Abstract
This cohort study examines the association of human papillomvirus vaccination with cervical cancer incidence and mortality rates in the US, comparing age groups understood to have differing levels of vaccination.
Human papillomavirus (HPV) is a common sexually transmitted infection and is implicated in most cervical cancer cases.1 Vaccination against HPV for women and girls aged 11 to 26 years was first recommended in 2006.1,2 Randomized clinical trials showed vaccine-driven decreases in precancerous lesions, and observational studies showed vaccine-associated decreases in cervical cancer incidence.1,2,3,4 However, data demonstrating vaccine-associated changes in cervical cancer mortality are lacking. We aimed to quantify associations between HPV vaccine implementation in the US and changes in cervical cancer incidence and mortality.
Methods
National age-adjusted cervical cancer incidence and mortality data from January 2001 through December 2017 for women and girls aged 15 to 39 years were obtained from the combined Surveillance, Epidemiology, and End Results and National Program of Cancer Registries databases (incidence) and the National Center for Health Statistics (mortality). Age and year were based on the date of diagnosis for incidence or the date of death for mortality. The study was exempt from institutional review board review and consent requirements, given the aggregated and deidentified nature of these ecological data. Reporting is per Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines.
We conducted quasi-experimental analyses comparing percentage changes in incidence and mortality from January 2001 through December 2005 (prevaccination) to January 2010 through December 2017 (postvaccination) in individuals aged 15 to 24 years vs 25 to 29 years or 30 to 39 years. The older 2 groups were included as comparisons, given their low vaccination rates (eMethods in the Supplement).1 We excluded January 2006 through December 2009 in our primary analysis and January 2006 through December 2015 in a sensitivity analysis, since time is required for carcinogenesis. The variance of estimates was derived using simulation (eMethods in the Supplement). Analyses were performed from November 2020 to July 2021 using R version 3.6.2 (R Foundation for Statistical Computing). All P values are 2-sided, and we defined P < .05 as the threshold of statistical significance.
Results
From January 2001 through December 2017, cervical cancer incidence rates were 0.68, 5.47, and 12.60 per 100 000 and cervical cancer mortality rates were 0.06, 0.57, and 1.89 per 100 000 in the groups aged 15 to 24 years, 25 to 29 years, and 30 to 39 years. The percentage reduction in incident cancer from 2001 through 2005 to 2010 through 2017 was greater among those aged 15 to 24 years (−37.70% [95% CI, −42.24% to −32.75%]) than those aged 25 to 29 years (−16.16% [95% CI, −19.45% to −12.69%]) and those aged 30 to 39 years (−8.03% [95% CI, −9.90% to −6.12%]; relative change P < .001; Table; Figure). The decrease in cervical cancer mortality among those aged 15 to 24 years (−43.35% [95% CI, −59.38% to −20.50%) was also greater than the changes in those aged 25 to 29 years (relative difference, −47.71% [95% CI, −71.16% to −22.06%]; relative change P = .001) and those aged 30 to 39 years (relative difference, −38.64% [95% CI, −55.64% to −15.25%]; relative change P = .004).
Table. Changes in Age-Adjusted Incidence and Mortality Rates Associated With the Introduction of Human Papillomavirus Vaccination.
| Age, y | Age-adjusted rate per 100 000 populationa | Change from 2001-2005 to 2010-2017b | Relative difference in % changec | |||
|---|---|---|---|---|---|---|
| 2001-2005 | 2010-2017 | Estimate (95% CI), % | P value | Estimate (95% CI) | P value | |
| Incidence | ||||||
| 15-24 | 0.86 | 0.54 | −37.70 (−42.24 to −32.75) | <.001 | NA | NA |
| 25-29 | 6.08 | 5.1 | −16.16 (−19.45 to −12.69) | <.001 | −21.53 (−27.09 to −15.82) | <.001 |
| 30-39 | 13.16 | 12.1 | −8.03 (−9.9 to −6.12) | <.001 | −29.66 (−34.6 to −24.38) | <.001 |
| Mortality | ||||||
| 15-24 | 0.08 | 0.04 | −43.35 (−59.38 to −20.5) | .002 | NA | NA |
| 25-29 | 0.57 | 0.59 | 4.36 (−10.02 to 22.18) | .58 | −47.71 (−71.16 to −22.06) | .001 |
| 30-39 | 1.95 | 1.86 | −4.71 (−9.84 to 0.80) | .09 | −38.64 (−55.64 to −15.25) | .004 |
Abbreviation: NA, not applicable.
The rate is the number of events per 100 000 population (age adjusted). The number of events over the study period of 2001 through 2017 were as follows: 2519, 9564, and 43 686 incident cases of cervical cancer and 212, 998, and 6508 cervical cancer deaths in those aged 15 to 24, 25 to 29, and 30 to 39 years, respectively.
Sensitivity analyses using data from January 2016 through December 2017 as the postvaccination period gave similar results, although with larger estimated effect sizes for the changes in cervical cancer incidence and mortality among young women and girls (incidence: those aged 15-24 years, −50.63% [95% CI, −57.62% to −43.58%]; 25-29 years, −18.14% [95% CI, −23.04% to −13.11%); 30-39 years, −2.91% [95% CI, −5.9% to 0.13%]; mortality, 15-24years, −65.83% [95% CI, −86.19% to −43.00%]; 25-29 years, 0.70% [95% CI, −18.06% to 22.89%]; 30-39 years, 0.36% [95% CI, −6.59% to 7.68%]). The relative difference in percentage change for these sensitivity analyses (%15-24 − %25-29 and %15-24 − %30-39) showed values significantly less than 0 (P < .001) for all incidence and mortality analyses. The parallel trends assumption was also satisfied for these analyses.
The estimates are from the quasi-experimental analyses, similar to a difference-in-differences analyses. The estimates represent the difference between the percentage change from January 2001 through December 2005 to January 2010 through December 2017 for those aged 15 to 24 years relative to the comparison groups (those aged 25-29 and 30-39 years), calculated as (%15-24 − %25-29) and (%15-24 − %30-39), respectively. To test whether the changes could be attributable to preexisting trends, we evaluated whether the relative changes in incidence and mortality were similar prior to human papillomavirus vaccine initiation in 2006. This parallel trends assumption was considered satisfied for all analyses (eMethods in the Supplement for details).
Figure. Temporal Patterns in Cervical Cancer Incidence and Mortality.
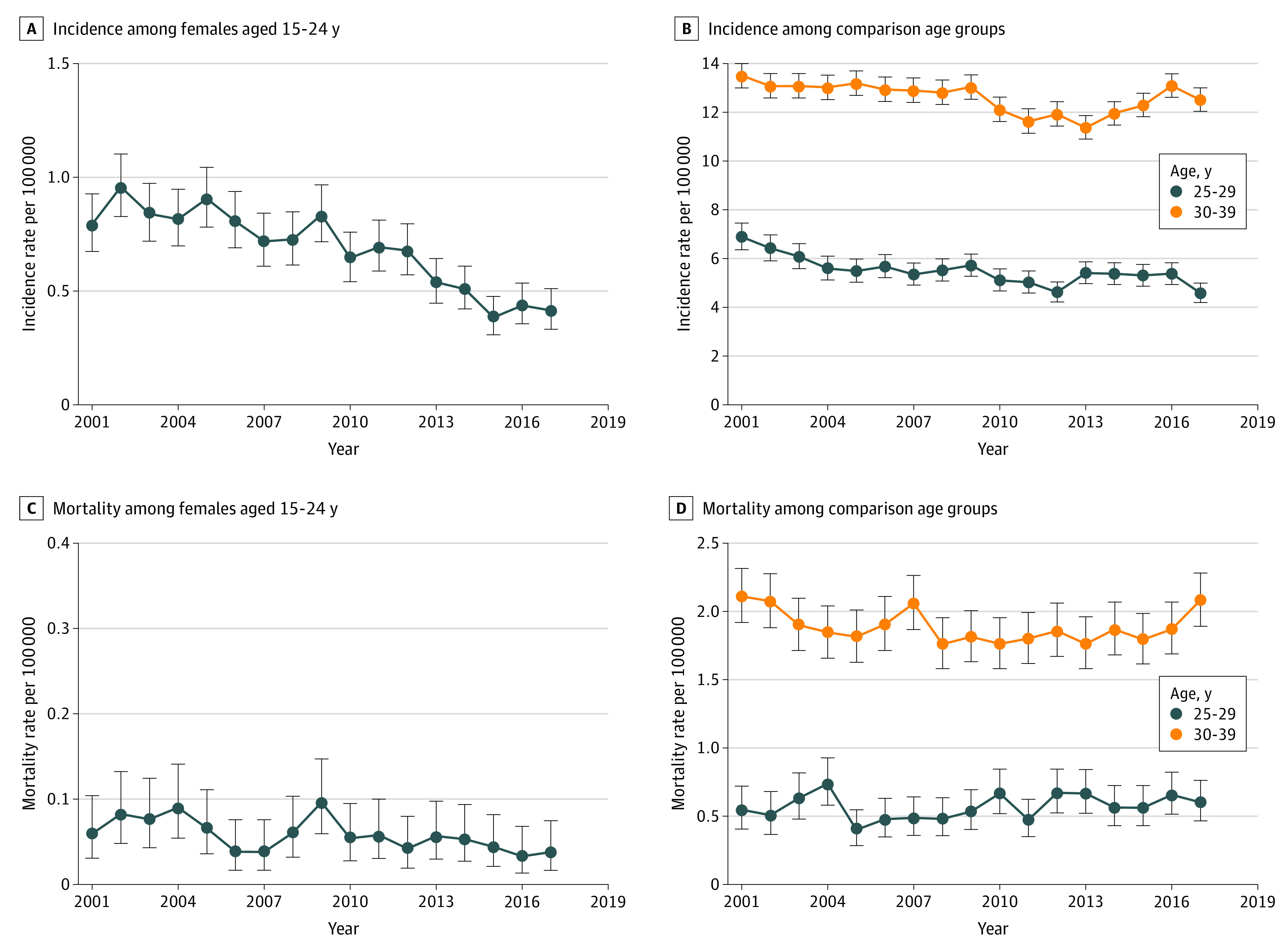
Cervical cancer incidence and mortality rates from 2001 through 2017 among girls and women aged 15 to 39 years are shown, separated by age subgroups. Data sources: Combined Surveillance, Epidemiology, and End Results and National Program of Cancer Registries databases (incidence) and National Center for Health Statistics (mortality).
Discussion
These nationwide data showed decreased cervical cancer incidence and mortality among women and girls aged 15 to 24 years after HPV vaccine introduction. The decreases were greater than changes in those aged 25 to 29 years and 30 to 39 years, suggesting possible associations with HPV vaccination. Vaccination against HPV prevented precancerous lesions in randomized clinical trials and was associated with decreased cervical cancer incidence in a Swedish observational study.3,4 Epidemiological US data have shown decreased cervical cancer incidence after vaccine implementation in women and girls aged 15 to 24 years but not older women.1,2 Thus, the current study adds to knowledge by quantitatively comparing changes in cervical cancer incidence by age-based vaccine eligibility and providing suggestive evidence for vaccine-associated decreases in cervical cancer mortality.
This study is limited by its ecological design. Changes in screening recommendations and practices, teenage sexual behaviors, and safer sex practices could also decrease cervical cancer incidence and mortality. However, screening rates decreased in young women and girls following changes in screening recommendations in 2009.5 Furthermore, despite decreased teenage sexual activity and increased condom use over recent decades, changes during the study period were small and unlikely to lead to large relative changes in cervical cancer incidence or mortality.6 Comparison groups were based on ages, which carry differing cervical cancer risks. Additionally, information regarding individual vaccination status was lacking, and some women older than 25 years were likely vaccinated. Finally, while the decreased cervical cancer mortality associated with HPV vaccination may translate to older age groups as HPV-vaccinated cohorts age, the number of deaths and hence the number of potentially averted deaths in young women and girls was small. While long-term prospective data are necessary to validate these findings, efforts to further improve vaccination uptake remain important.
eMethods.
eReferences.
References
- 1.Guo F, Cofie LE, Berenson AB. Cervical cancer incidence in young US females after human papillomavirus vaccine introduction. Am J Prev Med. 2018;55(2):197-204. doi: 10.1016/j.amepre.2018.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mix JM, Van Dyne EA, Saraiya M, Hallowell BD, Thomas CC. Assessing impact of HPV vaccination on cervical cancer incidence among women aged 15-29 years in the United States, 1999-2017: an ecologic study. Cancer Epidemiol Biomarkers Prev. 2021;30(1):30-37. doi: 10.1158/1055-9965.EPI-20-0846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.FUTURE II Study Group . Quadrivalent vaccine against human papillomavirus to prevent high-grade cervical lesions. N Engl J Med. 2007;356(19):1915-1927. doi: 10.1056/NEJMoa061741 [DOI] [PubMed] [Google Scholar]
- 4.Lei J, Ploner A, Elfström KM, et al. HPV vaccination and the risk of invasive cervical cancer. N Engl J Med. 2020;383(14):1340-1348. doi: 10.1056/NEJMoa1917338 [DOI] [PubMed] [Google Scholar]
- 5.Watson M, Benard V, Flagg EW. Assessment of trends in cervical cancer screening rates using healthcare claims data: United States, 2003-2014. Prev Med Rep. 2018;9:124-130. doi: 10.1016/j.pmedr.2018.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abma JC, Martinez GM. Sexual activity and contraceptive use among teenagers in the United States, 2011-2015. Natl Health Stat Report. 2017;104(104):1-23. Accessed May 27, 2021 https://www.cdc.gov/nchs/data/nhsr/nhsr104.pdf. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods.
eReferences.


