Abstract
Community mental health centers (CMHCs) provide the majority of mental health services for low-income individuals in the United States. Exposure and Response Prevention (ERP), the psychotherapy of choice for OCD, is rarely delivered in CMHCs. This study aimed to establish the acceptability and feasibility of testing a Behavioral Therapy Teams (BTT) intervention to deliver ERP in CMHCs. BTT consisted of individual information-gathering sessions followed by 12 weeks of group ERP and concurrent home-based coaching sessions. The sample consisted of 47 low-income individuals with OCD who were randomized to receive BTT or Treatment As Usual (TAU). Symptom severity and quality of life measures were assessed at pretreatment, post-treatment, 3-month and 6-month post-treatment. Feasibility of training CMHC staff was partially successful. CMHC therapists successfully completed rigorous training and delivered ERP with high fidelity. However, training paraprofessionals as ERP coaches was more challenging. ERP was feasible and acceptable to patients. BTT participants were more likely than TAU participants to attend their first therapy session and attended significantly more treatment sessions. A large between-group effect size was observed for reduction in OCD symptoms at post-treatment but differences were not maintained across 3- and 6-month follow-ups. For BTT participants, within-group effects sizes reflecting change from baseline to post-treatment were large. For TAU participants, depressions scores did not change during the active treatment phase but gradually improved during follow-up. Results support feasibility and acceptability of ERP for this patient population. Findings also underscore the importance of implementation frameworks to help understand factors that impact training professionals.
Keywords: OCD, cognitive-behavioral therapy, implementation, community mental health, Exposure and Response Prevention
Obsessive-compulsive disorder (OCD) is a chronic and often disabling psychiatric disorder affecting 1.6 to 2.3% of the general population (Kessler et al., 2005; Weissman et al., 1994). Exposure and Response Prevention (ERP) is the first-line psychosocial intervention for OCD (Koran et al., 2017). When delivered under optimal conditions, 65–85% of ERP treatment completers show clinically significant improvement and 40–70% achieve at least partial remission (Fisher & Wells, 2005; Foa et al., 2005). ERP (with or without medications) is superior to serotonin-reuptake inhibitor (SRI) monotherapy in acute outcome and in long-term maintenance of gains (Foa et al., 2014; Foa et al., 2005). Despite this demonstrated efficacy, very few people who seek mental health treatment for OCD actually receive ERP treatments (Eisen et al., 1999; Goisman et al, 1999; Mancebo et al., 2006; Steketee et al., 1999). The discrepancy between the recovery rates in clinical trials and utilization of ERP in routine clinical practice, referred to as the research-practice gap of evidence-based psychotherapies (EBPs), highlights the critical need to transport and implement ERP into community settings (Stirman et al., 2015).
Low-income individuals in the United States are particularly at risk for not receiving ERP because they lack the financial resources to access specialized treatment centers, experience more socioeconomic barriers to receiving care, and are more likely to drop-out of treatment (Foa et al., 2005; Wade et al., 1998). CMHCs provide the majority of mental health services for low-income populations in the United States but it is unclear whether standard ERP will “fit” the needs of this setting and patient population. Patients often present with severe functional impairment and comorbid serious mental illness (SMI) which present unique clinical challenges. The extent to which ERP generalizes to CMHC populations (i.e. individuals with comorbid SMI, low-income status, culturally diverse) is also unknown given that many existing studies, do not report these key patient characteristics, and those that do report on largely Caucasian and middle-class patient populations (Carter et al., 2012; Stewart & Chambless, 2009).
Recent studies suggest that community clinicians with little to no prior experience with Exposure Therapy for anxiety benefit from specialized training in this modality. Harned and colleagues (2013, 2014) found that clinicians who completed a high-quality online training program showed improved attitudes towards exposure therapies, increased proficiency in techniques as assessed by simulated role-plays, and higher rates of self-reported use of exposure techniques in their clinical practice. Another study comparing different training models (workshop, computerized, or workshop that emphasized active learning) found that training (workshop or computerized) did not result in changes in therapist behavior unless it was followed by post-workshop consultations (Beidas et al. 2012). In the only study to examine effectiveness of Exposure Therapy delivered in a publicly funded CMHC, Harned and colleagues found that adding Prolonged Exposure (Foa et al. 2019) to Dialectical Behavior Therapy (Linehan, 1993) improved post-traumatic stress disorder (PTSD) symptoms in patients with severe comorbidities (Harned et al., 2020).
In the present study, we evaluate feasibility and acceptability of a behavioral therapy team (BTT) approach to delivering ERP which was designed to meet the needs of CMHC providers and settings (Mancebo et al., 2017). In a previous treatment development study, we adapted group ERP for OCD to be delivered by a multidisciplinary team composed of a MA-level therapist and 2 paraprofessionals (case managers). Results of an open trial (n=8) supported the feasibility and acceptability of BTT in a CMHC setting but suggested that two modifications were necessary to improve implementation of the intervention (Mancebo et al., 2017). In this study, we use a rolling admission group model (vs closed admission groups) and we replaced the two-day workshop with a two-hour training workshop and a technology-based self-guided program with weekly supervision meetings. The primary aim of this study was to establish the acceptability and feasibility of testing BTT for OCD in a subsequent, fully powered clinical effectiveness trial. Specific aims were to: (1) demonstrate the feasibility of training CMHC teams to deliver ERP, (2) compare feasibility and acceptability of BTT versus Treatment as Usual (TAU) among low-income clients with OCD, and (3) evaluate potential clinical significance of effects of BTT versus TAU. We hypothesized that compared to TAU, BTT would: (1) be more acceptable to low-income clients (2) have fewer treatment dropouts, and (3) result in greater improvement in OCD symptoms and functioning at post-treatment and 3- and 6- month follow-up.
Methods
Study Design
A randomized controlled trial (RCT) was used to inform issues of feasibility, acceptability, and potential clinical significance of BTT compared to TAU. Participants were assigned to BTT or TAU using a 2:1 urn randomization procedure stratifying the groups based on: (1) severe OCD symptoms (Y-BOCS > 23) and (2) SRI status (taking an SRI or not). This randomization procedure, allocating more participants to BTT relative to TAU, was implemented to maximize the size of BTT therapy groups and data to inform BTT treatment development (i.e. more participants received the intervention and groups are more likely to resemble real-world settings). This allocation was also thought to facilitate study recruitment and retention. Participants completed an in-person screening interview prior to enrollment, a baseline assessment (which occurred 1–5 days prior to scheduled intake appointment for BTT or TAU psychotherapy), a post-treatment assessment immediately after treatment (or week 16 for TAU participants), and at 3- and 6- month post-treatment follow-ups (weeks 28 and 40).
CMHC administrators selected staff to participate in the study and time spent on the study was logged to adjust for staff productivity targets. Three MA-level therapists were trained. Two were clinical social workers and one was a mental health counselor. Only one was licensed to practice independently. All were white and two were female. Age ranged from 26–31 years. Thirteen paraprofessionals were selected as coaches. Job descriptions at the agency included case manager, rehabilitation/vocational specialist, or care coordinator. All these positions included home-based or community services. Time employed at the agency ranged from 6 months to 15 years (M=3.0, SD=4.0) The average age was 33.4 (SD=13.5). One coach was Hispanic and all other coaches were White. Nine (69%) were female. Highest level of education completed was high school (n=5, 38%) or Bachelor’s degree (n=8, 61%).
Patient participants were recruited from individuals receiving treatment at a large CMHC, a hospital-based OCD specialty clinic, and from community mental health service providers. Eligible individuals were between the age of 18–65 and had a principal diagnosis of OCD (defined as the psychiatric disorder that caused the most difficulties over the past year) according to DSM-IV (American Psychiatric Association, 2000). Additional inclusion criteria were: a score ≥ 16 on the Yale-Brown Obsessive Compulsive Scale (Y-BOCS; Goodman et al, 1989a; 1989b), low-income (total household income was less than three times the national poverty threshold for a household of their size (U.S. Department of Health and Human Services, 2008), stable medication regimen for at least 4 weeks, and no previous course of ERP (defined as 10 or more sessions of ERP). Participants were excluded if there was evidence of cognitive impairment or if they reported past-month prominent suicidal ideation, mania, substance use disorder, or psychosis. We also excluded individuals who endorsed prominent hoarding symptoms as this target problem requires a multicomponent CBT approach (Tolin et al., 2015). Individuals that were receiving psychotherapy primarily for anxiety or OCD symptoms were also excluded.
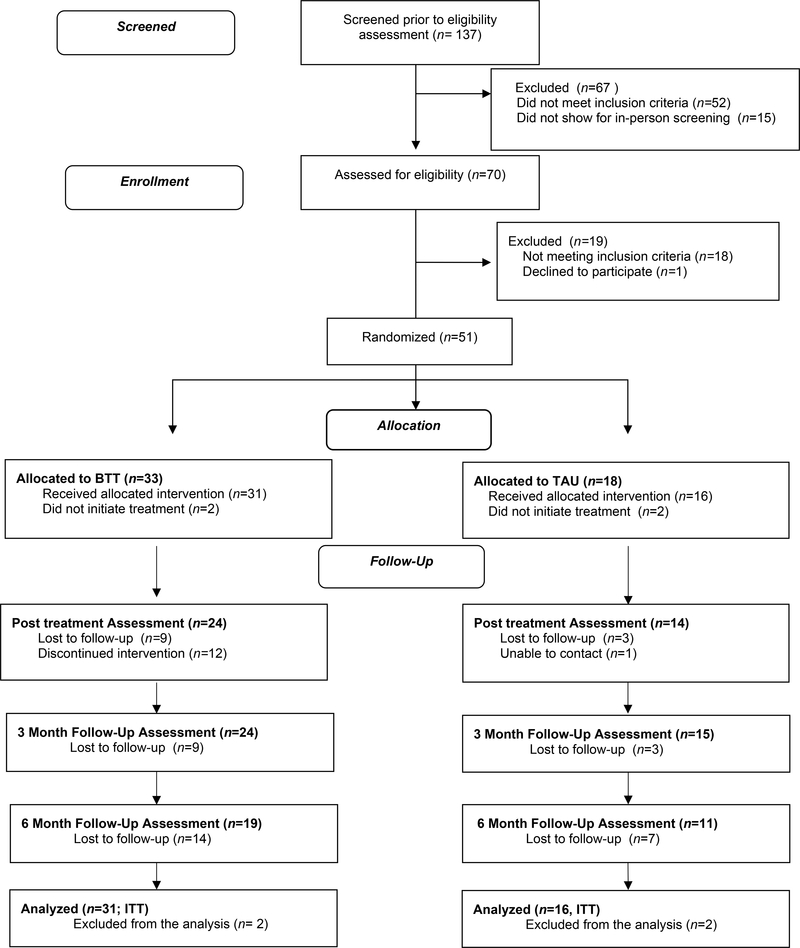
Figure 1 presents the CONSORT diagram of participant enrollment and flow throughout the study. Fifty-one participants were randomized to a treatment condition. The most common reasons for exclusions were: OCD was not primary diagnosis (n=5), prominent hoarding symptoms (n=4), and presence of acute psychotic symptoms (n=4). Four participants completed the screening interview and were randomized to a treatment condition but failed to attend the baseline assessment (or their initial therapy appointment) yielding an intent-to-treat (ITT) sample of 47 participants (31 were assigned to BTT and 16 were assigned to TAU).
Figure 1.
Consort Flowchart
Participants ranged in age from 19 to 55 (M = 38.4, SD =10.4) and 68% were women. Sixty-two percent of participants identified as White and 38% identified as racial/ethnic minorities. The majority (81%) were not married or partnered. Two participants were homeless and one lived in a supervised group home. All but five participants reported a history of paid employment for at least one year but 65% of the sample reported occupational disability due to psychiatric reasons. Two-thirds of participants reported an annual household income at the federal poverty level ($11,170/year or less). Sixty-one percent had publicly funded health insurance, 28% had commercial insurance, and 11% lacked any health insurance.
Regarding clinical characteristics, 55% reported a history of psychiatric hospitalizations and 29% identified OCD as the primary reason for psychiatric hospitalizations. All but one participant met diagnostic criteria for a comorbid Axis I disorder. Most common diagnoses were another anxiety disorder (49%), PTSD (32%), Major Depression (25%), and Body Dysmorphic Disorder (11%). In addition, 16% of the sample met lifetime criteria for a Psychotic Disorder (8%) or Bipolar Disorder (8%). Average age of onset of DSM-IV OCD was 19.9 years (SD= 12.2) and average number of years on psychotropic medications was 8.23 (SD=7.70). Seventy-five percent of the sample was taking an SRI.
Procedures
The Butler Hospital and Lifespan Institutional Review Boards approved this study. Enrollment began in December 2012 and continued through April 2015. Study staff met with each of the treatment teams at the CMHC and other clinical settings to describe the study, answer questions about the study, and distribute study brochures and referral forms. A research assistant (RA) conducted a phone screen to assess study eligibility and eligible participants were scheduled for an in-person screening assessment. At the screening assessment, the RA obtained written informed consent and administered the screening assessment measures to confirm study eligibility. Eligible participants were randomized to study treatment groups by a computerized algorithm. The RA then scheduled appointments for a baseline assessment (with a study Independent Evaluator) and the initial therapy intake (with a therapist). Baseline measures were administered within the week prior to the first therapy appointment. The study RA informed participants of their allocation assignment at the end of their baseline assessment. All participants that attended the baseline assessment were included in the ITT sample. Independent Evaluators (IEs) who were blind to study treatment assignment conducted baseline and follow-up study assessments. The IEs were post-doctoral fellows who completed rigorous training and interrater reliability assessments over a course of 2 months. Participants in both treatment conditions were paid to complete assessments ($25 for baseline and $50 for follow-ups) and if needed, were provided with transportation or childcare in order to attend therapy appointments.
Treatment Conditions.
TAU consisted of referrals to a CBT therapist in the community or an intake evaluation at Gateway CMHC (the treatment site). To prevent cross-over effects, participants receiving TAU were not assigned to BTT therapists or case managers. Participants were provided with assistance in scheduling the initial intake appointment. TAU therapists were contacted by study staff at week 20 of the study and asked to complete a self-report questionnaire to assess treatments utilized and client attendance. Therapists were paid $50 upon receipt of the completed questionnaire.
BTT Intervention consisted of three components delivered by CMHC staff over 16 weeks: (a) 3–4 pretherapy (information gathering) individual sessions with a MA-level therapist, (b) 12 weekly group sessions with a MA-level therapist, and (c) 10 individual coaching sessions with a paraprofessional during weeks 2–11 of the group. A rolling admission group structure allowed new members to join the group every 4 weeks. In addition, participants were offered an aftercare option of attending two monthly booster sessions following the completion of group therapy sessions. A BTT manual was adapted from existing individual and group treatment manuals (Kozak & Foa, 1997; Van Noppen et al., 1998). More details regarding initial intervention development can be found elsewhere (Mancebo et al., 2017).
During the pre-therapy individual sessions, the therapist gathered detailed information about OCD symptoms, described the treatment rationale, reviewed treatment expectations, and addressed fears/concerns about engaging in treatment. The therapist and patient developed an initial treatment plan and fear/avoidance hierarchy prior to the patient starting group therapy. Group therapy sessions were 90 minutes and held weekly over 12 consecutive weeks. New members were added at the beginning of every month to maximize group cohesion. The agenda for each group included a brief check-in, review of homework, exposure practice, and homework planning. Sessions that included a new member also consisted of introductions, brief review of group guidelines, group discussion of personal goals and progress made. Participants that were close to terminating group therapy (sessions 10–12) were also encouraged to discuss feelings regarding termination.
A coach was assigned to each participant and attended the third individual therapy session when possible. During this session, the therapist described the team model and reviewed the patient’s ERP treatment plan and the role of the coach (to help patient complete ERP exercises). The coach and participant then scheduled 10 individual coaching sessions during weeks 2 through 11 of group therapy. Sessions usually occurred in the patient’s home or in a predetermined public location. If scheduling issues did not permit a joint session, the coach scheduled a brief (30 minute) introductory meeting with the patient that took place before the first group therapy session. The coach also attended weekly team meetings and had access to group therapy notes which included a description of specific ERP homework goals. The coach and participant began each session by reviewing the participant’s homework goals and therapy notebook. Then the coach assisted the participant with completing the assigned exposure and provided encouragement or problem-solving as needed. The session ended with a specific plan for the participant to complete the same exercises on his/her own (daily homework completions).
BTT Training and Supervision.
Initial training for therapists and coaches consisted of a two-hour meeting to present an overview of study procedures and a technology-based self-guided training program based on the same content delivered during a two-day workshop training on ERP (Mancebo et al. 2017). A series of five self-guided 60-minute electronic modules on OCD, CBT principles, and ERP were available for staff to view individually in their offices. Staff completed pre- and post-training quizzes to assess knowledge. Staff also attended weekly group supervision meetings led by the PI. Therapists read the Mastery of OCD treatment manual (Kozak & Foa, 1997) and the BTT group therapy manual and attended three in-person sessions focused on behavioral rehearsal of key skills. Following the didactic training phase, therapists observed an experienced ERP therapist conducting information-gathering sessions and co-led a 12-week group. Coaches observed three coaching sessions with an experienced coach. Individual and group therapy sessions were videotaped and coaching sessions were audiotaped. Therapists and coaches completed self-adherence ratings at the end of each session. During the training phase, the PI viewed or listened to recordings of all therapy/coaching sessions and completed fidelity ratings for the first treatment episode (12 weeks of group or first coaching case). Discrepancies between self and observer ratings of fidelity were discussed during weekly supervision meetings as were items that were not covered in a session. Staff members were considered to have completed training when they completed the entire training protocol and were able to deliver BTT with high fidelity (at least 80% on first 12 sessions delivered).
Assessment Schedule and Measures.
Pretreatment assessments were conducted at the screening and baseline visits. Baseline visits occurred 1–5 days prior to the initial psychotherapy session. Post-treatment assessments were conducted at the end of treatment for BTT participants and week 16 for TAU participants. Follow-up assessments were conducted at 3-months (week 28) and 6-months (week 40) post-treatment. The OCD Database (Rasmussen & Eisen, 1992) was administered at the screening visit to collect demographic and clinical characteristics. Additional items were added to collect data on income and health insurance status. The Structured Clinical Interview for DSM-IV-TR Axis I Disorders – Patient version (SCID-I/P) and the Structured Clinical Interview for DSM-IV Axis II disorders (SCID-II) were used to determine Axis I and Axis II disorders (First et al., 1997; 2002).
The Psychosocial Treatment Inventory (PTI; Steketee et al., 1997) was used to collect frequency and type of psychotherapy techniques used during the study. The PTI is an interviewer-administered questionnaire that assesses frequency and type of psychotherapy techniques (behavioral, cognitive, supportive, psychodynamic, and family). The RA administered the PTI to participants at each follow-up assessment. In addition, all TAU therapists were contacted at week 16 and asked to complete the clinician self-report version of the questionnaire. The PTI includes items related to the primary treatment approach, therapist training, primary focus of sessions, total number of sessions attended, and treatment attendance. Discrepancies between the patients’ and therapists’ reports were noted.
Feasibility of implementing BTT was assessed by calculating percent of CMHC staff who completed the training protocol. Therapist and coach fidelity measures were adapted from those used to assess adherence to the Mastery of OCD ERP manual (Kozak & Foa, 1997). Group therapy sessions were videotaped and coaching sessions were audiotaped. During the active/study treatment phase, Independent Evaluators (who were not required to be blind to treatment allocation) rated video recordings of group therapy sessions and audio recordings of coaching sessions to assess adherence to group ERP and coaching protocols.
Treatment attendance and dropout decisions were recorded on a weekly basis for BTT participants and ascertained at post-treatment for TAU participants (participant interview and therapist questionnaire). Participants were classified as dropouts if they simply stopped attending sessions, contacted the therapist stating they no longer wished to attend sessions, attended less than 9 group ERP sessions (BTT) or failed to reschedule missed appointments (TAU).
Acceptability of the BTT intervention was ascertained using the Client Satisfaction Questionnaire (CSQ-8) and end-of-treatment qualitative interviews. The CSQ-8, an 8-item self-report, yields a total score that reflects global satisfaction with and perceived quality of mental health services (Larsen et al., 1979). Total scores range from 8–32 with higher scores indicating greater satisfaction. This scale has been used in mental health and other health centers, and has acceptable internal consistency (Larsen et al., 1979; Nguyen et al., 1983). For BTT participants, we added two items to assess the group therapy and coaching components of the intervention: “How helpful were the group therapy sessions?” and “How helpful were the individual coaching sessions?”. The CSQ-8 was administered at the post-treatment assessment only.
The qualitative interview was administered to BTT participants over the phone by the RA and consisted of open-ended questions such as “What did you find to be the most helpful about the treatment/group therapy/coaching sessions?” “What do you think needs improvement?”
Clinical Outcomes Measures
Clinical outcome measures were administered by independent evaluators at screening, baseline (week 0), immediate post-treatment (16 weeks) and 3-month (28 weeks)- and 6-month (40 weeks) post-treatment.
The Y-BOCS, an interviewer-administered 10-item scale with specific probes and anchors, assesses severity of obsessions and compulsions across five domains: time, distress, interference, resistance, and control. This scale, which has established reliability and validity, is widely accepted as the “gold” standard outcome measure for OCD (Goodman et al., 1989a, 1989b). Total score ranges from 0 (no symptoms) to 40 (extreme symptoms). The YBOCS was administered at each assessment visit as the primary clinical outcome measure. Internal consistency of the Y-BOCS in the present sample at baseline was good (Cronbach’s α = .81).
The Brown Assessment of Beliefs Scale (BABS) is a 7-item, reliable and valid interview that assesses insight into OCD symptoms (Eisen et al., 1998). The BABS provides a dimensional score ranging from 0 to 24 with higher scores indicating poor insight or delusionality. Internal consistency in the present sample was good (Cronbach’s α = .82).
The Beck Depression Inventory-II (BDI-II), a 21-item self-report questionnaire, was used to measure depression severity. The BDI-II has good internal consistency and construct validity (Beck et al., 1996). Internal consistency in the present sample was good (Cronbach’s α = .88).
The Social and Occupational Functioning Scale (SOFAS) is an interviewer-rated measure of global functioning during the worst week of the past month (American Psychiatric Association, 2000). Scores range from 1 to 100 with higher scores indicating better functioning. The Quality of Life Enjoyment and Satisfaction Questionnaire (Q-LES-Q) is a self-report instrument, widely used in psychiatric populations, with demonstrated reliability and validity (Endicott et al., 1993). The questionnaire consists of 16 items that assess 8 domains of quality of life. The first 14 items yield a total score (range 14 to 70) and is expressed as a percentage based on the maximum total score of the items (0–100%). Higher scores indicate greater life satisfaction. Internal consistency for this sample was acceptable (Cronbach’s α = .76).
Data Analysis
Analyses were conducted using R (R Core Team, 2013) and were aimed at: 1) examining feasibility and acceptability of implementing BTT in a CMHC setting and, 2) assessing feasibility of testing BTT effectiveness by comparing it to TAU in a subsequent fully powered clinical trial. For between group comparisons, t-tests were used to compare continuous variables and Chi-Square or Fisher’s tests were used for categorical variables.
R effsize package (Torchiano, 2016) was used to calculate between- and within-group Hedges g effect sizes to evaluate the magnitude of treatment effects at post-treatment and follow-up. The potential effects of BTT on the main outcome measure (Y-BOCS) and secondary treatment outcome measures (BDI-II, BABS, Q-LES-Q, SOFAS) were examined. To evaluate the clinical significance of the observed effects, we evaluated and compared the number of treatment responders. Consistent with prior research we defined treatment response as a 35% or greater decrease from pretreatment Y-BOCS (Farris et al., 2013; Simpson et al., 2006).
Comparisons between the two groups were made on an Intention-to-Treat (ITT) basis, and then among completers only (n=28). The ITT analyses included all randomized participants that completed baseline assessment procedures. BTT participants were considered treatment completers if they completed individual information-gathering sessions and attended at least 9 out of 12 group ERP sessions. TAU participants who reported that they completed therapy or continued to attend therapy sessions at post treatment were considered to be treatment completers. The proportions of participants from each group classified as treatment responders were compared using fisher’s exact test.
Results
There were no significant differences between groups on demographic and clinical characteristics of participants in the BTT and TAU groups (see Table 1). A comparison of participants with and without missing data also yielded no significant differences in baseline characteristics or in treatment allocation group.
Table 1.
Baseline Demographic and Clinical Characteristics
| BTT (n = 31) | TAU (n =16) | t or χ2 | p | |
|---|---|---|---|---|
| Age-years, M (SD) | 38.09 (10.40) | 38.28 (12.10 | −.05 | .95 |
| Female, n (%) | 22 (67) | 13 (72) | 1.67 | .68 |
| Married, living with partner n (%) | 7 (21) | 2 (11) | 0.81 | .366 |
| Race/Ethnicity, n (%) | 5.42 | .14 | ||
| White (non-Hispanic) | 24 (73) | 8 (44) | ||
| Black (Non-Hispanic) | 5 (15) | 3 (17) | ||
| Hispanic | 2 (6) | 4 (22) | ||
| Other | 2 (6) | 3 (17) | ||
| Education, n (%) | .81 | .84 | ||
| Less than high school | 4 (12) | 3 (17) | ||
| High school diploma/GED | 12 (16) | 5 (28) | ||
| Associate’s degree | 10 (30) | 7 (39) | ||
| Bachelor’s degree or higher | 7 (21) | 3 (17) | ||
| Duration of OCD, years M (SD) | 17.7 (12.7) | 20.0 (14.9) | −0.57 | .57 |
| On SRI, n (%) | 26 (79) | 12 (67) | .90 | .34 |
| Y-BOCS, M (SD) | 28.61 (4.9) | 29.94 (4.1) | −0.99 | .32 |
Note: BTT=Behavioral Therapy Teams; SRI=Serotonin Reuptake Inhibitor; TAU=Treatment As Usual; Y-BOCS=Yale Brown Obsessive Compulsive Scale.
Feasibility of training CMHC staff was partially successful. Overall, eleven (68%) of 16 staff members successfully completed all phases of training. Therapist training was considered successful. All three therapists that initiated training completed all phases of training and delivered therapy sessions throughout the study treatment phase. Observer ratings of videos of therapist sessions also indicated that therapists were able to deliver group ERP with high adherence to the ERP protocol (overall mean adherence rating was 90.6%). Fewer coaches completed training: 13 paraprofessionals initiated ERP coaching training and eight (61%) completed all aspects of the training and were able to deliver the protocol with high fidelity (89.8% across sessions). Two paraprofessionals left the agency prior to completing the training and three completed didactic trainings but were transferred to other departments prior to completing their training cases.
Eleven (78% of TAU participants who completed post-treatment assessments) reported that they received psychotherapy for OCD or anxiety during the active treatment phase. All reported receiving individual, office-based psychotherapy sessions and endorsed use of multiple treatment modalities in treatment sessions. Nine (64%) reported that therapy sessions focused primarily on OCD. Cognitive and dynamic techniques were the most frequently endorsed techniques (57%). Six (42%) reported behavioral methods including four participants (28%) who reported exposure techniques.
Ten TAU therapists completed the PTI at week 16 of the study. Therapist credentials included mental health counselor (40%), clinical social worker (30%), psychologist (20%), and unlicensed clinician/trainee (10%). Most TAU therapists reported that therapy sessions focused on OCD as well as other comorbid conditions and only one therapist reported that OCD was the primary focus of most therapy sessions. TAU therapists reported an average of 11.8 (SD=8.8) sessions but less than half of these sessions (M=4.6, SD=3.8) were focused on OCD treatment. Cognitive methods were the most frequently endorsed techniques (70%) followed by behavioral methods (40%). All four of the TAU therapists who endorsed behavioral methods reported occasional or frequent use of exposure techniques in sessions.
BTT participants were more likely than TAU participants to attend the first treatment session (97% vs 75%, respectively, Fisher’s p=.04) and were less likely to drop out of therapy (22% vs 43%, respectively, χ2 =5.3, p=.02). However, 16% of BTT participants were discontinued from BTT due to worsening of comorbid conditions that required hospitalization. Similarly, 14% of TAU participants reported hospitalization during the active study treatment phase. BTT participants received more sessions of therapy (M=9.7±5.4) than TAU participants (M=3.8±4.3; F = 14.1, p < .01). However, there were no significant differences between groups in number of treatment completers: 61% percent of BTT participants completed at least 9 group ERP sessions and 56% of TAU participants reported completing treatment (or continuing to attend psychotherapy) at the post-treatment assessment.
Thirteen (42%) BTT participants completed at least half of the 10 scheduled individual coaching sessions. Six BTT participants refused individual coaching sessions and preferred to attend group ERP only. Main reasons for refusal were discomfort with allowing someone into their home or beliefs that coaching sessions were not necessary. Eleven participants (58% of BTT completers) attended post-treatment group booster sessions. Main reasons for not attending group booster sessions included scheduling difficulties and dissatisfaction with group size (too small).
Overall, treatment satisfaction was high for both groups at post-treatment and there were no significant differences between groups. The average total score on the CSQ-8 at post-treatment was 27.4 (SD=4.1) for the BTT group and 26.1 (SD=2.4) for the TAU group. BTT participants also reported that they found group therapy sessions to be helpful (M= 3.2, SD = 0.8, range = 1–4) and coaching sessions to be helpful (M = 3.3, SD= 0.8). Clients identified group therapy as helpful:
“doing an exposure with someone. It greatly helped to keep me focused on the task”
“hearing about other people share about their symptoms and struggles alleviated my isolation, guilt, feeling less than.”
“…to be able to talk with other people with OCD and discuss ways to deal with OCD”.
Aspects of group therapy sessions that clients identified as needing improvement included group size, duration of intervention, and a preference for individual therapy:
“group was too small”
“I needed more time. I feel I have just scratched the surface”
“I don’t think it should be a group. It should be one on one all the time”.
Aspects of coaching sessions that clients identified as most helpful included:
“having more one on one time to express my feelings and work on coping skills”
“having my [family] there to help me with coaching sessions helped …all of us.”
“individualized program, at home, encouraged me to push through”
Aspects of coaching sessions that clients identified as needing improvement included:
“I think it depends on your coach. Mine was helpful, kind, truly genuine, caring person. I think other people might not have had the same kind of person as a coach.”
“I did not want to work with a coach. She should mind her own business.”
“My coach did not really understand what I was going through.”
Clinical Outcomes
Descriptive data for clinical outcome measures are shown in Table 2. Results were consistent for analyses conducted on the ITT sample and the treatment completers subset of the sample. Therefore, only results of analyses using the ITT sample are reported. Within-and between group Hedge’s g effect sizes are shown in Table 3.
Table 2.
Outcomes between conditions for Intent-to-Treat sample
| Pre-treatment |
Post-treatment |
Follow-up (3-months) |
Follow-up (6-months) |
|||||
|---|---|---|---|---|---|---|---|---|
| BTT (n = 31) |
TAU (n =16) |
BTT (n = 25) |
TAU (n =14) |
BTT (n = 24) |
TAU (n =15) |
BTT (n = 19) |
TAU (n =11) |
|
| M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | |
|
| ||||||||
| Y-BOCS | 28.2 (4.5) | 29.2 (4.9) | 20.1 (8.0) | 26.0 (8.7) | 23.5 (8.1) | 24.5 (9.9) | 21.8 (9.5) | 24.6 (10.5) |
| BDI-II | 26.1 (11.4) | 26.5 (11.3) | 20.6 (14.7) | 25.4 (14.0) | 22.7 (13.7) | 20.8 (11.1) | 21.4 (11.9) | 17.0 (9.9) |
| BABS | 11.5 (5.6) | 15.2 (5.0) | 9.9 (6.8) | 15.0 (7.8) | 13.4 (4.5) | 13.5 (6.7) | 10.6 (6.6) | 14.8 (6.8) |
| Q-LES-Q | 43.4 (14.3) | 43.0 (13.7) | 46.6 (20.7) | 48.9 (16.0) | 46.4 (14.8) | 52.8 (16.0) | 48.3 (16.8) | 53.8 (17.4) |
| SOFAS | 46.1 (9.4) | 43.9 (7.5) | 48.3 (10.9) | 44.1 (13.3) | 49.3 (11.1) | 46.3 (11.3) | 48.5 (12.9) | 42.2 (15.9) |
Note: BDI-II = Beck Depression Inventory-II; BTT = Behavior Therapy Teams; Q-LES-Q = Quality of Life Enjoyment and Satisfaction Questionnaire (expressed as % of maximum score); SOFAS = Social and Occupational Functioning Scale; TAU = Treatment As Usual; Y-BOCS = Yale Brown Obsessive Compulsive Scale.
Table 3.
Within- and between-group Hedge’s g effect sizes
| Within-group effect sizes [95% CI] |
Between-group effect sizes [95% CI] |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| BTT |
TAU |
BTT vs TAU |
|||||||
| Pre-Post | Pre-3mos | Pre-6mos | Pre-Post | Pre-3mos | Pre-6mos | Post | 3-mos | 6-mos | |
|
| |||||||||
| YBOCS | 1.18 [.56, 1.80] | .60 [.16, 1.04] | .81 [.22, 1.40] | .32 [−.12, .76] | .46 [.02, .89] | .45 [.04, .85] | .83 [.14, 1.53] | .09 [−.57, .75] | .29 [−.46, 1.03] |
| BDI-II | .35 [08, .61] | .33 [−.04, .70] | .56 [−.02, 1.15] | .04 [−.34, .42] | .35 [.11, .81] | .79 [.13, 1.45] | .32 [−.38, 1.02] | −.15 [−.85, .55] | −.38 [−1.18, .43] |
| BABS | .43 [−.02 .88] | .04 [−.28, .35] | .57 [.02, 1.11] | −.05 [−.40, .30] | .27 [−.16, .70] | .12 [−.40, .63] | .69 [−.11, 1.49] | .00 [−.78, .79] | .60 [−.29, 1.5] |
| Q-LESQ | −.14 [−.47, .19] | −.22 [−.64, .21] | −.34 [−.88 .21] | −.20 [−.55, .14] | −.45 [−.96, .07] | −.56 [−.98, -.13] | −.11 [−.58, .81] | .41 [−.29, 1.11] | .32 [−.46, 1.09] |
| SOFAS | −.28 [−.49, -.08] | −.26 [−.50, -.02] | −.13 [−.35, .10] | −.04 [−.36, .29] | −.21 [−.66, .24] | .15 [−.33, .63] | −.35 [−1.00, .31] | −.26 [−.96, .44] | −.43 [−1.53, .68] |
Note: BDI-II = Beck Depression Inventory-II; BTT = Behavior Therapy Teams; Q-LES-Q = Quality of Life Enjoyment and Satisfaction Questionnaire (expressed as % of maximum score); SOFAS = Social and Occupational Functioning Scale; TAU = Treatment As Usual; Y-BOCS = Yale Brown Obsessive Compulsive Scale
OCD symptom severity.
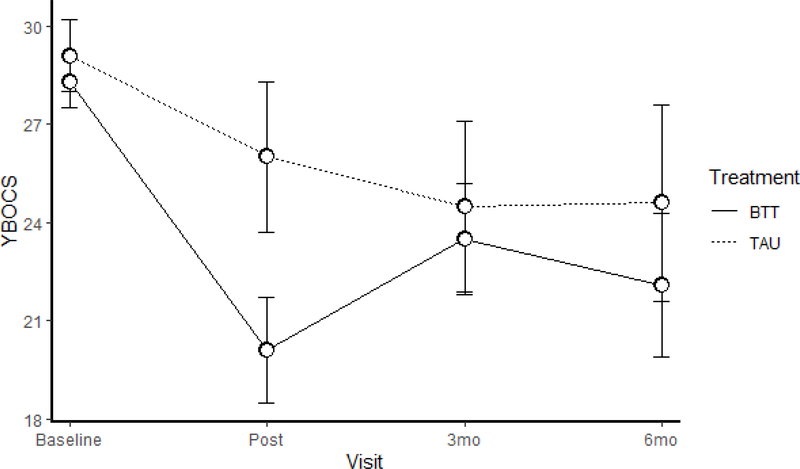
Figure 2 shows changes in Y-BOCS over time. For both groups, Y-BOCS scores were in the severe to extreme range at baseline. For BTT participants, within-group effect sizes for changes in Y-BOCS from baseline to post-treatment were large (see Table 3). However, baseline to follow-up differences fluctuated in magnitude from medium at 3-months post-treatment to large at 6-months post-treatment indicating that treatment gains were not consistently maintained during the follow-up phase of the study. For TAU participants, within-group changes in Y-BOCS from baseline to post-treatment were small in size and remained in this range throughout follow-up. Between-group differences between BTT and TAU favored BTT and ranged from a large effect at post-treatment to a small effect at the 6-month follow-up assessment.
FIG. 2.
Treatment mean profiles and standard errors for scores on the Yale-Brown Obsessive Compulsive Scale (Y-BOCS). TAU, treatment as usual; BTT, Behavioral Treatment Team. Data shown are for baseline, post-treatment, and at 3- and 6- month follow-up.
Twenty-five percent (n=6) of BTT participants who completed post-treatment assessments were classified as treatment responders. All but two participants maintained treatment gains at 3- and 6- month follow-ups. Fourteen percent (n=2) of TAU participants were classified as treatment responders at post-treatment and they also were able to maintain treatment gains at 3- and 6- month follow-up assessments. There were no significant between group differences in proportion of treatment responders.
Secondary clinical outcomes.
Between-group differences in OCD insight (BABS) at post-treatment and 6-month follow-up were medium in size but no differences were observed at the 3-month follow-up. Between-group differences on depression (BDI-II), quality of life (QLESQ) and functioning (SOFAS) ranged from negligible to medium across post-treatment and follow-up assessments. For TAU participants, within-group changes in depression (BDI-II) from baseline to post-treatment were negligible but increased to medium effect at 6-months, indicating that depressive symptoms gradually improved over time. Within-group differences for TAU participants also indicated gradual improvement in quality of life (QLESQ) from baseline to follow-up.
Discussion
This study evaluated a team-based approach (BTT) to delivering ERP in a CMHC setting. Findings suggest that the BTT model is feasible and a promising way of transporting ERP to CMHCs that service low-income populations. Three therapists completed rigorous training and were able to deliver group ERP with high adherence to the ERP protocol. Training paraprofessionals was more challenging due to inner setting factors such as high turnover rates at the agency and frequent reassignment of responsibilities within the agency (i.e. changes in roles or teams). We had difficulty sustaining coaches and needed to train twice as many paraprofessionals than originally anticipated. Only 60% (8/13) of coaches who initiated training were able to actually provide coaching services to BTT participants. These findings underscore the importance of implementation frameworks that utilize pre-implementation assessments of organizational characteristics (e.g. staff turnover, consistency in roles) to help understand how these factors will impact training professionals. Future work investigating more efficient models of training paraprofessionals to integrate exposure principles into the services that they provide to clients with OCD may be more cost-effective. Given the interpersonal challenges that some of the participants expressed in working with a coach, mobile apps or videoconferencing may also be a more cost-effective way of extending therapy sessions in outpatient settings (Boisseau et al., 2017; Vogel et al., 2014).
Overall, ERP appears to be a feasible and acceptable treatment for low-income clients with OCD. BTT participants were less likely to drop-out of therapy prematurely than TAU participants and 76% of BTT participants completed individual pretherapy sessions and attended at least one group therapy session. The somewhat low treatment completion rate for BTT (57%) is reflective of the challenges of delivering ERP to CMHC clients with other serious mental illness. 22% of BTT participants dropped out of treatment prematurely, usually within the first two sessions of individual pretherapy sessions or group therapy. This is slightly higher than dropout rates for ERP in clinical trials (Ong et al., 2016) but significantly less than the 43% self-reported drop-out rate in the TAU condition. Four BTT participants did not complete treatment because they experienced an exacerbation of other psychiatric symptoms which warranted a higher level of care. Although the broad inclusion criteria for this study are intended to recruit a sample that is representative of CMHC clients, it remains unclear how best to treat clients with comorbid Bipolar or Schizophrenia. It is unlikely that ERP exacerbated comorbid conditions as all but one of the clients worsened before entering the group ERP phase of treatment. Future studies may require a longer period (e.g. 3–6 months) of stable comorbid symptoms or stable medication regimens.
To our knowledge, this is the first study to evaluate ERP in a CMHC setting with a diverse sample of patients with severe OCD. More than one-third of the sample identified as an ethnic minority, all were low-income, one-third had concurrent PTSD and 16% had a lifetime history of psychosis or Bipolar disorder. The modest effects of ERP at post-treatment and follow-up assessments are promising but suggest that modifications need to be made in order to have a greater impact on this population. First, there is very little known about the use of ERP in individuals with psychotic or manic symptoms. In this study and in a previous open trial (Mancebo et al. 2017) participants with SMI that entered the group ERP phase were able to complete treatment and reported significant improvement. For patients with OCD and comorbid Bipolar Disorder, SSRIs are not a viable pharmacological option given the risk of inducing mania (Amerio et al., 2014; Math & Reddy, 2007), underscoring the importance of behavioral interventions such as ERP. However, it remains unclear if ERP is indicated for all patients with other comorbid SMI. The inclusion criteria of “one month of stable” symptoms may be too liberal as some patients had to discontinue treatment in the first weeks due to exacerbation of psychosis or suicidal ideation. Future work should examine whether ERP is the treatment of choice for this population or whether other approaches (e.g. Acceptance and Commitment Therapy) may be more beneficial. Second, one-third of our sample also had concurrent PTSD which also presents unique challenges for ERP treatment (Kirk et al., 2018; Ojserkis et al., 2017). Although Prolonged Exposure is also efficacious for PTSD (Foa et al., 2019), these patients may do better in individual treatment than in group ERP.
Consistent with previous controlled studies of ERP, effect size estimates of changes in Y-BOCS from pre-to-post treatment were large. However, treatment gains were not maintained over follow-up assessments and most BTT completers continued to have clinically significant symptoms at post-treatment. This study used a 12 session group therapy protocol that may be inadequate for patients with severe OCD complicated by other comorbid psychiatric conditions. In fact, qualitative data collected at post-treatment interviews indicated that patients believed that more sessions were needed. It remains unclear whether simply adding more sessions would be helpful or whether augmenting group ERP sessions with additional therapeutic interventions (e.g. motivational interviewing) would improve outcomes.
We attempted to use paraprofessional coaches as therapy extenders to boost the “dose” of ERP with home/community-based coaching sessions but surprisingly several BTT participants perceived coaching as yielding low utility or they felt uncomfortable having to work with a different provider. Although BTT participants on average rated coaching sessions to be helpful, these ratings are most likely inflated by selection bias as those participants who attended coaching sessions were more likely to rate them as helpful. This finding is surprising given that ERP coaching is common in residential or intensive OCD specialty programs and is in contrast to results from our initial open trial that indicated that CMHC clients completed coaching and rated it as a very helpful component of treatment (Mancebo et al. 2017). An important difference was that coaches in the open trial were case managers that were already known to BTT participants but in this study, we recruited a larger sample of patients across two sites of the same CMHC and BTT participants were usually assigned to therapists and coaches that they were not familiar with. Initial impressions of coaches were not always positive and we found that we spent quite a bit of time in supervision helping coaches switch from a “case management role” which required them to be more directive to a “coaching role” which was more collaborative and required more nonspecific therapeutic skills such as building rapport, reflective listening, and cultural sensitivity.
This study has several limitations. First, the goal of this pilot study was to establish feasibility and acceptability of implementing methods in a CMHC setting and was not powered to detect treatment differences between groups. However, the overall attrition rate in the BTT group (38%) was almost double than attrition rates reported in ERP efficacy studies. As expected, 22% of BTT participants dropped out of treatment but an additional 16% of participants were discontinued from BTT due to worsening of comorbid conditions. Second, the treatment as usual control group was impacted by changes in state policy that occurred during the first year of study recruitment. The CMHC teams were required to shift to “health home model” which resulted in a reorganization of teams and reassignment of caseloads for our paraprofessionals. This model also led to outsourcing some of the psychotherapy services (to hospital-based clinics and private practice clinicians) and thus TAU psychotherapy may not be representative of the psychotherapy that is delivered in CMHC. Future studies should focus on comparative effectiveness designs to determine which treatments are most cost-effective for this population.
Highlights.
Exposure and Response Prevention was feasible and acceptable to patients.
Therapists were able to deliver Exposure Therapy with high fidelity.
Training coaches was more challenging and only 68% completed training.
Large effect sizes for Behavioral Therapy Teams were observed.
Treatment As Usual was associated with gradual improvement in depression.
Acknowledgements
This work was supported by grant K23 MH091032 from the National Institute of Mental Health to the first author. We would like to thank Drs. Gail Steketee and Jordana Muroff for contributing to the development of the training program and fidelity measures. We would also like to thank the patients, therapists, coaches, and raters that contributed to this project.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association (2000). Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR. American Psychiatric Association. [Google Scholar]
- Amerio A, Odone A, Marchesi C, & Ghaemi SN (2014). Treatment of comorbid bipolar disorder and obsessive-compulsive disorder: A systematic review. Journal of Affective Disorders, 166, 258–263. 10.1016/j.jad.2014.05.026 [DOI] [PubMed] [Google Scholar]
- Bates D, Mächler M, Bolker BM, & Walker SC (2015). Fitting linear mixed-effects models using lme4. Journal of Statistical Software, 67(1),1–48. 10.18637/jss.v067.i01 [DOI] [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Manual for the Beck Depression Inventory-II. Psychological Corporation. [Google Scholar]
- Beck AT, Steer RA, Ball R, & Ranieri W (1996). Comparison of Beck Depression Inventories -IA and -II in psychiatric outpatients. Journal of Personality Assessment, (67), 588–597. 10.1207/s15327752jpa6703_13 [DOI] [PubMed] [Google Scholar]
- Beidas R, Edmunds JM, Marcus S, & Kendall P (2012). Training and consultation to promote implementation of an empirically supported treatment: a randomized trial. Psychiatric Services, 63(7), 660–665. 10.1176/appi.ps.201100401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boisseau CL, Schwartzman CM, Lawton J, & Mancebo MC (2017). App-guided exposure and response prevention for obsessive compulsive disorder: an open pilot trial. Cognitive Behaviour Therapy, 46(6), 447–458. 10.1080/16506073.2017.1321683 [DOI] [PubMed] [Google Scholar]
- Carter MM, Mitchell FE, & Sbrocco T (2012). Treating ethnic minority adults with anxiety disorders: current status and future recommendations. Journal of Anxiety Disorders, 26(4), 488–501. 10.1016/j.janxdis.2012.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisen JL, Goodman WK, Keller MB, Warshaw MG, DeMarco LM, Luce DD, & Rasmussen SA (1999). Patterns of remission and relapse in obsessive-compulsive disorder: a 2-year prospective study. The Journal of Clinical Psychiatry, 60(5), 346–351; 10.4088/JCP.v60n0514 [DOI] [PubMed] [Google Scholar]
- Eisen JL, Phillips KA, Baer L, Beer DA, Atala KD, & Rasmussen SA (1998). The Brown Assessment of Beliefs Scale: Reliability and validity. American Journal of Psychiatry, 155(1), 102–108. 10.1176/ajp.155.1.102 [DOI] [PubMed] [Google Scholar]
- Eisen JL, Sibrava NJ, Boisseau CL, Mancebo MC, Stout RL, Pinto A, & Rasmussen SA (2013). Five-year course of obsessive-compulsive disorder: Predictors of remission and relapse. Journal of Clinical Psychiatry, 74(3), 233–239. 10.4088/JCP.12m07657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Endicott J, Nee J, Harrison W, & Blumenthal R (1993). Quality of Life Enjoyment and Satisfaction Questionnaire: a new measure. Psychopharmacology Bulletin, 29(2), 321–326. 10.1111/j.1365-2850.2011.01735.x [DOI] [PubMed] [Google Scholar]
- Farris SG, Mclean CP, Van Meter PE, Simpson HB, & Foa EB (2013). Treatment response, symptom remission, and wellness in obsessive-compulsive disorder. The Journal of Clinical Psychiatry, 74, 685–690. 10.4088/jcp.12m07789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JBW (2002). Structured clinical interview for DSM-IV-TR axis I disorders, research version, patient edition. (SCID-I/P). Biometrics Research, New York State Psychiatric Institute. [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JBW, & Benjamin LS (1997). Structured clinical interview for DSM-IV axis II personality disorders (SCID-II). American Psychiatric Press. [Google Scholar]
- Fisher PL, & Wells A (2005). How effective are cognitive and behavioral treatments for obsessive-compulsive disorder? A clinical significance analysis. Behaviour Research and Therapy, 43, 1543–1558. 10.1016/j.brat.2004.11.007 [DOI] [PubMed] [Google Scholar]
- Foa EB, Liebowitz MR, Kozak MJ, Davies S, Campeas R, Franklin ME, Huppert JD, Kjernisted K, Rowan V, Schmidt AB, Simpson HB & Tu X (2005). Randomized, placebo-controlled trial of exposure and ritual prevention, clomipramine, and their combination in the treatment of obsessive-compulsive disorder. American Journal of Psychiatry, 162(1), 151–161. 10.1176/appi.ajp.162.1.151 [DOI] [PubMed] [Google Scholar]
- Foa EB, Hembree EA, Rothbaum BO, & Rauch SAM (2019). Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences (2nd ed). Oxford University Press. [Google Scholar]
- Foa EB, Simpson HB, Rosenfield D, Liebowitz MR, Cahill SP, Huppert JD, Bender J, McLean CP, Maher MJ, Campeas R, Hahn C, Imms P, Pinto A, Powers MB, Rodriguez CI, VanMeter PE, Vermes D & Williams MT (2015). Six-month outcomes from a randomized trial augmenting serotonin reuptake inhibitors with exposure and response prevention or risperidone in adults with obsessive-compulsive disorder. Journal of Clinical Psychiatry, 76(4), 440–446. 10.4088/JCP.14m09044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa EB, Yadin E, & Lichner TK (2015). Exposure and Response (Ritual) Prevention for Obsessive Compulsive Disorder: Therapist Guide. Oxford University Press. 10.1093/med:psych/9780195335286.001.0001 [DOI] [Google Scholar]
- Goisman RM, Warshaw MG, & Keller MB (1999). Psychosocial treatment prescriptions for generalized anxiety disorder, panic disorder, and social phobia, 1991–1996. The American Journal of Psychiatry, 156(11), 1819–1821. [DOI] [PubMed] [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, Henniger GR & Charney DS (1989a). The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Archives of General Psychiatry, Vol. 46, pp. 1006–1011. 10.1001/archpsyc.1989.01810110048007 [DOI] [PubMed] [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Delgado P, Heninger GR, & Charney DS (1989b). The Yale-Brown Obsessive Compulsive Scale. II. Validity. Archives of General Psychiatry, 46(11), 1012–1016. 10.1001/archpsyc.1989.01810110054008 [DOI] [PubMed] [Google Scholar]
- Harned MS, Dimeff LA, Woodcock EA & Contreras I (2013). Predicting adoption of exposure therapy in a randomized dissemination trial. Journal of Anxiety Disorders, 27(8), 754–762. 10.1016/j.janxdis.2013.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harned MS, Dimeff LA, Woodock EA, Kelly T, Zavertnik J, Contrearas I & Danner SM (2014). Exposing clinicians to exposure: A randomized dissemination trial of exposure therapy for anxiety disorders. Behavior Therapy, 45(6), 731–744. 10.1016/j.beth.2014.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill J & Gelman A (2006). Data Analysis Using Regression and Multilevel/Hierarchical Models. Cambridge University Press. [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, & Walters EE (2005). Lifetime Prevalence and age-of-onset distributions of. Archives of General Psychiatry, 62, 593–602. 10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- Koran LM, Hanna GL, Hollander E, Nestadt G, Simpson HB, & American Psychiatric Association (2007). Practice guideline for the treatment of patients with obsessive-compulsive disorder. American Journal of Psychiatry, 164(7 Suppl), 5–53. [PubMed] [Google Scholar]
- Kozak MJ, & Foa EB (1997). Mastery of Obsessive-Compulsive Disorder: A cognitive-behavioral approach. Graywind Publications. [Google Scholar]
- Larsen DL, Attkisson CC, Hargreaves WA, & Nguyen TD (1979). Assessment of client/patient satisfaction: development of a general scale. Evaluation and Program Planning, 2(3), 197–207. 10.1016/0149-7189(79)90094-6 [DOI] [PubMed] [Google Scholar]
- Little RJ, D’Agostino R, Cohen ML, Dickersin K, Emerson SS, Farrar JT, Frangakis C, Hogan JW, Molenberghs G, Murphy SA, Neaton JD, Rotnitzky A, Scharfstein D, Shih WJ, Siegel JP, & Stern H (2012) The prevention and treatment of missing data in clinical trials. New England Journal of Medicine, 357(14): 1355–1360. 10.1056/NEJMsr1203730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mancebo MC, Eisen JL, Pinto A, Greenberg BD, Dyck IR, & Rasmussen SA (2006). The Brown Longitudinal Obsessive Compulsive Study: Treatments received and patient impressions of improvement. Journal of Clinical Psychiatry, 67(11), 1713–1720. 10.4088/JCP.v67n1107 [DOI] [PubMed] [Google Scholar]
- Mancebo MC, Steketee G, Muroff J, Rasmussen SA & Zlotnick C (2017). Behavioral therapy teams for adults with OCD in a community mental health center: An open trial. Journal of Obsessive-Compulsive and Related Disorders, 13, 18–23. 10.1016/j.jocrd.2017.03.002 [DOI] [Google Scholar]
- Math SB, & Reddy JYC (2007). Issues in the pharmacological treatment of obsessive-compulsive disorder. International Journal of Clinical Practice, 61(7), 1188–1197. 10.1111/j.1742-1241.2007.01356.x [DOI] [PubMed] [Google Scholar]
- Matthews JNS, Altman DG, Campbell MJ, & Royston P (1990). Analysis of serial measurements in medical research. BMJ 1990; 300:230–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Research Council. (2010). The Prevention and Treatment of Missing Data in Clinical Trials. Panel on Handling Missing Data in Clinical Trials. Committee on National Statistics, Division of Behavioral and Social Sciences and Education. The National Academies Press. [Google Scholar]
- Nguyen TD, Attkisson CC, & Stegner BL (1983). Assessment of patient satisfaction: development and refinement of a service evaluation questionnaire. Evaluation and Program Planning, 6(3–4), 299–313. 10.1016/0149-7189(83)90010-1 [DOI] [PubMed] [Google Scholar]
- Ong CW, Clyde JW, Bluett EJ, Levin ME, & Twohig MP (2016). Dropout rates in exposure with response prevention for obsessive-compulsive disorder: What do the data really say? Journal of Anxiety Disorders, 40, 8–17. 10.1016/j.janxdis.2016.03.006 [DOI] [PubMed] [Google Scholar]
- Ojserkis R, Boisseau CL, Reddy MK, Mancebo MC, Eisen JL, & Rasmussen SA (2017). The impact of lifetime PTSD on the seven-year course and clinical characteristics of OCD. Psychiatry Research, 258, 78–82. 10.1016/j.psychres.2017.09.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen SA, & Eisen JL (1992). The epidemiology and clinical features of obsessive compulsive disorder. The Psychiatric Clinics of North America, 15(4), 743–758. [PubMed] [Google Scholar]
- R Core Team (2013). R: A language and environment for statistical computing. R Foundation for Statistical Computing. https://www.R-project-org [Google Scholar]
- Simpson HB, Huppert JD, Petkova E, Foa EB, & Liebowitz MR (2006). Response versus remission in obsessive-compulsive disorder. The Journal of Clinical Psychiatry, 67(2), 269–276. 10.4088/jcp.v67n0214 [DOI] [PubMed] [Google Scholar]
- Steketee G, Eisen J, Dyck I, Warshaw M, & Rasmussen S (1999). Predictors of course in obsessive-compulsive disorder. Psychiatry Research, 89(3), 229–238. 10.1016/S0165-1781(99)00104-3 [DOI] [PubMed] [Google Scholar]
- Steketee G, Perry JC, Goisman RM, Warshaw MG, Massion AO, Peterson LG, Langford L, Weinshenker N, Farreras IG, & Keller MB (1997). The psychosocial treatments interview for anxiety disorders. A method for assessing psychotherapeutic procedures in anxiety disorders. Journal of Psychotherapy Practice & Research, 6(3), 194–210. [PMC free article] [PubMed] [Google Scholar]
- Stewart RE, & Chambless DL (2009). Cognitive–behavioral therapy for adult anxiety disorders in clinical practice: A meta-analysis of effectiveness studies. Journal of Consulting and Clinical Psychology, 77(4), 595–606. 10.1037/a0016032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stirman SW, Gutner CA, Langdon K, & Graham JR (2015). Bridging the gap between research and practice in mental health service settings: An overview of developments in implementation theory and research. Behavior Therapy, 47(6), 920–936. 10.1016/j.beth.2015.12.001 [DOI] [PubMed] [Google Scholar]
- Sullivan TR, White IR, Salter AB, Ryan P, & Lee KJ (2018). Should multiple imputation be the method of choice for handling missing data in randomized trials? Statistical Methods in Medical Research, 27(9):2619–2626. 10.1177/0962280216683570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolin DF, Frost RO, Steketee G, & Muroff J (2015). Cognitive behavioral therapy for hoarding disorder: A meta-analysis. Depression and Anxiety, 32(3), 158–166. 10.1002/da.22327 [DOI] [PubMed] [Google Scholar]
- Torchiano M (2016). Effsize: a package for efficient effect size computation. doi: 10.5281/zenodo.1480624, R package version 0.8.1, https://CRAN.R-project.org/package=effsize. [DOI] [Google Scholar]
- U.S. Department of Health and Human Services. (2008). HHS Poverty Guidelines. Retrieved May 28, 2009, from https://aspe.hhs.gov/2008-hhs-poverty-guidelines
- Van Kirk N, Fletcher TL, Wanner JL, Hundt N, & Teng EJ (2018). Implications of comorbid OCD on PTSD treatment: A case study. Bulletin Menninger Clinic, 82(4), 344–359. 10.1521/bumc.2018.82.4.344 [DOI] [PubMed] [Google Scholar]
- Van Noppen BL, Pato MT, Marsland R, & Rasmussen SA (1998). A time-limited behavioral group for treatment of obsessive-compulsive disorder. The Journal of Psychotherapy Practice and Research, 7(4), 272–280. [PMC free article] [PubMed] [Google Scholar]
- Vogel PA, Solem S, Hagen K, Moen EM, Launes G, Håland ÅT, Hansen B, & Himle JA (2014). A pilot randomized controlled trial of videoconference-assisted treatment for obsessive-compulsive disorder. Behaviour Research and Therapy, 63, 162–168. 10.1016/j.brat.2014.10.007 [DOI] [PubMed] [Google Scholar]
- Wade W, Treat T & Stuart GL (1998). Transporting an empirically supported treatment for panic disorder to a service clinic setting: a benchmarking strategy. Journal of Consulting and Clinical Psychology, 66(2), 231–239. 10.1037/0022-006X.66.2.231 [DOI] [PubMed] [Google Scholar]
- Weissman MM, Bland RC, Canino GJ, Greenwald S, Hwu HG, Lee CK, Newman SC, Oakley-Browne MA, Rubio-Stipec M, Wickramaratne PJ, Wittchen H-U, & Yeh E-K (1994). The cross-national epidemiology of obsessive compulsive disorder. Journal of Clinical Psychiatry, 55 (suppl. 3), 5–10. [PubMed] [Google Scholar]