Abstract
Introduction
The provision of quality health care during the COVID-19 pandemic depends largely on the health of health care providers. However, healthcare providers as the frontline caregivers dealing with infected patients, are more vulnerable to mental health problems. Despite this fact, there is scarce information regarding the mental health impact of COVID-19 among frontline health care providers in South-West Ethiopia.
Objective
This study aimed to determine the levels and predictors of anxiety, depression, and stress during the COVID-19 pandemic among frontline healthcare providers in Gurage zonal public hospitals, Southwest Ethiopia, 2020.
Methods
An institutional-based cross-sectional study was conducted among 322 health care providers from November 10–25, 2020 in Gurage zonal health institutions. A simple random sampling technique was used to select the study participants. A pretested self -administered structured questionnaire was used as a data collection technique. The data were entered into the Epi-data version 3.01 and exported to SPSS version 25.0 for analysis. Both descriptive statistics and inferential statistics (chi-square tests) were presented Bivariable and Multivariable logistic regression analyses were made to identify variables having a significant association with the dependent variables.
Results
The results of this study had shown that the overall prevalence of anxiety, depression and stress among health care providers during the COVID-19 pandemic was 36%, [95% CI = (30.7%- 41.3%)], 25.8% [95% CI = (21.1%- 30.4%)] and 31.4% [95% CI = (26.4%- 36.0%)] respectively. Age, Adjusted Odds Ratio [AOR = 7.9], Educational status, [AOR = 3.2], low monthly income [AOR = 1.87], and presence of infected family members [AOR = 3.3] were statistically associated with anxiety. Besides this, gender, [AOR = 1.9], masters [AOR = 10.8], and degree holder [AOR = 2.2], living with spouse [AOR = 5.8], and family [AOR = 3.9], being pharmacists [AOR = 4.5], and physician [AOR = (0.19)], were found to be statistically significant predictors of depression among health care providers. Our study finding also showed that working at general [AOR = 4.8], and referral hospitals [AOR = 3.2], and low monthly income [AOR = 2.3] were found to be statistically significant predictors of stress among health care providers.
Conclusion
Based on our finding significant numbers of healthcare providers were suffered from anxiety, depression, and stress during the COVID-19 outbreak. So, the Government and other stakeholders should be involved and closely work and monitor the mental wellbeing of health care providers.
Introduction
Coronavirus (CoV) infections are emerging respiratory viruses that are known to cause illnesses ranging from the common cold to severe acute respiratory syndrome (SARS) [1]. As of January 30th, 2020, the “World Health Organization” (WHO) characterized the ongoing COVID-19 outbreak as a “Public Health Emergency of International Concern” (PHEIC) [2], and later, due to uncased fast spread, the severity of illness, the continual escalation in several affected countries, cases and causalities, WHO declared coronavirus disease 2019 (COVID-19) a global pandemic on 11 March 2020 [3].
The pandemic could have severe effects on the mental health of the general population and health care providers(HCPS) [4]. As a result, people have been comparing the emergence of a novel Coronavirus (2019-nCoV) to “the end of the world,” and the whole world reacts to the event with panic, insomnia, stress, irritability, and feelings of distractibility [5].
Healthcare providers are always at the forefront in the response to emerging infectious disease outbreaks which are encountering many sources of stress, and recent evidence showed that the COVID-19 pandemics can undermine not only physical health but also take a toll on these providers’ mental health and resilience [6, 7]. In a Chinese study, researchers found that a considerable proportion of participants reported symptoms of anxiety (44.6%), moderate to severe depression (50.4%), insomnia (34%), and moderate to severe psychological distress (71.5%) [8]. In addition to this, studies carried out in Italy revealed that 50.1% of participants reported symptoms of clinically relevant anxiety, 26.6% symptoms of depression and 53.8% showed symptoms of post-traumatic distress [9].
Mental health and psychosocial consequences of the COVID-19 pandemic may be particularly serious for health professionals because HCPs often have to respond to demanding and unforeseen medical emergencies [10]. In the initial phase of the SARS-CoV-2 outbreak, 29% of all hospitalized patients were HCPs [11]. A recent report from the International Council of Nurses (ICN), found that health worker infections ranged from 1–32% of all confirmed COVID-19 cases [12].
Globally, there have been more than 230,920,739 infections and 4,733,350 fatalities after the declaration of the pandemic by the WHO. In Africa, there are about 8,269,298 confirmed cases and 207,760 deaths reported as of September 23 /2021 [13]. According to the Amnesty International report, 17,000 health workers have died worldwide from COVID-19 over the last year, which implied that one health care worker was dying every 30 minutes, which was a “tragedy and an injustice” [14].
Ethiopia is one of the countries threatened by COVID- 19, with a total of 336,762 confirmed cases and 5,254 registered deaths as of September 23/2021 [13]. It is now the leading country in East Africa with the highest number of infected people. Thousands of HCPs have been infected with COVID-19 [15]. To minimize the risk of COVID-19 transmission in the community, the Ethiopian government declared an emergency and mandated compulsory physical distancing, the establishment of isolation and quarantine centers for suspected and confirmed cases, the activation of the Federal Emergency Operation Center, frequent hand washing, temporary closure of schools and higher education institutions, establishing alternative working modalities for public servants, and the suspension of mass gatherings [16, 17]. Despite the ongoing preventative and control measures, containing the spread of the virus could be challenging in light of the underlying social and infrastructural settings of the country.
The global COVID-19 pandemic has created a massive public health crisis and several challenges for healthcare providers [6]. The social, economic, and health effects are extensive, where they are related to increased all-cause mortality, occupational disability, poor quality of life, and cardiovascular disease risk [18]. Despite its multiple consequences, mental health is often neglected as a public health agenda [19].
The psychological effects related to the current pandemic are caused by numerous factors, including competency concerns when redeployed without adequate training, uncertainty about the duration of the crisis, misleading information about the effectiveness of the vaccine, depletion of personal protection equipment, feelings of being inadequately supported, the hefty workload, the need to take stressful precautions during the medical examination/ in the operative fields and frequent exposure to patients’ suffering and dying [10, 20–24].
Studies also showed that those health care workers who feared contagion and infection of their family, friends, and colleagues felt uncertainty and stigmatization [25, 26], reported reluctance to work or contemplate resignation and reported experiencing high levels of stress, anxiety, and depression symptoms which could have long term psychological implications. Similar concerns about the mental health, psychological adjustment, and recovery of health care workers treating and caring for patients with COVID-19 are now arising [25, 27].
To decrease the extent of the psychological consequences, some measures are taken such as avoiding intense exposure to COVID-19 media coverage, providing resilience training for HCPs, maintaining a compassionate and positive lifestyle by providing support to others [28]. Besides this, WHO called for action to address the immediate needs and measures needed to save lives and prevent a serious impact on the physical and mental health of healthcare providers [29].
A number of research articles published over the past few months showed that a significant proportion of healthcare providers who worked within primary, secondary, and tertiary hospitals developed adverse mental outcomes while providing service for the needy population [30–34]. Despite this fact, sufficient information is not available regarding the mental health impact of COVID-19 among frontline health care providers in South-West Ethiopia. So, the current study aimed to determine the levels and determinants of anxiety, depression, and stress among frontline healthcare providers in Gurage zonal public hospitals.
Methods and materials
Study design
An institutional-based cross-sectional study design was conducted.
Study period and area
The study was conducted in the Gurage zonal public health institutions of SNNPRE from October–December / 2020. Gurage Zone is one of the fifteen zones and four special woredas found in SNNPR state. Wolkite town is the capital of Gurage zone which is located 158 Km southwest of Addis Ababa and 260 Km from Hawasa. It has 20 woreda and two municipalities. According to the 2012 population projection by CSA the total population is 1,767,518.
There are seven hospitals in the Gurage zone. Five of the hospitals in the zone are primary hospitals, one general hospital and the remaining one is a specialized comprehensive hospital, there are 79 health centers (7 are NGO HC) and 444 Functional health posts serving the total population in the zone. There is also a COVID-19 testing center; some hospitals are readily organized to serve quarantine and treatment centers [35].
Source populations
All health care providers who are working in the selected public health institutions.
Study population
The randomly selected health care providers from the selected public health institution
Inclusion criteria
All health care providers who are working in the selected public health institutions.
Exclusion criteria
Those health care providers who are mentally/critically ill and on annual leave were excluded from the study.
Sample size
The minimum sample size was determined by using a single population proportion formula [n = [(Za/2)2.P (1-P)]/d2] by assuming a 95% confidence level (Z a/2 = 1.96), a margin of error of 5%, P = proportion health care providers who are anxious in Southern Ethiopia (29.3%) [36] and a 5% addition for non-response rate. The final sample size became 334.
Sampling technique and procedure
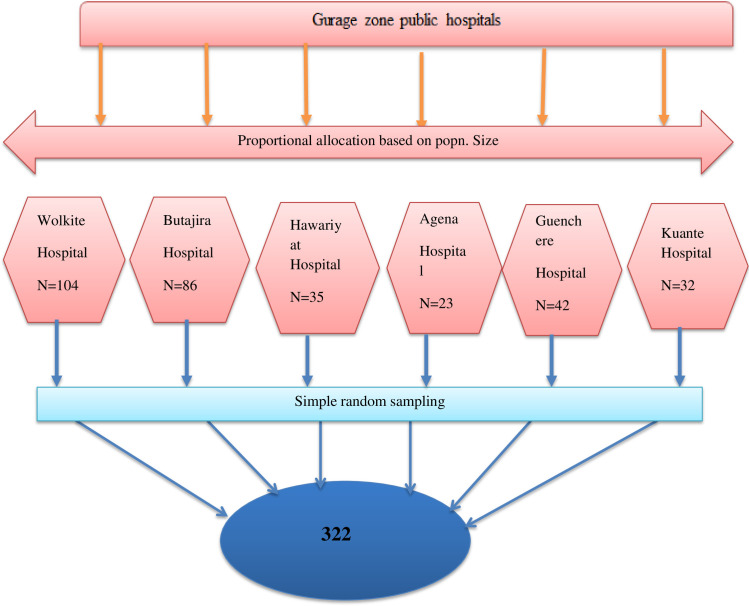
Six public hospitals were included in the study. The sample size in each hospital was allocated proportionally to the number of health professionals. The study participants were selected using simple random sampling techniques. Within each hospital, the sample was taken from each department based on the proportion of their health professionals (Fig 1).
Fig 1. The schematic presentation of the sampling procedure to select the study participants in Gurage zonal public hospital, SNNPR, Ethiopia, 2020 (n = 322).
Variables
Dependent variable
Anxiety, Depression, Stress.
Independent variable
Age, gender, religion, ethnicity, levels of education, marital status, job category, residence, monthly income, work experience, working setup, presence of infected colleague, presence of infected family members.
Data collection instrument (tools) and procedure
Data were collected through a pre-tested, structured, and self-administered questionnaire to assess for symptoms of anxiety, depression, and stress using Amharic versions of validated and reliable measurement tools [37, 38].
The questionnaire consisted of five main themes: 1) demographics, which surveyed participants’ socio-demographic information, including gender, age, educational status, marital status, ethnicity, and monthly income, 2) Occupational and personal-related characteristics of the participant such as job description, working setup, working experience, types of hospital, living condition, presence of suspected or confirmed colleagues and family members.
The third part comprised 7 items to assess the symptoms of anxiety by the Generalized Anxiety Disorder Scale (GAD 7-Scale) that contains a self-rated 7-item that asks for how often the participants have been bothered with the indicators over the past 2 weeks on a 4-point Likert scale, ranging from 0 (not at all) to 3 (nearly every day). The total GAD-7 score for the 7 items ranges from 0 to 21 and is classified as normal (0–4), mild (5–9), moderate (10–14), and severe (15–21) [39].
The fourth part comprised 9 items to assess symptoms of depression by the Patient Health Questionnaire (PHQ-9), a self-rated 9-item scale that asks if the participants have experienced symptoms of depression in the previous two weeks rated on a 4-point Likert-type scale ranging from 0 (not at all) to 3 (nearly every day). The total PHQ-9 scores range from 0 (absence of depressive symptoms) to 27 (most severe depressive symptoms) and classified into 0–4 = “Minimal depression,” 5–9 = “Mild depression,” 10–14 = “Moderate depression,” 15–19 = “Moderately severe depression,” and 20–27 = “Severe depression” [40, 41].
The fifth parts focus on the 10-item Perceived Stress Scale (PSS) which assesses the participants’ perceived psychological stress by rating their feelings and thoughts during the past month. Participants are asked to rate their levels of agreement on a 5-point Likert-type scale ranging from 0 (never) to 4 (very often). It consists of two subscales, including a 6-item positive factor asking the ability to manage the stressors and a 4-item negative factor. The summation scores range from 0–40 with a higher score indicating a higher level of stress. The scores from 0–13 indicate low stress, whereas scores from 14–26 and 27–40 indicate moderate and high levels of stress, respectively [42]. The cutoff score for detecting clinically significant anxiety, depression, and stress were 7, 10, and 21, respectively [40, 43, 44]. Participants who had scores greater than the cutoff threshold were characterized as having severe symptoms.
Data quality assurance and control
Data was collected from different healthcare workers in their respective wards using paper-based questionnaires. A questionnaire was developed and tested for reliability and validity and accordingly; the Cronbach alpha coefficient was found to be 0.88, 0.92, and 0.83 for anxiety, depression, and stress respectively. In addition, a pretest was done before actual data collection on 5% of a similar population in one hospital not included in actual data collection to assess flow, readability, and clarity of the questionnaire.
Eight data collectors and two supervisors were recruited for data collection, who have experience in data collection. To keep data quality supervisors and data collectors were oriented on how and what information they should collect from the targeted data sources. The completeness and consistency of the collected data were checked daily during data collection by the supervisor and the principal investigator. Whenever there appear incompleteness and ambiguity of recording, the filled information formats were crosschecked with source data soon. Individual records with incomplete data were also excluded.
Data processing and analysis
The data was cleaned, coded, and entered into EpiData 3.1 and then exported to SPSS version 25.0 statistical package for further analysis. Data cleaning was performed to check for accuracy, consistencies, and missing values and variables.
Descriptive statistics and inferential statistics (chi-square tests) were carried out to illustrate the percentage and frequencies of study variables. Both bivariable and multivariable analyses were used to see the association of different variables. Those variables which revealed a statistically significant value at a p-value of ≤0.25 in the bivariable analysis were selected for multivariable logistic regression. For model fit, Hosmer and Lemeshow test was carried out and found to be 0.28, 0.398, and 0.587 for anxiety, depression, and stress respectively which indicated the final model was well fitted and multi-collinearity was also assessed. An adjusted odds ratio with a 95% confidence interval was used to measure the degree of association between variables. A P-value of ≤ 0.05 was considered statistically significant during multivariable logistic regression.
Ethical considerations
Ethical Clearance approval was obtained from Wolkite University, Ethical Review Committee. Then data was collected after getting an official letter from the Zonal health department and permission from the medical director of each Hospital. The purpose of the study was explained to the study participants; anonymity, privacy, and confidentiality were ensured. Before data collection, informed verbal consent was obtained from the study participants. The respondents’ right to refuse or withdraw from participating in the study was also fully acknowledged. Results
Socio-demographic characteristics of the respondents
There were 322 study participants involved in the study with a response rate of 96.5%. The highest proportion of respondents 157 (48.8%) were within the age group of 26–30 years with a mean age of 28.71 with SD 5.288. It showed that there was nearly equal participation of males (51.9%) and females (48.1). around two-thirds of the participants were Gurage (64.6%) followed by Amhara (17.1%) and Oromo (10.2%). Half of the participants were orthodox Christian and 56.5% of the participants were married. Regarding the educational status of the respondents, 57.8% (186) were degree holders followed by 34.2% (110) diploma (Table 1).
Table 1. Socio-demographic information about health care providers in Gurage Zone, SNNPR, South West, Ethiopia, 2020.
| Variables | Categories | Number | Percent |
|---|---|---|---|
| Age | 18–25 | 92 | 28.6 |
| 26–30 | 157 | 48.8 | |
| 31–40 | 60 | 18.6 | |
| >40 | 13 | 4.0 | |
| Sex | Male | 167 | 51.9 |
| Female | 155 | 48.1 | |
| Religion | Orthodox | 160 | 49.7 |
| Muslim | 93 | 28.9 | |
| Protestant | 51 | 15.8 | |
| Catholic | 15 | 4.7 | |
| Other | 3 | .9 | |
| Marital status | Married | 182 | 56.5 |
| Single | 140 | 43.5 | |
| Ethnicity | Gurage | 208 | 64.6 |
| Oromo | 33 | 10.2 | |
| Amhara | 55 | 17.1 | |
| Tigre | 4 | 1.2 | |
| Others | 22 | 6.8 | |
| Educational status | Diploma | 110 | 34.2 |
| Degree | 186 | 57.8 | |
| Master’s Degree and above | 26 | 8.1 | |
| Average monthly income | Low | 142 | 44.1 |
| High | 180 | 55.9 |
Occupational and personal-related characteristics of the respondents
Concerning job description, more than one–thirds (35.1%) of the participants were nurses followed by the pharmacy (11.8%) and general practitioner (11.5%). Around two-thirds (66.1%) of the participants had ≤5 years of working experience with a mean experience of 4.7925 SD 3.58.one-thirds of the participants (34.5%) were employed at General Hospital. Nearly half of the participants (47.2%) of health care providers were living with their spouses. Most of the health care providers were practiced at the medical ward (13.3%) and POD followed by the emergency ward (11.8%) (Table 2).
Table 2. Occupational and personal-related characteristics of health care providers in Gurage Zone, SNNPR, South West, Ethiopia, 2020.
| Variables | Categories | Number | Percent |
|---|---|---|---|
| Job description | Nurse | 113 | 35.1 |
| Physicians | 44 | 13.7 | |
| Midwifery | 34 | 10.6 | |
| Pharmacy | 38 | 11.8 | |
| Lab Tech | 16 | 5.0 | |
| HO | 34 | 10.6 | |
| Environmental Health | 10 | 3.1 | |
| Others | 33 | 10.2 | |
| Living condition | Spouse | 152 | 47.2 |
| Family | 37 | 11.5 | |
| Friends | 7 | 2.2 | |
| Alone | 126 | 38.8 | |
| Year of service (Experience) | ≤5 | 213 | 66.1 |
| >5 | 109 | 33.9 | |
| Working setup | Emergency | 38 | 11.8 |
| Medical Ward | 43 | 13.3 | |
| Ophthalmology | 10 | 3.1 | |
| Surgical Ward | 25 | 7.7 | |
| Oby/Gyne ward | 33 | 10.2 | |
| Pediatric | 23 | 7.1 | |
| Medical Adult OPD | 43 | 13.3 | |
| Psychiatry OPD | 2 | .6 | |
| Dental Clinic | 1 | .3 | |
| Triage | 13 | 4.0 | |
| Pharmacy | 31 | 9.6 | |
| Laboratory | 15 | 4.6 | |
| OR | 8 | 2.5 | |
| ICU | 4 | 1.2 | |
| Others | 33 | 10.2 | |
| Types of hospital | Primary | 85 | 26.4 |
| General | 111 | 34.5 | |
| Referral | 47 | 14.6 | |
| Isolation center | 79 | 24.5 | |
| Presence of infected colleagues | Yes | 96 | 29.7 |
| No | 226 | 70.0 | |
| Presence of infected family member | Yes | 38 | 11.8 |
| No | 284 | 87.9 |
Prevalence of anxiety among health care providers in Gurage Zone, SNNPR, South West, Ethiopia, 2020
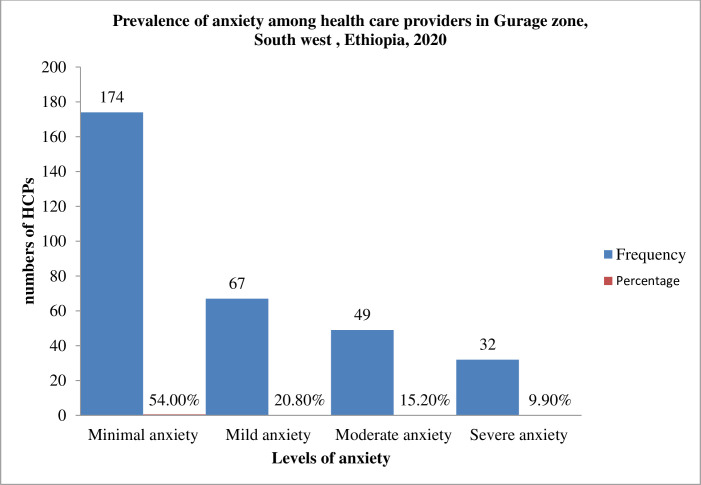
Table 3 shows the respondent’s responses to the 7 items of the GAD-7. Through the past 2 weeks before the study. These respondents responded honestly to the following as occurring for several days, more than half the days, or nearly every day. worrying too much about different things (52.5%); trouble relaxing (50.6%); feeling afraid as if something awful might happen (50.3%); being so restless that it is hard to sit still (48.8%); becoming easily annoyed or irritable (42.2%); not being able to stop or control worrying (38.8%); and feeling nervous, anxious or on edge (36.3%). Based on our findings 174(54%) of health care providers had minimal anxiety, 67(20.8%) had mild anxiety, 49(15.2%) had moderate anxiety and 32(9.9%) had severe anxiety.
Table 3. Prevalence of anxiety among health care providers in Gurage Zone, SNNPR, South West, Ethiopia, 2020.
| Variables | Categories | |||
|---|---|---|---|---|
| Not at all number (%) | under half the days | over half the days | nearly every day | |
| Number (%) | Number (%) | |||
| Number (%) | ||||
| Feeling nervous, anxious, or on edge | 205 (63.7) | 61 (18.9) | 29 (9.0) | 27 (8.4) |
| Not being able to stop or control worrying | 197 (61.2) | 63 (19.6) | 31 (9.6) | 31 (9.6) |
| Worrying too much about different things | 153 (47.5) | 84 (26.1) | 50 (15.5) | 35 (10.9) |
| Trouble relaxing | 159 (49.4) | 70 (21.7) | 59 (18.3) | 34 (10.6) |
| Being so restless that it’s hard to sit still | 165 (51.2) | 83 (25.8) | 44 (13.7) | 30 (9.3) |
| Becoming easily annoyed or irritable | 186 (57.8) | 75 (23.3) | 37 (11.5) | 24 (7.5) |
| Feeling afraid as if something awful might happen | 160 (49.7) | 75(23.3) | 55(17.1) | 32(9.9%) |
For descriptive purposes only, a cutoff of ≥7 was used to distinguish severity for anxiety.so.116 (36%) of health care providers had a generalized anxiety disorder (Fig 2).
Fig 2. Prevalence of anxiety among health care providers in Gurage Zone, SNNPR, South West, Ethiopia, 2020 (n = 322).
Factors associated with anxiety among health care providers in Gurage Zone, SNNPR, South West, Ethiopia, 2020
Bivariable and multivariable logistic regression analysis was conducted to see the presence of association and to measure the relative effect of each independent variable on Generalized Anxiety Disorder among health care providers. Age, gender, religion, marital status, educational status, ethnicity, occupation, types of health facility, monthly income, experience, presence of infected colleague and family were significant factors associated with Anxiety among health care providers.
Among fitted variables included in the binary regression model for bivariable analysis, Age, religion, educational status, marital status, monthly income, experience, and presence of infected family were variables taken into consideration for multivariable analysis with p-value < 0.25. Under multivariable analysis, age, Educational status, monthly income, and presence of infected family were found to be statistically significant predictors of Anxiety among health care providers.
Health care providers whose age >40 years old were significantly more likely to develop anxiety than health care providers whose age 18–25 years old [AOR = 7.983; 95% CI (1.443–44.174)].
Based on educational status, respondents whose educational status masters and above were significantly more likely to develop anxiety than respondents whose educational status diploma [AOR = 3.243; 95% CI (1.003–10.482)].
Regarding monthly income, the odds of having anxiety were 1.87 times among respondents who had low monthly income as compared with those respondents who had a high monthly income [AOR = 1.868; 95% CI (1.140–3.061)]. Moreover, Health care providers who had infected family members were significantly more likely to develop anxiety than respondents who didn’t have infected family members [AOR = 3.296; 95% CI (1.503–7.227)] (Table 4).
Table 4. Factors associated with anxiety among health care providers in Gurage Zone health institutions, SNNPR, South West, Ethiopia, 2020.
| Variable | Levels of Anxiety | COR(95%, CI) | AOR(95%, CI) | |
|---|---|---|---|---|
| No Anxiety n (%) | Anxiety n (%) | |||
| Age in year | ||||
| 18–25 | 65(20.18) | 27(8.38) | 1.00 | 1.00 |
| 26–30 | 111(34.47) | 46(12.8) | 0.998(0.567–1.756) | 1.064(0.587–1.929) |
| 31–40 | 28(8.43) | 32(9.93) | 2.751(1.398–5.416)* | 2.019(0.940–4.339) |
| >40 | 2(0.62) | 11(3.4) | 13.241(2.749–63.774)* | 7.983(1.443–44.174)** |
| Monthly income | ||||
| Low | 80(24.8) | 62(19.2) | 1.808(1.142–2.865)* | 1.868(1.140–3.061)** |
| High | 126(39.1) | 54(16.7) | 1.00 | 1.00 |
| Educational status | ||||
| Diploma | 73(22.67) | 37(11.49) | 1.00 | 1.00 |
| Degree | 126(39.13) | 60(18.63) | 0.940(0.569–1.550) | 0.998(0.570–1.747) |
| Masters and above | 7(2.1) | 19(5.9) | 5.355(2.066–13.883)* | 3.243(1.003–10.482)** |
| Infected family member | ||||
| No | 194(60.25) | 90(27.95) | 1.00 | 1.00 |
| Yes | 12(3.72) | 26(8.06) | 4.670(2.255–9.674)* | 3.296(1.503–7.227)** |
*p value<0.05 at bivariate logistic regression
**p value<0.05 at multivariate logistic regression.
Prevalence of depression among health care providers in Gurage Zone, SNNPR, South West, Ethiopia, 2020
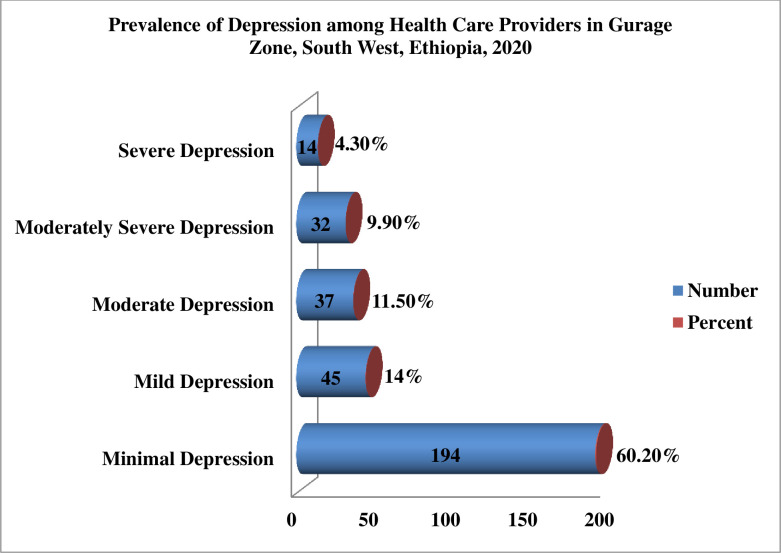
Table 5 shows the respondent’s responses to the 9 items of the PHQ-9. Through the past 2 weeks before the study. these providers replied honestly to the following as occurring for several days, more than half the days, or nearly every day: feeling tired or having little energy (42.5%); poor appetite or overeating (39.4%); little interest or pleasure in doing things (39.1%); moving or speaking so slowly that other people could have noticed; so fidgety or restless that you have been moving around a lot more than usual (37.6%); trouble falling or staying asleep or sleeping too much (37.3%); feeling bad about yourself or that you are a failure or have let yourself or your family down (34.2%); feeling down, depressed, or hopeless (31.4%); thoughts that you would be better off dead or of hurting yourself in some way (30.7%) and trouble concentrating on things, such as reading the newspaper or watching television (30.1%). Based on our finding three-fifth (60.2%) of health care providers had minimal depression, 45(14%) had mild depression, 37(11.5%) had moderate anxiety, 32(9.9%) had moderately severe depression and 14(4.3%) had severe depression.
Table 5. Prevalence of depression among health care providers in Gurage Zone, SNNPR, South West, Ethiopia, 2020.
| Variables | Categories | |||
|---|---|---|---|---|
| Not at all number (%) | under half the days | over half the days | nearly every day | |
| Number (%) | Number (%) | Number (%) | ||
| Little interest or pleasure in doing things | 196 (60.9) | 50 (15.5) | 42 (13.0) | 34 (10.6) |
| Feeling down, depressed, or hopeless | 221 (68.6) | 47(14.6) | 38 (11.8) | 16 (5.0) |
| Trouble falling or staying asleep, or sleeping too much | 202 (62.7) | 55 (17.1) | 43(13.4) | 22 (6.8) |
| Feeling tired or having little energy | 185 (57.5) | 69 (21.4) | 45 (14.0) | 23 (7.1) |
| Poor appetite or over eating | 195 (60.6) | 66 (20.5) | 41 (12.7) | 20 (6.2) |
| Feeling bad about yourself or that you are a failure or have let yourself or your family down | 212 (65.8) | 73 (22.7) | 24 (7.5) | 13 (4.0) |
| Trouble concentrating on things, such as reading the newspaper or watching television | 196 (69.9) | 53(16.5) | 50(15.5) | 23(7.1%) |
| Moving or speaking so slowly that other people could have noticed? Or the opposite—being so fidgety or restless that you have been moving around a lot more than usual | 201 (62.4%) | 66 (20.5%) | 36 (11.2%) | 19 (5.9%) |
| Thoughts that you would be better off dead or of hurting yourself in some way | 223 (69.3%) | 58 (18.0%) | 32 (9.9%) | 9 (2.8%) |
For descriptive purposes only, a cutoff of ≥10 was used to distinguish the severity of depression. So. One-fourths of (25.8%) of health care providers had depression related to covid-19 pandemics (Fig 3).
Fig 3. Prevalence of depression among health care providers in Gurage Zone, SNNPR, South West, Ethiopia, 2020 (n = 322).
Factors associated with depression among health care providers in Gurage Zone, SNNPR, South West, Ethiopia, 2020
First Bivariable logistic regression analysis was conducted to detect the presence of association and measure the relative effect of each independent variable against depression. As a result, among all other variables. Age, gender, marital status, educational status, ethnicity, occupation, types of health facility, living condition, monthly income, experience, and presence of infected colleague were found to have an association (i.e. p-value of < 0.25) and become eligible for multivariable analysis. Then, the multivariable logistic regression analysis showed that gender, educational status, living condition, occupation, and presence of infected family were found to be statistically significant predictors of depression among health care providers.
The odds of having depression were 1.9 times among male health care providers as compared with female health care providers [AOR = 1.908; 95% CI (1.040–3.500)].
Based on educational status, the odds of having depression among providers whose educational status masters and above were 10.8 times and degrees were 2.26 times as compared with those respondents whose educational status were diploma [AOR = 10.844; 95% CI (1.131–4.551)], and [AOR = 2.269; 95% CI (3.314–35.482)] respectively.
Health care providers who live with their husband/wife and those respondents who live with their families were significantly more likely to develop depression than health care providers who live alone [AOR = 5.824; 95% CI (1.896–17.888)] and [AOR = 3.938; 95% CI (1.380–11.242)] respectively. On the other hand, the odds of having depression among pharmacists were 4.5 times and among physicians were 0.2 times as compared with nurses, [AOR = (4.519; 95% CI (1.880–11.006)] and [AOR = (0.197; 95% CI (0.60–0.651))] respectively (Table 6).
Table 6. Factors associated with depression among health care providers in Gurage Zone health institutions, SNNPR, South West, Ethiopia, 2020.
| Variable | Levels of Depression | COR(95%, CI) | AOR(95%, CI) | |
|---|---|---|---|---|
| No Depression | Depression | |||
| n (%) | n (%) | |||
| Gender | ||||
| Male | 117(36,33) | 50(15.52) | 1.580(0.951–2.624) | 1.908(1.040–3.500)** |
| Female | 122(37.88) | 33(10.24) | 1.00 | 1.00 |
| Educational status | ||||
| Diploma | 90(27.95) | 20(6.2) | 1.00 | 1.00 |
| Degree | 138(42.85) | 48(14.90) | 1.565(0.872–2.811) | 2.269(1.131–4.551)** |
| Masters and above | 11(3.41) | 15(4.65) | 6.136(2.454–15.345)* | 10.844(3.314–35.482)** |
| Living status | ||||
| Husband | 104(32.29) | 48(14.90) | 2.308(1.292–4.122)* | 5.824(1.896–17.888)** |
| Family | 24(7.45) | 13(4.03) | 2.708(1.191–6.159)* | 3.938(1.380–11.242)** |
| Friend | 6(1.86) | 1(0.31) | 0.833(0.095–7.286) | 0.641(0.063–6.538) |
| Alone | 105(32.06) | 21(6.52) | 1.00 | 1.00 |
| Occupation | ||||
| Nurse | 85(26.39) | 28(8.7) | 1.00 | 1.00 |
| Physician | 38(11.8) | 6(1.86) | 0.479(0.183–1.253) | 0.197(0.60–0.651)** |
| Midwifery | 28(8.7) | 6(1.86) | 0.651(0.244–1.733) | 0.846(0.291–2.458) |
| Pharmacy | 19(5.9) | 19(5.9) | 3.036(1.411–6.530)* | 4.519(1.880–11.006)** |
| Lab technician | 13(4.03) | 3(0.93) | 0.701(0.186–2.638) | 1.303(0.307–5.522) |
| Health officer | 27(8.38) | 7(2.17) | 0.787(0.309–2.004) | 0.543(0.180–1.642) |
| Environmental Health | 6(1.86) | 4(1.24) | 2.024(0.532–7.693) | 0.716(0.142–3.593) |
| Others | 23(7.14) | 10(3/1) | 1.320(0.560–3.108) | 0.787(0.281–2.202) |
*p value<0.05 at bivariate logistic regression
**p value<0.05 at multivariate logistic regression.
Prevalence of perceived stress among health care providers in Gurage Zone, SNNPR, South West, Ethiopia, 2020
Table 7 shows the respondents’ responses to the 10 Item perceived stress scale (PSS) during the last month before the study. These providers replied honestly to the following as occurring for sometimes, fairly often, or very often. Felt difficulties were piling up so high that you could not overcome them (64.0%); been upset because of something that happened unexpectedly (58.4%); been angered because of things that were outside of your control (54.3%); found that you could not cope with all the things that you had to do (46.9%); felt that you were unable to control the important things in your life (45.9%); felt nervous and “stressed” (41.3%); been able to control irritations in your life (39.1%); felt that you were on top of things (44.7%); felt confident about your ability to handle your problems (60.5%) and felt that things were going your way (68.4%).
Table 7. Prevalence of perceived stress among health care providers in Gurage Zone, SNNPR, South West, Ethiopia, 2020.
| Variables | Categories | ||||
|---|---|---|---|---|---|
| Never (%) | Almost never (%) | Sometimes (%) | Fairly Often (%) | Very Often (%) | |
| Been upset because of something that happened unexpectedly? | 89 (27.6) | 45 (14.0) | 52 (16.1) | 62 (19.3) | 74 (23.0%) |
| Felt that you were unable to control the important things in your life? | 112 (34.8) | 62 (19.3) | 71 (22.0) | 45 (14.0) | 32 (9.9) |
| Felt nervous and “stressed”? | 119 (37.0) | 70 (21.7) | 64(19.9) | 46 (14.3) | 23 (7.1) |
| Felt confident about your ability to handle your problems? | 53 (16.5) | 74 (23.0) | 70 (21.7) | 68 (21.1) | 57 (17.7) |
| Felt that things were going your way? | 41 (12.7) | 61 (18.9) | 79 (24.5) | 86(26.7) | 55 (17.1) |
| Found that you could not cope with all the things that you had to do? | 51 (15.8) | 120 (37.3) | 75 (23.3) | 59 (18.3) | 17 (5.3) |
| Been able to control irritations in your life? | 49 (15.2) | 147 (45.7) | 64 (19.9) | 34 (10.6%) | 28 (8.7) |
| Felt that you were on top of things? | 47 (14.6) | 131(40.7%) | 54 (16.8%) | 53 (16.5%) | 37 (11.5) |
| Been angered because of things that were outside of your control? | 53 (16.5%) | 94 (29.2%) | 65 (20.2%) | 60 (18.6%) | 50 (15.5%) |
| Felt difficulties were piling up so high that you could not overcome them? | 65 (20.2) | 51 (15.8) | 58 (18.0) | 69 (21.4) | 79 (24.5) |
The bold letter indicates a 4-item negative factor asking the ability to manage the stressors.
Based on our finding three-fifth (60.2%) of health care providers had low stress, 45(14%) had moderate stress, and 14(4.3%) had high levels of stress.
The summation scores range from 0–40 with a higher score indicating a higher level of stress. The scores from 0–13 indicate low stress, whereas scores from 14–26 and 27–40 indicate moderate and high levels of stress, respectively.
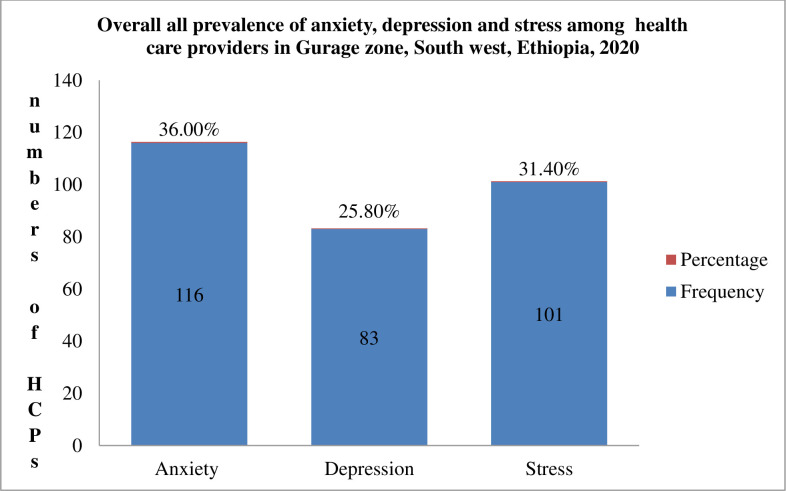
For descriptive purposes only, a cutoff of ≥21 was used to distinguish the severity of stress. So. 101 (31.4%) of HCPs had stress whereas 221 (68.6%) of HCPs had no stress related to covid-19 pandemics.
Factors associated with stress among health care providers in Gurage Zone, SNNPR, South West, Ethiopia, 2020
Bivariate and multivariate logistic regression analysis was conducted to see the presence of association and to measure the relative effect of each independent variable on overall perceived stress among health care providers. Age, gender, marital status, educational status, ethnicity, occupation, types of health facility, monthly income, experience, presence of infected colleague and family were significant factors associated with stress among health care providers.
Among fitted variables included in the binary regression model for bivariate analysis, gender, marital status, ethnicity, occupation, types of health facility, monthly income and experience were variables taken into consideration for multivariate analysis with a p-value < 0.25. Under multivariate analysis type of health facility and monthly income were found to be statistically significant predictors of stress among health care providers.
Health care providers who are working at general and referral hospitals were significantly more likely to develop stress than health care providers who were working at primary hospitals [AOR = 4.835; 95% CI (2.189–10.680)], and [AOR = 3.263; 95% CI (1.302–8.178)] respectively.
Health care providers who had low monthly income were significantly more likely to develop stress than health care providers who had high monthly income [AOR = 2.289; 95% CI (1.349–3.885)] (Table 8).
Table 8. Factors associated with stress among health care providers in Gurage Zone health institutions, SNNPR, South West, Ethiopia, 2020.
| Variable | Levels of Stress | COR(95%, CI) | AOR(95%, CI) | |
|---|---|---|---|---|
| No Stress n (%) | Stress n (%) | |||
| Types of health facility | ||||
| Primary | 75(23.29) | 10(3.1) | 1.00 | 1.00 |
| General | 64(19.88) | 47(14.6) | 5.508(2.577–11.774)* | 4.835(2.189–10.680)** |
| Referral | 31(9.63) | 16(4.97) | 3.871(1.583–9.465)* | 3.263(1.302–8.178)** |
| Isolation center | 51(15.84) | 28(8.7) | 4.118(1.841–9.209)* | 5.270(2.275–12.209)** |
| Monthly income | ||||
| Low | 85(26.3) | 57(17.7) | 2.073(1.286–3.342)* | 2.289(1.349–3.885)** |
| High | 136(42.2) | 44(13.67) | 1.00 | 1.00 |
*p value<0.05 at bivariate logistic regression
**p value<0.05 at multivariate logistic regression.
Generally, 36.0%, 25.80%, and 31.4% of health care providers in the Gurage zonal institution had anxiety, depression, and stress respectively (Fig 4).
Fig 4. Overall prevalence of anxiety, depression, and stress among HCPs in Gurage Zonal Health Institution’s, SNNPR, Ethiopia, 2020 (n = 322).
Discussion
The results of this study had shown that the overall prevalence of anxiety among health care providers in Gurage Zonal Public hospital was 36%, [95% CI = (30.7%- 41.3%)] which is in line with the previously reported study from Ethiopia(29.3%) [45], Nepal (38%) [46], India (31.6) [47].However, it is less than the findings in Gondar (69.6%) [48], Debre Tabor (63%) [49], Central Ethiopia (78%) [50], Addis Ababa (51.6) [51], Egypt, and Saudi Arabia (58.9%) [52]). Mali (73.3%) [53], Saudi Arabia (51.4%) [54], (78.8%) [55], Iran (67.55%) [56], Iraq (48.9%) [57], Nepal (41.9%) [58], Turkey (45.1%) [59], China (41.1%) [60], (44.6%) [4], North Italy (50.1%) [61], and USA (43%) [62]. However, it is higher than the study conducted in St Peter hospital, Addis Ababa (21.2%) [63], St Paul Hospital (21.9%) [64], multinational multi-center study (8.7%) [65], Middle East country (23.6%) [66], Iran (25.8%) [67], China 8.5% [68] (14.3%) [69], India (17.7%) [47], Italy (19.8%) [70], Malaysia (29.7%) [71], and Australia (21%). This discrepancy may be due to differences in workload, socioeconomic, cultural, and environmental factors, variation in the availability of personal protective equipment and resources, the difference in emotional response related to previous experience/exposure with SARS, MERS, and H1N1 epidemics, and also it may be related to the different cut-off scores used to define levels of clinically significant anxiety.
According to this study being older than 40 years is significantly associated with anxiety. The finding is also supported by a study reported from Debre tabor [49], Saudi Arabia [72, 73]. South Korea [74] and India [75]. This may be due to older health care providers are among the most affected by the COVID-19 pandemic in terms of illness severity and mortality, increased risk of transmission more prone to complications, and they could also live with young children and/or have older people in their extended family, which could cause them to worry about bringing the virus home to their family members as well as older health care workers tend to have lower stress reactivity, poor emotional regulation and well-being than younger HCPs. Moreover, they are also more likely to suffer psychological impacts such as anxiety due to isolation, heavy workload, and facts about the COVID-19 pandemic which is complicated by pre-existing physical health problems, medical comorbidities, and existing mental health symptoms.
Our finding also showed that having infected family members is significantly associated with anxiety. It is supported by a previous study conducted in Debre tabor [49], Gondar [76], and China [77]. This anxiety might arise from close family relationships and concerns about family members’ health conditions, the absence of specific treatments for COVID-19 during the initial periods of the pandemic, and isolation from their loved ones during quarantine for prolonged periods.
Our study also revealed that those health care providers who had low monthly income were significantly associated with anxiety. This is supported by research done in St Peter hospital [63]. This may due to preoccupation with fear of how to cope with the potential economical challenge faced during the pandemic and increased psychological and economic pressure resulting from socioeconomic challenges that may critically impact mental health.
Our study finding showed that 25.8% [95% CI = (21.1%- 30.4%)] of Gurage Zone health care providers are suffering from depression during COVID-19 outbreak which is in line with study done in Iran(24.3%) [67], Middle East counties (27.4%) [66], Saudi Arabia (26.1%) [55], India 25%) [78], Turkey (23.6%) [59], Australia (27.6%), Italy (24.73%, 26%) [61, 70], and USA(26%) [62].This finding is higher than the study conducted in St Paul Hospital, Ethiopia (20.2%) [79], multinational multi-center study (5.3%) [65], India (11.4%) [47], China (9.5%) [68], (10.7%) [69]. However, it is lower than in study carried out in Gondar (55.3%) [48], St Peter Hospital, Addis Ababa (36.5%) [63], Central Ethiopia (60.3%) [50], Mali (71.9%) [53], Egypt and Saudi Arabia (69%) [52], (55.2%) [54], systematic review in Iran (55.89%) [80], Oman (32.3%) [81], Nepal (37.5%) [58], Malaysia (31%) [71], China (46.9%) [60], (50%) [4]. The discrepancy could be explained by the difference in socioeconomic status, social support, study setting, variability of health care workers, sample size variation, the difference in methods, environmental and organization culture, as well as social and cultural issues, which might contribute to this difference.
Our study revealed that Males health care providers were about two times more likely to become depressed than females. This is in line with the study carried out in India [78]. This might be due to our socio-cultural norms males HCPs had an economic burden which is expected to help other members of the family and relatives as a result, they are more prone to financial deprivation, which leads to developing depression than their counterparts. But this finding is inconsistent with other studies conducted in Egypt and Saudi Arabia [52], Low and Middle-income countries [82], Middle East countries [66], Turkey [59], Iran [83], India [47, 84], Poland [85], Italy [70, 86], and United Kingdom [87] which states female HCPs were more prone to depression due to females being more commonly exposed to mental illness, cultural factors, and hormonal fluctuations.
Our finding also revealed that participants with high educational levels were more depressed than those with lower educational statuses. This could be related to the increments of workload to those who had higher educational attainment and they conducted and explored different types of scientific researches about the virulent nature of the COVID-19 pandemic which induces depression.
According to our study, Health care providers living with their spouse and family were more likely to develop depression than those HCPs living alone. This finding is supported by research findings in St Paul, Ethiopia [64], Saudi Arabia [55], India [75, 84], and the United Kingdom [87]. which states that HCWs who were either married or married with children were more depressed than those among unmarried HCWs/ living alone [84]. The possible explanation could be primary worry of all HCPs was the safety of their families during the COVID-19 pandemic, which was regarded as a major depressive factor. Furthermore, married HCPs were found to be more hopeless, concern for family members and their wellbeing could contribute to their feeling of hopelessness.
The results of our study found that Nurse and Pharmacists were more likely to develop depression. Similar results were reported in research conducted in Mali [53], Middle East countries [66], China [69, 88], and Brazil [89]. The possible explanation might be due to nurses are frontline healthcare workers, directly engaged in diagnosis, treatment, and care of patients with COVID-19 and they have long work shifts and closer contact with patients, by undertaking most of the tasks related to infectious disease containment, as a result, they are prone to fatigue, tension, and depression. Besides these in a study conducted in low and middle-income countries (LMICs) showed that Nurses and other HCPs in non-physician roles experienced greater depressive symptom severity compared to HCPs in physician roles [82]. The pharmacist is also involved directly to provide drugs for patients with COVID-19 and they are at high risk for developing depression.
Our study finding showed that during the COVID-19 pandemic, 31.4% [95% CI = (26.4%- 36.0%)] of HCPs had stress. Which is congruent with study finding in Central Ethiopia (33.8%) [50], benchi-sheko (32.5%) [90], The finding is less than study reported from Addis Ababa (43.4%) [91]), Dilla, Ethiopia (51.6%) [43], Egypt and Saudi Arabia (55.9%) [52], a systematic review in Iran (45%) [67], (62.9%) [80], China (69.1%) [60], and USA (80.1%) [62]. However, it is higher than in study done in Gondar (20.5%) [48], multinational multi-center study (2.2%) [65], Oman (23.8%) [81], Malaysia (23.5%) [71], and Italy(21.90%, 8.9%) [70, 92].
Health care providers who are working at general and referral hospitals were more likely to become stressed than health care providers who were working at primary hospitals. This is supported by a systematic review and meta-analysis conducted in china which states that a considerable proportion of healthcare workers within secondary and tertiary hospitals developed adverse psychological outcomes during the COVID-19 pandemic [32]. A similar study conducted in China showed that those HCPs working in secondary hospitals reported high levels of psychological problems [4].
In this study HCPs who had low monthly income were more likely to be stressed than those HCPs who had high monthly income. This is supported by research conducted in Addis Ababa, Ethiopia. This could be due to the socioeconomic impact of a virus might be much significant to the extent of unable to buy safety measures of prevention, such as facemask, soaps, and sanitizers. In addition during this pandemic period, they were not able to fulfill their basic needs of day-to-day life [93].
Strength of the study
We have used a previously validated and well-established instrument to measure our outcome variables GAD-7, PHQ, and PSS for the assessment of anxiety, depression, and stress respectively. Moreover, there was a proportionate representation of health care providers from each department in this study; this would likely mitigate the bias of having a higher number of nurses/ doctors as in previous studies conducted in other regions of Ethiopia.
Limitation of the study
The study has certain limitations which must be acknowledged. First, we did not explore the common risk factors for anxiety, depression, and stress, like a history of anxiety, depression, and stress, comorbidities like chronic diseases, social support, and communication. Second, responses to the survey were self-reported. It may have resulted in reporting biases for social desirability which may have affected the results and finally, this study cannot show cause and effect relationship since it is a cross-sectional type. Despite the identified limitations, these results contribute to the information relating to the overwhelming problem faced by HCPs especially related to the commonly encountered mental health problems while caring not only in Ethiopia but also at the global level.
Conclusion and recommendation
Based on our findings, significant numbers of healthcare workers were suffered from anxiety, depression, and stress during the COVID-19 outbreak. On most occasions, the mental health impact of a disease outbreak is usually neglected during pandemic management although the consequences are costly. Therefore, the Federal Ministry of Health in collaboration with hospitals should pass emergency legislation to protect healthcare providers who are at high risk of exposure to mental health problems. This should include financial protections for healthcare providers who contract COVID-19 and supplement additional safety requirements for healthcare facilities. Moreover, mental health professionals should pay attention to the role of family members’ health and monitor the mental wellbeing of health care providers too.
The finding revealed that age, educational status, monthly income, and the presence of infected families were statistically associated with anxiety. Besides this, gender, educational status, living condition, and occupation were found to be statistically significant predictors of depression among health care providers. Our study finding also showed that type of health facility and monthly income were found to be statistically significant predictors of stress among health care providers.
Supporting information
(SAV)
Acknowledgments
We would like to express our heartfelt gratitude to the Gurage zonal health department, hospital administration staff, and health care providers for their valuable supports while collecting the data. And our thanks go to go to all data collectors and supervisors for their endeavor.
List of abbreviation
- AOR
Adjusted Odds Ratio
- CoV
Corona Virus
- COVID-19
Corona Virus Disease 2019
- CSA
Central Statistics Agency
- GAD
Generalized Anxiety Disorder
- HC
Health Center
- HCPs
Health Care Providers
- HCWs
Health Care Workers
- ICN
International Council of Nurses
- IPC
Infection Prevention and Control
- LMICs
Low and Middle Income Countries
- NGO
Non-Governmental Organization
- NICU
Neonatal Intensive Care Unit
- OPD
Out Patient Department
- OR
Operation Room
- PHEIC
Public Health Emergency of International Concern
- PHQ
Patient Health Questionnaire
- PPE
Personal Protective Equipment’s
- PSS
Perceived Stress Scale
- PTSD
Post Traumatic Distress Syndrome
- SARS-CoV-2
Severe Acute Respiratory Syndrome Coronavirus 2
- SD
Standard Deviation
- SNNPRE
South Nation Nationality and Peoples Regions of Ethiopia
- SPSS
Statistical Package for Social Sciences
- WHO
World Health Organization
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Yin Y, RG W. MERS, SARS and other coronaviruses as causes of pneumonia. Respirology 2018. Feb 20;23(2):130–137 [FREE Full text] doi: 10.1111/resp.13196 [Medline: 29052924]. Feb 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Novel coronavirus (2019-nCoV) situation report– 12. https://www.who.int/docs/default-source/coronaviruse/situation-reports/202002022 / 24 1-sitrep-12-ncov.pdf?sfvrsn = 273c5d35_2. Accessed on 2 February, 2020.
- 3.WHO Director-General’s opening remarks at the media briefing on COVID-19–11 March 2020 n.d. https://www.who.int/dg/speeches/detail/who-director-general-s-openingremarks-at-the-media-briefing-on-covid-19—11-march-2020 (accessed April 10, 2020).
- 4.Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. 2020;3(3):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kennedy C, Lima T, Moreira P, Carvalho DM, Araújo I De, Silva A, et al. The emotional impact of Coronavirus 2019-nCoV (new Coronavirus disease). Psychiatry Res [Internet]. 2020;287:112915. Available from: doi: 10.1016/j.psychres.2020.112915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim SC, Quiban C, Sloan C, Montejano A. Predictors of poor mental health among nurses during COVID-19 pandemic. Nurs Open. 2021;8:900–907. doi: 10.1002/nop2.697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shigemura J, Ursano RJ, Morganstein JC, Kurosawa M, Benedek DM. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: mental health consequences and target populations. Psychiatry Clin Neurosci. 2020;74(4):281. doi: 10.1111/pcn.12988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw Open. 2020. Mar 23;3(3):e203976. doi: 10.1001/jamanetworkopen.2020.3976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lasalvia A, Bonetto C, Porru S, Carta A, Tardivo S, Bovo C, et al. Psychological impact of COVID-19 pandemic on healthcare workers in a highly burdened area of north-east Italy. Epidemiology and psychiatric sciences. 2021;30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Young KP, Kolcz DL, O’Sullivan DM, Ferrand J, Fried J, Robinson K. Health Care Workers’ Mental Health and Quality of Life During COVID-19: Results From a Mid-Pandemic, National Survey. Psychiatr Serv. 2021. Feb 1;72(2):122–8. doi: 10.1176/appi.ps.202000424 [DOI] [PubMed] [Google Scholar]
- 11.Zhu Z, Xu S, Wang H, Liu Z, Wu J, Li G et al. COVID-19 in Wuhan: Immediate Psychological Impact on 5062 Health Workers. medRxiv. 2020. 10.1101/2020.02.20. 20025338. [DOI] [Google Scholar]
- 12.International Council of Nurses. Protecting nurses from COVID-19 a top priority: A survey of ICN’s national nursing associations [Internet]. Geneva; 2020. (https://www.icn.ch/system/files/documents/2020-09/Analysis_COVID-19surveyfeedback_14.09.2020.pdf, accessed 13 October 2020).
- 13.COVID Live Update: 230,920,739 Cases and 4,733,350 Deaths from the Coronavirus—Worldometer [Internet]. [cited 2021 Sep 23]. Available from: https://www.worldometers.info/coronavirus/?utm_campaign=homeAdvegas1?
- 14.At least 17,000 health workers have died from COVID: Amnesty | Coronavirus pandemic News | Al Jazeera [Internet]. [cited 2021 Jun 16]. Available from: https://www.aljazeera.com/news/2021/3/5/at-least-17000-health-workers-have-died-from-covid-amnesty
- 15.The United Nations Office for the Coordination of Humanitarian Affairs (OCHA); ETHIOPIA: COVID-19 humanitarian impact situation update no. 11; 2020. Available from: www.unocha.org/ethiopia. Accessed September 20, 2020.
- 16.ETHIOPIA COVID-19 MULTI SECTORIAL PREPAREDNESS AND RESPONSE PLAN. 2020 Mar;
- 17.Jemal Kemal, Berhanu Senbeta Deriba Tinsae Abeya Geleta, Tesema Mengistu, Awol Mukemil, Mengistu Endeshaw, et al. Self-Reported Symptoms of Depression, Anxiety, and Stress Among Healthcare Workers in Ethiopia During the COVID-19 Pandemic. Neuropsychiatr Dis Treat. 2021;17:1363–73. doi: 10.2147/NDT.S306240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gelaye B, Lemma S, Deyassa N, Bahretibeb Y, Tesfaye M, Berhane Y, et al. Prevalence and correlates of mental distress among working adults in Ethiopia. Clin Pract Epidemiol Ment Health. (2012) 8:126–33. doi: 10.2174/1745017901208010126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jacob N, Coetzee D. Mental illness in the Western Cape Province, South Africa: a review of the burden of disease and healthcare interventions. South African Med J. (2018) 108:176–80. doi: 10.7196/SAMJ.2018.v108i3.12904 [DOI] [PubMed] [Google Scholar]
- 20.Devnani M. Factors associated with the willingness of health care personnel to work during an influenza public health emergency: an integrative review. Prehospital and Disaster Medicine. 2012; 27(6):551–66. doi: 10.1017/S1049023X12001331 [DOI] [PubMed] [Google Scholar]
- 21.Imai H, Matsuishi K, Ito A, Mouri K, Kitamura N, Akimoto K, et al. Factors associated with motivation and hesitation to work among health professionals during a public crisis: a cross-sectional study of hospital workers in Japan during the pandemic (H1N1) 2009. BMC Public Health. 2010; 10(1):672. doi: 10.1186/1471-2458-10-672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mitigating the psychological effects of COVID-19 on health care workers CMAJ 2020. April 27;192:E459–60. doi: 10.1503/cmaj.200519 early-released April 15, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Montemurro N, 2020. The emotional impact of COVID-19: From medical staff to common people, Brain Behav, Immun, 87:23–24. doi: 10.1016/j.bbi.2020.03.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.World Health Organization and the International Labour Office. Occupational Safety and Health in Public Health Emergencies: a manual for Protecting HealthWorkers and Responders. 2018, Geneva. Available online: https://apps.who.int/iris/bitstream/handle/10665/275385/9789241514347-eng.pdf (accessed on 21 July 2020).
- 25.Lin C. Survey of Stress Reactions Among Health Care Workers Involved With the SARS Outbreak. 2004;55(9):5–7. [DOI] [PubMed] [Google Scholar]
- 26.Maunder R, Hunter J, Vincent L, Bennett J, Peladeau N, Leszcz M, et al. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. 2003;168(10):1245–51. [PMC free article] [PubMed] [Google Scholar]
- 27.Lee AM, Wong JGWS, Mcalonan GM, Cheung V, Cheung C, Sham PC, et al. Stress and Psychological Distress Among SARS Survivors 1 Year After the Outbreak. 2007;52(4):233–40. [DOI] [PubMed] [Google Scholar]
- 28.Mukhtar S. Psychological health during the coronavirus disease 2019 pandemic outbreak. Int. J. Soc. Psychiatry 2020, 66, 512–516. [CrossRef]. doi: 10.1177/0020764020925835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.WHO, 2020. COVID 19 Public Health Emergency of International Concern (PHEIC) Global Research and Innovation Forum: Towards a Research Roadmap. R&D Blueprint: World Health Organization, pp. 1–7. [Google Scholar]
- 30.Guo J, Liao L, Wang B, Li X, Guo L, Tong Z, et al. (2020) Psychological effects of COVID-19 on hospital staff: a national cross-sectional survey of China mainland. SSRN Electronic Journal [published online March 24], available at https://ssrn.com/abstract=3550050. [Google Scholar]
- 31.Lai C, Shih T, Ko W, Tang H, Hsueh P. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. Int J Antimicrob Agents 2020. Mar;55(3):105924 [FREE Full text] doi: 10.1016/j.ijantimicag.2020.105924 [Medline: 32081636]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E and Katsaounou P (2020) Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behavior and Immunity 88, 901–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang Z, Liu S, Xianf M, et al. Protecting healthcare personnel from 2019-nCov infection risks: lessons and suggestions. Front Med. 2020;1–3. doi: 10.1007/s11684-020-0765-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhu J., Sun L., Zhang L., Wang H., Fan A., Yang B., et al. Prevalence and Influencing Factors of Anxiety and Depression Symptoms in the First-Line Medical Staff Fighting Against COVID-19 in Gansu. Front Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.00011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Central Statistical Agency. Population and household census of Ethiopia. 2007.
- 36.Elhadi M, Msherghi A, Alkeelani M, Zorgani A, Zaid A, Alsuyihili A, et al. Assessment of Healthcare Workers’ Levels of Preparedness and Awareness Regarding COVID-19 Infection in Low-Resource Settings. Am J Trop Med Hyg. 2020. Jun 18;103(2):828–33. doi: 10.4269/ajtmh.20-0330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gelaye B., Williams M.A., Lemma S., Deyessa N., Bahretibeb Y. et al., 2014. Validity of the Patient Health Questionnaire-9 for depression screening and diagnosis in East Africa. Psychiatry Res. 210(2). doi: 10.1016/j.psychres.2013.07.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hanlon C., Medhin G., Selamu M., Breuer E., Worku B., et al., 2015. Validity of brief screening questionnaires to detect depression in primary care in Ethiopia. Journal of Affective Disorders. Elsevier, 186, pp. 32–39. doi: 10.1016/j.jad.2015.07.015 [DOI] [PubMed] [Google Scholar]
- 39.Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- 40.Zhang YL, Liang W, Chen ZM, et al. Validity and reliability of Patient Health Questionnaire-9 and Patient Health Questionnaire-2 to screen for depression among college students in China. Asia Pac Psychiatry. 2013;5(4): 268–275. doi: 10.1111/appy.12103 [DOI] [PubMed] [Google Scholar]
- 41.Spitzer RL, Kroenke K, Williams JB; Primary Care Evaluation of Mental Disorders. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study: Primary Care Evaluation of Mental Disorders, Patient Health Questionnaire. JAMA. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737 [DOI] [PubMed] [Google Scholar]
- 42.Leung D. Y., Lam T. H., & Chan S. S. (2010). Three versions of Perceived Stress Scale: Validation in a sample of Chinese cardiac patients who smoke. BMC Public Health, 10, 513. doi: 10.1186/1471-2458-10-513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chekole YA, Yimer Minaye S, Mekonnen Abate S, Mekuriaw B. Perceived Stress and Its Associated Factors during COVID-19 among Healthcare Providers in Ethiopia: A Cross-Sectional Study. Adv Public Health. 2020. Sep 24;2020:1–7. [Google Scholar]
- 44.He XY, Li CB, Qian J, Cui HS, Wu WY. Reliability and validity of a generalized anxiety scale in general hospital outpatients. Shanghai Arch Psychiatry. 22(4):200–203. doi: 10.3969/j.issn.1002-0829.2010.04.002 [DOI] [Google Scholar]
- 45.Abinet Tashome MG et al. Generalized Anxiety Disorder and Its Associated Factors Among Health Care Workers Fighting COVID-19 in Southern Ethiopia. Psychol Res Behav management. 2020; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gupta AK, Mehra A, Kafle K, Deo SP. Prevalence of Anxiety and Depression among the Healthcare Workers in Nepal during the COVID-19 Pandemic. Asian J Psychiatr. 2020;54. doi: 10.1016/j.ajp.2020.102260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wilson W, Raj JP, Rao S, Ghiya M, Nedungalaparambil NM, Mundra H, et al. Prevalence and predictors of stress, anxiety, and depression among healthcare workers managing COVID-19 pandemic in India: A nationwide observational study. Indian J Psychol Med. 2020;42(4): 353–358. doi: 10.1177/0253717620933992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mekonen Enyew, Muluneh Niguse, Shetie Belayneh. The Psychological Impact of COVID-19 Outbreak on Nurses Working in the Northwest of Amhara Regional State Referral Hospitals, Northwest Ethiopia. Psychol Res Behav Manag. 2020;13. doi: 10.2147/PRBM.S291446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kibret S, Teshome D, Fenta E, Hunie M, Tamire T. Prevalence of anxiety towards COVID-19 and its associated factors among healthcare workers in a Hospital of Ethiopia. PloS one. 2020. Dec 8;15(12):e0243022. doi: 10.1371/journal.pone.0243022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.kemal Jemal, Berhanu Senbeta, Tinsae Abeya Geleta, Mukemil Awol. COVID-19 pandemic and self-reported symptoms of depression, anxiety, and stress among health care workers in Ethiopia. Res Sq. 2020; [Google Scholar]
- 51.Addisu Tadesse Sahile Mikiyas Ababu, Alemayehu Sinetsehay, Abebe Haymanot, Endazenew Getabalew, Wubshet Mussie, et al. Prevalence and Severity of Depression, Anxiety, and Stress During Pandemic of COVID-19 Among College Students in Addis Ababa, Ethiopia, 2020 A Cross-Sectional Survey. Int J Clin Exp Med Sci. 2020;6(6):126–32. [Google Scholar]
- 52.Arafa A, Mohammed Z, Mahmoud O, Elshazley M, Ewis A. Depressed, anxious, and stressed: What have healthcare workers on the frontlines in Egypt and Saudi Arabia experienced during the COVID-19 pandemic? J Affect Disord. 2021. Jan 1;278:365–71. doi: 10.1016/j.jad.2020.09.080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sagaon-Teyssier L, Kamissoko A, Yattassaye A, Diallo F, Rojas Castro D, Delabre R, et al. Assessment of mental health outcomes and associated factors among workers in community-based HIV care centers in the early stage of the COVID-19 outbreak in Mali. Health Policy Open. 2020. Dec;1:100017. doi: 10.1016/j.hpopen.2020.100017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mental health among healthcare providers during coronavirus disease (COVID-19) outbreak in Saudi Arabia | Elsevier Enhanced Reader [Internet]. [cited 2021 Mar 6]. Available from: https://reader.elsevier.com/reader/sd/pii/S1876034120306353?token=A7CF7D03151A15D73C0F46E157CD9DA7317CB52AACD275F366D254BC1DD859ABE52749FF54ED298BABB6473F913E5CBA [DOI] [PMC free article] [PubMed]
- 55.Ammari Al et al. Mental Health Outcomes Amongst Health Care Workers During COVID 19 Pandemic in Saudi Arabia. Front Psychiatry. 2021;11. doi: 10.3389/fpsyt.2020.619540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Robertson LJ, Maposa I, Somaroo H, Johnson O. Mental health of healthcare workers during the COVID-19 outbreak: A rapid scoping review to inform provincial guidelines in South Africa. S Afr Med J. 2020;110(10):1010–9. doi: 10.7196/SAMJ.2020.v110i10.15022 [DOI] [PubMed] [Google Scholar]
- 57.Karimet al. COVID-19-related anxiety disorder in Iraq during the pandemic: an online cross-sectional study. Middle East Curr Psychiatry. 2020;27(55). [Google Scholar]
- 58.Khanal P, Devkota N, Dahal M, Paudel K, Joshi D. Mental health impacts among health workers during COVID-19 in a low resource setting: a cross-sectional survey from Nepal. Glob Health. 2020. Sep 25;16(1):89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Özdina Selçuk, Şükriye Bayrak Özdin. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. Int J Soc Psychiatry. 2020;66(5):504–11. doi: 10.1177/0020764020927051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lin Kangguang, Bing Xiang Yang, Dan Luo, Liu Qian. The Mental Health Effects of COVID-19 on Health Care Providers in China. Am J Psychiatry. 2020. Jul;177(7). [DOI] [PubMed] [Google Scholar]
- 61.Lasalvia A, Bonetto C, Porru S, Carta A, Tardivo S, Bovo C, et al. (2021). The psychological impact of COVID-19 pandemic on healthcare workers in a highly burdened area of northeast Italy. Epidemiology and Psychiatric Sciences 30, e1, 1–13. 10.1017/S2045796020001158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kim SC, Quiban C, Sloan C, Montejano A. Predictors of poor mental health among nurses during COVID‐19 pandemic. Nurs Open [Internet]. 2020. Nov 20 [cited 2021 Mar 13]; Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7753542/ doi: 10.1002/nop2.697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Assefa Bizuayehu. Prevalence and Factors Associated with Depression and Anxiety of Hospitalized Patients with COVID-19 in St.peter Specialized Hospital Treatment Centers. J Psychiatry. 2020;23(14). [Google Scholar]
- 64.Mulatu HA, Tesfaye M, Woldeyes E, Bayisa T, Fisseha H, Asrat R. The prevalence of common mental disorders among health care professionals during the COVID-19 pandemic at a tertiary Hospital in East Africa. medRxiv. 2020. Jan 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chew N.W.S., et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID- 19 outbreak. Brain Behav Immun. 2020;88:559–65. doi: 10.1016/j.bbi.2020.04.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Aoun-Rahman-Mostafaet.al. Impact of the COVID-19 pandemic on health care workers’ mental health: A cross-sectional study. Allied J Med Res. 2020;4(1):http://www.alliedacademies.org/allied-journal-of-medical-research/. [Google Scholar]
- 67.Salari N, Khazaie H, Hosseinian-Far A, Khaledi-Paveh B, Kazeminia M, Mohammadi M, et al. The prevalence of stress, anxiety, and depression within front-line healthcare workers caring for COVID-19 patients: a systematic review and meta-regression. Hum Resour Health [Internet]. 2020. Dec 17 [cited 2021 Mar 13];18. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7745176/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zhang et al. Mental Health and Psychosocial Problems of Medical Health Workers during the COVID-19 Epidemic in China. Psychother Psychosom. 2020;89:242–50. doi: 10.1159/000507639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hu D, Kong Y, Li W, Han Q, Zhang X, Zhu LX, et al. Frontline nurses’ burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in Wuhan, China: A large-scale cross-sectional study. clinical medicine. 2020. Jul;24:100424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ross Rodolfo, Socci Valentina, Pacitti Francesca, Giorgio Di Lorenzo Antinisca Di Marco, Siracusano Alberto, et al. Mental Health Outcomes Among Frontline and Second-Line Health Care Workers During the Coronavirus Disease 2019 (COVID-19) Pandemic in Italy. JAMA Netw Open. 2020;3(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mohd Fauzi MF, Mohd Yusoff H, Muhamad Robat R, Mat Saruan NA, Ismail KI, Mohd Haris AF. Doctors’ Mental Health during COVID-19 Pandemic: The Roles of Work Demands and Recovery Experiences. Int J Environ Res Public Health [Internet]. 2020. Oct [cited 2021 Mar 13];17(19). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7579590/ doi: 10.3390/ijerph17197340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.AlAteeq DA, Aljhani S, Althiyabi I, Majzoub S. Mental health among healthcare providers during coronavirus disease (COVID- 19) outbreak in Saudi Arabia. J Infect Public Health. (2020) 13:1432–7. doi: 10.1016/j.jiph.2020.08.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Al-Hanawi MK, Mwale ML, Alshareef N, Qattan AMN, Angawi K, Almubark R, et al. Psychological distress amongst health workers and the general public during the COVID-19 pandemic in Saudi Arabia. Risk Manag Healthcare Policy. (2020) 13:733–42. doi: 10.2147/RMHP.S264037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ahn MH, Shin Y, Hye KJ, Kim HJ, Lee K. High Work-related Stress and Anxiety Response to COVID-19 among Healthcare Workers in South Korea: SAVE study. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chatterjee SS, Chakrabarty M, Banerjee D, Grover S, Chatterjee SS, Dan U. Stress, Sleep and Psychological Impact in Healthcare Workers During the Early Phase of COVID-19 in India: A Factor Analysis. Front Psychol [Internet]. 2021. Feb 25 [cited 2021 Mar 13];12. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7947354/ doi: 10.3389/fpsyg.2021.611314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mekonen E, Shetie B, Muluneh N. The Psychological Impact of COVID-19 Outbreak on Nurses Working in the Northwest of Amhara Regional State Referral Hospitals, Northwest Ethiopia. Psychology Research and Behavior Management. 2020;13:1353. doi: 10.2147/PRBM.S291446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Elsevier. Mental health problems faced by healthcare workers due to the COVID-19 pandemic–A review. Asian J Psychiatry. 2020;51(January). doi: 10.1016/j.ajp.2020.102119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Verma S, Mishra A. Depression, anxiety, and stress and socio-demographic correlates among general Indian public during COVID-19. Int J Soc Psychiatry. 2020;66(8):756–62. doi: 10.1177/0020764020934508 [DOI] [PubMed] [Google Scholar]
- 79.Hailu Abera Mulatu Muluken Tesfaye, Woldeyes Esubalew, Bayisa Tola, Fesseha Henok, Asrat Rodas. The prevalence of common mental disorders among health care professionals during the COVID-19 pandemic at a tertiary Hospital in East Africa. Res Sq. 2020; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Vizheh M, Qorbani M, Arzaghi SM, Muhidin S, Javanmard Z, Esmaeili M. The mental health of healthcare workers in the COVID-19 pandemic: A systematic review. J Diabetes Metab Disord. 2020. Oct 26;1–12. doi: 10.1007/s40200-020-00643-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Muna Alshekaili et al. Factors Associated with Mental Health Outcomes in Oman during COVID19: Frontline vs Non-frontline Healthcare Workers.: DOI: 10.1101/2020.06.23.20138032; [DOI] [PMC free article] [PubMed]
- 82.Moitra M, Rahman M, Collins PY, Gohar F, Weaver M, Kinuthia J, et al. Mental Health Consequences for Healthcare Workers During the COVID-19 Pandemic: A Scoping Review to Draw Lessons for LMICs. Front Psychiatry [Internet]. 2021. Jan 27 [cited 2021 Mar 8];12. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7873361/ doi: 10.3389/fpsyt.2021.602614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Pouralizadeh M, Bostani Z, Maroufizadeh S, Ghanbari A, Khoshbakht M, Alavi SA, et al. Anxiety and depression and the related factors in nurses of Guilan University of Medical Sciences hospitals during COVID-19: A web-based cross-sectional study. Int J Afr Nurs Sci. 2020;13:100233. doi: 10.1016/j.ijans.2020.100233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Gupta B, Sharma V, Kumar N, Mahajan A. Anxiety and Sleep Disturbances Among Health Care Workers During the COVID-19 Pandemic in India: Cross-Sectional Online Survey. JMIR Public Health Surveill. 2020;6(4):e24206. doi: 10.2196/24206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Maciaszek Julian, Ciulkowicz Marta, Misiak Blazej, Dorota Szczesniak et al. Mental Health of Medical and Non-Medical Professionals during the Peak of the COVID-19 Pandemic: A Cross-Sectional Nationwide Study. J Clin Med. 2020;9:2527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Conti C, Fontanesi L, Lanzara R, Rosa I, Porcelli P. Fragile heroes. The psychological impact of the COVID-19 pandemic on health-care workers in Italy. Kotozaki Y, editor. PLOS ONE. 2020. Nov 18;15(11):e0242538. doi: 10.1371/journal.pone.0242538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Pierce Matthias, Hope Holly, Ford Tamsin, Hatch Stephani, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Fang X-H, Wu L, Lu L-S, Kan X-H, Wang H, Xiong Y-J, et al. Mental health problems and social supports in the COVID-19 healthcare workers: a Chinese explanatory study. BMC Psychiatry. 2021. Jan 12;21(1):34. doi: 10.1186/s12888-020-02998-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ornell Felipe, Silvia Chwartzmann Halpern, Felix Henrique Paim Kessler, Joana Corrêa de Magalhães Narvaez. The impact of the COVID-19 pandemic on the mental health of healthcare professionals. Cad Saúde Pública. 2020;36(4):e00063520. doi: 10.1590/0102-311X00063520 [DOI] [PubMed] [Google Scholar]
- 90.Nigusie Shifera Aylie, Rahel Matiyas Mekuria, Mengistu Ayenew Mekonen. The Psychological Impacts of COVID-19 Pandemic Among University Students in Bench-Sheko Zone, South-west Ethiopia: A Community-based Cross-sectional Study. Psychol Res Behav Manag. 2020;13:813–21. doi: 10.2147/PRBM.S275593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Eleni Besfat. Depression, Anxiety, and Stress among Counseling Service Providers in Addis Ababa. Un Publ Source Thesis Submit Sch Psychol Addis Ababa Univ Partial Fulfillment Require Master Arts Degree Couns Psychol. 2020 Nov;
- 92.Lenzo Vittorio, Maria C Quattropani, Sardella Alberto, Martino Gabriella, Bonanno George A. Depression, Anxiety, and Stress Among Healthcare Workers During the COVID-19 Outbreak and Relationships With Expressive Flexibility and Context Sensitivity. Front Psychol. 2021. Feb 22;12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kassaw Chalachew. The Magnitude of Psychological Problem and Associated Factor in Response to COVID-19 Pandemic Among Communities Living in Addis Ababa, Ethiopia, March 2020: A Cross-Sectional Study Design. Psychol Res Behav Manag. 2020;13:631–40. doi: 10.2147/PRBM.S256551 [DOI] [PMC free article] [PubMed] [Google Scholar]