INTRODUCTION
Testing is an important part of medicine across all specialties and settings. As a result, the volume of testing is enormous, with an estimated 4–5 billion tests performed in the United States each year.1 Unnecessary laboratory testing and diagnostic imaging is believed to be common. Studies looking at testing of patients have found 40%−60% of tests to be unnecessary.1–3 Unnecessary tests can cause patient discomfort, patient harm, and increase health care costs. Unnecessary tests can also lead to false positive results, which often lead to other tests, a phenomenon known as a diagnostic cascade.4 To evaluate the extent of unnecessary testing and physician awareness of this problem, we conducted a chart review and questionnaire for resident physicians at two academic medical centers.
METHODS
Study Design
We conducted a retrospective review of electronic medical records from a convenience sample of patients admitted to medicine services at two hospitals (a tertiary care medical center and a Department of Veterans Affairs hospital). Participants were eligible if they were admitted to an Internal Medicine service from the Emergency Department. Data abstraction included all laboratory testing and imaging testing performed within the first 24 hours of medical care. Physician reviewers determined if each test or procedure was necessary based on a chart review. Necessity of test or procedure was defined with a 4-point scale (1 = absolutely unnecessary, 2 = somewhat unnecessary, 3 = somewhat necessary, 4 = absolutely necessary) by the reviewing physician, similar to past chart reviews for preventability of adverse events.5 Necessity was determined based upon most appropriate clinical guidelines or UpToDate, an evidence-based, physician-authored clinical decision support resource.6,7 Reviewers also reported if each identified test resulted in a change in management and if any other tests or procedures resulted because of the test. If changes in management were identified, the reviewer reported what these were. Finally, we recorded if any harms or benefits occurred as a result of tests or procedures.8
In addition to chart review, a paper questionnaire was administered in person to a convenience sample of frontline providers caring for these patients. The questionnaire was completed by providers within the first 24 hours of the patient’s hospitalization. Completion of the questionnaire was voluntary, and no provider-identifiable information was transferred to the database. The questionnaire contained a list of 10 common laboratory and 11 common imaging tests, as well as an open-ended section for other tests. Participants were asked to report all medical tests ordered within the first 24 hours of care for the patients without opening the patient’s chart for this information. Participants were also asked to grade the necessity of each test using the same 4-point scale as the chart reviews, and to report if the test led to a change in management. This study was approved by the institutional review board at each institution and a waiver of informed consent was granted for this study.
Statistical Methods
Chart review and questionnaire results were compiled and the frequency of each test type ordered, abnormal findings, changes in management, and other tests/procedure information were analyzed for all patients. Necessity scores were averaged for chart reviews and for physician questionnaires. Statistics were compiled using Microsoft Excel (Microsoft Corporation, Redmond, WA) and calculated using SAS version 9.4 (SAS Institute Inc., Cary, NC). Data entered in the database were deidentified.
RESULTS
Chart reviews and physician questionnaires were conducted from January 1,2017 to June 16,2017. During the study period 177 charts were reviewed. Additionally, 49 frontline provider questionnaires were collected on patients, which amounted to 28% (49 of 177) of chart reviews.
Chart Reviews
The 177 patients reviewed had a mean age of 68.5 years; 92% were male and 63% identified as black or African American. Overall, patients had a mean of 9.2 tests ordered within the first 24 hours of medical care. Of these, 31.5% (2.9/9.2) of tests were determined by review to be unnecessary (either a 1 or 2 on the 4-point scoring system). Chart review identified a total of 87.5% (155/177) of patients who received at least one unnecessary test during their first 24 hours of care (Figure). Of all 177 patients reviewed, 50.8% (90/177) had no change in management based on the laboratory or imaging studies ordered. Of all patients included, 49.2% (87/177) had a change in management. Thirteen percent (23/177) had an immediate change in management, of which 73.9% (17/23) were beneficial and 26.1% (6/23) were of no benefit. An additional 36% (64/177) of patients had a test that led to additional tests or procedures. Of these 64 patients who received additional tests or procedures, 43.8% (28/64) were beneficial, 50% (32/64) were of no benefit, and 6% (4/64) were harmful. Overall, 72.3% (128/177) of patients experienced no benefit or harms from testing, 25.4% (45/177) experienced benefit and 2.3% (4/177) harm. Test results that were harmful included 4 instances of unnecessary antibiotic prescription for asymptomatic bacteriuria. Test results that were judged to be beneficial included identifying cancer (4 patients), starting hemodialysis (2 patients), and receiving cardiac angioplasty and stenting (1 patient).
Figure.
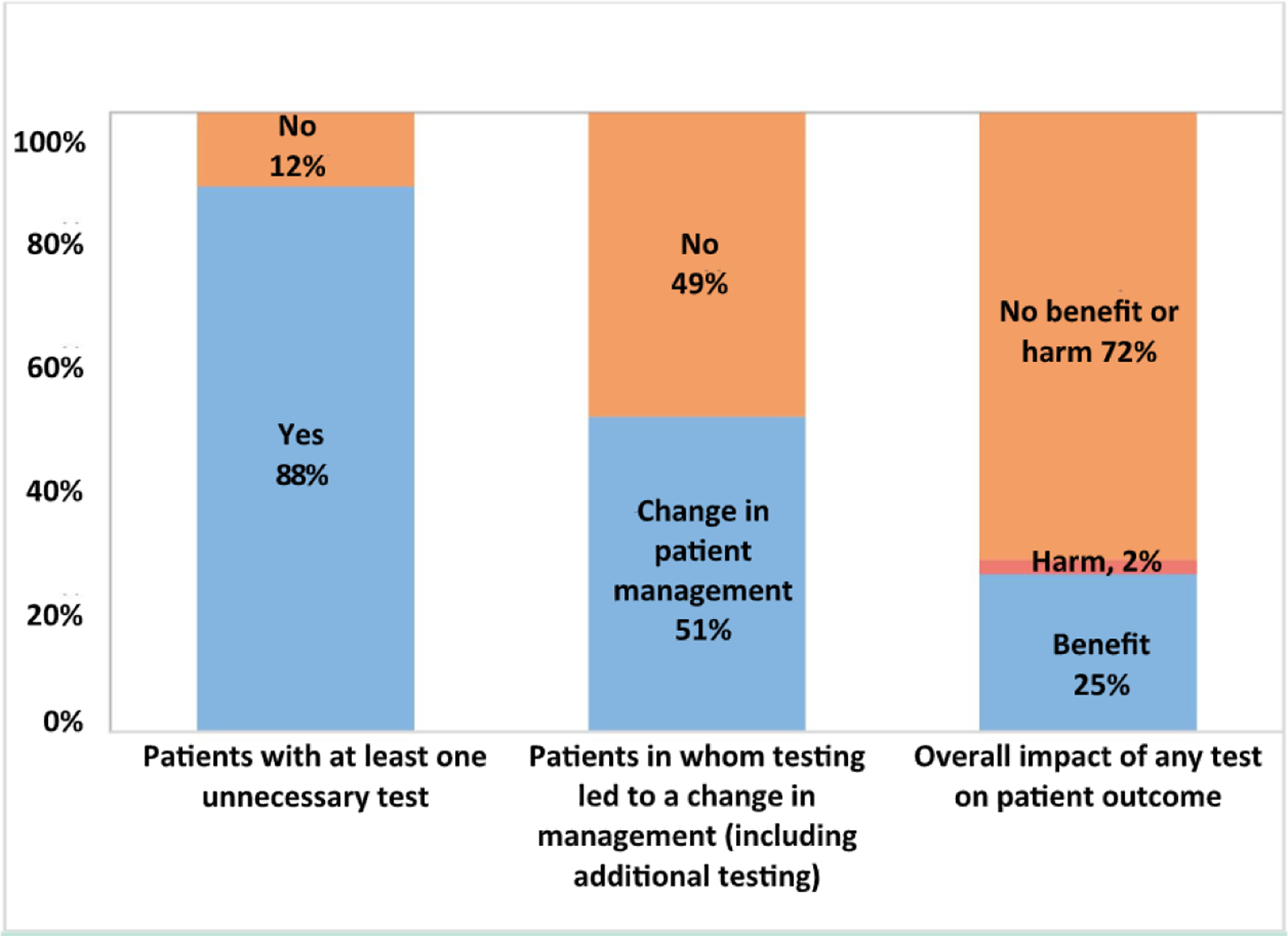
Proportion of patients with at least one unnecessary test based on chart review, frequency with which testing led to a change in patient management and the overall outcome of testing on patients.
The most commonly ordered tests were chemistry 7 panel (100%, 177/177), complete blood count (98.9%, 175/177), prothrombin time (PT)/partial thromboplastin time ([PTT] 73.4%, 130/177), electrocardiogram (72.8%, 129/177), and liver function tests ([LFTs] 68.9%, 122/177). Tests most commonly unnecessary were PT/PTT, 67% (87/130) unnecessary; LFTs, 59% (72/122) unnecessary; urinalysis, 50% (50/100) unnecessary; and lactate, 49% (26/53) unnecessary (Table).
Table.
Frequency of Unnecessary Tests by Chart Review (Total 177 Patients) and Tests Not Identified as Having Been Performed by Frontline Providers (49 Patients)
| Test Type | Frequency of Unnecessary Tests (Chart Review) | Frequency of Unnecessary Tests (per Frontline Providers) | Frequency Tests Were Missed by Frontline Providers |
|---|---|---|---|
| Laboratory tests | |||
| PT/PTT | 67% (87/130) | 75% (15/20) | 47% (18/38) |
| Liver function tests | 59% (72/122) | 67% (12/18) | 49% (17/35) |
| Urinalysis | 50% (50/100) | 45% (9/20) | 29% (8/28) |
| Lactate | 49% (26/53) | 14% (1/7) | 46% (6/13) |
| Troponin | 29% (15/52) | 42% (5/12) | 20% (3/15) |
| BNP | 18% (6/34) | 0% (0/5) | 50% (5/10) |
| Chemistry 7 panel | 3% (6/177) | 6% (3/47) | 2% (1/49) |
| Complete blood count (CBC) | 3% (5/175) | 6% (3/47) | 0% (0/47) |
| Imaging tests | |||
| Chest x-ray | 42% (44/106) | 42% (8/19) | 27% (7/26) |
| Lower extremity ultrasound | 33% (2/6) | 50% (1/2) | 50% (2/4) |
| CT head | 29% (11/38) | 25% (1/4) | 56% (5/9) |
| ECG | 23% (30/129) | 29% (6/21) | 45% (17/38) |
| Abdominal x-ray | 20% (2/10) | 0% (0/3) | 25% (1/4) |
| CT chest | 15% (5/34) | 14% (1/7) | 0% (0/7) |
| Abdominal ultrasound | 13% (1/8) | 50% (1/2) | 0% (0/2) |
| Transthoracic echocardiogram | 12% (2/17) | 0% (0/4) | 33% (2/6) |
| CT abdomen | 11% (3/27) | 0% (0/5) | 17% (1/6) |
| MRI of the head | 0% (0/2) | N/A | N/A |
| Microbiology tests | |||
| Urine culture | 44% (17/39) | 20% (1/5) | 44% (4/9) |
| Blood culture | 36% (15/42) | 38% (3/8) | 11% (1/9) |
BNP = brain natriuretic peptide; CT = computerized tomography; ECG = electrocardiogram; MRI = magnetic resonance imaging; N/A = test not performed on patients cared for by frontline providers; PT/PTT = prothrombin time/partial thromboplastin time.
Frontline Provider Interviews
A sub-sample of frontline providers for 49 patients were administered a questionnaire. Frontline providers were unaware of 39% of tests per patient that actually occurred (3.7/9.4 tests). The most commonly missed tests were PT/PTT 47.4% (18/ 38), LFTs 48.6% (17/35), lactate 46.2% (6/13), and electrocardiograms 44.7% (17/38). A total of 71.4% (35/49) of patients had a test their frontline physicians deemed to be either somewhat or absolutely unnecessary. Based on frontline physician judgment, after removing the 38.7% of tests that were missed (179/462), 27.2% (77/283) of all tests ordered were thought to be unnecessary. Overall, 55.4% (256/462) of all tests were either missed or reported as unnecessary by frontline providers. Frontline providers tended to miss tests that were identified as unnecessary by physician review. Of all tests that were missed by physicians, 52% (93/179) were found to be unnecessary (score of 1 or 2) on chart review.
CONCLUSIONS
We found that most patients experience unnecessary testing on the first day of an inpatient hospital stay. Around one-third of all tests were unnecessary by physician chart review. The most frequent types of unnecessary tests were laboratory tests. Beyond tests that were unnecessary by clinical guidelines, many appropriate tests did not change clinical care. Over the entire sample, 72% of patients did not have their care changed by testing.
Interestingly, frontline physicians reported similar results as reviewers that the majority of patients had at least one unnecessary test ordered, and around one-third of all tests were unnecessary. Additionally, these physicians were unaware of 39% of tests ordered on their own patients, the majority being the tests most commonly rated as unnecessary by chart review, including PT/PTT, LFTs, and lactate. Frontline physicians were unaware of a test being done or thought the test was unnecessary for more than half of all tests performed. Examples of unnecessary tests identified included a hypercoagulable work-up sent for a provoked pulmonary embolism, and magnetic resonance imaging of the spine for acute uncomplicated low back pain. Both of these examples directly contradict campaigns such as the ABIM Foundation’s Choosing Wisely and the American College of Physicians High-Value Care.9,10 There were multiple reasons for unnecessary testing. Tests were often ordered as part of a triage protocol initiated when a patient was first seen in the Emergency Department.11,12
Unnecessary testing has detrimental effects for patients as well as financial and operational implications to the health care system. Patients had on average 9 tests ordered in the first 24 hours, with 1 patient having 20 tests in this timeframe. Overall, 72% of patients had no change in management based on testing. This finding is consistent with other studies in outpatient medicine, finding testing aided in making a diagnosis in only 10%−20% of outpatients.13 Harms of testing noted included elevated white blood cell count or elevated lactate level in the absence of clinical infection; signs or symptoms led to unnecessary antibiotic usage in multiple patients. Many tests were judged to be necessary even though they did not change patient management. Tests with normal results can be helpful in screening or ruling out underlying disease processes.
Unnecessary tests can also lead to a cascade of events initiated by an unnecessary test resulting in additional tests or treatment that may cause harm as the results are pursued. One patient in our review had an inappropriately ordered D-dimer test. The abnormal result led to chest computed tomography (CT) angiography. The CT angiography found an incidental pulmonary nodule. Since the initial scan, the patient has undergone 2 additional CT scans and is scheduled for evaluation and possible biopsy.
This study was limited by the convenience sampling of patients, the subjective nature of assigning necessity of tests, and focusing on the first 24 hours of hospitalization. Our methods likely led to a conservative estimate of whether harms occurred due to testing. Likewise, tests that did not explicitly change patient management on review may have helped clinicians rule out disease at the time of being ordered. Strengths of this study include physician chart review and real-time interview with treating frontline providers.
Our study found most patients receive tests deemed to be unnecessary, and frontline physicians were often unaware of testing or reports that tests are unnecessary. Testing modified care for only a minority of patients. Current practice likely represents overtesting, and testing can likely be reduced without negative impact on patients.
Funding:
Department of Veterans Affairs (DJM).
Footnotes
Conflict of Interest: DJM is supported by the VA Health Services Research & Development (12–307) and the Agency for Healthcare Research and Quality (R01 HS025456–01), and has received editorial honoraria from Springer for serving as a book and journal editor. Other authors report no potential conflicts of interest.
References
- 1.Zhi M, Ding EL, Theisen-Toupal J, Whelan J, Amaout R. The landscape of inappropriate laboratory testing: a 15-year meta-analysis. PLoS One. 2013;8(11):e78962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Miyakis S, Karamanof G, Liontos M, Mountokalakis TD. Factors contributing to inappropriate ordering of tests in an academic medical department and the effect of an educational feedback strategy. Postgrad MedJ. 2006;82(974):823–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rehmani R, Amanullah S. Analysis of blood tests in the emergency department of a tertiary care hospital. Postgrad Med J. 1999;75:662–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nguyen LT, Sullivan CT, Makam AN. The diagnostic cascade of incidental findings: a teachable moment. JAMA Intern Med. 2015;175(7): 1089–1090. [DOI] [PubMed] [Google Scholar]
- 5.Brennan TA, Leape LL, Laird NM, et al. Incidence of adverse events and negligence in hospitalized patients: results of the Harvard Medical Practice Study I. N Engl J Med. 1999;324(6):370–376. [DOI] [PubMed] [Google Scholar]
- 6.Judd H, Chase M. Evaluation of the adult with chest pain in the emergency department. In: Post T, ed. UpToDate. Waltham, MA: UpToDate Inc.; 2017. Available at: www.uptodate.com. Accessed January 1, 2017. [Google Scholar]
- 7.Ahmed A, Graber M. Evaluation of the adult with dyspnea in the emergency department. In: Post T, ed. UpToDate. Waltham, MA: UpToDate Inc.; 2017. Available at: www.uptodate.com. Accessed January 1, 2017. [Google Scholar]
- 8.Canzoniero JV, Afshar E, Hedian H, Koch C, Morgan DJ. Unnecessary hospitalization and related harm for patients with low-risk syncope. JAMA Intern Med. 2015; 175(6): 1065–1067. [DOI] [PubMed] [Google Scholar]
- 9.Cassel CK, Guest JA. Choosing wisely: helping physicians and patients make smart decisions about their care. JAMA. 2012;307(17): 1801–1802. [DOI] [PubMed] [Google Scholar]
- 10.Owens DK, Qaseem A, Chou R, Shekelle P. High-value, cost-conscious health care: concepts for clinicians to evaluate the benefits, harms, and costs of medical interventions. Ann Intern Med. 2011; 154(3): 174–180. [DOI] [PubMed] [Google Scholar]
- 11.Rowe B, Villa-Roel C, Guo X, et al. The role of triage nurse ordering on mitigating overcrowding in emergency departments: a systematic review. Acad Etnerg Med. 2011;18(12): 1349–1357. [DOI] [PubMed] [Google Scholar]
- 12.Retezar R, Bessman E, Ding R, et al. The effect of triage diagnostic standing orders on emergency department treatment time. Ann Emerg Med. 2011;57:89–99, e2. [DOI] [PubMed] [Google Scholar]
- 13.Kroenke K A practical and evidence-based approach to common symptoms: a narrative review. Ann Intern Med. 2014;161:579–586. [DOI] [PubMed] [Google Scholar]


