Abstract
Objective
Several studies have been conducted to investigate the relationship between addiction and crimes, but little is known about the treatment of individuals with substance use disorder (SUD) with criminal records. This study aimed to assess the treatment progress of a group of individuals with SUD who underwent treatment within a residential community, and to analyze their personality profiles to identify drop-out predictors.
Method
We evaluated 49 subjects using the Psychopathic Personality Inventory-Revised (PPI-R), the Psychological Treatment Inventory (PTI), the Barratt Impulsiveness Scale-11 (BIS-11), and the Toronto Alexithymia Scale (TAS-20) and carrying out various statistical analyses, including the t-test, Cohen’s d, analysis of variance (ANOVA), and discriminant analysis.
Results
Results are discussed within the context of previous studies on this topic. Our results showed that variables such impulsiveness, cold-heartedness, alexithymia, and psychopathic traits influenced the premature treatment abandonment of individuals with SUD and criminal records.
Conclusions
This study provides a further piece for the understanding of subjects with SUD and criminal records, suggesting the importance of a psychodynamic integrated approach, and showing the impact of some psychopathological features on treatment drop-out.
Keywords: process-outcome research, psychological treatment, psychotherapy, addiction, assessment
Introduction
There have been a large number of studies conducted on the link between drug addiction and crime. A meta-analysis of 30 studies showed that individuals with substance use disorder (SUD) are between 2.8 and 3.8 times more likely to commit crimes than non-drug users (Bennett, Holloway, & Farrington, 2008). Indeed, people with SUD get involved in the criminal justice system for diverse types of crimes, and many of these offenses are related to the use of drugs (UNODC, 2013). The three drugs that are most frequently associated with criminal conduct are crack, heroin, and cocaine. People abusing these drugs are more likely to commit crimes (6, 3, and 2.5 times greater, respectively) than the users of other drugs (Bennett, Holloway, & Farrington, 2008). Furthermore, the relationship between criminal activity and drug use varies according to the type of substance. Property crimes, prostitution, shoplifting, and theft are the crimes most frequently associated with users of crack, heroin, and cocaine (Mc Bride, 1981; Hunt, Lipton, & Spunt, 1984; Kuhns, Heide, & Silverman, 1992; Graham & Wish, 1994; Yacoubian et al., 2001; Holloway & Bennett, 2004).
The link between addiction and felony is complex and multifaceted. An individual with a substance use disorder may commit a crime as a direct result of the effects of drug intoxication, but these individuals may also commit crimes as a result of withdrawal symptoms, especially if he or she exhibits specific personality traits, such as antisocial or narcissistic ones (Echeburúa & Fernández-Montalvo, 2007). In light of this, the clinical literature has set forth multiple theories that try to explain the nature of the relationship between the use of drugs and criminal behavior. Some theoretical models proposed a direct causal relationship, where one of the variables causes the other. According to the Economic Compulsive Model (Goldstein, 1985), heavy drug users engage in criminal conduct to raise funds to purchase drugs.
Other hypotheses argue an indirect causal connection. Here, the theory of “common cause” indicates that different kinds of variables (sociological, psychological, or environmental factors) foster both substance dependence and crime, which are therefore linked by common causal roots (White, 1990; White, Brick, & Hansell, 1993).
Finally, the third group of theories includes the “systemic theories.” Here, the relation between crime and drug use is considered an underlying aspect of a deviant lifestyle/ deviant subculture (Goode, 1997; White & Gorman, 2000).
Individuals within the criminal justice system have higher rates of drug use disorders compared to the general population (UNODC, 2013); both the prevalence and frequency of offenses are higher among individuals with SUD compared to non-abusers (Holloway & Bennett, 2004). However, the long-term imprisonment of people with SUD is expensive. Adequate treatment and the care of individuals with SUD would help to reduce both drug use and recidivism to crime for those who have committed offenses (UNODC, 2010; UNODC & WHO, 2018). In fact, entry into the prison system seems to worsen the psychopathology of individuals with SUD (Bondenson, 2009).
According to some theories (e.g., Leshner, 1997), addiction can be seen as a chronic and relapsing brain disease or a neurological disorder. Consequently, related actions are manifestations of the disease. In this view, individuals with SUD are believed to be constrained in their choice of research and abuse. Other theories (e.g., Heyman, 2009) which include awareness of the constraints imposed by dependency, show how some individuals tend to stop when the costs are too high. At the very least, these theories posit that individuals delay their use when the contextual conditions are not favorable (Morse, 2011). According to this perspective, dependence and criminal conduct are not forcibly associated. More likely, other environment and subjective variables also influence this relationship. Indeed, to be distinct differences between individuals with and without criminal records were reported. Specifically, individuals with SUD and criminal behaviors exhibit significantly more antisocial traits, while individuals with SUD but no criminal records scored considerably higher on the phobic, dependent, and self-destructive personality disorder scales (Fernández-Montalvo et al., 2013). Some studies have reported a significant association between SUD and psychopathic traits (Taylor & Lang, 2006; Kimonis et al., 2012; Muratori et al., 2018). This, however, appears to be more pronounced in subjects with criminal histories (Gori et al., 2017). Furthermore, individuals with SUD with criminal histories have more externalizing symptoms, have a propensity for risk-taking behaviors, and are more inclined to perceive the external world as hostile and to consider others as responsible for their own problems and difficulties (Gori et al., 2017). Research shows that individuals with SUD who broke the law scored higher on psychoticism (40%) and neuroticism (64%) as compared to a non-drug user control group (Aggarwal et al., 2015).
Numerous studies (Gori et al., 2014, 2017) have shown that psychopathic traits are present among individuals with SUD who commit crimes. In particular, these impulsive-antisocial traits include impulsivity, irresponsibility, weak behavioral control, and criminal versatility (Hare, 2003). These traits are positively correlated with drug use (Lage, 2013). Interpersonal-affective traits, which indicate deceitfulness, superficial charm, manipulativeness, deficient empathy, and lack of remorse (Hare, 2003) show a negative relationship to substance abuse symptoms (Schulz, Murphy, & Verona, 2016).
According to this theoretical framework, the purposes of this study were to:
assess treatment outcomes in individuals with SUD and crime records, by repeated administration of various tests over time and at termination;
investigate and describe the psychopathological features in a sample of individuals with SUD with criminal records involved in treatment;
identify variables linked to the drop-out rate in order to prevent abandonment from the treatment.
Methods
Participants and procedures
Forty-nine subjects participated in this research [43 males (87.5%), six females (12.5%)] with an average age of 36.83 years (SD = 8.25, age-range 21–54). Among these subjects, 48 were of Italian descent and one of African descent. Most of the subjects were residents in the Tuscany (50%) and Lazio (37%) regions of Italy. Concerning marital/conjugal status, most of the subjects were single (76.6%), 6.4% said they were married, another 6.4% said they were divorced, 4.3% separated, and other 6.4% cohabitants. Regarding educational qualifications, 44.7% declared that they had a lower secondary school diploma, and another 44.7% reported having graduated high school; 8.5% said they attended only primary school, while 2.1% said they had a degree (see table 1).
Table 1.
Sociodemographic Characteristic of the sample
| Sociodemographic Characteristics | |||
|---|---|---|---|
| Age | M= 36.83, SD= 8.25 | ||
| Gender | |||
| n | % | ||
| Male | 43 | 87.5 | |
| Female | 6 | 12.5 | |
| Nationality | |||
| Italian | 48 | 98 | |
| African | 1 | 2 | |
| Marital Status | |||
| Single | 38 | 76.6 | |
| Married | 3 | 6.4 | |
| Divorged | 3 | 6.4 | |
| Separated | 2 | 4.3 | |
| Cohabitant | 3 | 6.4 | |
| Study degree | |||
| Elementary school | 4 | 8.5 | |
| Middle School diploma | 22 | 44.7 | |
| High School diploma | 22 | 44.7 | |
| University degree | 1 | 2.1 | |
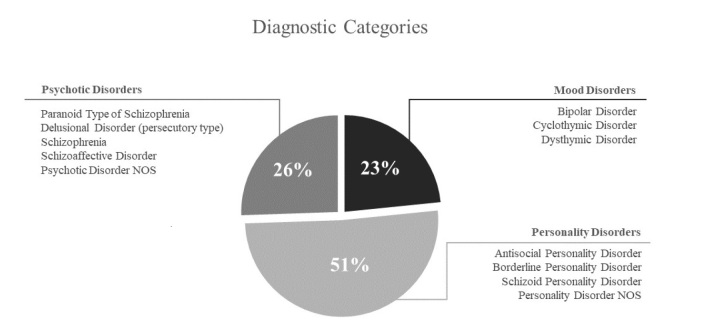
With regards to the diagnostic characteristics of the analyzed subjects, it was considered convenient (for methodological reasons) to group the diagnostic categories, based on the personality organization levels of the Kernberg’s model (Kernberg, 1993; Caligor, Kernberg, & Clarkin, 2007). These groups included, 1) Mood Disorders (which mainly includes disorders with a “high borderline personality organization”, i.e. conditions that show a fair working and social adaptation, with moderate ability to have a certain degree of intimacy in object relations and a benign cycle of intimate involvements, albeit presenting identity diffusion); 2) Personality Disorders (with a “low borderline personality organization”, i.e. conditions that show an inability to maintain work and sentimental relationships, with primitive defensive mechanisms and poor self-integration, as well as an identity diffusion); and 3) Psychotic Disorders (that is, symptomatic psychoses with a “psychotic personality organization”, i.e. conditions characterized by a loss of the reality testing, with a lack of differentiation between the internal and external experiences, as well as between the self and the object representations). In this way, the fusion of two perspectives—psychopathological and psychodynamic—facilitates a full understanding of deviant behaviors, as already shown by previous studies (Craparo et al., 2018). The first group included subjects diagnosed with bipolar disorder, cyclothymic disorder, and dysthymic disorder. The second group included two subjects with antisocial personality disorder, 15 subjects with borderline personality disorder, four subjects with personality disorder not otherwise specified, and three subjects with schizoid personality disorder. The third group included one subject with paranoid type of schizophrenia, three subjects with delusional disorder (persecutory type), two subjects with schizophrenia, two subjects with psychotic disorder not otherwise specified, and four subjects with schizoaffective disorder (see figure 1).
Figure 1.
Diagnostic Categories
Moreover, all subjects had SUD. Most of the participants said they preferred cocaine (29.8%) and heroin (25.5%). Additionally, 23.4% of the sample reported having a previous history of poly-drug SUD.
There were 49 participants who underwent residential treatment in a therapeutic community, with an average duration of 593.13 days (DS= 316.301; range 68–1317). These individuals were subjected to methadone therapy associated with specific pharmacological treatments based on their diagnosis. Subjects with Mood disorders were prescribed anxiolytics, antidepressants, and mood stabilizers; subjects with Psychotic disorders were prescribed mood stabilizers and neuroleptics; and subjects with Personality disorders were prescribed anxiolytics and mood stabilizers. Subjects with borderline Personality disorders were an exception to this latter trend. These individuals followed a more complex therapy consisting of anxiolytics, antidepressants, neuroleptics, and mood stabilizers.
All subjects had histories of committing crimes, and 83% of the participants were detained at least once. Most of the sample (65.3%) committed multiple crimes (see table 2). Concerning their current legal situation, 21.3% of the sample were not incarcerated; 12.8% were under house arrest; 42.6% were being tested for social services; 8.5% were receiving in-home detention; and 14.9% were participants in another legal regime (not specified) (see table 2). Most of the subjects in the sample had been detained for less than a year (24.5%) over their total lifetimes (see table 2).
Table 2.
Legal features of the sample
| Legal Situation | ||
|---|---|---|
| Type of crime | ||
| n | % | |
| Shoplifting, Property damage | 1 | 2.0 |
| Drug | 3 | 6.1 |
| Robbery, Handling, Snatching | 1 | 2.0 |
| Burglary | 5 | 10.2 |
| Assault, Scuffle | 2 | 4.1 |
| Other | 3 | 6.1 |
| Multiple crimes | 32 | 65.3 |
| Missing | 2 | 4.1 |
| Current Custodial Status | ||
| Freedom | 10 | 21.3 |
| House arrest | 6 | 12.8 |
| Tested for social services | 21 | 42.6 |
| Home detention | 4 | 8.5 |
| Other | 8 | 14.9 |
| Duration of Detention | ||
| Less than one year | 12 | 24.5 |
| One year | 1 | 2.0 |
| Two years | 3 | 6.1 |
| Three years | 2 | 4.1 |
| Three to five years | 7 | 14.3 |
| Five to ten years | 6 | 12.2 |
| More than ten years | 7 | 14.3 |
| Missing | 11 | 22.4 |
The measures, together with a demographic questionnaire (i.e., age, sex, marital status) were administered to participants. The participants were selected from the therapeutic communities of the Gruppo Incontro Società Cooperativa Sociale in Pistoia. All assessment measures were administered by the qualified staff of the Gruppo Incontro: all researchers were psychologist authorized to use the tests, and the diagnoses were established by the psychiatrists at the Center according to DSM-IV-TR criteria. The study was approved by the Ethics committee of the Italian National Health Service (INHS) of the Local Health Union (USL 3 section of Pistoia), and all participants gave free and informed consent to participation. This research was made possible thanks to the contribution of the Tuscany Region and thanks to the collaboration of the Gruppo Incontro Società Cooperativa Sociale in Pistoia.
Measures
1)Psychopathic Personality Inventory-Revised (PPI-R).
The PPI-R (Lilienfeld & Widows, 2005) is a self-report measure of psychopathic traits in adults. The PPI-R was developed from the original version of the Psychopathic Personality Inventory (Lilienfeld & Andrews, 1996). The revised version includes 154 items presented on a 4-point Likert scale (from 1= “false” to 4= “true”). It yields a total psychopathic index (PPI-R, total score) as well as scores on eight subscales, which are grouped into three factors: 1) The Fearless Dominance (FD) factor is associated with fearless, assertiveness, interpersonally dominant demeanor and thrill-seeking and includes Social Influence, Fearlessness, and Stress Immunity subscales; 2) The Self-Centered Impulsivity (SCI) factor is related to anger, aggressiveness, impulsivity, externalizing behaviors (including substance use), suicidal ideation, and acts and consists of the Machiavellian Egocentricity, Rebellious Nonconformity, Blame Externalization, and Carefree Nonplanfulness subscales; 3) finally, although a two-factor model has proved valid (Benning et al., 2003), some authors (e.g., Neumann, Malterer, & Newman, 2008) observe that consider Cold-heartedness (CH; which assesses callousness and lack of empathy and guilt) as a third separated factor is more effective. Machiavellian Egocentricity (ME), the first of the eight subscales, indicates an absence of empathy, the tendency to manipulate others, lie, alter the rules to achieve one’s own goals, and a sense of detachment. The Rebellious Nonconformity (RN) subscale assessed susceptibility to boredom, a tendency to rebel, negative attitudes against authority and resistance to social norms, and to culturally acceptable behaviors. The Blame Externalization (BE) subscale measures the tendency to blame others or bad luck for one’s problems, the vision of the external world as hostile, and the perception of oneself as victims. The Carefree Non-Planfulness (CN) refers to a lack of planning and difficulty to act before thinking, not considering the consequences of one’s actions. The Social Influence (SOI) subscale indicates the ability to charm and influence others, with a sense of security, a lack of social anxiety, and verbal ease. The Fearlessness (F) subscale assessed the eagerness for risk-seeking behaviors with a lack of both anticipatory anxiety and fear for one’s physical safety. The Stress Immunity (STI) subscale measures the ability to keep calm and detached in the presence of anasiogenic stimuli and a lack of tension under pressure. Finally, CH refers to an inability to keep relationships with others and to a lack of both affectionate, social emotions, and regard for others’ feelings. The PPI-R also includes three validity scales: Deviant Responding, Virtuous Responding, and Inconsistent Responding which measure aberrant responding/ malingering, positive impression management, and careless or random responding, respectively. The Italian version showed good psychometric characteristics (La Marca, Berto, & Rovetto, 2008).
2) Psychological Treatment Inventory (PTI)
The PTI (Gori, Giannini, & Schuldberg, 2008; 2013) is a measure designed for personality assessment, composed by client and clinician versions, which are respectively self-report and hetero-evaluation scales. The PTI client version, which was the only version used in this study, was composed of 268 items presented on a 5-point Likert scale (1 = not at all, 2 = a little, 3 = enough, 4 = a lot; and 5 =very much). The PTI was designed to include items in various domains central to planning psychological treatment and evaluating its outcome. Each construct was grouped into 4 areas:
The validity scales area included six subscales (Lie, Compliance, Ambiguity Intolerance, Low Attention, Incoherence, and Negative Self Presentation);
-
The Psychological Resources Area was composed of two clusters:
Psychological Resources cluster was articulated into five scales (Self Efficacy, Self Esteem, Perceived Social Support, Creative Tendencies, and Self-Regulation):
Quality of Life cluster was composed of five subscales (Life Satisfaction, Work Interference, Familiar Problems, Social Introversion, and Distress);
The Clinical Area included two clusters (Symptoms and Psychological Types). Symptoms were articulated into ten Internalized Symptoms Scales and three Externalized Symptoms Scales. Psychological Types were determined by 12 single-item scales.
-
The Psychological Treatment Area was composed of four clusters:
Attachment Styles (four scales: Secure, Preoccupied, Avoidant, Disorganized);
Predominant Defense Styles (four scales: Mature, Anxious neurotic, Avoidant neurotic, Immature);
Negative Treatment Indicators (five scales: Alexthimia, Frustration Intolerance, Negative Self-Image, Change Resistance, Manipulation);
Psychological Mindedness (four scales: Empathy, Insight Propensity, Treatment Expectation, Working Alliance).
The PTI has shown good psychometric properties (Giannini et al., 2010; Gori, Giannini, & Schuldberg, 2013).
3) Barratt Impulsiveness Scale-11 (BIS-11)
The BIS-11 (Patton, Stanford, & Barratt, 1995) is a 30-item self-report questionnaire used to assess general impulsivity, considering the multifactorial nature of the construct. It yields a total score and six first-order factors, which were grouped into three second-order factors: 1) Attentional Impulsiveness measures ability to focus attention or concentrate and includes attention and cognitive instability factors; 2) Motor Impulsiveness refers to a tendency to engage in acts without thinking and consists of motor and perseverance factors; 3) Non-planning Impulsiveness assesses the likelihood of making quick decisions without thinking about the possible consequences and is composed of cognitive complexity and self-control factors. Concerning the six subscales, Attention measures the ability to focus on current activities, Cognitive Instability verifies the presence of intrusive thoughts, Motor indicates the tendency to act quickly and impulsively, Perseverance concerns the tendency to have a stable lifestyle, Cognitive Complexity indicates the enjoyment in mentally challenging and stimulating activities, Self-Control measures the ability to control one’s thoughts and plan some life aspects. Each item on the measure is rated on a four-point scale ranging from 1 (Rarely/ Never) to 4 (Almost Always/Always), and the total score is achieved by adding the first or second-order factors. In the present study, the Italian version of BIS-11 (Fossati et al., 2001) was used.
4) Toronto Alexithymia Scale (TAS-20).
The TAS-20 (Bagby, Parker, & Taylor, 1994) is a 20-item questionnaire, scored on a 1 to 5 Likert scale, which assesses the level of alexithymia. It includes three factors: (1) difficulty in identifying feelings and distinguishing between feelings and bodily sensations in emotional activation, (2) difficulty with the verbal expression of emotions, and (3) externally oriented thinking. The total score is calculated by summing all the items and a high score indicates a higher level of alexithymia. As stated by Taylor and collaborators (1997), scores higher than 61 are considered indicators of an alexithymic profile. The original version of the TAS-20 has adequate psychometric properties. The reliability of the total scale is equal to .81, and the reliabilities of the three factors are .78, .75, and .66, respectively (Bagby, Parker, & Taylor, 1994). The validity of TAS-20 is also adequate (Bagby, Taylor, & Parker, 1994). This study employed the Italian version of TAS-20 (Bressi et al., 1996).
Data analysis
Descriptive statistics for the sample were calculated. To verify the variations between Time 1, Time 2, and Time 3, various statistical techniques were used, including the t-test, Cohen’s d, and ANOVA. To assess differences in differential diagnosis, an ANOVA was carried out with the diagnostic categories as the independent variable (groups) and the scales of the various instruments as dependent variables. An ANOVA was also used to assess differences related to the conclusion of the treatment, with the conclusion/continuation of the treatment as the independent variable (groups) and the scales of the various instruments as dependent variables. A series of discriminant analyses were performed to identify the impact and contribution of the variables on the discriminating function (i.e., the most useful variables for classifying purposes, concerning the two groups Interruption and In-Treatment).
Results
49 subjects participated in the assessment at Time 1; 34 of them were again involved in the assessment at Time 2 (after eight months of treatment); 18 individuals underwent three administrations: Time 1, Time 2 (after eight months) and Time 3 (after 12-14 months). Given the difficulty of finding such a specific sample, administrations were performed at different times, trying to respect the time constraints indicated above.
By the end of the research, 12 subjects (24%) completed their treatment, 25 subjects (52%) remained on treatment, and 12 (24%) prematurely stopped the residential treatment and abandoned their communities (drop-out; see figure 2).
Figure 2.
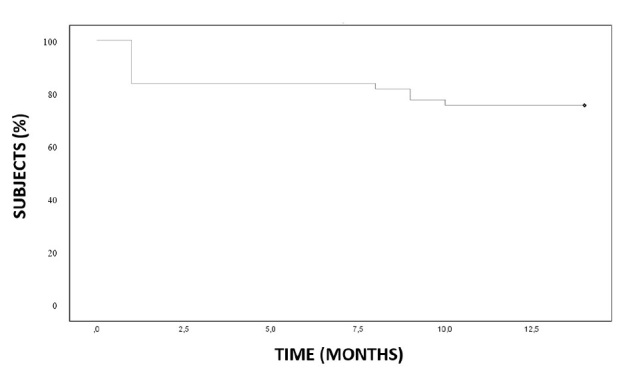
Kaplan–Meier plot regarding patients drop-out
No significant differences emerged in the scales scores at the three different times of assessment. Regarding the analyses between groups related to the diagnosis, differences emerged about the tendency to lie and were more pronounced in subjects within the Mood disorder and Personality disorder groups (p = .001). The Mood disorder group appeared to have greater difficulty tolerating states of ambiguity (p = .033) and declared more-frequent family problems (p = .032) than the other two groups. The Personality disorders group appears to have lower levels of self-esteem (p = .011) than the other two groups, while the Psychotic disorder group appears to perceive higher levels of social support (p = .009).
The Psychotic disorder group appeared to show a more pronounced and severe symptomatology than the other two groups, as evidenced by the results in table 3 (part I and part II). Furthermore, the Psychotic disorder group showed a higher level of anxiety compared to the other groups and seemed to activate a broader and more immature defensive style than the other two groups. The Personality disorders group showed greater resistance to change than the Mood disorders group and lower empathy levels compared to the other two groups (p = .024).
Table 3.
ANOVA among the groups in relation to Diagnostic Categories and to the state of treatment (PTI scale) – part I
| PTI Scales | Diagnostic Categories | F | p | State of Treatment | F | p | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mood Disorder | Personality Disorder | Psychotic Disorder | Conclusion | Drop-out | In-Treatment | |||||||||||
| N | M (SD) | N | M (SD) | N | M (SD) | N | M (SD) | N | M (SD) | N | M (SD) | |||||
| Validity Scales | ||||||||||||||||
| Lie* | 11 | 7.64 (1.29) | 24 | 6.75 (1.54) | 12 | 5.25 (1.42) | 8.06 | .001 | 12 | 6.25 (2.22) | 12 | 7.17 (1.40) | 25 | 6.92 (1.71) | .88 | .42 |
| Compliance | 11 | 1.27 (1.19) | 24 | 1.54 (.98) | 12 | 1.67 (.78) | .48 | .621 | 12 | 1.83 (1.19) | 12 | 1.67 (.98) | 25 | 2.20 (1.19) | 1.01 | .37 |
| Ambiguity Intolerance* | 11 | 3.63 (1.43) | 24 | 2.67 (1.13) | 12 | 2.42 (.90) | 3.68 | .033 | 12 | 2.83 (.72) | 12 | 3 (1.54) | 25 | 3.12 (1.42) | .19 | .83 |
| Low Attention | 11 | 4 (.89) | 24 | 3.25 (1.26) | 12 | 3 (1.28) | 2.24 | .119 | 12 | 3.42 (1.24) | 12 | 3.17 (1.19) | 25 | 3.24 (1.13) | .15 | .86 |
| Negative Self Presentation | 11 | 3.73 (1.35) | 24 | 3.96 (1.04) | 12 | 3.42 (1.38) | .814 | .450 | 12 | 4 (.85) | 12 | 3.17 (1.75) | 25 | 3.48 (1.48) | 1.05 | .36 |
| Resources Area | ||||||||||||||||
| Self-Efficacy | 11 | 19.73 (.85) | 24 | 17.50 (3.93) | 12 | 20.67 (5.55) | 2.40 | .103 | 12 | 19.08 (4.50) | 12 | 16.17 (4.41) | 25 | 20.28 (5.13) | 2.96 | .062 |
| Self-Esteem*** | 11 | 13.27 (3.5) | 24 | 11.04 (2.14) | 12 | 13.83 (3.19) | 4.97 | .011 | 12 | 12.17 (3.07) | 12 | 10.58 (2.87) | 25 | 13.76 (2.67) | 5.33 | .008 |
| Social Support*** | 11 | 17.18 (5.34) | 24 | 15.88 (3.09) | 12 | 20.58 (3.06) | 5.29 | .009 | 12 | 15.92 (4.50) | 12 | 15.08 (4.01) | 25 | 19.88 (3.73) | 7.49 | .002 |
| Creative Tendencies** | 11 | 17.18 (5.19) | 24 | 17.17 (3.34) | 12 | 19.33 (3.31) | 1.42 | .253 | 12 | 17.58 (3.15) | 12 | 14.58 (4.70) | 25 | 19.44 (5.51) | 4.09 | .023 |
| Self-Regulation | 11 | 19.82 (4.58) | 24 | 19.50 (5.26) | 12 | 23.17 (5.81) | 2.07 | .139 | 12 | 18 (6.09) | 12 | 17.67 (3.87) | 25 | 20.52 (4.63) | 1.88 | .163 |
| Life Satisfaction | 11 | 16 (5.33) | 24 | 16.88 (5.64) | 12 | 18.17 (6.69) | .40 | .670 | 12 | 14.58 (5.58) | 12 | 16 (7.07) | 25 | 17.88 (6.20 | 1.19 | .313 |
| Work Interference | 11 | 9.64 (3.67) | 24 | 10.29 (3.92) | 12 | 11.58 (4.10) | .76 | .473 | 12 | 10.17 (4.06) | 12 | 10.42 (3.82) | 25 | 8.80 (3.34) | 1.04 | .361 |
| Familiar Problems* | 11 | 14.18 (6.52) | 24 | 9.58 (4.28) | 12 | 12.08 (3.73) | 3.73 | .032 | 12 | 10.58 (4.96) | 12 | 10.67 (5.79) | 25 | 11.48 (5.28) | .16 | .854 |
| Social Introversion | 11 | 9.73 (4.61) | 24 | 10.46 (4.15) | 12 | 9.83 (2.69) | .17 | .841 | 12 | 11.08 (4.14) | 12 | 9.83 (4.99) | 25 | 9.08 (3.09) | 1.08 | .347 |
| Distress | 11 | 11 (3.85) | 24 | 11 (4.60) | 12 | 14.25 (2.93) | 2.85 | .068 | 12 | 11.92 (4.78) | 12 | 12.25 (5.28) | 25 | 11.76 (3.94) | .05 | .953 |
| Clinical Area | ||||||||||||||||
| Depressive Aspects | 11 | 9.27 (5.64) | 24 | 10.25 (4.65) | 12 | 12.92 (5.20) | 1.71 | .193 | 12 | 11.25 (6.18) | 12 | 11 (6.12) | 25 | 10.40 (3.62) | .14 | .873 |
| General Anxiety | 11 | 9.82 (5.79) | 24 | 10.42 (5.10) | 12 | 11.33 (2.42) | .30 | .742 | 12 | 11.17 (6.74) | 12 | 9.25 (3.98) | 25 | 10.32 (4.11) | .47 | .626 |
| Obsessiveness | 11 | 10.27 (3.55) | 24 | 9.58 (3.65) | 12 | 11.75 (3.96) | 1.37 | .265 | 12 | 9.92 (4.12) | 12 | 11.25 (4.77) | 25 | 10.68 (3.22) | .36 | .699 |
| Somatization | 11 | 8.09 (3.96) | 24 | 9.17 (4.57) | 12 | 9.17 (4.57) | 1.76 | .184 | 12 | 9.08 (4.17) | 12 | 9 (5.10) | 25 | 9.36 (2.91) | .04 | .958 |
| Phobic Traits | 11 | 8.82 (5.49) | 24 | 10.67 (4.26) | 12 | 10.75 (3.55) | .76 | .472 | 12 | 11.75 (5.97) | 12 | 9.83 (4.47) | 25 | 9.72 (4.28) | .79 | .460 |
| PTSD | 11 | 10.75 (3.55) | 24 | 13.67 (6.77) | 12 | 17.83 (6.12) | 2.15 | .129 | 12 | 13 (8.62) | 12 | 10.67 (4.08) | 25 | 12.60 (6.40) | .46 | .633 |
| Risk of eating disorder* | 11 | 14.45 (10.08) | 24 | 13.08 (5.87) | 12 | 21.33 (6.07) | 5.57 | .007 | 12 | 15.17 (9.74) | 12 | 15.67 (6.53) | 25 | 16.88 (9.11) | .18 | .834 |
| Paranoid ideation* | 11 | 11.73 (1.43) | 24 | 12.88 (1.13) | 12 | 17.17 (.90) | 5.01 | .011 | 12 | 14.58 (4.74) | 12 | 14.42 (5.66) | 25 | 13 (4.59) | .58 | .566 |
| Bizarre Thought | 11 | 10 (4.73) | 24 | 11.25 (6.39) | 12 | 13.08 (5.35) | .84 | .441 | 12 | 10.67 (4.40) | 12 | 11.83 (7.65) | 25 | 11.24 (5.27) | .12 | .884 |
| Sexual discomfort* | 11 | 6 (2.37) | 24 | 6.17 (2.91) | 12 | 10 (4.02) | 6.92 | .002 | 12 | 6.50 (2.97) | 12 | 6.83 (3.66) | 25 | 6.72 (3.49) | .03 | .970 |
*Significant differences among Diagnostic Categories;
**Significant differences among different states of treatment;
***Significant differences in both Diagnostic Categories and State of treatment
On the BIS-11 scale, a test for measuring impulsiveness and its traits, the Personality disorders group scored higher than the other two groups on the Self-control scale (Non-planning Impulsiveness category) (p = .001), Non-planning Impulsiveness (p =.001) and on the total BIS-11 scale (p =.004) (see table 4).
Table 3.
ANOVA among the groups in relation to Diagnostic Categories and to the state of treatment (PTI scale) – part II
| PTI Scales | Diagnostic Categories | F | p | State of Treatment | F | p | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mood Disorder | Personality Disorder | Psychotic Disorder | Conclusion | Drop-out | In-Treatment | |||||||||||
| N | M (SD) | N | M (SD) | N | M (SD) | N | M (SD) | N | M (SD) | N | M (SD) | |||||
| Clinical Area | ||||||||||||||||
| Deviance | 11 | 19.09 (6.44) | 24 | 17.63 (4.76) | 12 | 18.33 (3.31) | .35 | .708 | 12 | 16.83 (4.02) | 12 | 17.25 (4.16) | 25 | 18.64 (5.27) | .72 | .493 |
| Impulsiveness | 11 | 15.82 (6.43) | 24 | 14.33 (3.29) | 12 | 12.67 (3.89) | 1.52 | .230 | 12 | 14.67 (6.57) | 12 | 15.17 (4.32) | 25 | 15.20 (4.08) | .05 | .949 |
| Hypomania | 11 | 12.36 (5.73) | 24 | 12.79 (4.09) | 12 | 14 (5.98) | .35 | .708 | 12 | 12.83 (3.97) | 12 | 12.17 (5.17) | 25 | 12.64 (5.14) | .06 | .941 |
| Cluster A – Pers. Disorder* | 11 | 5.09 (2.17) | 23 | 6.65 (2.76) | 12 | 7.75 (1.81) | 3.51 | .039 | 12 | 6.50 (2.65) | 12 | 6.33 (3.06) | 25 | 5.80 (2.12) | .39 | .682 |
| Cluster B- pers. Disorder | 11 | 9.45 (4.32) | 23 | 10.13 (2.88) | 12 | 12.75 (3.70) | 3.10 | .055 | 12 | 9.42 (3.90) | 12 | 8.50 (3.34) | 25 | 11.64 (4.00) | 3.18 | .051 |
| Cluster C – Pers. Disorder* | 11 | 4.73 (2.15) | 23 | 7.17 (2.62) | 12 | 8 (3.19) | 4.71 | .014 | 12 | 6.58 (2.47) | 12 | 5.75 (2.09) | 25 | 6.16 (2.48) | .37 | .696 |
| Psychological Treatment Area | ||||||||||||||||
| Secure attachment style | 10 | 17.90 (4.01) | 23 | 16.17 (4.38) | 12 | 17.50 (4.76) | .68 | .512 | 10 | 14.60 (3.57) | 11 | 15.00 (4.34) | 25 | 17.60 (4.27) | 2.61 | .086 |
| Anxious attachment style* | 10 | 9 (1.78) | 23 | 13.96 (5.66) | 12 | 16.92 (4.78) | 6.62 | .003 | 10 | 13.90 (5.93) | 11 | 11.73 (5.06) | 25 | 13 (5.10) | .46 | .637 |
| Avoidant attachment style | 10 | 11.60 (5.32) | 23 | 10.78 (4.71) | 12 | 12.25 (6.09) | .32 | .725 | 10 | 10.21 (3.99) | 11 | 10.55 (3.62) | 25 | 11 (4.25) | .15 | .860 |
| Unresolved attachment style | 10 | 7 (1.56) | 23 | 8.70 (4.38) | 12 | 10.58 (4.58) | 2.20 | .123 | 10 | 7.30 (1.49) | 11 | 8.18 (4.00) | 25 | 9.04 (3.86) | .91 | .410 |
| Mature defence style* | 11 | 16.18 (1.54) | 24 | 16.08 (3.24) | 12 | 19.17 (4.47) | 3.80 | .031 | 10 | 15.83 (3.13) | 11 | 15.17 (3.16) | 25 | 17 (3.52) | 1.35 | .270 |
| Anxious defence style | 11 | 11 (4.38) | 24 | 11.88 (4.60) | 12 | 12.25 (2.53) | .28 | .757 | 10 | 10.50 (4.46) | 11 | 10.50 (3.09) | 25 | 11.84 (3.87) | .74 | .483 |
| Avoidant defence style* | 11 | 9.72 (2.94) | 24 | 11.29 (2.61) | 12 | 12.92 (2.50) | 4.12 | .023 | 10 | 11.17 (2.95) | 11 | 10.58 (2.84) | 25 | 11.28 (2.91) | .24 | .787 |
| Immature defence style* | 11 | 11.09 (4.59) | 24 | 11.83 (3.67) | 12 | 15.17 (4.57) | 3.46 | .040 | 10 | 10.83 (3.27) | 11 | 11.33 (4.03) | 25 | 13.04 (4.57) | 1.40 | .258 |
| Alexithymia | 11 | 9.18 (3.37) | 24 | 11.96 (4.36) | 12 | 12.83 (5.08) | 2.25 | .117 | 12 | 11.42 (4.08) | 12 | 11 (4.11) | 25 | 11.40 (4.33) | .04 | .959 |
| Frustration Intolerance | 11 | 9.81 (2.27) | 24 | 11.71 (3.82) | 12 | 12.42 (4.25) | 1.58 | .217 | 12 | 11.17 (3.69) | 12 | 10.33 (2.93) | 25 | 10.76 (3.49) | .18 | .837 |
| Negative Impression | 11 | 10.64 (3.93) | 24 | 11.92 (4.81) | 12 | 14.50 (2.47) | 2.69 | .079 | 12 | 11.08 (4.64) | 12 | 10.67 (4.03) | 25 | 10.96 (3.74) | .04 | .966 |
| Resistance to change* | 11 | 5.27 (1.62) | 24 | 9 (3.99) | 12 | 8.42 (3.90) | 4.24 | .021 | 12 | 7.08 (3.34) | 12 | 7.33 (3.42) | 25 | 7.12 (3.92) | .02 | .983 |
| Manipulation* | 11 | 9 (3.35) | 24 | 10.63 (3.76) | 12 | 13.08 (4.32) | 3.38 | .043 | 12 | 10.08 (3.87) | 12 | 9.58 (2.81) | 25 | 10.48 (4.17) | .23 | .798 |
| Empathy* | 11 | 17.82 (4.07) | 24 | 15.00 (3.75) | 12 | 19.17 (5.69) | 4.06 | .024 | 12 | 15.92 (4.36) | 12 | 17.17 (4.80) | 25 | 18.64 (5.04) | 1.36 | .267 |
| Propensity to Insight | 11 | 19.36 (3.93) | 24 | 16.88 (4.55) | 12 | 20 (5.56) | 2.17 | .126 | 12 | 17 (4.22) | 12 | 15.75 (4.73) | 25 | 18.76 (5.41) | 1.59 | .215 |
| Treatment Expectation | 11 | 15.91 (4.11) | 24 | 14.71 (4.51) | 12 | 15.92 (4.27) | .45 | .642 | 12 | 15.83 (3.30) | 12 | 15.25 (5.14) | 25 | 17.40 (4.96) | 1.02 | .369 |
| Working Alliance | 8 | 18 (3.61) | 20 | 15.75 (4.78) | 7 | 18.14 (3.44) | .94 | .404 | 11 | 16.73 (3.50) | 7 | 19 (5.95) | 15 | 18.67 (4.27) | .79 | .461 |
*Significant differences among Diagnostic Categories;
**Significant differences among different states of treatment;
***Significant differences in both Diagnostic Categories and State of treatment
The TAS-20 measured alexithymia and its traits. The Personality disorder group and the Psychotic disorder group obtained higher scores on the externally-oriented thinking subscale (p = .019) compared to the Mood disorder group (see table 4).
At the conclusion of treatment, the In-Treatment group showed higher levels of psychological resources (referring to self-esteem and perceived social support), and lower levels of impulsivity, than the other two groups (see table 3- part I and table 4).
The following variables—Self-control, Non-Planning Impulsiveness, the total of the BIS-11, CH, the total of the PPI-R, and the total of the TAS-20—represented adequate markers for interpreting discriminant functions. So, considering these discriminant function coefficients (CDF), the discriminant function obtained is:
f = 0.591 [CDF1] + 0.566 [CDF2] + 0.533 [CDF3] + 0.512 [CDF4] + 0.371 [CDF5] + 0.362 [CDF6]
where the values of f are the discriminant scores, CDF1 is Self-control, CDF2 is Non-Planning Impulsiveness, CDF3 is the total of the BIS-11, CDF4 is Cold Heartedness, CDF5 is total of the PPI-R and CDF6 is the total of the TAS-20. With these variables, the function variables correctly classified the cases (subjects) into one of two hypothesized groups—Drop-Out or In-Treatment—with an accuracy of 59.5% within the cross-validation condition. (see table 5).
Table 4.
ANOVA among the groups in relation to Diagnostic Categories and to the state of treatment (PPI-R, BIS-11 and TAS20 Scales)
| Scales | Diagnostic Categories | F | p | State of Treatment | F | p | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mood Disorder (N=12) | Personality Disorder (N=25) | Psychotic Disorder (N=12) | Conclusion (N=12) | Drop-out (N=12) | In-Treatment (N=25) | |||||
| M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | |||||
| Virtuous Responding | 31.64 (3.93) | 31.33 (5.98) | 32.08 (4.60) | .08 | .921 | 31 (5.85) | 32 (4.86) | 29.92 (5.67) | .60 | .554 |
| Inconsistent Responding | 15.73 (4.15) | 18.38 (4.64) | 19 (4.973) | 1.68 | .198 | 17.58 (5.63) | 17.25 (4.41) | 16.40 (4.24) | .31 | .736 |
| Machiavellian Egocentricity | 40.45 (7.47) | 42.33 (8.56) | 42 (5.66) | .23 | .795 | 42.75 (8.07) | 45 (5.54) | 41.84 (7.62) | .76 | .473 |
| Rebellious Nonconformity | 36.36 (7.92) | 37.54 (7.44) | 39.83 (8.72) | .59 | .557 | 35.92 (7.95) | 37.75 (5.67) | 38.56 (8.01) | .50 | .608 |
| Blame Externalization | 33.45 (7.69) | 37.96 (8.55) | 39.17 (7.91) | 1.59 | .215 | 38.08 (7.63) | 35.83 (6.38) | 37.88 (8.60) | .33 | .722 |
| Carefree Nonplanfulness | 36.27 (5.37) | 40.71 (9.12) | 43.58 (9.29) | 2.18 | .125 | 41.75 (11.86) | 41.50 (7.09) | 39.04 (6.55) | .60 | .551 |
| Social Influence | 43.8 (6.59) | 43.88 (8.37) | 46.33 (5.43) | .51 | .605 | 43.50 (7.60) | 45.75 (6.48) | 47.80 (6.94) | 1.57 | .219 |
| Fearlessness | 38.45 (8.42) | 38.46 (6.54) | 38.42 (5.73) | .00 | 1 | 37 (6.66) | 41.33 (5.47) | 38.36 (7.24) | 1.34 | .273 |
| Stress Immunity | 32.09 (5.01) | 31.62 (7.87) | 33.33 (3.34) | .29 | .752 | 31.17 (7.66) | 33.17 (5.13) | 31.52 (6.23) | .36 | .700 |
| Cold-heartedness | 33.91 (3.51) | 36.88 (5.62) | 32.08 (10.17) | 2.21 | .122 | 36.00 (7.72) | 38.75 (15.41) | 31.88 (6.89) | 2.17 | .126 |
| The Self-Centered Impulsivity | 146.55 (23.24) | 158.54 (21.56) | 164.58 (15.97) | 2.27 | .116 | 158.50 (23.74) | 160.08 (11.51) | 157.32 (21.65) | .076 | .927 |
| Fearless Dominance | 114.36 (12.82) | 113.96 (17.18) | 118.08 (10.02) | .33 | .719 | 111.67 (14.95) | 120.25 (9.55) | 117.68 (14.34) | 1.31 | .280 |
| TOT. PPI-R | 294.82 (31.01) | 309.38 (25.02) | 314.75 (12.19) | 2.13 | .131 | 306.17 (22.12) | 319.08 (21.69) | 306.88 (26.90) | 1.16 | .323 |
| Attention | 9.56 (2.98) | 10.96 (2.85) | 11.08 (2.47) | 1.15 | .325 | 11.75 (2.70) | 11.33 (2.31) | 10.08 (2.87) | 1.86 | .168 |
| Motor | 13.18 (2.79) | 15.42 (2.80) | 13.42 (3.29) | 3.08 | .056 | 14.25 (3.55) | 15.75 (3.02) | 14.56 (3.28) | .74 | .485 |
| Self-control*** | 12 (2.90) | 16.21 (2.40) | 12.92 (2.50) | 12.99 | .001 | 16.08 (2.43) | 15.92 (3.15) | 13.68 (2.81) | 4.18 | .021 |
| Cognitive Complexity | 13.09 (2.55) | 14.21 (2.78) | 13.42 (1.44) | .92 | .405 | 14.42 (1.83) | 14.08 (1.78) | 12.88 (2.68) | 2.23 | .120 |
| Perseverance | 9.45 (1.13) | 8.33 (1.90) | 9 (2.73) | 1.28 | .288 | 8.67 (2.02) | 9.42 (1.08) | 8.88 (2.49) | .41 | .665 |
| Cognitive Instability | 5 (1.67) | 6.13 (1.68) | 5.67 (1.07) | 2.02 | .145 | 6.17 (2.25) | 6.08 (1.68) | 6.16 (1.72) | .01 | .992 |
| Attentional Impulsiveness | 14.55 (3.67) | 17.08 (3.28) | 16.75 (2.45) | 2.48 | .096 | 17.92 (4.19) | 17.42 (2.02) | 16.24 (3.78) | 1.05 | .359 |
| Motor Impulsiveness | 22.64 (3.04) | 23.75 (4.05) | 22.42 (3.65) | .64 | .531 | 22.92 (4.76) | 25.17 (3.76) | 23.44 (4.10) | .99 | ,379 |
| Non-planning Impulsiveness*** | 25.09 (4.64) | 30.42 (4.26) | 26.33 (2.77) | 8.15 | .001 | 30.50 (3.34) | 30 (4.02) | 26.56 (4.96) | 4.34 | .019 |
| TOT. BIS-11* | 62.27 (7.93) | 71.25 (8.02) | 65.50 (4.74) | 6.40 | .004 | 71.33 (9.47) | 72.58 (7.29) | 66.24 (9.93) | 2.39 | .103 |
| Difficulty identifying feelings | 14.73 (6.36) | 16.96 (7.85) | 19.50 (7.72) | 1.17 | .321 | 16.75 (8.87) | 17.92 (6.20) | 16.84 (7.32) | .10 | .905 |
| Difficulty describing feelings | 12 (4.31) | 14.83 (5.18) | 13.25 (3.60) | 1.51 | .232 | 14.92 (6.39) | 15.50 (2.50) | 13.28 (3.96) | 1.22 | .304 |
| Externally- Oriented Thinking * | 16.27 (5.20) | 21.17 (3.66) | 19.75 (5.50) | 4.37 | .019 | 21.75 (4.07) | 19.92 (4.98) | 18.08 (5.67) | 2.12 | .132 |
| TOT. TAS20 | 43 (13.00) | 52.96 (14.19) | 52.50 (10.49) | 2.37 | .105 | 53.42 (16.52) | 53.33 (9.67) | 48.20 (11.45) | 1.05 | .358 |
*Significant differences among Diagnostic Categories; **Significant differences among different states of treatment; ***Significant differences in both Diagnostic Categories and State of treatment
Table 5.
Classification Results by Discriminant Analysis 1,2
| Treatment | Prediction of Group Membership | ||||
|---|---|---|---|---|---|
| Drop-Out | In-Treatment | Total | |||
| Original | Units | Drop-Out | 9 | 3 | 12 |
| In-Treatment | 6 | 19 | 25 | ||
| Cases number | 27 | 38 | 65 | ||
| % | Drop-Out | 75 | 25 | 100 | |
| In-Treatment | 24 | 76 | 100 | ||
| % Cases | 41.5 | 58.5 | 100 | ||
| Cross-Validated | Units | Drop-Out | 6 | 6 | 12 |
| In-Treatment | 9 | 16 | 25 | ||
| % | Drop-Out | 50 | 50 | 100 | |
| In-Treatment | 36 | 64 | 100 | ||
| 1. 75.7% of the original groups were correctly classified. | |||||
| 2. 59.5% of the cross-validated groups were correctly classified. | |||||
Discussion
The present study sought to assess residential treatment outcomes in a therapeutic community by repeated test administration (over time and at termination), investigation of psychopathological features in a sample of individuals with substance use disorders and criminal records, and the identification of the variables related to drop-out to prevent premature treatment abandonment, relapses, and risky behaviors.
Concerning the first purpose, no significant differences emerged among the variables under investigation. These results are in agreement with the scientific literature according to which the complexity of these pathologies requires treatments with a long-term perspective, safe and protective living environments, flexibility of clinicians and programs, and integration of mental health and substance abuse therapies (Drake et al., 1993). Indeed, several studies have highlighted the importance of a biopsychosocial approach to complex treatments for addiction diseases linked to criminal behaviors. This approach stresses a close linkage among lifestyles, behavior patterns, traumatic events, and vulnerability factors, distinctive of this condition (Esbec & Echeburúa, 2016; Widom & White, 1997; Da Silva Roggi et al., 2015). The effects of substance abuse differ between individuals and depend on biological, situational, and psychological factors (Walters, 2014).
However, our results provided interesting data when we compared the three diagnostic groups: Mood Disorders, Personality Disorders, and Psychotic Disorders.
From the results obtained, an initial cluster seemed to emerge. This cluster corresponded to the Mood Disorders group, and these individuals tended to emphasize their own problems and exhibited a more specific symptomatology. This cluster seemed to be less-impulsive and had a greater predisposition to remain in treatment, compared to the two groups. These individuals were likely more inclined to assume responsibility for their actions, as also shown by their lower scores on the Externally Oriented Thinking scale. This suggests that these individuals possessed more of an internal locus of control compared to the other two groups. Indeed, according to the personality organization model (Kernberg, 1993; Caligor, Kernberg, & Clarkin, 2007), they exhibited higher levels of borderline personality organization, which include more adaptation, better capacity for intimate involvement, better superego integration, and sufficient nonconflictual development of some ego functions, even though there was obvious identity diffusion. These characteristics are also typical of mafia members, supporting the evidence described above. Adhering to a criminal and sociopathic framework, mafia members maintain very close ties with both the family and the group to which they belong. All the while, they tend to exhibit identity instability and an internal emotional world characterized by a narcissistic vulnerability (Schimmenti et al., 2014; Crapraro et al., 2018).
A second cluster corresponded to the Personality Disorders group. These individuals exhibited greater resistance to change, lower levels of self-esteem, and less social support than the other groups. They were also more impulsive and, as shown by their characteristically high scores on the Externally Oriented Thinking scale, had more of an external locus of control than the first cluster. This cluster exhibited specific characteristics such as instability, difficulty delaying needs satisfaction, and a tendency to externalize blame. This is in line with the Kernberg’s considerations, which underline how patients with a Low Borderline Organization show diffusion, manifestations of primitive defensive operations, and severe distortions in their interpersonal relations. These qualities manifest as anger, emotional lability, and self-destructive impulsive behaviors (Kernberg, 1993; Caligor, Kernberg, & Clarkin, 2007) such as substance abuse. Several studies (e.g., Ball & Cecero, 2001; Brune, Ghiassi, & Ribbert, 2010) have shown that, in many cases, patients with personality disorders have experienced different forms of traumatic experiences (for example abandonment, instability, mistrust, abuse) and this is reflected in the present study by problems related to a familiar issue, poor social support and low self-esteem. According to this perspective, a deficiency in self-control can be linked to difficulty and dysfunctional coping strategies in dealing with negative emotions (Lacey & Evans, 1986; Kennedy & Grubin, 1990; Craparo, 2014; Di Pierro, Benzi, & Madeddu, 2015; Napryeyenko et al., 2019). This results in a substances abuse as an attempt to self-medicate the feelings derived from traumatic experiences (Caretti et al., 2018; Kuss et al., 2017; Spada & Marino, 2017; Pace et al., 2013; Caretti & La Barbera, 2005). To complicate this picture, the absence of self-control is also closely associated with crime and violence, especially antisocial personality disorder and borderline personality disorder (Edwards et al., 2003; Yarvis 1991; Longshore, 1998; Longshore, Turner, & Stein, 1996).
Finally, according to the hypothesized diagnostic distinctions, a third cluster emerged, with a more variegated (and probably more severe) symptomatology, and more pronounced paranoid ideation. Individuals in this group exhibited greater levels of anxiety in relationships and, as demonstrated by group member’s high scores on the Externally Oriented Thinking scale, a more external locus of control than the first cluster. Members of this cluster showed a failure to differentiate between representations of the self and the object, a loss in reality testing (Kernberg, 1993) and non-adherence with treatment (Soyka, 2000).
These data confirm the complex framework of individuals with SUD and criminal records, which was characterized by a constellation of emotional, interpersonal, and behavioral difficulties (Gori et al., 2017). So, these results about the clinical groups allow a greater understanding of the specific situations and can facilitate useful reflections to develop diversified therapy methods, in order to improve insight (Gori et al., 2015), and to be able to offer a type of treatment that is both more effective and increasingly tailored to individual needs.
Our results also suggest important predictors of drop-out: psychopathic traits, CH, Non-planning Impulsiveness, and alexithymia. These results are in line with the results of the study by Staton-Tindall and colleagues (2007), which highlighted the significant relationship between CH and low treatment engagement, specifically for males. The data shows that even impulsivity is associated with a greater drop-out risk, confirming previous research (Gori et al., 2016). Those who abuse substances and exhibit higher levels of impulsivity in action and choices do not seem to benefit from addiction treatment programs to the same extent as their less-impulsive counterparts (Charney et al., 2007; Stevens et al., 2014). Specifically, the Self-control subscale seems to be particularly relevant. Indeed, several studies show how subjects which practice and improved this dimension can improve adherence to treatment, abstain longer and undergo fewer relapses (Muraven, 2010; Hobuen et al., 2012; Houben et al., 2011; Garavan & Hester, 2007).
Other important reflections concern the role of psychopathic traits on therapy outcome. Traditionally, individuals with these traits are considered unsuitable for treatment due to poor empirical support of their treatability. Therapeutic actions or rehabilitation programs that are commonly administered in prisons are often useless and counterproductive (Hughes et al., 1998; Ogloff, Wong, & Greenwood, 1990; Rice, Harris, & Cormier, 1992; Seto & Barbaree 1999; Barbaree, 2005; Anderson & Kiehl, 2014).
Nevertheless, several studies (Olver, Lewis, & Wong, 2013; Caldwell et al., 2006) have shown how the treatment of individuals with psychopathic characteristics is more effective when is based mainly on the features linked to their criminal behaviors. This leads to a decrease in the rate of recurrent offenses (Polasheck, 2014). In particular, a study by Seager and colleagues (2006) indicated that individuals who refused treatment or dropped out had six times the rate of repeat sexual and violent offences compared to those who completed the treatment. Hence, the clinical approach to treat psychopathic features should not be focused on mere rehabilitation; rather, it should be aimed at reducing the rate of repeat offences.
Clinical research indicates that individuals with high psychopathic trait scores are charged with violent crimes twice as frequently as non-psychopathic offenders (Hare & Jutai, 1983). Moreover, these individuals are more likely to be motivated to commit violent acts because of CH or unemotional traits (Walters, 2006; Williamson, Hare, & Wong, 1987).
Psychopathic traits and alexithymia have been largely studied previously (Kroner & Forth, 1995; Louth, Hare, & Linden, 1998), and several studies have shown particular deficits in emotional processing of both alexithymic and psychopathic subjects. These include difficulties interpreting facial expressions (Dolan & Fullam, 2006), understanding emotional tone in language (Herve, Hayes, & Hare, 2003), and describing one’s own feelings (Luminet et al., 2004); therefore the lack of emotional processing may mediate the relationship between psychopathic characteristics and aggression, including illegal behaviors (Porter & Woodworth, 2006).
All these data are of additional importance in light of previous research that highlights how addiction treatment permanence is strongly associated with important reductions in the most common forms of crime (Hubbard et al., 1989; Ball & Ross, 1991; Hunt, Lipton, & Spunt, 1984; Flynn et al., 2002; Flynn et al., 2003): therefore, substantial changes in behavior have been noted, and these changes have considerable personal, social and clinical importance (Gossop et al., 2005). These features, if viewed in their global configuration, may help to develop a specific model to predict drop-outs and relapses in these specific patients. Further investigations are considered necessary to validate the role of these variables in predicting the treatment outcomes (Gori et al., 2010).
This was a preliminary study; thus, several limitations warrant consideration. Data collection from this cohort was challenging. We did not use structured interviews to detect traits inherent to psychopathy. Finally, our analyses were the result of examination of a relatively small cohort. Therefore, our results cannot serve as a basis for a final therapeutic or predictive model and may not be generalizable to individuals with SUD as a whole. To provide more reliable data, future studies should examine a larger sample. However, despite these limitations, this study provides a further piece for the understanding of subjects with SUD and criminal records, suggesting the importance of an integrative approach for addictive behaviors, including a psychodynamic oriented framework, and showing the impact of impulsiveness, cold-heartedness, alexithymia, and psychopathic traits on treatment drop-out.
References
- Aggarwal, A., Vaish, S., Sharma, D. K., Sushil, C. S., Usman, N., & Sudarsanan, S. (2015). A study of personality profile and criminal behavior in substance abusers. Industrial psychiatry journal, 24 (1), 35-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson, N. E., & Kiehl, K. A. (2014). Psychopathy: developmental perspectives and their implications for treatment. Restorative neurology and neuroscience, 32(1), 103-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ball, S. A., & Cecero, J. J. (2001). Addicted patients with personality disorders: Traits, schemas, and presenting problems. Journal of personality disorders, 15(1), 72-83. [DOI] [PubMed] [Google Scholar]
- Ball J. C., & Ross, A. (1991). The Effectiveness of Methadone Maintenance Treatment: Patients, Programs, Services, and Outcome. Springer-Verlag. [Google Scholar]
- Bagby, R. M., Parker, J. D. A., & Taylor, G. J. (1994). The Twenty-Item Alexithymia Scale-I. Item selection and cross-validation of the factor structure. Journal of Psychosomatic Research, 38, 33-40. [DOI] [PubMed] [Google Scholar]
- Bagby, R. M., Taylor, G. J., & Parker, J. D. A. (1994). The twenty-Item Toronto alexithymia Scale-II. Convergent, Discriminant, and Concurrent Validity. Journal of Psychosomatic Research, 38 (1), 33-40. [DOI] [PubMed] [Google Scholar]
- Barbaree, H. E. (2005). Psychopathy, treatment behavior, and recidivism: An extended follow-up of Seto and Barbaree. Journal of Interpersonal Violence, 20(9), 1115-1131. [DOI] [PubMed] [Google Scholar]
- Bennett, H. T., Holloway, K., & Farrington D.P., (2008). The statistical Association between Drug Misuse and Crime: A Meta-analysis. Aggression and Violent Behavior, 13, 107-118. [Google Scholar]
- Benning, S. D., Patrick, C. J., Hicks, B. M., Blonigen, D. M., & Krueger, R. F. (2003). Factor structure of the psychopathic personality inventory: validity and implications for clinical assessment. Psychological assessment, 15(3), 340. [DOI] [PubMed] [Google Scholar]
- Best, D., Sidwell, C., Gossop, M., Harris, J., & Strang, J. (2001). Crime and expenditure amongst poly drug misusers seeking treatment - the connection between prescribed methadone and crack use, and criminal involvement. British Journal of Criminology, 41, 119-126. [Google Scholar]
- Bondeson, U. V. (2009). A comparative study of recidivism rates between prison and suspended prison sanctions”. European Journal of Criminology, 6, 459-480. [Google Scholar]
- Bressi, C., Taylor, G., Parker, J., Bressi, S., Brambilla, V., Aguglia, E., ... & Todarello, O. (1996). Cross validation of the factor structure of the 20-item Toronto Alexithymia Scale: an Italian multicenter study. Journal of psychosomatic research, 41(6), 551-559. [DOI] [PubMed] [Google Scholar]
- Brune, M., Ghiassi, V., & Ribbert, H. (2010). Does borderline personality disorder reflect the pathological extreme of an adaptive reproductive strategy? Insights and hypotheses from evolutionary life-history theory. Clinical Neuropsychiatry, 3-10.
- Caldwell, M., Skeem, J., Salekin, R., & Van Rybroek, G. (2006). Treatment response of adolescent offenders with psychopathy features: A 2-year follow-up. Criminal Justice and Behavior, 33(5), 571-596. [Google Scholar]
- Caligor, E., Kernberg, O. F., & Clarkin, J. F. (2007). Handbook of dynamic psychotherapy for higher level personality pathology. American Psychiatric Pub. [Google Scholar]
- Caretti, V., & La Barbera, D. (2005). Alessitimia, valutazione e trattamento. Astrolabio.
- Caretti, V., Gori, A., Craparo, G., Giannini, M., Iraci-Sareri, G. & Schimmenti, A. (2018). A new measure for assessing substance-related and addictive disorders: The Addictive Behavior Questionnaire (ABQ). Journal of Clinical Medicine, 7 (8), 194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charney, D. A., & Gill, K. J. (2007). Impulsivity, personality disorders and the engagement in addiction treatment. European Psychiatry, 22, S184. [Google Scholar]
- Craparo, G. (2014). The role of dissociation, affect dysregulation, and developmental trauma in sexual addiction. Clinical Neuropsychiatry, 11(2), 86-90. [Google Scholar]
- Craparo, G., David, V., Costanzo, G., & Gori, A. (2018). Cosa Nostra and the Camorra: Assessment of personality, alexithymic traits, and attachment styles. International journal of law and psychiatry, 58, 17-26. [DOI] [PubMed] [Google Scholar]
- Da Silva Roggi, M. P., Da Gama, F. N. M., Neves, S. F., & Garcia, F. (2015). Update on treatment of craving in patients with addiction using cognitive behavioral therapy. Clinical Neuropsychiatry, 12(5), 118-127. [Google Scholar]
- Di Pierro, R., Benzi, M. A. I., & Madeddu, F. (2015). Difficulties in emotion regulation among inpatients with substance use disorders: The mediating effect of mature defenses mechanisms. Clinical neuropsychiatry, 12(4), 83-89. [Google Scholar]
- Dolan, M., & Fullam, R. (2006). Face affect recognition deficits in personality- disordered offenders: Association with psychopathy. Psychological Medicine, 36, 1563-1569. [DOI] [PubMed] [Google Scholar]
- Drake, R. E., Bartels, S. J., Teague, G. B., Noordsy, D. L., & Clark, R. E. (1993). Treatment of substance abuse in severely mentally ill patients. Journal of Nervous and Mental Disease, 181(10), 606-611. [DOI] [PubMed] [Google Scholar]
- Echeburúa, E., & Fernández-Montalvo, J. (2007). Male batterers with and without psychopathy: An exploratory study in Spanish prisons. International Journal of Offender Therapy and comparative criminology, 51(3), 254-263. [DOI] [PubMed] [Google Scholar]
- Edwards, D. W., Scott, C. L., Yarvis, R. M., Paizis, C. L., & Panizzon, M. S. (2003). Impulsiveness, impulsive aggression, personality disorder, and spousal violence. Violence and Victims, 18(1), 3. [DOI] [PubMed] [Google Scholar]
- Esbec, E., & Echeburúa, E. (2016). Substance abuse and crime: considerations for a comprehensive forensic assessment. Adicciones, 28(1), 48-56. [DOI] [PubMed] [Google Scholar]
- Fernández-Montalvo, J., López-Goñi, J. J., Arteaga, A., & Cacho, R. (2013). Criminological profile of patients in addiction treatment. Adicciones, 25(2), 146-155. [PubMed] [Google Scholar]
- Flynn, P. M., Joe, G. W., Broome, K. M., Simpson, D. D., & Brown, B. S. (2003). Looking back on cocaine dependence: Reasons for recovery. American Journal on Addictions, 12(5), 398-411. [PubMed] [Google Scholar]
- Flynn, P. M., Porto, J. V., Rounds-Bryant, J. L., & Kristiansen, P. L. (2002). Costs and benefits of methadone treatment in DATOS-Part 1: Discharged versus continuing patients. Journal of Maintenance in the Addictions, 2(1-2), 129-149. [Google Scholar]
- Fossati, A., Di Ceglie, A., Acquarini, E., & Barrat, E. S. (2001). Psychometric Properties of an Italian Version of the Barratt Impulsiveness Scale-11 (BIS-11) in Nonclinical Subjects. Journal of Clinical Psychology, 57(6), 815–828. [DOI] [PubMed] [Google Scholar]
- Garavan, H., & Hester, R. (2007). The role of cognitive control in cocaine dependence. Neuropsychology review, 17(3), 337-345. [DOI] [PubMed] [Google Scholar]
- Gerstein, D. R. & Harwood, H. J. (1990). Treating drug problems (vol 1). A study of effectiveness and financing of public and private drug treatment systems. Washington DC, Institute of Medicine, National Academy Press. [PubMed] [Google Scholar]
- Goode, E. (1997). Between politics and reason. New York: St Martin’s Press. [Google Scholar]
- Goldstein, P. J. (1985). The drugs/violence nexus: A tripartite conceptual framework. Journal of Drug Issues, 39, 143−174. [Google Scholar]
- Gori, A., Giannini, M., & Schuldberg, D. (2008, May). Mind and body together? A new measure for planning treatment and assessing psychotherapy outcome. Paper presented at the SEPI XXIV Annual Meeting, Boston.
- Gori, A., Lauro-Grotto, R., Giannini M., & Schuldberg D. (2010). Predicting treatment outcome by combining different assessment tools: Toward an integrative model of decision support in psychotherapy. Journal of Psychotherapy Integration, 20 (2) 251-259. [Google Scholar]
- Gori, A., Giannini, M., & Schuldberg, D. (2013). PTI— Psychological Treatment Inventory (PTI), Manuale e questionari. Firenze: Giunti OS-Organizzazioni Speciali. [Google Scholar]
- Gori, A., Craparo, G., Iraci-Sareri, G., Caretti, V., Giannini, M., & Meringolo, P. (2014). Antisocial and psychopathic personalities in a sample of addicted subjects: differences in psychological resources, symptoms, alexithymia and impulsivity. Comprehensive psychiatry, 55(7), 1580-1586. [DOI] [PubMed] [Google Scholar]
- Gori, A., Craparo, G., Giannini, M., Loscalzo, Y., Caretti, V., La Barbera, D., Manzoni, GM., Castelnuovo, G., Tani, F., Ponti, L., Dewey, D., & Schuldberg, D. (2015). Development of a new measure for assessing insight: psychometric properties of the insight orientation scale (IOS). Schizophrenia research, 169(1-3), 298-302. [DOI] [PubMed] [Google Scholar]
- Gori, A., Craparo, G., Caretti, V., Giannini, M., Iraci-Sareri, G., Bruschi, A., Janiri, L., Ponti, L. & Tani, F. (2016). Impulsivity, alexithymia and dissociation among pathological gamblers in different therapeutic settings: A multisample comparison study. Psychiatry research, 246, 789-795. [DOI] [PubMed] [Google Scholar]
- Gori, A., Ponti, L., Tani, F., Iraci Sareri, G., Giannini, M., Meringolo, P., Craparo, G., Bruschi, A., Caretti, V., Cacioppo, M., Paterniti, R., & Schuldberg, D. (2017). Psychopathological features in a sample of substance‐ abusing individuals with criminal history: Towards a definition of a personality prototype of an ‘Addict with Criminal Conduct’. Criminal Behaviour and Mental Health, 27(4), 312-325. [DOI] [PubMed] [Google Scholar]
- Gossop, M., Trakada, K., Stewart, D., & Witton, J. (2005). Reductions in criminal convictions after addiction treatment: 5-year follow-up. Drug and alcohol dependence, 79(3), 295-302. [DOI] [PubMed] [Google Scholar]
- Gottfredson, M. R., & Hirschi, T. (1990). A general theory of crime. Stanford: Stanford University Press. [Google Scholar]
- Graham, N., & Wish, E. (1994). Drug use among female arrestees: Onset, patterns, and relationships to prostitution. Journal of Drug Issues, 24(2), 315−329. [Google Scholar]
- Grann, M., & Fazel, S. (2004). Substance misuse and violent crime: Swedish population study. British Medical Journal, 328, 1233-1234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guydish, J., Wolfe, E., Tajima, B., & Woods, W.J. (2001). Drug court effectiveness: a review of California evaluation reports, 1995-99. J Psychoactive Drugs 33, 369-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hare, R. D. (2003). Manual for the hare psychopathy checklist, 2nd edn, revised. Toronto, ON: Multi-Health Systems. [Google Scholar]
- Hare, R. D., & Jutai, J. W. (1983). Criminal history of the male psychopath: Some preliminary data. In Van Dusen K.T., Mednick S.A. (eds) Prospective studies of crime and delinquency. Longitudinal Research in the Behavioral, Social and Medical Sciences 2 (pp. 225-236). Springer, Dordrecht. [Google Scholar]
- Herve, H. F., Hayes, P. J., & Hare, R. D. (2003). Psychopathy and sensitivity to the emotional polarity of metaphorical statements. Personality and Individual Differences, 35, 1497-1507. [Google Scholar]
- Heyman, G. M. (2009). Addiction: A disorder of choice. Cambridge, MA: Harvard University Press. [Google Scholar]
- Holloway, K., & Bennett, T. (2004). The results of the first two years of the NEW-ADAM programme. London: Home Office. [Google Scholar]
- Houben, K., Havermans, R. C., Nederkoorn, C., & Jansen, A. (2012). Beer à No‐Go: Learning to stop responding to alcohol cues reduces alcohol intake via reduced affective associations rather than increased response inhibition. Addiction, 107(7), 1280-1287. [DOI] [PubMed] [Google Scholar]
- Houben, K., Nederkoorn, C., Wiers, R. W., & Jansen, A. (2011). Resisting temptation: decreasing alcohol-related affect and drinking behavior by training response inhibition. Drug and alcohol dependence, 116(1-3), 132-136. [DOI] [PubMed] [Google Scholar]
- Hough, M. (2002). Drug user treatment within the criminal justice context. Substance use misuse, 37, 985-996. [DOI] [PubMed] [Google Scholar]
- Hubbard, R. L., Marsden, M. E., Rachal, J. V., Harwood, H. J., Cavanaugh, E. R., & Ginzburg, H. M. (1989). Drug abuse treatment: A national study of effectiveness. University of North Carolina Press. [Google Scholar]
- Hughes, G., Hogue, T., Hollin, C., & Champion, H. (1997). First-stage evaluation of a treatment programme for personality disordered offenders. Journal of Forensic Psychiatry, 8(3), 515-527. [Google Scholar]
- Hunt, D. E., Lipton, D. S., & Spunt, B. (1984). Patterns of criminal activity among methadone clients and current narcotics users not in treatment. Journal of Drug Issues, 14(4), 687−702. [Google Scholar]
- Kennedy, H. G., & Grubin, D. H. (1990). Hot‐headed or impulsive?. British Journal of Addiction, 85(5), 639-643. [DOI] [PubMed] [Google Scholar]
- Kernberg, O. F. (1993). Severe personality disorders: Psychotherapeutic strategies. Yale University Press. [Google Scholar]
- Kimonis, E. R., Tatar, I. I., Joseph, R., & Cauffman, E. (2012). Substance-related disorders among juvenile offenders: What role do psychopathic traits play?. Psychology of Addictive Behaviors, 26(2), 212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroner, G.D., & Forth, E.A (1995) The Toronto Alexithymia scale with incarcerated offenders. In Personality and Individual Differences, 19, 625-634. [Google Scholar]
- Kuhns, J.B., Heide, K.M., & Silverman, I. (1992). Substance use/misuse among female prostitutes and female arrestees. International Journal of the Addictions, 27(11),1283−1292. [DOI] [PubMed] [Google Scholar]
- Kuss, D. J., Dunn, T. J., Wölfling, K., Müller, K. W., Hędzelek, M., & Marcinkowski, J. (2017). Excessive Internet use and psychopathology: The role of coping. Clinical Neuropsychiatry: Journal of Treatment Evaluation, 14(1), 73-81. [Google Scholar]
- La Marca, S., Berto, D., & Rovetto, F. (2008). Traduzione ed adattamento italiano del PPI-R: psychopathic personality inventory revised-PPI-R. Firenze, Italy: OS. [Google Scholar]
- Lacey, J. H., & Evans, C. D. H. (1986). The impulsivist: A multi‐impulsive personality disorder. British Journal of Addiction, 81(5), 641-649. [DOI] [PubMed] [Google Scholar]
- Lage, G. M. (2013). Impulsivity: The Behavioral and Neurological Science of Discounting. Clinical Neuropsychiatry, 10(2), 120-121. [Google Scholar]
- Leshner, A. I. (1997). Addiction is a brain disease, and it matters. Science, 278(5335), 45-47. [DOI] [PubMed] [Google Scholar]
- Lilienfeld, S. O., & Andrews, B. P. (1996). Development and preliminary validation of a self-report measure of psychopathic personality traits in noncriminal population. Journal of personality assessment, 66(3), 488-524. [DOI] [PubMed] [Google Scholar]
- Lilienfeld, S.O., & Widows, M.R. (2005). Psychopathic Personality Inventory-Revised: Professional Manual. Lutz, Florida: Psychological Assessment Resources, Inc. [Google Scholar]
- Lo, C.C. & Stephans, R.C. (2000). Drugs and Prisoners: Treatment Needs on Entering Prison. American Journal of Drug and Alcohol Abuse, 26, 229-245. [DOI] [PubMed] [Google Scholar]
- Longshore, D. (1998). Self-control and criminal opportunity: A prospective test of the general theory of crime. Social Problems, 45(1), 102-113. [Google Scholar]
- Longshore, D., Rand, S. T., & Stein, J. A. (1996). Self‐control in a criminal sample: An examination of construct validity. Criminology, 34(2), 209-228. [Google Scholar]
- Louth, S. M., Hare, R. D., & Linden, W. (1998). Psychopathy and alexithymia in female offenders. Canadian Journal of Behavioural Science / Revue canadienne des sciences du comportement, 30(2), 91-98. [Google Scholar]
- Luminet, O., Rime, B., Bagby, R. M., & Taylor, G. J. (2004). A multimodal investigation of emotional responding in alexithymia. Cognition & Emotion, 18, 741-766. [Google Scholar]
- McBride, D. (1981). Drugs and violence. In Inciardi J. A. (Eds.). The drugs–crime connection. (pp. 105−123). Beverly Hills: Sage Publications. [Google Scholar]
- Morse, S. J. (2011). Addiction and criminal responsibility. In Poland J. & Graham G. (Eds.), Addiction and responsibility (pp. 159–199). New York: The MIT Press. [Google Scholar]
- Muratori, P., Pisano, S., Levantini, V., Manfredi, A., Papini, M., Ruglioni, L., ... & Masi, G. (2018). Predictive utility of psychopathy dimensions in italian children with disruptive behavior disorder. Clinical Neuropsychiatry, 15(6), 333-337. [Google Scholar]
- Muraven, M. (2010). Practicing self-control lowers the risk of smoking lapse. Psychology of Addictive Behaviors, 24(3), 446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Napryeyenko, O., Napryeyenko, N., Marazziti, D., Loganovsky, K., Mucci, F., Loganovskaja, T., & Tsekhmister, Y. (2019). Depressive syndromes associated with alcohol dependence. Clinical Neuropsychiatry, 16(5/6), 206-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumann, C. S., Malterer, M. B., & Newman, J. P. (2008). Factor structure of the Psychopathic Personality Inventory (PPI): Findings from a large incarcerated sample. Psychological assessment, 20(2), 169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogloff, J. R. P., Wong, S., & Greenwood, A. (1990). Treating criminal psychopaths in a therapeutic community program. Behavioral Sciences & the Law, 8(2), 181-190. [Google Scholar]
- Olver, M. E., Lewis, K., & Wong, S. C. P. (2013). Risk reduction treatment of high-risk psychopathic offenders: The relationship of psychopathy and treatment change to violent recidivism. Personality Disorders: Theory, Research, and Treatment. 4, 160–167. [DOI] [PubMed] [Google Scholar]
- Pace, U., Schimmenti, A., Zappulla, C., & Di Maggio, R. (2013). Psychological variables characterizing different types of adolescent gamblers: A discriminant function analysis. Clinical Neuropsychiatry, 10(6), 253-259. [Google Scholar]
- Patton, J. H., Stanford, M. S., & Barratt, E. S. (1995). Factor structure of the Barratt impulsiveness scale. Journal of clinical psychology, 51(6), 768-774. [DOI] [PubMed] [Google Scholar]
- Polaschek, D. L. (2014). Adult criminals with psychopathy: Common beliefs about treatability and change have little empirical support. Current Directions in Psychological Science, 23(4), 296-301. [Google Scholar]
- Porter, L., Arif, A. & Curran, W. J. (1986). The law and the treatment of drug- and alcohol- dependent persons: a comparative study of existing legislation. Geneva, WHO. [DOI] [PubMed] [Google Scholar]
- Porter, S., & Woodworth, M. (2006). Psychopathy and Aggression. In Patrick C. J. (Ed.), Handbook of psychopathy (pp. 481-494). New York, NY, US: The Guilford Press. [Google Scholar]
- Rice, M. E., Harris, G. T., & Cormier, C. A. (1992). An evaluation of a maximum security therapeutic community for psychopaths and other mentally disordered offenders. Law and human behavior, 16(4), 399-412. [Google Scholar]
- Seager, J. A., Jellicoe, D., & Dhaliwal, G. K. (2004). Refusers, dropouts, and completers: Measuring sex offender treatment efficacy. International Journal of Offender Therapy and Comparative Criminology, 48(5), 600-612. [DOI] [PubMed] [Google Scholar]
- Schimmenti, A., Caprì, C., La Barbera, D., & Caretti, V. (2014). Mafia and psychopathy. Criminal Behaviour and Mental Health, 24(5), 321-331. [DOI] [PubMed] [Google Scholar]
- Schulz, N., Murphy, B., & Verona, E. (2016). Gender differences in psychopathy links to drug use. Law and Human Behavior, 40(2), 159-168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seto, M. C., & Barbaree, H. E. (1999). Psychopathy, treatment behavior, and sex offender recidivism. Journal of interpersonal violence, 14(12), 1235-1248. [DOI] [PubMed] [Google Scholar]
- Simpson, M. (2003). The relationship between drug use and crime: a puzzle inside an enigma. International journal of drug policy, 14, 307-319. [Google Scholar]
- Soyka, M. (2000). Substance misuse, psychiatric disorder and violent and disturbed behaviour. The British Journal of Psychiatry, 176(4), 345-350. [DOI] [PubMed] [Google Scholar]
- Spada, M. M., & Marino, C. (2017). Metacognitions and emotion regulation as predictors of problematic internet use in adolescents. Clinical Neuropsychiatry, 14(1), 59-63. [Google Scholar]
- Staton-Tindall, M., Garner, B. R., Morey, J. T., Leukefeld, C., Krietemeyer, J., Saum, C. A., & Oser, C. B. (2007). Gender differences in treatment engagement among a sample of incarcerated substance abusers. Criminal Justice and Behavior, 34(9), 1143-1156. [Google Scholar]
- Stevens, L., Verdejo-García, A., Goudriaan, A. E., Roeyers, H., Dom, G., & Vanderplasschen, W. (2014). Impulsivity as a vulnerability factor for poor addiction treatment outcomes: a review of neurocognitive findings among individuals with substance use disorders. Journal of Substance Abuse Treatment, 47(1), 58-72. [DOI] [PubMed] [Google Scholar]
- Taylor, J., & Lang, A. R. (2006). Psychopathy and Substance Use Disorders. In Patrick C. J. (Ed.), Handbook of psychopathy (p. 495–511). The Guilford Press. [Google Scholar]
- United Nations Office on Drugs and Crime (UNODC, 2013). Handbook of Strategies to reduce overcrowding in prisons. New York, NY, US: United Nations Office on Drugs and Crime (UNODC). [Google Scholar]
- United Nations Office on Drugs and Crime & World Health Organization (UNODC & WHO, 2018). Treatment and Care for people with drug use disorder in contact with the criminal justice system. Alternative to Conviction or Punishment. Retrieved online 06.03.2020 on https://www.unodc.org/documents/UNODC_WHO_Alternatives_to_Conviction_or_Punishment_2018.pdf [Google Scholar]
- Walters, G. D. (2006). Appraising, researching and conceptualizing criminal thinking: A personal view. Criminal Behaviour and Mental Health, 16, 87-99. [DOI] [PubMed] [Google Scholar]
- Walters, G. D. (2014). Drugs, crime, and their relationships: Theory, research, practice, and policy. Jones & Bartlett Publishers. [Google Scholar]
- White, H.R. (1990). The drug use – delinquency connection in adolescence. In Weisheit, R. (Ed.) Drugs, crime and criminal justice. Cincinnati: Anderson Publishing Company. [Google Scholar]
- White, H. R., Brick, J., & Hansell, S. (1993). A longitudinal investigation of alcohol use and aggression in adolescence. Journal of Studies on Alcohol, Supplement, (11), 62-77. [DOI] [PubMed] [Google Scholar]
- White, H. R., & Gorman, D. M. (2000). Dynamics of the drug–crime relationship. Criminal Justice, 1, 151−218.
- Widom, C. S., & White, H. R. (1997). Problem behaviours in abused and neglected children grown up: prevalence and co‐occurrence of substance abuse, crime and violence. Criminal behaviour and mental health, 7(4), 287-310. [Google Scholar]
- Williamson, S., Hare, R. D., & Wong, S. (1987). Violence: Criminal psychopaths and their victims. Canadian Journal of Behavioural Science/Revue canadienne des sciences du comportement, 19(4), 454-462. [Google Scholar]
- Yacoubian, G. S., Urbach, B. J., Larsen, K. L., Johnson, R. J., & Peters, R. J., Jr. (2001). A comparison of drug use between prostitutes and other female arrestees. Journal of Alcohol and Drug Education, 46(2), 12−26. [Google Scholar]
- Yarvis, R. M. (1991). Homicide: Causative factors and roots (pp. 15-20). Lexington: Lexington Books. [Google Scholar]
- This research was partially supported by the Tuscan Region (Italy) and by Gruppo Incontro Social Cooperative of Pistoia (Italy).