Abstract
In this article, we argue that fear experiences during the COVID-19 pandemic are organized on the psychological level around four interrelated dialectical domains, namely (1) fear of the body/fear for the body, (2) fear of significant others/fear for significant others, (3) fear of not knowing/fear of knowing, and (4) fear of taking action/fear of inaction. These domains represent the bodily, interpersonal, cognitive, and behavioural features of fear, respectively. We propose ways of addressing these fears and minimising their impact by improving appraisal of the body, fostering attachment security, improving emotion regulation, adopting acceptance and promoting responsibility.
Keywords: COVID-19, coronavirus, fear, body, relationships, emotion regulation
The coronavirus pandemic poses a huge challenge to the society because it tests its ability to cope with a multifarious threat under the constraints of the situation. Political actions are taken in the realm of health management, public security, financial economics, protection of assets and production of goods. Although important, psychological health is probably the most neglected aspect of the COVID-19 pandemic. It is not an immediately visible part of the global picture of this disaster, but the negative psychological impact of the pandemic and measures taken in response to the pandemic is well known (Brooks et al., 2020; Morganstein, Fullerton, Ursano, & Holloway, 2017).
Crucially, the resilience of a society facing such a catastrophic event also depends on how its individual members cope with their anxiety and fears. Widespread fears of aloneness, contagion and death affect our sense of agency, relatedness and the way we behave, in addition to restrictions imposed by governments. Coping with these fears is thus critical on the individual level, and effective coping can also help the society to better manage the pandemic.
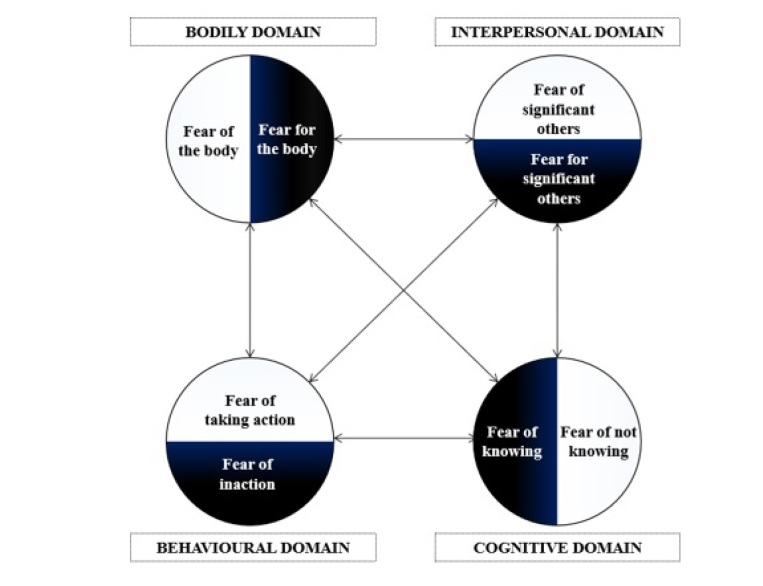
Fear is a basic emotion that is activated in response to perceived threat. In the current article, we propose that fear during the COVID-19 pandemic is organized on the psychological level around four interrelated dialectical domains. These domains of fear are (1) fear of the body/fear for the body, (2) fear of significant others/fear for significant others, (3) fear of not knowing/fear of knowing and (4) fear of taking action/fear of inaction, and they represent the bodily, interpersonal, cognitive, and behavioural features of fear, respectively. We contend that the four domains of fear observed during the COVID-19 pandemic reflect the main psychological means of grasping the reality. Moreover, we propose a dialectical structure of the identified fears, whereby each aspect of a fear domain may coexist with its counterpart (the apparent opposite) and may relate to the aspects of other fear domains. Thus, fear domains and their aspects are not organised in a hierarchical manner and represent “ingredients” of the complex experience of fear during the pandemic.
Figure 1 provides a graphical representation of the domains of fears and their reciprocal interactions. These “four horsemen of fear” are discussed in more detail in the next section.
Figure 1.
The “four horsemen” of fear (the four domains of fear) during the COVID-19 pandemic. Each fear domain consists of the two seemingly opposite aspects
The four horsemen of fear during the COVID pandemic
The first domain of fear (fear of the body/fear for the body) concerns the body and its signals. The body is the first organizer of our human experience (Stern, 1985) and it “keeps the score” (van der Kolk, 2015) of events that threaten our physical and psychological integrity. In the current experience of the COVID-19 pandemic, fear of the body relates to a sense of physical vulnerability due to which the body is a potential source of danger and cannot be trusted (Starcevic, 2005). Such perception of one’s body is linked with a fear of “body betrayal” via infection, which ultimately leads to death. This fear of the body manifests itself in different ways in the setting of the COVID-19 pandemic. People typically become hypervigilant about any bodily changes that might suggest the COVID-19 infection, fearfully anticipating their surrender to it. The other body-related fear (fear for the body) pertains to a need to protect the body. In this type of fear, body is not perceived as a threat, but as a treasure that may be lost; hence, body is valued for survival and needs to be cared for. The fear of the body and the fear for the body can alternate very quickly, generating inconsistent and potentially body-damaging behaviours. For example, Italian news recently reported that many people who survived a heart attack preferred to stay at home than to go to the hospital for the fear of being infected (la Repubblica, 2020). Thus, fear of the body and a need to protect it may be so intertwined that the underlying estimates of threat (risk of dying from a repeated heart attack or its complications versus risk of becoming infected with COVID-19 and dying from it) may be biased and result in a behaviour that ultimately does not protect the body.
The second domain of fear (fear of significant others/fear for significant others) relates to important interpersonal relationships. As Aristotle said in his Politics (Lord, 2003), human beings are by nature “social animals”. Interpersonal relationships are at the core of human identity, especially those involving attachment figures such as parents, offspring and people with whom we have romantic relationships. These individuals provide us with a safe haven and a secure base (Bowlby, 1988) from which we feel comfortable to explore our internal experience and the external world. The COVID-19 pandemic has affected our perception of close interpersonal relationships with the recommendations surrounding “social distancing”. We are told by the authorities that maintaining a physical distance even from people to whom we are attached will slow down the spread of the coronavirus and keep everyone safe. The consequence of this is a perception that even the loved ones might harm us or kill us, although unwittingly. Therefore, instead of providing protection or a sense of safety, a parent, a child or an intimate partner becomes a potential threat, with our survival possibly depending on protecting ourselves against people with whom we have the strongest affective bonds. Conversely, we experience ourselves as being potentially dangerous to our loved ones and responsible if they become infected. We are thereby deprived of our normal role to care for them or protect them. These changes have profound consequences not only in terms of how we relate to the significant others, but also in terms of further undermining our sense of safety and our need to “be there” for our loved ones.
The third domain of fear (fear of not knowing/fear of knowing) concerns the cognitive aspect of mastering the situations. In the context of the current COVID-19 pandemic, knowledge about the pandemic is bounded and partial, which is deeply unsettling. One way of coping with this situation is using the availability heuristic (Tversky & Kahneman, 1973), that is, relying on information that can be recalled, usually information to which the person was exposed very recently. This leads to a biased reasoning, whereby “things” that are recalled have a greater value for understanding than those that cannot be recalled readily. Biases in reasoning such as the availability heuristic may paradoxically give a person some sense of understanding or control, but they act as a defence against a profound confusion as to what one should know or needs to know about the pandemic as opposed to what is better left unknown. The information is never “neutral” and a careful balancing act between useful and survival-promoting information and frightening and paralysing information may be difficult to achieve. For example, we may both want to know and avoid knowing how many people have been infected in our local community. While this type of information may help some people cope better, others may find it overwhelming and would rather be left “in the dark”. What is most confusing, as with other types of fear described in the context of the COVID-19 pandemic, is a quick alternation of a need to know (fear of not knowing) and a need not to know (fear of knowing); such an alternation is likely to interfere with decision making and related actions. For example, frantic searching for COVID-19-related information online may increase anxiety and distress and thus lead to cyberchondria (Starcevic, 2017); at the same time, important and even survival-promoting information may be overlooked or missed due to a fear of knowing. The result can be a paralysing inaction alternating with risk-taking behaviour.
The fourth domain of fear (fear of taking action/fear of inaction) concerns behavioural consequences of fear during the COVID-19 pandemic. Our lives also consist of actions, that is, intentional and purposeful activities that are not reflexive, but are subjectively meaningful (Davidson, 1980). As already noted, fears in the bodily, interpersonal and cognitive domains often have a direct impact on the behaviour. This is especially the case when the “mutually opposing” fears alternate quickly, producing indecisiveness and paralysing action. For example, it may be very difficult to decide whether to visit one’s elderly parents because of the possibility of infecting them; such a person is torn between a duty to care for parents and responsibility for keeping them safe by avoiding such visits. In some vulnerable individuals, a fear of taking action may manifest itself in obsessive doubts about doing simple things, such as buying groceries or opening a package sent from a parent living in a heavily contaminated area. The other “side of the coin” in this fear domain relates to people who have a strong need to take some action and who may be afraid of being passive or of being perceived as such. This may explain the behaviour of individuals who became hyperactive on social networking sites only during the COVID-19 pandemic. Such individuals spend most of the time online, going live on webcams, publishing their own pictures or videos or posting news related to the pandemic. In addition to alleviating these individuals’ fear of inaction and of being invisible in the world of the social media, such behaviour may satisfy their narcissistic needs (Gnambs & Appel, 2018) and/or a need for belonging to a group that might provide a sense of security. However, this behavioural pattern may also reflect the problematic use of social networking sites or apps which may have addictive aspects that are difficult to attenuate and could require clinical intervention.
Managing fear domains
Conquering pathological fear in the context of the COVID-19 pandemic requires measures that are relatively simple, as well as those that are more complex and are best implemented in collaboration with a mental health professional. Considering a need to maintain social distance, psychoeducation and psychological treatment delivered remotely via communication technologies can provide individuals with appropriate support (Sucala, Schnur, Constantino, Miller, Brackman, & Montgomery, 2012) and improve their quality of life (Lange, van de Ven, & Schrieken, 2003).
In fact, improving psychological health of individuals is vital for strengthening the resilience of the society as a whole. We argue here that this objective could be achieved by applying the following measures: (a) improving appraisal of the body, (b) fostering attachment security, (c) improving emotion regulation, (d) adopting acceptance and (e) promoting responsibility.
Brief descriptions of interventions that can be delivered to address fears in the context of the coronavirus pandemic are provided below. Considering that there is no substitute for a tailored clinical evaluation and individualized therapeutic approaches (Gazzillo, Schimmenti, Formica, Simonelli, & Salvatore, 2017), our aim is to list and discuss procedures and techniques that can be integrated into traditional (offline) psychotherapeutic interventions. Importantly, these approaches can also be used within a framework of online or phone-mediated psychological interventions, and some can serve as stand-alone measures for people experiencing fear and related psychological difficulties but are not undergoing any psychological intervention (i.e., probably the majority of people with such emotional problems during the COVID-19 pandemic).
Improving appraisal of the body
It is crucial for people in the midst of a pandemic to be able to accurately appraise the physiological signals of their bodies and to neither underestimate nor overestimate their susceptibility to infections and the associated physical threat. Most people find useful physical and mental exercises that increase the feelings of safety and control over the body, such as improving posture (Weineck, Messner, Hauke, & Pollatos, 2019), tracking the body autonomic response (Porges & Dana, 2018) and practicing mindfulness (Gibson, 2019). People who are severely anxious about their health or develop a full-blown hypochondriasis may need further psychological treatment that specifically addresses their bodily concerns (Bouman, 2014); sometimes, this approach can be accompanied by antidepressants (Harding & Fallon, 2014).
Fostering attachment security
Developing secure attachments is likely to improve coping with the fear of the significant others and fear for the significant others. Secure attachment has been linked with the positive quality of interpersonal interactions (including interactions with strangers; Roisman, 2006) and with a capacity for effective self-regulation and top-down control (Pallini, Chirumbolo, Morelli, Baiocco, Laghi, & Eisenberg, 2018). Attachment security can be fostered in the family and in other relationships via mutually constructive communication (Domingue & Mollen, 2009) that involves synchronous interactions (e.g., by phone, if the communication partner is not present; Gentzler, Oberhauser, Westerman, & Nadorff, 2011). When problematic relationships in the context of the fears of COVID-19 call for a clinical intervention, improving the capacity to represent and mentalize the internal states and the interpersonal motivations of the significant others may be critical for both adults (Allen & Fonagy, 2006) and children (Midgley, Ensink, Linqvist, Malberg, & Muller, 2017). Also, it is important to assess the quality of the attachment relationships, identify the problems in these relationships and address any internal conflicts that may surround the problems (Lemma, Target, Fonagy, 2011). This should make a tailored intervention to interpersonal fears possible.
Improving emotion regulation
Improving emotion regulation is central for better coping in relation to fears of knowing and not knowing. An adequate emotion regulation fosters the identification, monitoring and modification of emotional reactions and makes it possible to tolerate distress inherent in conflictual and complex situations (Koole, 2009). There is evidence that a limited access to adaptive emotion regulation strategies may contribute to more severe psychopathologies characterised by affect dysregulation and behavioural dyscontrol (Schimmenti, Santoro, La Marca, Costanzo, & Gervasi, 2019). Adaptive forms of emotion regulation include a constructive reevaluation of the events and restructuring of beliefs that play a key role in the development or maintenance of various psychopathological manifestations. In contrast, maladaptive strategies encompass a suppression of emotion, dramatization, blaming oneself or others, abstract rumination, excessive reassurance seeking or use of alcohol or psychotropic drugs (Philippot, 2013; Watkins, 2016). Promoting and learning effective emotion regulation strategies will help the individual entrapped in the fear of knowing/fear of not knowing better cope with the negative affect related to the pandemic, also reducing the risk of activating primitive defence mechanisms, such as denial or acting out and exclusive use of emotion-based coping.
Adopting acceptance
One way of addressing fears of taking or not taking action is through acceptance, which refers to the adoption of an open, receptive, and flexible attitude with respect to experience (Stewart, 2014). Acceptance allows the individual to recognize and acknowledge the reality of a current scenario, condition or situation, even if negative, along with its related dynamics. There is evidence that acceptance is linked with a better quality of life (Garcia, Al Nima, Kjell, 2014). In the context of the coronavirus pandemic, acceptance aims to better balance one’s need to act with the realisation that many aspects of the situation are beyond one’s control. Meditation techniques (Stewart, 2014) and mindfulness (Hayes, Levin, Plumb-Vilardaga, Villatte, & Pistorello, 2013) promote acceptance and self-compassion. Clinical interventions based on acceptance and compassion target the maladaptive emotional avoidance and the unwillingness to experience negatively evaluated feelings, sensations and thoughts that generate inappropriate or detrimental behaviours. These interventions increase flexibility and allow adaptive behavioural change.
Promoting responsibility
Finally, situations like the COVID-19 pandemic may bring out both the best and the worst in people. It is a test of human ability to empathise, exhibit solidarity and put the good of the society above one’s own interests. Thus, individual responsibility is crucial in the time of the COVID-19 pandemic. Individuals are moral agents and their actions may positively or negatively affect the lives of other people. Therefore, promoting awareness of the pandemic and responsible behaviour towards oneself and others may help people feel morally sustained when confronting their fears. Ultimately, it is responsible action that may prove critical for our survival.
References
- Allen, J. G., & Fonagy, P. (Eds.). (2006). The handbook of mentalization-based treatment. New York, NY: John Wiley & Sons Inc. [Google Scholar]
- Bouman, T. K. (2014). Cognitive and behavioral models and cognitive-behavioral and related therapies for health anxiety and hypochondriasis. In Starcevic, V., & Noyes, R. (Eds.). Hypochondriasis and Health Anxiety: A Guide for Clinicians (pp. 149-198). New York, NY: Oxford University Press. [Google Scholar]
- Bowlby, J. (1988). A secure base. Clinical applications of attachment theory. London, UK: Routledge. [Google Scholar]
- Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N., & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet, 395(10227), 912–920. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson, D. (1980). Essay on Actions and Events. Oxford, UK: Oxford University Press. [Google Scholar]
- Domingue, R., & Mollen, D. (2009). Attachment and conflict communication in adult romantic relationships. Journal of Social and Personal Relationships, 26(5), 678–696. 10.1177/0265407509347932 [DOI] [Google Scholar]
- Garcia, D., Al Nima, A., & Kjell, O. N. E. (2014). The affective profiles, psychological well-being, and harmony: Environmental mastery and self-acceptance predict the sense of a harmonious life. PeerJ, 2, e259. 10.7717/peerj.259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gazzillo, F., Schimmenti, A., Formica, I., Simonelli, A., & Salvatore, S. (2017). Effectiveness is the gold standard of clinical research. Research in Psychotherapy: Psychopathology, Process and Outcome. 10.4081/ripppo.2017.278 [DOI] [PMC free article] [PubMed]
- Gentzler, A. L., Oberhauser, A. M., Westerman, D., & Nadorff, D. K. (2011). College students’ use of electronic communication with parents: Links to loneliness, attachment, and relationship quality. Cyberpsychology, Behavior and Social Networking, 14(1–2), 71–74. 10.1089/cyber.2009.0409 [DOI] [PubMed] [Google Scholar]
- Gibson, J. (2019). Mindfulness, Interoception, and the Body: A Contemporary Perspective. Frontiers in Psychology, 10. 10.3389/fpsyg.2019.02012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gnambs, T., & Appel, M. (2018). Narcissism and Social Networking Behavior: A Meta-Analysis. Journal of Personality, 86(2), 200–212. 10.1111/jopy.12305 [DOI] [PubMed] [Google Scholar]
- Harding, K. J. K., & Fallon, B. A. (2014). Pharmacological treatment and neurobiology of hypochondriasis, illness anxiety, and somatic symptoms. In Starcevic, V., & Noyes, R. (Eds). Hypochondriasis and Health Anxiety: A Guide for Clinicians (pp. 241-258). New York, NY: Oxford University Press. [Google Scholar]
- Hayes, S. C., Levin, M. E., Plumb-Vilardaga, J., Villatte, J. L., & Pistorello, J. (2013). Acceptance and commitment therapy and contextual behavioral science: Examining the progress of a distinctive model of behavioral and cognitive therapy. Behavior Therapy, 44(2), 180–198. 10.1016/j.beth.2009.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koole, S. L. (2009). The psychology of emotion regulation: An integrative review. Cognition and Emotion, 23(1), 4–41. 10.1080/02699930802619031 [DOI] [Google Scholar]
- Lange, A., van de Ven, J.-P., & Schrieken, B. (2003). Interapy: Treatment of post-traumatic stress via the internet. Cognitive Behaviour Therapy, 32(3), 110–124. 10.1080/16506070302317 [DOI] [PubMed] [Google Scholar]
- la Repubblica (2020). Coronavirus, l’allarme dei cardiologi: ‘Per il timore contagi meno ricoveri per infarto’ [Coronavirus, the cardiologists’ alarm: “Due to fear of contagion, less ospitalization for infartion”]. (2020, March 25). Retrieved from https://www.repubblica.it/salute/medicina-e-ricerca/2020/03/23/news/coronavirus_meno_ricoveri_per_infarto_si_teme_il_contagio-252070598/
- Lemma, A., Target, M., & Fonagy, P. (2011). Brief Dynamic Interpersonal Therapy: A Clinician’s Guide. Oxford, UK: Oxford University Press. [Google Scholar]
- Lord (2003). Aristotle’s Politics. Chicago, IL: University of Chicago Press. [Google Scholar]
- Midgley, N., Ensink, K., Lindqvist, K., Malberg, N., & Muller, N. (2017). Mentalization-based treatment for children: A time-limited approach. Washington, DC: American Psychological Association. 10.1037/0000028-000 [DOI] [Google Scholar]
- Morganstein, J. C., Fullerton, C. S., Ursano, R. J., & Holloway, H. C. (2017). Pandemics: Health Care Emergencies. In Ursano, R. J., Fullerton, C. S., Weisaeth, L., & Raphael, B. (eds.). Textbook of Disaster Psychiatry (2nd ed., pp. 270–284). Cambridge, NY: Cambridge University Press. [Google Scholar]
- Pallini, S., Chirumbolo, A., Morelli, M., Baiocco, R., Laghi, F., & Eisenberg, N. (2018). The relation of attachment security status to efortful self-regulation: A meta-analysis. Psychological Bulletin, 144(5), 501–531. 10.1037/bul0000134 [DOI] [PubMed] [Google Scholar]
- Philippot, P. (2013). Emotion Regulation: A Heuristic Paradigm for Psychopathology. Journal of Experimental Psychopathology, 4(5), 600–607. 10.5127/jep.034513 [DOI] [Google Scholar]
- Porges, S.W., & Dana, D. (2018). Clinical Applications of the Polyvagal Theory: The Emergence of Polyvagal-Informed Therapies. New York, NY: WW Norton. [Google Scholar]
- Roisman, G. I. (2006). The role of adult attachment security in non-romantic, non-attachment-related first interactions between same-sex strangers. Attachment & Human Development, 8(4), 341–352. 10.1080/14616730601048217 [DOI] [PubMed] [Google Scholar]
- Schimmenti, A., Santoro, G., La Marca, L., Costanzo, A., & Gervasi, A. M. (2019). Emotion dysregulation: a correlation network analysis. Psychotherapy and Psychosomatics, 88(S1), 115. https://doi.org/ 10.1159/000502467.359 [Google Scholar]
- Starcevic, V. (2005). Fear of Death in Hypochondriasis: Bodily Threat and Its Treatment Implications. Journal of Contemporary Psychotherapy, 35(3), 227–237. 10.1007/s10879-005-4317-0 [DOI] [Google Scholar]
- Starcevic, V. (2017). Cyberchondria: Challenges of Problematic Online Searches for Health-Related Information. Psychotherapy and Psychosomatics, 86(3), 129–133. 10.1159/000465525 [DOI] [PubMed] [Google Scholar]
- Stewart, J. M. (2014). Mindfulness, acceptance, and the psychodynamic evolution. Oakland, CA: Context Press. [Google Scholar]
- Stern, D. N. (1985). The Interpersonal World of the Infant: A View from Psychoanalysis and Developmental Psychology. New York, NY: Basic Books. [Google Scholar]
- Sucala, M., Schnur, J. B., Constantino, M. J., Miller, S. J., Brackman, E. H., & Montgomery, G. H. (2012). The therapeutic relationship in e-therapy for mental health: A systematic review. Journal of Medical Internet Research, 14(4), e110. 10.2196/jmir.2084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tversky, A., & Kahneman, D. (1973). Availability: A heuristic for judging frequency and probability. Cognitive Psychology, 5(2), 207–232. 10.1016/0010-0285(73)90033-9 [DOI] [Google Scholar]
- van der Kolk, B. (2015). The Body Keeps the Score: Mind, Brain and Body in the Transformation of Trauma. New York, NY: Penguin Random House. [Google Scholar]
- Watkins, E. R. (2016). Rumination-focused cognitive-behavioral therapy for depression. New York, NY: Guilford Press. [Google Scholar]
- Weineck, F., Messner, M., Hauke, G., & Pollatos, O. (2019). Improving interoceptive ability through the practice of power posing: A pilot study. PLoS ONE, 14(2). 10.1371/journal.pone.0211453 [DOI] [PMC free article] [PubMed] [Google Scholar]