Abstract
OBJECTIVE.
To directly observe healthcare workers in a nursing home setting to measure frequency and duration of resident contact and infection prevention behavior as a factor of isolation practice.
DESIGN.
Observational study.
SETTING AND PARTICIPANTS.
Healthcare workers in 8 VA nursing homes in Florida, Maryland, Massachusetts, Michigan, Washington, and Texas.
METHODS.
Over a 15-month period, trained research staff without clinical responsibilities on the units observed nursing home resident room activity for 15–30-minute intervals. Observers recorded time of entry and exit, isolation status, visitor type (staff, visitor, etc), hand hygiene, use of gloves and gowns, and activities performed in the room when visible.
RESULTS.
A total of 999 hours of observation were conducted across 8 VA nursing homes during which 4,325 visits were observed. Residents in isolation received an average of 4.73 visits per hour of observation compared with 4.21 for nonisolation residents (P < .01), a 12.4% increase in visits for residents in isolation. Residents in isolation received an average of 3.53 resident care activities per hour of observation, compared with 2.46 for residents not in isolation (P < .01). For residents in isolation, compliance was 34% for gowns and 58% for gloves. Healthcare worker hand hygiene compliance was 45% versus 44% (P = .79) on entry and 66% versus 55% (P < .01) on exit for isolation and nonisolation rooms, respectively.
CONCLUSIONS.
Healthcare workers visited residents in isolation more frequently, likely because they required greater assistance. Compliance with gowns and gloves for isolation was limited in the nursing home setting. Adherence to hand hygiene also was less than optimal, regardless of isolation status of residents.
Older adults in nursing homes are predisposed to healthcare-associated infections due to a multitude of risk factors including multiple comorbid conditions, indwelling devices, more frequent hospital visits, functional impairment, and increased use of medications including antibiotics.1,2 An estimated 2 million infections occur in US nursing homes each year, increasing mortality, antibiotic resistance, and healthcare costs.1–5 Methicillin-resistant Staphylococcus aureus (MRSA) is the most common pathogenic organism, and up to 58% of nursing home residents are reported to be colonized with MRSA.4,6,7 In healthcare settings, MRSA is mainly spread by person-to-person contact, most often between healthcare workers (HCWs) and patients, and by indirect contact with contaminated environmental surfaces and fomites. Many acute-care hospitals attempt to limit the spread of MRSA and other multidrug-resistant organisms (MDROs) by using contact precautions for patients colonized or infected with MRSA.8 In nursing homes, contact precautions are less desirable because of the communal setting and the emphasis on a homelike environment. Potential disadvantages of placing nursing home residents in isolation include stigmatizing residents, fewer HCW visits, increased costs, and greater burden on staff.9–13 Using isolation on nursing home residents might undermine the goal of emulating a homelike setting, creating significant challenges for infection prevention programs.
The Department of Veterans Affairs (VA) operates 133 community living centers (nursing homes), which provide care for up to 12,000 veterans per day.6,14 In these nursing homes, the VA is committed to providing veteran residents with long-term, skilled nursing and rehabilitative care in a homelike setting. The VA practice differs from most non-VA nursing homes, where active surveillance is rarely performed and under a third report using isolation for residents with MDRO carriage.12,16
In this study, our objective was to conduct direct observation of HCWs in the nursing home setting to measure frequency and duration of resident contact and infection prevention behavior as a factor of isolation status.
METHODS
This observational study was conducted over 15 months (February 2016 to April 2017) in 24 skilled nursing units in 8 VA nursing homes in 6 states: Miami, Florida; Boston, Massachusetts; Ann Arbor, Michigan; Baltimore, Maryland; Perry Point, Maryland; Vancouver, Washington; Kerrville, Texas; and San Antonio, Texas. Hospice and palliative care only units were excluded from observation. The VA Central Institutional Review Board deemed the study exempt from approval under category 2. During the study period, all VA nursing home facilities were required to perform MRSA active surveillance culturing on admission and to implement barrier precautions (often referred to as isolation) including gowns and gloves for most care of colonized or infected residents or contact with their environment.15
Direct Observation
Trained research staff who did not have clinical responsibilities on the units randomly selected nursing home rooms from a list of rooms at their site. All observers completed “secret shopper” observation training with the data collection tool and worked with a supervising local primary investigator. Each observation lasted 15–30 minutes. Observers recorded time of entry and exit, isolation status, visitor type (HCW, staff, visitor, etc), hand hygiene, use of gloves and gowns, and care activities performed in the room when visible using a standard form. Care activities observed were bathing, hygiene, toileting, feeding, dressing change, transfer, IV care, medications, Foley catheter care, physical exam, glucose monitoring, physical therapy, occupational therapy, and respiratory care. Observations did not include resident–provider encounters outside resident rooms.
For this study, nursing home staff and visitors were considered compliant with isolation precautions if they donned gloves and gowns at time of room entry or were observed using gowns and gloves within the resident room when care activities were observed or the environment was touched. Nursing home staff and visitors were considered compliant with hand hygiene if hand hygiene was performed immediately before or after entering or exiting a resident room during observations where any care activities were observed or the environment was touched. We did not observe all World Health Organization (WHO) 5 Moments for Hand Hygiene because in-room observation would not be possible without being conspicuous.17 We did not inform nursing home staff of observation.
We defined HCWs as medical doctors or medical students (MDs), registered nurses (RNs), or patient care technicians (PCs). All other visitors were considered non-HCWs.
Isolation Precautions
We collected and reviewed the isolation policies from each participating nursing home. All nursing homes have similar policies for infection control precautions for MDRO residents, as recommended by the VA.15
Statistical Analyses
The average number of visits per hour of observation was calculated. Care activities were calculated as a proportion of total visits. Visits per hour and care activities were compared between isolation and nonisolation observations using the Wilcoxon rank-sum test after testing the normality of the distribution. Compliance with hand hygiene was calculated as a proportion of hand hygiene observed of opportunities observed and compared between isolation and nonisolation observations using a χ2 test. Statistical analyses were performed using SAS version 9.3 software (SAS Institute, Cary, NC).
RESULTS
In-Room Observation Data
In total, 999 hours of observation were conducted across 8 VA nursing homes, during which 4,325 visits were observed. The hours observed at each site ranged between a minimum of 35 hours and a maximum of 222 hours, with a median of 114 hours per site. Observations occurred between 7:00 AM and 6:00 PM. There were 677 hours observed for rooms of residents not in isolation and 322 hours observed for rooms of residents in isolation. Of 4,325 visitors observed, 3,084 (70%) were HCWs.
Frequency and Duration of Visits
Residents on any type of isolation received an average of 4.73 visits per hour of observation compared with 4.21 for nonisolation residents (P < .01), a 12.4% increase in visits for residents in isolation (Table 1). A similar result was seen in average number of HCW visits per hour, which were 15.1% higher in residents in isolation than those who were not (3.43 vs 2.98; P < .01). Non-HCW visits per hour were not significantly different, averaging 1.22 visits per hour in nonisolation residents and 1.30 in residents in isolation (P = .12).
TABLE 1.
Visits Per Hour and Minutes of Healthcare Worker (HCW) Contact by HCW Type for Isolated and Nonisolated Residents
| Visits Per Person Hour |
Minutes of Contact Per Person Hour |
|||||
|---|---|---|---|---|---|---|
| HCW Type | Isolation | Nonisolation | P Value | Isolation | Nonisolation | P Value |
| Overall | 4.73 | 4.21 | < .01 | 22.1 | 19.9 | < .01 |
| All HCWs | 3.43 | 2.98 | < .01 | 16.1 | 12.6 | < .01 |
| Provider (MD) | 0.36 | 0.31 | .77 | 1.97 | 1.70 | .98 |
| Nurse (RN) | 1.57 | 1.56 | .25 | 6.70 | 6.00 | .03 |
| Other (PC) | 1.50 | 1.11 | < .01 | 7.50 | 4.90 | < .01 |
| Non-HCWs | 1.30 | 1.22 | .12 | 5.90 | 7.30 | .20 |
NOTE. MD, medical doctor; RN, registered nurse; PC, patient care technician.
For every hour of observation, residents on any type of isolation received an average of 22.1 visit minutes compared with 19.9 visit minutes for residents not in isolation (P < .01). Healthcare worker visit minutes per hour were in line with this finding. Those in isolation received an average of 16.1 HCW visit minutes per hour compared with 12.6 for residents not in isolation (P < .01). Non-HCW visit minutes per hour were not significantly different, averaging 5.9 for residents in isolation compared with 7.3 visit-minutes per hour for residents not in isolation (P = .20).
Resident Care Activities
Residents in isolation received, on average, 3.53 resident care activities per hour of observation, compared with 2.46 for residents not in isolation (P < .01). The 5 most common resident care activities were the same for residents in isolation and nonisolation. For residents in isolation, the most common care activities in order were (1) oral medication, (2) assistance with toileting, (3) hygiene, (4) transfer, and (5) physical exam. For residents not in isolation, the most common care activities were (1) oral medication, (2) transfer, (3) physical exam, (4) assistance with toileting, and (5) hygiene. For all of these activities except for physical exam, residents in isolation had significantly higher numbers of activities performed when compared with residents not in isolation (Table 2).
TABLE 2.
Proportion of Healthcare Worker (HCW) Contact by Type of Resident Care and Isolation Status
| Isolation Visits (N = 1,498) |
Nonisolation Visits (N = 2,827) |
||
|---|---|---|---|
| Type of Resident Care | Proportion of Visits With Resident Care, No. (%) | Proportion of Visits With Resident Care, No. (%) | P Value |
| Oral medication | 223 (14.9) | 339 (12.0) | <.01 |
| Assistance with toileting | 153 (10.2) | 165 (5.8) | <.01 |
| Hygiene | 123 (8.2) | 162 (5.7) | <.01 |
| Transfer | 124 (8.3) | 182 (6.4) | .01 |
| Physical exam | 112 (7.5) | 192 (6.8) | .20 |
Gown and Glove Compliance
For residents in isolation, gowns and gloves were indicated when resident care was given or the environment was touched (N = 1,368). For residents in isolation, gowns were worn for 469 of 1,368 visits (34%), and gloves were worn for 793 of 1,368 visits (58%). For residents not in isolation where neither gowns nor gloves were required, gowns were worn for 62 of 2,538 visits (2.4%), and gloves were worn for 946 of 2,538 visits (37.3%).
Hand Hygiene
Hand hygiene opportunities were defined as observed entry and/ or exit to resident rooms during a visit where resident care was given or the environment was touched. (Figure 1; Table 3). The overall compliance rate with hand hygiene on room entry was 38% (1,113 of 2,920 observed opportunities) and was 50% (1,476 of 2,930) on room exit. For residents in isolation, the compliance rate was 38% (399 of 1,047) on room entry and was 54% (558 of 1,024) on room exit. For residents not in isolation, the compliance rate was 38% (714 of 1,873) on room entry and was 48% (918 of 1,906) on room exit. Hand hygiene compliance on entry between residents in isolation and residents not in isolation was the same (38% vs 38%; P = .99). On room exit, hand hygiene compliance was significantly better for residents in isolation than residents not in isolation (54% vs 48%; P < .01).
FIGURE 1.
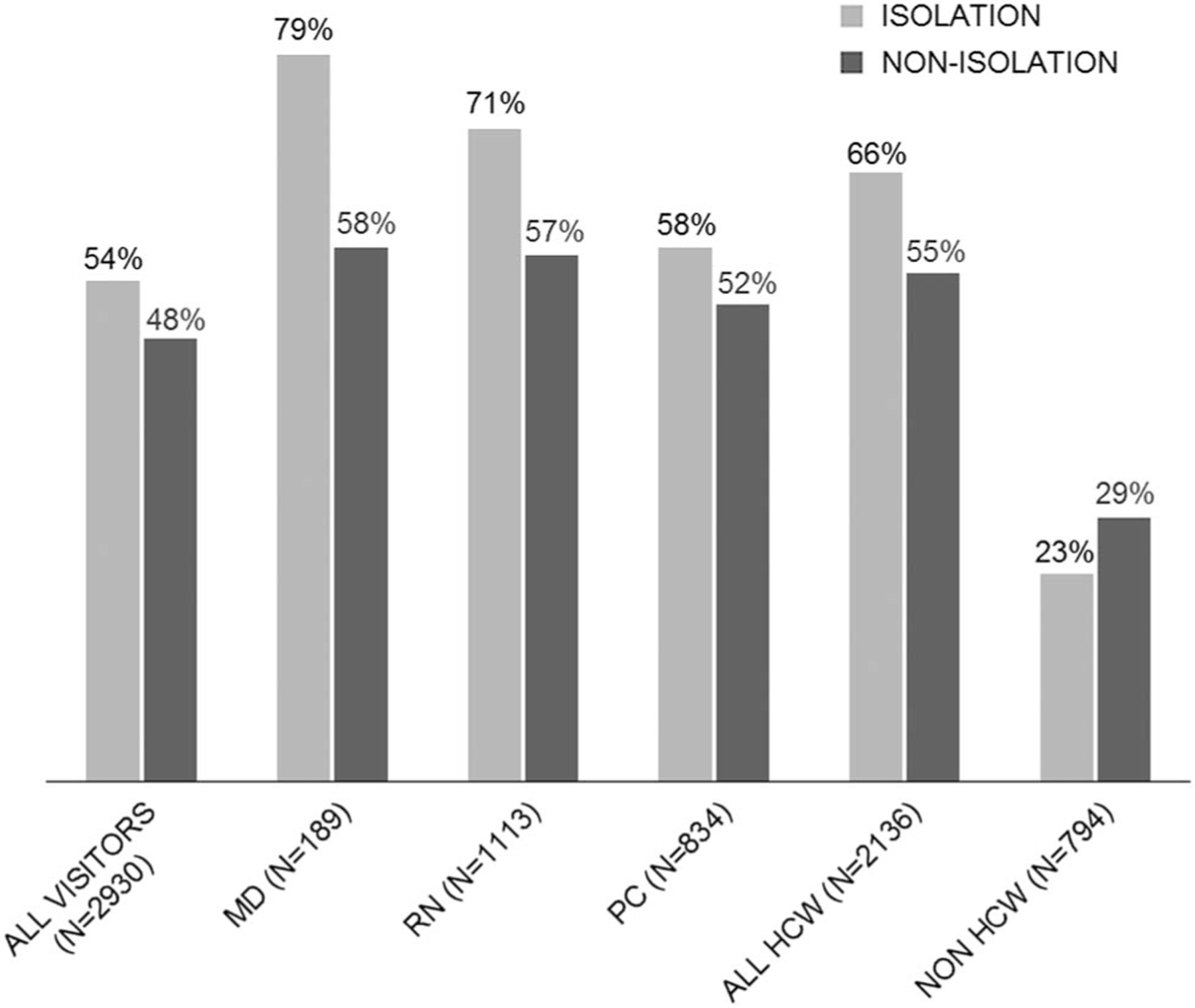
Hand hygiene compliance on exit for isolation versus nonisolation status by type of healthcare worker. NOTE. HCW, healthcare worker; MD, HCW provider; RN, registered nurse; PC, patient care technician.
TABLE 3.
Hand Hygiene (HH) Compliance on Room Entry and Exit by Type of Visitor for Residents in Isolation Versus Nonisolation
| HH Entry Compliance |
HH Exit Compliance |
|||||
|---|---|---|---|---|---|---|
| Isolation, n/N (%) | Nonisolation, n/N (%) | P Value | Isolation, n/N (%) | Nonisolation, n/N (%) | P Value | |
| Overall | 399/1,047 (38) | 714/1,873 (38) | .99 | 558/1,024 (54) | 918/1,906 (48) | < .01 |
| All HCWs | 338/758 (45) | 594/1,350 (44) | .79 | 495/746 (66) | 770/1,390 (55) | < .01 |
| Provider (MD) | 42/75 (56) | 52/103 (50) | .47 | 57/72 (79) | 68/117 (58) | < .01 |
| Nurses (RN) | 181/357 (51) | 363/745 (49) | .54 | 253/356 (71) | 434/757 (57) | < .01 |
| Other (PC) | 115/326 (35) | 179/502 (36) | .91 | 185/318 (58) | 268/516 (52) | .08 |
| Non-HCWs | 61/289 (21) | 120/523 (23) | .54 | 63/278 (23) | 148/516 (29) | .07 |
NOTE. HCW, healthcare worker; MD, medical doctor; RN, registered nurse; PC, patient care technician.
DISCUSSION
This study describes the effect of isolation precautions on HCW resident interactions across 8 VA nursing homes in the United States. Residents were primarily in isolation due to MRSA colonization. Isolated residents generally required more care and were seen more often by HCWs. Moreover, HCWs wore gowns 34% of the time and wore gloves 58% of the time when caring for residents in isolation. Gloves were worn during the care of 37% of nonisolated residents. Overall hand hygiene compliance was 38% on entry and 50% on exit. Encouragingly, hand hygiene compliance was clearly better for HCWs versus non-HCWs. Also, HCW compliance with hand hygiene was slightly higher after visiting isolated residents.
Residents in isolation received more HCW visits than residents not in isolation. Studies of acute care have consistently found fewer visits for residents who were in isolation, presumably due to the effort required to don gloves and gowns.18,19 We hypothesize that more contact was observed because residents colonized with antibiotic-resistant bacteria may be more dependent on staff for care and assistance with activities of daily living (ADLs). In this study, residents in isolation received more visits for hygiene, toilet assistance, transfers and giving oral medications, mostly from patient care technicians and nurses, supporting this hypothesis. Also, in a large retrospective study of non-VA nursing homes, Cohen et al12 found that less independence with ADLs was associated with isolation.
The rate of compliance with gowns and gloves was low, but it was consistent with other studies of resident isolation.20,21 Likewise, compliance with hand hygiene was lower than often reported; however, our compliance rate was within the range of what is reported when more rigorous, secret shopper methodology is used.1,22 Notably, patient care technicians have a low compliance with hand hygiene that was not impacted by isolation status; this may indicate an opportunity for further education in this group. Our findings of lower compliance on entry as well as a small increase in compliance on exit when residents are isolated was consistent with other studies.23,24 The finding that hand hygiene increased after glove use could be due to the HCW perceptions of being more contaminated after caring for residents on isolation. Previous studies in acute-care settings yielded similar results.18,25 These findings suggest that focusing efforts on proper precautions during high risk for contamination activities and basic hand hygiene rather than resident-directed activities may be useful. In late 2016, the VA revised its Community Living Center MRSA Prevention Initiative to define certain activities (eg, giving oral medications as “low risk” for transmission) that do not require gowns and gloves, reducing the burden on HCWs.26 However, gowns and gloves are still recommended for most care activities for residents colonized or infected with MRSA or other antibiotic resistant bacteria.
One limitation of our study may have been the use of “secret shoppers.” In reality, these observers were most likely recognized as some type of external monitor given the relatively small staff and less busy hallways at nursing homes compared to acute-care facilities. However, being recognized as an observer would be expected to have increased compliance due to the Hawthorne effect. Another limitation is that observations did not include the evening shift when less staffing may affect compliance with isolation and hand hygiene.
Additionally, our results may not generalize to non-VA nursing homes as the approach to isolation in the VA is more comprehensive than most nursing homes, using both active surveillance for MRSA and gowns and gloves for most care of residents found to be positive. Although we were not able to observe the WHO Five Moments of Hand Hygiene, we were able to limit hand hygiene compliance opportunities to visits where resident care was performed or the environment was touched, eliminating instances where hand hygiene may not be indicated. Also, all observations were of residents in their rooms. Residents in nursing homes have many interactions in common areas which potentially may play a greater role in transmission. A strength of our study was the rigor of independent observation; we formally trained research staff for observations and standardized data collection in 8 geographically diverse nursing homes.
In summary, a comprehensive approach to the use of contact precautions in nursing homes was associated with limited compliance with gown and glove use, did not appear to negatively affect frequency of visits and was associated with improved hand hygiene. However, adherence to hand hygiene was less than optimal, regardless of the isolation status of residents.
ACKNOWLEDGMENTS
We would like to thank the study coordinators Jwan Mohammadi (Oregon), Diana Sams (Michigan), Melissa Hibner (Texas), Carol Ramos (Florida), Alexandra Rochman (Massachusetts), Corey Lonberger (Massachusetts), Makaila Decker (Massachusetts), and Georgia Papaminas (Maryland). The contents do not represent the views of the US Department of Veterans Affairs or the United States Government.
Financial support: This work was supported by Collaborative Research to Enhance and Advance Transformation and Excellence (CREATE) Initiative (grant no. HX-12–018) and Merit Review (grant no. I01 HX001128) from the United States Department of Veterans Affairs Health Services Research and Development Service (HSR&D).
Footnotes
Potential conflicts of interest: All authors report no conflicts of interest relevant to this article.
REFERENCES
- 1.Montoya A, Mody L. Common infections in nursing homes: a review of current issues and challenges. Aging Health 2011;7:889–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Strausbaugh LJ, Joseph CL. The burden of infection in long-term care. Infect Control Hosp Epidemiol 2000;21:674–679. [DOI] [PubMed] [Google Scholar]
- 3.Cassone M, Mody L. Colonization with multi-drug resistant organisms in nursing homes: scope, importance, and management. Curr Geriatr Rep 2015;4:87–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dantes R, Mu Y, Belflower R, et al. National burden of invasive methicillin-resistant Staphylococcus aureus infections, United States, 2011. JAMA Intern Med 2013;173:1970–1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Herzig CTA, Dick AW, Sorbero M, et al. Infection trends in US nursing homes, 2006–2013. J Am Med Dir Assoc 2017;18: 635.e9–635.e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Evans ME, Kralovic SM, Simbartl LA, et al. Nationwide reduction of health care-associated methicillin-resistant Staphylococcus aureus infections in Veterans Affairs long-term care facilities. Am J Infect Control 2014;42:60–62. [DOI] [PubMed] [Google Scholar]
- 7.Stone ND, Lewis DR, Johnson TM 2nd, et al. Methicillin-resistant Staphylococcus aureus (MRSA) nasal carriage in residents of Veterans Affairs long-term care facilities: role of antimicrobial exposure and MRSA acquisition. Infect Control Hosp Epidemiol 2012;33:551–557. [DOI] [PubMed] [Google Scholar]
- 8.Siegel JD, Rhinehart E, Jackson M, Chiarello L, Healthcare Infection Control Practices Advisory Committee. Management of multidrug-resistant organisms in healthcare settings. Am J Infect Control 2007;35(10 Suppl 2):S165–S193. [DOI] [PubMed] [Google Scholar]
- 9.Morgan DJ, Diekema DJ, Sepkowitz K, Perencevich EN. Adverse outcomes associated with contact precautions: a review of the literature. Am J Infect Control 2009;37:85–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Morgan DJ, Wenzel RP, Bearman G. Contact precautions for endemic MRSA and VRE: time to retire legal mandates. JAMA 2017;318:329–330. [DOI] [PubMed] [Google Scholar]
- 11.Furuno JP, Krein S, Lansing B, Mody L. Health care worker opinions on use of isolation precautions in long-term care facilities. Am J Infect Control 2012;40:263–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cohen CC, Dick A, Stone PW. Isolation precautions use for multidrug-resistant organism infection in nursing homes. J Am Geriatr Soc 2017;65:483–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dumyati G, Stone ND, Nace DA, Crnich CJ, Jump RL. Challenges and strategies for prevention of multidrug-resistant organism transmission in nursing homes. Curr Infect Dis Rep 2017;19 18–017-0576–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tsan L, Langberg R, Davis C, et al. Nursing home-associated infections in Department of Veterans Affairs community living centers. Am J Infect Control 2010;38:461–466. [DOI] [PubMed] [Google Scholar]
- 15.Department of Veterans Affairs. Revised guideline for implementation of the VHA MRSA prevention initiative in community living centers Unpublished internal document, 2013. [Google Scholar]
- 16.Ye Z, Mukamel DB, Huang SS, Li Y, Temkin-Greener H. Healthcare-associated pathogens and nursing home policies and practices: results from a national survey. Infect Control Hosp Epidemiol 2015;36:759–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chang NC, Reisinger HS, Jesson AR, et al. Feasibility of monitoring compliance to the My 5 Moments and Entry/Exit hand hygiene methods in US hospitals. Am J Infect Control 2016;44:938–940. [DOI] [PubMed] [Google Scholar]
- 18.Harris AD, Pineles L, Belton B, et al. Universal glove and gown use and acquisition of antibiotic-resistant bacteria in the ICU: a randomized trial. JAMA 2013;310:1571–1580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morgan DJ, Pineles L, Shardell M, et al. The effect of contact precautions on healthcare worker activity in acute care hospitals. Infect Control Hosp Epidemiol 2013;34:69–73. [DOI] [PubMed] [Google Scholar]
- 20.Dhar S, Marchaim D, Tansek R, et al. Contact precautions: more is not necessarily better. Infect Control Hosp Epidemiol 2014;35:213–221. [DOI] [PubMed] [Google Scholar]
- 21.Anderson DJ, Weber DJ, Sickbert-Bennett E. On contact precautions: the good, the bad, and the ugly. Infect Control Hosp Epidemiol 2014;35:222–224. [DOI] [PubMed] [Google Scholar]
- 22.Schweon SJ, Edmonds SL, Kirk J, Rowland DY, Acosta C. Effectiveness of a comprehensive hand hygiene program for reduction of infection rates in a long-term care facility. Am J Infect Control 2013;41:39–44. [DOI] [PubMed] [Google Scholar]
- 23.Thompson BL, Dwyer DM, Ussery XT, Denman S, Vacek P, Schwartz B. Handwashing and glove use in a long-term-care facility. Infect Control Hosp Epidemiol 1997;18:97–103. [DOI] [PubMed] [Google Scholar]
- 24.Mody L. Infection control issues in older adults. Clin Geriatr Med 2007;23:499–514, vi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Almaguer-Leyva M, Mendoza-Flores L, Medina-Torres AG, et al. Hand hygiene compliance in patients under contact precautions and in the general hospital population. Am J Infect Control 2013;41:976–978. [DOI] [PubMed] [Google Scholar]
- 26.Department of Veterans Affairs. Guidelines for standard and transmission-based precautions (formerly isolation) Unpublished internal document, 2016. [Google Scholar]


