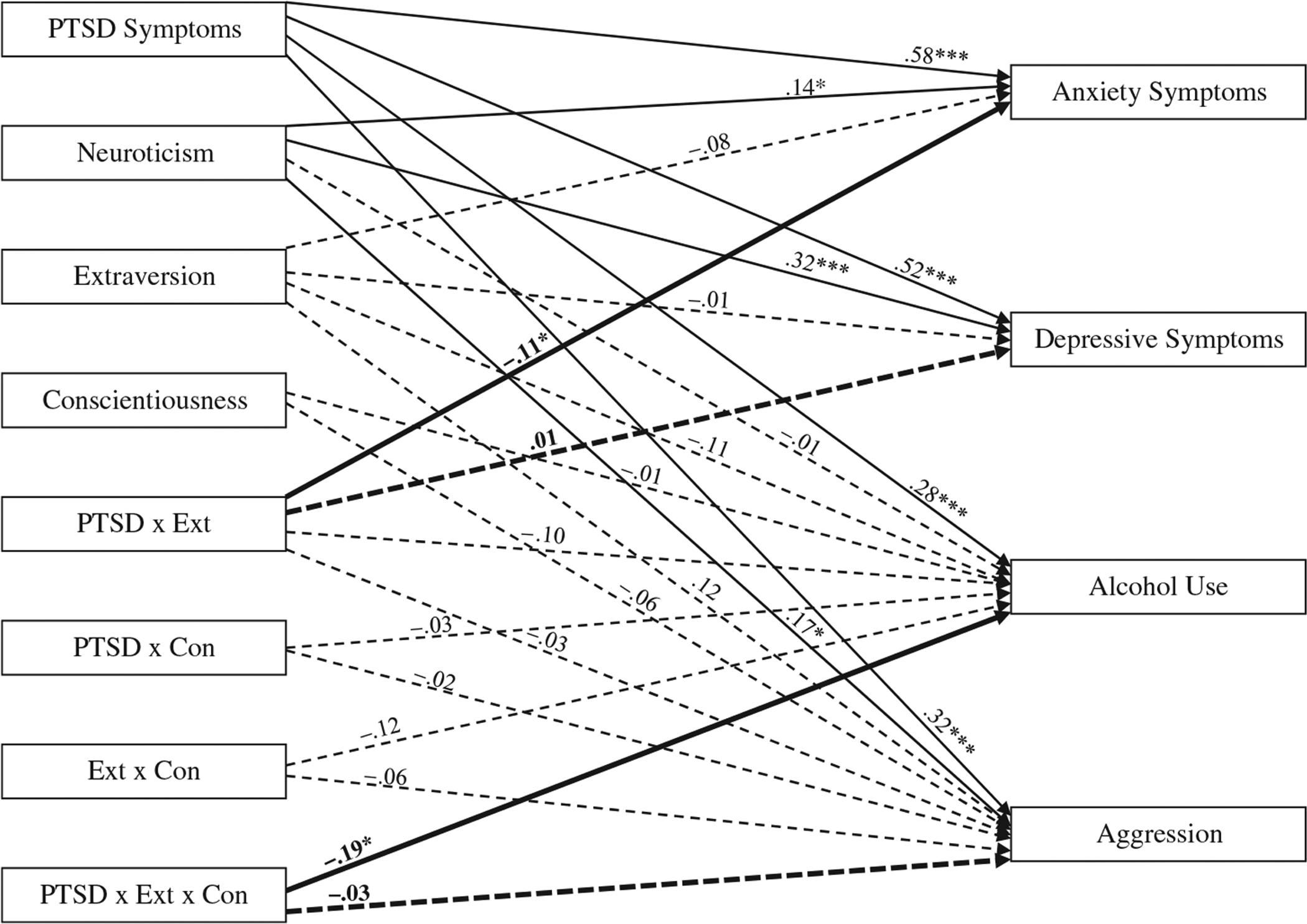
Path analysis of the full model, with standardized coefficients shown. Primary tests of hypotheses are shown in bold. Nonsignificant paths are shown as dotted lines. Covariances are not shown but are available on request from the first author. PTSD = posttraumatic stress disorder; EXT = extraversion; Con = conscientiousness. *p < .05; ***p < .001.
To test the hypothesis that PTSD symptoms would be more strongly associated with internalizing symptoms at lower levels of extraversion, we specified structural paths to both anxiety and depressive symptoms from (a) PTSD symptoms, (b) neuroticism, (c) extraversion, and (d) the interaction of PTSD symptoms and extraversion (see Figure 1). The primary hypothesis was evaluated via significance of the structural paths from the interaction term to anxiety and depression.
To test the hypothesis that PTSD symptoms would be more strongly associated with externalizing symptoms at higher levels of extraversion and lower levels of conscientiousness, we specified structural paths to both alcohol use and aggression from (a) PTSD symptoms, (b) neuroticism, (c) extraversion, (d) conscientiousness, and (e) four related interaction terms. Given our operationalization of externalizing personality as a combination of high extraversion and low conscientiousness, the primary interaction term of interest was a three-way interaction among PTSD, extraversion, and conscientiousness. To test this interaction, we had to include the three related two-way interaction terms (PTSD and extraversion, PTSD and conscientiousness, and extraversion and conscientiousness). The primary hypothesis was evaluated based on the significance of the structural paths from the three-way interaction term to alcohol use and aggression.
We centered all predictor variables and created interaction terms by multiplying centered variables together (Aiken & West, 1991). Significant interactions were probed by creating high and low versions of the moderating variables and rerunning analyses (Aiken & West, 1991). In addition to the chi-square value (which can be unduly influenced by sample size), we examined the root mean square error of approximation (RMSEA) and the comparative fit index (CFI) to evaluate model fit. Various authors have recommended RMSEA values of .08, .06, or .05 and lower, and CFI values of .90 or .95 and higher, as indicative of good fit (e.g., Hu & Bentler, 1999; Marsh, Hau, & Wen, 2004). Of note, some of our models contained only one or two degrees of freedom, which typically produces high model fit. Thus, the primary emphasis was on the significance of the path estimates. All path analyses were conducted in Amos 19.0 and used full information maximum likelihood procedures to handle missing data. Thus, the complete sample (N = 224) was used for all analyses.
RESULTS
Means, standard deviations, and correlations for all measures are reported in Table 1. The mean on the PCL-M was near the cutoff recommended by Bliese and colleagues (2008) to indicate possible PTSD. Specifically, 30.7% of participants had a score on the PCL-M at or above the cutoff of 33 recommended by Bliese et al., and 10.2% had a score at or above the cutoff of 50 recommended by Weathers et al. (1993). Although the means for depression and anxiety were in the normal range on the Depression Anxiety Stress Scales, 22.5% of participants had scores indicative of at least mild depression (10 or higher on the depression subscale), with 13.7% evidencing moderate to severe depression (14 or higher). Similarly, 21.4% had at least mild anxiety (8 or higher on the anxiety subscale), with 15.4% reporting moderate to severe anxiety (10 or higher). Thus, overall our participants were fairly representative of the recent veteran population (e.g., Hoge et al., 2004).
TABLE 1.
Means, Standard Deviations, and Correlations
| Variable | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. PTSD | 30.55 | 12.44 | – | |||||||
| 2. Neuroticism | 20.47 | 5.68 | .43*** | – | ||||||
| 3. Extraversion | 26.11 | 6.05 | −.06 | −.32*** | – | |||||
| 4. Conscientiousness | 35.27 | 4.84 | −.17* | −.32*** | .20** | – | ||||
| 5. Aggression | 32.61 | 8.59 | .42*** | .28*** | .04 | −.11 | – | |||
| 6. Alcohol | 3.72 | 5.77 | .29*** | .13 | −.08 | −.00 | .26*** | – | ||
| 7. Depression | 5.31 | 7.08 | .66*** | .54*** | −.15* | −.24*** | .35*** | .25*** | – | |
| 8. Anxiety | 3.90 | 5.84 | .68*** | .42*** | −.17* | −.12 | .40* | .36*** | .72*** | – |
Notes: PTSD = posttraumatic stress disorder.
p < .05
p < .01
p < .001
As shown in Table 1, PTSD and the internalizing symptoms of anxiety and depression were all strongly positively correlated, as expected. In addition, PTSD symptoms were strongly positively correlated with externalizing symptoms of aggression and alcohol use, although aggression and alcohol use themselves were only modestly correlated with each other. Neuroticism was strongly positively correlated with all types of symptoms, with the exception of alcohol use, whereas extraversion and conscientiousness exhibited small or nonsignificant associations with most symptoms.
Path Analysis
The initial model was an excellent fit for the data, χ2(10, N = 224) = 14.84, p = .138, CFI = .99, RMSEA = .05. As shown in Figure 1, there were significant main effects of PTSD symptoms on all outcome variables and significant main effects of neuroticism on all outcome variables except alcohol use, and two interaction terms were significant. The interaction of PTSD symptoms and extraversion significantly predicted anxiety symptoms, and the three-way interaction of PTSD symptoms, extraversion, and conscientiousness significantly predicted alcohol use. Both of these results were consistent with a priori hypotheses. Contrary to hypotheses, however, the interaction of PTSD and extraversion did not predict depressive symptoms, nor did the three-way interaction predict aggression.
To ease the interpretability of results when probing the interactions, we split the model into one predicting only internalizing symptoms (including PTSD, neuroticism, extraversion, and the interaction of PTSD and extraversion) and a separate model predicting only externalizing symptoms (including all eight exogenous variables). The overall model fit of the reduced internalizing model and the externalizing model remained excellent, consistent with models with few degrees of freedom: internalizing, χ2(1, N = 224) = 1.14, p = .286, CFI = 1.00, RMSEA = .02; externalizing, χ2(2, N = 224) = 1.26, p = .531, CFI = 1.00, RMSEA = .00. Of note, the pattern of significance for all structural paths remained the same.
The probe of the internalizing model was consistent with our hypothesis, in that the positive association of PTSD symptoms with anxiety symptoms was stronger at low (−1 SD) levels of extraversion (b = .70, p < .001) than at high (+1 SD) levels of extraversion (b = .47, p < .001). The probe of the externalizing model was partially consistent with our hypothesis, in that the association of PTSD symptoms with extent of alcohol use was weakest at high (+1 SD) extraversion and high (+1 SD) conscientiousness (b = −.03, p = .861), significant but small at low (−1 SD) extraversion and low (−1 SD) conscientiousness (b = .23, p < .05), and significant and stronger at high (+1 SD) extraversion and low (−1 SD) conscientiousness (b = .41, p < .05). However, the association was strongest at low (−1 SD) extraversion and high (+1 SD) conscientiousness (b = .52, p < .001), which was not predicted.
DISCUSSION
Previous research has established that veterans with PTSD often report comorbid symptoms of anxiety, depression, substance abuse, and aggression (Bleich, Koslowsky, Dolev, & Lerer, 1997; Ginzburg, Ein-Dor, & Solomon, 2010; Kessler et al., 1995). Several groups have found that personality characteristics can help predict patterns of comorbidity in veterans with PTSD (Forbes et al., 2010; Miller et al., 2003, 2004, 2012; Wolf et al., 2011, 2012). Specifically, individuals with internalizing personality profiles, characterized by high neuroticism and low extraversion, are more likely to have internalizing disorders, such as depression and anxiety, co-occurring with PTSD. In contrast, individuals with externalizing comorbidity patterns, characterized by high neuroticism and low constraint (or high neuroticism, high extraversion, and low conscientiousness), are more likely to have externalizing problems, such as substance abuse or aggression, co-occurring with PTSD. However, little research has examined this issue in a nonclinical sample of veterans. Our findings build on prior studies by examining comorbidity at the symptom level, treating symptoms and personality traits as continuous variables, in a sample of veterans who served during the recent era of conflicts in Iraq and Afghanistan.
Regarding internalizing symptoms, although the direct associations of PTSD symptoms with depressive and anxiety symptoms were strong, the association of PTSD and anxiety symptoms was significantly moderated by extraversion. Specifically, as predicted, the association of PTSD and anxiety was stronger when extraversion was lower. These findings are consistent with prior findings regarding internalizing personality profiles and diagnostic comorbidity but are novel in their use of continuous personality traits and symptoms. Contrary to expectations, however, extraversion did not moderate the association of PTSD symptoms with depressive symptoms.
Regarding externalizing symptoms, although PTSD symptoms were significantly associated with both aggression and alcohol abuse, the association with extent of alcohol use also was moderated by a combination of extraversion and conscientiousness. Specifically, the association was stronger when extraversion was higher and conscientiousness was lower. This finding is consistent with previous research and our hypothesis and may be reflective of a lack of constraint that promotes excessive drinking in the context of PTSD symptoms. Unexpectedly, however, we also found that the association of PTSD and alcohol use was stronger when extraversion was lower and conscientiousness was higher. It may be that this unpredicted pattern reflects an internalizing component of alcohol abuse, whereby individuals use alcohol for self-medication of symptoms and/or avoidance of negative emotional states (Cooper, Agocha, & Sheldon, 2000). However, our data are cross-sectional, precluding analysis of the direction of effects. Thus, these seemingly contrary findings suggest a need for further research addressing the association of PTSD with differing motivations for alcohol abuse (e.g., binge drinking vs. daily drinking, solitary drinking vs. social drinking). Moreover, research exploring associations between PTSD and the abuse of other substances (e.g., prescription drugs or marijuana) would add substantially to researchers’ knowledge and possibly enable further tailoring of treatments. Notably, contrary to expectations, the association of PTSD symptoms with aggression was not moderated by extraversion or conscientiousness.
There are potential clinical implications of our findings. Our study indicates that personality impacts associations of internalizing and externalizing symptoms with PTSD symptoms across a full range of symptom severity. This suggests that the evaluation of individual personality traits may assist clinicians in understanding various symptom manifestations in veterans who suffer not only from diagnosable PTSD but also from subclinical PTSD symptoms. Moreover, these findings highlight the fact that symptoms such as alcohol abuse, aggression, and depression do not occur in a vacuum. Even in the absence of full diagnostic criteria, subclinical reactions to trauma may be associated with other clinical or subclinical conditions. Our findings suggest that personality traits may represent one way of predicting various potential patterns of co-occurring symptoms.
However, prospective research is needed to investigate whether personality trait levels truly predict the development of comorbid symptoms. Prior research has suggested both that personality profiles can influence the development of posttraumatic responses (e.g., Chung, Dennis, Easthope, Werrett, & Farmer, 2005) and that traumatic experiences can alter personality profiles (e.g., Widiger, 2011). Thus, no causal inferences can be drawn here. However, if future research replicates our findings, such information could allow for targeted interventions aimed at preventing the development of comorbid symptom patterns for those with PTSD symptoms and specific personality profiles. Indeed, personality psychologists have previously suggested that personality assessment “may be useful to clinicians in understanding the patient, formulating a diagnosis … anticipating the course of therapy, and selecting the optimal treatment for the patient” (Costa & McCrae, 1992, p. 5). Applying such assessment to treatment planning in the context of combat-related PTSD and comorbid conditions is a novel and potentially effective usage.
However, there are also limitations to this current study. Our sample was demographically homogenous, in that most participants were married and members of the Mormon Church. Both groups drink alcohol less frequently on average, which may have impacted our findings regarding alcohol use. These characteristics of our sample, combined with the tendency of service members to underreport substance use, may have altered the findings. The most likely possibility is that increased reporting of substance use and psychopathology would strengthen the findings by increasing range. Future research is needed to explore this possibility. Moreover, the inclusion of partner/spouse reports or clinical interview assessment of these constructs would provide additional validity to the current self-reported data and potentially confirm the findings. Our participants were also predominantly White, older on average than other samples of Iraq/Afghanistan veterans, and composed solely of NG/R members; thus, findings may not be generalizable to other military veterans. Finally, as previously stated, our data were cross-sectional. Longitudinal data would permit a more comprehensive examination of change in symptoms and comorbidity over time based on personality profiles. Despite these limitations, our findings indicate that, even at subclinical symptom levels, comorbidity with PTSD symptoms is impacted by levels of personality traits. This finding highlights personality testing as a potentially useful tool in the early detection of specific patterns of symptomatology.
REFERENCES
- Aiken L, & West SG (1991). Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage Publications. [Google Scholar]
- American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: Author. [Google Scholar]
- Bleich A, Koslowsky M, Dolev A, & Lerer B (1997). Posttraumatic stress disorder and depression: An analysis of comorbidity. British Journal of Psychiatry, 170, 479–482. doi: 10.1192/bjp.170.5.479 [DOI] [PubMed] [Google Scholar]
- Bliese PD, Wright KM, Adler AB, Cabrera O, Castro CA, & Hoge CW (2008). Validating the Primary Care Posttraumatic Stress Disorder Screen and the Posttraumatic Stress Disorder Checklist with soldiers returning from combat. Journal of Consulting and Clinical Psychology, 76, 272–281. doi: 10.1037/0022-006X.76.2.272 [DOI] [PubMed] [Google Scholar]
- Buss AH, & Perry M (1992). The Aggression Questionnaire. Journal of Personality and Social Psychology, 63, 452–459. doi: 10.1037/0022-3514.63.3.452 [DOI] [PubMed] [Google Scholar]
- Campbell SB, & Renshaw KD (2013). PTSD symptoms, disclosure, and relationship distress: Explorations of mediation and associations over time. Journal of Anxiety Disorders, 27, 494–502. doi: 10.1016/j.janxdis.2013.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung MC, Dennis I, Easthope Y, Werrett J, & Farmer S (2005). A multiple-indicator multiple-cause model for posttraumatic stress reactions: Personality, coping, and maladjustment. Psychosomatic Medicine, 67, 251–259. doi: 10.1097/01.psy.0000155675.56550.5f [DOI] [PubMed] [Google Scholar]
- Clark L, & Watson D (1999). Temperament: A new paradigm for trait psychology. In Pervin LA & John OP (Eds.), Handbook of personality: Theory and research (2nd ed., pp. 399–423). New York, NY: Guilford Press. [Google Scholar]
- Cooper ML, Agocha VB, & Sheldon MS (2000). A motivational perspective on risky behaviors: The role of personality and affect regulatory processes. Journal of Personality, 68, 1059–1088. doi: 10.1111/1467-6494.00126 [DOI] [PubMed] [Google Scholar]
- Costa PT, & McCrae RR (1992). Normal personality assessment in clinical practice: The NEO Personality Inventory. Psychological Assessment, 4, 5–13. doi: 10.1037/1040-3590.4.1.20 [DOI] [Google Scholar]
- Davidson JR, Kudler HS, Saunders WB, & Smith RD (1990). Symptom and comorbidity patterns in World War II and Vietnam veterans with posttraumatic stress disorder. Comprehensive Psychiatry, 31, 162–170. doi: 10.1016/0010-440X(90)90020-S [DOI] [PubMed] [Google Scholar]
- Forbes D, Elhai JD, Miller MW, & Creamer M (2010). Internalizing and externalizing classes in posttraumatic stress disorder: A latent class analysis. Journal of Traumatic Stress, 23, 340–349. [DOI] [PubMed] [Google Scholar]
- Ginzburg K, Ein-Dor T, & Solomon Z (2010). Comorbidity of posttraumatic stress disorder, anxiety, and depression: A 20-year longitudinal study of war veterans. Journal of Affective Disorders, 123, 249–257. doi: 10.1016/j.jad.2009.08.006 [DOI] [PubMed] [Google Scholar]
- Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, & Koffman RL (2004). Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine, 351, 13–22. doi: 10.1056/NEJMoa040603 [DOI] [PubMed] [Google Scholar]
- Hu L, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. doi: 10.1080/10705519909540118 [DOI] [Google Scholar]
- Jacobsen LK, Southwick SM, & Kosten TR (2001). Substance use disorders in patients with posttraumatic stress disorder: A review of the literature. American Journal of Psychiatry, 158, 1184–1190. doi: 10.1176/appi.ajp.158.8.1184 [DOI] [PubMed] [Google Scholar]
- John O, Donahue E, & Kentle R (1991). The “Big Five” Inventory—Versions 4a and 54. Berkeley: University of California, Berkeley, Institute of Personality and Social Research. [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, & Nelson CB (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52, 1048–1060. doi: 10.1001/archpsyc.1995.03950240066012 [DOI] [PubMed] [Google Scholar]
- Kotov R, Gamez W, Schmidt F, & Watson D (2010). Linking “big” personality traits to anxiety, depressive, and substance use disorders: A meta-analysis. Psychological Bulletin, 136, 768–821. doi: 10.1037/a0020327 [DOI] [PubMed] [Google Scholar]
- Krueger RF, & Eaton NR (2010). Personality traits and the classification of mental disorders: Toward a more complete integration in DSM–5 and an empirical model of psychopathology. Personality Disorders: Theory, Research, and Treatment, 1, 97–118. doi: 10.1037/a0018990 [DOI] [PubMed] [Google Scholar]
- Lovibond P, & Lovibond S (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy, 33, 335–343. doi: 10.1016/0005-7967(94)00075-U [DOI] [PubMed] [Google Scholar]
- Malouff JM, Thorsteinsson EB, & Schutte NS (2005). The relationship between the five-factor model of personality and symptoms of clinical disorders: A meta-analysis. Journal of Psychopathology and Behavioral Assessment, 27, 101–114. doi: 10.1007/s10862-005-5384-y [DOI] [Google Scholar]
- Marsh HW, Hau K-T, & Wen Z (2004). In search of golden rules: Comment on hypothesis-testing approaches to setting cutoff values for fit indexes and dangers in overgeneralizing Hu and Bentler’s (1999) findings. Structural Equation Modeling: A Multidisciplinary Journal, 11(3), 320–341. doi: 10.1207/s15328007sem1103_2 [DOI] [Google Scholar]
- Miller MW, Greif JL, & Smith AA (2003). Multidimensional Personality Questionnaire profiles of veterans with traumatic combat exposure: Externalizing and internalizing subtypes. Psychological Assessment, 15, 205–215. doi: 10.1037/1040-3590.15.2.205 [DOI] [PubMed] [Google Scholar]
- Miller MW, Kaloupek DG, Dillon AL, & Keane TM (2004). Externalizing and internalizing of combat-related PTSD: A replication and extension using the PSY-5 scales. Journal of Abnormal Psychology, 113, 636–645. doi: 10.1037/0021-843X.113.4.636 [DOI] [PubMed] [Google Scholar]
- Miller MW, Wolf EJ, Reardon A, Greene A, Ofrat S, & McInerney S (2012). Personality and the latent structure of PTSD comorbidity. Journal of Anxiety Disorders, 26, 599–607. doi: 10.1016/j.janxdis.2012.02.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrzak RH, Goldstein MB, Malley JC, Johnson DC, & Southwick SM (2009). Subsyndromal posttraumatic stress disorder is associated with health and psychosocial difficulties in veterans of Operations Enduring Freedom and Iraqi Freedom. Depression and Anxiety, 26, 739–744. doi: 10.1002/da.20574 [DOI] [PubMed] [Google Scholar]
- Pietrzak RH, Goldstein RB, Southwick SM, & Grant BF (2011). Prevalence and Axis I comorbidity of full and partial posttraumatic stress disorder in the United States: Results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Anxiety Disorders, 25, 456–465. doi: 10.1016/j.janxdis.2010.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pratt EM, Brief DJ, & Keane TM (2006). Recent advances in psychological assessment of adults with posttraumatic stress disorder. In Follette VM & Ruzek JI (Eds.), Cognitive-behavioral therapies for trauma (2nd ed., pp. 34–61). New York, NY: Guilford Press. [Google Scholar]
- Renshaw KD, Rodebaugh TL, & Rodrigues CS (2010). Psychological and marital distress in spouses of Vietnam veterans: Importance of spouses’ perceptions. Journal of Anxiety Disorders, 24, 743–750. doi: 10.1016/j.janxdis.2010.05.007 [DOI] [PubMed] [Google Scholar]
- Seal KH, Metzler TJ, Gima KS, Bertenthal D, Maguen S, & Marmar CR (2009). Trends and risk factors for mental health diagnoses among Iraq and Afghanistan veterans using Department of Veterans Affairs Health Care, 2002–2008. American Journal of Public Health, 99, 1651–1658. doi: 10.2105/AJPH.2008.150284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanielian TL, & Jaycox L (2008). Invisible wounds of war psychological and cognitive injuries, their consequences, and services to assist recovery. Santa Monica, CA: RAND Center for Military Health Policy Research. [Google Scholar]
- Weathers F, Litz B, Herman D, Huska J, & Keane T (1993, November). The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. Paper presented at the annual meeting of the International Society for Traumatic Stress Studies, San Antonio, TX. [Google Scholar]
- WHO ASSIST Working Group. (2002). The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): Development, reliability and feasibility. Addiction, 97, 1183–1194. doi: 10.1046/j.1360-0443.2002.00185.x [DOI] [PubMed] [Google Scholar]
- Widiger TA (2011). Personality and psychopathology. World Psychiatry, 10, 103–106. doi: 10.1002/j.2051-5545.2011.tb00024.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widiger TA, & Trull TJ (2007). Plate tectonics in the classification of personality disorder: Shifting to a dimensional model. American Psychologist, 62, 71–83. doi: 10.1037/0003-066X.62.2.71 [DOI] [PubMed] [Google Scholar]
- Wolf EJ, Miller MW, & Brown TA (2011). The structure of personality disorders in individuals with posttraumatic stress disorder. Personality Disorders: Theory, Research, and Treatment, 2, 261–278. doi: 10.1037/a0023168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf EJ, Miller MW, Harrington KM, & Reardon A (2012). Personality-based latent classes of posttraumatic psychopathology: Personality disorders and the internalizing/externalizing model. Journal of Abnormal Psychology, 121, 256–262. doi: 10.1037/a0023237 [DOI] [PMC free article] [PubMed] [Google Scholar]


