Abstract
The health emergency we are experiencing due to the spread of the COVID-19 disease has strongly influenced the psychological and physical health of the general population, including the health care professionals. The aim of this brief article is a preliminary analysis of the psychological interventions following the infectious disease outbreak in order to 1) implement guidelines for the existing emerging psychological crisis for people directly and indirectly affected by COVID-19, and 2) establish adequate procedures and prompt responses.
Keywords: COVID-19, emergency psychology, mental health, psychological intervention, emotional epidemiology
In December 2019, the Chinese authorities informed the world of the rapid spread of a new type of virus, initially named CoV-2019, identifying its epicentre in the city of Wuhan belonging to the Hubei province. In February 2020, the International Committee on Taxonomy of Viruses (ICTV) assigned the definitive name to the new coronavirus: “SARS-CoV-2”. During the same period, the World Health Organization (WHO) announced “COVID-19” as the official name of the new disease, to identify the severe acute respiratory syndrome caused by SARS-CoV-2.
The aim of this brief article is a preliminary analysis of the psychological interventions following the infectious disease outbreak in order to 1) implement guidelines for the existing emerging psychological crisis for people directly and indirectly affected by COVID-19, and 2) establish adequate procedures and prompt responses.
In the context of an infectious disease outbreak, much has been written about the epidemiology of infectious diseases, while the so called “emotional epidemiology” (Ofri, 2009) has been neglected (Duan, Linder, & Huremović, 2019). As highlighted by Duan and Zu (2020), in The Lancet Psychiatry, under rigid infection measures, non-essential personnel such as psychologists, psychiatrists, and mental health workers are discouraged from accessing isolation wards or isolation rooms designated for patients with COVID-19. Consequently, psychological interventions, addressed to inpatients, are mainly provided by frontline health-care workers. In general terms, with the disease progression, clinical symptoms become more severe, along with a possible worsening of the mental health status in infected patients. Acknowledging it, psychological interventions “should be targeted and adapted as appropriate” (Duan & Zu, 2020). As the novel coronavirus outbreak has intensified worldwide, Public Health Officials have urged the public to practice social distancing and self-quarantine to limit the virus spread amongst others. Currently, the global population is living under stressful conditions of forced quarantine (i.e., isolated at home, ordinary isolation ward or intensive care unit) characterized by self-isolation, social distancing, separation, accompanied by a deep loss of freedom, uncertainty and intolerance of uncertainty. Quarantine is often characterized by negative emotions such as fear, anger and frustration which may lead to anxiety, boredom and/or a feelings of uneasiness (Brooks et al., 2020; Qiu et al., 2020), which endorses negative beliefs about the individual ability to cope. An even worst case-scenario can be envisaging for vulnerable mental health patients within the community, at risk for developing more anxiety about the pandemic, particularly if they are already treated for anxiety (Huremović, 2019) or if they are susceptible to uncertainty.
Results emerging from empirical researches, carried out in comparable periods of quarantine, underlined additional components of psychological distress such as: maladaptive behaviours (excessive information seeking, avoidance, or impulsive decision-making) (Carleton, Mulvogue, Thibodeau, McCabe, Antony & Asmundson, 2012; Pawluk & Koerner, 2013), feelings of loss. In particular, feelings of loss seem to consistently correlate with the conflict between a sense of duty (I’m staying at home in order to contain the infection spread/I’m going to work because I cannot abandon my patients) and disruptive sensations such as frustration, anger and fear (Robertson, Hershenfield, Grace, & Stewart, 2004). In this contest, a recent review of the literature points out attention on a few factors which seem to negatively influence our system during the quarantine period: 1) the duration of the quarantine itself; 2) the fear to get infected/spread the infection; 3) feelings of frustration and boredom; 4) inadequate supply capacity; and 5) lack of sufficient/salient information (Brooks et al., 2020). In addition, the study highlighted the extent of the impact the quarantine period on the mental health status and the resulting delay in returning to routines, as other examples from prolonged distress situations (Conversano, 2019; Martino, Langher, Cazzato, & Vicario, 2019). With respect to the factors mentioned above, psychological intervention provides the adequate “tools” to assess potential risk factors leading to psychological maladaptive responses. Besides, they can help with the management of feelings of fear and anxiety, panic, boredom, frustration and intolerance of uncertainty.
Recently, institutions and universities worldwide, have activated online counselling services, using social media platforms, e-mails or electronic letters (Xiao, Zhang, Kong, Li, & Yang, 2020) to promote psychological support for those in need. Several national and international psychological associations have shared guidelines in order to deal with the immediate emergency. The aim of these informative materials is to enhance motivation for action to deal with the emerging emotional challenges. Prompt responses and psychological interventions to the current emergency psychological crisis for people affected by COVID-19 and the health service personnel are required in order to contain the evolution of psychopathological changes, resulting in maladaptive behaviours and broader range of emotional disorders. For the healthcare professionals, anxiety, panic, distress, acquired helplessness, represent worsening factors for their own mental health and in terms of professional performance, modulating the treatment of patients and family members (Xiang et al., 2020) but also the communication with them related to the final stage of the individual’s life (Iasevoli et al., 2012). The last aspect mentioned is particularly pressing in countries such Italy, Spain and China which are now witnessing the relentless rise in COVID-19 deaths.
Measures planned and implemented by the Chinese authorities include the provision of online questionnaires on mental health status, in order to provide guidance in the allocation of resources and the development of patient-tailored treatments. We believe that it is appropriate to take action in order to plan appropriate responses to the current psychological crisis caused by the COVID-19 health emergency. In line with a few outstanding Chinese contributions (Zhang, Wu, Zhao, & Zhang, 2020; Ho, Chee, & Ho, 2020, Liu et al., 2020), we have attempted herein to conceptualize the phases of psychological intervention as displayed in Fig.1.
Figure 1.
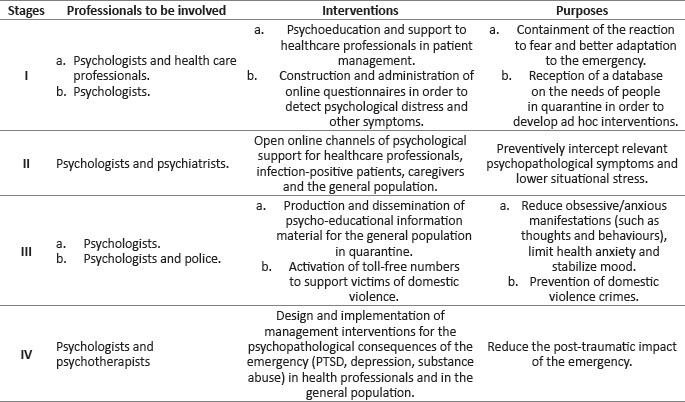
Phases of psychological intervention
During the early weeks of the outbreak of infections, it is fundamental to activate support systems for healthcare professionals and open online communication pathways via smart devices in order to make psychological support available. Moreover, such interventions should also be guaranteed for infected individuals and their caregivers. Interventions aimed at healthcare professionals should, through the support of psychologists, focus on the management and containment of population’s behaviours. Secondly, psychologists and psychotherapists should create questionnaires that can easily disseminated amongst the general population (e.g. through online administration), healthcare professionals and all infected and quarantined individuals, in order to assess the presence/absence of psychologically negative indicators (or risk factors) and, possibly, formulate a set of data with respect to the highlighted needs.
Subsequently, and immediately following the previous actions, a psychological support channel for operators (via telephone and/or online platforms) is required, which must remain open for the duration of the emergency. Simultaneously, a support channel for infected individuals and family members, as well as for the general population, should be guaranteed, engaging psychologists trained in emergency psychology and adequately informed of the most reliable media channels. In both circumstances, psychologists should be able to direct individuals who show marked psychopathological symptoms to psychiatrists for further telephone counselling. As regards to interventions in the general population, during a third phase, psychologists should produce and disseminate information materials on the psychological consequences of the quarantine and toll-free numbers should simultaneously be activated, in collaboration with the police, in order to support all those who are confronted with situations of domestic violence, including children.
Studies carried out with survivors of health emergencies caused by other viruses (e.g. SARS) or other traumatic events, support the notion of the presence of a high rate of depressive disorders and post-traumatic stress disorders (PTSD) in adults, children and in healthcare professionals as well (Hawryluck, Gold, Robinson, Pogorski, Galea, & Styra, 2004; Sprang & Sielman, 2013; Liu et al., 2012; Carmassi et al., 2016; Carmassi et al., 2017; Carmassi et al., 2018; Di Giuseppe et al., 2020). For this latter group, further complications identified included an increase in substance abuse even at 3 years following the onset of the epidemic (Wu et al., 2008; Lee, Chan, Chau, Kwok, & Kleinman, 2005). The long-term consequences of prolonged distress can have disastrous effects on cognitive functioning, including damage to the memory and hippocampal neuroplasticity as well as an increased risk of developing symptoms (McEwen, 1999). For this reason, at the end of the third phase of intervention, it should be possible for the professional community of psychologists to develop interventions and projects in order to stem the psychological consequences of enforced quarantine or difficult working environments in an emergency situation.
For all the reasons reported herein, fine tuning effective psychological interventions are a future need, given that after the public health emergency psychological distress emergency seems at the horizon.
References
- Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N., & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: rapid review of the evidence. The Lancet. DOI: 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed]
- Carleton, R. N., Mulvogue, M. K., Thibodeau, M. A., McCabe, R. E., Antony, M. M., & Asmundson, G. J. (2012). Increasingly certain about uncertainty: Intolerance of uncertainty across anxiety and depression. Journal of anxiety disorders, 26(3), 468-479. DOI: 10.1016/j.janxdis.2012.01.011 [DOI] [PubMed] [Google Scholar]
- Carmassi, C., Bertelloni, C. A., Gesi, C., Conversano, C., Stratta, P., Massimetti, G., ... & Dell’Osso, L. (2017). New DSM-5 PTSD guilt and shame symptoms among Italian earthquake survivors: Impact on maladaptive behaviors. Psychiatry research, 251, 142-147. DOI: 10.1016/j.psychres.2016.11.026 [DOI] [PubMed] [Google Scholar]
- Carmassi, C., Gesi, C., Corsi, M., Cremone, I. M., Bertelloni, C. A., Massimetti, E., ... & Dell’Osso, L. (2018). Exploring PTSD in emergency operators of a major University Hospital in Italy: a preliminary report on the role of gender, age, and education. Annals of general psychiatry, 17(1), 17. DOI: 10.1186/s12991-018-0184-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmassi, C., Gesi, C., Simoncini, M., Favilla, L., Massimetti, G., Olivieri, M. C., ... & Dell’Osso, L. (2016). DSM-5 PTSD and posttraumatic stress spectrum in Italian emergency personnel: correlations with work and social adjustment. Neuropsychiatric disease and treatment, 12, 375. DOI: 10.2147/NDT.S97171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conversano, C. (2019). Psychological common factors in chronic diseases. Frontiers in Psychology, 10, 2727. DOI: 10.3389/fpsyg.2019.02727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Giuseppe, M. Miniati, M., Miccoli, M., Ciacchini, R., Orrù, G., Lo Sterzo, R., Di Silvestre A., Conversano, C. (2020). Defensive responses to stressful life events associated with cancer diagnosis. Mediterranean Journal of Clinical Psychology, 8(1). DOI: 10.6092/2282-1619/mjcp-2384 [Google Scholar]
- Duan, C., Linder, H., & Huremović, D. (2019). Societal, Public, and [Emotional] Epidemiological Aspects of a Pandemic. In Psychiatry of Pandemics (pp. 45-53). Springer, Cham. DOI: 10.1007/978-3-030-15346-5_4
- Duan, L., & Zhu, G. (2020). Psychological interventions for people affected by the COVID-19 epidemic. The Lancet Psychiatry. DOI: 10.1016/S2215-0366(20)30073-0 [DOI] [PMC free article] [PubMed]
- Hawryluck, L., Gold, W. L., Robinson, S., Pogorski, S., Galea, S., & Styra, R. (2004). SARS control and psychological effects of quarantine, Toronto, Canada. Emerging Infectious Diseases, 10(7), 1206. DOI: 10.3201/eid1007.030703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho, C. S., Chee, C. Y., & Ho, R. C. (2020). Mental Health Strategies to Combat the Psychological Impact of COVID-19 Beyond Paranoia and Panic. Annals of the Academy of Medicine, Singapore, 49 (1), 1. [PubMed] [Google Scholar]
- Huremović, D. (2019). Preparing for the Outbreak. In Psychiatry of Pandemics (pp. 65-76). Springer, Cham. DOI: 10.1007/978-3-030-15346-5_6
- Iasevoli, M., Giantin, V., Voci, A., Valentini, E., Zurlo, A., Maggi, S., ... & Manzato, E. (2012). Discussing end-of-life care issues with terminally ill patients and their relatives: comparisons among physicians, nurses and psychologists. Aging clinical and experimental research, 24(3 Suppl), 35-42 [PubMed] [Google Scholar]
- Lee, S., Chan, L. Y., Chau, A. M., Kwok, K. P., & Kleinman, A. (2005). The experience of SARS-related stigma at Amoy Gardens. Social science & medicine, 61(9), 2038-2046. DOI: 10.1016/j.socscimed.2005.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, S., Yang, L., Zhang, C., Xiang, Y. T., Liu, Z., Hu, S., & Zhang, B. (2020). Online mental health services in China during the COVID-19 outbreak. The Lancet Psychiatry. DOI: 10.1016/S2215-0366(20)30077-8 [DOI] [PMC free article] [PubMed]
- Liu, X., Kakade, M., Fuller, C. J., Fan, B., Fang, Y., Kong, J., ... & Wu, P. (2012). Depression after exposure to stressful events: lessons learned from the severe acute respiratory syndrome epidemic. Comprehensive psychiatry, 53(1), 15-23. DOI: 10.1016/j.comppsych.2011.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martino, G., Langher, V., Cazzato, V., & Vicario, C. M. (2019). Psychological factors as determinants of medical conditions. Frontiers in psychology, 10, 2502. DOI: 10.3389/fpsyg.2019.02502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen, B. S. (1999). Stress and hippocampal plasticity. Annual review of neuroscience, 22(1), 105-122. DOI: 10.1146/annurev.neuro.22.1.105 [DOI] [PubMed] [Google Scholar]
- Ofri D. (2009). The emotional epidemiology of H1N1 influenza vaccination. N Engl J Med., 36(27): 2594-5. DOI: 10.1056/NEJMp0911047 [DOI] [PubMed] [Google Scholar]
- Pawluk, E. J., & Koerner, N. (2013). A preliminary investigation of impulsivity in generalized anxiety disorder. Personality and Individual Differences, 54(6), 732-737. DOI: 10.1016/j.paid.2012.11.027 [Google Scholar]
- Qiu, J., Shen, B., Zhao, M., Wang, Z., Xie, B., & Xu, Y. (2020). A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. General Psychiatry, 33(2). DOI: 10.1136/gpsych-2020-100213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson, E., Hershenfield, K., Grace, S. L., & Stewart, D. E. (2004). The psychosocial effects of being quarantined following exposure to SARS: a qualitative study of Toronto health care workers. The Canadian Journal of Psychiatry, 49(6), 403-407. DOI: 10.1177/070674370404900612 [DOI] [PubMed] [Google Scholar]
- Sprang, G., & Silman, M. (2013). Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster medicine and public health preparedness, 7(1), 105-110. DOI: 10.1017/dmp.2013.22 [DOI] [PubMed] [Google Scholar]
- World Health Organization. Novel Coronavirus (2019-nCoV) technical guidance. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance.
- Wu, P., Liu, X., Fang, Y., Fan, B., Fuller, C. J., Guan, Z., ... & Litvak, I. J. (2008). Alcohol abuse/dependence symptoms among hospital employees exposed to a SARS outbreak. Alcohol & Alcoholism, 43(6), 706-712. DOI: 10.1093/alcalc/agn073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiang, Y. T., Yang, Y., Li, W., Zhang, L., Zhang, Q., Cheung, T., & Ng, C. H. (2020). Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. The Lancet Psychiatry, 7(3), 228-229. DOI: 10.1016/S2215-0366(20)30046-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao, H., Zhang, Y., Kong, D., Li, S., & Yang, N. (2020). The Effects of Social Support on Sleep Quality of Medical Staff Treating Patients with Coronavirus Disease 2019 (COVID-19) in January and February 2020 in China. Medical Science Monitor, 26. DOI: 10.12659/MSM.923549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, J., Wu, W., Zhao, X., & Zhang, W. (2020). Recommended psychological crisis intervention response to the 2019 novel coronavirus pneumonia outbreak in China: a model of West China Hospital. Precision Clinical Medicine. DOI: 10.1093/pcmedi/pbaa006 [DOI] [PMC free article] [PubMed]


