Abstract
Hypertension is the leading single contributor to all-cause death and disability worldwide. However, there is scarce evidence on the prevalence and risk factors of hypertension for Chinese youth. This study aimed to investigate the prevalence of hypertension among Chinese college freshmen and to identify the influencing factors. We conducted a cross-sectional study of all freshmen from 2015 to 2017 at a university in Wuhan, China by physical examination and standard-structured questionnaire. The Pearson chi-square test was used to compare categorical variables. Forward stepwise logistic regression method was used in the multivariate analysis to identify independent predictors of hypertension in youth. A total of 12,849 participants were included, and the prevalence of hypertension of Chinese college freshmen was 4.3% (7.9% in men and 1.6% in women). Men had a higher risk of hypertension than women (odds ratio [OR]: 5.358, 95% confidence interval [CI]: 4.345–6.607, P < 0.001). Obese people were more likely to develop hypertension than those with normal body mass index (OR: 10.465, 95% CI: 8.448–12.964, P < 0.001). People with elevated resting heart rate (RHR) had a higher prevalence of hypertension (OR: 4.987, 95% CI: 3.641–6.832, P < 0.001). Staying up late (OR: 2.957, 95% CI: 2.482–3.523, P < 0.001), physical inactivity (OR: 4.973, 95% CI: 4.141–5.972, P < 0.001), living in urban district (OR: 1.864, 95% CI: 1.493–2.329, P < 0.001) and family history of cardiovascular diseases (CVDs) (OR: 2.685, 95% CI: 2.108–3.421, P < 0.001) were related to higher prevalence of hypertension in youth. Male, obesity, elevated RHR, physical inactivity and family history of CVDs were identified as important risk factors of hypertension in youth. These risk factors should be given more attention when designing and implementing the interventional programs.
Subject terms: Cardiology, Health care, Risk factors
Introduction
Cardiovascular diseases (CVDs, including coronary heart disease, heart failure, stroke, myocardial infarction and atrial fibrillation etc.) are the most common non-communicable diseases globally and responsible for estimated 17.9 million deaths each year1,2, which caused an increasing burden to the society and families. Although CVDs are usually detected in the elderly, the disease development process that cannot be observed obviously may occur at a younger age, and there is an increasing tendency of mortality among the young3,4. Hypertension, as the most common preventable risk factor for CVDs, is the leading single contributor to all-cause death and disability worldwide5. Increasing studies have provided ample evidence that some adult hypertension develops in childhood, meaning that children and adolescents with elevated blood pressure tend to end up as adults with recognizable hypertension6,7. From a public health point of view, the prevention and control of hypertension are essential to maintain and promote human health, particularly in childhood.
In China, the prevalence of hypertension among youth rose from 1.6%8 in 2004 to 4.0%9 in 2015, but there is scarce evidence on the prevalence and risk factors of hypertension for Chinese youth. The aim of the cross-sectional study was to investigate the prevalence of hypertension of college freshmen as well as its influencing factors, which would provide scientific bases for the primary prevention of CVDs. We hope to awaken the students’ attention to take active measures to keep their blood pressure within the normal range.
Methods
Ethics statement
Our study was approved by the Research Ethics Committee in Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China. All study subjects understood the purpose of this survey and signed informed consent forms. All identifiable personal information was removed for privacy protection. All methods were performed in accordance with the Declaration of Helsinki.
Settings and study subjects
The cross-sectional study was an investigation of the prevalence of hypertension among college freshmen and the influencing factors associated with it. We investigated all the freshmen of a university in Wuhan, China from 2015 to 2017, who had graduated from high schools all over China. Finally, we identified 12,849 college freshmen to take part in our survey, not including students who were demoted to the freshman from other grades.
Data collection
Organized by the college as a unit, college freshmen had orderly physical examinations and standard-structured questionnaires. Physical examination included height, weight, resting heart rate (RHR), systolic blood pressure (SBP) and diastolic blood pressure (DBP) and so on. Based on literature research and expert consultation, standard-structured questionnaires were designed and distributed to the participants. The contents of the questionnaire were as follows: enrollment year, gender, age, residence, region, whether they exercised at least 150 min per week, whether they slept less than six hours per day, and whether they had a family history of CVDs (first-degree relatives had a history of CVDs). Height and weight were measured using a calibrated scale and a stadiometer, with the participants barefoot and in light clothing. After the participants had been seated and rested for five minutes, blood pressure and RHR were measured three times by an Omron HEM-705P arm-type electronic sphygmomanometer, with an interval of no less than two minutes between every two measurements. The average of the last two readings was taken in the analysis.
Definition of hypertension
According to the diagnostic criteria of Chinese Guidelines for The Prevention and Treatment of Hypertension10, we divided SBP < 120 mmHg and DBP < 80 mmHg as normal blood pressure, 120 mmHg ≤ SBP < 140 mmHg and/or 80 mmHg ≤ DBP < 90 mmHg as normal high blood pressure, and SBP ≥ 140 mmHg and/or DBP ≥ 90 mmHg as hypertension. Our current study aimed to explore the factors affecting hypertension, so we combined normal blood pressure and normal high blood pressure as the contrary of hypertension.
Explanatory variables
Most of the variables were self-explanatory, but a few needed explanations. Based on the formula for calculating the body mass index (BMI), we calculated the value of BMI of each participant and classified them according to the diagnostic criteria for overweight and obesity in Chinese adults11. We classified BMI between 18.5 and 23.9 kg/m2 as normal weight, BMI between 24 and 27.9 kg/m2 as overweight, and BMI ≥ 28 kg/m2 as obesity; the classification standards for minors referred to Table 1. According to the normal range of RHR , RHR < 60 beats/min was defined as bradycardia, RHR between 60 beats/min and 100 beats/min was defined as normal heart rate, and RHR > 100 beats/min was defined as tachycardia12. We defined RHR greater than 100 beats/min as elevated RHR, and the others were the contrary. Adequate physical activity was defined as more than 150 min of exercise per week. Stay up late was defined as less than 6 h of sleep duration per day.
Table 1.
Guidelines for the prevention and control of overweight and obesity in school-age children in China.
| Age, years old | Overweight (BMI, kg/m2) | Obesity (BMI, kg/m2) | ||
|---|---|---|---|---|
| Male | Female | Male | Female | |
| 15 | 23.1 | 23.4 | 26.9 | 26.9 |
| 16 | 23.5 | 23.7 | 27.4 | 27.4 |
| 17 | 23.8 | 23.8 | 27.8 | 27.7 |
Statistical analysis
Data from physical examinations and questionnaires were recorded into Excel 2016 and statistical analysis was performed by the SPSS 22. The quantitative data were presented in form of mean ± standard deviation (SD), and the qualitative data were presented in form of percentage. The one-way ANOVA and the t test were performed to evaluate continuous data. Pearson chi-square tests were used to compare categorical variables. Forward stepwise logistic regression method was used in the multivariate analysis to identify independent predictors of hypertension among college freshmen using odds ratio (OR) with 95% confidence interval (95% CI). Variables were retained in the model based on the likelihood ratio χ2 statistic at P-values < 0.05. All comparisons were two-tailed, and P-values less than 0.05 were considered statistically significant.
Results
Demographic characteristics of the participants
A total of 12,849 participants were enrolled in the analysis, including 7197 females and 5652 males (Table 2). The mean ± SD of SBP and DBP were 119.4 ± 12.5 mmHg and 70.9 ± 8.9 mmHg, respectively. The participants from the Western, Midland and Eastern regions accounted for 7.5%, 79.8% and 12.7%, respectively, and there was significant discrepancy of mean blood pressure in various region (P < 0.05). 72.3% of the freshmen lived in urban district before entering the college. 12.8% of the college freshmen were overweight, and 5.5% of them were obesity with an average SBP of 131.3 mmHg. 67.6% of the respondents usually exercised ≥ 150 min per week, and the students with physical inactivity had higher SBP and DBP (P < 0.05). 19.5% of the students habitually stayed up late, and their average SBP was 125.2 ± 11.7 mmHg, which was significantly higher than that of the students with regular sleep (P < 0.05). Students with a family history of CVDs were found to account for 6.7% of the college freshmen, and their average DBP was 72.0 ± 10.0 mmHg. The participants who had elevated RHR had higher SBP (127.3 ± 15.0 mmHg) and DBP (78.8 ± 10.2 mmHg) than the students whose RHR were under 100 beats/min (P < 0.05).
Table 2.
Socio-demographic characteristics and blood pressure of the participants.
| Variables | N | % | Blood pressure (mmHg) | |||
|---|---|---|---|---|---|---|
| Systolic blood pressure mean ± standard deviation |
P-value | Diastolic blood pressure mean ± standard deviation |
P-value | |||
| Total | 12,849 | 100.0 | 119.4 ± 12.5 | 70.9 ± 8.9 | ||
| Year | < 0.001 | < 0.001 | ||||
| 2015 | 4436 | 34.5 | 118.8 ± 12.3 | 70.4 ± 9.1 | ||
| 2016 | 4128 | 32.1 | 118.5 ± 12.4 | 71.1 ± 8.3 | ||
| 2017 | 4285 | 33.4 | 121.1 ± 12.6 | 71.3 ± 9.1 | ||
| Gender | < 0.001 | < 0.001 | ||||
| Male | 5652 | 44.0 | 125.7 ± 11.1 | 72.6 ± 9.1 | ||
| Female | 7197 | 56.0 | 114.5 ± 11.2 | 69.6 ± 8.4 | ||
| Residence | < 0.001 | < 0.001 | ||||
| Urban | 9289 | 72.3 | 120.0 ± 12.6 | 71.4 ± 8.9 | ||
| Rural | 3560 | 27.7 | 118.0 ± 12.0 | 69.6 ± 8.8 | ||
| Region | < 0.001 | < 0.001 | ||||
| West | 959 | 7.5 | 116.0 ± 12.1 | 68.3 ± 8.3 | ||
| Midland | 10,259 | 79.8 | 119.8 ± 12.5 | 71.2 ± 9.0 | ||
| East | 1631 | 12.7 | 119.3 ± 12.3 | 70.3 ± 8.4 | ||
| Body mass index | < 0.001 | < 0.001 | ||||
| Normal | 10,497 | 81.7 | 117.6 ± 11.9 | 69.9 ± 8.4 | ||
| Overweight | 1646 | 12.8 | 126.1 ± 11.4 | 74.0 ± 9.2 | ||
| Obesity | 706 | 5.5 | 131.3 ± 11.1 | 78.6 ± 9.8 | ||
| Adequate physical activity | < 0.001 | < 0.001 | ||||
| Yes | 8687 | 67.6 | 115.5 ± 11.3 | 69.0 ± 7.9 | ||
| No | 4162 | 32.4 | 127.7 ± 10.5 | 74.8 ± 9.5 | ||
| Stay up late | < 0.001 | < 0.001 | ||||
| Yes | 2511 | 19.5 | 125.2 ± 11.7 | 73.4 ± 9.3 | ||
| No | 10,338 | 80.5 | 118.0 ± 12.2 | 70.3 ± 8.7 | ||
| Family history of cardiovascular diseases | 0.565 | 0.001 | ||||
| Yes | 856 | 6.7 | 119.2 ± 13.9 | 72.0 ± 10.0 | ||
| No | 11,993 | 93.3 | 119.5 ± 12.3 | 70.8 ± 8.8 | ||
| Resting heart rate | < 0.001 | < 0.001 | ||||
| ≤ 100 | 12,555 | 97.7 | 119.3 ± 12.3 | 70.7 ± 8.8 | ||
| > 100 | 294 | 2.3 | 127.3 ± 15.0 | 78.8 ± 10.2 | ||
Table 3 shows the prevalence of hypertension and the comparison between groups according to different characteristics of college freshmen. Overall, 558 participants (4.3%) had hypertension. Pearson chi-square tests indicated that hypertension was associated with students’ gender, residence, and BMI (P < 0.001). Notably, students with elevated RHR, with physical inactivity, students who slept late and who had a family history of CVDs were more likely to have hypertension (P < 0.001).
Table 3.
The association between hypertension and socio-demographic characteristics of college freshmen.
| Variables | Hypertension (N, %) | χ2 | P-value | |
|---|---|---|---|---|
| No | Yes | |||
| Total | 12,291 (95.7) | 558 (4.3) | … | … |
| Year | 109.4 | < 0.001 | ||
| 2015 | 4303 (97.0) | 133 (3.0) | ||
| 2016 | 4003 (97.0) | 125 (3.0) | ||
| 2017 | 3985 (93.0) | 300 (7.0) | ||
| Gender | 302.8 | < 0.001 | ||
| Male | 5207 (92.1) | 445 (7.9) | ||
| Female | 7084 (98.4) | 113 (1.6) | ||
| Residence | 31.0 | < 0.001 | ||
| Urban | 8828 (95.5) | 461 (5.0) | ||
| Rural | 3463 (97.3) | 97 (2.7) | ||
| Region | 10.7 | 0.005 | ||
| West | 937 (97.7) | 22 (2.3) | ||
| Midland | 9793 (95.5) | 466 (4.5) | ||
| East | 1561 (95.7) | 70 (4.3) | ||
| Body mass index | 650.9 | < 0.001 | ||
| Normal | 10,220 (97.4) | 227 (2.6) | ||
| Overweight | 1521 (92.4) | 125 (7.6) | ||
| Obesity | 550 (77.9) | 156 (22.1) | ||
| Adequate physical activity | 353.4 | < 0.001 | ||
| Yes | 8513 (98.0) | 174 (2.0) | ||
| No | 3778 (90.8) | 384 (9.2) | ||
| Stay up late | 160.2 | < 0.001 | ||
| Yes | 2286 (91.0) | 225 (9.0) | ||
| No | 10,005 (96.8) | 333 (3.2) | ||
| Family history of cardiovascular diseases | 68.9 | < 0.001 | ||
| Yes | 771 (90.1) | 85 (9.9) | ||
| No | 11,520 (96.1) | 473 (3.9) | ||
| Resting heart rate | 122.5 | < 0.001 | ||
| ≤ 100 | 12,048 (96.0) | 507 (4.0) | ||
| > 100 | 243 (82.7) | 51 (17.3) | ||
Factors associated with hypertension of college freshmen
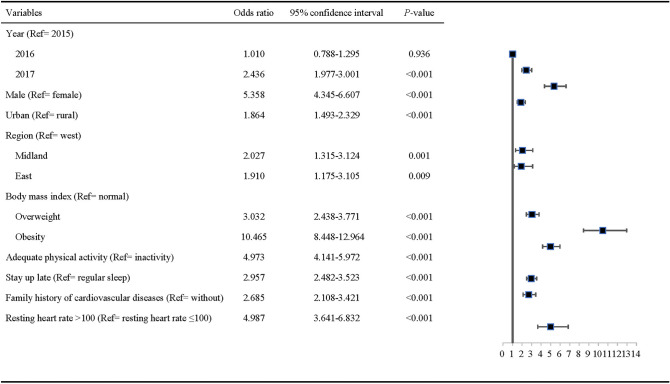
Figure 1 presents the factors associated with participants’ hypertension by multivariable logistic regression model. The prevalence of hypertension was higher in men than in women (OR: 5.358, 95% CI: 4.345–6.607, P < 0.001). Freshmen who lacked of regular exercise were more likely to have hypertension (OR: 4.973, 95% CI: 4.141–5.972, P < 0.001). The college freshmen who came from urban district had a higher risk (OR: 1.864, 95% CI: 1.493–2.329, P < 0.001) of hypertension compared with students from rural district. People with a family history of CVDs were more likely to have hypertension (OR: 2.685, 95% CI: 2.108–3.421, P < 0.001). People who stayed up late had a higher risk of hypertension (OR: 2.957, 95% CI: 2.482–3.523, P < 0.001). Obese students were more likely to develop hypertension than students with normal BMI (OR: 10.465, 95% CI: 8.448–12.964, P < 0.001). When the RHR was more than 100 beats per minute, the risk of hypertension would increase in youth (OR: 4.987, 95% CI: 3.641–6.832, P < 0.001). Students from the middle of the country had a higher risk of hypertension (OR: 2.027, 95% CI: 1.315–3.124, P < 0.001) compared to western students.
Figure 1.
Factors associated with hypertension of college freshmen in multivariable logistic regression model.
Discussion
Hypertension is a global epidemic and has become an increasingly important medical problem in children and adolescents. More and more researches on hypertension in adolescents remind us to strengthen the prevention and control of hypertension in the special population. However, information on the risk factors of hypertension in youth around the age of 18 years was limited. This study included 12,849 college freshmen with a mean age of 18.5 years, and we found that the prevalence of hypertension among freshmen in the university was similar to that of adolescent boys in Delhi, India13. Perhaps the reason was that both countries are developing countries, and a previous study had showed that the prevalence of hypertension in low- and middle-income countries has surpassed that in high-income countries14. Hypertension is an important risk factor for a variety of health conditions, such as CVDs, stroke, and kidney failure. Nevertheless, this burden is unevenly distributed in society, with higher rates of hypertension in men than in women15, which was in line with our findings. The reason may be that men were more likely to lack healthy eating and exercise habits. Women usually are more aware of and are more active in managing and treating their blood pressure, which was consistent with a previous research on women’s health-seeking behaviors16. The prevalence of hypertension was significantly lower in rural areas than that in urban areas, which was consistent with some relevant studies17,18. It was perhaps because that students from different residences had different eating habits and study pressure. People are prone to hypertension in stressful situations. Students from the middle land of the country had the highest rate of hypertension, which may be due to a prevalent excessive salty diet.
In recent decades, many epidemiological studies have reported a positive correlation between overweight and high blood pressure in pediatric populations6,19, and reported that obesity was a major risk factor for essential hypertension20. In our study, compared with students of normal BMI, those who were overweight or obese had a significantly higher prevalence of hypertension. The obese people were 10.5 times more likely to have hypertension than people of normal BMI, which was consistent with previous reports21,22. An epidemiological study showed that abdominal fat accumulation was associated with a higher risk of CVD incidence and mortality 23. On the one hand, this is possibly related to their sedentary lifestyle, increased fat content in their diet and decreased physical activities. On the other hand, the development of hypertension caused by obesity can occur via multiple mechanisms, such as insulin resistance, adipokine alterations, inappropriate sympathetic nerve function and renin–angiotensin–aldosterone system activation, structural and functional abnormalities in the kidney, heart and vascular changes, and immune maladaptation20,24. Uric acid and incretin or dipeptidyl peptidase 4 activity alteration also contribute to the development of hypertension in the context of obesity24. In addition, using BMI alone to diagnosis obesity would lead to about half of patients with abdominal obesity being missed.
Doing exercise is considered one of the most effective methods to control the weight of college students. Physical activity can not only reduce the subcutaneous and visceral fat of obese people, but also play a positive role in promoting cardiac function, autonomic nervous system and immune ability. This study showed that the detection rate of hypertension among college freshmen who do not participate in exercise regularly was significantly higher than that among those who exercised regularly. Physical exercise is a protective factor of hypertension. Owen et al. found that 10% increase in physical activity among adolescents can significantly reduce the risk of obesity and CVDs25. Moderate exercise was good for health and heart function. However, it did not mean that excessive exercise was better. Over the last several years, sudden deaths of trained athletes were usually associated with immoderate exercise, which have become highly visible events fueled by news media reports26. Therefore, moderate exercise is the best option.
Correlation analysis shows that blood pressure was most closely related to RHR, which was consistent with previous research results27. The detection rate of hypertension was 17.3% in students with elevated RHR, and the elevated RHR was also a risk factor for hypertension. The value of RHR reflected the balance between autonomic nerves and the function of heart. The acceleration of RHR could increase the fluctuation of blood flow, change the velocity and direction of blood flow, and cause damage to the vascular endothelium. The lipid then seeped into the lining of the blood vessels and promoted the development and progression of atherosclerosis28, which was the pathological basis of CVDs. An increase of 10 beats per minute in heart rate was associated with at least 20% increase in the risk of cardiac death29,30. Therefore, RHR control is an important target for the prevention of hypertension, which could reduce the risk of target organ damage and adverse cardiovascular events in patients with hypertension.
We found that 9.0% of the freshmen who stayed up late had been diagnosed with hypertension, which was much higher than the proportion of hypertension among the freshmen who had regular sleep (3.2%). Previous studies had shown that sleep deprivation was associated with high blood pressure31,32. Staying up late was a very common phenomenon among college students, because they were more relaxed academically and could spend more time to surf the internet after the college entrance examination. In recent years, the use of smart phones has become more and more popular in Chinese adolescents. The overall prevalence of Internet addiction was 26.50% among adolescents in China33, which is much higher than that in other Asian countries (range: 6.2–21.2%)34,35. Internet addiction was found to affect sleep quality and lead to negative impact on health-related quality of life in adolescents35. Students with poor quality sleep may be at a higher risk of elevated blood pressure that could lead to CVDs in adolescents32. The possible explanation was that insufficient sleep put the students in a state of mild stress, and the psychological stress could act as a stressor on the human body and produce a stress response. Moreover, insufficient sleep acts on target organs through the thalamus-pituitary-adrenal system, which makes the sympathetic nervous system overactive, increases the release of catecholamines, and causes an increase in blood pressure.
The majority (90–95%) of the hypertensive patients have a highly heterogeneous primary hypertension with a multifactorial gene-environment etiology36. Our results showed that the family history was an important risk factor for hypertension. People with hypertension often have a positive family history, with the heritability (a measure of how much of the variation in a trait is due to variation in genetic factors) estimated between 35 and 50% in the majority of studies37,38.
Strengths and limitations
The strengths of the current study were as follows. Firstly, the included participants were about 18 years, who were easily exposed to disease-related risk factors but did not have adequate disease prevention awareness. This investigation highlighted the early prevention of hypertension and played an early warning role in the occurrence of CVDs. Secondly, the sample size of this study was relatively large, and the results were relatively reliable. Thirdly, the sample is nationally representative to some extent, for all participants were just graduated from high schools all over the country.
Several limitations of this study should be listed. First of all, we failed to track the changes in hypertension during the following years of college, and the cross-sectional nature of the study limits drawing of inferences about causation. The second limitation was that we did not assess some other potential factors associated with hypertension, such as daily eating habits (especially salt intake), usage of stimulants and depression. Thirdly, not being able to collect data about use of antihypertensives means that the current study might have underestimate true prevalence of hypertension.
Conclusions
In summary, the detection rate of hypertension in male was significantly higher than that in female of college freshmen in China. Obesity, physical inactivity, staying up late and elevated RHR were identified as important modifiable risk factors of hypertension in youth. It is necessary to change the lifestyle of these vulnerable groups and implement intervention plans in the early stage, especially for obese and inactive men.
Data availability
Data are available purposes upon request.
Author contributions
S.C. and C.L. contributed to the conception or design of the work. Q.J. and Q.Z. contributed to the acquisition or interpretation of data for the work. Q.J., Q.Y. and T.W. contributed to the analysis of data and drafted the manuscript. S.C. contributed to guiding article writing. All authors critically revised the manuscript. All authors gave final approval and agree to be accountable for all aspects of the work ensuring integrity and accuracy.
Funding
This project was funded by the Fundamental Research Funds for the Central Universities, Huazhong University of Science and Technology (2020WKZDJC015).
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Chun Liu, Email: liuchuntongji@163.com.
Shiyi Cao, Email: caoshiyi@hust.edu.cn.
References
- 1.Roth GA, Abate D, Abate KH, et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1736–1788. doi: 10.1016/S0140-6736(18)32203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al-Mawali A. Non-communicable diseases: shining a light on cardiovascular disease Oman’s Biggest Killer. Oman Med. J. 2015;30:227–228. doi: 10.5001/omj.2015.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hong YM. Atherosclerotic cardiovascular disease beginning in childhood. Korean Circ. J. 2010;40:1–9. doi: 10.4070/kcj.2010.40.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Raitakari OT, Juonala M, Kähönen M, et al. Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthoodthe cardiovascular risk in young finns study. JAMA. 2003;290:2277–2283. doi: 10.1001/jama.290.17.2277. [DOI] [PubMed] [Google Scholar]
- 5.Blacher J, Levy BI, Mourad JJ, Safar ME, Bakris G. From epidemiological transition to modern cardiovascular epidemiology: hypertension in the 21st century. Lancet (Lond. Engl.) 2016;388:530–532. doi: 10.1016/s0140-6736(16)00002-7. [DOI] [PubMed] [Google Scholar]
- 6.Bao W, Threefoot SA, Srinivasan SR, Berenson GS. Essential hypertension predicted by tracking of elevated blood pressure from childhood to adulthood: the Bogalusa Heart Study. Am. J. Hypertens. 1995;8:657–665. doi: 10.1016/0895-7061(95)00116-7. [DOI] [PubMed] [Google Scholar]
- 7.Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood: a systematic review and meta-regression analysis. Circulation. 2008;117:3171–3180. doi: 10.1161/circulationaha.107.730366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rao J, et al. The risk of hypertension doubles every 10 years in china: age, period, and birth cohort effects on the prevalence of hypertension from 2004 to 2013. Am. J. Hypertens. 2019;32:492–502. doi: 10.1093/ajh/hpz003. [DOI] [PubMed] [Google Scholar]
- 9.Wang Z, et al. Status of hypertension in china: results from the china hypertension survey, 2012–2015. Circulation. 2018;137:2344–2356. doi: 10.1161/circulationaha.117.032380. [DOI] [PubMed] [Google Scholar]
- 10.Revision JCFG. 2018 Chinese guidelines for prevention and treatment of hypertension-a report of the revision committee of chinese guidelines for prevention and treatment of hypertension. J. Geriatr. Cardiol. JGC. 2019;16:182–241. doi: 10.11909/j.issn.1671-5411.2019.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Force., G. O. C. O. T. [Body mass index reference norm for screening overweight and obesity in Chinese children and adolescents]. Zhonghua liu xing bing xue za zhi = Zhonghua liuxingbingxue zazhi25, 97–102 (2004). [PubMed]
- 12.Fox K, et al. Resting heart rate in cardiovascular disease. J. Am. Coll. Cardiol. 2007;50:823–830. doi: 10.1016/j.jacc.2007.04.079. [DOI] [PubMed] [Google Scholar]
- 13.Singh SK, Verma A. Prevalence of hypertension among school going adolescent boys in Najafgarh, Delhi, India. Int. J. Adolesc. Med. Health. 2020 doi: 10.1515/ijamh-2019-0005. [DOI] [PubMed] [Google Scholar]
- 14.Mills KT, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134:441–450. doi: 10.1161/circulationaha.115.018912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mozaffarian D, et al. Executive summary: heart disease and stroke statistics–2016 update: a report from the american heart association. Circulation. 2016;133:447–454. doi: 10.1161/cir.0000000000000366. [DOI] [PubMed] [Google Scholar]
- 16.Galdas PM, Cheater F, Marshall P. Men and health help-seeking behaviour: literature review. J. Adv. Nurs. 2005;49:616–623. doi: 10.1111/j.1365-2648.2004.03331.x. [DOI] [PubMed] [Google Scholar]
- 17.Chow CK, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013;310:959–968. doi: 10.1001/jama.2013.184182. [DOI] [PubMed] [Google Scholar]
- 18.Mohan B, et al. Prevalence of sustained hypertension and obesity in urban and rural school going children in Ludhiana. Indian Heart J. 2004;56:310–314. [PubMed] [Google Scholar]
- 19.Muntner P, He J, Cutler JA, Wildman RP, Whelton PK. Trends in blood pressure among children and adolescents. JAMA. 2004;291:2107–2113. doi: 10.1001/jama.291.17.2107. [DOI] [PubMed] [Google Scholar]
- 20.Jiang SZ, Lu W, Zong XF, Ruan HY, Liu Y. Obesity and hypertension. Exp. Ther. Med. 2016;12:2395–2399. doi: 10.3892/etm.2016.3667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McGavock JM, Torrance B, McGuire KA, Wozny P, Lewanczuk RZ. The relationship between weight gain and blood pressure in children and adolescents. Am. J. Hypertens. 2007;20:1038–1044. doi: 10.1016/j.amjhyper.2007.04.018. [DOI] [PubMed] [Google Scholar]
- 22.Hu J, et al. Relation of body mass index (BMI) to the prevalence of hypertension in children: A 3years' school-based prospective study in Suzhou China. Int. J. Cardiol. 2016;222:270–274. doi: 10.1016/j.ijcard.2016.07.217. [DOI] [PubMed] [Google Scholar]
- 23.Kuo RJ, Wu YH, Chen LK. Inability of waist-to-height ratio to predict new onset diabetes mellitus among older adults in Taiwan: a five-year observational cohort study. Arch. Gerontol. Geriatr. 2011;53:e1–4. doi: 10.1016/j.archger.2010.05.005. [DOI] [PubMed] [Google Scholar]
- 24.DeMarco VG, Aroor AR, Sowers JR. The pathophysiology of hypertension in patients with obesity. Nat. Rev. Endocrinol. 2014;10:364–376. doi: 10.1038/nrendo.2014.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Owen CG, et al. Physical activity, obesity and cardiometabolic risk factors in 9- to 10-year-old UK children of white European, South Asian and black African-Caribbean origin: the Child Heart And health Study in England (CHASE) Diabetologia. 2010;53:1620–1630. doi: 10.1007/s00125-010-1781-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maron BJ, Pelliccia A. The heart of trained athletes: cardiac remodeling and the risks of sports, including sudden death. Circulation. 2006;114:1633–1644. doi: 10.1161/circulationaha.106.613562. [DOI] [PubMed] [Google Scholar]
- 27.Shi Y, et al. Resting heart rate and the risk of hypertension and heart failure: a dose-response meta-analysis of prospective studies. J. Hypertens. 2018;36:995–1004. doi: 10.1097/hjh.0000000000001627. [DOI] [PubMed] [Google Scholar]
- 28.Shigetoh Y, et al. Higher heart rate may predispose to obesity and diabetes mellitus: 20-year prospective study in a general population. Am. J. Hypertens. 2009;22:151–155. doi: 10.1038/ajh.2008.331. [DOI] [PubMed] [Google Scholar]
- 29.Perret-Guillaume C, Joly L, Benetos A. Heart rate as a risk factor for cardiovascular disease. Prog. Cardiovasc. Dis. 2009;52:6–10. doi: 10.1016/j.pcad.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 30.Morcet JF, Safar M, Thomas F, Guize L, Benetos A. Associations between heart rate and other risk factors in a large French population. J. Hypertens. 1999;17:1671–1676. doi: 10.1097/00004872-199917120-00003. [DOI] [PubMed] [Google Scholar]
- 31.Paciência I, Barros H, Araújo J, Ramos E. Association between sleep duration and blood pressure in adolescents. Hypertens. Res. Off. J. Jpn. Soc. Hypertens. 2013;36:747–752. doi: 10.1038/hr.2013.36. [DOI] [PubMed] [Google Scholar]
- 32.Narang I, et al. Sleep disturbance and cardiovascular risk in adolescents. CMAJ Can. Med. Assoc. J. J. Assoc. Med. Can. 2012;184:913–920. doi: 10.1503/cmaj.111589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Xin M, et al. Online activities, prevalence of Internet addiction and risk factors related to family and school among adolescents in China. Addict. Behav. Rep. 2018;7:14–18. doi: 10.1016/j.abrep.2017.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mak KK, et al. Epidemiology of internet behaviors and addiction among adolescents in six Asian countries. Cyberpsychol. Behav. Soc. Netw. 2014;17:720–728. doi: 10.1089/cyber.2014.0139. [DOI] [PubMed] [Google Scholar]
- 35.Tran BX, et al. A study on the influence of internet addiction and online interpersonal influences on health-related quality of life in young Vietnamese. BMC Public Health. 2017;17:138. doi: 10.1186/s12889-016-3983-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Oparil S, et al. Hypertension. Nat. Rev. Dis. Primers. 2018;4:18014. doi: 10.1038/nrdp.2018.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fagard R, et al. Heritability of conventional and ambulatory blood pressures. A study in twins. Hypertension (Dallas, Tex.: 1979) 1995;26:919–924. doi: 10.1161/01.hyp.26.6.919. [DOI] [PubMed] [Google Scholar]
- 38.Luft FC. Twins in cardiovascular genetic research. Hypertension (Dallas, Tex.: 1979) 2001;37:350–356. doi: 10.1161/01.hyp.37.2.350. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available purposes upon request.