Abstract
Introduction
Diabetic Foot (DF) as a common complication of Diabetes should be intensive intervention for prevention, management and rehabilitation. In this regard, Diabetes Research Center of Endocrinology and Metabolism Research Institute (EMRI) of Tehran University of Medical Sciences (TUMS) considered DF as a priority research area to investigate multidimensional aspects of DF care. We are intended to summarize DF research studies affiliated to the EMRI for over the last two decades.
Methods
Three Electronic databases including Web of Science, PubMed, and Scopus were searched until January 2020 to find articles about DF published affiliated to EMRI. The main concepts of search strategies were “diabetes”, “Foot”. 115 documents retrieved from these databases which screened for inclusion and exclusion criteria. The visualization of the network of co-authorship of authors and co-occurrence of keywords was illustrated and documents were analyzed for content according to the Main areas of DF Research studies.
Result
64 related documents including original articles, reviews, letters, notes, and book chapter have included to this study. According to the objectives of the retrieved studies, DF documents and research studies categorized in the two main groups including DF prevention, classification and risk stratification in addition management of DF.
Conclusion
Despite conducted research and educational activities in DF prevention and management, the following topics would be considered as well: effective offloading treatment, correcting the nutritional status for improving wound healing and novel educational strategies for diabetic foot multi-disciplinary team.
Keywords: Diabetic Foot, EMRI, Multi-disciplinary Approach
Introduction
Diabetic Foot (DF) is one of the most important and common complications of Diabetes Mellitus (DM) with neurologic and vascular disorders [1]. Actually it is estimated that every 20 s an amputation is performed in the lower limb because of DM in the world [2]. The global DF ulcer prevalence was estimated at 6.3% [3]. The prevalence of DFU in Iran was stated that about 3% in 2010 [4] and 6.4% in 2018 [5]. Regarding the rising health care costs [6], it could be cause of excessive burden on the patient, family and society[7].
Iranian Diabetic Foot Group as a subgroup of Diabetes Research Center of Endocrinology and Metabolism Research Institute (EMRI) actively participate in education, research, and care of DF for about two decades. Considering the importance of implementing the multidisciplinary approach to address DF [8], Iranian Diabetic Foot Research Group (IDFRG) affiliated to Diabetes Research Center of EMRI of Tehran University of Medical Sciences (TUMS) have established from 2014 [9].
In this current overview we intended to summarize the research and educational activities of EMRI on DF.
Method
Three Electronic databases including Web of Science, PubMed, and Scopus were searched until January 2020 to find articles about DF published affiliated to EMRI. The main concepts used in the search strategies for each database were “diabetes”, “foot”. The Mesh terms, Emtree terms and synonyms or related words also were used for retrieving all related publications in this subject. Keywords related to affiliation and address of EMRI was also included in the search strategy as well. It should be mentioned that we have inspected the main achievements of EMRI in the field of DF research and education.
115 documents retrieved from these databases and after screening these documents to identify the studies which had inclusion criteria that was each documents with topic of diabetic foot and EMRI affiliation and excluding unrelated documents. Two researchers (MA and NM) independently screened the abstracts from the searched documents. Disagreements were discussed with the third research team member to reach a consensus for including document. Finally 64 publications had included that the document types of them were original articles, reviews, letters, notes, and book chapter and all of these documents were included in the current review.
First, the visualization of the network of co-authorship of authors and co-occurrence of keywords is illustrated. Then these documents were analyzed for content according to the main areas of DF research studies.
The results explained in the text and presented in the figures.
Result
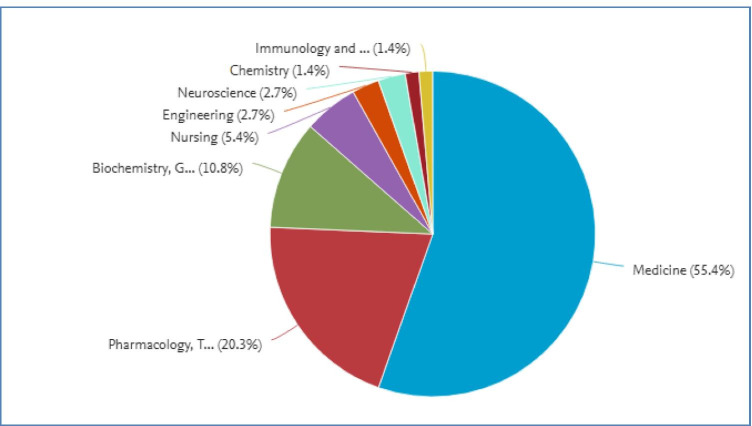
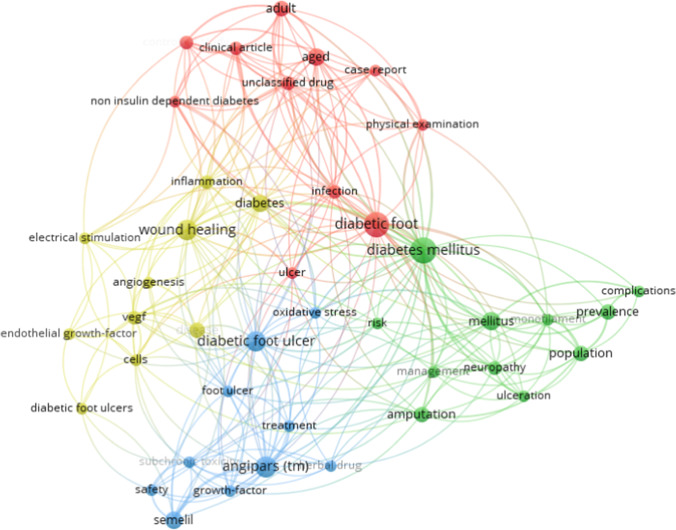
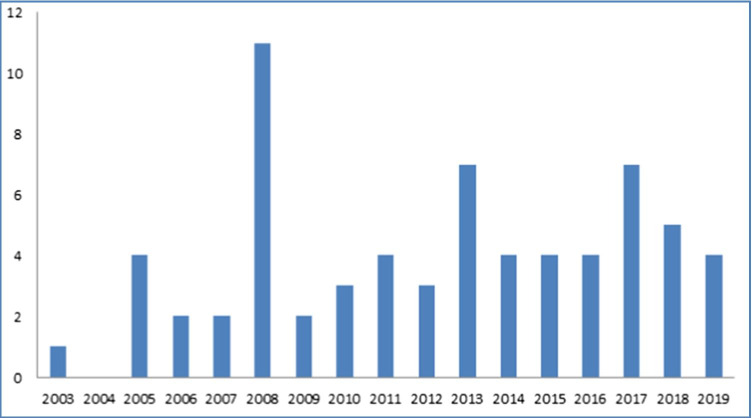
Different types of research documents in the form of original articles, reviews, letters, notes, and book chapter have been published. The research area has also shown (Fig. 1) and co-occurrence of keywords has shown in figure (Fig. 2). The year of publications also has demonstrated (Fig. 3). After studying the entered documents and reviewing the objectives of the retrieved studies, as well as based on the main topics of DF guidelines such as IWGDF guideline, DF documents and research studies categorized in the two main groups including DF prevention, classification and risk stratification as the first and prognosis and management of DF as the second one..
Fig. 1.
Diabetic Foot area in published articles
Fig. 2.
Network visualizations of co-occurance of keyword
Fig. 3.
Year of publications
DF prevention, classification and risk stratification
The studies which covered the prevention and risk stratification of DF classified into two subjects consist of education and screening.
In order to empower health care providers, team-based training workshops designed and endorsed by International Diabetes Federation (IDF) during 2014–2016 and European Wound Management Association (EWMA) during 2016–2019 as well. These workshops about prevention, education, assessment, and DF management implemented from 2014 tonow regularly [10]. Additionally 19 two-day and 8 one-day DF workshops round the country and 2 DF vocational course based on needs and the interest of health care providers have been held [9]. With regards to the health care providers progression and their role, Shokoohi et al., showed that residents of Internal Medicine as Educational Influentials (EIs) in clinical settings, play a key role in knowledge transfer [11]. Moreover, considering continuous education about foot self-care practice is necessary for patients with DM, a study with the aim of comparing the cognitive status and foot self-care practice in overweight patients with type 2 diabetes, conducted and the result showed that regular physical activity could promote the cognitive status and foot self-care practice [12].
Along with DF education, screening for risk stratification is another important subject would be considered in DF prevention area. One study with the aim of recognizing the potential risk factors for Diabetic Peripheral Neuropathy (DPN) showed that old age, male gender, poor DM control, and long-duration of DM are the main risk factors of DPN [13]. Moreover, DFU could be associated with high plantar pressure followed by DPN. In this regard, comparing the plantar pressure distribution in patients who suffered DPN with those without ones showed that the progression of DPN caused higher plantar pressure [14]. Additionally, the result of a study on detecting DPN showed that a combination of Michigan and monofilament test could be an accurate screening tool for DPN [15]. As well correlation of Michigan neuropathy screening instrument (MNSI), United Kingdom screening test (UKST), and nerve conduction studies (NCS) for early detection of DPN assessed in another study. Since NCS is considered as an objective, simple, and non-invasive tool with potential to determine the level of damage and regeneration in peripheral nerves, electro diagnosis would be recommended for screening, confirming, and follow up of DPN [16]. However, the comparison of different screening tests for detecting diabetic foot neuropathy in another study showed that the results of different peripheral neuropathy screening tests, even in the same group of patients, are different [17].
Prognosis and management of DF
In the area of DF management, novel medications and herbal therapies have been investigated in EMRI. In this regard, several studies were designed and developed to assess the effect of a new herbal extract called ANGIPARS in the wound healing process. It would be mentioned that the origin of Angipars is Melilotus officinalis. In the first step, toxicologic studies aiming at evaluating the acute and sub-chronic toxicity of Semelil (ANGIPARS) were performed [18–20]. Then, the maximum tolerated dose of this new herbal drug was assessed as the first phase of clinical research in this field which reported that the maximum tolerated dose of the medication is 10 mL/day [21]. In the second phase of clinical research about the safety and efficacy of ANGIPARS, results indicated that administering 4 mL (125 mg) of ANGIPARS intravenously and daily for 28 days could reduce the wound size at least 50% during eight weeks without any side effects [22]. In the third phase of clinical research about the therapeutic efficacy of different formulations of ANGIPARS including intravenous, oral, topical, and combination of oral and topical forms of the medication, a significant decrease in the size of DFUs was shown, while no clinical or paraclinical adverse effects were reported [23–26]. Finally, post-marketing surveillance on safety and effectiveness of ANGIPARS in DFU treatment was evaluated in which not only no adverse drug reactions (ADR) of oral and topical application of ANGIPARS was reported but also the immense effect and safety of ANGIPARS on treatment of diabetic foot ulcers was suggested [27]. In which the ulcers mean surface area was decreased (6.05 ± 11.1 cm2 VS 2.4 ± 6.9 cm2) ABI and TBI were risen (p < 0.05) after six weeks of therapy.
Other preliminary studies with the aim of wound healing are related to the various products of local therapies such as low-level laser therapy (LLLT) in which promoting the chronic healing process of wound with reduced microcirculation. Kaviani et al. [11] showed that At week 4, the size of ulcers significantly decreased in the LLLT group (p = 0.04) after 4 weeks and concluded that LLLT can improve the healing process of chronic DFUS and may shorten the period to reach complete healing [28]. Finally, a review on the role of antioxidants in the management of diabetes and its complications showed that use of antioxidants could be reduced the oxidative stress and alleviates diabetic complications [29].
Since infected DFU is a serious threat to the affected limb, it must be evaluated and treated promptly. Accordingly, some studies designed and developed considering this subject.
In this regard, a protocol for septic DFUs (including blood glucose control, intravenous antibiotic therapy, comorbidities control, revascularization, ulcer drainage and irrigation, systematic debridement, dressing changes and wound care, and amputation if necessary) has designed and followed for 2 years. It would be concluded that the septic DFU is not necessarily an amputation indication why aggressive management consist of metabolic and surgical care could be effective [30]. In another study, a clinical study investigated microbial pathogens and their antibiotic susceptibility profile in infected diabetic foot ulcers in Iranian patients indicated that most of infected DFU classified as Wagner grades 2 and 3 (15.7 and 75.7%). Therefore, appropriate empiric treatment to cover both gram positive and negative pathogens would be crucially considered [31].
In the overview about effectiveness of Negative Pressure Wound Therapy (NPWT), 23 systematic reviews on the effectiveness, safety, and cost benefits of NPWT interventions were considered. This overview illustrated that well-designed RCTs and meta-analysis can shed light on different aspects of NPWT would be essential [32].
Mohajeri-Tehrani et al., to evaluate the efficacy of a bioimplant dressing as a novel dressing in comparison with a wet dressing in patients with DFU found that the bioimplant dressing was significantly superior in DF wound healing. In which the complete healing rate (wound closure) in the control group was 16.7% while in bioimplant group was 40.7%. In this regard ease of use, lack of adverse effects and a wound healing process facilitation considered which make it properties [33].
In a study on evaluatation the efficacy and safety of transplanting autologous mesenchymal stem cells (MSCs), from granulocytecolony-stimulating factor (G-CSF)-mobilised peripheral blood in diabetic patients with critical limb ischemia, it was found that the transplantation of autologous peripheral blood MSCs, mobilized by G-CSF, induces angiogenesis and improves the wound healing process [34]. Not only pain was educed in the transplanted group (P = 0.014) but also the ABI of the transplanted group were improved significantly (P = 0.035).
In another study which intended to determine the efficacy of low-frequency ultrasound (LFU) in chronic wound healing and infection outcome in DFU, the result of the study showed that LFU debridement accompanied by standard wound care has a positive effect on wound healing and infection. The complete healing rate in UAW group was higher than control group (43.47% VS17.39%). There was no significant difference between the two modalities in the healing rate after three months, but LFU debridement can accelerate ulcer healing [35].
Actually, different novel treatment agents have been suggested to improve wound healing, including local-use of epidermal growth factor [36], vacuum-compression therapy (VCT), hyperbaric oxygen, and peripheral stem cell injection. Since all these treatments considered with partial effects for DFU improvement and amputation rate, more studies are necessary in this area [37].
From 537 keywords, 47 keywords meet the thresholds that were the occcurance of keyword at least 3 times and article, human, male and female keywords that were almost general words removed.
Discussion and conclusion
In spite of all conducted research in the past two decades and considering the multidimensional aspects of DF care, it is important to understand gaps based on the existing conditions to ensure that the best research map is adequately provided.
What's Ahead in Our Journey in Diabetic Foot Research?
It would be mentioned that all patients suffering from DFU should be referred to a multidisciplinary DF team rather than being in isolation without delay [1] to improve patient outcomes. DF care strategies that include prevention, classification, and risk stratification, patient and health care-providers education, prognosis, and management should be considered under the multidisciplinary approach umbrella that could reduce the burden of DFUs. Thus, the strategic plan of DFRG affiliated to the EMRI is toward to the right direction for improving a multidisciplinary team, as part of a comprehensive care plan [9, 38, 39].
Despite progress regarding the research and educational activities in DF prevention and management in our institute (EMRI), thereof still requires much research for the future about following topics: effective offloading treatment, correcting the nutritional status with the aim of improving healing and novel educational strategies based on the need assessment of the diabetic foot community.
We find gaps in knowledge to improve awareness of health care providers involved in DFU management, patient education, and dedicated podiatry facilities and clinics of DF care.
IWGDF guideline which developed by D-foot international groups should be translated and adopted for promoting its usage in both primary and referral settings all across the nation and implementing in the Iranian health care system.
In order to access the standard of care, specific pathways for DF care could be defined, cleared and implemented in primary and referral settings to avoid delayed referral and amputations.
Finally, patient registry system as a great utilization in accurate registration of Iranian patients with DF have detrimental role in control and alleviation of the burden of this grave consequence of diabetes in both inpatient and outpatient settings the country.
Acknowledgements
The authors would like to thank for Endocrinology and Metabolism Research Institute for fully support in preparing all included articles in the area of Diabetic Foot in the current review.
Declarations
Competing interests
None declared.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Neda Mehrdad, Email: nmehrdad@tums.ac.ir.
Mohammad Reza Amini, Email: mramini@tums.ac.ir.
Reference
- 1.Lipsky BA, Aragón-Sánchez J, Diggle M, Embil J, Kono S, Lavery L, et al. IWGDF guidance on the diagnosis and management of foot infections in persons with diabetes. Diabetes Metab Res Rev. 2016;32:45–74. doi: 10.1002/dmrr.2699. [DOI] [PubMed] [Google Scholar]
- 2.Bakker K, Apelqvist J, Lipsky B, Van Netten J, Schaper N, Foot IWGotD. The, IWGDF guidance documents on prevention and management of foot problems in diabetes: development of an evidence-based global consensus. Diabetes Metab Res Rev. 2015;2016(32):2–6. doi: 10.1002/dmrr.2694. [DOI] [PubMed] [Google Scholar]
- 3.Zhang P, Lu J, Jing Y, Tang S, Zhu D, Bi Y. Global epidemiology of diabetic foot ulceration: a systematic review and meta-analysis. Ann Med. 2017;49(2):106–116. doi: 10.1080/07853890.2016.1231932. [DOI] [PubMed] [Google Scholar]
- 4.Tabatabaei-Malazy O, Mohajeri-Tehrani MR, Pajouhi M, Fard AS, Amini MR, Larijani B. Iranian diabetic foot research network. Adv Skin Wound Care. 2010;23(10):450–454. doi: 10.1097/01.ASW.0000383222.79771.93. [DOI] [PubMed] [Google Scholar]
- 5.Yazdanpanah L, Shahbazian H, Nazari I, Arti HR, Ahmadi F, Mohammadianinejad SE, et al. Prevalence and related risk factors of diabetic foot ulcer in Ahvaz, south west of Iran. Diabetes Metab Syndr. 2018;12(4):519–524. doi: 10.1016/j.dsx.2018.03.018. [DOI] [PubMed] [Google Scholar]
- 6.Jeffcoate WJ, Vileikyte L, Boyko EJ, Armstrong DG, Boulton AJ. Current challenges and opportunities in the prevention and management of diabetic foot ulcers. Diabetes Care. 2018;41(4):645–652. doi: 10.2337/dc17-1836. [DOI] [PubMed] [Google Scholar]
- 7.Apelqvist J. The diabetic foot syndrome today: a pandemic uprise. The Diabetic Foot Syndrome. 26: Karger Publishers; 2018. p. 1–18.
- 8.Blume P, Wu S. Updating the Diabetic Foot Treatment Algorithm: Recommendations on Treatment Using Advanced Medicine and Therapies. Wounds: a compendium of clinical research and practice. 2018;30(2):29–35. [PubMed]
- 9.Aalaa M, Sanjari M, Mohajeri-Tehrani MR, Mehrdad N, Amini MR. A multidisciplinary team approach in Iranian diabetic foot research group. J Diabetes Metab Disord. 2019;18(2):721–723. doi: 10.1007/s40200-019-00450-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aalaa M, Sanjari M, Shahbazi S, Shayeganmehr Z, Abooeirad M, Amini MR, et al. Diabetic foot workshop: Improving technical and educational skills for nurses. Med J Islam Repub Iran. 2017;31:8. doi: 10.14196/mjiri.31.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shokoohi M, Nedjat S, Majdzadeh R. A social network analysis on clinical education of diabetic foot. J Diabetes Metab Disord. 2013;12(1). [DOI] [PMC free article] [PubMed]
- 12.Madarshahian F, Hassanabadi M, Koshniat Nikoo M. Cognitive status and foot self care practice in overweight diabetics, engaged in different levels of physical activity. J Diabetes Metab Disord. 2014;13(1). [DOI] [PMC free article] [PubMed]
- 13.Booya F, Bandarian F, Larijani B, Pajouhi M, Nooraei M, Lotfi J. Potential risk factors for diabetic neuropathy: a case control study. BMC Neurol. 2005;5. [DOI] [PMC free article] [PubMed]
- 14.Abri H, Aalaa M, Sanjari M, Amini MR, Mohajeri-Tehrani MR, Larijani B. Plantar pressure distribution in diverse stages of diabetic neuropathy. J Diabetes Metab Disord. 2019;18(1):33–39. doi: 10.1007/s40200-019-00387-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tabatabaei-Malazy O, Mohajeri-Tehrani MR, Madani SP, Heshmat R, Larijani B. The Prevalence of Diabetic Peripheral Neuropathy and Related Factors. Iran J Public Health. 2011;40(3):55–62. [PMC free article] [PubMed] [Google Scholar]
- 16.Fateh HR, Madani SP, Heshmat R, Larijani B. Correlation of Michigan neuropathy screening instrument, United Kingdom screening test and electrodiagnosis for early detection of diabetic peripheral neuropathy. J Diabetes Metab Disord. 2016;15. [DOI] [PMC free article] [PubMed]
- 17.Forouzandeh F, Ahari AA, Abolhasani F, Larijani B. Comparison of different screening tests for detecting diabetic foot neuropathy. Acta Neurol Scand. 2005;112(6):409–413. doi: 10.1111/j.1600-0404.2005.00494.x. [DOI] [PubMed] [Google Scholar]
- 18.Abdollahi M, Farzamfar B, Salari P, Khorram KHR, Larijani B, Farhadi M, et al. Evaluation of acute and sub-chronic toxicity of Semelil (ANGIPARS (TM)), a new phytotherapeutic drug for wound healing in rodents. Daru. 2008;16:7–14. [Google Scholar]
- 19.Farzamfar B, Abdollahi M, Ka'abinejadian S, Heshmat R, Shahhosseiny MH, Novitsky YA, et al. Sub-chronic toxicity study of a novel herbal-based formulation (Semelil) on dogs. Daru. 2008;16:15–19. [Google Scholar]
- 20.Khorram KHR, Sadeghi B, Heshmat R, Abdollahi M, Salari P, Farzamfar B, et al. In vivo and in vitro genotoxicity studies of Semelil (ANGIPARS (TM)) Daru. 2008;16:20–24. [Google Scholar]
- 21.Heshmat R, Mohammad K, Mohajeri TMR, Tabatabaie MO, Keshtkar AA, Gharibdoust F, et al. Assessment of maximum tolerated dose of a new herbal drug, Semelil (ANGIPARS (TM)) in patients with diabetic foot ulcer: A phase I clinical. Daru. 2008;16:25–30. [Google Scholar]
- 22.Masoompour SM, Bagheri MH, Borhani HA, Novitsky YA, Sadeghi B, Gharibdoust F, et al. Effect of ANGIPARS (TM), a new herbal drug on diabetic foot ulcer: A phase 2 clinical study. Daru. 2008;16:31–34. [Google Scholar]
- 23.Larijani B, Heshmat R, Bahrami A, Delshad H, Ranjbar OG, Mohammad K, et al. Effects of intravenous Semelil (ANGIPARS (TM)) on diabetic foot ulcers healing: A multicenter clinical trial. Daru-Journal of Faculty of Pharmacy. 2008;16:35–40. [Google Scholar]
- 24.Bahrami A, Kamali K, Ali-Asgharzadeh A, Hosseini P, Heshmat R, Khorram KHR, et al. Clinical application of oral form of ANGIPARS (TM) and in combination with topical form as a new treatment for diabetic foot ulcers: A randomized clinical trial. Daru. 2008;16:41–48. [Google Scholar]
- 25.Shamimi NK, HESHMAT R, Karimian R, Nasli E, Novitsky Y, Farhadi M, et al. Intravenous Semelil (ANGIPARS™) as a novel therapy for pressure Ulcers: A randomized clinical trial. 2008.
- 26.Shamimi NK, Karimian R, Nasli E, Kamali K, Chaman R, Farhadi M, et al. Topical application of Semelil (ANGIPARS™) in treatment of pressure ulcers: A randomized clinical trial. 2008.
- 27.Ebrahimi M, Bakhshayeshi S, Heshmat R, Shahbazi S, Aala M, Peimani M, et al. Post marketing surveillance on safety and effectiveness of ANGIPARS in treatment of diabetic foot ulcers. Daru. 2009;17:45–49. [Google Scholar]
- 28.Kaviani A, Djavid GE, Ataie-Fashtami L, Fateh M, Ghodsi M, Salami M, et al. A Randomized Clinical Trial on the Effect of Low-Level Laser Therapy on Chronic Diabetic Foot Wound Healing: A Preliminary Report. Photomed Laser Surg. 2011;29(2):109–114. doi: 10.1089/pho.2009.2680. [DOI] [PubMed] [Google Scholar]
- 29.Rahimi R, Nikfar S, Larijani B, Abdollahi M. A review on the role of antioxidants in the management of diabetes and its complications. Biomed Pharmacother. 2005;59(7):365–373. doi: 10.1016/j.biopha.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 30.Shojaiefard A, Khorgami Z, Larijani B. Septic diabetic foot is not necessarily an indication for amputation. J Foot Ankle Surg. 2008;47(5):419–423. doi: 10.1053/j.jfas.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 31.Rouhipour N, Hayatshahi A, Nikoo MK, Yazdi NM, Heshmat R, Qorbani M, et al. Clinical microbiology study of diabetic foot ulcer in Iran; pathogens and antibacterial susceptibility. Afr J Microbiol Res. 2012;6(27):5601–5608. [Google Scholar]
- 32.Mohseni S, Aalaa M, Atlasi R, Tehrani MRM, Sanjari M, Amini MR. The effectiveness of negative pressure wound therapy as a novel management of diabetic foot ulcers: an overview of systematic reviews. J Diabetes Metab Disord. 2019:1–17. [DOI] [PMC free article] [PubMed]
- 33.Mohajeri-Tehrani MR, Variji Z, Mohseni S, Firuz A, Annabestani Z, Zartab H, et al. Comparison of a Bioimplant Dressing With a Wet Dressing for the Treatment of Diabetic Foot Ulcers: A Randomized, Controlled Clinical Trial. Wounds-Compend Clin Res Pract. 2016;28(7):248–254. [PubMed] [Google Scholar]
- 34.Mohammadzadeh L, Samedanifard SH, Keshavarzi A, Alimoghaddam K, Larijani B, Ghavamzadeh A, et al. Therapeutic Outcomes of Transplanting Autologous Granulocyte Colony-stimulating Factor-mobilised Peripheral Mononuclear Cells in Diabetic Patients with Critical Limb Ischaemia. Exp Clin Endocrinol Diabet. 2013;121(1):48–53. doi: 10.1055/s-0032-1311646. [DOI] [PubMed] [Google Scholar]
- 35.El Fattah AMA, Shaaban M, Gawish H, El Mashad N, Dawood AED. Effect of ultrasound-assisted debridement on wound healing and infection outcomes in diabetic foot. Menoufia Medical Journal. 2018;31(2):462. [Google Scholar]
- 36.Larijani B, Afshari M, Fadaei M, Pajouhi M, Bastanhagh M, Baradar JR. Effect of local epidermal growth factor on wound healing in diabetic foot. Iranian Journal of Endocrinology and Metabolism. 2003;5(2):107–110. [Google Scholar]
- 37.Larijani B, Hasani RS. Overview of diabetic foot; novel treatments in diabetic foot ulcer. Daru. 2008;16:1–6. [Google Scholar]
- 38.Mohajeri-Tehrani MR, Aalaa M, Mohseni SH, Anabestani Z, Larijani B. Multidisciplinary Approach in Diabetic Foot Care in Iran (New Concept) Iran J Public Health. 2012;41(6):103–104. [PMC free article] [PubMed] [Google Scholar]
- 39.Malazy OT, Mohajeri-Tehrani MR, Pajouhi M, Fard AS, Amini MR, Larijani B. Iranian Diabetic Foot Research Network. Adv Skin Wound Care. 2010;23(10):450–454. doi: 10.1097/01.ASW.0000383222.79771.93. [DOI] [PubMed] [Google Scholar]