Abstract
Aims and background
Physical inactivity is leading to obesity and consequently insulin resistance and diabetes. Feasible and cost efficient strategies like Pilates and total body resistance exercise (TRX) training can impede obesity and its compilation. The aim of this study was to investigate the effects of 8 weeks Pilates and TRX training programs on irisin concentration and insulin resistance in overweight women.
Method
Thirty overweight women (Body mass index (BMI): 25–29.9 kg/m2) were divided, based on their BMI, into 3 groups; control, Pilates and TRX. The participants in the training groups were subjected to moderate intensity of Pilates or TRX exercise training 3 times a week for 8 weeks. Blood samples were taken at pre-test and 48 h after the last training session and used for analyzing irisin, insulin and glucose. Data were analyzed by ANCOVA and paired-samples t-test.
Results
The finding showed that the Pilates training decreased body weight and BMI compared to the pre-test (P < 0.05). Also, it has been revealed that irisin concentration in response to Pilates and TRX training programs were increased in comparison with the control group (P < 0.05). However, there was no significant difference in irisin concentrations between training groups (p > 0.05). Moreover, fasting insulin, glucose and insulin resistance were significantly reduced after exercise intervention compared to the pre-test which were significantly lowered compared to the control group as well.
Conclusion
The results suggest Pilates and TRX trainings are two efficient model of exercise that by eliciting an exercise-hormone, irisin, can improve insulin resistance in overweight women.
Keywords: Obesity, Exercise training, Diabetes, Pilates, TRX
Introduction
Excessive calorie intake and sedentary lifestyle are two major risk factors for overweight and obesity [1]; leading to chronic diseases such as diabetes [2]. Insulin resistance is a hallmark feature of type 2 diabetes (T2D) [3]. By increasing obesity-related metabolic diseases such as T2D, many biologically metabolic factors have been investigated as therapeutic target factors of glucose homeostasis [4].
Irisin is a poly peptide hormone which expresses profoundly in the heart and skeletal muscles [5]. It is evidenced that irisin improves insulin resistance andT2D through increasing insulin receptors sensitivity in skeletal muscles and browning whit adipose tissue [6, 7]. In addition, it has been found that irisin concentration is higher in obese people compared to normal weight individuals, which has a significant positive correlation with fat mass and negative correlation with fat free mass [8].
It is widely known that the regular exercise training has metabolic benefits to T2D patients [9]. The protective effect of physical activity, in part, is related to the secretion of myokines from skeletal muscles during workouts [10]. These molecules are linked between exercise and metabolic disorders amelioration [11]. Irisin is considered as an exercise hormone which a link between physical activity and metabolic homeostasis [12]. In this regard, it has been suggested that exercise-induced elevated irisin could reduce weight in obese and insulin resistance individuals [13, 14]. Irisin levels are modulated by exercise type. Accordingly, Tsuchiya et al. showed that resistance exercise elicits a greater irisin response compared to aerobic exercise [15].
Some physical exercises may put overload on knee joints in overweight or obese individuals [16]. It is essential to investigate the suitable form of exercise for overweight and obese people. Exercise training such as total body resistance exercise (TRX) with the use of suspension system [17] and Pilates [18] are favorable for rehabilitation and home based exercise during gym lockdown. The ease of using TRX method has derived much more research attention than traditional resistance training with expensive equipment [17]. TRX training has the beneficial effects on muscular fitness as same as traditional resistance training [19]. On the other hand, Pilates is a good option for overweight and obese subject with difficulty to performing traditional exercise training [20]. Pilates is mainly consisted of isometric contraction of the core muscles and combined movements of gymnastics, yoga, dance and meditation [21]. Pilates considered as a popular training model improves cardiorespiratory fitness in overweight and obese individuals [18].
A growing body of evidence showed that Pilates [22] and TRX training [17] methods are widely used as enjoyable and safe exercise strategy for health promotion. Given the use on TRX and Pilates training as appealing therapeutic targets for treating obesity and diabetes in the overweight and obese individuals, the aim of this study was to investigate the effects of TRX and Pilates training on exercise hormone, Irisin, and insulin resistance in overweight women. It can provide some insights into the metabolic effects of TRX and Pilates training for obesity managment.
Method
Subjects
Thirty overweight volunteer women were participated in the study. The study protocol was approved by the ethical committee of the University of …. The inclusion criteria’s was included; body mass index (BMI) between 25 and 29.9 kg/m2, sedentary lifestyle in the past six months and no drug treatment. The exclusion criteria was having joint and muscle problem with exercise movements, two sessions absence in row or four sessions overall. The subjects had right to withdraw in anytime during the study.
Procedure
After filling out medical and physical questionnaires’, the physical characteristic of subjects including, weight, height, fat percentage, waist circumference, hip waist and BMI were measured and calculated. Then, the blood samples were taken in the fast state and, according to their body weight; the subjects were equally divided into 3 groups of Pilates, TRX and control. The subjects in the TRX and Pilates groups performed designed exercise training program for 8 weeks (3 times a week). Forty-eight hours after the last exercise session, the subjects were attended to the laboratory to evaluate anthropometric characteristics and drown blood samples similar to the pre-test condition.
TRX protocol
After two sessions of familiarization with the exercise movements, the subject completed three exercise sessions on non-consecutive day during the study. Training program was included 10 min of warm up, 40 min of body exercise and 10 min of cool down. The body exercise was including, chest press, tow arm row, suspended lunges, squat, single-leg squat, YTM, revers mountain climber, triceps extension, hamstring curl, plunk, front squat, power pull. As presented in Table 1, the number of sets, repetitions and angle was gradually increased throughout the study. Moreover, exercise movements were gradually shifted from basic to advance levels (Table 1) the TRX training protocol was adapted from the previously studies [17]. The exercise intensity was controlled by the rate of perceived exertion (RPE) scale (15 points; 0–20). The moderate exercise intensity was chosen in the entire sessions (RPE; 12).
Table 1.
TRX training program with type of exercises, sets, repetitions and angle
| Exercise | Week 0–2 | Week 3–4 | Week 5–6 | Week 7–8 |
|---|---|---|---|---|
| Sets × rep /angle | Sets × rep /angle | Sets × rep / angle | Sets × rep /angle | |
| Chest press | 2 × 10 /30° | 2 × 12 /30° | 2 × 10 /50° | 2 × 12 /65° |
| Tow arm row | 2 × 10 /30° | 2 × 12 /30° | 2 × 10 /50° | 2 × 10 /65° |
| Suspended lunges | 2 × 10 | 2 × 12 | 2 × 10 | - |
| squat | 2 × 10 | 2 × 12 | 3 × 12 | 3 × 12 |
| Single-leg squat | - | - | 2 × 12 | 3 × 12 |
| YTM | 2 × 10 | 2 × 12 | - | - |
| Reverse mountain climber | 2 × 12 | 3 × 10 | - | - |
| Triceps extension | 2 × 10 | 2 × 12 | - | - |
| Hamstring curl | 2 × 5 | 2 × 8 | 2 × 10 | 2 × 12 |
| plunk | 8 × 12 s | 8 × 15 s | 8 × 20 s | 8 × 25 s |
| Front squat | - | - | 2 × 12 | 3 × 10 |
| Power pull | - | - | 2 × 12 | 3 × 10 |
Pilates training protocol
The Pilates training program was guided by a professional instructor. Training protocol was involved 10 min war up, 40 min body exercise and 10 min cool down (relaxation). The exercise movement similar to TRX training was designed to stimulate the whole body muscles which including; single-leg circles, squat, ball marches, leg lift supine, elbow flexion and extension, abduction of lower and upper limbs, shoulder bridge, side, front and back kick, bend and stretch, shoulder bridge, let pull front. The number of sets, repetition and exercise movements was presented in details in table 2 as described previously [23]. The exercise intensity was similar to the TRX training sessions.
Laboratory assessment
Anthropometrics characteristics of subjects were measured before and after training period. The body fat percentage was estimated by Slim Guide and Jackson Pollack’s three points skinfolds including triceps, supariliac and thigh. Six milliliters of blood were drawn from a forearm vein into a sterile tube containing EDTA and centrifuged for 10 min at 1000 g to separate plasma and stored in -80 centigrade temperature. Plasma was used for Irisin analysis by ELISA method (Zell bio, Germany), insulin (Mercodia co, Sweden). Plasma glucose was analyzed by photometric method (Pars Azmoon kit, Iran). Insulin resistance was calculated with the homeostasis model assessment (HOMA-IR) by the following formula: fasting plasma glucose (mmol/L) x fasting serum insulin (μU/mL)/22.5.
Statistical analysis
The data normality was tested using a Shapiro–Wilk test. The one way of ANOVA and ANCOVA were used to compare differences among groups. In case of differences among groups, Bonfroni post hoc test was applied. A paired t-test was used to measure within group changes. Pearson correlation was utilized to determine the relationship between variables. The statistical significance level was set to α ≤ 0.05.
Results
The results showed no significant differences in body weight and BMI among three groups (P > 0.05). However, the Pilates training group significantly reduced body weight and BMI after intervention compared to the pre-test (P < 0.001, Table 2).
Table 2.
The physical characteristic of the subjects, Data is expressed as mean ± SD
| groups | |||
|---|---|---|---|
| Control | TRX | Pilates | |
| age | 30.44 ± 3.17 | 30.44 ± 3.39 | 30.22 ± 3.31 |
| Weight (kg) | |||
| Pre | 72.78 ± 9.60 | 72.62 ± 9.63 | 74.44 ± 12.77 |
| post | 73.22 ± 9.97 | 68.45 ± 8.76 | 72.51 ± 12.97* |
| BMI (kg/m2) | |||
| Pre | 28.06 ± 5.48 | 27.59 ± 2.92 | 28.84 ± 4.67 |
| post | 28.22 ± 5.58* | 26.01 ± 2.62 | 28.08 ± 4.76* |
| Waist circumference (cm) | |||
| Pre | 85.33 ± 4.78 | 88.67 ± 4.78 | 97.56 ± 11.10 |
| post | 84.56 ± 3.61 | 84.56 ± 3.61 | 90.33 ± 11.78 |
| Hip circumference (cm) | |||
| Pre | 97.00 ± 8.11 | 105.22 ± 7.61 | 107.22 ± 7.69 |
| post | 99.11 ± 9.03 | 101.67 ± 8.23 | 104.89 ± 7.25 |
*significant difference with pre-test. P value sets at < 0.05
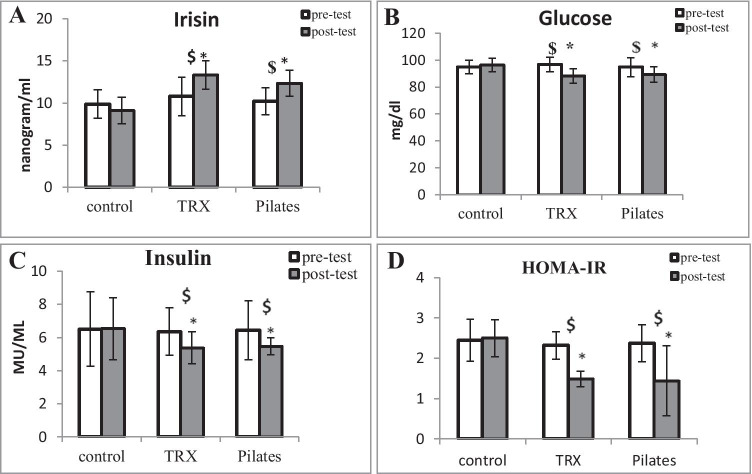
The finding showed that irisin concentrations were increased after 8 weeks of TRX and Pilates training in comparison with pre-test (P = 0.009, P = 0.006; respectively). Moreover, irisin concentrations did not change in the control group (P = 0.228). Further analysis showed that significant differences in Irisin concentration among groups were found (F = 6.948, P = 0.002). Post hoc test revealed that Irisin concentrations in TRX and Pilates training group were significantly higher compared to the control group (P = 0.002, P = 0.044; respectively). However, there was no significant difference between two training groups (P = 0.815) (Fig. 1A).
Fig. 1.
The effects of TRX and Pilates training programs on Irisin (A), glucose (B), insulin (C) and insulin resistance index (HOMA-IR). Data are expressed as mean ± SD. *significant difference from pre-test, $ significant difference from the control group. P value set at 0.05
After 8 weeks of intervention, insulin concentrations were attenuated in response to TRX and Pilates training compared to pre-test (P < 0.001). In comparing among groups (F = 9.337, P < 0.001), the post hoc bonfroni test showed that insulin concentrations leveled off in the TRX and Pilates training groups compared to the control group (P = 0.001, P = 0.004; respectively). But, there were no significant difference between two groups (P > 0.05, Fig. 1). Glucose concentrations were reduced after 8 weeks intervention of TRX and Pilates training (P < 0.001, P = 0.008; respectively). ANCOVA analysis revealed that glucose concentrations were different among groups (F = 4.630, P < 0.001). Further analysis demonstrated that glucose concentrations were diminished by TRX and Pilates training group in comparison with the control group (P = 0.048, P = 0.024; respectively). Furthermore, the finding showed that, based on the insulin and glucose concentrations, HOMA-IR was significantly reduced after TRX and Pilates training program in overweight women compared to the pre-test (P < 0.001). Significant differences were found in HOMA-IR among groups (F = 7.904, P = 0.001). Moreover, HOMA-IR was diminished in TRX and Pilates training compared to the control group (P = 0.003, P = 0.004; respectively) (Fig. 1).
Discussion
The main findings of this study demonstrated that TRX and Pilates training methods (1) increased circulating irisin concentrations and (2) improved glucose homeostasis which was reflected by decreasing fasting glucose and insulin concentrations and insulin resistance in overweight women after 8 weeks of intervention.
In a study conducted by Melo et al. (2018), 12 weeks pilates training improved postprandial glycemic control and decreased HBA1c in older women with T2D but had no effect on fasting glucose [23]. Also, Yucel and uysal (2018) reported reduction in fasting blood glucose after 12 weeks Pilates in women [24]. In a meta-analysis research, it has been reported that pilats is associated with s significant decrease in body weight, BMI and percentage of body fat in overweight and obese adults [21]. In addition, it is reported that TRX training method is an effective method to improve lipid profile [25]. To date, there has been a lack of scientific reports on the bases of TRX and Pilates training method on metabolic adaptations in obese individuals as alternative methods to traditional resistance and aerobic exercises.
There is conflicting data regarding irisin response to exercise training, in agreement with our study, Irisin concentrations were increased after 8 weeks resistance exercise training [13]. Contrarily, A 12-week of heavy resistance training had no effect on serum irisin level in women [26]. But in another study, 10 weeks of aerobic exercise increased plasma irisin levels by twofold [14]. It has been reported that Irisin expression and secretion depend on physical activity, intensity, type, time and frequency of exercise [27]. This can partly explain the conflict results.
Most clinical studies have been revealed that circulating irisin are lower in T2D [28] but higher in obese individuals [29]; suggesting that increased irisin during excessive energy intake could be a compensatory mechanism to impede weight gain and insulin resistance by increasing energy expenditure [30]. It has been demonstrated that serum irisin level has a positive correlation fat mass, waist circumference and lipid and glucose hemostasis disturbances [7, 29]. Dianatinasab et al. (2020) showed that 8 weeks of aerobic, resistance and combined training had no effects on irisin concentrations in overweight women [31]. However, insulin resistance was decreased in response to training programs. They also demonstrated that serum irisin has a positive correlation with fat percentage and insulin resistance [31]. Although, the possible mechanism of Pilates and TRX training on glycemic control is not clear, it is speculated that exercise training improves insulin sensitivity and muscle GLUT-4 expression and [32]. In this study, we found that Pilates and TRX training programs increases irisin concentrations concomitant with decreasing insulin resistance. Regarding to these findings, this implies that synthesis and secretion is stimulated by exercise and peroxisome proliferator- activated receptor-γ (PPAR-γ) coactivator 1-α (PGC1α) [33]. It is important to mention that exercise activity stimulates PGC-1α and its downstream protein, fibronectin type III doman-containing 5 (FNDC5) [5]; eventually leading to cleaved of FNDC5 to irisin in skeletal muscle [34]. Very recently, it has been suggested that irisin may enhance skeletal muscle fiber size by increasing contractile proteins [35] which may affect glucose uptake from bloodstream. However, due to the study limitation, we did not analyze irisin in skeletal muscle in response to TRX or Pilates training that need to be investigated.
Insulin resistance development mostly is due to insulin receptors desensitization and defect in its substrates phosphorylation [5]. It is also reported that irisin regulates glucose uptake in skeletal muscles via calcium and P38 AMK mediated AMPK pathway [5]. Moreover, irisin stimulates glucose uptake in skeletal muscle by GLUCT-4 translocation [6]. Another possible mechanism is that irisin improves insulin sensitivity by reducing fasting glucose level via suppressing gluconeogenesis and increasing glycogenesis in the liver [36]. Furthermore, irisin acts as anti-apoptotic on pancreas beta cells, stimulated beta cell proliferation, and biosynthesis and secretion of insulin [37]. Thus, it can be speculated that increased levels of irisin due to Pilates and TRX training methods can improve glucose tolerance and decrease insulin resistance which may be considered as therapeutic strategies in diabetes treatment.
In obesity conditions, adipose tissue considered as important factors in the irisin secretion, which may lead to irisin resistance [8]. Studies have pointed out that increased irisin concentrations are accompanied by increased levels of inflammatory factors [38] which have a significant role in developing insulin resistance [39]. It is demonstrated that overexpression of FNDC5 in adipose tissue of obese mice is associated with improving hyperlipidemia and increasing lipolysis [40]. FNDC5 plays an important role in diminishing adipose tissue inflammation and insulin resistance [40]. FNDC5 acts via AMPK which reduces inflammation and M1 macrophage polarization [41]. Another possible limitation was that we were not able to measure adipose tissue macrophages and their connection to exercise-induced irisin responses.
In this regards, it has been shown that12 weeks of exercise training increased PGC-1α transcription and FNDC5 mRNA expression in obese and pre-diabetic individuals [33]. Another study, reported that 6 weeks of aerobic and resistance exercise training in healthy individuals increased FNDC5 compared to that of the control group [42]. In fact, resistance training by contracting muscles and depleting energy can stimulate AMPK/PGC-1α pathway [43]; suggesting the underlying mechanism of exercise-induced increased irisin concentration.
It is concluded that Pilates and TRX training programs are tow feasible and cost efficient strategies to improve glucose homeostasis in overweight women. In fact, our study revealed that Pilates and TRX training methods were accompanied by increasing exercise hormone, irisin, which was associated with improving fasting glucose, insulin and insulin resistance in overweight women. These findings reflect the potential roles of Pilates and TRX training modalities on T2D management as alternative to the traditional and expensive exercise training.
Acknowledgements
The authors would like to thank all the participants who gave us their time and participated in this trial.
Funding
The author(s) received no specific funding for this work.
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Declarations
Disclosure of interest
The authors declare that they have no conflicts of interest concerning this article.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Morgen CS, Sørensen TI. Global trends in the prevalence of overweight and obesity. Nat Rev Endocrinol. 2014;10(9):513–514. doi: 10.1038/nrendo.2014.124. [DOI] [PubMed] [Google Scholar]
- 2.Organization WH. Noncommunicable diseases country profiles 2018. 2018.
- 3.Sousa RALD, Improta-Caria AC, Souza BSdF. Exercise–linked irisin: consequences on mental and cardiovascular health in type 2 diabetes. Int J Mol Sci. 2021;22(4):2199. doi: 10.3390/ijms22042199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang T, Zhang H, Li Y, Li S, Fernandez C, Bazzano L, et al. Long-term impact of temporal sequence from childhood obesity to hyperinsulinemia on adult metabolic syndrome and diabetes: the Bogalusa heart study. Sci Rep. 2017;7(1):1–7. doi: 10.1038/srep43422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gizaw M, Anandakumar P, Debela T. A review on the role of irisin in insulin resistance and type 2 diabetes mellitus. J Pharmacopuncture. 2017;20(4):235. doi: 10.3831/KPI.2017.20.029. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 6.Zhang Y, Li R, Meng Y, Li S, Donelan W, Zhao Y, et al. Irisin stimulates browning of white adipocytes through mitogen-activated protein kinase p38 MAP kinase and ERK MAP kinase signaling. Diabetes. 2014;63(2):514–525. doi: 10.2337/db13-1106. [DOI] [PubMed] [Google Scholar]
- 7.Hee Park K, Zaichenko L, Brinkoetter M, Thakkar B, Sahin-Efe A, Joung KE, et al. Circulating irisin in relation to insulin resistance and the metabolic syndrome. J Clin Endocrinol Metab. 2013;98(12):4899–4907. doi: 10.1210/jc.2013-2373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pardo M, Crujeiras AB, Amil M, Aguera Z, Jimenez-Murcia S, Banos R, et al. Association of irisin with fat mass, resting energy expenditure, and daily activity in conditions of extreme body mass index. Int J Endocrinol. 2014;2014. [DOI] [PMC free article] [PubMed]
- 9.Riddell MC, Miadovnik L, Simms M, Li B, Zisser H. Advances in exercise, physical activity, and diabetes mellitus. Diabetes Technol Ther. 2013;15(S1):S-96-S-106. doi: 10.1089/dia.2013.1511. [DOI] [PubMed] [Google Scholar]
- 10.Benedini S, Dozio E, Invernizzi PL, Vianello E, Banfi G, Terruzzi I, et al. Irisin: a potential link between physical exercise and metabolism—an observational study in differently trained subjects, from elite athletes to sedentary people. J Diabetes Res. 2017;2017. [DOI] [PMC free article] [PubMed]
- 11.Choi KM. The impact of organokines on insulin resistance, inflammation, and atherosclerosis. Endocrinol Metab. 2016;31(1):1. doi: 10.3803/EnM.2016.31.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Polyzos SA, Kountouras J, Shields K, Mantzoros CS. Irisin: a renaissance in metabolism? Metab-Clin Exp. 2013;62(8):1037–1044. doi: 10.1016/j.metabol.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 13.Kim H-J, Lee H-J, So B, Son JS, Yoon D, Song W. Effect of aerobic training and resistance training on circulating irisin level and their association with change of body composition in overweight/obese adults: a pilot study. Physiol Res. 2016;65(2):271. doi: 10.33549/physiolres.932997. [DOI] [PubMed] [Google Scholar]
- 14.Boström P, Wu J, Jedrychowski MP, Korde A, Ye L, Lo JC, et al. A PGC1-α-dependent myokine that drives brown-fat-like development of white fat and thermogenesis. Nature. 2012;481(7382):463–468. doi: 10.1038/nature10777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tsuchiya Y, Ando D, Takamatsu K, Goto K. Resistance exercise induces a greater irisin response than endurance exercise. Metabolism. 2015;64(9):1042–1050. doi: 10.1016/j.metabol.2015.05.010. [DOI] [PubMed] [Google Scholar]
- 16.Hun-Young P, Won-Sang J, Jisu K, Hyejung Hwang KL. Changes in the paradigm of traditional exercise in obesity therapy and application of a new exercise modality: A narrative review article. Iran J Public Health. 2019;48(8):1395. [PMC free article] [PubMed] [Google Scholar]
- 17.Gaedtke A, Morat T. TRX suspension training: A new functional training approach for older adults–development, training control and feasibility. Int J Exerc Sci. 2015;8(3):224. doi: 10.70252/SWSX2936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rayes ABR, de Lira CAB, Viana RB, Benedito-Silva AA, Vancini RL, Mascarin N, et al. The effects of Pilates vs. aerobic training on cardiorespiratory fitness, isokinetic muscular strength, body composition, and functional tasks outcomes for individuals who are overweight/obese: a clinical trial. PeerJ. 2019;7:e6022. doi: 10.7717/peerj.6022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Janot J, Heltne T, Welles C, Riedl J, Anderson H, Howard A, et al. Effects of TRX versus traditional resistance training programs on measures of muscular performance in adults. J Fitness Res. 2013;2(2):23–38. [Google Scholar]
- 20.de Souza Cavina AP, Junior EP, Machado AF, Biral TM, Lemos LK, Rodrigues CRD, et al. Effects of the Mat Pilates Method on Body Composition: Systematic Review With Meta-Analysis. J Phys Act Health. 2020;17(6):673–681. doi: 10.1123/jpah.2019-0171. [DOI] [PubMed] [Google Scholar]
- 21.Wang Y, Chen Z, Wu Z, Ye X, Xu X. Pilates for overweight or obesity: A meta-analysis. Front Physiol. 2021;12. [DOI] [PMC free article] [PubMed]
- 22.Fernández-Rodríguez R, Álvarez-Bueno C, Ferri-Morales A, Torres-Costoso AI, Cavero-Redondo I, Martínez-Vizcaíno V. Pilates method improves cardiorespiratory fitness: a systematic review and meta-analysis. J Clin Med. 2019;8(11):1761. doi: 10.3390/jcm8111761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Melo KCB, de Souza AF, Júnior CCMC, de Andrade KTP, Moreira SR. Pilates method training: Functional and blood glucose responses of older women with type 2 diabetes. J Strength Condition Res. 2020;34(4):1001–1007. doi: 10.1519/JSC.0000000000002704. [DOI] [PubMed] [Google Scholar]
- 24.Yucel H, Uysal O. Pilates-based mat exercises and parameters of quality of life in women with Type 2 diabetes. Iran Red Crescent Med J. 2018;20(S1).
- 25.Nowak A, Morawiec M, Gabrys T, Nowak Z, Szmatlan-Gabryś U, Salcman V. Effectiveness of Resistance Training with the Use of a Suspension System in Patients after Myocardial Infarction. Int J Environ Res Public Health. 2020;17(15):5419. doi: 10.3390/ijerph17155419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ellefsen S, Vikmoen O, Slettaløkken G, Whist JE, Nygård H, Hollan I, et al. Irisin and FNDC5: effects of 12-week strength training, and relations to muscle phenotype and body mass composition in untrained women. Eur J Appl Physiol. 2014;114(9):1875–1888. doi: 10.1007/s00421-014-2922-x. [DOI] [PubMed] [Google Scholar]
- 27.Yang D, Yang Y, Li Y, Han R. Physical exercise as therapy for type 2 diabetes mellitus: from mechanism to orientation. Ann Nutr Metab. 2019;74(4):313–321. doi: 10.1159/000500110. [DOI] [PubMed] [Google Scholar]
- 28.Du X-L, Jiang W-X. Lower circulating irisin level in patients with diabetes mellitus: a systematic review and meta-analysis. Horm Metab Res. 2016;48(10):644–652. doi: 10.1055/s-0042-108730. [DOI] [PubMed] [Google Scholar]
- 29.Arhire LI, Mihalache L, Covasa M. Irisin: a hope in understanding and managing obesity and metabolic syndrome. Front Endocrinol. 2019;10:524. doi: 10.3389/fendo.2019.00524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guilford BL, Parson JC, Grote CW, Vick SN, Ryals JM, Wright DE. Increased FNDC 5 is associated with insulin resistance in high fat-fed mice. Physiol Rep. 2017;5(13):e13319. doi: 10.14814/phy2.13319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dianatinasab A, Koroni R, Bahramian M, Bagheri-Hosseinabadi Z, Vaismoradi M, Fararouei M, et al. The effects of aerobic, resistance, and combined exercises on the plasma irisin levels, HOMA-IR, and lipid profiles in women with metabolic syndrome: A randomized controlled trial. J Exerc Sci Fit. 2020;18(3):168–176. doi: 10.1016/j.jesf.2020.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Colberg SR, Sigal RJ, Fernhall B, Regensteiner JG, Blissmer BJ, Rubin RR, et al. Exercise and type 2 diabetes: the American College of Sports Medicine and the American Diabetes Association: joint position statement. Diabetes Care. 2010;33(12):e147–e167. doi: 10.2337/dc10-9990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Norheim F, Langleite TM, Hjorth M, Holen T, Kielland A, Stadheim HK, et al. The effects of acute and chronic exercise on PGC-1α, irisin and browning of subcutaneous adipose tissue in humans. FEBS J. 2014;281(3):739–749. doi: 10.1111/febs.12619. [DOI] [PubMed] [Google Scholar]
- 34.Gouni-Berthold I, Berthold HK, Huh JY, Berman R, Spenrath N, Krone W, et al. Effects of lipid-lowering drugs on irisin in human subjects in vivo and in human skeletal muscle cells ex vivo. PLoS ONE. 2013;8(9):e72858. doi: 10.1371/journal.pone.0072858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Momenzadeh S, Zamani S, Pourteymourfard-Tabrizi Z, Barreiro C, Jami M-S. Muscles proteome analysis; irisin administration mimics some molecular effects of exercise in quadriceps muscle. Biochimie. 2021;189:144–157. doi: 10.1016/j.biochi.2021.06.016. [DOI] [PubMed] [Google Scholar]
- 36.Liu T-Y, Shi C-X, Gao R, Sun H-J, Xiong X-Q, Ding L, et al. Irisin inhibits hepatic gluconeogenesis and increases glycogen synthesis via the PI3K/Akt pathway in type 2 diabetic mice and hepatocytes. Clin Sci. 2015;129(10):839–850. doi: 10.1042/CS20150009. [DOI] [PubMed] [Google Scholar]
- 37.Qiao X, Nie Y, Ma Y, Chen Y, Cheng R, Yin W, et al. Irisin promotes osteoblast proliferation and differentiation via activating the MAP kinase signaling pathways. Sci Rep. 2016;6(1):1–12. doi: 10.1038/srep18732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Viitasalo A, Atalay M, Pihlajamäki J, Jääskeläinen J, Korkmaz A, Kaminska D, et al. The 148 M allele of the PNPLA3 is associated with plasma irisin levels in a population sample of Caucasian children: the PANIC Study. Metabolism. 2015;64(7):793–796. doi: 10.1016/j.metabol.2015.01.010. [DOI] [PubMed] [Google Scholar]
- 39.Steinberg GR, Michell BJ, van Denderen BJ, Watt MJ, Carey AL, Fam BC, et al. Tumor necrosis factor α-induced skeletal muscle insulin resistance involves suppression of AMP-kinase signaling. Cell Metab. 2006;4(6):465–474. doi: 10.1016/j.cmet.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 40.Xiong X-Q, Chen D, Sun H-J, Ding J, Wang J-J, Chen Q, et al. FNDC5 overexpression and irisin ameliorate glucose/lipid metabolic derangements and enhance lipolysis in obesity. Biochim Biophys Acta (BBA)-Mol Basis Dis. 2015;1852(9):1867–1875. doi: 10.1016/j.bbadis.2015.06.017. [DOI] [PubMed] [Google Scholar]
- 41.Xiong X-Q, Geng Z, Zhou B, Zhang F, Han Y, Zhou Y-B, et al. FNDC5 attenuates adipose tissue inflammation and insulin resistance via AMPK-mediated macrophage polarization in obesity. Metabolism. 2018;83:31–41. doi: 10.1016/j.metabol.2018.01.013. [DOI] [PubMed] [Google Scholar]
- 42.Timmons JA, Baar K, Davidsen PK, Atherton PJ. Is irisin a human exercise gene? Nature. 2012;488(7413):E9–E10. doi: 10.1038/nature11364. [DOI] [PubMed] [Google Scholar]
- 43.Atherton PJ, Babraj JA, Smith K, Singh J, Rennie MJ, Wackerhage H. Selective activation of AMPK-PGC-1α or PKB-TSC2-mTOR signaling can explain specific adaptive responses to endurance or resistance training-like electrical muscle stimulation. FASEB J. 2005;19(7):1–23. doi: 10.1096/fj.04-2179fje. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.