Abstract
The current COVID-19 pandemic is causing direct and indirect effects in the global population. In this paper, fear and its possible forthcoming consequences on health will be investigated and discussed. Fear is an innate reactive emotion to the immediate threats produced by danger. It is hardwired within subcortical survival circuits and originally had to defend the organism from predators. Besides, fear is a cognitive emotional process mediated by the cortical structures, and implies a subjective evaluation both at implicit (subsymbolic, unconscious) and explicit (symbolic, conscious) levels. Within a defensive taxonomy framework, fear can be defined as a reflex triggering a prompt behavior aimed at surviving from predating attacks (freezing), whereas anxiety as a deliberate pattern aimed at planning behaviors for anticipating and avoiding future harm. Fear and anxiety overlap at a subjective level, but are generated by different neurobiological networks and serve different evolutionary goals. The current viral danger and the need for social distancing worsen the sense of loneliness. A wide body of experimental and epidemiological literature evidence that psychological stress, social isolation, and loneliness have a detrimental effect on multiple health-related outcomes including comorbidity, multimorbidity, and mortality. The negative effects can be even higher for people currently living a massive limitation of physical and interpersonal contacts. A strong effort to integrate psychological and medical care is needed to face post-pandemic health issues.
Keywords: anxiety, fear, loneliness, neurobiology, psychosomatics
According to the Inter-Agency Standing Committee (IASC) (2020), people are obviously expected to be both directly and indirectly affected by stressful experiences during the current COVID-19 as well as during any epidemic. The most common responses to this outbreak are fear (of falling ill and dying; of losing livelihoods due to the impossibility to work as quarantined, and of being dismissed from work; of being socially excluded/placed in quarantine due to stigma for being associated with the disease; of being separated from loved ones and caregivers due to quarantine regime; of reliving the experience of a previous epidemic) and fear-related behaviors (e.g., avoiding approaching health facilities due to fear of becoming infected while in care; feelings of helplessness, boredom, loneliness and depression due to isolation). Long-term consequences within communities, families, and vulnerable individuals include the deterioration of social networks, local dynamics, and economies; stigma towards the surviving patients resulting in rejection by communities; anger and aggression against the government and frontline workers; increase of family and intimate partner violence; relapses and other negative outcomes for people with developing or existing mental health and substance use disorders due to avoidance or inability to access their care providers. According to an Italian survey (broadcast on a large TV network, La7), about 60% of people are actually experiencing fear and high distress, and 8% declare to be feeling frozen and scared to death (April 7, 2020). Furthermore, in this war-like period people are experiencing a combination of the basic fears for human beings, namely uncertainty, unsafety, and loneliness. Of course, fear (as well as all other negative emotions as anxiety, stress, pain, etc.) may definitely give some advantages, such as providing information about the environment and our internal state in interacting with the world around.
In this paper, I will focus on our perception of fear and on the consequences of prolonged periods of distressing feelings, namely on the extent by which fear per se can be a risk condition for health vulnerability.
1. What is fear?
It is known that although mosquitoes are the most dangerous animals on Earth (causing 800,000 deaths in 2015: World Health Organization, 2020), we are scared of sharks (causing 6 deaths: International Shark Attack File, 2017) and, although car accidents account for 1,250,000 deaths in the world (World Health Organization, 2017), we have fear of air flying (578 deaths: Bureau of Aircraft Accidents, 2019). In other words, we have less fear facing the most objectively dangerous situations. Fear is not simply the evaluation of a threatening situation but the way we perceive our sense of impotence against a threat. Fear involves a combination of subjective incompetence (I am not able to cope with it), hopelessness (I can do nothing about it), helplessness (no one can help me), and catastrophizing (imminent death is coming closer).
The human mind has a powerful tool aimed to build the sense of self-consistency i.e. the ability to form consistent narratives of our mental images for preserving ourselves. Concerning fear, the basic units for building the image or mental representation are constituted by (a) the thing (sharks, aircrafts), (b) what we think of the thing (disease, death), (c) the feeling triggered by the thing (fear, impotence, self-esteem), and (d) the memory of the thing (past experience with the thing and its real or symbolic context). In one word, fear is my feeling towards the cause of disruption of my existence, i.e. to put it better, the cause of disruption of the continuity and consistency of the self. It is what all the other organisms in nature do through the physical and biochemical communication aimed at preserving their consistency in space and time called homeostasis (Damasio, 2018). Diseases and illnesses (or agents causing infection such as viruses and bacteria) represent major threats to the continuity and the coherence of the self. We tend to use the symbolic function of our mind to complete the stability of the self by relying more on our expectations (priors in the terms of the Predictive Processing Model) rather than on actual inputs (posteriors) (Smith, Weihs, Alkozei, Killgore, & Lane, 2019; Van den Bergh, Witthöft, Petersen, & Brown, 2017). Normally, expectations (priors) fit adequately with actual somatic sensations (posteriors), but individuals are more prone to adhere to anticipations than to somatic inputs in dealing with epidemics or when the subjects are vulnerable to somatization. In psychosomatic medicine, the problematic relationship with one’s own health is conceived as the more or less difficult balance between body feelings and mental expectations of self-coherence. Table 1 shows a summary of the clinical manifestations of this relationship. They range from common reactions occurring in particularly stressful situations (body preoccupation, disease fear and conviction) to progressively more severe clinical forms (from abnormal illness behavior and cyberchondria to hypochondriasis) included in widely used classifications such as DSM-5 (American Psychiatric Association, 2013), ICD-11 (World Health Organization, 2018), and DCPR (Porcelli & Guidi, 2015).
Table 1.
Examples of manifestations of the relationship between perceived and actual bodily sensations from common reactions to clinical forms
| Hypochondriasis (ICD-11; DCPR-R) | Fearful conviction of having a serious life-threatening disease based on a (cognitive) misinterpretation of bodily signals or somatic symptoms. |
| Illness Anxiety Disorder (DSM-5) | High level of anxiety about health with excessive health-related behaviors (e.g., repeatedly checking one's body for signs of illness) or maladaptive avoidance (e.g., avoiding doctors' appointments and hospitals), in the absence of somatic symptoms |
| Bodily Distress Disorder (ICD-11) | Distressing, persistent, and often multiple bodily symptoms and excessive attention directed toward the symptoms, which may be manifest by repeated contact with health care providers. Excessive attention is not alleviated by appropriate clinical examination and investigations and appropriate reassurance. |
| Illness Denial (DCPR-R) | Persistent denial of having a physical disorder and needing treatment (e.g., lack of compliance, delayed seeking of medical attention for serious and persistent symptoms, counterphobic behavior) as a reaction to the symptoms, signs, diagnosis, or medical treatment of a physical illness, despite the subject has been provided an adequate appraisal of the medical situation and management (if any) to be followed, with opportunity for discussion and clarification. |
| Cyberchondria | Unfounded escalation of concerns about common somatic symptoms based on repeated or compulsive online search. |
| Abnormal Illness Behavior | Abnormal ways whereby individuals respond to bodily indications, how they monitor internal states, define and interpret symptoms, make attributions, take remedial actions and utilize various sources of informal and formal care. It may be directed towards disease affirming (health anxiety, disease phobia) or disease denying (illness denial) |
| Disease conviction | A belief one has a serious illness from which one cannot be dissuaded by explanation of the unlikelihood of disease, lack of laboratory or physical examination findings consistent with disease, or negative testing. |
| Disease fear | The worry of developing serious illness, which leads to heightened distress when presented with any suggestion of the possibility of illness. |
| Bodily preoccupation | A heightened salience of physiologic functions, benign bodily sensations and sources of discomfort, and physical limitations. |
2. The perception of fear
A wide body of literature on affective neuroscience has shown wide evidence of the interdependence between mental and somatic functions to such an extent that they are conceived as the same thing even though experienced as the two sides of the same neural coin, according to the “dual-aspect monism” paradigm (Panksepp, 2005).
A clear-cut example of how fear can trigger human behavior was given several years ago (1984) by the psychoanalyst I. Matte Blanco. You can provoke an acute distressing reaction of high anxiety and fear in a relaxed Mr.X by injecting 1-mg adrenaline in his blood even if he was said it was just an isotonic saline solution. Conversely, if an unknown but well-dressed man rang his doorbell and gently said in an unknown language You are a traitor and have been condemned to death by our organization, Mr.X would remain calm and relaxed. Moreover, if the stranger at his door was dressed as a terrorist and harshly cried something in an unknown language, the reaction of Mr. X would have been the same as if triggered by an IV adrenaline injection. Thus, the same acute reaction of fear could actually be induced through a bottom-up (adrenaline) or an up-down (terrorist) pathway depending on the given situation, provided that Mr.X correctly interpreted the non-verbal meaning of his experience. The physical reaction of fear has a double complementary salience embedded in one single manifestation. One side of the coin mirrors emotions and involves the biological component of affect, that is the neuro-physiological and motor-expressive domain of the response mediated by the subcortical and limbic structures. Emotions are largely based on non-verbal clues and provide the organism with the physiological adjustments necessary to meet the environmental changes. This is what happens “in the theater of the body” (Damasio, 2003). Contrarily, the other side of the coin mirrors feelings, involving the psychological component of affect, that is the subjective cognitive-experiential domain of response mediated by the cortical structures. It is largely based on the symbolic function that enables past and current emotional experiences to be accessed and used for decision-making and interaction in the social world. This is what happens “in the theater of the mind” (Damasio, 2003). These two complementary and co-existing opposite poles may be however loosely coupled. Someone might show physiological and behavioral indications of fear or panic without much of the subjective component and vice versa.
Feelings are mental experiences that portray the state of internal organs and internal operations (milieu intérieur) which are mental experiences that go along with a change in the state of the body. Referring to the above example of Mr. X, an IV injection of adrenaline induces fear and anxiety as emotions stemming from homeostasis imbalance and prompting a behavior aimed at regulating aroused emotions (fight-flight or freezing response) within the so-called body loop (Damasio, 1999; Damasio & Carvalho, 2013). However, the same emotions and behaviors can be prompted by the meaning of the threatening image processed by the brain cortical areas and experienced as feelings within the downstreaming network (as-if body loop).
Emotions and feelings are two sides of the same coin and they do not undergo sequential, but parallel processing. According to W. Bucci’s (1997) Multiple Code Theory, feelings are processed in simultaneous multi-channel processes at different intertwingled levels of subsymbolic (spontaneous, unconscious emotions stemming from sensory, visceral, and kinesthetic sensations experienced during the states of emotional arousal), non-verbal symbolic (mental images that can be translated into words, even though they are not actually in the subject’s conscious awareness), and symbolic (translation of sensations and images into verbal and symbolic language) language . Briefly, fear is neither the somatic modification triggered by the emotion alone nor the conscious awareness of the menacing object alone, but it is both. We share the component fear with all the other mammals and, furthermore, each human being shares common (e.g., sharks or snakes) and individual images/objects of fear.
The main task of cognitive development for the mankind has been to learn how to meet our needs in order to maintain homeostasis, allowing our brain circuits to predict the best behavior in dangerous situations. Predators are pervasively harmful to animals, not to say that predators themselves can also be prey to other animals. It is not surprising that nervous system includes the predatory defense system as part of the adaptation equipment. Defense from predatory attacks is therefore a primary goal for most animals, including mammals and human beings. Defense from predators as a basic requirement for survival has some relevant consequences for humans. For example, we do not need to learn how to cope with harms and threats because we are born with the innate need to protect ourselves. Moreover, the way we are able to defend ourselves from external predatory attacks is hardwired in our subcortical neural circuits, so that the layout of our responses is pre-established, quite rigid, and shared with all the other species. If we focus on something that intrudes on the satisfaction of our needs, we behave aggressively and feel rage just as all the other animals do (fighting response). Similarly, if we perceive a situation as dangerous, we actually feel fear and need to escape from the predator (flighting response). In contrast with vertebrates, not only we have the emotional reaction but we feel also the somatic sensation. Moreover, and differently from mammals, we can also think about our feelings. Thereby we become aware of ourselves and we can try to make plans to anticipate dangers and improve our life. For this reason, even if we do not need to learn the how for meeting our needs because emotions are embedded within our cortico-thalamic network, we however need to learn what to fear in our life and how to cope with external and internal stimuli. By doing so, we manage to maintain biological homeostasis and psychological continuity, stability, and coherence, namely safety and identity (Solms, 2018).
During our evolution, we have become able to use our brain first to place our species at the top of the food chain, and second to protect our fellows and us from the external threats by erecting walls, buildings, prejudices, stigma, weapons, etc. Therefore, we are sensitive to threats, to their meaning (being harmed from something that makes me feel impotent), and most of all to those situations we feel out of our control (e.g. sharks but not mosquitos, planes but not cars). Sometimes we have to face a kind of threat that proves to be totally out of our control, unexpected, and difficult to locate and prevent. It may even be immune to our biological (immune system) and chemical (medicine) defenses, though it may be living inside us just as a virus. Therefore, fear is easily coupled with the worst terrifying memories we have experienced in our lives both as individuals (trauma, danger, pain, suffering) and as humans (plagues, starvation, war, death).
3. Fear and anxiety
Fear and anxiety surely overlap. Most of the subjective, physiological, and behavioral components of both feelings are quite identical. However, fear and anxiety are not exactly the same thing. Generally, the differences rely on locus of danger (external in fear, internal in anxiety), temporal focus (immediate present in fear, future in anxiety), and duration (strictly tied to danger exposure in fear, diffuse apprehension about possible danger in anxiety). Things are however more complex than this. In a co-authored paper, J. LeDoux, a leading authority in the field, clearly explains the relationship between fear and anxiety as parts of a defensive taxonomy (LeDoux & Daw, 2018) (table 2).
Table 2.
Taxonomy of behavioral and reactive defenses (adapted from LeDoux & Daw, 2018)
| Reactions and behaviors | Goal-directed | Implicit / Explicit | Example |
|---|---|---|---|
| Reflexes | No | Implicit | Startle |
| Fixed reaction patterns | No | Implicit | Freezing |
| Deliberate actions (implicit) | Yes | Implicit | Avoidance of possible harm by implicitly anticipating a potentially dangerous event |
| Deliberate actions (explicit) | Yes | Explicit | A conscious feeling of fear motivating a plan to scape from present harm or to avoid future harm |
Reflexes are common to all the species members as part of the species heritage. Reflexes are hardwired stimulus-response connections automatically and rapidly triggered by an innately programmed stimulus, e. g. when an insect flies close to my eye and I reflexively blink to protect the underlying tissues. One of the most studied reflexes in mammals is startle. Since the back of the body is outside of the visual field, startle reflexes may protect the organism from predatory attacks by shortening and stiffening muscles, therefore reducing exposure and making penetration more difficult. Similar to reflexes, fixed reaction patterns are innate and automatic behavioral responses and are common to all the members of a species. However, differently to reflexes, fixed reaction patterns are less directly related to stimulus and more to contextual clues, besides being slower in onset and involving complex patterns of coordinated responses. An example is found in the imminence of threat that shifts the aim of behavior from oriented to catch information from the environment, to detecting danger and prompting avoidance (e.g., freezing), and eventually preparing the organism to the fight/flight response. Deliberate actions may be either implicit (i.e., without conscious awareness but with coordinated goal-directed behavior) or explicit (i.e., with full awareness of procedures and goals). These behaviors are typically emitted (rather than elicited or triggered) in the presence of relevant stimuli and include the organism active involvement in deciding what to do when. One example is the active avoidance of possible harm when past experiences, implicit beliefs, interiorized self- and object-representations, learned behavior, schemas based on procedural memory, and memories of events contribute to shape behaviors such as hiding behind a shelter, explicitly planning social distancing or food catching during epidemics. In most animals, including humans, many interpersonal and personality factors may influence the cognitive processing of implicit and explicit deliberate actions. Explicit emotional regulation can be seen as a conscious effort for initiation and demands active emotional monitoring during the implementation. Thus, it is associated with some level of insight and awareness. The most commonly studied strategy of explicit regulation is reappraisal, which entails explicit alteration of the self-relevant meaning of an emotion-inducing stimulus. On the other hand, implicit emotional regulation is characterized by the absence of an explicit instruction, it is evoked automatically by the stimulus itself, runs to completion without conscious monitoring, and can happen without insight and awareness. A typical example of this type of regulation is the inhibition of fear (Etkin, Büchel, & Gross, 2015).
The clinical manifestations of illness perception shown in table 1 can be interpreted as complex forms of defense for self-protection in fearful situations as illnesses. Differently from other animals and partly different from mammals, humans do not just freeze in front of a bear but they actually feel fear. This is not because “we feel fear because we freeze”, as William James would say, but because we feel fear and freeze at the same time, because the feeling of fear and the freezing reaction are two sides of the same coin. Since they come together simultaneously, we do not realize they are not exactly the same, although we feel them as the same thing. However, according to LeDoux and Daw, they involve two different neural networks: one prompts for an immediate more ancient behavior developed to cope with the sources of threats and harms, while the other prompts for feelings of more recent evolutionary development that generates our awareness. Fear is the immediate sensation involving the downstreaming connections between amygdala, ventral tegmental area (VTA), the ‘reptilian’ areas in the brainstem as reticular ascending system (RAS) and the periaqueductal gray (PAG) triggering behavioral fixed reaction patterns. Fear is also the name of what we feel cognitively as a body sensation, i.e. it is the cognitive schema of fear we have in our mind. Fear also involves the upstreaming connections between amygdala, hippocampus (stored memories of similar situations we have experienced in the past), insula, cingulate cortex, and prefrontal cortex (PFC). In other words, the complex neural interactions not only contain a representation of the sentient self in the immediate moment, but also at each moment over a given period of time. It involves an automatic comparison of the present feelings with those occurred in the past and anticipated in the future, as well as the expectation of other people’s reactions towards me (Craig, 2002). Once the overall somatic and mental pattern is completed, it becomes the personal, unique schema of experience − the body image in my brain (Damasio, 1999).
Interestingly, in a recent fMRI study (Fung, Qi, Hassabis, Daw, & Mobbs, 2019) experimental subjects were exposed to virtual predator images and had to earn as much money as possible avoiding to be caught. Subjects showed difference in brain areas activity between the situation in which the virtual predator was distant (approach mode) and when it suddenly became very close (attack mode). When the predator was in the close attack mode, subjects showed the activation of the subcortical survival circuit (mainly, PAG), whereas when the predator was in the approach mode, they showed the activation of the cognitive circuit (mainly, amygdala, hippocampus, insula, ventral and medial PFC) but only if they scored high in a self-report scale of trait anxiety. This study showed the existence of a sort of hierarchy ranging from fear to anxiety and based on evolutionary demands: fear is an immediate automatic reaction triggered by survival needs, whereas anxiety requires sufficient time to activate behavioral control − particularly if the individual is prone to activate feelings of anxiety in cognitively processing threatening situations.
At the clinical level, there are also examples of a possible decoupling between fear and anxiety. Individuals with amygdala damage are not expected to feel fear. However, in a recent study (Feinstein, Buzza, Hurlemann, Follmer, Dahdaleh, Coryell, Welsh, Tranel, & Wemmie, 2013), three patients with bilateral amygdala damage due to a rare genetic disease were exposed to carbon dioxide inhalation and surprisingly showed a panic attack even if the neural base for feeling fear was damaged. One of them reported it was the first time he had experienced fear since his childhood. Two of those patients were also given isoproterenol (a rapidly acting peripheral β-adrenergic agonist akin to adrenaline) and a saline solution. Isoproterenol infusion induced anxiety in both patients and full-blown panic in one. Both patients showed signs of diminished awareness of cardiac sensation but the subject who did not panic reported a complete lack of awareness of dyspnea, providing further evidence that the amygdala is not required for the conscious experience of fear induced via interoceptive sensory channels (Khalsa, Feinstein, Li, Feusner, Adolphs, & Hurlemann, 2016). Fear can even be experienced if the bottom-up neural pathways are damaged (Damasio’s body loop) and feelings are prompted by top-down circuits (Damasio’s as-if body loop). Conversely, fear can also be experienced without being aware of the experience. Namely we are able to activate only the subcortical survival circuit of the complex behavioral response with no awareness of what we are feeling. It is reported that a patient with atrophic gastritis and H.pylori infection experienced a sudden attack of very severe gastric pain with no organic explanation by medical and instrumental check-ups. The psychological assessment outlined a picture of ‘non-fearful panic disorder’, characterized by all the clinical somatic manifestations of panic disorder without a conscious awareness of fear i.e. without fear of dying, ‘going crazy’, or losing control (Porcelli & DeCarne, 2008). The alexithymia construct is a deficit of the cognitive processing of feelings and affective regulation and may be considered an appropriate example of the disconnections between emotions and feelings (Luminet, Bagby, & Taylor, 2018). For example, patients with irritable bowel syndrome were assessed for alexithymia (that is, an implicit dimension of blindfeeling) and gastrointestinal-specific anxiety (GSA), that is an explicit form of anxiety due to the exposition to aversive gastrointestinal-related situations as eating certain food or going to certain locations in which bathroom facilities are not known or difficult to reach (Porcelli, DeCarne, & Leandro, 2014). Alexithymia, but not GSA, independently predicted illness severity by explaining 23% of its variance: the more the patients were less aware of their anxiety, the higher they perceived their intestinal symptoms. Conversely, their conscious awareness of anxious feelings about the illness was associated with higher symptom perception only if the individual alexithymic traits were involved in the process.
4. Fear, loneliness, and health-relatedconsequences
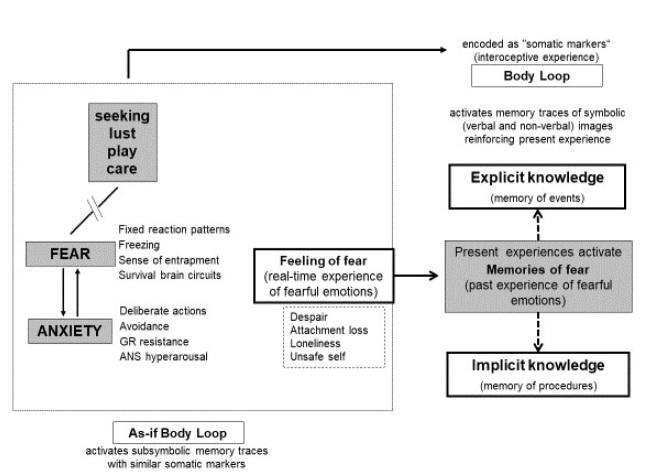
Although fear and anxiety overlap at a subjective level, they are generated by different neurobiological networks aimed at responding to different evolutionary demands. At the human level, evolutionary needs are experienced as feelings by the somatic markers in the brain (body loop). Anxiety implies the cognitive evaluation and control of the human behavior in facing challenging situations, whereas fear is related to the basic needs of survival threatened by immediate harm. The overall experience elicits explicit (events) and implicit (procedures) memories through the circuits reinforcing symbolically the present experience and activating acquired schemas of cognition and behaviors (as-if body loop).
The cognitive component of anxiety makes this feeling partly overlap with fear at the level of emotion, and partly independent for the different neurobiological and behavioral aspects. In Panksepp’s (1998) model, the brain networks involved in the fear system reciprocally reinforce each other with the separation-distress (or panic) system. Both have excitatory influence on the rage system and can be inhibited by other ‘positive’ systems as the seeking, lust, play, and care systems. At the subjective level, part of these modulating systems involves the real or representational presence of another person, indicating that the lack of social support can be highly problematic and even detrimental for effective emotional regulation. In fact, anxiety, fear, and panic trigger feelings of despair, hopelessness, helplessness, loneliness and lead individuals to feel unsafe.
One of the most stressful and dangerous consequences of a prolonged condition of interpersonal isolation is constituted by the combination of fear/ anxiety and loneliness. Unfortunately, this is a negative health complication due to the necessary social distancing remedy to pandemics. Social distancing is actually the best solution both for healthy people and for infected people hospitalized in ICU wards. Social media have been constantly reporting the experiences of physicians and nurses during this COVID-19 epidemic. They have to cure severely ill patients avoiding any direct physical contact and protected by white airtight suits, facial masks, eyeglasses, helmets, and caps making them dramatically look like warriors in a science fiction movie. Healthcare providers cannot take care of their patients by relying on the interpersonal warmth and trustful relation that is the standard psychological equipment in caregiving and, in addition to this, they report these hospitalized patients would need greater interpersonal attention, particularly if they are aware to be living a life-threatening critical clinical condition. Hopelessness, helplessness, and loneliness could maybe become the ‘normal’ distressing and negative feeling experience of both caregivers and patients. The lack of non-verbal communication, at both physical and prosodic level, can make the caring relationship ineffective because it is source of stress and frustration in itself (Porges, 2011). There is strong evidence that the effect of many pharmacological treatments, as analgesics, dramatically decrease if drugs are administered through a mechanical device when compared with drug administration by nurse or physician (e.g., Amanzio, Pollo, Maggi, & Benedetti, 2001). Loneliness and experiences of social isolation may have a detrimental effect also at the epigenetic level by shortening the telomere length and thus enhancing biological aging. A cohort of 101 male Israeli veterans formerly Prisoners-of-War who fought in the 1973 Yom Kippur War and fell captive on the Egyptian and Syrian fronts was approached 40 years later when they were 60 years-old or older (Stein, Levin, Lahav, Uziel, Abumock, & Solomon, 2018). Their UCLA Loneliness Scale score and the lack of social support after repatriation were both significantly and negatively associated with telomere length several decades later. Both factors uniquely contributed to the subsequent telomere length, even more and independently from the PTSD and the depressive symptoms. Loneliness and lack of perceived social support in early adulthood may therefore accelerate biological aging during the transition to the old age in a population that has faced severe stress as experienced by patients and healthcare providers in critical care units.
Nobody knows what the health consequences of COVID-19 pandemic will be, but a wide body of literature suggests a connection between severe stress (maybe further worsened by following economic crisis and increased unemployment) and serious health consequences. For example, stress may limit the response to vaccination. Studies from the laboratory of Anna Philips at the University of Birmingham, UK, reported poorer response to the vaccination for influenza in young healthy adults showing a high burden of stressful events over the past year (Phillips, Burns, Carroll, Ring, & Drayson, 2005), in older adults who experienced bereavement over the past year and had an unhappy marriage (Phillips, Carroll, Burns, Ring, Macleod, & Drayson, 2006), and in caregiving parents of children suffering from autism or Down syndrome (Gallagher, Phillips, Drayson, & Carroll, 2009). A wide epidemiologic survey in more than 140,000 general population subjects from Sweden, followed up to 27 years, compared individuals with a stress-related disorder (post-traumatic stress disorder, acute stress reaction, adjustment disorder, and other stress reactions) with siblings with a diagnosed stress-related disorder, and healthy individuals without such a diagnosis (Song, Fall, Fang, Erlendsdóttir, Lu, Mataix-Cols, Fernández de la Cruz, D’Onofrio, Lichtenstein, Gottfreðsson, Almqvist, & Valdimarsdóttir, 2019). People were young (the average age at diagnosis of stress-related disorder was 37 years) and the incidence of life-threatening infections was 3x1000 person-years. They had 50% increased risk of being severely infected compared with both the control groups, with the highest relative risk observed for meningitis and endocarditis. Younger age at diagnosis of a stress-related disorder and the occurrence of a psychiatric comorbidity − especially substance use disorders – increased the risk of infection. They also resulted to have 60% of increased risk for cardiovascular disease (CVD), particularly for heart failure (Song, Fang, Arnberg, Mataix-Cols, Fernández de la Cruz, Almqvist, Fall, Lichtenstein, Thorgeirsson, & Valdimarsdóttir, 2019). A recent study on 123,000 Swedish people showed that individuals with a stress-related disorder had up to 80% increased risk for vascular neurodegenerative disease, particularly Alzheimer (Song, Sieurin, Wirdefeldt, Pedersen, Almqvist, Larsson, Valdimarsdóttir, & Fang, 2020).
Psychological distress may have dramatic consequences also on lethal effects and mortality. An individual participant meta-analysis of 10 large prospective cohort studies from the Health Survey for England evaluated 68,222 people with mean age 55 years old, followed up for 8 years (Russ, Stamatakis, Hamer, Starr, Kivimäki, & Batty, 2012). It was found a clear dose-response association between mortality and the full range of psychological distress evaluated with the General Health Questionnaire-12 (GHQ-12) adjusted for all the co-factors (age, gender, social status, BMI, blood pressure, exercise, smoking, alcohol, and diabetes). The increased any-cause, cardiac-related, and even cancer-related mortality risk was 20% for subclinical symptoms (GHQ-12 score=1-3), 43% for moderate symptoms (score 4-6), and up to 94% for severe scores (scores 7-12). Direct effects were found for CV physiology alterations, HPA axis dysregulation, and inflammation markers as C-reactive protein (CRP), as well as indirect effects for lifestyle, physical inactivity, smoking. Moreover, the detrimental effect of psychological distress on mortality was amplified by a low socio-economic status (SES). People included in higher SES categories – who might have better coping strategies and larger support networks together with greater biobehavioral and economic resources for dealing with adversity – had lower mortality rates even when they reported high levels of psychological distress (Lazzarino, Hamer, Stamatakis, & Steptoe, 2013).
It is likely that one of the most important underlying mechanisms connecting stress and health negative effects is the strict connection between psychological factors and the immune system. Particularly, wide evidence was found in depression (e.g., Read, Sharpe, Modini, & Dear, 2017; Lee, Stockings, Harris, Doi, Page, Davidson, & Barendregt, 2019), mostly as depression proves to be one the main research focuses both in psychology and psychiatry. Depression was declared a leading cause of disability by WHO and it is a major contributor to the overall global burden of diseases (GBD 2017 Disease and Injury Incidence and Prevalence Collaborators, 2018). For instance, a cohort study of 808 Dutch patients with current diagnosis of depression was assessed for depressive symptoms, BMI, metabolic syndrome, CRP, IL-6, and TNF-α (Lamers, Milaneschi, de Jonge, Giltay, & Penninx, 2018). The results were quite clear and the authors called for a new diagnostic category of immune-metabolic depression that integrated atypical depressive symptoms and atypical increased appetite. Atypical increased appetite in atypical depression could be the result of a combination of high distress, defective psychological and interpersonal resources, and frustration leading to a disturbance on reward perception that is regulated by the mesolimbic reward centers (see figure 1). Eating palatable foods (high in sugar and fat) trigger neuroadaptive responses (via dopamine D2 receptors) in the same brain regions related to reward and pleasure that are active in drug addiction. Increased food intake as response to a stressful event can be indeed interpreted as a compensatory form of self-medication. As a result, in this study obesity and inflammation were found to go hand in hand, as the production of cytokines in adipose tissue such as TNF-α and IL-6, giving rise to a pro-inflammatory state in obesity. Further evidence of the close association between depression, immune system, and morbidity is nowadays largely confirmed by several well-conduced longitudinal studies using large samples of clinical and non-clinical subjects, even considering healthy individual from the general population that had no somatic or psychiatric disorders at the time of assessment. These findings are particularly relevant for shedding light on a prospective risk for people who are not currently ill, but are experiencing high psychological distress during this epidemic. Consistent results have been evidenced by several longitudinal surveys carried out among the general population worldwide with long-term follow-ups up to 20 years. For instance, a Dutch survey has found a significantly higher annual incidence of somatic diseases (37%), particularly CVD, pain, and GI disorders. They also showed a dose-response relation between depressive symptoms and disease incidence (Gaspersz, Lamers, Beekman, van Hemert, Schoevers, Penninx, 2018). An Australian study showed that women who developed depressive symptoms during a period of high difficulty (difficulty in managing on their available income, overweight or obesity, low physical activity, drinking, and smoking) had 80% increased risk of developing common chronic diseases as hypertension, diabetes, heart disease, stroke, cancer, asthma, chronic obstructive pulmonary disease, arthritis, and osteoporosis (Xu, Mishra, & Jones, 2019).
Figure 1.
Schematic model of factors involved in fear and anxiety
As stated previously, fear/anxiety and social isolation trigger each other, leading to even higher arousing perceived distress due to the poor neural inhibiting effect of the caring system and to the high psychological effect of perceived loneliness defined as the poor quality of social and emotional support available to individuals (Barger, 2013). Beyond quite obvious relationships with psychosocial outcomes (increased psychopathology, lower subjective wellbeing, higher hypervigilance for interpersonal threats, or reduced executive functioning), social support and sense of loneliness have been shown to have a significant and clinically harmful association with several medical outcomes. They actually increase brain glucocorticoid receptor sensitivity, pro-inflammatory activity, and blood pression, lower immune defenses, and heighten the rates of metabolic syndromes, the risk of cognitive decline, dementia, and even mortality (Holt-Lunstad, Smith, & Layton, 2010; Jacob, Haro, & Koyanagi, 2019). Moreover, a recent US survey among primary care patients showed that perceived loneliness was significantly associated with the number of days in illness, medical visits including emergency, and hospitalizations, though this association was particularly stronger in adolescents than in elderly (Mullen, Tong, Sabo, Liaw, Marshall, Nease, Krist, & Frey, 2019). This finding may suggest that perceived loneliness may play a major role in socially isolated adolescents because of their lower personal resources for dealing with self-esteem issues compared with older individuals. The burden of loneliness on younger people was further confirmed by another recent survey investigating the association with chronic medical multimorbidity in more than 7,000 UK subjects (Stickley & Koyanagi, 2018). The risk of having chronic multimorbid diseases increased in a dose-response relationship with scores to a self-report questionnaire on perceived loneliness, but the associations were stronger across all the levels of disease (from 1 to 5+ diseases in the youngest age group). Once again, this finding may outline higher difficulty for younger people in adjusting to circumstances where their sense of unsafety is reinforced by lower self-esteem, impoverishment of interpersonal relationships, and vulnerability to disease.
5. Conclusion
According to affective neuroscience and neuropsychoanalysis, we can feel emotions because in humans the function of consciousness works as the biological function of emotion at the elementary level of animal life (Solms, 2015). At the most elementary level, emotion is ‘felt’ on a rudimentary scale from pleasurable (enhancing your chances of surviving and reproducing) to unpleasurable (limiting your chances and detecting threats). Feeling is the cognitive awareness of feeling that motivates you to do things that are biologically good for you and to avoid things that are biologically bad. The world is more complex than just ‘good’ vs ‘bad’, so that more complex and subtle forms of emotion evolved to give subtler responses than just ‘approach’ or ‘withdraw’.
Fear and anxiety perfectly fit with this view and are normal reactions to fostering adaptation. Though their manifestations largely overlap, they perform two different functions within the defensive taxonomy. Fear is a fixed emotional reaction triggered by immediate danger that activates subcortical circuits prompting feelings, thoughts, and behaviors aimed to preserve survival. Contrarily, anxiety is a cognitive processing of fear linked to the activity of cortical areas allowing decision and control. This is the reason why we can create our objects of fear only within our mind and different forms of anxiety are related to the body (e.g., body dysmorphic disorder and anorexia nervosa) and illness representations, as those shown in Tab. 1.
The worldwide crisis generated by the COVID-19 pandemic is an obvious source of fear for everyone and behavioral responses can range from denial (dangerously claimed also by some of state leaders) to true panic attacks. After the period of acute crisis, the national healthcare systems will be maybe facing another big deal, specifically the psychiatric and medical consequences of the negative distressing feelings that people are actually living. Along with this, the current impairment of social relationships and increased feelings of loneliness can be dramatic for specific individuals as well as for both severe patients and health professional working in ICU units experiencing extreme forms of helplessness.
Fear and anxiety are necessary to defend the integrity and the unity of our self. However, as decades of clinical research on PTSD has taught us, trauma and other forms of intense stress may be the source of danger for our mental health as well as of vulnerability to morbidity and mortality. Kendler recently wrote that psychiatry has tried to mimic biological medicine in the latter half of the 20th century by searching monocausal theories of psychopathology. However, in these same years “Western medicine and medical epidemiology moved from a focus on monocausal infectious diseases to the multifactorial chronic disease model. In the late 20th century, it would have been more accurate for psychiatry to claim that we treated ‘real’ disorders because they were multicausal, similar to coronary artery disease, hypertension, rheumatoid arthritis, and type 2 diabetes, not that they were monocausal, such as classic infectious or mendelian medical disorders” (Kendler, 2019, p.1089). This is particularly true today. We need full efforts not only by psychologists but also by physicians and psychiatrists to integrate clinical psychology, medicine, and psychiatry within a larger biopsychosocial framework to the benefit of the general health condition. We definitely need to take this step forward in order to face the likely consequences of this acute epidemic.
Acknowledgements
The author thanks Dr. Marzia Iasenza for helping with the English translation.
References
- Amanzio, M., Pollo, A., Maggi, G., & Benedetti, F. (2001). Response Variability to Analgesics: A Role for Non-Specific Activation of Endogenous Opioids. Pain, 90, 205-215. 10.1016/s0304-3959(00)00486-3 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association Publishing. [Google Scholar]
- Barger, S.D. (2013). Social Integration, Social Support and Mortality in the US National Health Interview Survey. Psychosomatic Medicine, 75, 510-517. 10.1097/PSY.0b013e318292ad99 [DOI] [PubMed] [Google Scholar]
- Bucci. W. (1997). Psychoanalysis and Cognitive Science: A Multiple Code Theory
- Bureau of Aircraft Accidents. (2019). Retrieved April 13, 2020 from https://www.baaa-acro.com/statistics/death-rate-per-year. [Google Scholar]
- Craig, A.D. (2002). How Do You Feel? Interoception: The Sense of the Physiological Condition of The Body. Nature Reviews Neuroscience, 3, 655-666. 10.1038/nrn894 [DOI] [PubMed] [Google Scholar]
- Damasio, A. (1999). The Feeling of What Happens: Body and Emotion in the Making of Consciousness. New York: Harcourt Brace. [Google Scholar]
- Damasio, A. (2003). Looking for Spinoza. London: William Heinemann. [Google Scholar]
- Damasio, A. (2018). The Strange Order of Things. Life, Feeling, and the Making of Cultures. New York: Pantheon Books. [Google Scholar]
- Damasio, A., & Carvalho, G.B. (2013). The nature of feelings: evolutionary and neurobiological origins. Nature Reviews Neuroscience, 14, 143-152. 10.1038/nrn3403 [DOI] [PubMed] [Google Scholar]
- Etkin, A., Büchel, C., & Gross, J.J. (2015). The Neural Bases of Emotion Regulation. Nature Reviews Neuroscience, 16, 693-700. 10.1038/nrn4044 [DOI] [PubMed] [Google Scholar]
- Feinstein, J.S., Buzza, C., Hurlemann, R., Follmer, R.L., Dahdaleh, N.S., Coryell, W.H., Welsh, M.J., Tranel, D., & Wemmie, J.A. (2013). Fear and Panic in Humans With Bilateral Amygdala Damage. Nature Neuroscience, 16, 270-272. 10.1038/nn.3323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fung, B.J., Qi, S., Hassabis, D., Daw, N., & Mobbs, D. (2019). Slow Escape Decisions Are Swayed by Trait Anxiety. Nature Human Behaviour, 3, 702-708. 10.1038/s41562-019-0595-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallagher, S., Phillips, A.C., Drayson, M.T., & Carroll, D. (2009). Caregiving for Children With Developmental Disabilities is Associated with A Poor Antibody Response to Influenza Vaccination. Psychosomatic Medicine, 71, 341-344. 10.1097/PSY.0b013e31819d1910 [DOI] [PubMed] [Google Scholar]
- Gaspersz, R., Lamers, F., Beekman, A.T.F., van Hemert, A.M., Schoevers, R.A., Penninx, B.W.J.H. (2018). The Impact of Depressive Disorder Symptoms and Subtypes on 6-Year Incidence of Somatic Diseases. Psychotherapy and Psychosomatics, 87, 308-310. 10.1159/000491933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. (2018). Global, Regional, and National Incidence, Prevalence, and Years Lived With Disability for 354 Diseases and Injuries for 195 Countries And Territories, 1990-2017: A Systematic Analysis for the Global Burden of Disease Study 2017. Lancet, 392, 1789-1858. 10.1016/S0140-6736(18)32279-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad, J., Smith, T.B., & Layton, J.B. (2010). Social Relationships and Mortality Risk: A Meta-Analytic Review. PLoS Medicine, 7, e1000316. 10.1371/journal.pmed.1000316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inter-Agency Standing Committee (IASC). (2020). Addressing Mental Health and Psychosocial Aspects of COVID-19 Outbreak, February 2020. Retrieved April 8, 2020 from https://interagencystandingcommittee.org/iasc-reference-group-mental-health-and-psychosocial-support-emergency-settings/interim-briefing
- International Shark Attack File. (2017). Retrieved April 13, 2020 from https://www.floridamuseum.ufl.edu/shark-attacks. [Google Scholar]
- Jacob, L., Haro, J.M., & Koyanagi, A. (2019). Relationship Between Living Alone and Common Mental Disorders in the 1993, 2000 and 2007 National Psychiatric Morbidity Surveys. PLoS One, 14, e0215182. 10.1371/journal.pone.0215182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler, K.S. (2019). From Many to One to Many-the Search for Causes of Psychiatric Illness. JAMA Psychiatry, 76: 1085-1091. 10.1001/jamapsychiatry.2019.1200 [DOI] [PubMed] [Google Scholar]
- Khalsa, S.S., Feinstein, J.S., Li, W., Feusner, J.D., Adolphs, R., & Hurlemann, R. (2016). Panic Anxiety in Humans with Bilateral Amygdala Lesions: Pharmacological Induction via Cardiorespiratory Interoceptive Pathways. Journal of Neuroscience, 36: 3559-3566. 10.1523/JNEUROSCI.4109-15.2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamers, F., Milaneschi, Y., de Jonge, P., Giltay, E.J., & Penninx, B.W.J.H. (2018). Metabolic and Inflammatory Markers: Associations with Individual Depressive Symptoms. Psychological Medicine, 48, 1102-1110. 10.1017/S0033291717002483 [DOI] [PubMed] [Google Scholar]
- Lazzarino, A.I., Hamer, M., Stamatakis, E., & Steptoe, A. (2013). The Combined Association of Psychological Distress and Socioeconomic Status with All-Cause Mortality: A National Cohort Study. JAMA International Medicine, 173, 22-27. 10.1001/2013.jamainternmed.951 [DOI] [PubMed] [Google Scholar]
- LeDoux, J., E Daw, N.D. (2018). Surviving Threats: Neural Circuit and Computational Implications of A New Taxonomy of Defensive Behaviour. Nature Reviews Neuroscience, 19, 269-282. 10.1038/nrn.2018.22 [DOI] [PubMed] [Google Scholar]
- Lee, Y.Y., Stockings, E.A., Harris, M.G., Doi, S.A.R., Page, I.S., Davidson, S.K., & Barendregt, J.J. (2019). The Risk of Developing Major Depression Among Individuals with Subthreshold Depression: A Systematic Review and Meta-Analysis of Longitudinal Cohort Studies. Psychological Medicine, 49, 92-102. 10.1017/S0033291718000557 [DOI] [PubMed] [Google Scholar]
- Luminet, O., Bagby, R. M., & Taylor, G. J. (Eds.) (2018). Alexithymia: Advances in research, theory, and clinical practice. Cambridge, UK: Cambridge University Press. 10.1017/9781108241595 [DOI] [Google Scholar]
- Matte Blanco, I. (1984), Concetti basilari per una medicina psicosomatica [Basic concepts of psychosomatic medicine]. In Pancheri P. (Ed.), Trattato di medicina psicosomatica [Psychosomatic Medicine Treatise] (pp.3-21). Florence: USES. [Google Scholar]
- Mullen, R.A., Tong, S., Sabo, R.T., Liaw, W.R., Marshall, J., Nease, D.E., Krist, A.H., & Frey, J.J. (2019). Loneliness in Primary Care Patients: A Prevalence Study. Annals of Family Medicine, 17, 108-115. 10.1370/afm.2358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panksepp, J. (1998). Affective Neuroscience: The Foundations of Human and Animal Emotions. New York: Oxford University Press. [Google Scholar]
- Panksepp, J. (2005). Affective Consciousness: Core Emotional Feelings in Animals and Humans. Consciousness and Cognition, 14, 30-80. 10.1016/j.concog.2004.10.004 [DOI] [PubMed] [Google Scholar]
- Phillips, A.C., Burns, V.E., Carroll, D., Ring, C., & Drayson, M. (2005). The Association Between Life Events, Social Support, and Antibody Status Following Thymus-Dependent and Thymus-Independent Vaccinations in Healthy Young Adults. Brain Behavior and Immunity, 19, 325-333. 10.1016/j.bbi.2004.10.004 [DOI] [PubMed] [Google Scholar]
- Phillips, A.C., Carroll, D., Burns, V.E., Ring, C., Macleod, J., & Drayson, M. (2006). Bereavement and Marriage are Associated with Antibody Response to Influenza Vaccination in the Elderly. Brain Behavior and Immunity, 20, 279-289. 10.1016/j.bbi.2005.08.003 [DOI] [PubMed] [Google Scholar]
- Porcelli, P., & DeCarne, M. (2008). Non-Fearful Panic Disorder in Gastroenterology. Psychosomatics, 49, 543-545. 10.1176/appi.psy.49.6.543 [DOI] [PubMed] [Google Scholar]
- Porcelli, P., DeCarne, M., & Leandro, G. (2014). Alexithymia and Gastrointestinal-Specific Anxiety in Moderate to Severe Irritable Bowel Syndrome. Comprehensive Psychiatry, 55, 1647-1653. 10.1016/j.comppsych.2014.05.022 [DOI] [PubMed] [Google Scholar]
- Porcelli, P., & Guidi, J. (2015). The clinical utility of the Diagnostic Criteria for Psychosomatic Research (DCPR): a review of studies. Psychotherapy and Psychosomatics, 84, 265-72. 10.1159/000430788 [DOI] [PubMed] [Google Scholar]
- Porges, S.W. (2011). The Polyvagal Theory: Neurophysiological Foundations of Emotions, Attachment, Communication, and Self-Regulation. New York: Norton & Co. [Google Scholar]
- Read, J.R., Sharpe, L., Modini, M., & Dear, B.F. (2017). Multimorbidity and depression: A systematic review and meta-analysis. Journal of Affective Disorders, 221, 36-46. 10.1016/j.jad.2017.06.009 [DOI] [PubMed] [Google Scholar]
- Russ, T.C., Stamatakis, E., Hamer, M., Starr, J.M., Kivimäki, M., & Batty, G.D. (2012). Association between Psychological Distress and Mortality: Individual Participant Pooled Analysis of 10 Prospective Cohort Studies. British Medical Journal, 345, e4933. 10.1136/bmj.e4933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith, R., Weihs, K.L., Alkozei, A., Killgore, W.D.S., & Lane, R.D. (2019). An Embodied Neurocomputational Framework for Organically Integrating Biopsychosocial Processes: An Application to the Role of Social Support in Health and Disease. Psychosomatic Medicine, 81, 125-145. 10.1097/PSY.0000000000000661 [DOI] [PubMed] [Google Scholar]
- Solms, M. (2015) The Feeling Brain: Selected Papers on Neuropsychoanalys. London: Karnac Books. [Google Scholar]
- Solms, M. (2018). The scientific standing of psychoanalysis. British Journal of Psychiatry International, 15, 5-8. 10.1192/bji.2017.4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song, H., Fang, F., Arnberg, F.K., Mataix-Cols, D., Fernández de la Cruz, L., Almqvist, C., Fall, K., Lichtenstein, P., Thorgeirsson, G., & Valdimarsdóttir, U.A. (2019). Stress Related Disorders and Risk of Cardiovascular Disease: Population Based, Sibling Controlled Cohort Study. British Medical Journal, 365, 11255. 10.1136/bmj.l1255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song, H., Fall, K., Fang, F., Erlendsdóttir, H., Lu, D., Mataix-Cols, D., Fernández de la Cruz, L., D’Onofrio, B.M., Lichtenstein, P., Gottfreðsson, M., Almqvist, C., & Valdimarsdóttir, U.A. (2019). Stress Related Disorders and Subsequent Risk of Life Threatening Infections: Population Based Sibling Controlled Cohort Study. British Medical Journal, 367, 15784. 10.1136/bmj.l5784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song, H., Sieurin, J., Wirdefeldt, K., Pedersen, N.L., Almqvist, C., Larsson, H., Valdimarsdóttir, U.A., & Fang, F. (2020). Association of Stress-Related Disorders with Subsequent Neurodegenerative Diseases. JAMA Neurology (in press). 10.1001/jamaneurol.2020.0117 [DOI] [PMC free article] [PubMed]
- Stein, J.Y., Levin, Y., Lahav, Y., Uziel, O., Abumock, H., & Solomon, Z. (2018). Perceived Social Support, Loneliness, and Later Life Telomere Length Following Wartime Captivity. Health Psychology, 37, 1067-1076. 10.1037/hea0000669 [DOI] [PubMed] [Google Scholar]
- Stickley, A., & Koyanagi, A. (2018). Physical Multimorbidity and Loneliness: A Population-Based Study. PLoS One, 13(1):e0191651. 10.1371/journal.pone.0191651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van den Bergh, O., Witthöft, M., Petersen, S., & Brown, R.J. (2017). Symptoms and the Body: Taking the Inferential Leap. Neuroscience and Biobehavioral Reviews, 74(Pt A), 185-203. 10.1016/j.neubiorev.2017.01.015 [DOI] [PubMed] [Google Scholar]
- Xu, X., Mishra, G. D., & Jones, M. (2019). Depressive symptoms and the development and progression of physical multimorbidity in a national cohort of Australian women. Health Psychology, 38, 812–821. 10.1037/hea0000738 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2018). International Classification of Diseases, 11th Revision. Geneve: World Health Organization. [Google Scholar]
- World Health Organization. (2017). Global Health Observatory. Road Traffic Deaths. Retrieved April 13, 2020 from https://www.who.int/gho/road_safety/mortality.
- World Health Organization. (2020). Vector-borne diseases. Retrieved April 13, 2020 from https://www.who.int/en/news-room/fact-sheets/detail/vector-borne-diseases.