Abstract
Objectives. To determine whether there have been shifts in nonmedical ketamine use, poisonings (“exposures”), and seizures.
Methods. We used generalized additive models to detect trends in past-year use (2006–2019), exposures (1991–2019), and seizures (2000–2019) involving ketamine in the United States.
Results. There was a quarterly increase in self-reported past-year nonmedical ketamine use in 2006 to 2014 (Β = 0.21; P = .030) and an increase in 2015 to 2019 (Β = 0.29; P = .036), reaching a peak of 0.9% in late 2019. The rate of exposures increased from 1991 through 2019 (Β = 0.87; P = .006), and there was an increase to 1.1 exposures per 1 000 000 population in 2014, with rates remaining stable through 2019. The rate of ketamine seizures increased from 2000 through 2019 (Β = 2.27; P < .001), with seizures reaching a peak in 2019 at 3.2 per 1000 seizures.
Conclusions. Indicators suggest that ketamine use and availability has increased, including before increased medical indications, but nonmedical use is still currently uncommon despite increased acceptance and media coverage. (Am J Public Health. 2021;111(11):2046–2049. https://doi.org/10.2105/AJPH.2021.306486)
Ketamine is a dissociative anesthetic that has been prevalent as a recreational drug in nightclubs for decades.1,2 However, ketamine has been used as an anesthetic in both animals and humans for a half century.3 Evidence indicates that ketamine produces analgesia without substantial respiratory depression in both children and adults, and thus its use is particularly common in prehospital settings (e.g., among emergency medical technicians) and in field conditions (e.g., in low-income countries).3 Ketamine has not been widely used in psychiatry until recently. Randomized double-blind controlled-placebo trials have recently determined that intranasal nonanesthetic doses of esketamine, an enantiomer of ketamine, can have an ultrarapid antidepressant effect among those with major depression.4 In response to studies demonstrating the drug’s efficacy in treating treatment-resistant depression, on March 5, 2019, the US Food and Drug Administration approved the use of esketamine nasal spray to treat this condition.
Findings on the drug’s efficacy and Food and Drug Administration approval led to increased availability of ketamine in psychiatric treatment settings. Such coverage, however, also led to extensive media coverage of the drug. Since ketamine’s approval for use in psychiatric settings, the drug has been covered in many major US news sources, including USA Today and the New York Times,5,6 and many articles refer to ketamine as a “club drug” or refer to it by its street name: “Special K.” Given that media coverage can affect drug use patterns in the general population,7 it is unknown whether such coverage about the benefits of use of a club drug may have created mixed messages regarding the drug’s safety or acceptability to use recreationally. Estimated past-year use of ketamine—which is assumed to be nonmedical use—was found to have significantly increased among nightclub and dance festival attendees in New York City between 2016 and 2019 (from 5.9% to 15.3%),2 but trends in use in the general population have remained largely unknown. We examined trends in ketamine use and availability using multiple forms of national indicator data.
METHODS
We analyzed data from 3 national data sources. First, we estimated trends in quarterly prevalence of ketamine use based on past-year report among participants aged 12 to 34 years in the 2006 to 2019 National Survey on Drug Use and Health (NSDUH), a nationally representative survey of noninstitutionalized individuals in the United States.8 Ketamine use was asked about in a section querying hallucinogen or psychedelic use in which participants were asked about use of “ketamine, also called ‘Special K’ or ‘Super K,’ ” so we assumed reported use to be mainly nonmedical use.
We examined quarterly trends in past-year use separately (using weighted data) before and after 2015 because of a change in survey design.8 Then, we estimated trends in poisonings (“exposures”) reported to poison control centers (PCCs) involving ketamine and its analogs from 1991 to 2019. There are 55 PCCs that cover the United States and its territories, and, since 2003, data have been stored in the National Poison Data System, which replaced the previous Toxic Exposure Surveillance System.9 We converted counts to rates per 1 000 000 persons based on the US Census. Finally, we estimated trends in seizures tracked by the Drug Enforcement Administration’s National Forensic Laboratory Information System (NFLIS) from 2000 to 2019 based on counts converted into rates per 1000 annual total drug seizures.
The NFLIS systematically collects seizure results from federal, state, and local forensic laboratories throughout all 50 states.10 We chose years for inclusion for all data sources based on data availability. We analyzed case-level data for NSDUH and extracted count data from PCCs and the NFLIS from annual reports.9,10 We used generalized additive models with cubic basis functions to fit regression splines with automated selection of knots to visually capture nonlinear trends. We plotted trends with 95% confidence intervals for model predictions. We then modeled trends with orthogonal polynomial terms. Data and code can be found at https://github.com/caroruth/ketaminetrends.
RESULTS
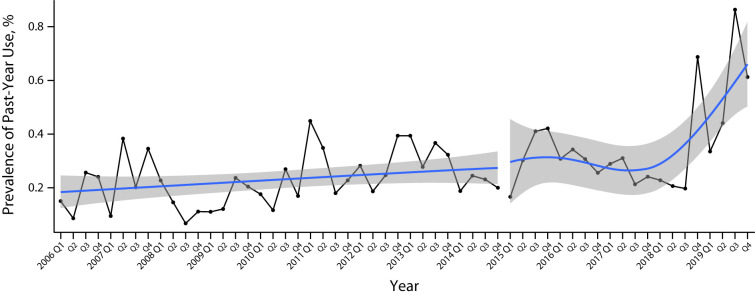
There was a linear quarterly increase in self-reported past-year ketamine use (via the NSDUH) in 2006 to 2014 (Β = 0.21; SE = 0.01; P = .030) with a nadir in late 2008 of 0.1% and then a cubic increase in 2015 to 2019 (Β = 0.29; SE = 0.13; P = .036), reaching a peak of 0.9% in late 2019 (Figure 1). The rate of exposures reported to PCCs increased in a cubic manner from 1991 through 2019 (Β = 0.87; SE = 0.29; P = .006; Figure A, available as a supplement to the online version of this article at https://www.ajph.org). Reported exposures began in 1991 at 0.1 exposures per 1 000 000 population and increased to a peak of 1.4 exposures per 1 000 000 in 2000. Rates then decreased to 0.4 exposures per 1 000 000 in 2008 and increased to 1.1 exposures per 1 000 000 in 2014 and remained somewhat stable through 2019. The rate of seizures increased in a quadratic manner from 2000 through 2019 (Β = 2.27; SE = 0.33; P < .001), with seizures reaching a nadir in 2004 to 2005 at 0.27 per 1000 and increasing from 2011 through a peak in 2019 at 3.2 per 1000 (Figure B, available as a supplement to the online version of this article at https://www.ajph.org).
FIGURE 1—
Trends in Self-Reported Past-Year Ketamine Use, Aged 12–34 Years: United States, 2006–2019
DISCUSSION
Our results suggest increased nonmedical use and availability of ketamine in recent years—particularly in the past year. However, despite a recent increase in prevalence of nonmedical ketamine use, prevalence remained relatively rare, below 1%. Exposures as reported to PCCs were highest in 2000 to 2001, which was also the peak in use of other club drugs such as MDMA (3,4-methylenedioxymethamphetamine), also known as ecstasy,11 possibly suggesting ketamine’s close link to recreational use in nightlife scenes. After a decline in exposures, there was an increase again through 2014, but exposures have remained relatively consistent thereafter. Rates of ketamine seizures, however, have increased exponentially since 2012, suggesting increasing availability, although seizures are still uncommon relative to other drugs. Overall, results suggest that use and availability are indeed increasing, but ketamine remains an uncommon recreational drug.
Detected increases in ketamine use corroborate recent detected increases in recreational use among nightclub and dance festival attendees in New York City,2 so use appears to be increasing both in this high-risk population and in the general population. However, to better inform prevention and harm reduction efforts, future research is needed to determine use and exposure trends according to demographic and other drug use characteristics to obtain a clearer picture regarding which subpopulations are increasing use. Further, studies are needed to directly determine whether findings on the efficacy of ketamine and associated media coverage are directly linked to increasing use.
Limitations
This study is not without limitations. Data on ketamine use and exposure are likely underreported because data rely on self-report. We assumed NSDUH data on ketamine use to refer to nonmedical use, but it is possible that some use was medical use. Count data from PCCs was limited, as we were not able to deduce with confidence the extent of “abuse” or intentional misuse among cases. Finally, people who use synthetic drugs such as ecstasy can be unknowingly exposed to ketamine as an adulterant, and this also leads to underreporting of use.12
Public Health Implications
National indicator data suggest that nonmedical ketamine use and availability are increasing in the United States, but use is still uncommon—even despite increased acceptance and media coverage. Ketamine is used medically throughout much of the world, and access to appropriate medical use is warranted; however, it is important for surveillance efforts focusing on nonmedical use to also continue to inform prevention and harm reduction.
ACKNOWLEDGMENTS
This research was supported by the National Institute on Drug Abuse, National Institutes of Health ([NIH] grant R01DA044207 to J. J. P. and U01DA051126 to Linda P. Cottler).
Note. The NIH did not have a role in the design of the study, the analysis of the data, the writing of the article, or the decision to submit the present research.
CONFLICTS OF INTEREST
J. J. Palamar has consulted for the biopharmaceutical company Alkermes plc. The authors have no other potential conflicts of interest to declare.
HUMAN PARTICIPANT PROTECTION
This study was exempt from institutional review board review because it was a secondary data analysis and therefore did not include human participants.
REFERENCES
- 1. Halkitis PN, Palamar JJ, Mukherjee PP. Poly-club-drug use among gay and bisexual men: a longitudinal analysis. Drug Alcohol Depend. . 2007;89(2–3):153–160. doi: 10.1016/j.drugalcdep.2006.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Palamar JJ, Keyes KM. Trends in drug use among electronic dance music party attendees in New York City, 2016–2019. Drug Alcohol Depend. . 2020;209:107889. doi: 10.1016/j.drugalcdep.2020.107889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kohtala S. Ketamine—50 years in use: from anesthesia to rapid antidepressant effects and neurobiological mechanisms. Pharmacol Rep. . 2021;73(2):323–345. doi: 10.1007/s43440-021-00232-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zheng W, Cai DB, Xiang YQ, et al. Adjunctive intranasal esketamine for major depressive disorder: a systematic review of randomized double-blind controlled-placebo studies. J Affect Disord. . 2020;265:63–70. doi: 10.1016/j.jad.2020.01.002. [DOI] [PubMed] [Google Scholar]
- 5.Bacon J.2019. https://www.usatoday.com/story/news/nation/2019/03/06/esketamine-nasal-spray-drug-could-transform-treatment-depression/3077883002
- 6.Carey B.2019. https://www.nytimes.com/2019/02/12/health/depression-drugs-ketamine.html
- 7. Lu CY, Zhang F, Lakoma MD, et al. Changes in antidepressant use by young people and suicidal behavior after FDA warnings and media coverage: quasi-experimental study. BMJ. . 2014;348:g3596. doi: 10.1136/bmj.g3596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Survey on Drug Use and Health 2014 and 2015 Redesign Changes. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2015. [PubMed] [Google Scholar]
- 9. Gummin DD, Mowry JB, Beuhler MC, et al. 2019 Annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 37th annual report. Clin Toxicol (Phila). . 2020;58(12):1360–1541. doi: 10.1080/15563650.2020.1834219. [DOI] [PubMed] [Google Scholar]
- 10.National Forensic Laboratory Information System: NFLIS-Drug 2019 Annual Report. Springfield, VA: US Department of Justice; 2020. [Google Scholar]
- 11.Miech RA, Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE, Patrick ME.Monitoring the Future National Survey Results on Drug Use, 1975–2019. Volume 1: Secondary School Students. Ann Arbor, MI: University of Michigan Institute for Social Research; 2020. [Google Scholar]
- 12. Palamar JJ, Salomone A, Rutherford C, Keyes KM. Extensive underreported exposure to ketamine among electronic dance music party attendees. J Gen Intern Med. . 2021;36(1):235–237. doi: 10.1007/s11606-020-05672-x. [DOI] [PMC free article] [PubMed] [Google Scholar]