Abstract
Objective:
The Emergency Medical Treatment and Labor Act (EMTALA) is a federal law enacted in 1986 prohibiting patient dumping, refusing or transferring patients with emergency medical conditions without appropriate stabilization, and discrimination based upon ability to pay. We evaluate hospital-level features associated with citation for EMTALA violation.
Methods:
A retrospective analysis of observational data on EMTALA enforcement (2005–2013). Regression analysis evaluates the association between facility-level features and odds of EMTALA citation by hospital-year.
Results:
Among 4,916 EMTALA-obligated hospitals there were 1,925 EMTALA citation events at 1,413 facilities between 2005 and 2013, with 4.3% of hospitals cited per year. In adjusted analyses, increased odds of EMTALA citations were found at hospitals that were: for-profit (OR 1.61;95%CI_1.32–1.96), in metropolitan areas (OR1.32;95%CI_1.11–1.57); that admitted a higher proportion of Medicaid patients (OR1.01;95%_CI_1.0–1.01); and were in the top quartiles of hospital size (OR1.48;95%CI_1.10–1.99) and ED volume (OR1.56;95%CI_1.14 – 2.12). Predicted probability of repeat EMTALA citation in the year following initial citation was 17% among for-profit and 11% among other hospital types. Among citation events for patients presenting to the same hospital’s ED, there were 1.30 EMTALA citation events per million ED visits, with 1.04 at private not-for-profit, 1.47 at government-owned, and 2.46 at for-profit hospitals.
Conclusions:
For-profit ownership is associated with increased odds of EMTALA citations after adjusting for other characteristics. Efforts to improve EMTALA might be considered to protect access to emergency care for vulnerable populations, particularly at large, urban, for-profit hospitals admitting high proportions of Medicaid patients.
Keywords: Health Policy, Health Law, Emergency Department, Access to Care, EMTALA, Emergency Medical Treatment and Labor Act
INTRODUCTION
Enacted in 19861 in response to publicized incidents of inadequate, delayed or denied treatment of uninsured patients,2–5 the Emergency Medical Treatment and Labor Act (EMTALA) is perhaps the most important federal legislation governing United States (U.S.) emergency care.6 EMTALA is intended to stop the dangerous and discriminatory practice of hospitals refusing or transferring financially disadvantaged patients without appropriate stabilization.2,5 EMTALA requires hospitals provide patients who present to a dedicated emergency department (ED) with a timely medical screening evaluation, stabilization of emergent conditions, and transfer if specialized services needed for stabilization are not available at the presenting hospital, regardless of ability to pay.1 EMTALA also requires hospitals to accept transfer of patients if the receiving facility has specialized services (e.g. neurosurgery) required to stabilize an emergent condition.1
EMTALA compliance is a condition of Medicare provider participation.7 The ten regional offices of the Centers for Medicare and Medicaid Services (CMS) are responsible for EMTALA enforcement. If an EMTALA violation is identified, and a hospital fails to propose acceptable corrective actions in response to citation, the hospital’s Medicare provider agreement can be terminated. In rare cases, financial penalties may be levied.8–11 Terminations have catastrophic implications for a hospital’s ability to operate given that Medicare reimburses almost half of inpatient costs nationwide.12
Nevertheless, and despite substantial consequences associated with noncompliance, refusal of emergency care continues as citations for EMTALA violations continue. Between 2005 and 2014, EMTALA citations were issued to more than 25% of U.S. hospitals.6 Recent studies evaluating EMTALA enforcement and compliance shed light on: the characteristics of EMTALA violations,6 the relatively rare civil monetary penalty settlements resulting from EMTALA citations,8–11 as well as barriers to EMTALA compliance.7 However, no studies examine hospital features associated with EMTALA citations. Understanding characteristics of hospitals cited for EMTALA violations is essential to informing future efforts to enhance or improve EMTALA and better-target enforcement activities.
MATERIALS AND METHODS
Study Design
This is a retrospective analysis of observational data on U.S. hospital-level EMTALA enforcement between 2005 and 2013. Any individual or institution may report suspected violation of EMTALA to CMS. Following initial inquiry, CMS regional offices can authorize an EMTALA investigation by state survey agencies. State survey agencies complete the investigation and provide findings to CMS regional offices. In the course of an EMTALA investigation, state officials typically review hospital compliance with all aspects of the EMTALA statute (see Supplement 1 for EMTALA requirements), and may identify any observed deficiencies.6 CMS regional offices are responsible for determining whether EMTALA was violated, and whether the hospital will be cited with an immediate, 23- or 90-day notice that the hospital’s Medicare provider agreement will be terminated if acceptable corrective actions are not proposed. EMTALA investigations can result in citations for multiple deficiencies;6 we refer to the sum of EMTALA deficiency citations from an investigation as an EMTALA citation event. If a cited hospital fails to propose an acceptable plan of corrective actions to resolve identified deficiencies within the designated timeframes, CMS provider agreements can be terminated. Prior work indicates that 44% of EMTALA investigations result in citation.6
Consistent with prior work,9 hospitals subject to EMTALA were identified for our study using the number of unique facilities (identified by Medicare provider identification numbers) reporting core measure data between 2005 and 2013. We linked multiple databases using facility-specific Medicare provider identification numbers to create a longitudinal analytic file at the hospital-year level for all EMTALA-governed hospitals. This file included yearly information on facility characteristics from the American Hospital Association (AHA) Survey Database for the years 2005 through 2013,13 annual CMS quality measures, and dates of EMTALA citations between 2005 and 2013 (Supplement 2). EMTALA citations and associated deficiency tags were identified from CMS data obtained via Freedom of Information Act using methods described in prior work.6 We analyzed all available EMTALA citations at the time of the study’s design for which AHA Survey data was available.
Hospitals were characterized as being located in metropolitan or non-metropolitan areas via Rural Health Research Center criteria.14 Hospital quality was measured with annual data from CMS’s Hospital Compare database from 2005 to 2013, which tracks hospital performance by reporting the share of patients meeting predefined quality criteria.15,16 Data were collected through the Hospital Inpatient Quality Reporting (Hospital IQR) program.17 We employed a normalized measure of quality based on whether a hospital scores in the bottom 25th percentile or top 75th percentile of hospitals within groups of metrics (e.g., acute myocardial infarction (AMI), congestive heart failure (HF), or pneumonia (PNA)- specific measures). 18 Additional details are included in Supplement 3.
We used multivariable logistic regression to evaluate the association between facility-level features (independent variables) and receipt of any EMTALA citation (dependent variable), at the hospital-year level, treating each hospital-year as a separate observation. Odds ratios (OR) and predicted probabilities are reported. Models control for: a vector of facility-level features detailed in Supplement 2, CMS region, and year fixed effects. Because this analysis uses repeated measures of hospitals over time, clustered standard errors were computed to allow for correlation at the hospital-level over time. In addition, a vector of quality measures as reported in the same hospital-year is included.
While most EMTALA citations are directed at hospitals where a patient presented to an ED for care, approximately 16% of EMTALA citation events involve hospitals that fail to accept appropriate transfer of a patient at another ED requiring specialized services for stabilization.6 EMTALA citation events involving failure to accept appropriate transfer are identified by EMTALA deficiency tag 2411. To determine whether hospital features associated with EMTALA citation differed by the presence of deficiency tag 2411, we performed subgroup analyses separately evaluating hospital features of citation events involving deficiency tag 2411, and those that did not.
Though some EMTALA deficiencies do not target the ED (e.g. failure to accept appropriate transfer), all cases involved in EMTALA citations result from an ED visit. Therefore the number of ED visits provides a general estimation of the number of opportunities for EMTALA violation. Among EMTALA citations not involving failure to accept appropriate transfer, rates of EMTALA citation events per million ED visits were calculated overall and for each hospital ownership type.
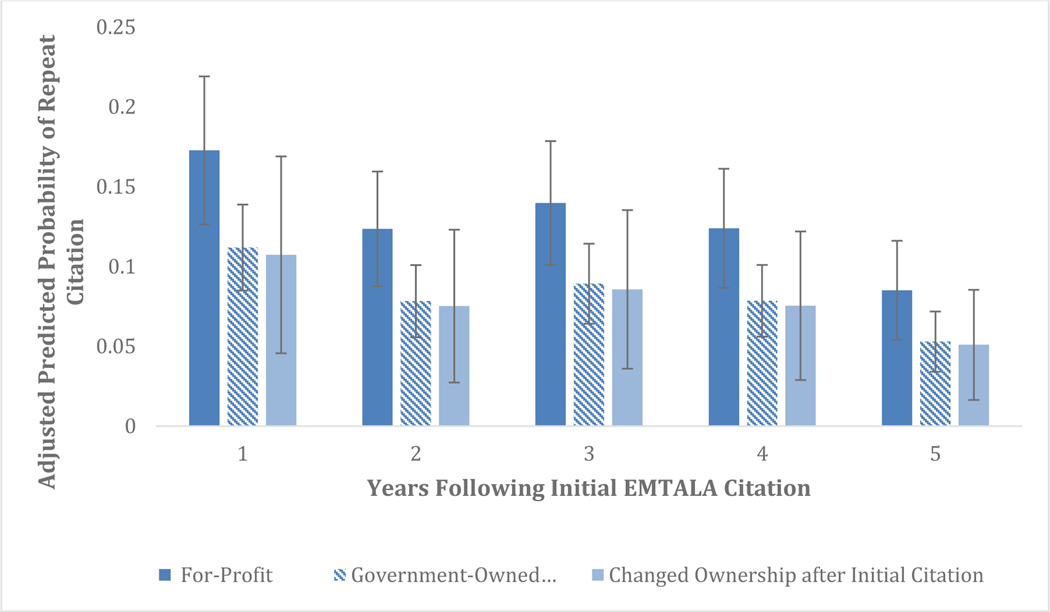
We also estimate how hospital ownership influenced the likelihood of repeat EMTALA citations following initial citation. Among hospitals with at least 5 years of records after first citation, the predicted probability of another citation was calculated annually by hospital ownership type, adjusting for the same covariates used in the main regression (private not-for-profit and government hospitals were grouped for display). Predicted probabilities were separately calculated for those hospitals that changed ownership during the study period for comparison. These numbers represent the mean predicted probability of repeat citation by year after initial citation.
The share of all admissions paid for by Medicaid (hereafter, Medicaid share of admissions) was used as a proxy for poor payer mix as a similar measure for uninsured admissions or visits was unavailable in the datasets used. This measure enters regressions as the effect of a one-percentage point increase in the Medicaid share of admissions (e.g. from 25 to 26% of admissions). Predicted probability of EMTALA citations by Medicaid share of admissions was also estimated, adjusting for the same hospital-level features used in the main regression. Data were managed using Stata/MP13 (StataCorp. 2013. College Station, TX). This study was completed using hospital-level citation data and does not constitute human subjects research.
Study Sample
During the study period, 5,527 hospitals reported CMS core measure data. Because CMS reporting is required of hospitals with CMS provider agreements and these hospitals are subject to EMTALA, this represents the universe of EMTALA-obligated hospitals during the study period. There were 1,925 reported EMTALA citation events at 1,413 unique hospitals between 2005 and 2013. We included 1,713 of 1925 (89%) citation events occurring at the 1,237 hospitals appearing in the AHA Survey Database. We further narrowed our sample to those hospital-years with CMS quality measures, resulting in a final sample of 4916 unique hospitals and 1642 citation events (38,128 hospital-year records). Of these 4916 unique hospitals, 1237 (25%) had at least one citation event (1642 events in total) during the study period, and 3679 (75%) had no citations. Of 1642 citation events, 264 (16.1%) involved citations for deficiency tag 2411 (failure to accept appropriate transfer from another hospital’s ED). Overall 226(18.3%) of 1237 cited hospitals had citations involving deficiency tag 2411.
Study Results:
Association between hospital characteristics and EMTALA citation event
On average, 4.31% of hospitals received an EMTALA citation in a given year. Characteristics of hospitals by ownership type are included in Table 1. In multivariate analyses, private for-profit hospitals had higher adjusted odds of EMTALA citations (OR 1.61; 95% CI 1.32–1.96, p<0.001) compared to government-owned hospitals (see Table 2). Private for-profit hospitals also had increased odds of EMTALA citations compared with private not-for-profit hospitals (OR=1.44; 95% CI 1.23–1.69, p<0.001). Increased odds of EMTALA citations were found at hospitals in metropolitan areas (OR 1.32; 95% CI, 1.11–1.57, p=0.002) and hospitals in the top quartile of hospital size (OR 1.48; 95% CI, 1.10–1.99, p=0.010) and ED volume (OR 1.56, 95% CI, 1.14 – 2.12, p=0.005). The Medicaid share of admissions was positively associated with increased odds of EMTALA citation (OR 1.01; 95% CI, 1.00–1.01, p=0.015, for a one percentage point increase in Medicaid share of admissions). Adjusted predicted probability of EMTALA citation varied by quintile of Medicaid share of admissions (Supplement 4). Hospital quality measures generally were not associated with EMTALA citations with one exception; hospitals in the 75th percentile of AMI quality measures had marginally decreased odds of EMTALA citation (OR 0.74; 95% CI 0.56–0.99: p=0.040). Odds of EMTALA citations did not vary significantly by share of Medicare admissions, indigent care-, critical access-, rural referral- or teaching hospital status.
Table 1.
Features of Hospital Ownership by Hospital-Year Records, 2005–2013
| Overall | Government Owned* | Not-for-Profit* | For-Profit* | Changed Ownership** | p-value | |||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||
| n | n | % | n | % | n | % | n | % | ||
| Hospitals-Year Records | 38128 | 7354 | 19% | 21748 | 57% | 5440 | 14% | 3586 | 9% | |
| Hospital-Year Citation Records*** | 1642 | 256 | 3% | 888 | 4% | 351 | 6% | 147 | 4% | <0.001 |
| Number of unique hospitals | 4916 | 1008 | 21% | 2712 | 55% | 766 | 16% | 430 | 9% | |
| Unique hospitals with an EMTALA citation event | 1237 | 201 | 20% | 690 | 25% | 234 | 31% | 112 | 26% | <0.001 |
| Unique hospitals with repeat EMTALA citation events | 307 | 44 | 4% | 160 | 6% | 79 | 10% | 24 | 6% | <0.001 |
| Total citations**** | 1713 | 265 | 920 | 369 | 159 | |||||
| Total ED visits (million) | 1093 | 152 | 729 | 127 | 85 | |||||
| Citations per million ED visits***** | 1.57 | 1.74 | 1.26 | 2.91 | 1.87 | |||||
| Hospital Characteristics | ||||||||||
| Critical access hospital | 8365 | 3034 | 41% | 4394 | 20% | 203 | 4% | 734 | 20% | <0.001 |
| Regional referral center | 2440 | 384 | 5% | 1548 | 7% | 365 | 7% | 143 | 4% | <0.001 |
| Indigent care hospital | 6045 | 1165 | 17% | 4361 | 21% | 132 | 3% | 387 | 12% | <0.001 |
| Teaching hospital | 2419 | 534 | 7% | 1690 | 8% | 67 | 1% | 128 | 4% | <0.001 |
| Metropolitan status | 20908 | 2176 | 30% | 12960 | 60% | 3856 | 71% | 1916 | 53% | <0.001 |
| ED Volume (mean annual visits) | 28554 | 20558 | 33410 | 23110 | 23753 | <0.001 | ||||
| Hospital Size (mean bed total) | 177 | 128 | 206 | 150 | 142 | <0.001 | ||||
| Payer mix (mean % inpatient admissions) | ||||||||||
| Medicare | 48% | 48% | 49% | 46% | 49% | <0.001 | ||||
| Medicaid | 17% | 18% | 17% | 18% | 18% | <0.001 | ||||
Data was collected at the hospital-year level, and hospital-year observations are reported by hospital ownership type.
Hospitals with consistent ownership (government, not-for-profit, for profit) during the study period
Hospitals that changed ownership categorization during the study period
Whether a hospital was cited in a specific year (1 vs 0), regardless of having multiple citations in that year (outcome in the regression models)
Total count of EMTALA citation events, including multiple citation events within the same year. A citation event includes all EMTALA deficiencies tags resulting from a single investigation. Of note, EMTALA citation events often include numerous deficiency tags.
This calculation includes those citation events involving patients presenting to the ED of the cited hospital, and not those involving failure to accept transfer
Key: EMTALA: Emergency Medical Treatment and Labor Act; ED: Emergency Department
Table 2.
Hospital Features Associated with Emergency Medical Treatment and Labor Act (EMTALA) Citation Events
| Observations with a citation* | Adjusted ** | Adjusted Non- 2411 deficiencies*** | Adjusted 2411 deficiencies | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| n(%) | OR | 95 CI% | p-values | OR | 95 CI% | p-values | OR | 95 CI% | p-values | |
| Ownership | ||||||||||
| Government Owned | 298 (3.6%) | |||||||||
| Private not-for-profit | 943 (4.1%) | 1.11 | 0.94, 1.32 | 0.203 | 1.12 | 0.93, 1.34 | 0.234 | 1.10 | 0.74, 0.72 | 0.638 |
| Private for profit | 401 (6.2%) | 1.61 | 1.32, 1.96 | 0.000 | 1.74 | 1.40, 2.16 | 0.000 | 1.14 | 0.72, 1.81 | 0.579 |
| CMS Quality Measures **** | ||||||||||
| AMI 75th Percentile | 64 (2.8%) | 0.74 | 0.56, 0.99 | 0.040 | 0.76 | 0.57, 1.03 | 0.072 | 0.41 | 0.10, 1.64 | 0.210 |
| HF 75th Percentile | 34 (4.1%) | 1.15 | 0.78, 1.68 | 0.484 | 1.15 | 0.76, 1.73 | 0.511 | 1.13 | 0.50, 2.57 | 0.765 |
| PNA 75th Percentile | 13 (3.8%) | 0.86 | 0.42, 1.79 | 0.694 | 0.90 | 0.45, 1.79 | 0.754 | 0.72 | 0.09, 5.48 | 0.754 |
| Hospital Characteristics | ||||||||||
| Critical access hospital | 228 (2.7%) | 1.10 | 0.82, 1.47 | 0.521 | 1.10 | 0.82, 1.49 | 0.519 | 1.00 | ||
| Regional referral center | 122 (5.0%) | 1.01 | 0.81, 1.26 | 0.902 | 0.91 | 0.71, 1.16 | 0.442 | 1.51 | 1.00, 2.27 | 0.051 |
| Indigent care hospital | 280 (4.6%) | 0.95 | 0.79, 1.12 | 0.520 | 0.99 | 0.82, 1.19 | 0.896 | 0.84 | 0.60, 1.17 | 0.299 |
| Teaching hospital | 160 (6.6%) | 1.22 | 0.97, 1.51 | 0.084 | 0.99 | 0.76, 1.29 | 0.945 | 2.19 | 1.49, 3.20 | 0.000 |
| Metropolitan status | 1099 (5.3%) | 1.32 | 1.11, 1.57 | 0.002 | 1.28 | 1.07, 1.54 | 0.009 | 1.60 | 1.04, 2.45 | 0.033 |
| ED Volume (1st Quartile reference) | ||||||||||
| 1st Quartile (smallest) | 256 (2.7%) | |||||||||
| 2nd Quartile | 350 (3.7%) | 1.26 | 0.98, 1.63 | 0.071 | 1.29 | 0.99, 1.67 | 0.055 | 0.73 | 0.29, 1.83 | 0.500 |
| 3rd Quartile | 450 (4.7%) | 1.29 | 0.97, 1.71 | 0.079 | 1.26 | 0.94, 1.68 | 0.128 | 0.99 | 0.39, 2.56 | 0.989 |
| 4th Quartile (largest) | 586 (6.2%) | 1.56 | 1.14, 2.12 | 0.005 | 1.58 | 1.14, 2.19 | 0.005 | 1.00 | 0.37, 2.68 | 0.998 |
| Hospital Size (1st Quartile reference) | ||||||||||
| 1st Quartile (smallest) | 265 (2.8%) | |||||||||
| 2nd Quartile | 333 (3.5%) | 1.03 | 0.80, 1.32 | 0.805 | 0.98 | 0.76, 1.26 | 0.852 | 6.09 | 0.74, 50.00 | 0.092 |
| 3rd Quartile | 432 (4.6%) | 1.21 | 0.93, 1.59 | 0.163 | 1.05 | 0.79, 1.38 | 0.756 | 13.10 | 1.59, 107.73 | 0.017 |
| 4th Quartile (largest) | 612 (6.4%) | 1.48 | 1.09, 1.99 | 0.010 | 1.16 | 0.85, 1.60 | 0.347 | 22.06 | 2.67, 182.55 | 0.004 |
| Medicare Admissions (% of Inpatient Admissions) | 1.00 | 0.99, 1.00 | 0.581 | 1.00 | 0.99, 1.01 | 0.635 | 1.00 | 0.99, 1.01 | 0.934 | |
| Medicaid Admissions (% of Inpatient Admissions) | 1.01 | 1.00, 1.01 | 0.015 | 1.01 | 1.00, 1.01 | 0.033 | 1.01 | 1.00, 1.02 | 0.128 | |
Number of hospital-year observations with an EMTALA citation and percentage of all hospital-year observations in category with a citation
The adjusted model uses contemporaneous ownership category at the hospital-year level
This excludes citation events involving a citation for deficiency 2411 (recipient hospittal responsibilities), these are hospitals where the citation event involved a patient presenting to the same hospital receiving the citation, and not a hospital refusing to accept appropriate transfer of a patient at another ED
This output represents hospitals scoring in the top quartile of quality compared with those not in the top quartile. We additionally controlled for bottom quartile of quality measures compared with not in the bottom quartile, however,no significant relationship between odds of citation and low quality was identified.
Key: CMS: Centers for Medicare & Medicaid Services; AMI: Acute Myocardial Infarction; HF: Heart Failure; PNA; Pneumonia; ED; Emergency Department
In a subgroup analysis, we evaluated hospital features associated with EMTALA citation not involving deficiency tag 2411: failure to accept appropriate transfer (Table 2). Again, we found that for-profit (OR 1.74; 95% CI 1.40–2.16; p=0.000) and metropolitan status (OR 1.28; 95% CI 1.07–1.54;p=0.009), top quartile of ED volume (OR 1.58; 95% CI 1.14–2.19; p=0.005) and Medicaid share of admissions (OR 1.01; 95% CI 1.00–1.01; p=0.033, for a one percentage point increase in Medicaid share of admissions) were associated with a higher odds of EMTALA citations, but hospital size and quality measures were not. Among the subset of citation events involving deficiency tag 2411, only top quartile of hospital size (OR 22.05; 95% CI 2.67–182.55; p=0.004), teaching hospital (OR 2.18; 1.49–3.20; 95% CI; p<0.001) and metropolitan status (OR 1.59; 95% CI 1.04–2.45; p=0.033) were associated with increased odds of EMTALA citation, whereas ownership status, ED volume and Medicaid share of admissions had no significant association.
Characteristics of hospitals with repeated EMTALA citation events during the study period
Among 1,237 hospitals with EMTALA citations, 332 (26.84%) were noted to have EMTALA citations in subsequent years after the initial citation observed in the study period. Receipt of repeated citations in future years occurred in 35% of private for-profit, 25% of private not-for profit, and 24% of government-owned hospitals (p=0.003). The predicted probability of a repeat EMTALA citation in the years after an initial citation among hospitals that did not change ownership status was 17% among for-profit hospitals and 11% among other hospital ownership categories. Among hospitals that changed ownership type after initial citation, the predicted probability of repeat citation was similar to that of government-owned and not-for-profit hospitals (see Figure 1 and Supplement 5, which represents an alternative display of information provided in Figure 1 for reviewers to consider).
Figure 1.
Predicted Probability of Repeat EMTALA Citation Following Initial Citation, by Hospital Ownership
DISCUSSION
EMTALA was intended to stop the blatantly dangerous and discriminatory practice of denying emergency care to financially disadvantaged patients by imposing penalties with financial implications to hospitals denying emergency care. More than three decades after its passage, and despite substantial consequences associated with noncompliance, one-quarter of U.S. hospitals were cited for EMTALA noncompliance during the study period and 4.3% of hospitals cited in an average year. Hospitals that are large, metropolitan, for-profit, admit a sizeable proportion of Medicaid patients, and have high ED volumes have increased odds of EMTALA citation after regression adjustment. Private for-profit hospitals are more likely to have repeat EMTALA citations compared to private not-for-profit or government-owned hospitals. Overall, private for-profit hospitals incur more than twice as many EMTALA citations per million ED visits as private not-for-profit hospitals.
For-profit hospitals are under greater pressure to produce net income for investors and have financial incentive to avoid patients for whom revenue is low or non-existent such as those with Medicaid or the uninsured. Prior studies have demonstrated negative hospital profit margins for ED care of patients who are uninsured (−54.4%) or covered by Medicaid (−35.9%).19 Given negative profit margins with ED visits for uninsured or Medicaid patients, hospitals, and for-profit hospitals in particular, have significant financial incentive to avoid these patients. A prior study that assessed transfers out of EDs in the U.S. found that payer status – particularly Medicaid or self-pay increased the likelihood of transfer out, and that this effect was greater in for-profit hospitals.20 The most consistent and substantial effect observed in this study surrounded for-profit hospitals, who may discriminate more based on payer than non-profit hospitals due to their mission, and as a result, be cited more for this behavior. If the costs of providing emergency care for uninsured or Medicaid patients exceed the costs of penalization for an EMTALA violation, hospitals may not have strong financial incentive to avoid EMTALA noncompliance.
Our finding that hospitals with a poor payer mix have higher odds of EMTALA citation might be explained by Medicaid reimbursement policies and rates. Nonpayment (or underpayment) for EMTALA screening exams have been cited as important contributors to financial pressure for hospitals to avoid devoting resources to these patients.7 Further, these hospitals may have patients facing a relatively higher socioeconomic burden of disease and have fewer resources to invest in patient care. Focusing on Medicaid patients is worthy of consideration as approximately 10 million previously uninsured Americans gained healthcare coverage through the Medicaid expansion under the Affordable Care Act.21,22 While Medicaid expansion may have improved access to primary or specialty care,23,24 Medicaid expansion has been associated with increased demand for ED services.25,26 Increased demand for ED services will likely place increased financial strain on hospitals disproportionately serving the Medicaid population.
We also find that large hospitals and those with high ED volumes have increased odds of EMTALA citation. As each ED visit represents an opportunity for a hospital to violate EMTALA, larger hospitals may have more opportunities for violation or citation. The association between metropolitan hospitals and EMTALA citation might be explained by proximity to other hospitals. Hospitals located in rural areas are unlikely to have many facilities in close proximity where patients could be transferred or formally or informally referred for care. In contrast, hospitals in urban areas likely have many proximate facilities where they might suggest a patient seek care.
In contrast, only one measure of hospital quality had a weak association with odds of EMTALA citation. Taken together, our findings suggest that EMTALA compliance is not a reflection of overall hospital quality. Hospitals may provide top quality care to admitted patients while simultaneously violating EMTALA in ED patients. Solutions to improving EMTALA compliance will need to be EMTALA-specific and not necessarily part of a broader, hospital-wide, quality improvement initiative. Importantly, CMS has recently added ED-specific quality metrics and their association with EMTALA enforcement warrants future investigation.
The most severe financial consequence for a hospital failing to resolve an EMTALA citation is termination of the Medicare provider agreement.6 While corrective actions to attain EMTALA compliance may be costly and onerous for hospitals, they are at least theoretically, achievable, with more than 99.5% of cited facilities implementing acceptable plans for compliance and avoiding termination.6 Increasing terminations would likely result in hospital closures and could adversely affect communities served by these facilities. That a quarter of hospitals received an EMTALA citation during the study period suggests that perhaps the consequence of termination as currently enforced does not serve as a strong deterrent to EMTALA noncompliance. Policy makers might consider alternate penalties with a greater ability to deter violations while continuing to safeguard access to care for vulnerable populations.
The Office of the Inspector General (OIG) has the power to levy civil monetary penalties to hospitals violating EMTALA. However, these are rarely employed as only 7.9% of EMTALA citations result in a civil monetary penalty.10 Furthermore, these rare financial penalties are not particularly large, especially when compared to penalties like those for Medicare billing fraud. The average hospital settlement amount between 2002 and 2015 was $33,435.7 In 2016, three decades after EMTALA was enacted the OIG inflation-adjusted the maximum civil monetary penalty of 50,0001 to $103,139.27 In contrast, fines for Medicare billing fraud are large and impactful. Prior to 2016, the largest penalty related to an EMTALA citation event was $180,000 in 2012.28 In 2017 the OIG issued a record penalty of 1.295 million dollars (resulting from stacked fines) related to an EMTALA citation event at a South Carolina hospital, still lower than many billing fraud fines.28,29 While EMTALA citations are inconvenient for hospitals, given the rarity of financial penalties, relatively small size of the penalties, and the rarity of termination of Medicare provider agreements, hospitals are not strongly incentivized to comply with EMTALA. While the notable rate of repeat citation after initial citation event might be explained by increased scrutiny of cited hospitals, the differential probability of repeat citation event following initial citation by hospital payer type suggests that for-profit hospitals may be less motivated to comply with EMTALA based upon current penalties as enforced, or less capable of implementing proposed corrective actions than hospitals in other ownership groups.
Among the policy solutions proposed to improve EMTALA compliance include increased reporting and positive and negative financial incentives.
Rosenbaum and colleagues have noted that there is no ongoing transparent and public reporting system for EMTALA citations,30 and advocated for a more effective system for reporting EMTALA violations. Perhaps required public notice or posting of EMTALA citations, similar to Hospital Compare, would motivate hospitals to avoid EMTALA noncompliance. More closely aligning payment policies with EMTALA, such as guaranteed payment at Medicare rates for EMTALA-obligated activities, has been suggested as a means to improve EMTALA compliance.7 Finally, encouraging reimbursement strategies for ED providers that shelter a provider’s take home pay from the patient’s ability to pay (e.g. salary) may discourage differential care for vulnerable populations.
Though this study provides the first comprehensive assessment of hospital features associated with EMTALA violations, we acknowledge a number of potential limitations. First, findings depend upon administrative data and therefore, may be limited by coding inconsistencies inherent to secondary data analysis. However, we do not have reason to suspect systematic error in data recording. Second, findings from citations likely represent an underestimate of true EMTALA violations as hospital administrators report reluctance to report suspected violations.7 However, we believe that information obtained from CMS represents the best available data source to study EMTALA enforcement. Third, evaluation is limited to the years for which EMTALA, AHA, and CMS data was available at the time of analysis. Further evaluation of the association between ED-specific quality measures and EMTALA citation will be warranted as additional years of ED-specific data become available. Fourth, though it would have been ideal to include the proportion of uninsured patients in the hospital payer mix, this information was not reliably available in databases used. The proportion of inpatient admissions at a hospital paid by Medicaid is used instead as Medicaid patients are represent a financially undesirable group of patients as they often result in lost revenue for hospitals,19 and financial incentives to avoid Medicaid patients have been identified as a motivator for EMTALA noncompliance.7 While most ED visits do not result in admissions, we believe the proportion of inpatient admissions at a hospital with Medicaid as payer is a general indicator of the payer mix of the patients served by the institution. Fifth, it is possible that hospitals with citations that matched with hospitals in the AHA Database differed systematically from those that did not thereby biasing results. Additionally, AHA data is self-reported by hospitals, and therefore, may be prone to reporting error as compared to administratively derived data like Hospital Compare. Finally, enforcement bias rather than true differences in EMTALA noncompliance might explain some patterns identified, and this may be particularly relevant for hospitals with repeat violations.
CONCLUSIONS
This is the first comprehensive assessment of hospital features associated with EMTALA citations. Understanding characteristics of hospitals cited for EMTALA violations is essential to informing future efforts to enhance EMTALA and better-target enforcement activities. Continued and repeated violation of EMTALA suggests that the current law does not ensure compliance. Given that EMTALA noncompliance continues and may be driven by financial incentives, perhaps hospitals, and for-profit hospitals in particular, need greater disincentives for EMTALA noncompliance or greater motivation to care for patients. Regulators and policy makers should evaluate how EMTALA might be strengthened to protect access to emergency care for vulnerable populations, and to promote EMTALA compliance, particularly among hospitals at high likelihood of poor compliance.
Supplementary Material
Supplemental Digital Content 1. EMTALA Deficiency Tags and Summary of EMTALA Interpretive Guidelines
Supplemental Digital Content 3. Use of Hospital Quality Measures
Supplemental Digital Content 2. Data Sources and Elements Used in Analysis
Supplementary Digital Content 4. Predicted Probability of EMTALA Citation Event by Quintile of Medicaid Admissions
Supplemental Digital Content 5. Predicted Probability of Repeat EMTALA Citation Event Following Initial Citation Event, By Hospital Ownership
Acknowledgements
An abstract based upon preliminary findings was presented at the 2016 ACEP Scientific Assembly, Las Vegas, NV. Authors thank Raquel Martinez for her assistance with figure and table creation and manuscript submission.
Funding
The Agency for Healthcare Research and Quality (AHRQ R03 HS 25281-01A1) awarded funding for this study. Study sponsors did not have any role in study design or collection, analysis or interpretation of the data; in the writing of the report; or the decision to submit the article for publication.
Footnotes
Conflicts of Interest
Authors do not report any pertinent conflicts of interest.
REFERENCES:
- 1.42 U.S. Code § 1395dd.
- 2.Ansell DA. Patient dumping. Status, implications, and policy recommendations. JAMA: The Journal of the American Medical Association. 1987;257(11):1500–1502. [DOI] [PubMed] [Google Scholar]
- 3.Schiff RL, Ansell DA, Schlosser JE, Idris AH, Morrison A, Whitman S. Transfers to a public hospital. A prospective study of 467 patients. The New England journal of medicine. 1986;314(9):552–557. [DOI] [PubMed] [Google Scholar]
- 4.Stark FP. “Dumped” patients paying with their lives. . In. 131 Congressional Record: 35813–35814. . [Google Scholar]
- 5.Azoulay E, Chevret S, Didier J, et al. Infection as a trigger of diabetic ketoacidosis in intensive care-unit patients. Clin Infect Dis. 2001;32(1):30–35. [DOI] [PubMed] [Google Scholar]
- 6.Terp S, Seabury SA, Arora S, Eads A, Lam CN, Menchine M. Enforcement of the Emergency Medical Treatment and Labor Act, 2005 to 2014. Annals of emergency medicine. 2017;69(2):155–162 e151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hsuan C, Horwitz JR, Ponce NA, Hsia RY, Needleman J. Complying with the Emergency Medical Treatment and Labor Act (EMTALA): Challenges and solutions. Journal of healthcare risk management : the journal of the American Society for Healthcare Risk Management. 2018;37(3):31–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Terp S, Wang B, Burner E, Arora S, Menchine M. Penalties for Emergency Medical Treatment and Labor Act Violations Involving Obstetrical Emergencies. Western Journal of Emergency Medicine. 2020;21(2):235–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Terp S, Wang B, Raffetto B, Seabury SA, Menchine M. Individual Physician Penalties Resulting From Violation of Emergency Medical Treatment and Labor Act: A Review of Office of the Inspector General Patient Dumping Settlements, 2002–2015. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2017;24(4):442–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zuabi N, Weiss L, Langdorf M. Emergency Medical Treatment and Labor Act (EMTALA) 2002–15: Review of Office of Inspector General Patient Dumping Settlements. Western Journal of Emergency Medicine. 2016;XVII(3):245–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McKenna RM, Purtle J, Nelson KL, Roby DH, Regenstein M, Ortega AN. Examining EMTALA in the era of the patient protection and Affordable Care Act. AIMS Public Health. 2018;5(4):366–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Agency for Healthcare R, Quality. National Inpatient Hospital Costs: The Most Expensive Conditions by Payer, 2011. The HCUP Report : Healthcare Cost and Utilization Project (HCUP): Statistical Briefs;2013 ASI 4186–20.160;Statistical Brief No. 160. 2013. [Google Scholar]
- 13.American Hospital Association (AHA) Annual Survey Database. In:FY2003-2013. [Google Scholar]
- 14.Rural_Health_Research_Center. RUCA Data. Code Definitions: Versions 2.0. . http://depts.washington.edu/uwruca/ruca-codes.php. Accessed 11 September 2018.
- 15.Centers for Medicare & Medicaid Services. Medicare.gov - Hospital Compare. https://www.medicare.gov/hospitalcompare/search.html. Published 2015. Accessed 5 October, 2015.
- 16.Centers for Medicare & Medicaid Services. HOSArchive_Revised_Flatfiles_20150122.zip. In:2015. [Google Scholar]
- 17.Centers for Medicare & Medicaid Services. Hospital Inpatient Quality Reporting Program. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/HospitalRHQDAPU.html. Published 2015. Accessed October 5, 2015.
- 18.Werner RM, Bradlow ET. RElationship between medicare’s hospital compare performance measures and mortality rates. JAMA. 2006;296(22):2694–2702. [DOI] [PubMed] [Google Scholar]
- 19.Wilson M, Cutler D. Emergency department profits are likely to continue as the Affordable Care Act expands coverage. Health affairs. 2014;33(5):792–799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kindermann DR, Mutter RL, Cartwright-Smith L, Rosenbaum S, Pines JM. Admit or transfer? The role of insurance in high-transfer-rate medical conditions in the emergency department. Annals of emergency medicine. 2014;63(5):561–571. e568. [DOI] [PubMed] [Google Scholar]
- 21.Cohen RA, Martinez ME, Zammitti EP. Health Insurance Coverage: Early Release of Estimates from the National Health Interview Survey, January-March, 2018.: National Center for Health Statistics;2018. [Google Scholar]
- 22.Long-term Trends in Health Insurance Coverage: Estimates from the National Health Interview Survey, 1968–2017. National Center for Health Statistics;2018. [Google Scholar]
- 23.Tipirneni R, Rhodes KV, Hayward RA, Lichtenstein RL, Reamer EN, Davis MM. Primary care appointment availability for new Medicaid patients increased after Medicaid expansion in Michigan. Health affairs. 2015;34(8):1399–1406. [DOI] [PubMed] [Google Scholar]
- 24.Eguia E, Cobb AN, Kothari AN, et al. Impact of the Affordable Care Act (ACA) Medicaid Expansion on Cancer Admissions and Surgeries. Annals of surgery. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Taubman SL, Allen HL, Wright BJ, Baicker K, Finkelstein AN. Medicaid increases emergency-department use: evidence from Oregon’s Health Insurance Experiment. Science. 2014;343(6168):263–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Finkelstein AN, Taubman SL, Allen HL, Wright BJ, Baicker K. Effect of Medicaid Coverage on ED Use - Further Evidence from Oregon’s Experiment. The New England journal of medicine. 2016;375(16):1505–1507. [DOI] [PubMed] [Google Scholar]
- 27.Annual Civil Monetary Penalties Inflation Adjustment (82 FR § 9174). 2016. [Google Scholar]
- 28.Terp S WB, Burner E, Connor D, Seabury S, Menchine M. Civil monetary penalties resulting from violations of the Emergency Medical Treatment and Labor Act (EMTALA) involving psychiatric emergencies, 2002–2018. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2019;In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Department of Justice USAsO, Northern District of Georgia. ANMED Health agrees to pay $7 million to settle False Claims Act allegations. https://www.justice.gov/usao-ndga/pr/anmed-health-agrees-pay-7-million-settle-false-claims-act-allegations. Published 2017. Updated September 27, 2017. Accessed 1 March 2019.
- 30.Rosenbaum S, Cartwright-Smith L, Hirsh J, Mehler PS. Case studies at Denver Health: ‘patient dumping’ in the emergency department despite EMTALA, the law that banned it. Health affairs. 2012;31(8):1749–1756. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content 1. EMTALA Deficiency Tags and Summary of EMTALA Interpretive Guidelines
Supplemental Digital Content 3. Use of Hospital Quality Measures
Supplemental Digital Content 2. Data Sources and Elements Used in Analysis
Supplementary Digital Content 4. Predicted Probability of EMTALA Citation Event by Quintile of Medicaid Admissions
Supplemental Digital Content 5. Predicted Probability of Repeat EMTALA Citation Event Following Initial Citation Event, By Hospital Ownership