Abstract
Background & Aims:
There were an estimated 4.8 million new cases of gastrointestinal (GI) cancers and 3.4 million related deaths, worldwide, in 2018. GI cancers account for 26% of the global cancer incidence and 35% of all cancer-related deaths. We investigated the global burden from the 5 major GI cancers as well as geographic and temporal trends in cancer-specific incidence and mortality.
Methods:
Data on primary cancers of the esophagus, stomach, colorectum, liver, and pancreas were extracted from the GLOBOCAN database for the year 2018, as well as from the Cancer Incidence in 5 Continents series, and the World Health Organization mortality database from 1960 onward. Age-standardized incidence and mortality rates were calculated by sex, country, and level of human development.
Results:
We observed geographic and temporal variations in incidence and mortality for all 5 types of GI cancers. Esophageal, gastric, and liver cancers were more common in Asia than in other parts of the world, whereas of the burden from colorectal and pancreatic cancers was highest in Europe and North America. There was a uniform decrease in gastric cancer incidence but an increasing incidence of colorectal cancer in formerly low-incidence regions over the studied time period. We found slight increases in incidence of liver and pancreatic cancer in some high-income regions.
Conclusions:
Although the incidence of some GI cancer types has decreased, this group of malignancies continues to pose major challenges to public health. Primary and secondary prevention measures are important for controlling these malignancies—most importantly reducing consumption of tobacco and alcohol, obesity control, immunizing populations against hepatitis B virus infection, and screening for colorectal cancer.
Keywords: cancer, global, incidence, mortality, risk factors, epidemiology
Introduction
With an estimated 4.8 million new cases and 3.4 million deaths worldwide in 2018, cancers of the gastrointestinal (GI) tract represent over one-quarter (26%) of the global cancer incidence and over one-third (35%) of all cancer-related deaths (Figure 1).1 The principle malignant conditions of the GI tract, namely cancers of the stomach (approximately 1.0 million new cases in 2018), liver (840 000 cases), oesophagus (570 000 cases), pancreas (460 000 cases), and colorectum (1.8 million cases), share a few common risk factors, but are largely distinct in their etiologies and descriptive epidemiologic profiles.
Figure 1.
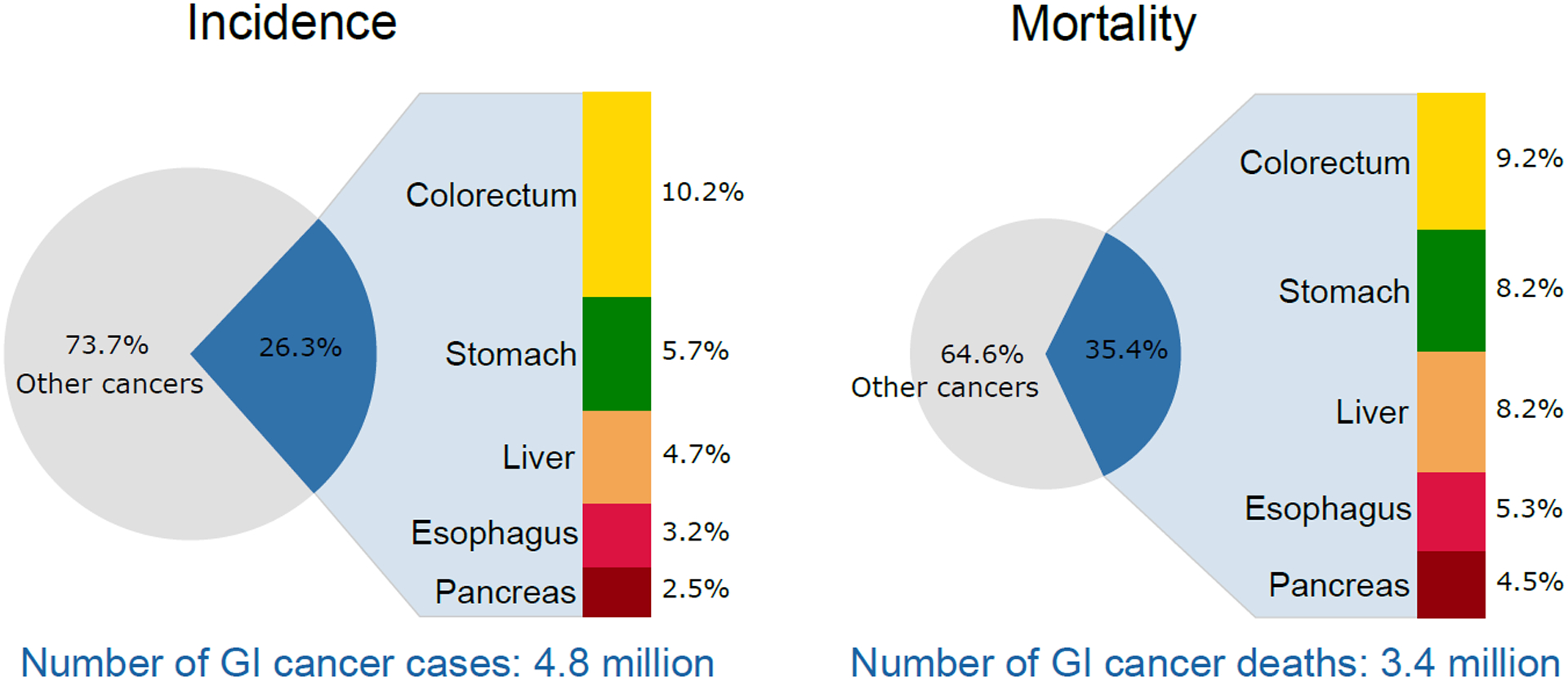
Contribution of major gastrointestinal cancers to global cancer cases and deaths in 2018. Source: GLOBOCAN 2018
According to recent studies, more than half of all GI cancers are caused by modifiable risk factors, including alcohol consumption and tobacco smoking, as well as infection, diet and obesity.2–7 The marked temporal variations in the incidence of the main GI cancer types over the past decades have been largely ascribed to changes in the prevalence of these risk factors.8,9 Prognosis tends to be poor given the late-stage of most diagnoses10,11, and hence site-specific mortality trends continue to mirror those of incidence, with the exception of colorectal cancer for which prognosis is generally good as a consequence of advances in both early detection and treatment.
Based on projected changes in the age composition and growth of the world population, the global number of new cases of, and deaths from GI cancers are predicted to increase by 58% and 73% to 7.5 and 5.6 million, respectively, by 2040.12 The extent of the pending burden serves to both highlight the necessity of future clinical services planning for GI cancers, and the need to prioritize and implement preventative actions that can avert many future diagnoses and deaths.
In this article, we describe the global burden from the major cancers of the GI tract: cancers of the esophagus, stomach, colorectum, liver, and pancreas. While the primary focus is a geographic description of cancer- and sex-specific incidence and mortality patterns by world region, we also present historical trends in incidence and mortality, and discuss associated risk factors, as well as prospects for prevention and impact on clinical practice.
Materials and Methods
The current GLOBOCAN database1, which comprises estimates of cancer incidence and mortality by country, cancer site and sex for the year 2018 available at the Global Cancer Observatory (http://gco.iarc.fr/today), was used to describe the burden of GI cancers from a global perspective. Incidence and mortality rates are presented globally and for 20 aggregated world regions, as defined by the United Nations Population Division.13 We also characterize the burden of GI cancers according to the human development index (HDI), which was created by the United Nations Development Program to highlight the importance of national policy decisions beyond economic growth in assessing development outcomes. Country-level estimates can be retrieved from the Global Cancer Observatory.
A second source, the Cancer Incidence in Five Continents series (CI5, http://ci5.iarc.fr/) compiles high-quality recorded cancer incidence data from national or subnational level population-based cancer registries (PBCR) worldwide.14 To obtain insights into real-world geographic disparities and trends over time, we used data from Volume XI of the CI5 series containing recorded incidence data from 343 high-quality population-based cancer registries (PBCR) in 65 countries for the 2008–2012 period.15 To explore long-term trends in incidence since the 1960s, annual data were extracted from the CI5 plus database (http://ci5.iarc.fr/CI5plus). Mortality data were obtained from the WHO mortality database compiled by IARC for countries with long term data available from 1985 onwards.
From each source, the numbers of new cancer cases and cancer deaths were extracted for five main GI cancers using the International Classification of Diseases 10th Revision codes (ICD-10): esophagus (ICD-10 C15), stomach (C16), colorectum (C18–21), liver (C22, including intrahepatic bile ducts) and pancreas (C25). Age-standardized rates (ASRs) per 100,000 person-years were calculated using the direct method and the world standard population.16 The cumulative risk of developing or dying from cancer before age 75 years, assuming the absence of competing causes of death, was calculated using the age-specific rates and is expressed as a percentage.17 Both these indicators allow comparisons between populations, adjusting for differences in age structures.
Results & Discussion
Of the 4.8 million new cases and 3.4 million deaths from GI cancers in 2018, it is estimated that 63% of cases and 65% of deaths occurred in Asia (38% and 41% in China alone, respectively), followed by Europe and North America, which together accounted for 26% of the global cases and 23% of the deaths (Figure 2). In contrast, the proportion of deaths from GI cancers is greater than that of new cancer cases in Africa (5% vs 4%) and Asia (65% vs 63%) given the case distribution but also the generally higher case fatality rates. The distribution of specific GI cancer types also differed across world regions. While esophageal, gastric and liver cancers were more common in Asia, a larger proportion of colorectal and pancreatic cancers occurred in Europe and North America. This is also reflected in the distribution of cases across levels of human development, with 53% of all pancreatic and 49% of colorectal cancer cases occurring in very high HDI countries (Annex Tables 1–5). Globally, GI cancers are twice as common in men as they are in women; 8 in 100 men and 4 in 100 women will develop a GI cancer before age 75.
Figure 2.
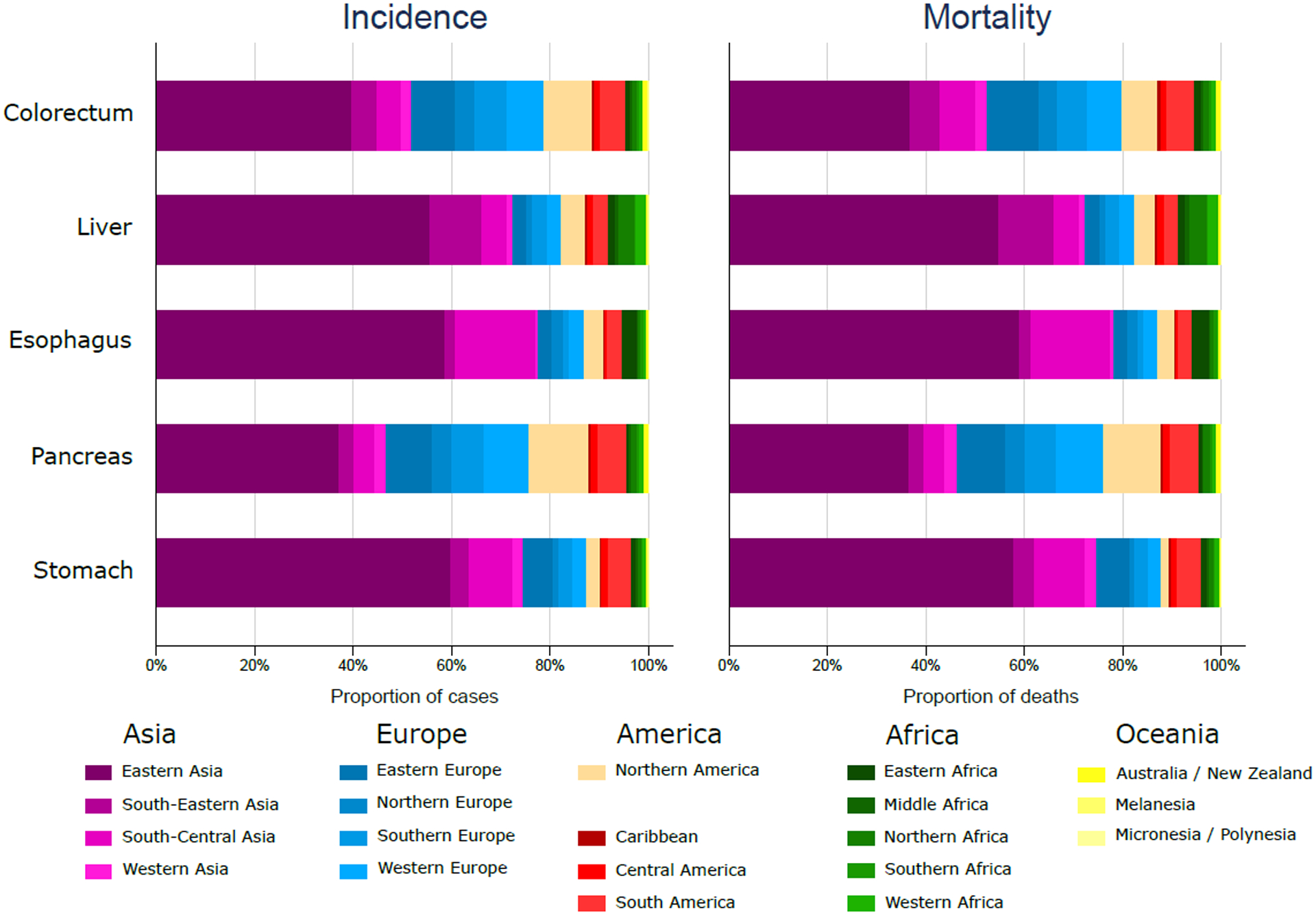
Distribution of new cases and deaths by world area and cancer site in 2018. Source: GLOBOCAN 2018
1. Esophageal cancer
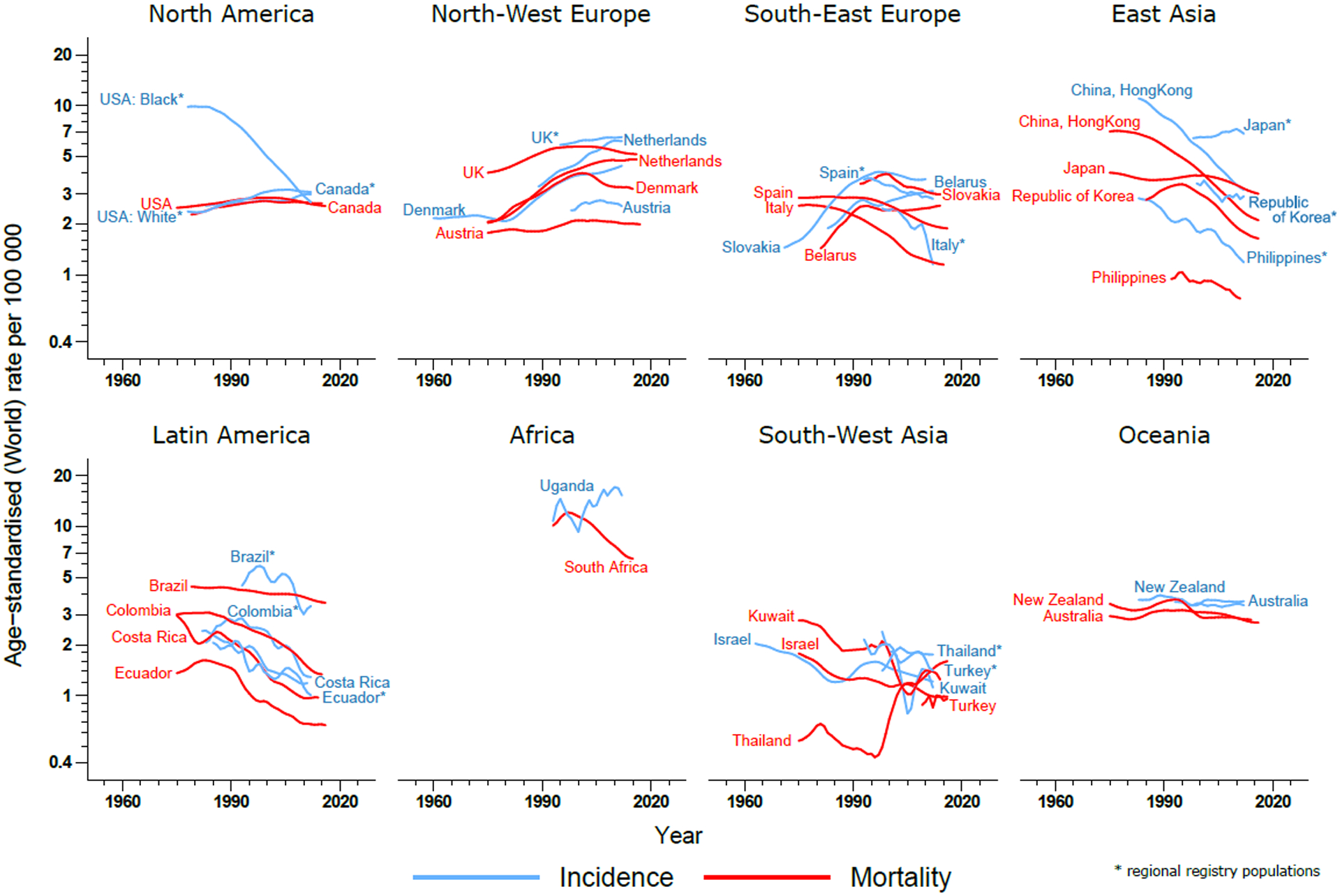
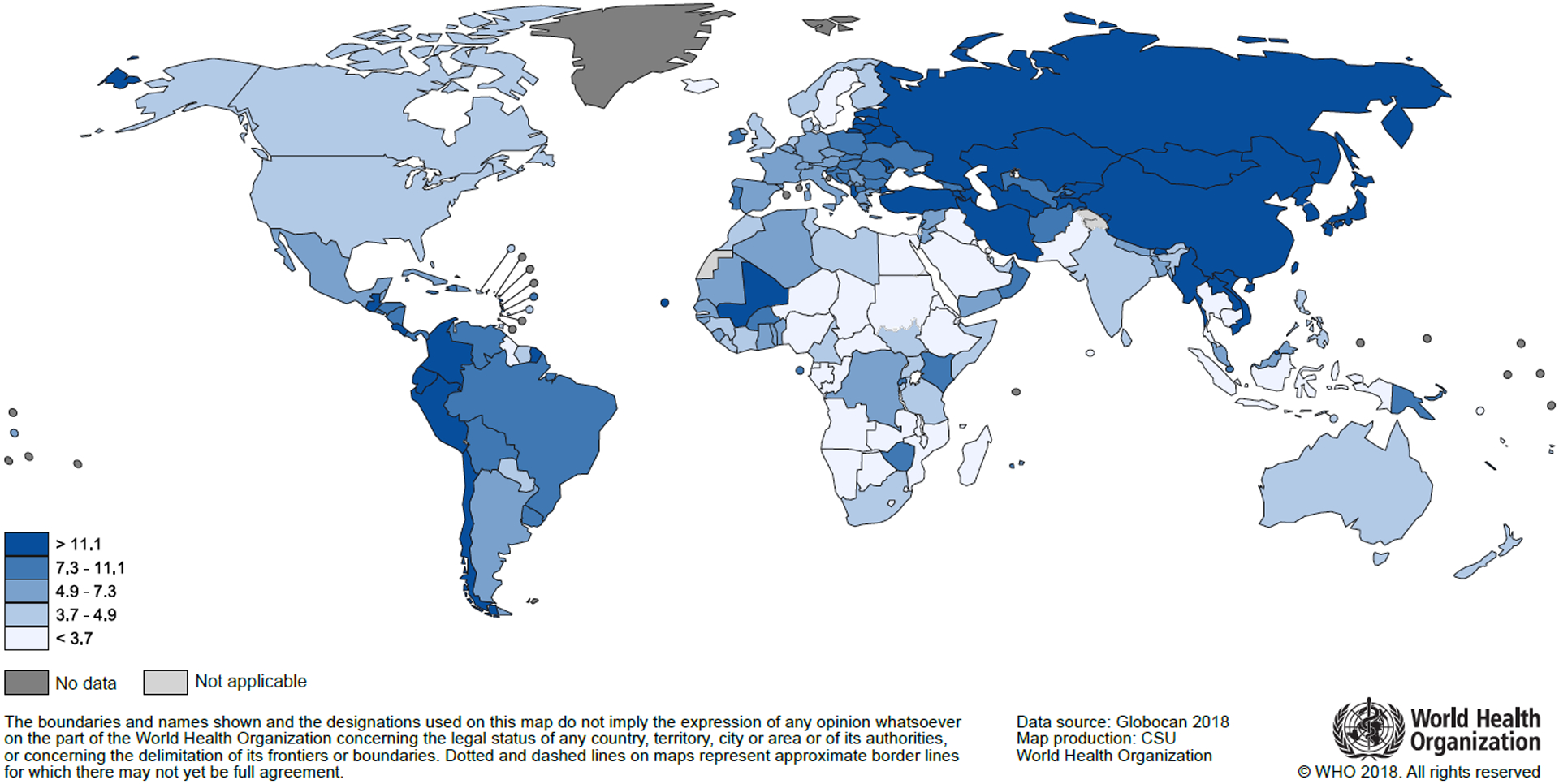
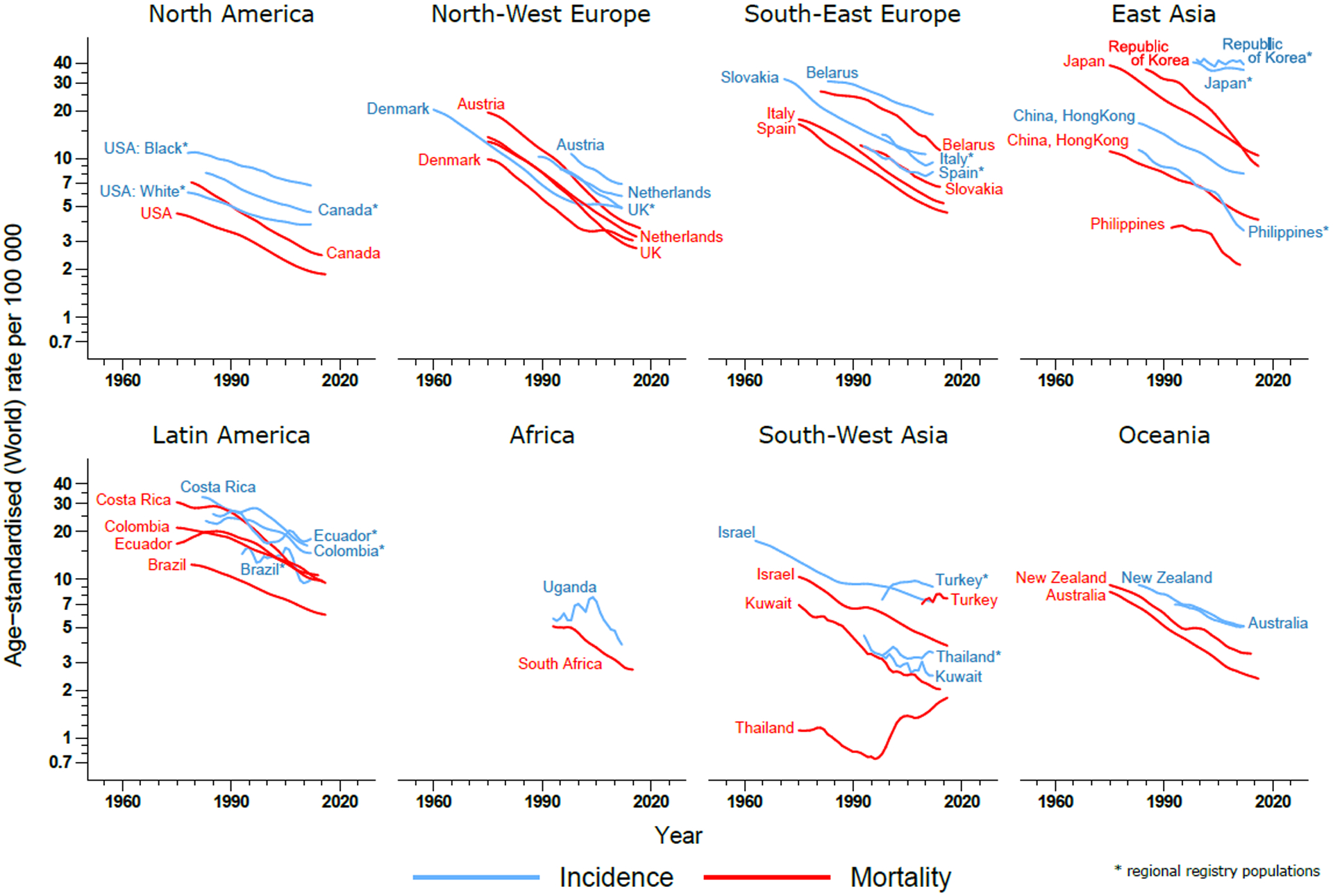
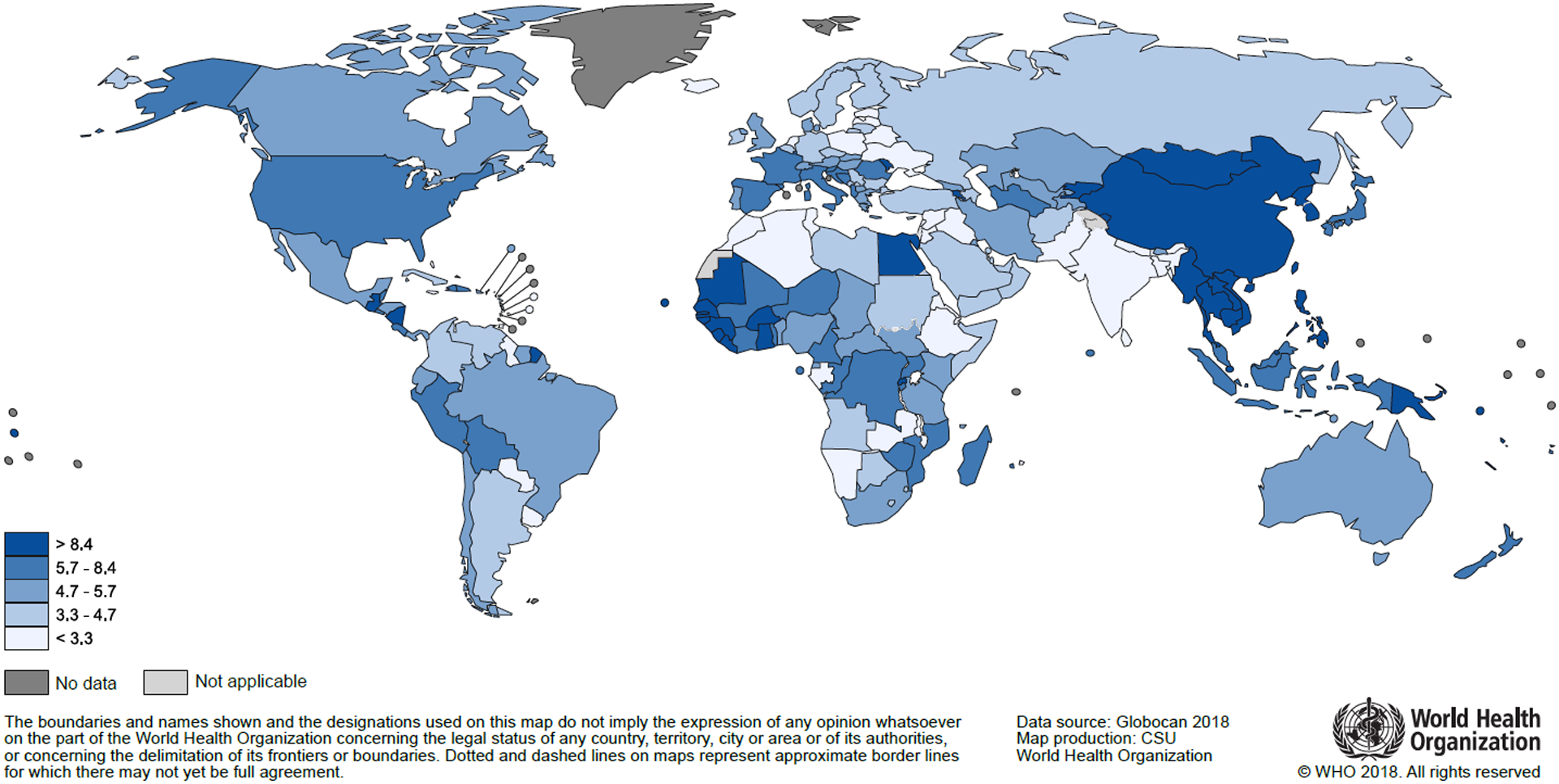
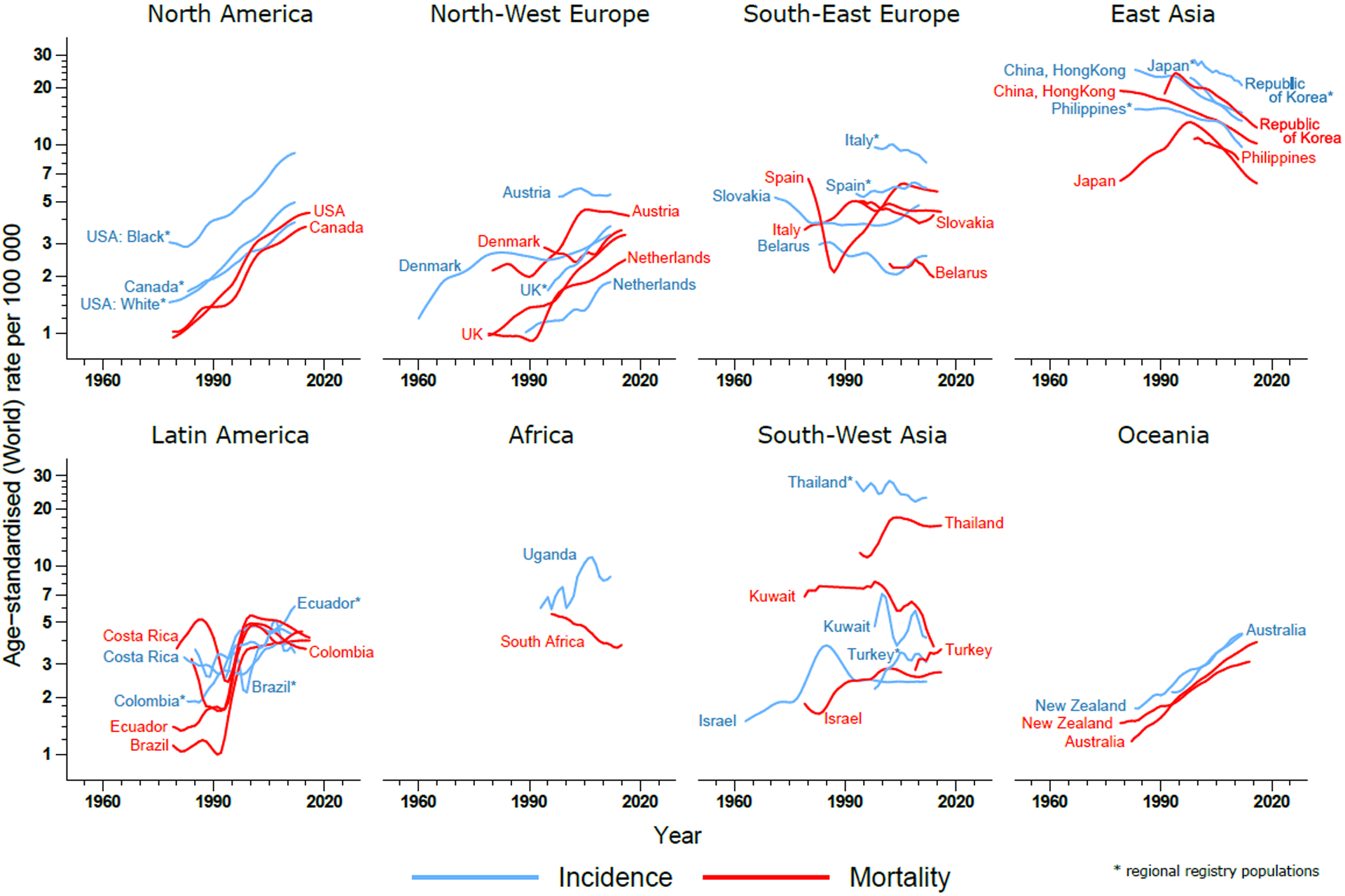
With about 572,000 new cases and 508,000 deaths in 2018, esophageal cancer is the 7th most common cause of cancer morbidity and the 6th most common cause of cancer-related death worldwide. Both incidence and mortality vary greatly across countries and world regions (Figure 3), and rates are 2–3 fold higher in men relative to women. Esophageal cancer is most common in Eastern Asia (ASR 12.2 per 100,000 person-years) and Eastern Africa (8.3), followed by Southern Africa (7.4); incidence rates are below 2 per 100,000 in the remaining regions of Africa as well as in Central America (Annex Table 1, Annex Figure 1). The vast majority of cases occur in Asia, with an estimated 307,000 cases (54% of the global burden) in China alone (Figure 2). Patterns of mortality closely follow those of incidence, reflecting the poor average prognosis associated with these tumors. Globally, the highest mortality rates were in the Eastern Asian and Eastern African regions, where mortality from esophageal cancer ranks among the top five causes of cancer-related death. Even larger variations in incidence rates between and within world regions are evident when examining the cancer registry data worldwide (Annex Figure 2), with the highest incidence rates of 129 per 100,000 observed in Cixian, China, and a greater than 100-fold difference in rates across registries. However, patterns have changed substantially over time and decreasing incidence trends in most Asian populations can be observed that contrast with the increasing rates seen in historically low-risk countries including the United Kingdom, the Netherlands and United States Whites (Figure 4A). These trends are most evident in males; incidence rates in females have remained at a much lower level and have changed little over time.
Figure 3.
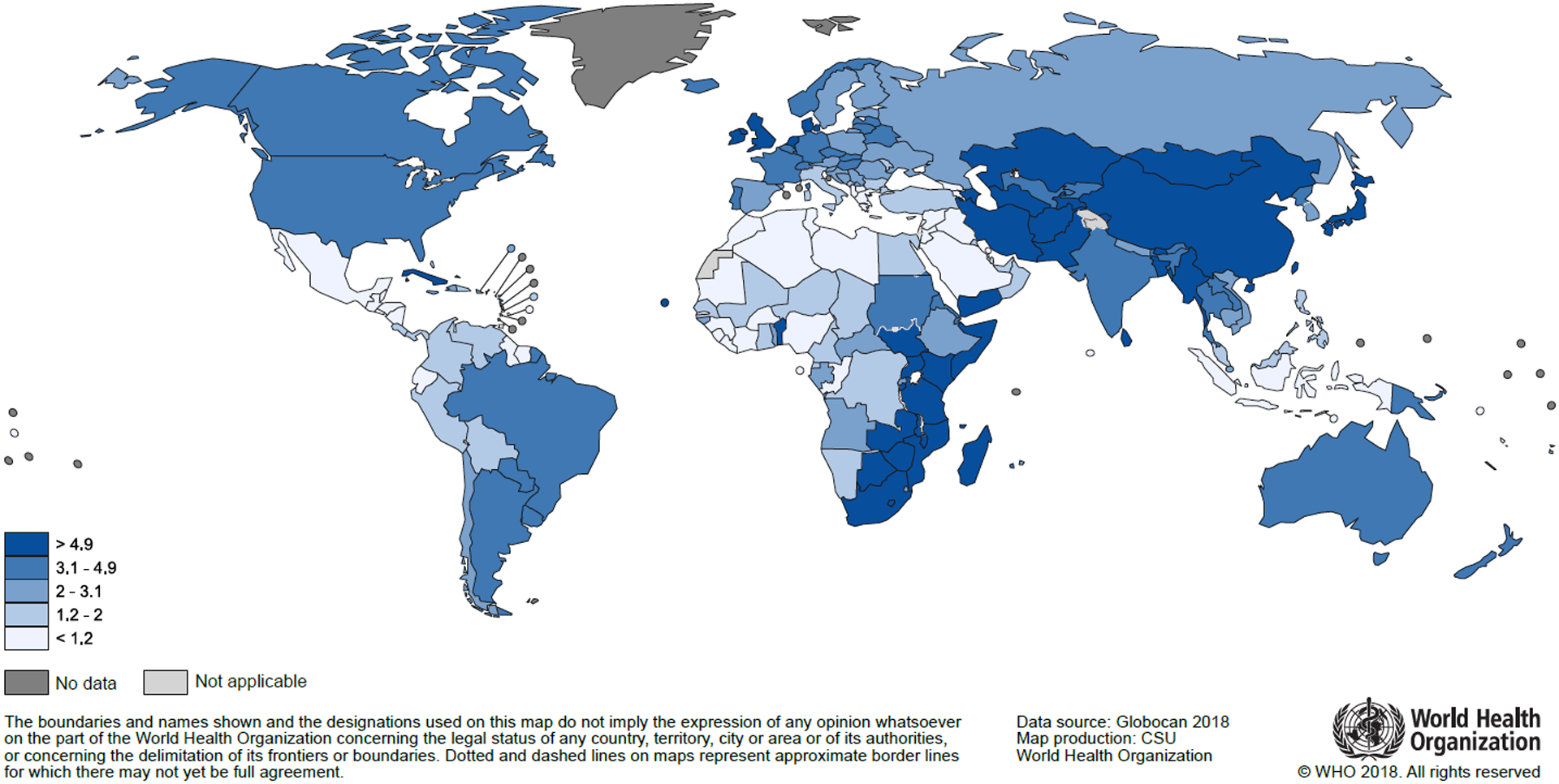
Esophageal cancer: Estimated age-standardized incidence rates per 100,000 person-years in 2018. Source: GLOBOCAN 2018
Figure 4.
Esophageal cancer: Trends in age-standardized incidence and mortality rates by country. Source: CI5plus and WHO Mortality Database.
The geographical differences and trends over time are striking and can partly be explained by varying distributions of the two main histological subtypes of esophageal cancer, adenocarcinoma (AC) and squamous cell carcinoma (SCC), which represent about 90–95% of all esophageal cancers.18 The latter histological subtype is linked to tobacco smoking and heavy alcohol consumption, but also opium intake, air pollution and diet. SCC is the most common form of esophageal cancer globally, particularly in high-risk regions, where it represents more than 90% of all esophageal cancer cases.18–20 Other contributors to the high incidence observed in some countries, including the so-called central Asian esophageal cancer belt21 and Eastern Africa’s esophageal cancer corridor22, remain to be elucidated. AC has been associated with obesity and gastroesophageal reflux disease (GERD) and today represents up to two-thirds of esophageal cancer in a relatively small number of high-income countries including the United Kingdom and the United States.18,23,24 While SCC incidence rates are declining in most countries, rates of esophageal AC appear to be rising in an expanding number of countries. These trends are likely attributable to shifts in the prevalence of key risk factors, including increases in the prevalence of obesity paralleled by decreasing levels of both smoking and chronic infection with Helicobacter pylori (H. pylori), which has been inversely related with esophageal AC incidence.25 These trends are predicted to continue in the near future, with AC surpassing SCC in many mainly high-income countries and obesity becoming an increasingly important contributor to the future burden of esophageal cancer.25
With no specific symptoms of early esophageal cancers, most tumors are diagnosed at a late and rapidly progressing to an advanced stage when treatment options are limited and cure is not possible. In high-income settings, only about a quarter of all patients diagnosed with esophageal cancer are still alive five after diagnosis.11 Efforts to screen for esophageal cancer in high-incidence areas of China using endoscopy showed some evidence of a significant reduction in mortality26 and survival has been increasing in China over the past decades.27 Yet, to-date, population-based endoscopic screening has not been recommended given the associated relatively high cost and risk of complication, and non-endoscopic cell-sampling methods have been found to lack the necessary specificity.28 Clinical trials of other, less invasive screening methods, (e.g. inflatable balloons and sponges) are currently underway, and may be a more favorable approach to screen for esophageal cancer in the future, given improvements in specificity and risk stratification.28,29. For now, primary prevention measures, including obesity control in high-income settings and continuing interventions that seek to reduce the smoking and alcohol prevalence in the community, remain key to reducing the incidence of disease.
2. Gastric cancer
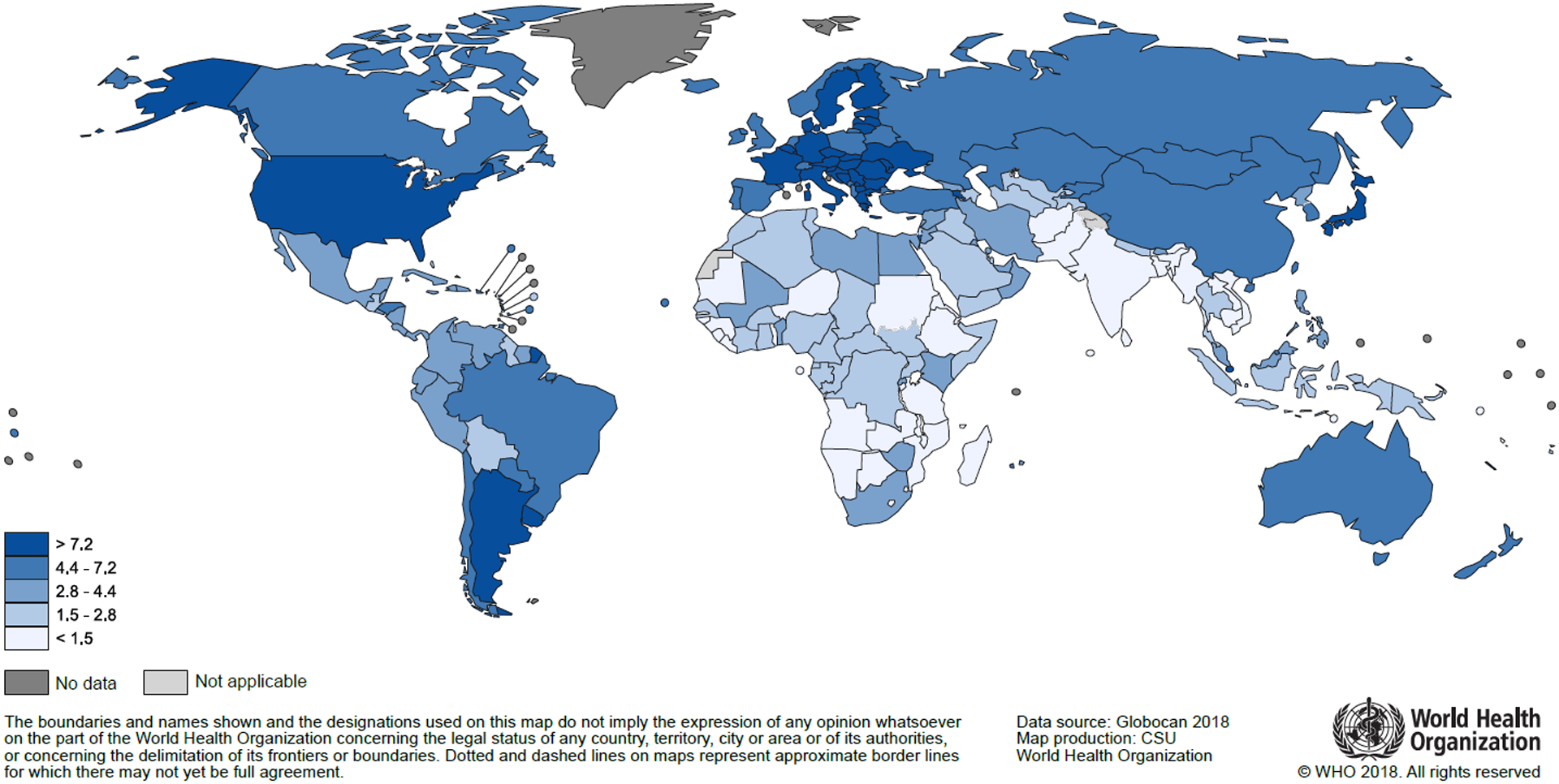
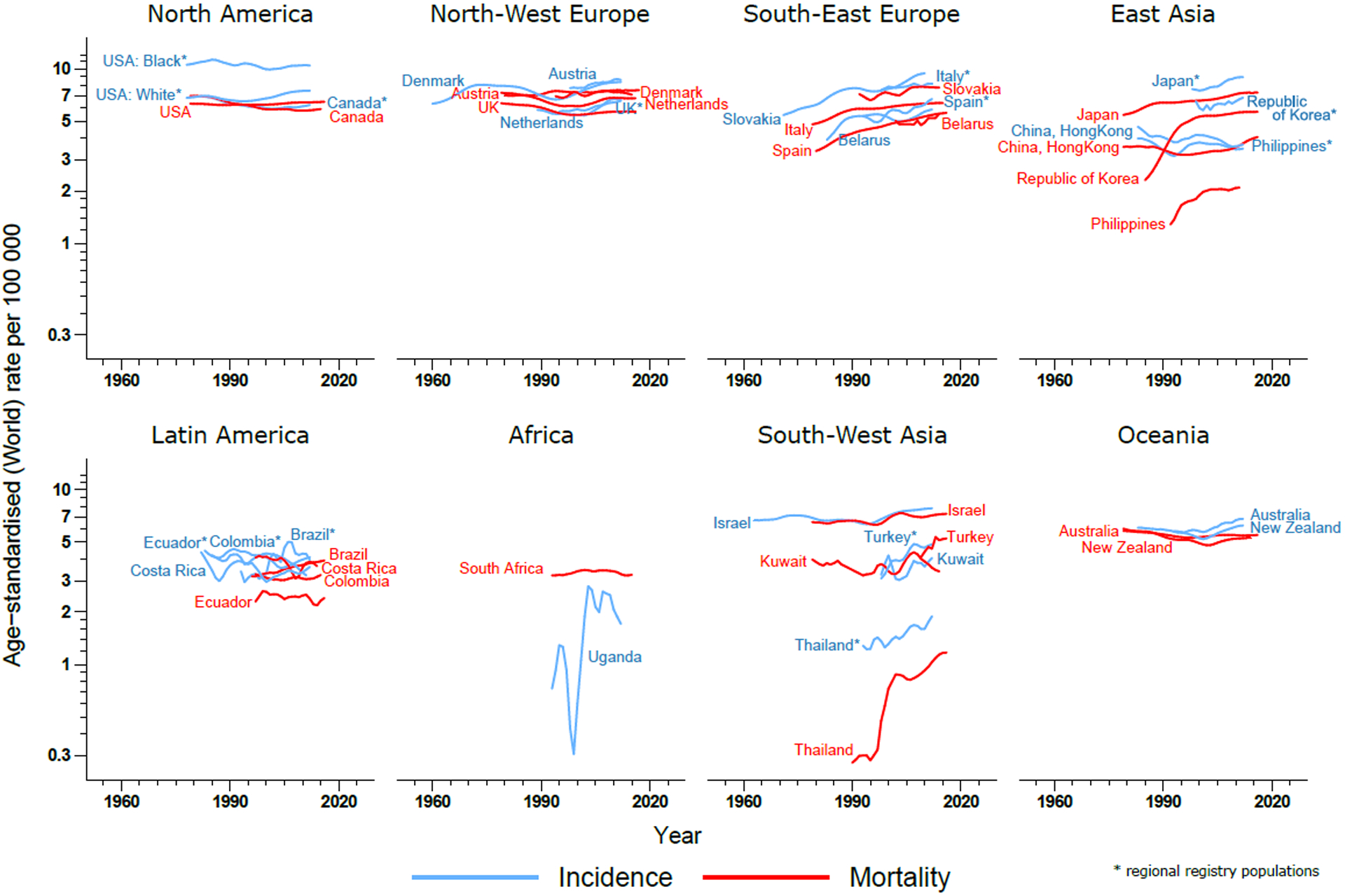
Even though uniform declines in incidence have been observed in many parts of the world for decades, gastric cancer remains an important cause of cancer-related incidence and mortality, with over one million new cases and close to 800,000 deaths in 2018. It is the fifth most frequently diagnosed cancer and the third-leading cause of cancer death. Incidence rates are generally two-fold higher in men relative to women and range from 22 per 100,000 person-years in Eastern Asia to less than 5 per 100,000 in in Africa, as well as Northern America and Northern Europe (Annex Table 2, Annex Figure 3). Countries with the highest incidence rates of gastric cancer include the Republic of Korea, Mongolia and Japan, while variations in recorded incidence rates remains high globally, most markedly in Asia (Figure 5, Annex Figure 4). As gastric cancer is rarely detected early, mortality from this cancer is often high. Geographic and temporal variations in mortality are therefore often closely aligned with those of incidence, yet with a proportionally lower share of deaths from the disease occurring in very high HDI countries compared to medium and low HDI countries, where gastric cancer often ranks among the top causes of cancer-related death. Since the beginning of cancer registration several decades ago, steady declines in the incidence and mortality from gastric cancer have been observed consistently across world regions in both men and women (Figure 6).
Figure 5.
Gastric cancer: Estimated age-standardized incidence rates per 100,000 person-years in 2018. Source: GLOBOCAN 2018
Figure 6.
Gastric cancer: Trends in age-standardized incidence and mortality rates by country. Source: CI5plus and WHO Mortality Database.
The observed declines in the incidence and mortality from gastric cancer were once termed “an unplanned triumph” of cancer prevention, as this took place in the absence of active primary prevention programs and, outside of Japan and Korea, population-based screening.30 Part of these decreases has been attributed to better food preservation practices, linked to refrigeration during the transportation and storage of food. At the same time, economic development has led to improved living conditions, including reduced overcrowding and better hygiene, leading to a reduced prevalence of H. pylori, an established cause of gastric cancer.31 Other risk factors include tobacco smoking, low consumption of fruits and vegetables, as well as high intake of salt-preserved foods and possibly alcohol.6,32,33 Although often reported as a single entity, gastric cancers can be broadly classified into two major topographical subsites, the cardia (CGC) and non-cardia (NCGC). CGC arises in the area of the stomach adjoining the esophageal-gastric junction, while NCGC develops from more distal regions of the stomach, and the two entities differ in terms of etiology, risk factors and geographical patterns. While CGC is associated with obesity and GERD in Western populations (resembling etiological factors attributed to esophageal AC), the vast majority of NCGC cases are associated with H. pylori infection.34–36 The contributions of NCGC and CGC to the overall burden from gastric cancer varies greatly across countries; most are NCGC in global terms, but this is particularly the case in low HDI settings. The proportion of CGCs tends to be highest in high HDI regions and small in most high-risk populations such as China or Japan, although exceptions include a high proportion of CGC in the high-incidence regions of Iran.37–39 Risks for each subsite also differ across ethnic groups, with, for example, CGC more common in non-Hispanic Whites in the United States than in other ethnic groups.40 Opposing the overall decreases in gastric cancer incidence and mortality rates, are the recent increases in the incidence of both CGC and cancer of the gastric corpus (a non-cardia subsite), as seen among younger generations, e.g. those aged 25–39 years in the United States.41,42 Such trends may lead to a deceleration or a reversal of the overall declining gastric cancer rates.
A recent global study indicated that mortality rates have decreased more rapidly than incidence, ascribed to socioeconomic development and better access to diagnostic and treatment facilities.43 As early-stage gastric cancer rarely causes symptoms, early detection continues to pose many challenges and five-year survival ranges between 20–40% in most countries.10,11 Japan and the Republic of Korea, two high-risk countries, have implemented national screening programs using endoscopic and/or radiographic methods (biennial gastro-fibre scope (endoscopy) for adults aged 50 and over in addition to the existing upper GI series (barium meal followed by radiography). These efforts have led to an increasing number of cases diagnosed at an early, curable stage and relatively high survival proportions of over 60% in both countries.44,45 As the introduction of screening also led to an increase in incidence, it remains to be determined as to how much of these survival increases are attributable to lead time and detection bias. Although routine screening in low-risk populations has not proven to be cost-effective, the implementation of population-based screening in high-risk regions has shown some promise, although whether this will translate into a true mortality reduction is yet to be confirmed.46,47 In parallel, the cost-effectiveness of H. pylori eradication is being explored in several ongoing randomized controlled trials indicating that treatment lowers gastric cancer risk48 and may aid in gastric cancer prevention in some settings.49
3. Colorectal cancer
In 2018, colorectal cancer remains the most commonly diagnosed GI cancer, representing 1.8 million cases and 881 000 deaths globally, and constituting one in ten cancer cases and deaths. Incidence rates vary by up to 10-fold across world regions, with Australia/New Zealand having the highest and South-Central Asia the lowest rates (Annex Table 3, Annex Figure 5). At a country level, elevated incidence is found in a diverse set of countries, with rates in Hungary, the Republic of Korea, Slovakia and Norway above 40 per 100,000 (Figure 7). Incidence rates are about 3-fold higher in high and very high HDI when compared with low and medium HDI countries. Recorded incidence rates from cancer registries reveal high risks in two Canadian populations (Northwest Territories, Newfoundland and Labrador) and substantial variation in rates within world regions (Annex Figure 6). Variations in colorectal cancer mortality rates tend to be less pronounced due to the higher case fatality in lower HDI settings. Colorectal cancer incidence rates are still rising rapidly in many less-developed countries, particularly in Eastern Europe, Asia and South America, while trends are stabilizing or decreasing in highly developed countries, such as Canada and in Northern Europe, where rates remain among the highest in the world. (Figure 8)
Figure 7.
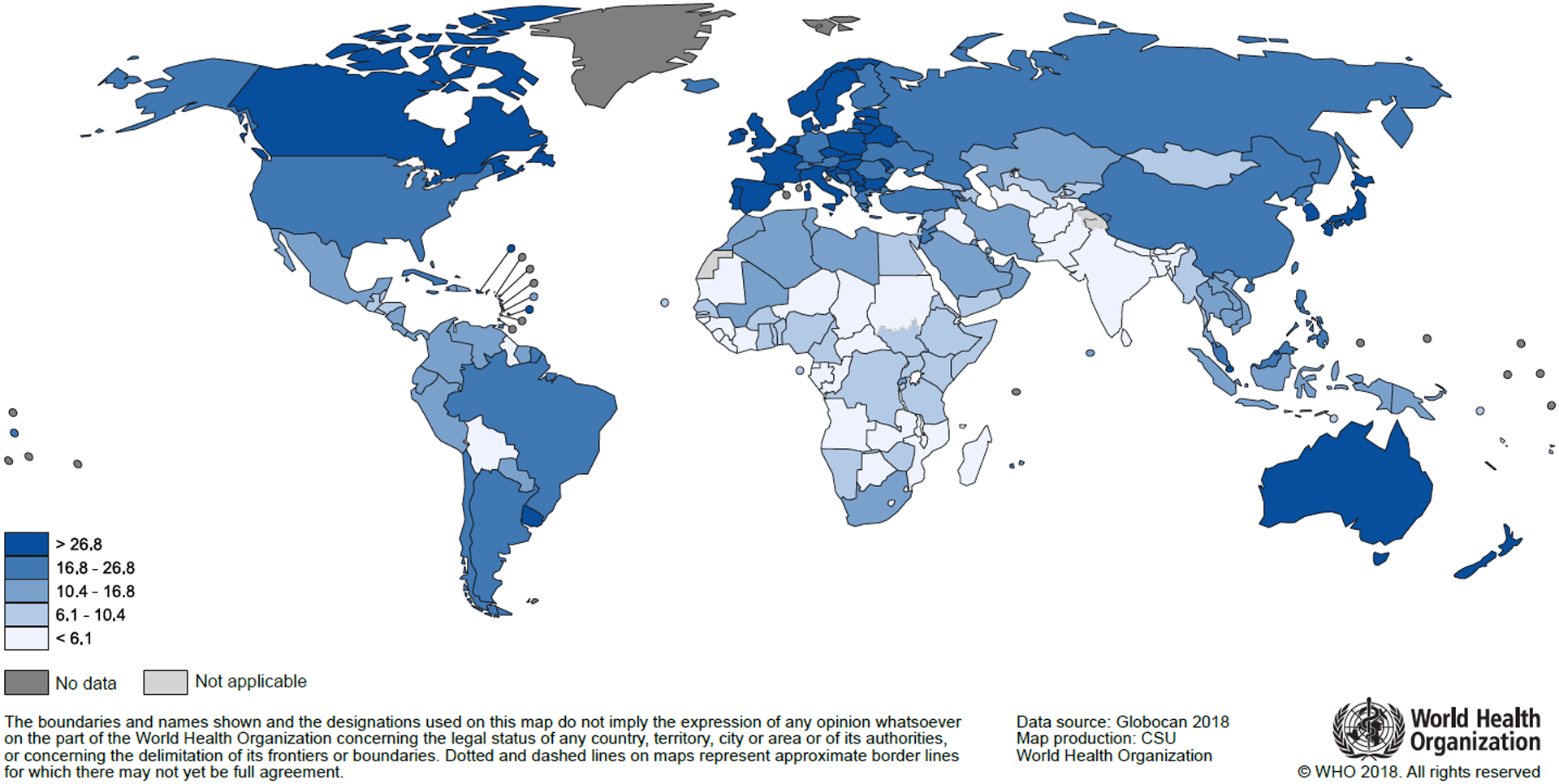
Colorectal cancer: Estimated age-standardized incidence rates per 100,000 person-years in 2018. Source: GLOBOCAN 2018
Figure 8.
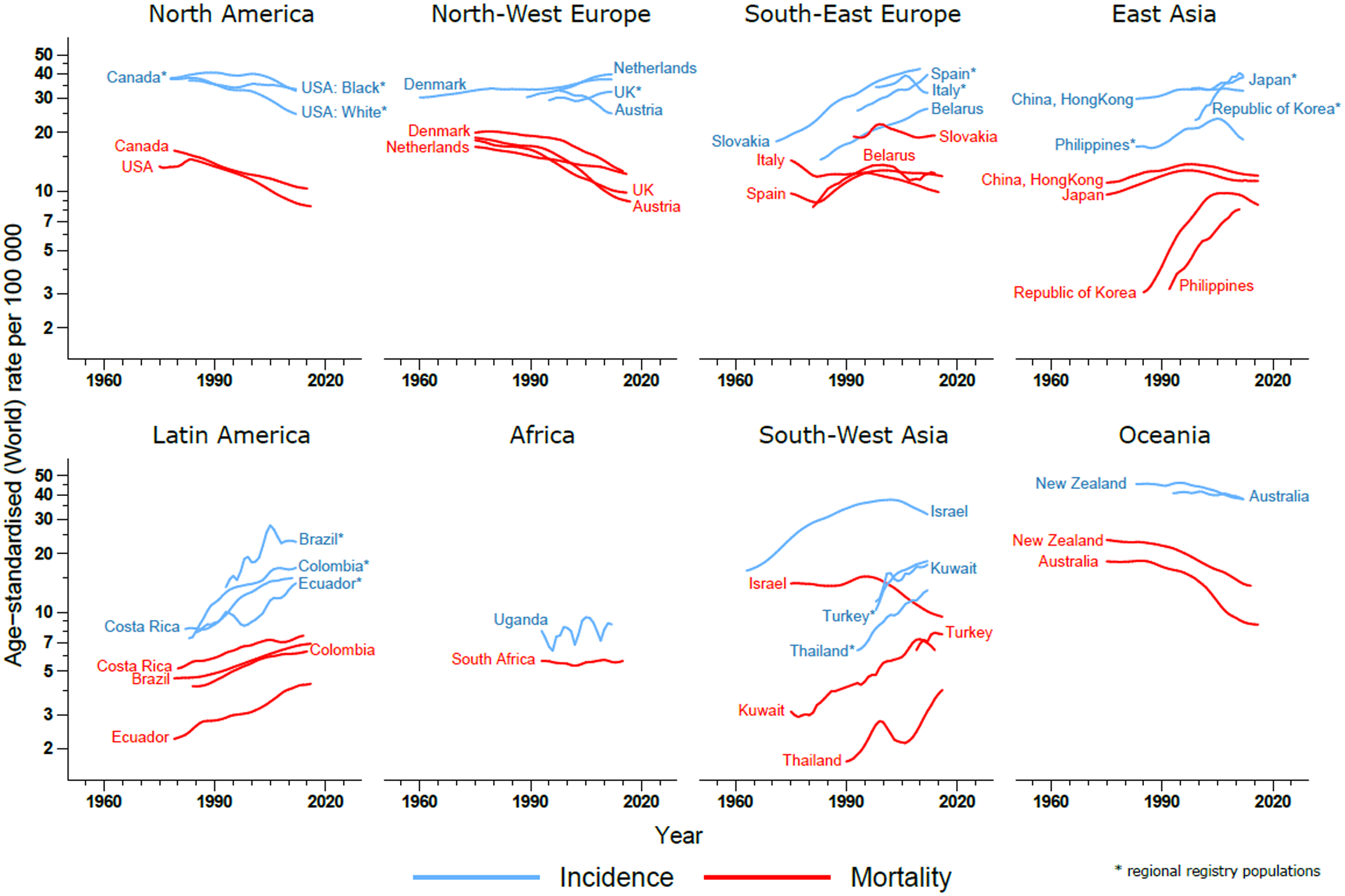
Colorectal cancer: Trends in age-standardized incidence and mortality rates by country. Source: CI5plus and WHO Mortality Database.
Colorectal cancer is one of the clearest markers of the cancer transition, with infection-related cancers being gradually displaced with those linked to rapid societal and economic change.50 Colorectal cancers can be broadly subdivided into colon, rectal and anal cancers; while colon and rectal cancer share a number of risk factors, a large proportion of anal cancers have been attributed to infection with human papilloma virus (HPV), most notably HPV-16.51 That combined incidence rates are steadily increasing in formerly low incidence regions can primarily be attributed to changes in lifestyle and diet, shifts towards an increased intake of fat, sugar and animal-source foods, paralleled by increases in sedentary behavior and obesity. Established risk factors for colorectal cancer include alcohol consumption52, high consumption of red and processed meat53,54, obesity55 and physical inactivity4. Additional risk factors include and smoking56. In contrast, diets rich in wholegrains, dairy products and foods containing dietary fiber have been found to protect from colorectal cancer.4 A recent global study concluded that the three most important contributors to age-standardized disability-adjusted life years (DALYs) of colorectal cancer globally were diets low in calcium (20.5%) and alcohol use (15.2%).57 Decreasing or stabilizing incidence rates in some high HDI and high-risk countries have been mainly attributed to population-level changes towards healthier lifestyle choices, coupled with the introduction and implementation of population-based screening. Precursor lesions of colorectal cancer can be detected and removed during screening, typically carried out using either stool-based tests (e.g. guaiac-based fecal occult blood test (gFOBT) or fecal immunochemical test (FIT)) and/or endoscopic methods such as sigmoidoscopy and colonoscopy, all of which have been associated with reductions in colorectal cancer mortality.58 The introduction of population-based screening in a growing number of countries over recent years and decades may thus have contributed to decreasing incidence and mortality rates in some regions.59 Yet, despite overall decreasing trends in some high-income countries, recent increases in incidence rates have been observed in younger generations, specifically in adults younger than 50 years.60–62 While these trends point towards changes in early-life exposures, further etiologic research is needed to elucidate the causal factors driving these trends.
While the prospects of cure from colorectal cancer are generally good, marked survival differences have long existed, even across high-income countries.10 These disparities can partly be explained by stage at diagnosis, an important determinant for prognosis affected by early detection and screening programs as well as diagnostic pathways and clinical procedures. Yet, as the implementation of screening programs is yet to be fully implemented in most countries59, the impact of colorectal cancer screening on stage distributions and mortality trends is likely to be limited to a handful of countries where activities started more than a decade ago. Treatment is also an important determinant of survival and considerable advances have been made, including improved surgical techniques, radiotherapy, chemotherapy, targeted therapy and palliative care. The adoption of best practices in treatment and management have led to declining mortality rates in most parts of the world. Colorectal cancer remains more common in older people and due to ongoing population aging and growth alone, the number of older adults with cancer is predicted to double in all world regions by 2035, with colorectal cancer representing one of the main contributors.63
4. Liver cancer
Liver cancer was the sixth most commonly diagnosed cancer (841,000 cases) and the fourth leading cause of cancer death (782,000 deaths) globally. Similar to other GI cancers, both incidence and mortality rates are up to 2–3 fold higher in men compared to women. The overall burden from liver cancer is most pronounced in transitioning countries; rates are highest in Eastern Asia (17.7), Micronesia (15.2), and Northern Africa (14.1), with Mongolia the country with by far the highest incidence and mortality rates worldwide (93.7 and 75.4, respectively) (Figure 9, Annex Table 4, Annex Figure 7). Recorded data from individual cancer registries emphasize the variation in incidence rates between and within world regions, particularly in Asia (Annex Figure 8). Due to the poor prognosis associated with liver cancer, incidence and mortality patterns are typically closely aligned and show similar patterns across world regions. Yet country-level trends in incidence and mortality are quite heterogeneous; while rising incidence rates have been observed in many parts of the world over recent decades, including the United States, Australia and most parts of Europe, decreasing rates have been observed in some Asian countries such as the Republic of Korea, Japan and China (Figure 10).
Figure 9.
Liver cancer: Estimated age-standardized incidence rates per 100,000 person-years in 2018. Source: GLOBOCAN 2018
Figure 10.
Liver cancer: Trends in age-standardized incidence and mortality rates by country. Source: CI5plus and WHO Mortality Database.
Different sets of risk factors are likely responsible for these patterns and trends. Primary liver cancer, which can be broadly subdivided into hepatocellular carcinoma (HCC) (typically representing 75–85% of all liver cancer cases) and intrahepatic cholangiocarcinoma (ICC) (representing about 10–15% of cases), and other, more rare types. While ICC has been linked with primary sclerosing cholangitis, fibropolycystic liver disease, parasitic infection and intrahepatic biliary stones64, HCC has been mainly associated with chronic infection with hepatitis B or C virus (HBV or HCV) as well as exposure to aflatoxin, excess alcohol consumption, obesity, type 2 diabetes and smoking.
In high-risk areas such as Eastern Asia, infection with HBV and aflatoxin are considered the main underlying risk factors for HCC, whereas HCV is the predominant cause in Japan and Egypt. Decreases in the prevalence of both infections and in exposure to aflatoxin have likely contributed to declines seen in the incidence of liver cancer in these regions.65 Increasing incidence trends in low-risk areas have been postulated to be related to the rising prevalence of obesity and metabolic disorders like diabetes, offsetting the gains made through reductions in the prevalence of HBV and HCV.66,67 Thus, while obesity is becoming more prevalent and its importance on the burden of liver cancer is growing, HBV vaccination remains key for primary prevention of HCC globally, as HBV is responsible for more cases than any other factor. Where mass vaccination has been introduced during the early-1980s, as in Taiwan, there has been a marked reduction in the prevalence of HBV infection as well as HCC incidence in childhood68 and early adulthood69. While HCC trends largely reflect those of primary liver cancer, a notable exception is Thailand, where ICC is the dominant type of liver cancer70 and rates of HCC have been in decline71. Liver fluke infections are a major risk factor for ICC, particularly in the Northeast of the country where Opisthorchis viverrini is endemic.72
Early detection of liver cancer remains challenging as the disease is commonly diagnosed at an advanced stage. In high-income settings, screening can be carried out for patients at high risk of developing liver cancer (e.g. with long-standing cirrhosis), using alpha-fetoprotein (AFP) blood tests and ultrasound exams every 6 months. Prognosis remains poor with the maximum 5-year survival estimated at 18% in high-income countries.10
5. Pancreatic cancer
Pancreatic cancer is only the 12th most common cancer, but is the 7th most common cause of cancer death. In 2018 the number of deaths from pancreatic cancer was almost the same as the number of cases (432,000 and 459,000 respectively). Incidence and mortality rates are about 3–4 fold higher in high compared with low and medium HDI countries and are slightly higher in men than in women. Incidence and mortality rates are highest in Europe, North America and Australia/New Zealand and differ only marginally in their magnitude due to the poor prognosis of the disease (Annex Table 5, Annex Figure 9). Hungary and Uruguay are the countries with the globally highest incidence and mortality rates, while marked differences in incidence have been recorded across populations living in the same world region (Figure 11, Annex Figure 10). Historically, both incidence and mortality rates have been either stable or slightly increasing in most recent decades (Figure 12).
Figure 11.
Pancreatic cancer: Estimated age-standardized incidence rates per 100,000 person-years in 2018. Source: GLOBOCAN 2018
Figure 12.
Pancreatic cancer: Trends in age-standardized incidence and mortality rates by country. Source: CI5plus and WHO Mortality Database.
To-date, risk factors of pancreatic cancer remain poorly understood, although evidence suggests that smoking, diabetes, body fatness, and some dietary factors including the consumption of red and processed meat as well as excessive alcohol intake are likely all associated with an increased disease risk.5 According to recent estimates, about 21% of all deaths from pancreatic cancer are due to smoking, followed by high fasting plasma glucose levels (9%) and excess body fatness (6%).73 Variations in the prevalence of these underlying factors might therefore explain parts of the geographic differences in the burden of the disease. Trends in incidence could furthermore be affected by differences in (access to) diagnostic practices. With patients rarely exhibiting specific symptoms, the diagnosis of pancreatic cancer is reliant on imaging, even though this can be challenging for early-stage tumors.74 Increasing incidence rates in some countries could therefore also reflect improvements in the registration of pancreatic cancer.
Even in the highest income countries worldwide most pancreatic cancer patients are diagnosed with metastatic or locally advanced disease precluding curative surgery, and only about 10% are still alive five years after diagnosis.11 Prognosis improves in cases detected at an operable stage with 5-year survival rates after surgical resection ranging up to 25%.75 Yet, in the absence of sensitive and specific tumor markers that would allow detecting the disease early, screening for pancreatic cancer remains extremely challenging. Current screening activities (in high-income settings) are limited to people with family histories and to those with inherited mutations known to increase the risk of developing the disease, often carried out using MRI or endoscopic ultrasound.74 Despite rather constant incidence and mortality rates in many high-risk countries, the number of new cases will continue to rise in the future, largely due to population ageing and growth. Due to this development, coupled with ongoing advances and improvements in the prognosis of other cancer sites, pancreatic cancer has become or is set out to become one of the leading causes of cancer-related death in many countries.73 As an example, in the European Union (EU), it has been predicted that deaths from pancreatic cancer surpassed those of breast cancer in 2017, with the disease becoming the third most important cause of cancer death in the EU, after lung and colorectal cancer.76
Summary and Conclusion
Cancers of the gastrointestinal tract are important contributors to the global cancer burden today, with substantial increases in the numbers of new cases and deaths expected in the future for each of the five major sites in almost every world region. While there have been some positive developments in their control, such as the marked overall declines gastric cancer rates, a number of challenges lie ahead in the fight against GI cancers.
Firstly, the burden of colorectal cancer continues to shift towards transitioning countries, which are less equipped to manage this increasing burden. Additionally, although all-ages rates of colorectal cancer have largely stabilized or been in decline in high-income countries, incidence rates appear to be rising in adults younger than 50 years. Recent analyses of US data have shown that incidence rates of subtypes of all five GI cancers (esophageal adenocarcinoma, gastric cardia, colorectum, liver and pancreas) have increased significantly in young adults aged 25–49 years over the 1995–2014 period, increasing in recent generations.77
Secondly, some cancer subtypes have differing trends and geographic patterns that match their differing etiology and causal pathways, as is the case for esophageal, gastric and liver cancer; it is thus no longer appropriate to examine cancer sites as single entities. Rising rates of esophageal AC in many high-income countries, the most common subtype of esophageal cancer in most of these countries, contrast with declines in the incidence of esophageal SCC. Similarly, HCC of the liver is increasing in many high-income, decreasing among most low-risk countries, while rates of ICC appear to be on the rise in a number of countries, irrespective of income. Many of these temporal developments are linked to changes in the prevalence of underlying risk factors, including rising obesity rates, unhealthy diets and other potentially modifiable risk factors that vary between countries and across populations.
Third, with the exception of colorectal cancer, GI cancers continue to contribute 1.4–1.8 times as much to global cancer deaths as they do to cancer cases. This is related to the fact that most esophageal, gastric, liver and pancreatic cancers remain extremely difficult to detect early and curative treatment options are either very limited or unavailable at the time of diagnosis. Yet, the implementation of early detection and screening programs for gastric cancer in high-risk regions such as Japan and Korea, and for esophageal cancer in China have shown promising results.26,46,47 Pancreatic cancer on the other hand is becoming a more important contributor to cancer-related mortality as a consequence of improved diagnosis and management of the historically most common forms of cancer death.
Forth, while there are advances in treatment and early detection, primary prevention remains the key strategy to reduce the global burden from GI cancers in the foreseeable future. While all GI cancer have distinct risk factors, many of the causes – tobacco, alcohol, obesity, sedentary lifestyles and metabolic abnormalities – are amenable to prevention. Healthy lifestyle choices, including physical activity as well as a healthy body weight and diet have been shown to represent key factors driving the past and future burden from GI cancers.8,78,79
Finally, the availability and quality of the data present an important challenge. Currently, only 15% of the world population is covered by functioning and high-quality population-based cancer registries (PBCR), representing the cornerstone of cancer control planning.15,80 While estimates of incidence and mortality are available for most countries, these are in many instances based on proxy indicators or very sparse data that can in no way substitute real (recorded) data. Where data series from PBCRs exist, there remains a need to further increase the specificity of morphological diagnoses of GI cancers given the heterogeneity in the epidemiologic patterns between subtypes. For this reason, we were not able to present analyses of subtype-specific rates in this overview. More broadly, increasing the capacity and supporting the development of cancer registries worldwide remains essential as these underlie the development of adequate cancer prevention and control plans, including screening strategies, disease management and resource allocation.
In conclusion, GI cancers pose a major challenge to public health. Primary and secondary prevention measures remain the most important tools to control this group of malignancies, particularly in light of their preventability and often dreadful prognosis. This comprises tobacco and alcohol control (for esophageal SCC) and obesity control (for esophageal AC and gastric cardia cancers), but also hepatitis B immunization (for liver cancer) and screening for colorectal cancer via FOBT followed by timely treatment – all forming part of the WHO Global Action Plan 2013–2020.81
Supplementary Material
Acknowledgements
The authors gratefully acknowledge all cancer registries and their staff who have contributed in sharing their data needed for this study.
Where authors are identified as personnel of the International Agency for Research on Cancer / World Health Organization, the authors alone are responsible for the views expressed in this article and they do not necessarily represent the decisions, policy or views of the International Agency for Research on Cancer / World Health Organization.
Footnotes
Conflict of interest: All authors declare no conflicts of interest.
References
- 1.Ferlay J, Ervik M, Lam F, et al. Global Cancer Observatory: Cancer Today. Lyon, France: International Agency for Research on Cancer. Available from: https://gco.iarc.fr/today; 2018. [Google Scholar]
- 2.Islami F, Goding Sauer A, Miller KD, et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. CA Cancer J Clin 2018; 68(1): 31–54. [DOI] [PubMed] [Google Scholar]
- 3.Diet, Nutrition, Physical activity, and Liver Cancer. Continuous Update Project Report: World Cancer Research Fund / American Institute for Cancer Research, 2015.
- 4.Diet, Nutrition, Physical activity, and Colorectal Cancer. Continuous Update Project Expert Report 2018.: World Cancer Research Fund / American Institute for Cancer Research, 2018.
- 5.Food, Nutrition, Physical activity, and the Prevention of Pancreatic Cancer. Continuous Update Project Report: World Cancer Research Fund / American Institute for Cancer Research, 2012.
- 6.Diet, Nutrition, Physical activity, and Stomach Cancer. Continuous Update Project Report: World Cancer Research Fund / American Institute for Cancer Research, 2016.
- 7.Diet, Nutrition, Physical activity, and Oesophageal Cancer. Continuous Update Project Report: World Cancer Research Fund / American Institute for Cancer Research, 2016.
- 8.Song M, Giovannucci E. Preventable Incidence and Mortality of Carcinoma Associated With Lifestyle Factors Among White Adults in the United States. JAMA Oncol 2016; 2(9): 1154–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arnold M, Pandeya N, Byrnes G, et al. Global burden of cancer attributable to high body-mass index in 2012: a population-based study. Lancet Oncol 2015; 16(1): 36–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Allemani C, Matsuda T, Di Carlo V, et al. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet 2018; 391(10125): 1023–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arnold M, Rutherford MJ, Bardot A, et al. Progress in cancer survival, mortality, and incidence in seven high- income countries 1995–2014 (ICBP SURVMARK-2): a population-based study. Lancet Oncol 2019; 11(19): 30456–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ferlay J, Ervik M, Lam F, et al. Global Cancer Observatory: Cancer Tomorrow. Lyon, France: International Agency for Research on Cancer. Available from: https://gco.iarc.fr/tomorrow; 2018. [Google Scholar]
- 13.Human Development Report 2019. Beyond income, beyond averages, beyond today: Inequalities in human development in the 21st century. New York: United Nations Development Programme (UNDP), 2019. [Google Scholar]
- 14.Ferlay J, Colombet M, Bray F. Cancer Incidence in Five Continents, CI5plus: IARC CancerBase No. 9. Lyon, France: International Agency for Research on Cancer; 2018. [Google Scholar]
- 15.Bray F, Colombet M, Mery L, et al. Cancer Incidence in Five Continents, Vol. XI (electronic version). Lyon: International Agency for Research on Cancer.; 2017. [Google Scholar]
- 16.Segi M Cancer mortality for selected sites in 24 countries (1950–57). Sendai, Japan: Department of Public Health, Tohoku University of Medicine; 1960. [Google Scholar]
- 17.Day NE. A New Measure of Age Standardized Incidence, the Cumulative Rate. In: Waterhouse J, Muir CS, Correa P, Powell C, eds. Cancer incidence in Five Continents, Vol III (IARC Scientific Publications No 15). Lyon: International Agency for Research on Cancer; 1976: 443–52. [Google Scholar]
- 18.Arnold M, Soerjomataram I, Ferlay J, Forman D. Global incidence of oesophageal cancer by histological subtype in 2012. Gut 2015; 64(3): 381–7. [DOI] [PubMed] [Google Scholar]
- 19.Abnet CC, Arnold M, Wei WQ. Epidemiology of Esophageal Squamous Cell Carcinoma. Gastroenterology 2018; 154(2): 360–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sheikh M, Poustchi H, Pourshams A, et al. Individual and Combined Effects of Environmental Risk Factors for Esophageal Cancer Based on Results From the Golestan Cohort Study. Gastroenterology 2019; 156(5): 1416–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Semnani SH, Besharat S, Abdolahi N, et al. Esophageal cancer in northeastern Iran. Indian J Gastroenterol 2005; 24(5): 224. [PubMed] [Google Scholar]
- 22.Loon KV, Mwachiro MM, Abnet CC, et al. The African Esophageal Cancer Consortium: A Call to Action. Journal of Global Oncology 2018; (4): 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McColl KEL. What is causing the rising incidence of esophageal adenocarcinoma in the West and will it also happen in the East? J Gastroenterol 2019; 54(8): 669–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thrift AP. The epidemic of oesophageal carcinoma: Where are we now? Cancer Epidemiol 2016; 41: 88–95. [DOI] [PubMed] [Google Scholar]
- 25.Arnold M, Laversanne M, Brown LM, Devesa SS, Bray F. Predicting the Future Burden of Esophageal Cancer by Histological Subtype: International Trends in Incidence up to 2030. Am J Gastroenterol 2017; 112(8): 1247–55. [DOI] [PubMed] [Google Scholar]
- 26.Wei WQ, Chen ZF, He YT, et al. Long-Term Follow-Up of a Community Assignment, One-Time Endoscopic Screening Study of Esophageal Cancer in China. J Clin Oncol 2015; 33(17): 1951–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zeng H, Chen W, Zheng R, et al. Changing cancer survival in China during 2003–15: a pooled analysis of 17 population-based cancer registries. Lancet Glob Health 2018; 6(5): e555–e67. [DOI] [PubMed] [Google Scholar]
- 28.Lao-Sirieix P, Fitzgerald RC. Screening for oesophageal cancer. Nature Reviews Clinical Oncology 2012; 9: 278. [DOI] [PubMed] [Google Scholar]
- 29.Offman J, Muldrew B, O’Donovan M, et al. Barrett’s oESophagus trial 3 (BEST3): study protocol for a randomised controlled trial comparing the Cytosponge-TFF3 test with usual care to facilitate the diagnosis of oesophageal pre-cancer in primary care patients with chronic acid reflux. BMC Cancer 2018; 18(1): 784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Howson CP, Hiyama T, Wynder EL. The decline in gastric cancer: epidemiology of an unplanned triumph. Epidemiol Rev 1986; 8: 1–27. [DOI] [PubMed] [Google Scholar]
- 31.Hooi JKY, Lai WY, Ng WK, et al. Global Prevalence of Helicobacter pylori Infection: Systematic Review and Meta-Analysis. Gastroenterology 2017; 153(2): 420–9. [DOI] [PubMed] [Google Scholar]
- 32.Praud D, Rota M, Pelucchi C, et al. Cigarette smoking and gastric cancer in the Stomach Cancer Pooling (StoP) Project. Eur J Cancer Prev 2018; 27(2): 124–33. [DOI] [PubMed] [Google Scholar]
- 33.Rota M, Pelucchi C, Bertuccio P, et al. Alcohol consumption and gastric cancer risk-A pooled analysis within the StoP project consortium. Int J Cancer 2017; 141(10): 1950–62. [DOI] [PubMed] [Google Scholar]
- 34.De Martel C, Georges D, Bray F, Ferlay J, Clifford G. The global burden of cancer attributable to infections in 2018. Lancet Glob Health 2019; in press. [DOI] [PubMed] [Google Scholar]
- 35.Hoyo C, Cook MB, Kamangar F, et al. Body mass index in relation to oesophageal and oesophagogastric junction adenocarcinomas: a pooled analysis from the International BEACON Consortium. Int J Epidemiol 2012; 41(6): 1706–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kamangar F, Dawsey SM, Blaser MJ, et al. Opposing risks of gastric cardia and noncardia gastric adenocarcinomas associated with Helicobacter pylori seropositivity. J Natl Cancer Inst 2006; 98(20): 1445–52. [DOI] [PubMed] [Google Scholar]
- 37.Colquhoun A, Arnold M, Ferlay J, Goodman KJ, Forman D, Soerjomataram I. Global patterns of cardia and non-cardia gastric cancer incidence in 2012. Gut 2015; 64(12): 1881–8. [DOI] [PubMed] [Google Scholar]
- 38.Taghavi N, Nasrollahzadeh D, Merat S, et al. Epidemiology of upper gastrointestinal cancers in Iran: a sub site analysis of 761 cases. World J Gastroenterol 2007; 13(40): 5367–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Babaei M, Pourfarzi F, Yazdanbod A, et al. Gastric cancer in Ardabil, Iran--a review and update on cancer registry data. Asian Pac J Cancer Prev 2010; 11(3): 595–9. [PubMed] [Google Scholar]
- 40.Gupta S, Tao L, Murphy JD, et al. Race/Ethnicity-, Socioeconomic Status-, and Anatomic Subsite-Specific Risks for Gastric Cancer. Gastroenterology 2019; 156(1): 59–62 e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Anderson WF, Rabkin CS, Turner N, Fraumeni JF Jr., Rosenberg PS, Camargo MC. The Changing Face of Noncardia Gastric Cancer Incidence Among US Non-Hispanic Whites. J Natl Cancer Inst 2018; 110(6): 608–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Camargo MC, Anderson WF, King JB, et al. Divergent trends for gastric cancer incidence by anatomical subsite in US adults. Gut 2011; 60(12): 1644–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Collaborators GBDSC. The global, regional, and national burden of stomach cancer in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease study 2017. Lancet Gastroenterol Hepatol 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jung KW, Won YJ, Kong HJ, Lee ES. Cancer Statistics in Korea: Incidence, Mortality, Survival, and Prevalence in 2016. Cancer Res Treat 2019; 51(2): 417–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Matsuda T, Saika K. Cancer burden in Japan based on the latest cancer statistics: need for evidence-based cancer control programs. Annals of Cancer Epidemiology 2018; 2. [Google Scholar]
- 46.Hamashima C, Systematic Review G, Guideline Development Group for Gastric Cancer Screening G. Update version of the Japanese Guidelines for Gastric Cancer Screening. Jpn J Clin Oncol 2018; 48(7): 673–83. [DOI] [PubMed] [Google Scholar]
- 47.Jun JK, Choi KS, Lee HY, et al. Effectiveness of the Korean National Cancer Screening Program in Reducing Gastric Cancer Mortality. Gastroenterology 2017; 152(6): 1319–28 e7. [DOI] [PubMed] [Google Scholar]
- 48.Ford AC, Forman D, Hunt RH, Yuan Y, Moayyedi P. Helicobacter pylori eradication therapy to prevent gastric cancer in healthy asymptomatic infected individuals: systematic review and meta-analysis of randomised controlled trials. BMJ 2014; 348: g3174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Areia M, Carvalho R, Cadime AT, Rocha Goncalves F, Dinis-Ribeiro M. Screening for gastric cancer and surveillance of premalignant lesions: a systematic review of cost-effectiveness studies. Helicobacter 2013; 18(5): 325–37. [DOI] [PubMed] [Google Scholar]
- 50.Fidler MM, Bray F, Vaccarella S, Soerjomataram I. Assessing global transitions in human development and colorectal cancer incidence. Int J Cancer 2017; 140(12): 2709–15. [DOI] [PubMed] [Google Scholar]
- 51.de Martel C, Georges D, Bray F, Ferlay J, Clifford GM. Global burden of cancer attributable to infections in 2018: a worldwide incidence analysis. Lancet Glob Health 2019. [DOI] [PubMed] [Google Scholar]
- 52.Fedirko V, Tramacere I, Bagnardi V, et al. Alcohol drinking and colorectal cancer risk: an overall and dose-response meta-analysis of published studies. Ann Oncol 2011; 22(9): 1958–72. [DOI] [PubMed] [Google Scholar]
- 53.Bouvard V, Loomis D, Guyton KZ, et al. Carcinogenicity of consumption of red and processed meat. Lancet Oncol 2015. [DOI] [PubMed] [Google Scholar]
- 54.Norat T, Lukanova A, Ferrari P, Riboli E. Meat consumption and colorectal cancer risk: dose-response meta-analysis of epidemiological studies. Int J Cancer 2002; 98(2): 241–56. [DOI] [PubMed] [Google Scholar]
- 55.Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet 2008; 371(9612): 569–78. [DOI] [PubMed] [Google Scholar]
- 56.Botteri E, Iodice S, Bagnardi V, Raimondi S, Lowenfels AB, Maisonneuve P. Smoking and colorectal cancer: a meta-analysis. JAMA 2008; 300(23): 2765–78. [DOI] [PubMed] [Google Scholar]
- 57.Collaborators GBDCC. The global, regional, and national burden of colorectal cancer and its attributable risk factors in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol 2019; 4(12): 913–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lauby-Secretan B, Vilahur N, Bianchini F, Guha N, Straif K, International Agency for Research on Cancer Handbook Working G. The IARC Perspective on Colorectal Cancer Screening. N Engl J Med 2018; 378(18): 1734–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Schreuders EH, Ruco A, Rabeneck L, et al. Colorectal cancer screening: a global overview of existing programmes. Gut 2015. [DOI] [PubMed] [Google Scholar]
- 60.Araghi M, Soerjomataram I, Bardot A, et al. Changes in colorectal cancer incidence in seven high-income countries: a population-based study. Lancet Gastroenterol Hepatol 2019; 4(7): 511–8. doi: 10.1016/S2468-1253(19)30147-5. Epub 2019 May 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Siegel RL, Fedewa SA, Anderson WF, et al. Colorectal Cancer Incidence Patterns in the United States, 1974–2013. J Natl Cancer Inst 2017; 109(8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Vuik FE, Nieuwenburg SA, Bardou M, et al. Increasing incidence of colorectal cancer in young adults in Europe over the last 25 years. Gut 2019; 68(10): 1820–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Pilleron S, Sarfati D, Janssen-Heijnen M, et al. Global cancer incidence in older adults, 2012 and 2035: A population-based study. Int J Cancer 2019; 144(1): 49–58. [DOI] [PubMed] [Google Scholar]
- 64.Khan SA, Thomas HC, Davidson BR, Taylor-Robinson SD. Cholangiocarcinoma. Lancet 2005; 366(9493): 1303–14. [DOI] [PubMed] [Google Scholar]
- 65.Petrick JL, McGlynn KA. The changing epidemiology of primary liver cancer. Curr Epidemiol Rep 2019; 6(2): 104–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.NCD Risk Factor Collaboration., Di Cesare M, Bentham J, et al. Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet 2016; 387(10026): 1377–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Collaboration NCDRF. Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet 2016; 387(10027): 1513–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chang MH, Chen CJ, Lai MS, et al. Universal hepatitis B vaccination in Taiwan and the incidence of hepatocellular carcinoma in children. Taiwan Childhood Hepatoma Study Group. N Engl J Med 1997; 336(26): 1855–9. [DOI] [PubMed] [Google Scholar]
- 69.Chang MH, You SL, Chen CJ, et al. Decreased incidence of hepatocellular carcinoma in hepatitis B vaccinees: a 20-year follow-up study. J Natl Cancer Inst 2009; 101(19): 1348–55. [DOI] [PubMed] [Google Scholar]
- 70.Prueksapanich P, Piyachaturawat P, Aumpansub P, Ridtitid W, Chaiteerakij R, Rerknimitr R. Liver Fluke-Associated Biliary Tract Cancer. Gut Liver 2018; 12(3): 236–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Petrick JL, Florio AA, Znaor A, et al. International trends in hepatocellular carcinoma incidence, 1978–2012. Int J Cancer 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Songserm N, Promthet S, Sithithaworn P, et al. Risk factors for cholangiocarcinoma in high-risk area of Thailand: role of lifestyle, diet and methylenetetrahydrofolate reductase polymorphisms. Cancer Epidemiol 2012; 36(2): e89–94. [DOI] [PubMed] [Google Scholar]
- 73.Collaborators GBDPC. The global, regional, and national burden of pancreatic cancer and its attributable risk factors in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol 2019; 4(12): 934–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kleeff J, Korc M, Apte M, et al. Pancreatic cancer. Nat Rev Dis Primers 2016; 2: 16022. [DOI] [PubMed] [Google Scholar]
- 75.Huang L, Jansen L, Balavarca Y, et al. Stratified survival of resected and overall pancreatic cancer patients in Europe and the USA in the early twenty-first century: a large, international population-based study. BMC Med 2018; 16(1): 125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ferlay J, Partensky C, Bray F. More deaths from pancreatic cancer than breast cancer in the EU by 2017. Acta Oncol 2016; 55(9–10): 1158–60. [DOI] [PubMed] [Google Scholar]
- 77.Sung H, Siegel RL, Rosenberg PS, Jemal A. Emerging cancer trends among young adults in the USA: analysis of a population-based cancer registry. Lancet Public Health 2019; 4(3): e137–e47. [DOI] [PubMed] [Google Scholar]
- 78.Keum N, Bao Y, Smith-Warner SA, et al. Association of Physical Activity by Type and Intensity With Digestive System Cancer Risk. JAMA Oncol 2016; 2(9): 1146–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Moore SC, Lee IM, Weiderpass E, et al. Association of Leisure-Time Physical Activity With Risk of 26 Types of Cancer in 1.44 Million Adults. JAMA Intern Med 2016; 176(6): 816–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018; 68(6): 394–424. [DOI] [PubMed] [Google Scholar]
- 81.WHO. Global Action Plan for the Prevention of Non-Communicable Diseases 2013–2020. Geneva: World Health Organization, 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


