Abstract
Introduction
Research indicates a link between adolescent e-cigarette use and combustible tobacco cigarette (CTC) initiation, and recent studies suggest their connection with marijuana uptake. Our 3-year longitudinal cohort study investigated the implications of adolescent, peer, and family e-cigarette use with adolescents’ expectations and willingness to initiate CTC use, and subsequent CTC and marijuana use.
Aims and Methods
Relationships were examined in a secondary analysis of a 3-year longitudinal cohort subsample involving adolescents enrolled in alternative California high schools (N = 1025). Analyses examined responses over three yearly observations. Family, peer, and respondents’ e-cigarette use, respondents’ positive cigarette expectancies and willingness to use CTCs were assessed in the study’s first year (T1). CTC use in the survey’s second year (T2) and marijuana use in the third year (T3) were assessed via path analysis.
Results
Respondents reporting at least one family member or peer using e-cigarettes were more likely to use e-cigarettes at T1 than those whose peers/family members did not. They reported more positive expectancies about CTCs and greater willingness to initiate use. These variables predicted CTC use at T2, which directly anticipated marijuana use in the survey’s third year (T3), as did adolescents’ use of e-cigarettes at T1. All model relations were statistically significant.
Conclusions
Analysis demonstrated the strong association of family members’ and peers’ behaviors with adolescent e-cigarette use, and the temporal precedence of e-cigarette use with subsequent CTC and marijuana uptake. The predictive implications of e-cigarettes for other dangerous substance use should be examined in future prevention campaigns.
Implications
The presented study expands upon existing literature connecting adolescent e-cigarette use and later CTC and marijuana use. The findings indicate the significant implications of exposure to e-cigarette use by parents and peers and demonstrate in a longitudinal 4-year panel survey the direct and indirect predictive implications of e-cigarette use for CTC and marijuana uptake. The research illustrates the utility of programs and campaigns that target peer and family groups to maximize impacts on adolescent willingness to try CTCs, positive expectancies, and possible onset of CTC and marijuana use.
Introduction
Few topics in public health today are as contentious as those involving the use of electronic cigarettes (also termed e-cigarettes, vapes, ENDS, etc.), handheld battery-operated devices that range from instruments resembling conventional combustible tobacco cigarettes (CTCs) to vape pens and vaporizers.1,2 Unlike CTCs that burn tobacco to generate smoke, e-cigarettes heat liquids containing nicotine, propylene glycol or glycerin, flavorings, and other compounds to create inhalable vapor. Both CTCs and e-cigarettes deliver nicotine, tobacco’s addictive agent, but e-cigarette manufacturers insist their products do not expose users to many chemical constituents responsible for tobacco-related diseases, thus offering the tantalizing prospect of reducing the harms of CTCs, a leading cause of preventable death and disability worldwide.2,3 In addition to research on these claims, recent research also has focused attention on the association of e-cigarette use in adolescents and onset of CTC and marijuana use, the focus of present concerns.
Adolescent E-Cigarette Use
A Monitoring the Future (MTF) analysis of e-cigarette use by US adolescents found ever-use rates of 36% in 12th-grade students,4 representing a clear danger signal, as e-cigarettes may attract young smokers for whom regular CTC use is initially unappealing.5 Youth subsequently may become addicted to nicotine, and once smoking is normalized, transition to harmful tobacco products.6–8 Further, adolescents may be more prone than adults to nicotine addiction after e-cigarette exposure due to the nature of the still-developing brain, which during adolescence is especially sensitive to nicotine.9
The possibility that adolescent e-cigarette use may lead CTC use has been supported in prior research, with some studies examining the relation longitudinally.10,11 Soneji et al.10 examined this relationship in a meta-analysis of nine studies that supported the link between e-cigarette use and later CTC initiation. Their findings demonstrated the combined odds ratio for later CTC initiation was nearly four times greater for ever versus never e-cigarette users after controlling for known demographic, psychosocial, and behavioral risk factors.
Research also has examined the connection between e-cigarette use and marijuana initiation. Studies by Dai et al.12 and Audrain-McGovern et al.13 examined this link longitudinally, and both found that adolescents who reported ever using an e-cigarette were significantly more likely to report initiation of marijuana in 1- and 2-year follow-ups. These studies did not investigate motivators for CTC initiation.
Research has examined youths’ perceptions of e-cigarettes to identify potential usage motivators. Among many risk factors, attitudes and family or peer use of e-cigarettes have been identified as significant predictors of youth e-cigarette usage.14,15 These risk variables also have been identified as strong predictors of marijuana initiation. Variables implicated in marijuana initiation, which may follow from e-cigarette use, involve parent and peer behaviors, and attitudes, expectancies, and willingness to engage in risky behavior. Parental behaviors, for example, have been identified as critical in the initiation or prevention of psychotropic substance use.16 E-cigarette use by adolescents’ family members may influence e-cigarette initiation, which in turn may encourage CTC and marijuana use.16 Similarly, normative pressures in adolescence have been shown to affect marijuana usage, with noteworthy consequences for adolescent health.14,17–19 Attitudes toward marijuana and positive expectations of their effects also have been related strongly to usage.16,20
Family Influence
The impact of family substance use on adolescent initiation of CTC or marijuana use is well documented.21,22 Many studies have found substance use by immediate family members predicts uptake or concurrent use by adolescent family members.22,23 However, the association between family members’ and peers’ e-cigarette use on abstinent adolescents’ e-cigarette use has attracted only limited examination.23,24 Carey et al.24 found adolescents who reported having a family member who used e-cigarettes were significantly more likely to initiate e-cigarettes than those reporting no family member use. Lozano et al.25 examined this relationship in middle school students in Mexico. Their results indicated student susceptibility to e-cigarette use and self-reported e-cigarette use were higher in those reporting family members used e-cigarettes. However, after thoroughly examining the literature we have found no studies that have investigated the link between family e-cigarette use, self-reported e-cigarette use, and later use of CTCs and marijuana. The current study is designed to extend the literature on this linkage.
Overview and Hypotheses
Generalizing from the CTC–marijuana use literature, our study was designed to investigate to the role of self-reported e-cigarette use, peer and family e-cigarette use, and CTC expectations, attitudes, and willingness to enact risky behavior on adolescents’ susceptibility to subsequent CTC and marijuana use. Respondents were attendees of alternative high schools in California. These schools serve students unable to attend regular high schools for various reasons, including low school achievement, conduct problems, and substance use. As a group, these students are at considerably higher risk than those attending traditional high schools for a number of health-related problems, including use of psychoactive substances.26 For example, El-Shahawy et al.27 found self-reported past month CTC use among these students ranged between 36% and 42%, up to three times the average of Californian traditional high school students (13.6%). Our analysis was designed to extend this research by examining the longitudinal structural relations of e-cigarette exposure with CTC and marijuana use in this at-risk group. It examined predictive relationships at T1 between normative variables, and e-cigarette use with adolescent cigarette use in the second year of the study (T2) and marijuana use in study’s third year (T3).
Hypotheses
We hypothesize respondents with family members or peers reporting e-cigarette use will exhibit greater use of e-cigarettes (H1). Further, adolescents’ e-cigarette use will be associated with more positive expectancies toward CTCs (H2) and greater willingness to try them (H3). Willingness to try CTCs at T1 (H4) and positive cigarette expectancies at T1 (H5) will be positively associated with CTC use (H6) at T2. To examine and expand on previous findings on the direct link of e-cigarette use to later CTC and marijuana use, we hypothesize that adolescent e-cigarette use at T1 (H7) and adolescent CTC use at T2 (H8) will be directly and positively associated with marijuana use at T3.
Methods
Sampling
Data were collected for a longitudinal study examining the influence of point-of-sale advertising on the use of nicotine and tobacco products by alternative high school students in southern California.28 Information from the California Department of Education was used to identify 183 eligible alternative high schools. Schools were considered eligible if they had least 100 students and were within 100 miles of the program offices in Claremont, CA. After obtaining approval from the Claremont Graduate University Institutional Review Board, all 183 schools were contacted and invited to enroll in the 3-year longitudinal panel study. Of the 183 schools contacted, 33 agreed to participate; however, four schools were dropped from the study due to low participation during the consent process, leaving a final sample of 29 sites (16%) successfully participating.
Respondents and Procedure
Between October 14, 2014 and May 18, 2015, research staff distributed interest forms to 6870 high school students who attended one of the 29 schools; 2726 students returned forms. Students returning forms were assigned a staff member who obtained written consent and provided a link to a web-based survey. Parental consent and youth assent were obtained for students under the age of 18. Students and their parent(s) or guardian(s) were told the study concerned health behaviors and that respondents would be asked about underage tobacco and drug use. All students were given until September 1, 2015 to complete the approximately 90-minute survey. A total of 1060 students took part in the initial (T1) assessment. Each respondent received a $45 gift card to compensate them for their time.
Respondents were tracked using established procedures.28 One-year follow-up assessments (T2) were completed by 87.1% of the original sample (n = 923). Most of these respondents (96.6%) completed a web-based survey. Those without access to a web-enabled device (3.4%) completed a computer-assisted telephone interview. Among the 137 respondents who did not complete a follow-up assessment, 93.5% failed to respond to repeat contact attempts, 5.8% withdrew from the study, and 0.7% were incarcerated. Respondents received a $50 gift card for completing the 1-year follow-up.
Two-year follow-up assessments (T3) were completed by 81.0% of the original sample (n = 859). Most respondents (96.9%) completed a web-based survey, and some (3.1%) completed a computer-assisted telephone interview. Among the 201 respondents not completing an assessment, 93.0% failed to respond to repeated contact attempts, 4.5% withdrew from the study, 1.5% passed away, 0.5% were incarcerated, and 0.5% were deployed overseas after enrolling in the military. Respondents received a $100 gift card for completing the 2-year follow-up.
Measures
Demographics
Respondents reported age, sex, and ethnicity at T1.
Family E-Cigarette Use
Family e-cigarette use (T1) was assessed with one item: “Does anyone who lives with you now use electronic cigarettes, vaporizers, or vape pens?” Options were coded 0 (no) or 1 (yes). The measure was adapted from the Centers for Disease Control and Prevention’s National Youth Tobacco Survey (NYTS).29
Peer E-Cigarette Use
Peer e-cigarette use (T1) was examined by asking, “How many of your four closest friends use electronic cigarettes, vaporizers, or vape pens?” Responses ranged from 0 (none) to 4 (four). The measure was adapted from the California Department of Public Health (CDPH) 2011–2012 California student tobacco survey (CSTS).30
Positive Expectancies
Adolescents’ positive expectancies (T1; α = .97) about smoking CTCs were assessed using 12 items from the short form smoking consequences questionnaire (S-SCQ).31 Responses were assessed with 5-point Likert-type items whose options ranged from 1 (Extremely unlikely) to 5 (Extremely likely). Example items included, “Cigarettes taste good,” and “Cigarettes help reduce anxiety.” A mean score was computed—higher scores indicate more positive expectations.31
Willingness
Willingness to use CTCs (T1) was assessed by presenting respondents with the following item, “Suppose you were with a group of friends at a party and there were tobacco products there that you could try if you wanted. If it were offered by one of your friends, how willing would you be to try cigarettes?” Responses were based on a 4-point Likert-type item that ranged from 1 (Definitely No) to 4 (Definitely Yes).32
Adolescent Substance Use
A validated drug use questionnaire33 was adapted to query students on their use of CTCs, e-cigarettes, vaporizers, or vape pens, and marijuana in the past 30 days. Original response options ranged from 0 (0 times) to 10 (91 or more times) but were truncated to achieve a normal distribution. The final response scales ranged from 0 (0 times) to 3 (21 or more times). While the measure has not been validated for novel nicotine products such as vape pens, the measure has been used in prior studies comparing frequencies in at-risk groups reporting use of many addictive substances including CTCs and methamphetamine.34
Eligibility Criteria and Data Preparation
This prevention investigation focused on adolescent substance use; thus, students between the ages of 14 and 18 during the first assessment (T1) were considered eligible for participation. Thirty-five respondents falling beyond the age range were removed from the sample (resultant N = 1025). Distribution of the data was examined using measures of skew and kurtosis (ie, skew < 3, kurtosis < 10).35 Analysis revealed all variables within boundaries usually considered normal or acceptable. Multicollinearity was not an issue—the highest variance inflation factor was 2.33, which fell below the cutoff of 2.5.36
Analytic Plan
To examine potential clustering effects of school environment, an intraclass correlation was calculated in SPSS version 24, with marijuana use (T3) specified as the outcome variable. Findings revealed a minimal association between school and marijuana use (Intra-Class Correlations = .02), supporting inclusion of individuals as the unit of analysis.37
R statistical software was used for the remaining analyses. Several variables had missing data, common in longitudinal designs. Patterns of missingness are shown in Table 1. To correct for missing data bias, multiple imputation using 100 imputations was implemented under the conditions of missing at random (MAR) using R’s Mice package. A path model was tested using R’s (version 3.3.1) lavaan package with 100 imputed datasets and maximum-likelihood estimation. Age, sex, and ethnicity were added as covariates in the model; that is, paths from initial (T1) substance use (CTC, e-cigarette, and marijuana) to each outcome variable (positive expectancies and willingness T1, CTC use T2, and marijuana use T3) were estimated to control for initial level of use.38 Sex and ethnicity were dummy coded prior to model entry. The reference group for sex was female; non-Hispanic was the reference group for ethnicity. Prior use of e-cigarettes, CTCs, and marijuana at T1 also were entered to control for initial usage levels. Model fit was evaluated with three robust fit indices—the comparative fit index (CFI), Tucker–Lewis fit index (TFI), and root mean square error of approximation (RMSEA). For the CFI and TFI, scores close to 1.00 indicate good fit. The RMSEA indicates good fit if values are below .05.38
Table 1.
Same Characteristics and Statistics Measure Summary Information (N = 1025)
| Age | Range | 14–18 |
| M (SD)/missing | 17.40 (0.82)/n = 0 | |
| Sex | Male/female/missing | n = 522/ n = 499/n = 4 |
| Ethnicity | Non-Hispanic/Hispanic/missing | n = 250/ n = 752/n = 23 |
| Family e-cigarette use (T1) | No/yes/missing | n = 802/ n = 147/n = 76 |
| Peer e-cigarette use (T1) | M (SD)/missing | 1.25 (1.45)/n = 228 |
| Positive expectancies (T1) | M (SD)/missing | 1.92 (1.11)/n = 43 |
| Willingness (T1) | M (SD)/missing | 1.63 (1.01)/n = 32 |
| Adolescent e-cigarette use (T1; past 30 days) | 0 times | n = 780 |
| 1–10 times | n = 103 | |
| 11–20 times | n = 30 | |
| 21 or more times | n = 59 | |
| Missing | n = 53 | |
| Adolescent cigarette use (T1; past 30 days) | 0 times | n = 818 |
| 1–10 times | n = 78 | |
| 11–20 times | n = 27 | |
| 21 or more times | n = 52 | |
| Missing | n = 50 | |
| Adolescent marijuana use (T1; past 30 days) | 0 times | n = 598 |
| 1–10 times | n = 133 | |
| 11–20 times | n = 44 | |
| 21 or more times | n = 171 | |
| Missing | n = 79 | |
| Adolescent cigarette use (T2; past 30 days) | 0 times | n = 780 |
| 1–10 times | n = 103 | |
| 11–20 times | n = 30 | |
| 21 or more times | n = 59 | |
| Missing | n = 53 | |
| Adolescent marijuana use (T3; past 30 days) | 0 times | n = 530 |
| 1–10 times | n = 69 | |
| 11–20 times | n = 29 | |
| 21 or more times | n = 127 | |
| Missing | n = 270 |
In estimating the hypothesized model, paths from family e-cigarette use, peer e-cigarette use, and adolescent CTC use (T1) to adolescent e-cigarette use (T1), and from adolescent e-cigarette use (T1) to positive expectancies and willingness (T1) were specified. Paths from positive expectancies and willingness (T1) with CTC use (T2) also were estimated. Further, a direct path from CTC use (T2) to marijuana use (T3) was assessed. Based on the modification indices, one additional direct path was added from adolescent e-cigarette use (T1) to marijuana use (T3). Based on the findings of the modification indices, covariance between positive expectancies and willingness was estimated. Indirect effects of family and peer e-cigarette use (T1) on marijuana use (T3) via adolescent e-cigarette use (T1), willingness (T1), and CTC use (T2) also were estimated using the Delta (Sobel) method in the R lavaan package.39–41
Results
For descriptive information on all key study variables, see Table 1. The model chi-square was not statistically significant, χ 2 (9) = 10.14, p = .34, indicating good fit of model with data. The other goodness of fit indices demonstrated good model fit (CFI = .99, TLI = .99, RMSEA = .01 [90% confidence interval: .00– .04]).
Direct and Indirect Effects
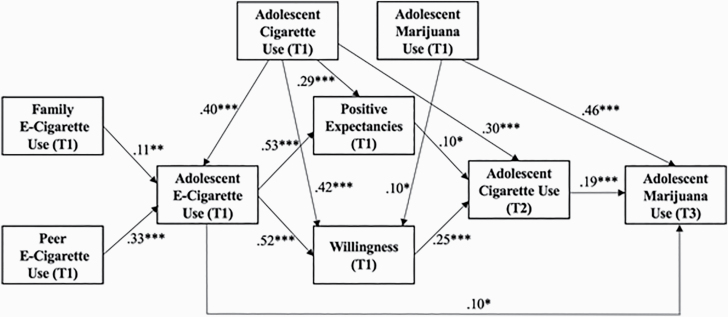
The final model relationships presented in Figure 1 show statistically significant direct paths from peer and family e-cigarette use (T1) to adolescent e-cigarette use (T1). Adolescent CTC use (T1) also was linked directly to adolescent e-cigarette use, positive expectancies, willingness (all T1), and CTC use at T2. Adolescent CTC use at T2 was directly linked directly to marijuana use at T3, as were adolescent e-cigarette and marijuana use (both T1).
Figure 1.
Path analytic model of proposed study relationships. Age, sex, and ethnicity (all T1) were entered into the model as covariates but are not pictured to maintain conceptual clarity. T1 substance use also was controlled for. T1 substance use variables (e-cig, CTC, and marijuana) also were entered in the model. Paths between marijuana use (T1) with family e-cigarette use (T1), positive expectancies (T1), and adolescent cigarette use at (T2), and paths between e-cigarette use (T1) and cigarette use (T2) were included in the estimated model, but were not statistically significant, and are not pictured. Covariance between positive expectancies and willingness was estimated but is not pictured to provide diagrammatic simplicity. T = time. *p < .05, **p < .01, ***p < .001.
Furthermore, adolescent e-cigarette use was directly related to positive expectancies about CTC use and greater willingness to try CTCs (both T1), and CTC use at T2. Teens scoring higher in positive expectancies and willingness at T1 also were more likely to use CTC at T2.
E-cigarette use and marijuana use (both at T1) and CTC use at T2 were direct predictors of marijuana use at T3.
Indirect effects were estimated using the guidelines for analysis recommended in the lavaan package for R software (Delta/Sobel method).39–41 No direct effect between family or peer e- cigarette use (T1) with marijuana use (T3) was proposed. Instead, we predicted these relationships would operate via the mediators (adolescent e-cigarette use, positive expectancies, and willingness [all T1] and CTC use [T2]). The indirect effects of both family e-cigarette use (T1; B = .17, p < .001) and peer e-cigarette use (T1; B = .14, p < .001) on marijuana usage (T3), as mediated by adolescent e-cigarette use (T1), willingness (T1), and CTC use (T2), were statistically significant. The same model was estimated treating marijuana usage at T3 as a binary outcome variable (0 = no; 1 = yes) using probit regression estimation. Findings from this alternative model revealed a similar pattern of results and significance levels
Discussion
Accumulating evidence suggests the effects of e-cigarette use for adults and adolescents.41,42 The current research indicates that e-cigarette use and marijuana use may be linked, and as such, this association deserves close scrutiny. Analysis of a unique 3-year longitudinal sample of alternative high school students in California disclosed an unsettling pattern of results considering prior research on adolescents’ use of psychoactive substances. Based on a longitudinal panel survey involving 859 respondents, the results of this analysis support the plausibility of a well-established developmental sequence in which e-cigarette initiation is furthered by family and peer use, which may be associated with more positive expectations and openness to CTCs. These positive responses could give rise to subsequent CTC use, which prior research has related to marijuana initiation, which was demonstrated in the current research. We realize many factors have been established as strongly implicated in adolescents’ decisions to use marijuana, including peer use and positive predispositions toward the substance.21–24 The current study indicates that e-cigarette use also may be considered to have an influence on marijuana use, a substance clearly not indicated for use by adolescents, and thus its potential effects, too, should be pointed out and monitored carefully.43,44
Earlier studies across a host of psychotropic substances have implicated peer and family use as strong antecedents to adolescents’ own usage.23,45,46 Our analysis demonstrated the association between peer and family use and adolescents’ own e-cigarette use at the first measurement session (T1). Adolescents’ e-cigarette use at T1 was associated with positive expectancies toward CTCs and willingness to use them, and this was realized behaviorally in the second year of the study. That these social psychological constructs anticipated CTC use at T2 could be predicted by Fishbein and Ajzen’s theory of reasoned action, which is popular in many studies bearing on public health.47 In turn, CTC use at T2 significantly predicted marijuana use at T3. It also is noteworthy that adolescent e-cigarette use at T1 was directly and significantly associated with marijuana use 2 years later at T3.
The analysis showed that e-cigarette use was associated with positive expectancies regarding CTC use, along with a willingness to try them. It supported the proposed hypotheses with strong associations, raising concerns about the potential short- and long-term effects of e-cigarettes for adolescents, whose use is growing at a rapid rate despite increasing evidence of the negative health implications raised in response to their use.9,12,13 For vulnerable populations like the alternative high school students examined in this study, the pressures exerted by peers and even some parents may lead to CTC use by increasing positive expectations and to a greater willingness to experiment with e-cigarettes, which we have shown to have statistically significant associations with subsequent marijuana use, even after accounting for earlier marijuana use.
Limitations
The reported results should be considered in light of their limitations. Although the sample was large, a strength, it consisted of students attending alternative high schools in California. Such high school students are not representative of the general population of students in the state, and thus, the results may be viewed as restricted to a nonrepresentative group whose generalization to the population at large is uncertain. However, the sample was of the same age as most high school students in the state. Further, research suggests alternative students are at greater risk of substance use than students attending more usual (ie, nonalternative) high schools; however, the results do not suggest that the developmental pattern of psychoactive substance use implicated in this study is materially different between these two groups. The developmental patterns of our study are not unusual, and the bulk of prior literature is based on responses of students attending more standard high schools, not alternative schools.47
Another possible limitation to generalizability is the low volunteer rate to the initial call for participants. Reasons for students/parents’ refusing to volunteer cannot be known, insofar as refusals occurred before any other data were collected. A reasonable hypothesis is that heavy substance users might have been reluctant to participate in a study in which they would be asked to report on their usage, and a large refusal rate might have rendered a school ineligible to participate. However, because analyses controlled for initial usage at T1, along with age, sex, and ethnicity, the nonvolunteer rate, although not desirable, was not seen as overly problematic.
A third objection might be that the research was based on nonexperimental methods, and so inferences of causation are not supported unambiguously. However, path analytic techniques making use of longitudinal panel data are generally accepted as the best examples of this analytic form. Even so, though we do not make strong causal claims, we do suggest the current pattern of findings fits well with prior research, supporting the plausibility of the possibilities raised herein.
Conclusion
The country is faced with some obvious facts relevant to e-cigarette use by adolescents. The first of these is that the growth of e-cigarette use in this population is nothing short of phenomenal.48 The second is that CTC use is dangerous, especially for youth, whose developmental trajectories render them particularly prone to nicotine addiction. A third fact is that CTC use is a major threat to public health, a source of death and disability.48 The Surgeon General’s report of 2019 stated the danger succinctly: “Every day, more than 1,200 people in this country die due to smoking. For each of those deaths, at least two youth or young adults become regular smokers each day. Almost 90% of those replacement smokers smoke their first cigarette by age 18.” The fourth fact is that some of our best scientists have concluded that marijuana, if started early and used intensively, arrests the brain development of young people.5
Now let us leave the land of facts for the land of conjecture. Suppose the developmental findings reported in this analysis are the result of the predicted causal sequence. The patterns suggested in the path analysis are far from controversial. Parent and peer influences on adolescent substance use are well established. CTC use has been established as dangerous to health and has been linked to marijuana uptake in many studies. The new ingredient added to this standard recipe, as both a direct and indirect factor, is the electronic nicotine delivery system (ENDS). It fits well with all the established patterns and suggests that we strongly consider ENDS as an ominous addition to the long list of threats to healthy development of our youth. If this warning is taken seriously by policy makers, parents, and the scientific community, this threat should be minimized or eliminated.
Supplementary Material
A Contributorship Form detailing each author’s specific involvement with this content, as well as any supplementary data, are available online at https://academic.oup.com/ntr.
Acknowledgments
The authors wish to thank Sandy Asad, Sara J. Asad, Melissa Garrido, Sarah Z. Gonzalez, Hannah Jornacion, and Brenda Lisa Lucero for their tireless efforts recruiting and tracking alternative high school students. Additional thanks to Jerry Grenard for helping to design the study and refine the central concepts.
Funding
Research reported in this publication was supported by the National Institute of Child Health and Human Development and the Food and Drug Administration Center for Tobacco Products (R01HD077560). The content is solely the responsibility of the authors and does not necessarily represent the views of the National Institutes of Health or the Food and Drug Administration.
Declaration of Interests
None declared.
References
- 1. Pearson JL, Richardson A, Niaura RS, Vallone DM, Abrams DB. E-cigarette awareness, use, and harm perceptions in US adults. Am J Public Health. 2012;102(9):1758–1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. WHO Study Group on Tobacco Production Regulation. WHO Study Group on Tobacco Product Regulation. Report on the Scientific Basis of Tobacco Product Regulation: Third Report of a WHO Study Group. World Health Organization Technical Report Series 955. 2009:1–41. [PubMed] [Google Scholar]
- 3. Vansickel AR, Eissenberg T. Electronic cigarettes: effective nicotine delivery after acute administration. Nicotine Tob Res. 2013;15(1):267–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Miech RA, Schulenberg JE, Johnston LD, et al. National Adolescent Drug Trends in 2017: Findings Released. Ann Arbor, MI: Monitoring the Future; 2017. http://www.monitoringthefuture.org. Accessed June 9, 2020. [Google Scholar]
- 5. Chadi N, Hadland SE, Harris SK. Understanding the implications of the “vaping epidemic” among adolescents and young adults: a call for action. Subst Abus. 2019;40(1):7–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Schneider S, Diehl K. Vaping as a catalyst for smoking? An initial model on the initiation of electronic cigarette use and the transition to tobacco smoking among adolescents. Nicotine Tob Res. 2016;18(5):647–653. [DOI] [PubMed] [Google Scholar]
- 7. Wills TA, Knight R, Sargent JD, Gibbons FX, Pagano I, Williams RJ. Longitudinal study of e-cigarette use and onset of cigarette smoking among high school students in Hawaii. Tob Control. 2017;26(1):34–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Barrington-Trimis JL, Kong G, Leventhal AM, et al. E-cigarette use and subsequent smoking frequency among adolescents. Pediatrics. 2018;142(6):e20180486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Abreu-Villaça Y, Seidler FJ, Slotkin TA. Impact of adolescent nicotine exposure on adenylyl cyclase-mediated cell signaling: enzyme induction, neurotransmitter-specific effects, regional selectivities, and the role of withdrawal. Brain Res. 2003;988(1–2):164–172. [DOI] [PubMed] [Google Scholar]
- 10. Soneji S, Barrington-Trimis JL, Wills TA, et al. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatr. 2017;171(8):788–797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Primack BA, Shensa A, Sidani JE, et al. Initiation of traditional cigarette smoking after electronic cigarette use among tobacco-naïve US young adults. Am J Med. 2018;131(4):443.e1–443.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dai H, Catley D, Richter, et al. Electronic cigarettes and future marijuana use: a longitudinal study. Pediatrics. 2018;141(5):1–10. [DOI] [PubMed] [Google Scholar]
- 13. Audrain-McGovern J, Stone MD, Barrington-Trimis J, et al. Adolescent e-cigarette, hookah, and conventional cigarette use and subsequent marijuana use. Pediatrics. 2018;142(3):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kong G, Morean ME, Cavallo DA, Camenga DR, Krishnan-Sarin S. Reasons for electronic cigarette experimentation and discontinuation among adolescents and young adults. Nicotine Tob Res. 2015;17(7):847–854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hemovich V, Lac A, Crano WD. Understanding early-onset drug and alcohol outcomes among youth: the role of family structure, social factors, and interpersonal perceptions of use. Psychol Health Med. 2011;16(3):249–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Miller SM, Siegel JT, Crano WD. Parents’ influence on children’s cannabis use. In: Preedy VR, ed. Handbook of Cannabis and Related Pathologies: Biology, Pharmacology, Diagnosis, and Treatment. San Diego, CA: Academic Press; 2017. [Google Scholar]
- 17. Hohman ZP, Crano WD, Siegel JT, Alvaro EM. Attitude ambivalence, friend norms, and adolescent drug use. Prev Sci. 2014;15(1):65–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sheeran P, Maki A, Montanaro E, et al. The impact of changing attitudes, norms, and self-efficacy on health-related intentions and behavior: a meta-analysis. Health Psychol. 2016;35(11):1178–1188. [DOI] [PubMed] [Google Scholar]
- 19. Grunbaum JA, Lowry R, Kann L. Prevalence of health-related behaviors among alternative high school students as compared with students attending regular high schools. J Adolesc Health. 2001;29(5):337–343. [DOI] [PubMed] [Google Scholar]
- 20. Siegel JT, Crano WD, Alvaro EM, Lac A, Hackett JD, Hohman ZP. Differentiating common predictors and outcomes of marijuana initiation: a retrospective longitudinal analysis. Subst Use Misuse. 2014;49(1–2):30–40. [DOI] [PubMed] [Google Scholar]
- 21. Liao Y, Huang Z, Huh J, Pentz MA, Chou CP. Changes in friends’ and parental influences on cigarette smoking from early through late adolescence. J Adolesc Health. 2013;53(1):132–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ewing BA, Osilla KC, Pedersen ER, Hunter SB, Miles JN, D’Amico EJ. Longitudinal family effects on substance use among an at-risk adolescent sample. Addict Behav. 2015;41:185–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Vogel EA, Ramo DE, Rubinstein ML. Prevalence and correlates of adolescents’ e-cigarette use frequency and dependence. Drug Alcohol Depend. 2018;188:109–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Carey FR, Rogers SM, Cohn EA, Harrell MB, Wilkinson AV, Perry CL. Understanding susceptibility to e-cigarettes: a comprehensive model of risk factors that influence the transition from non-susceptible to susceptible among e-cigarette naïve adolescents. Addict Behav. 2019;91:68–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lozano P, Barrientos-Gutierrez I, Arillo-Santillan E, et al. A longitudinal study of electronic cigarette use and onset of conventional cigarette smoking and marijuana use among Mexican adolescents. Drug Alcohol Depend. 2017;180:427–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Johnson KE, McMorris BJ, Kubik MY. Comparison of health-risk behaviors among students attending alternative and traditional high schools in Minnesota. J Sch Nurs. 2013;29(5):343–352. [DOI] [PubMed] [Google Scholar]
- 27. El-Shahawy O, Sun P, Tsai JY, Rohrbach LA, Sussman S. Sense of coherence and tobacco use myths among adolescents as predictors of at-risk youth cigarette use. Subst Use Misuse. 2015;50(1):8–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. McCuller WJ, Sussman S, Holiday K, Craig S, Dent CW. Tracking procedures for locating high-risk youth. Eval Health Prof. 2002;25(3):345–362. [DOI] [PubMed] [Google Scholar]
- 29. Centers for Disease Control and Prevention (CDC). 2012 National Youth Tobacco Survey (NYTS).2014. http://www.cdc.gov/TOBACCO/data_statistics/surveys/NYTS/index.htm. Accessed June 9, 2020.
- 30. CDPH. 2011–2012 California Student Tobacco Survey (CSTS).2014. http://www.cdph.ca.gov/programs/tobacco/Pages/default.aspx
- 31. Myers MG, McCarthy DM, MacPherson L, Brown SA. Constructing a short form of the Smoking Consequences Questionnaire with adolescents and young adults. Psychol Assess. 2003;15(2):163–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Gerrard M, Gibbons FX, Houlihan AE, et al. A dual-process approach to health risk decision making: the prototype willingness model. Dev Rev. 2008;28(1):29–61. [Google Scholar]
- 33. Graham JW, Flay BR, Johnson CA, Hansen WB, Grossman L, Sobel JL. Reliability of self-report measures of drug use in prevention research: evaluation of the Project SMART questionnaire via the test-retest reliability matrix. J Drug Educ. 1984;14(2):175–193. [DOI] [PubMed] [Google Scholar]
- 34. Ames SL, Xie B, Shono Y, Stacy AW. Adolescents at risk for drug abuse: a 3-year dual-process analysis. Addiction. 2017;112(5):852–863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kline RB. Principles and Practice of Structural Equation Modeling. 2nd ed.New York, NY: Guilford Press; 2011. [Google Scholar]
- 36. O’Brien RM. A caution regarding rules of thumb for variance inflation factors. Qual Quantity. 2007;41(5):673–690. [Google Scholar]
- 37. Crano WD, Donaldson CD, Siegel JT, Alvaro EM, O’Brien EK. Selective invalidation of ambivalent pro-marijuana attitude components. Addict Behav. 2019;97:77–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model. 1999;6(1):1–55. [Google Scholar]
- 39. Zhang Z, Wang L.. Advanced Statistics Using R. Granger, IN: ISDSA Press; 2017. [Google Scholar]
- 40. Rousseel Y. Lavaan: an R package for structural equation modeling. J Stat Softw. 2012;48(2):1–36. http://www.jstatsoft.org/. [Google Scholar]
- 41. Sobel ME. Direct and indirect effects in linear structural equation models. Sociol Methods Res. 1987;16(1):155–176. [Google Scholar]
- 42. Callahan-Lyon P. Electronic cigarettes: human health effects. Tob Control. 2014;2(2):ii36–ii40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. King JL, Reboussin BA, Wiseman KD, et al. Adverse symptoms users attribute to e-cigarettes: results from a national survey of US adults. Drug Alcohol Depend. 2019;196:9–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. National Academies of Sciences, Engineering, and Medicine. The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research. Washington, DC: National Academies Press; 2017. [PubMed] [Google Scholar]
- 45. Mooney-Leber SM, Gould TJ. The long-term cognitive consequences of adolescent exposure to recreational drugs of abuse. Learn Mem. 2018;25(9):481–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Schuler MS, Tucker JS, Pedersen ER, D’Amico EJ. Relative influence of perceived peer and family substance use on adolescent alcohol, cigarette, and marijuana use across middle and high school. Addict Behav. 2019;88:99–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Fishbein M, Ajzen I.. Predicting and Changing Behavior: The Reasoned Action Approach. New York, NY: Psychology Press; 2011. [Google Scholar]
- 48. Chadi N, Schroeder R, Jensen JW, Levy S. Association between electronic cigarette use and marijuana use among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatr. 2019;173(10):E1–E10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.