Abstract
Background
This study aimed to evaluate traumatic stress and mental health problems associated with the prolonged coronavirus disease pandemic and to determine the differences across different age groups.
Methods
A total of 1,151 individuals who visited Gwangmyeong City Mental Health Welfare Center, South Korea, or accessed the website from September 1 to December 31, 2020, were included in the study. Mental health problems such as traumatic stress (Primary Care Posttraumatic Stress Disorder Screen for the Diagnostic and Statistical Manual of Mental Disorder-5); depression (Patient Health Questionnaire-9 and Children's Depression Inventory); anxiety (Generalized Anxiety Disorder-7 and Penn State Worry Questionnaire for Children); suicide risk (P4 Screener); and demographic information were evaluated. The participants were divided into three groups based on age group: children and adolescents, adults, and the elderly.
Results
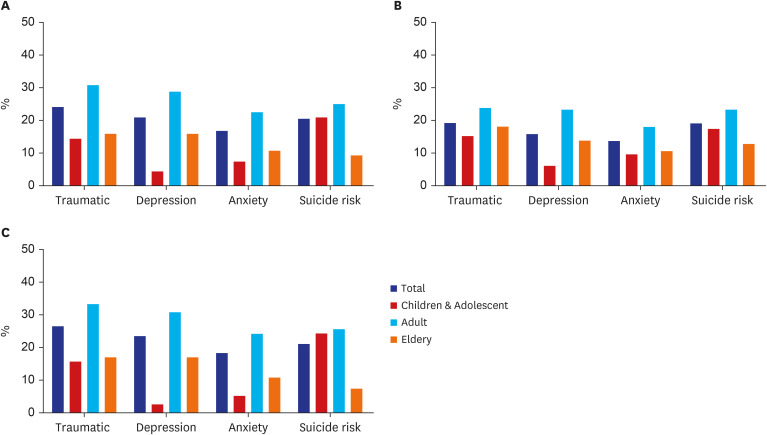
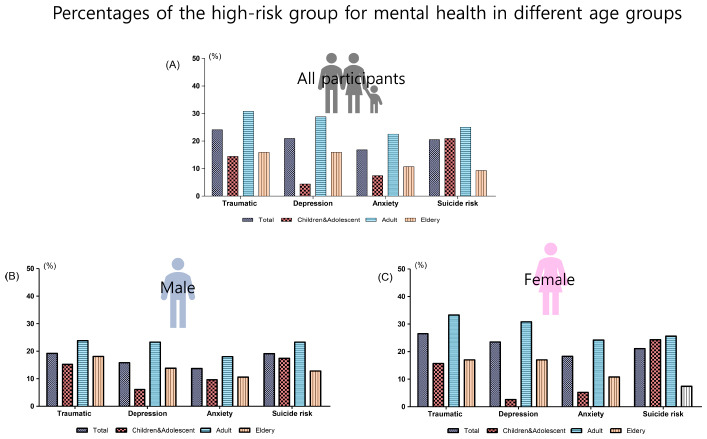
The results showed that 24.7%, 20.9%, 16.8%, and 20.5% of the participants were at high-risk for traumatic stress, depression, anxiety, and suicide, respectively. The difference in the proportion of high-risk groups by age of all participants was significant for traumatic stress, depression, anxiety, and suicide risk. In particular, the percentage of high-risk groups in all areas was the highest in the adult group. Also, in most areas, the ratio of the high-risk groups for children and adolescent group was the lowest, but the suicide risk-related ratio was not (adolescent group: 20.9%, adult group: 25%, elderly group 9.3%).
Conclusion
These results suggest that there is a need for continued interest in the mental health of the general population even after the initial period of coronavirus disease. Additionally, this study may be helpful when considering the resilience or risk factors of mental health in a prolonged disaster situation.
Keywords: COVID-19, Traumatic Stress, Depression, Anxiety, Suicide Risk, Age Differences
Graphical Abstract
INTRODUCTION
Coronavirus disease 2019 (COVID-19), a novel infectious disease, has spread worldwide in 2020. The World Health Organization has declared a public health emergency of international concern over the COVID-19 pandemic. COVID-19 is characterized by rapid human-to-human transmission and varying levels of infection and can cause acute respiratory failure syndrome, leading to the death of a vulnerable person. The world has been confused by the outbreak of new infectious diseases with unknown prognoses and characteristics. Accordingly, the government of each country is taking social isolation measures such as maintaining physical distance, banning social gatherings, and restricting attendance to prevent the spread of COVID-19. In South Korea, social isolation policies such as restrictions on the number of students and a ban on social gatherings continued until February 2021, when vaccination began.
COVID-19 is not a past disaster event that meets the diagnostic criteria for the Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM-5)1 post-traumatic stress disorder (PTSD); however, it is considered another disaster event due to the possibility of infection and indirect exposure through the media.2 Additionally, these new traumatic stressors have been shown to exacerbate other related mental health problems, such as anxiety and depression. Studies on COVID-19 have shown that approximately 13–15% of the general population experience PTSD-like symptoms2,3 even if they are not directly exposed to COVID-19, and approximately 30% of the general population experience depression and anxiety.4 These results are higher than the lifetime prevalence rate (depression: 5.1%, anxiety: 9.3%) of the 2016 Korean Mental Health Survey.5 However, most studies have been conducted in the early stages of the COVID-19 pandemic, and there are few studies on the mid-to-long-term effects of the ongoing pandemic. Therefore, it is necessary to study whether continuous indirect exposure to COVID-19 causes stresses similar to PTSD and other mental health problems such as depression, anxiety, and suicide risk. There is also a need for research into whether traumatic stress responses from COVID-19 are related to other mental health problems.
Additionally, as the COVID-19 pandemic continues, it is becoming more important to identify high-risk mental health groups based on individual factors. Various factors affect mental health, such as age, occupation, and sex. In particular, in the case of COVID-19, the influence of age is considered important. This is because the severity and fatality rate of COVID-19 varies with age,6 and the degree of social isolation according to government guidelines also differs depending on age. Psychiatrically, it can also be caused by different perceptions of illness and death at each step of life.7
Therefore, we hypothesized that the continuous COVID-19 pandemic induces traumatic stress response and other mental health problems due to the disaster situation in the general population and that there is a difference in the degree of influence by age group. Additionally, traumatic stress responses are expected to be associated with other mental health problems such as anxiety and depression in each age group. To confirm this hypothesis, we investigated the level of traumatic stress, depression, anxiety, and suicide risk associated with COVID-19 in the general population of 1,152 individuals, including children and adolescents, adults, and the elderly.
METHODS
Participants and procedure
We collected data from September 1, 2020 to December 31, 2020, using in-person visits and the Gwangmyeong Mental Health Welfare Center's web-based platform. Participants were recruited using online and offline advertisements provided by the Gwangmyeong City Health Center. Participants (n = 1,151, average age = 41.03 ± 24.01 years, men = 33.0%) completed a demographic questionnaire that included age, sex, education, and occupation. Thereafter, participants were divided into three groups: children and adolescents (aged 6–18 years), adults (aged 19–64 years), and the elderly (aged ≥ 65 years). Each group used different combinations of measures, as each scale had a different usable range depending on the age group (children: Primary Care PTSD Screen for DSM-5 [PC-PTSD-5], Children's Depression Inventory [CDI], and Penn State Worry Questionnaire for Children [PSWQ-C]; adolescents: PC-PTSD-5, CDI, Generalized Anxiety Disorder Scale-7 [GAD-7], and P4 screener; adults:PC-PTSD-5, Patient Health Questionnaire-9 [PHQ-9], GAD-7, and P4 screener; and the elderly:PC-PTSD-5, PHQ-9, GAD-7, and P4 screener).
Additionally, they were asked to complete the Korean versions of posttraumatic stress symptoms (PC-PTSD-5),8 depression (PHQ-9 and CDI,9,10 anxiety [GAD-7 and PSWQ-C]11,12), and suicide risk scale [P4 screener]13). The participants of each age group were asked to complete a scale suitable for evaluating that age group, and high-risk groups were identified according to the cutoff of each scale.
Measures
Assessment of PTSD symptoms
The PC-PTSD-514 is a self-report measure that reflects the DSM-5 PTSD diagnostic criteria. Respondents were asked to answer five items (reexperience, avoidance, hyperarousal, paralysis, and negative change) over the past month (0 = no symptom and 1 = experience). Several studies have demonstrated excellent diagnostic accuracy and clinical usefulness in the primary care patient group when using a score of 3 as a screening cutoff.14,15 We used the validated Korean version of the PC-PTSD-58 to investigate the traumatic stress caused by COVID-19 in all age groups, and set three points as the cutoff point that requires additional intervention.
Assessment of depression
The PHQ-916 is a self-reported measure developed using the DSM-5 major depression disorder criteria. Respondents were asked to rate nine items on a four-point Likert scale based on the severity of each symptom (0 = not at all, 1 = several days, 2 = more than half a day, and 3 = nearly every day). It is a reliable and valid measure of depressive symptoms, and a score of 10 is generally used as a cutoff to identify “moderate” levels of depression that require additional intervention.17 We investigated depression in the adult and elderly groups using a validated Korean version of the PHQ-9.9
The CDI18 is a self-reported measure of depression using the Beck Depression Inventory adapted for children and adolescents. Respondents were asked to indicate their status in one of the three sentences for 27 items. According to the total score, it is classified as “no depression,” “mild depression,” “significant depression,” and “severe depression.” In this study, we considered a score of ≥ 26,19 which is a significant depression cutoff, as depression requires psychiatric intervention. We used the Korean version of the CDI10 in children and adolescents aged < 18 years.
Assessment of anxiety
The GAD-720 is a simple self-report measure for those aged 13 years and overdeveloped to screen for anxiety disorders. It is designed with seven questions on a four-point Likert scale (0 = not at all, 1 = several days, 2 = more than half a day, and 3 = nearly every day). Studies have shown that a score of ≥ 10 on the GAD-7 represents a reasonable cutoff for identifying cases of an anxiety disorder.20 We used the Korean version of the GAD-711 to investigate anxiety in adolescent, adult, and elderly groups and considered that there was significant anxiety with a score of ≥ 10.
The PSWQ-C21 is one of the most frequently used scales for measuring uncontrollable worries in children. This is a 14-item self-report tool on a four-point Likert scale with excellent sensitivity and validity (0 = not at all, 1 = sometimes yes, 2 = frequently yes, and 3 = always yes). Respondents were asked to answer how often symptoms were associated with anxiety. We used the Korean version of the PSWQ-C to investigate anxiety in children aged < 12 years, and according to a previous study, a score of ≥ 21 was considered to indicate significant anxiety.12
Assessment of suicide risk
The P4 screener13 evaluates participants through four types of questions (Pre-Q, thought of actually hurting yourself; Q1, past suicidal attempts at any time; Q2, suicide planning; Q3, suicidality; and Q4, preventive factors). Depending on the participant's response, they were classified as having minimal (Pre-Q = “no”), low (Q1 or Q2 = “yes,” Q3 and Q4 = “no”), or high-risk (Q3 = “somewhat likely” or “very likely,” or Q4 = “no”). This tool has the advantage of being able to easily assess suicide risk. We classified the minimal and low-risk groups as the low suicide risk group and high-risk group as the high suicide risk group among the three groups based on the results of the P4 screener. The P4 screener was evaluated in the adolescent, adult, and elderly groups, excluding children.
Statistical analyses
All statistical analyses were performed using SPSS software (version 25.0; SPSS Inc., Chicago, IL, USA). Participants were divided into groups of children and adolescents, adults, and the elderly. Demographic data, means, and standard deviations of traumatic stress, depression, and anxiety scores were obtained for each age group. Thereafter, χ2 analysis was performed to compare the differences in the proportions of the high-risk groups of traumatic stress, depression, anxiety, and suicide risk according to the three age groups. In addition, considering the sex differences in each age group, the differences in the ratio of the high-risk group of traumatic stress, depression, anxiety, and suicide risk by age group were investigated in each of the male and female groups. Finally, Pearson's correlation analyses were performed to investigate the correlation between traumatic stress, depression, and anxiety in each age group. The significance level was set at P < 0.05.
Ethical considerations
The study protocol was approved by the Institutional Review Board of Korea Medical University. Written informed consent was obtained from all participants and legal guardians of children and adolescents (IRB No. 2021GR0165).
RESULTS
Demographics data
A total of 1,151 participants were included in this study. Their average age was 41.04 years, and 33.0% were male individuals. A total of 229 participants (19.9%) were in the children and adolescent group, 652 (56.6%) were in the adult group, and 270 (23.5%) were in the elderly group. The average PC-PTSD-5 scores were 1.32 points for all participants, 0.95 points for the children and adolescent group, 1.59 points for the adult group, and 0.98 points for the elderly group. Based on the results of the PHQ-9, which is a measure of depression in the adult and elderly groups, the adult group scored 6.77 points and the elderly group scored 4.65 points. The CDI score of the children and adolescent group was 7.81. The average anxiety scores evaluated by the GAD-7 were 2.77 points for the adolescent group, 5.44 points for the adult group, and 2.88 points for the elderly group. Additionally, the average anxiety score of the children group evaluated by the PSWQ-C was 8.99 points. Further details are provided in Table 1.
Table 1. Demographic data of participants.
| Data | Children and adolescent (n = 229) | Adult (n = 652) | Elderly (n = 270) | Total (n = 1,151) | |
|---|---|---|---|---|---|
| Age | 10.22 ± 4.05 | 37.53 ± 12.37 | 75.62 ± 6.43 | 41.04 ± 24.01 | |
| Sex | |||||
| Male | 114 (49.8) | 172 (26.4) | 94 (34.8) | 380 (33.0) | |
| Female | 115 (50.2) | 480 (73.6) | 176 (65.2) | 771 (67.0) | |
| Survey method | |||||
| Face to face | 163 (71.2) | 323 (49.5) | 265 (98.1) | 751 (65.2) | |
| Online | 66 (28.8) | 329 (50.5) | 5 (1.9) | 400 (34.8) | |
| Occupation | |||||
| Unemployed | 108 (16.6) | 155 (57.0) | 263 (28.5) | ||
| Self-employed | 31 (4.8) | 4 (1.5) | 35 (3.8) | ||
| Employee | 304 (46.6) | 10 (3.7) | 314 (34.1) | ||
| Housekeeper | 105 (16.6) | 60 (22.2) | 165 (17.9) | ||
| Student | 83 (12.7) | 0 (0.0) | 83 (9.0) | ||
| Education | |||||
| Illiterate | 5 (0.8) | 28 (11.6) | 33 (3.9) | ||
| Elementary | 10 (1.6) | 73 (30.2) | 83 (9.8) | ||
| Junior high school | 19 (3.1) | 55 (22.7) | 74 (8.7) | ||
| High school | 215 (35.4) | 66 (27.3) | 281 (33.1) | ||
| University | 358 (59.0) | 20 (8.2) | 378 (44.6) | ||
| PC-PTSD-5 | 0.95 ± 1.36 | 1.59 ± 1.78 | 0.98 ± 1.41 | 1.32 ± 1.65 | |
| PHQ-9 | 6.77 ± 7.09 | 4.65 ± 5.89 | |||
| CDI | 7.81 ± 8.20 | ||||
| GAD-7 | 2.77 ± 4.18a | 5.44 ± 5.87 | 2.88 ± 4.57 | ||
| PSWQ-C | 8.99 ± 7.03b | ||||
Data are shown as mean ± standard deviation or number (%).
Data are represented as below: children and adolescent, 6–18 years; adult, 19–64 years; elderly, ≥ 65 years.
PC-PTSD-5 = Primary Care Posttraumatic Stress Disorder Screen for DSM-5, PHQ-9 = Patient Health Questionnaire-9, CDI = Children's Depression Inventory, GAD-7 = Generalized Anxiety Disorder Scale-7, PSWQ-C = Penn State Worry Questionnaire for Children.
aResult of the adolescent group (n = 139); bResult of the children group (n = 90).
High-risk groups for each measure in different age groups
Of a total of 1,151 participants, 24.1% (n = 277) scored above the PC-PTSD-5 cutoff. The proportion of the high-risk group for traumatic stress in each group was 14.4% (n = 33) in the children and adolescent group, 30.8% (n = 201) in the adult group, and 15.9% (n = 43) in the elderly group (P < 0.001).
Of the 1,151 participants, 20.9% (n = 241) experienced significant depression. In each group, the rate of the high-risk group for depression was 4.4% (n = 10) in the children and adolescent group, 28.8% (n = 188) in the adult group, and 15.9% (n = 43) in the elderly group (P < 0.001).
A total of 16.8% (n = 193) of all participants reported anxiety symptoms requiring additional intervention. A total of 7.4% (n = 17) of the children and adolescent group, 22.5% (n = 145) of the adult group, and 10.7% (n = 29) of the elderly group were at high-risk of anxiety (P < 0.001).
A total of 20.5% (n = 217) of all participants were assessed as a high-risk group for suicide. We found that 20.9% (n = 29) of the adolescent group, 25.0% (n = 163) of the adult group, and 9.3% (n = 25) of the elderly group had a high suicide risk (P < 0.001). Additionally, the proportion of past suicidal attempts, one of the P4 screening items, was 5.7% (n = 8) in the adolescent group, 13.3% (n = 87) in the adult group, and 6.2% (n = 17) in the elderly group. More details are illustrated in Table 2 and Fig. 1.
Table 2. Percentages of a high-risk group for mental health in the general population by age group.
| Mental health problems | Total | Children and adolescent | Adult | Elderly | P value | |
|---|---|---|---|---|---|---|
| All participants | (n = 1,151) | (n = 229) | (n = 652) | (n = 270) | ||
| Traumatic stress | 277 (24.1) | 33 (14.4) | 201 (30.8) | 43 (15.9) | < 0.001 | |
| Depression | 241 (20.9) | 10 (4.4) | 188 (28.8) | 43 (15.9) | < 0.001 | |
| Anxiety | 193 (16.8) | 17 (7.4) | 147 (22.5) | 29 (10.7) | < 0.001 | |
| Suicide risk | 217 (20.5) | 29 (20.9)a | 163 (25.0) | 25 (9.3) | < 0.001 | |
| Male group | (n = 380) | (n = 114) | (n = 172) | (n = 94) | ||
| Traumatic stress | 73 (19.2) | 15 (15.2) | 41 (23.8) | 17 (18.1) | 0.077 | |
| Depression | 60 (15.8) | 7 (6.1) | 40 (23.3) | 13 (13.8) | < 0.001 | |
| Anxiety | 52 (13.7) | 11 (9.6) | 31 (18.0) | 10 (10.6) | 0.080 | |
| Suicide risk | 64 (19.1) | 12 (17.4) a | 40 (23.3) | 12 (12.8) | 0.106 | |
| Female group | (n = 771) | (n = 115) | (n = 480) | (n = 176) | ||
| Traumatic stress | 204 (26.5) | 18 (15.7) | 160 (33.3) | 26 (14.8) | < 0.001 | |
| Depression | 181 (23.5) | 3 (2.6) | 148 (30.8) | 30 (17.0) | < 0.001 | |
| Anxiety | 141 (18.3) | 6 (5.2) | 116 (24.2) | 19 (10.8) | < 0.001 | |
| Suicide risk | 153 (21.1) | 17 (24.3)a | 123 (25.6) | 13 (7.4) | < 0.001 | |
Values are presented as number (%).
Data are represented as below: children and adolescents, 6–18 years; adult, 19–64 years; elderly, ≥ 65 years; high-risk group, primary care posttraumatic stress disorder screen for DSM-5 ≥ 3; Patient Health Questionnaire-9 ≥ 10; Children's Depression Inventory ≥ 26; Generalized Anxiety Disorder Scale-7 ≥ 10; Penn State Worry Questionnaire for Children ≥ 21.
aResults of the adolescent group (n = 139; male = 69; female = 70).
Fig. 1. Percentages of high-risk groups for mental health in different age groups (A) Percentages of the high-risk group for mental health in all participants. (B) Percentages of the high-risk group for mental health in male participants. (C) Percentages of the high-risk group for mental health in female participants.
Comparison of the proportion of high-risk groups for each measure in different age groups by sex
Of the 380 male participants, 19.2% (n = 73) were at a high-risk of traumatic stress. A total of 15.2% (n = 15) of the children and adolescent group, 23.8% (n = 41) of the adult group, and 18.1% (n = 17) of the elderly group were investigated as a high-risk group for traumatic stress (P = 0.077). The proportion of male participants in the high-risk group for depression was 15.8% (n = 60). We observed that 6.1% (n = 7) of the children and adolescent group, 23.3% (n = 40) of the adult group, and 13.8% (n = 13) of the elderly group were at high-risk for depression (P < 0.001). A total of 13.7% (n = 52) of the male participants were classified into the high-risk anxiety group. The proportion of the high-risk group for anxiety was 9.6% (n = 11) in the children and adolescent group, 18.0% (n = 31) in the adult group, and 10.6% (n = 10) in the elderly group (P = 0.080). We found that 19.1% (n = 64) of all male participants, 17.4% (n = 12) of the children and adolescent group, 23.3% (n = 40) of the adult group, and 12.8% (n = 12) of the elderly group were at high-risk of suicide (P = 0.106). The details are presented in Table 2 and Fig. 1.
From the analysis of 771 female participants, the high-risk group for traumatic stress was 26.5% (n = 104). A total of 15.7% (n = 18) of the children and adolescent group, 33.3% (n = 160) of the adult group, and 14.8% (n = 26) of the elderly group reported a high-risk of traumatic stress (P < 0.001). Of the female participants, 23.5% (n = 181) were evaluated as having a high-risk of depression. In addition, 2.6% (n = 3) of the children and adolescent group, 30.8% (n = 148) of the adult group, and 17.0% (n = 30) of the elderly group were at high-risk for depression (P < 0.001). The proportion of female participants evaluated as having high-risk anxiety was 18.3% (n = 141); 5.2% (n = 6) of the children and adolescent group, 24.2% (n = 116) of the adult group, and 10.8% (n = 19) of the elderly group were evaluated as high-risk anxiety groups (P < 0.001). Finally, 21.1% (n = 153) of all female participants, 24.3% (n = 17) of the adolescent group, 25.6% (n = 123) of the adult group, and 7.4% (n = 13) of the elderly group had a high suicide risk (P < 0.001). The details are presented in Table 2 and Fig. 1.
Pearson's correlation between traumatic stress, depression, and anxiety measures
In the children and adolescent group, a significant positive correlation was observed as a result of the correlation analysis between the PC-PTSD-5 and CDI scores (r = 0.41, P < 0.001). The PC-PTSD-5 and PSWQ-C scores (r = 0.53, P < 0.001), and the CDI and PSWQ-C scores (r = 0.68, P < 0.001) in the children group were positively correlated. In the adolescent group, the PC-PTSD-5 and GAD-7 scores (r = 0.45, P < 0.001), CDI score, and GAD score (r = 0.46, P < 0.001) also showed a positive correlation.
As a result of the correlation analysis in the adult group, significant positive correlations were found in the PC-PTSD-5 and PHQ-9 scores (r = 0.64, P < 0.001), PC-PTSD-5 score, and GAD-7 score (r = 0.68, P < 0.001), and PHQ-9 and GAD-7 scores (r = 0.88, P < 0.001).
Similarly, in the elderly group, a positive correlation was observed between the PC-PTSD-5 and PHQ-9 scores (r = 0.48, P < 0.001), PC-PTSD-5 and GAD-7 scores (r = 0.57, P < 0.001), and PHQ-9 and GAD-7 scores (r = 0.82, P < 0.001), which were statistically significant. The results of the correlation analysis are presented in Table 3.
Table 3. Pearson's correlation between symptoms of traumatic stress, depression, and anxiety.
| Age group | Research tools | CDI | PSWQ-C |
|---|---|---|---|
| Children | PTSD-PC-5 | 0.41a (< 0.001) | 0.53 (< 0.001) |
| CDI | 0.68 (< 0.001) | ||
| CDI | GAD-7 | ||
| Adolescent | PTSD-PC-5 | 0.41a (< 0.001) | 0.46 (< 0.001) |
| CDI | 0.53 (0.00) | ||
| PHQ-9 | GAD-7 | ||
| Adult | PTSD-PC-5 | 0.64 (< 0.001) | 0.68 (< 0.001) |
| PHQ-9 | 0.88 (< 0.001) | ||
| Elderly | PTSD-PC-5 | 0.48 (< 0.001) | 0.57 (< 0.001) |
| PHQ-9 | 0.82 (< 0.001) |
Values are presented as Pearson's r (P value).
Data are represented as below: children and adolescents, 6–18 years; adult, 19–64 years; elderly = ≥ 65 years.
PTSD-PC-5 = Primary Care Posttraumatic Stress Disorder Screen for DSM-5, CDI = Children's Depression Inventory, PSWQ-C = Penn State Worry Questionnaire for Children, PHQ-9 = Patient Health Questionnaire-9, GAD-7 = Generalized Anxiety Disorder Scale-7.
aResults of the children and adolescents group.
DISCUSSION
This study investigated the proportion of high-risk groups of traumatic stress, depression, anxiety, and suicide risk among residents in urban areas in South Korea, and the difference in the proportion of high-risk groups by age during the COVID-19 pandemic. The results showed that 24.7% of the participants were at high-risk for traumatic stress, 20.9% were at high-risk for depression, 16.8% were at high-risk for anxiety, and 20.5% were at high-risk for suicide. The difference in the proportion of high-risk groups by age group of all participants was significant for traumatic stress, depression, anxiety, and suicide risk. After stratifying by sex, in male participants, there was a difference in the proportion of high-risk groups between age groups, which was significant for depression alone. In female participants, significant differences in the distribution of high-risk groups among age groups were observed for traumatic stress, depression, anxiety, and suicide risk. Additionally, significant positive correlations were observed between traumatic stress, depression, and anxiety in all age groups.
COVID-19 is not a traumatic event, such as a traffic accident or a natural disaster; however, it is considered another disaster situation due to the possibility of infection, unpredictable disease progression, and social isolation.2 Thus, there has been increased interest in the impact on the mental health of the uninfected general population, and several studies have reported an increased risk of mental health during the COVID-19 pandemic.2,3,4 It is difficult to compare the proportions of the high-risk mental health groups of previous studies to the proportions of our study as the COVID-19-related situation in each country is not the same and different assessment tools were used between studies. However, the results consistently show that the proportions of groups at high-risk of traumatic stress, depression, anxiety, and suicide in the COVID-19 pandemic are higher than the generally known prevalence. Moreover, through the high positive correlation between COVID-19-related traumatic stress and other mental health, we may be able to predict changes in mental health in the general population after the COVID-19 pandemic.
Along with the interest in the impact of COVID-19 on mental health, there is also an increasing interest in personal factors that can be considered risk or resilience factors. Among them, age is one of the basic factors of an individual. In studies comprising children and adolescents alone, several experts have expressed concerns regarding their mental health following the prolonged COVID-19 pandemic.22,23 A study in the early stages of COVID-19 reported that 22.6% of children experienced symptoms of depression, and 18.9% of them experienced symptoms of anxiety.24 In contrast, we found that traumatic stress in children and adolescents due to COVID-19 was observed in 14.4%; however, the high-risk group for depression comprised 4.4%, and the high-risk group for anxiety comprised 7.4%. These results are not significantly different from the mental health levels (depression: 3.1%, anxiety: 7.2%) suggested by the Centers for Disease Control and Prevention of the United States before the COVID-19 pandemic.25 Adversity in children and adolescents is an important factor in the development of resilience in handling various stresses. This resilience is related to general adaptive systems, such as relationships with competent and warmly caring adults, effective community relationships, and self-belief.26 Dvorsky et al.27 suggested that individuals, families, communities and governments working together to mobilize capacity in response to COVID-19 will help children and adolescents develop resilience. Additionally, for children and adolescents who had faced challenges in the traditional school system, the current situation can be an opportunity to learn at an individual pace, increase self-efficacy, and develop new abilities, giving greater control over life. Therefore, the results of this study may have reflected the adaptability and resilience of children and adolescents in that the study was conducted during the mid-to-long-term period of the COVID-19 pandemic. However, traumatic stress associated with COVID-19 was observed in 14.1% of children and adolescents, and traumatic stress is highly correlated with other mental health problems. In addition, considering previous studies that show that younger children and adolescents have more behavioral problems than emotional problems in the COVID- 19 pandemic,28 mental health problems in children and adolescents may have been underestimated due to self-report assessment of emotional difficulties.
In particular, the ratio of high-risk group with suicide risk among adolescents was 20.9%, which is not consistent with the relatively low ratio of high-risk groups for other mental issues. This result is higher than the 12.4% in a previous study before COVID-19 pandemic,29 which defined adolescents who had attempted suicide or suicidal idea in the past year as a high-risk group. It was also found that 5.7% of the adolescent group attempted suicide. This is about 1.8 times higher than the result of a suicide attempt rate survey among Korean adolescents in 2018,30 before the COVID-19 pandemic. Taken together, we suggest that the proportion of adolescents reported of depression and anxiety may not increase during the prolonged COVID-19 pandemic, but nonfunctional coping methods such as suicide may increase regardless of the severity of mental issues.
As a result of this study, the highest percentage of the high-risk groups was observed in the adult group in all assessments. Additionally, the proportion of the high-risk groups for COVID-19-related traumatic stress observed in the adult group was higher than 13–15%, as suggested in previous studies on COVID-19.2,3 According to the Stress in America 2020, it was reported that young adults had the greatest long-term potential consequences of pandemic trauma among adults, and the highest stress was observed in adults aged 18–23 years compared with other generations.31 Additionally, as age increases in adults, stress levels tend to decrease. Younger adults are at a pivotal moment in their lives, and experiencing adulthood at a moment when the future appears uncertain can be the cause of great stress. Birditt et al.32 suggested that young adults may be relatively more vulnerable, with younger people having more pandemic-related stress, more life changes, more social isolation, and higher quality of negative relationships than older people. In addition, the reasons for higher mental distress in the adult population may include lower social support and economic obligations compared with that in the elderly, children, and adolescents. Alternatively, adults have a responsibility to continue their lives in the face of COVID-19 and to support their children and parents. The adult group play a potential role in the mental health of all age groups, as a model for children and adolescents and as an emotional support system for the elderly. Therefore, it will be necessary to intervene the mental health problems of the adult group in order to prevent the mental health risks of all age groups due to COVID-19.
Previous studies have reported relatively consistently fewer negative outcomes related to mental health in the COVID-19 pandemic situation in the elderly group than in the young adult group,32,33 which is consistent with our findings. The paradox of aging, which tends to maintain or to improve emotional stability, has already been reported.34 The paradox of aging applies even in disaster situations. As a result of studies related to the 9/11 terrorist attacks, less mental distress, less fear of future attacks, and a sharp decrease in PTSD prevalence over time was observed in older adults.35 Although COVID-19 has a higher mortality rate in the elderly population,6 as the disaster situation prolongs, the elderly may focus on positive things and choose activities that reduce stress.36 Additionally, there is a hypothesis that the elderly experience high perceived family support due to their limited time in life,37 and these characteristics of the elderly are associated with high resilience and low mental distress in COVID-19 situations.38 Moreover, considering that overexposure to COVID-19-related information through the media increases stress or anxiety,39,40 lesser media use in the elderly group than in the adult group may also have an impact.
This study has some limitations. First, this study used self-reported questionnaires for those who accessed the health center homepage. Second, it is a cross-sectional study that cannot reflect changes and causal relationships in the COVID-19 pandemic situation. Third, there is a possibility that it may not reflect the general population because the proportion of female in the adult and elderly groups is high. Therefore, we additionally performed sex-stratified comparison of the age group. And, the tendency for mental health issues by age group was maintained. Forth, differences in the proportion between face-to-face and non-face-to-face survey methods by age groups may have affected attitudes towards mental issues related to social desirability. However, there is no consistent study on the difference in results according to the survey method, and there is also a study that the survey method and social desirability are not related.41 Fifth, compared with other mental health issues, the proportion of high-risk groups with suicide risk is higher, particularly in adolescents. There is a limitation that sensitivity and specificity of the Korean version of P4 screener have not yet been evaluated for the South Korean population. Additionally, it is possible that the participants of this study, especially the adolescents, did not clearly distinguish the intention of self-harm from the pre-question “thought of actually hurting yourself”. However, considering that suicide ranks higher among the causes of death among adolescents than among other age groups42 and that many people who have considered or attempted suicide for the first time in their lives did so in adolescence,43 the high-risk of suicide among adolescents may be a meaningful outcome. In addition, this study has the strength of examining mental health after the initial stage of the COVID-19 pandemic in a large number of participants. Moreover, this is the first study to compare participants according to age group, including children and adolescents.
Therefore, according to the results of this study, there is a need for continued interest in the increase in traumatic stress, depression, anxiety, and suicide risk observed even after the initial period of COVID-19. Additionally, this study may be helpful when considering the resilience or risk factors of mental health in a prolonged disaster situation.
ACKNOWLEDGMENTS
The authors would like to thank all the participants in our study.
Footnotes
Funding: This research was supported by the COVID-19 Disaster Psychological Support Program through Gwangmyeong Mental Health Welfare Center funded by Gwangmyeong City Health Center in 2020.
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Ko M, Lee MS.
- Data curation: Ko M, Cho HM.
- Formal analysis: Ko M, Cho HM, Park J, Chi S, Han C.
- Funding acquisition: Yi HS.
- Methodology: Ko M, Cho HM, Lee MS.
- Writing - original draft: Ko M, Lee MS.
- Writing - review & editing: Lee MS.
References
- 1.American Psychological Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®) 5th ed. Washington, D.C., USA: American Psychiatric Association; 2013. [Google Scholar]
- 2.Bridgland VM, Moeck EK, Green DM, Swain TL, Nayda DM, Matson LA, et al. Why the COVID-19 pandemic is a traumatic stressor. PLoS One. 2021;16(1):e0240146. doi: 10.1371/journal.pone.0240146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.González-Sanguino C, Ausín B, Castellanos MÁ, Saiz J, López-Gómez A, Ugidos C, et al. Mental health consequences during the initial stage of the 2020 coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun. 2020;87:172–176. doi: 10.1016/j.bbi.2020.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Salari N, Hosseinian-Far A, Jalali R, Vaisi-Raygani A, Rasoulpoor S, Mohammadi M, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Global Health. 2020;16(1):57. doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hong J, Lee D, Ham B, Lee S, Sung S, Yoon T. The Survey of Mental Disorders in Korea. Sejong, Korea: Ministry of Health & Welfare; 2017. [Google Scholar]
- 6.O'Driscoll M, Ribeiro Dos Santos G, Wang L, Cummings DAT, Azman AS, Paireau J, et al. Age-specific mortality and immunity patterns of SARS-CoV-2. Nature. 2021;590(7844):140–145. doi: 10.1038/s41586-020-2918-0. [DOI] [PubMed] [Google Scholar]
- 7.Chopik WJ. Death across the lifespan: age differences in death-related thoughts and anxiety. Death Stud. 2017;41(2):69–77. doi: 10.1080/07481187.2016.1206997. [DOI] [PubMed] [Google Scholar]
- 8.Jung YE, Kim D, Kim WH, Roh D, Chae JH, Park JE. A brief screening tool for PTSD: validation of the Korean version of the primary care PTSD screen for DSM-5 (K-PC-PTSD-5) J Korean Med Sci. 2018;33(52):e338. doi: 10.3346/jkms.2018.33.e338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Park SJ, Choi HR, Choi JH, Kim K, Hong JP. Reliability and validity of the Korean version of the Patient Health Questionnaire-9 (PHQ-9) Anxiety Mood. 2010;6(2):119–124. [Google Scholar]
- 10.Cho SC, Lee YS. Development of the Korean form of the Kovacs' Children's Depression Inventory. J Korean Neuropsychiatr Assoc. 1990;29(4):943–956. [Google Scholar]
- 11.Seo JG, Park SP. Validation of the Generalized Anxiety Disorder-7 (GAD-7) and GAD-2 in patients with migraine. J Headache Pain. 2015;16(1):97. doi: 10.1186/s10194-015-0583-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kang SG, Shin JH, Song SW. Reliability and validity of the Korean version of the Penn State Worry Questionnaire in primary school children. J Korean Med Sci. 2010;25(8):1210–1216. doi: 10.3346/jkms.2010.25.8.1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dube P, Kurt K, Bair MJ, Theobald D, Williams LS. The p4 screener: evaluation of a brief measure for assessing potential suicide risk in 2 randomized effectiveness trials of primary care and oncology patients. Prim Care Companion J Clin Psychiatry. 2010;12(6):e1–e8. doi: 10.4088/PCC.10m00978blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Prins A, Bovin MJ, Smolenski DJ, Marx BP, Kimerling R, Jenkins-Guarnieri MA, et al. The primary care PTSD screen for DSM-5 (PC-PTSD-5): development and evaluation within a veteran primary care sample. J Gen Intern Med. 2016;31(10):1206–1211. doi: 10.1007/s11606-016-3703-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bovin MJ, Kimerling R, Weathers FW, Prins A, Marx BP, Post EP, et al. Diagnostic accuracy and acceptability of the Primary Care Posttraumatic Stress Disorder Screen for the Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition) among US veterans. JAMA Netw Open. 2021;4(2):e2036733. doi: 10.1001/jamanetworkopen.2020.36733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Manea L, Gilbody S, McMillan D. Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): a meta-analysis. CMAJ. 2012;184(3):E191–E196. doi: 10.1503/cmaj.110829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kovacs M. The Children's Depression, Inventory (CDI) Psychopharmacol Bull. 1985;21(4):995–998. [PubMed] [Google Scholar]
- 19.Bang YR, Park JH, Kim SH. Cut-off scores of the children's depression inventory for screening and rating severity in Korean adolescents. Psychiatry Investig. 2015;12(1):23–28. doi: 10.4306/pi.2015.12.1.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 21.Chorpita BF, Tracey SA, Brown TA, Collica TJ, Barlow DH. Assessment of worry in children and adolescents: an adaptation of the Penn State Worry Questionnaire. Behav Res Ther. 1997;35(6):569–581. doi: 10.1016/s0005-7967(96)00116-7. [DOI] [PubMed] [Google Scholar]
- 22.Jiao WY, Wang LN, Liu J, Fang SF, Jiao FY, Pettoello-Mantovani M, et al. Behavioral and emotional disorders in children during the COVID-19 epidemic. J Pediatr. 2020;221:264–266.e1. doi: 10.1016/j.jpeds.2020.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oosterhoff B, Palmer CA, Wilson J, Shook N. Adolescents' motivations to engage in social distancing during the COVID-19 pandemic: associations with mental and social health. J Adolesc Health. 2020;67(2):179–185. doi: 10.1016/j.jadohealth.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xie X, Xue Q, Zhou Y, Zhu K, Liu Q, Zhang J, et al. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatr. 2020;174(9):898–900. doi: 10.1001/jamapediatrics.2020.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ghandour RM, Sherman LJ, Vladutiu CJ, Ali MM, Lynch SE, Bitsko RH, et al. Prevalence and treatment of depression, anxiety, and conduct problems in US children. J Pediatr. 2019;206:256–267.e3. doi: 10.1016/j.jpeds.2018.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Masten AS. Ordinary magic. Resilience processes in development. Am Psychol. 2001;56(3):227–238. doi: 10.1037//0003-066x.56.3.227. [DOI] [PubMed] [Google Scholar]
- 27.Dvorsky MR, Breaux R, Becker SP. Finding ordinary magic in extraordinary times: child and adolescent resilience during the COVID-19 pandemic. Eur Child Adolesc Psychiatry. 2021;30:1829–1831. doi: 10.1007/s00787-020-01583-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schmidt SJ, Barblan LP, Lory I, Landolt MA. Age-related effects of the COVID-19 pandemic on mental health of children and adolescents. Eur J Psychotraumatol. 2021;12(1):1901407. doi: 10.1080/20008198.2021.1901407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jung JS, Park SJ, Kim EY, Na KS, Kim YJ, Kim KG. Prediction models for high risk of suicide in Korean adolescents using machine learning techniques. PLoS One. 2019;14(6):e0217639. doi: 10.1371/journal.pone.0217639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ministry of Education, Ministry of Health and Welfare, Korea Centers for Disease Control and Prevention. The 14th (2018) Korea Youth Risk Behavior Web-based Survey Statistics. Seoul, Korea: Ministry of Education, Ministry of Health and Welfare; 2018. [Google Scholar]
- 31.American Psychological Association. Stress in America 2020: a National Mental Health Crisis. Washington, D.C., USA: American Psychiatric Association; 2020. [Google Scholar]
- 32.Birditt KS, Turkelson A, Fingerman KL, Polenick CA, Oya A. Age differences in stress, life changes, and social ties during the COVID-19 pandemic: Implications for psychological well-being. Gerontologist. 2021;61(2):205–216. doi: 10.1093/geront/gnaa204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bruine de Bruin W. Age differences in COVID-19 risk perceptions and mental health: evidence from a national US survey conducted in March 2020. J Gerontol B Psychol Sci Soc Sci. 2021;76(2):e24–e29. doi: 10.1093/geronb/gbaa074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Carstensen LL. Integrating cognitive and emotion paradigms to address the paradox of aging. Cogn Emotion. 2019;33(1):119–125. doi: 10.1080/02699931.2018.1543181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Scott SB, Poulin MJ, Silver RC. A lifespan perspective on terrorism: age differences in trajectories of response to 9/11. Dev Psychol. 2013;49(5):986–998. doi: 10.1037/a0028916. [DOI] [PubMed] [Google Scholar]
- 36.Neubauer AB, Smyth JM, Sliwinski MJ. Age differences in proactive coping with minor hassles in daily life. J Gerontol B Psychol Sci Soc Sci. 2019;74(1):7–16. doi: 10.1093/geronb/gby061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Carstensen LL. Evidence for a life-span theory of socioemotional selectivity. Curr Dir Psychol Sci. 1995;4(5):151–156. doi: 10.1177/09637214211011468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li F, Luo S, Mu W, Li Y, Ye L, Zheng X, et al. Effects of sources of social support and resilience on the mental health of different age groups during the COVID-19 pandemic. BMC Psychiatry. 2021;21(1):16. doi: 10.1186/s12888-020-03012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 2020;33(2):e100213. doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.World Health Organization. Mental Health and Psychosocial Considerations during the COVID-19 Outbreak. Geneva, Switzerland: World Health Organization; 2020. [Google Scholar]
- 41.Fox S, Schwartz D. Social desirability and controllability in computerized and paper-and-pencil personality questionnaires. Comput Human Behav. 2002;18(4):389–410. [Google Scholar]
- 42.Cha CB, Franz PJ, M Guzmán E, Glenn CR, Kleiman EM, Nock MK. Annual Research Review: suicide among youth - epidemiology, (potential) etiology, and treatment. J Child Psychol Psychiatry. 2018;59(4):460–482. doi: 10.1111/jcpp.12831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry. 1999;56(7):617–626. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]