Abstract
BACKGROUND
During the surge in coronavirus disease 2019 (COVID-19) infections in early 2020, many medical organisations began developing strategies for implementing teleconsultation to maintain medical services during lockdown and to limit physical contact. Therefore, we developed a teleconsultation preoperative evaluation platform to replace on-site preoperative meetings.
OBJECTIVE
This study assessed the feasibility of a teleconsultation for preoperative evaluation and procedure-associated adverse events.
DESIGN
Implementation study.
SETTING
A tertiary care university hospital in Germany from April 2020 to October 2020.
PATIENTS
One hundred and eleven patients scheduled for elective surgery.
INTERVENTION
Patients were assigned to receive teleconsultation for preoperative evaluation and to complete a subsequent survey.
MAIN OUTCOME MEASURES
Primary endpoints were medical and technical feasibility, user satisfaction and time savings.
RESULTS
For 100 out of 111 patients, telepreoperative consultations allowed for adequate perioperative risk assessment, patient education and also for effective collection of legal signatures. For six patients (5.4%), consultations could not be started because of technical issues, whereas for five patients (4.8%), clearance for surgery could not be granted because of medical reasons. A clear majority of anaesthetists (93.7%) rated the telepreoperative evaluations as equivalent to on-site meetings. The majority of the patients considered teleconsultation for preoperative evaluation as convenient as an on-site meeting (98.2%) and would choose a teleconsultation again (97.9%). Median travel time saved by patients was 60 min (Q1 40, Q3 80). We registered one adverse event: we detected atrial fibrillation in one patient only immediately prior to surgery.
CONCLUSION
Telepreoperative evaluations are medically and technically feasible, yielding high satisfaction rates on both sides. However, regarding patient safety, not every patient is equally well suited. Overall, implementation of teleconsultation for preoperative evaluation into clinical routine could help maintain medical care during the COVID-19 pandemic.
TRIAL REGISTRATION
NCT04518514, ClinicalTrials.gov
Introduction
During the coronavirus disease 2019 (COVID-19) pandemic, many entities and organisations have swiftly implemented teleconsultation to maintain medical services during lockdown or to limit physical contact during consultations. However, these approaches frequently rely on proprietary software that was not developed for the highly sensitive field of medical services. We investigated strategies through which teleconsultation could be properly established and its benefits harnessed for the field of anaesthesiology.
We developed considerable expertise with implementation of teleconsultation in acute care,1–4 and given the current pandemic, noticed an obvious need for remote preoperative evaluation. Each anaesthesiological procedure requires a comprehensive preoperative evaluation, conducted by an experienced anaesthetist.5 The anaesthetist surveys the medical history, carries out a physical examination, and assesses individual perioperative risks.6 The anaesthetist explains the exact procedure together with any related risks and possible complications. In most European countries, the patient is required to agree to the proposed procedures by signing an informed consent form.7
On-site meetings often carry significant burdens in terms of waiting and travel time for each patient.8 In addition, employees often must take time off on a workday to attend their appointment, and that may have financial implications. The coronavirus pandemic has further hampered in-person preoperative evaluation through the effects of widely issued travel restrictions and increased risk of infection. Evaluation of young patients without preexisting morbid conditions can be achieved in a timely manner. Preoperative evaluation of older, multimorbid patients is frequently hampered by the absence of required examinations. Patients must often reschedule, get in touch with their general practitioners, or make appointments with specialists before valid perioperative risk assessments can be made. For both groups, a televisual approach to preoperative evaluation may offer benefits.
Only a few studies have investigated preoperative teleconsultation. Wong et al.9 conducted a pilot study in which the physician was located in a clinic while the patient was in a telecommunication centre in a remote region. Although this investigation supported the feasibility of such an approach with high satisfaction rates, the patient still had to travel to a remote facility. Mullen-Fortino et al.10 introduced an additional teleconsultation appointment prior to the conventional on-site presurgical assessment, which recorded high patient satisfaction and reduced time spent at the on-site meeting. However, they did not assess a stand-alone teleconsultation approach, replacing the in-person consultation.
In the United States, a recently published study by Kamdar et al.11 showed for the first time that preoperative consultations could be conducted via teleconsultation only, using Zoom (Zoom Communications, Inc., San Jose, California, USA) at first and then another videoconference tool linked to the electronic medical record (EMR) system. They showed high patient satisfaction and cost savings, as well as low case cancellation rates.
At the beginning of the COVID-19 pandemic, the American College of Surgeons and the American Society of Anesthesiologists called for the implementation of teleconsultation into preoperative patient evaluations.12 Following this call, we developed a teleconsultation preoperative evaluation platform called TARA (Telemedical Anamnesis and Risk Assessment) and this study reports its implementation at a major German university hospital. The aim of this study was to assess the medical and technical feasibility of teleconsultation for preoperative evaluation and also procedure-associated adverse events.
Methods
Study design and ethics
We conducted a single-centre implementation study, designed according to the StaRi criteria13 (Supplemental Material). Software development was initiated in December 2019 but then accelerated with the beginning of the COVID-19 pandemic in order to maintain medical services and to reduce physical contact.
The study was approved by the ethics committee of the RWTH Aachen University Hospital (EK 389/19) on 16 December 2019 and complies with the Declaration of Helsinki on ethical principles for medical research involving human subjects. Written informed consent was obtained from every patient.
The trial was registered on ClinicalTrials.gov and is available under the reference number NCT04518514. We filed written data analysis and statistical plans with the institutional review board before accessing the data.
The study was conducted at the Department of Anaesthesiology of the RWTH Aachen University Hospital, a tertiary care university hospital in Germany, which annually performs about 23 000 anaesthetic procedures.
Participants
Patients undergoing elective surgery who met the eligibility criteria were asked to participate in our study. To be eligible, patients were required to be of legal age (≥18 years); have been assigned an ASA I/II classification based on the ASA classification system; have elective surgery scheduled at least 14 days in the future; and have access to a Windows 10-based personal computer with a webcam. Exclusion criteria included language or cognitive barriers, high-risk procedures with need for postoperative ICU stay and acute infection with required auscultation.
Intervention
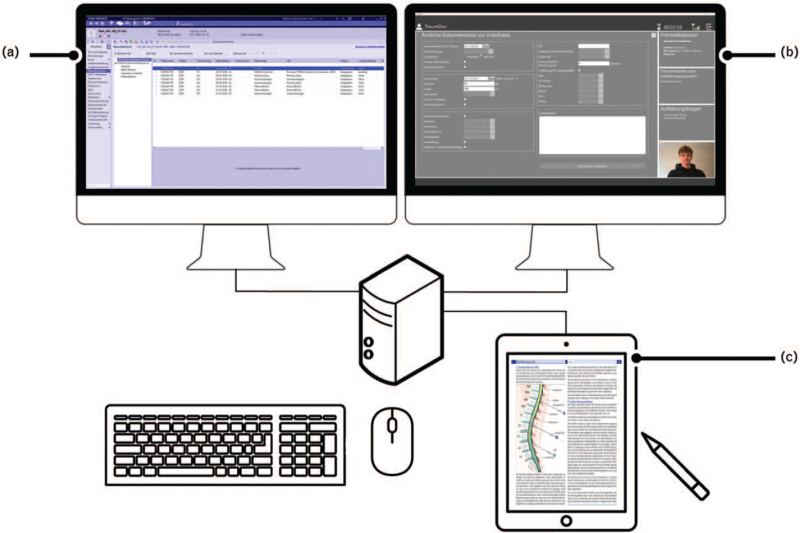
Eligible patients were asked by phone whether they would like to participate in telepreoperative evaluations. Those who agreed received an individual username, password and a download link for the software TARA (Telemedical Anamnesis and Risk Assessment; Docs in Clouds Telecare GmbH, Aachen, Germany). For the tele-anaesthetist, a suitable workplace was set up enabling videotelephony, access to the hospital information system (HIS) and documentation (Fig. 1).
Fig. 1.
The tele-anaesthesia workplace in the hospital enables access to the hospital information system (a), software support for preoperative evaluation (b), and documentation of the patient's medical history and performed education on a touch screen (c)
Before the joint consultation, patients had the opportunity to inform themselves extensively about the planned anaesthesiological procedures and to complete medical history forms embedded in the software in PDF format. After completion, the answers were sent to the anaesthetist. On the day of appointment, a joint video conference took place in which the parties reviewed the documents completed so far, and if necessary, supplemented the information and provided further explanation. Using a high-resolution touchscreen and a stylus, anaesthetists could highlight and make annotations complementing their explanations of the procedures. Any remarks added to the PDF were simultaneously mirrored within the same PDF document on the patient's screen. After the patient gave consent for the anaesthesia and the anaesthetist gave approval, the patient and doctor signed the shared document. The final document was provided read-only to both parties and transferred into the HIS. The abovementioned software features provided by TARA can be divided into usability, interoperability and legal issues (Table 1). The latter included technical features in order to fulfil the same legal and privacy standards as an in-person consultation.
Table 1.
Features provided by the telemedicine software enabling adequate patient education
| Usability features | Interoperability features | Legal and privacy features |
| Patient information regarding anaesthesia can be given in advance | Anaesthetist has simultaneous access to the electronic health record | Platform provides transport-encrypted direct peer-to-peer connections |
| Medical history form can be completed by the patient prior to the consultation | Platform is interfaced to hospital information system | Platform uses certified video-consultation (Internet Privacy Standard) |
| Patient and anaesthetist communicate through videotelephony | Signature is drawn with mouse or digital pen | |
| Medical history and information sheet are jointly edited by the patient and the anaesthetist | Patient's live signature is visible to the doctor | |
| Patient needs only a standard computer, no special equipment | Further IT-derived evidence of conducted education (IP address, time stamps, etc.) is automatically recorded |
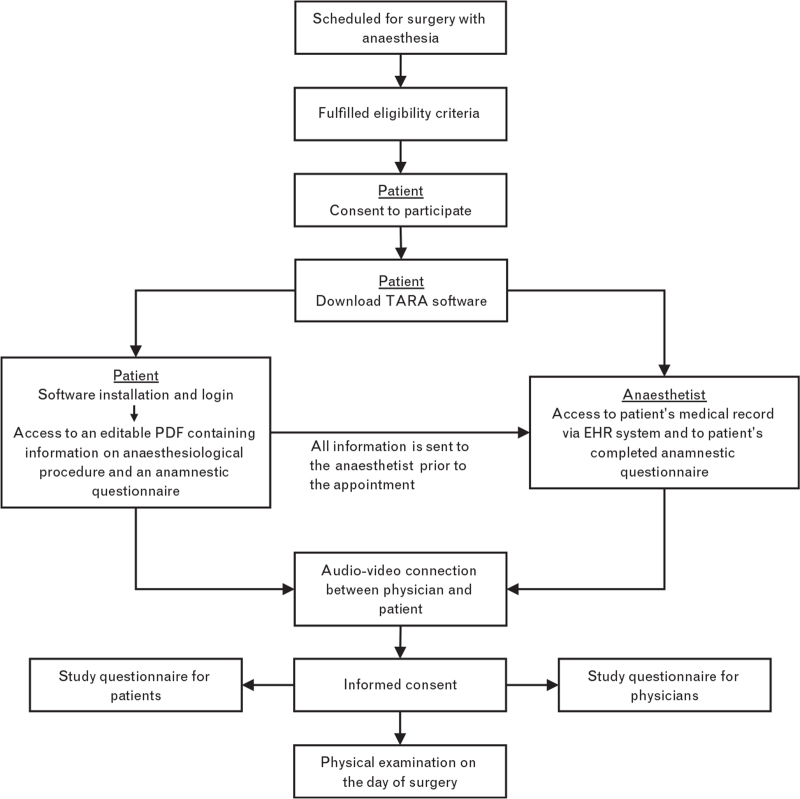
For evaluation purposes, participants were asked to complete study questionnaires. The questionnaires were based on a previously published study1 and used a four-point Likert scale with a ‘no answer’ option. Patients were asked to report the estimated travel time saved. Physical examinations, if required, took place on the day of surgery (Fig. 2).
Fig. 2.
Visualisation of the process for telemedical information and risk assessment of a patient within the framework of our study
Outcomes
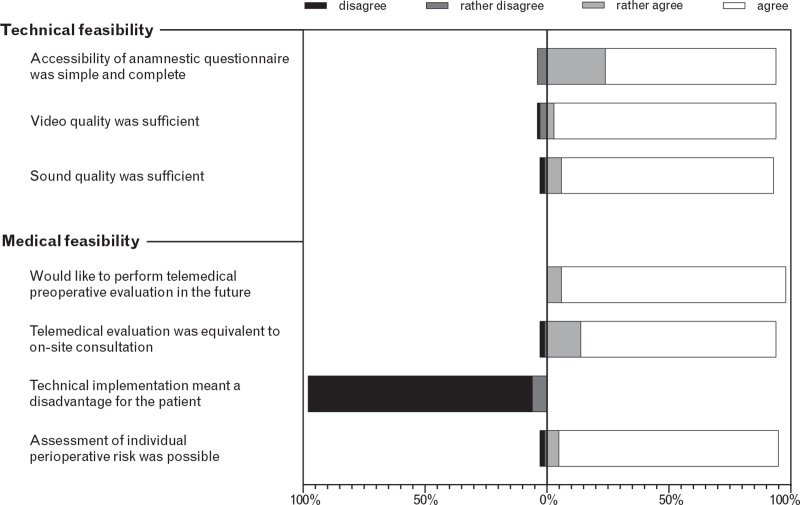
Primary endpoints included medical and technical feasibility. To assess medical feasibility, we collected data on adverse perioperative events, including unrecognised disorders and rescheduling of surgery because of insufficient telepreoperative evaluation, and measured whether anaesthetists were able to assess the individual perioperative risk during the teleconsultation. Furthermore, we measured the willingness to use the technology in the future and its equivalence with on-site consultation. The measured outcomes were evaluated by a questionnaire four-point Likert scale (Fig. 3).
Fig. 3.
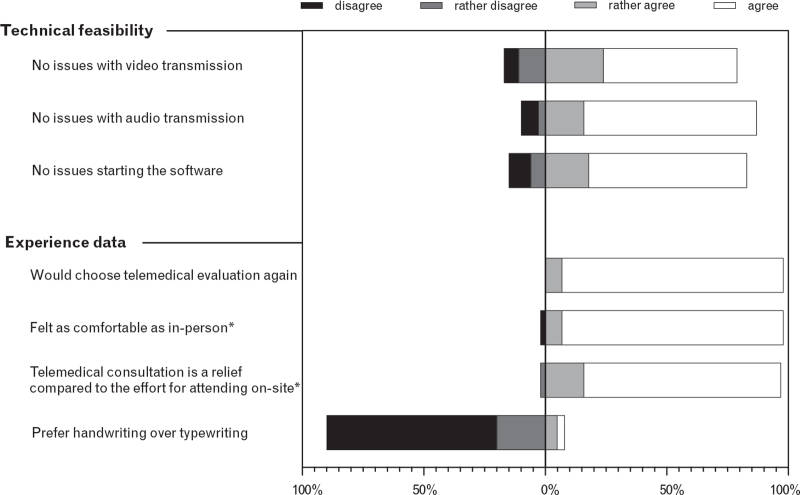
Results of the questionnaire filled out by participating anaesthetists
Technical feasibility refers to the successful completion of the consultation as well as attaining or exceeding established medical standards for an in-person interview.14 To assess technical feasibility, we collected data on successful establishment of an audiovisual connections, technical problems that led to termination of the teleconsultation, and also operational readiness of software features (Table 1). For analytical purposes, we measured accessibility of the anamnestic questionnaire, problems concerning the audiovisual connection, and issues with booting the software (Fig. 4). We also assessed patient acceptance and satisfaction and time savings with consecutive study questionnaires. To evaluate acceptance and satisfaction, we measured the willingness to choose teleconsultation again, relief and convenience compared with on-site evaluation, and preference in terms of handwriting or typewriting. The measured outcomes were evaluated by a questionnaire four-point Likert scale. For two items in the questionnaire (see Fig. 4), we included only patients who already had an on-site preoperative evaluation for other reasons to guarantee comparability. Further details on variables and assessment tools can be found in the supplement.
Fig. 4.
Results of the questionnaire filled out by participating patients
Sample size
We calculated the required sample size for this study according to Viechtbauer et al.15 Therefore, the following potential problems were identified in advance and the likely rate of occurrences were estimated based on six pilot patients:
-
(1)
The telepreoperative evaluation could be completed but adverse events occurred perioperatively (unrecognized disorders emerged) (3%)
-
(2)
The procedure had to change from teleconsultation to in-person education because of technical or medical reasons (3%)
-
(3)
The patient experienced operating difficulties (5%)
The required sample size was calculated separately for each scenario as followed:
n = sample size, x = number of patients for which problem occurred,
π = probability of occurrence, and P (x > 0) = γ
With 99 patients to be enrolled we could be sure to reach at least a 95% confidence level in each scenario.
Statistical methods
We performed all statistical analyses using IBM SPSS Statistics (Version 26). Categorical and ordinal variables were summarised as count (percentage) and continuous variables as mean ± SD or median [interquartile range].
Results
We sent 111 patients a hyperlink for downloading the software via e-mail. In six cases (5.4%), the consultation failed because of technical issues. In 105 cases (94.6%), the consultation started as scheduled. Study participants were 33 ± 7.5 years old and were recruited from various clinical specialities (Table 2). Ninety-seven patients completed our questionnaire (Supplemental Figure 1). In addition, 96 responses from anaesthetists were collected.
Table 2.
Characteristics of study participants
| Variables | ||
| Age (years) | ||
| 33 ± 7.5 | ||
| Sex | ||
| Male | 25 | 25% |
| Female | 75 | 75% |
| ASA score | ||
| ASA I | 44 | 44% |
| ASA II | 56 | 56% |
| Surgery classification | ||
| Class I | 28 | 28% |
| Class II | 21 | 21% |
| Class III | 13 | 13% |
| Nondisclosed | 38 | 38% |
| Clinical specialty | ||
| Obstetrics | 38 | 38% |
| Gynaecology | 15 | 15% |
| Trauma surgery | 11 | 11% |
| Urology | 10 | 10% |
| Abdominal surgery | 7 | 7% |
| Oral and maxillofacial surgery | 6 | 6% |
| Plastic surgery | 4 | 4% |
| Otolaryngology | 4 | 4% |
| Reproduction medicine | 4 | 4% |
| Vascular surgery | 1 | 1% |
Data are given as mean ± SD or n (%).
The majority of anaesthetists rated telepreoperative evaluation as equivalent to an on-site meeting (93.7%), and expressed interest in continuing the practice in the future (98.0%), responding ‘rather agree’ or ‘agree’. In addition, 94.8% claimed that they were able to assess the individual perioperative risk during telepreoperative evaluation, responding ‘rather agree’ or ‘agree’. From the anaesthetists’ perspective, image, sound and video quality were considered sufficient in almost all consultations (more than 90% responded ‘rather agree’ or ‘agree’, Fig. 3).
Fifty-seven patients already had an on-site preoperative evaluation for other reasons. The majority of these patients considered telepreoperative evaluation as convenient as an on-site meeting (98.2% responded ‘rather agree’ or ‘agree’, Fig. 4).
Starting the software was largely unproblematic (82.4% responded ‘rather agree’ or ‘agree’). In these cases, the video connection was usually stable and the audio connection almost never caused problems. Patients saved a median of 60 min [IQR 40 to 80] in travel time. A waiting time while idle could also occur during the teleconsultation appointment, and was therefore, not accounted for in these estimates. Of the patients, 89.7% preferred completing the anamnestic questionnaire digitally over a paper-based version and 97.9% of the patients would choose the video telephony again (Fig. 4).
In five cases (4.8%), the preoperative evaluation could not be completed as important preliminary examinations were missing. In two cases (1.9%), the teleconsultation appointment revealed undisclosed genetic diseases; one patient needed pulmonary function testing prior to surgery; one patient (1.0%) exhibited psychiatric symptoms; and another patient was classified as ASA III during the appointment, and therefore, excluded (see inclusion criteria). As a consequence, two surgical interventions (1.9%) had to be postponed as they would have been in an on-site meeting. In addition, one patient had previously undiagnosed atrial fibrillation, only noticed on the day of surgery. However, this complication did not have negative consequences for the planned surgery. Thus, there were no procedure-associated adverse events or complications.
Discussion
This study was the first field trial of teleconsultation for preoperative evaluation at a major university hospital in Europe, using software specifically developed for this purpose. We demonstrated feasibility for ASA I to II patients with simultaneous consideration of legal certainty and privacy concerns. From a technical point of view, consultations could be conducted in 94.6% of the patients, meeting the predefined criteria for technical feasibility. In 94.8% of the cases, the anaesthetist could assess and optimise the perioperative risk, and obtain informed consent, proving medical feasibility. In addition, no procedure-associated adverse events or complications occurred. Participating patients and anaesthetists perceived the procedure as beneficial and convenient (more than 93% responded ‘rather agree’ or ‘agree’) with a median time saving of 60 min for patients.
In our study, teleconsultation for preoperative evaluation was rated from the participating anaesthetists as equivalent to the on-site meeting, having no influence on postoperative outcome. However, the main difference between remote and in-person risk assessment remains the limited capability for medical examination given the lack of on-site medical equipment and assistants. One patient was found preoperatively to have undiagnosed atrial fibrillation that might have been detected in an on-site evaluation when the pulse was taken. However, even in ordinary preoperative examinations, preexisting diseases occasionally remain undetected. Phillips et al.16 investigated the detection of new or unknown medical conditions during preoperative medical examination in patients undergoing ophthalmic surgery. Retrospectively, they identified new or unstable conditions in 40% of the patients, of which half were uncovered during preanaesthesia evaluation. Limiting factors to consider for the relevance of these data in our context are the study's elderly population (more than 50% ≥75 years) and the fact that a telepreoperative evaluation can also be based on physical examination and test results. This information would have to be collected prior to the teleconsultation, which could be done by the patient's general practitioner or by implementation of further smart health devices. However, it seems obvious that not all patients are equally well suited for telepreoperative evaluation. In 4.8%, we had to reschedule because of missing preliminary examinations, which is bothersome but occurs also on a regular basis in on-site consultation.
Due to the higher bandwidth requirements, video connections were less stable than audio connections. In one case, the latency was so great that a proper consultation was not possible. In three cases, video connections could not be established because of problems with the patients’ cameras. Strategies to ensure prior testing of the required equipment by the patient should be implemented.
Regarding overall patient satisfaction, we validated earlier findings from teleconsultations in series with in-person appointments.9,10,17 Patient acceptance was high for televisual education, even though a quarter of the patients were not accustomed to video chats in their everyday lives.
In contrast to other studies, we asked patients directly for their travel time and thus, obtained an accurate picture of saved travel time for patients. Median travel time was 60 min both ways, plus waiting time in the hospital. A previously published study conducted at a German university hospital8 showed a mean waiting time of 58.6 ± 30.3 min. However, we conducted this study in a large city (250 000 inhabitants and close to the largest metropolitan region in Germany). In rural regions, the benefits should be even greater because of longer distances to hospitals.9,11
In contrast to the recently published study by Kamdar et al.11 in which more than 50% of the patients were classified as ASA III or IV, we exclusively studied ASA I and II patients. In these patients, the risk of overlooking important medical findings that would be detected during an on-site meeting might be considered minimal. However, we identified key questions that must be asked during every preoperative teleconsultation that were related to the New York Heart Association classification, sports activities, and oedema in the lower extremities. Our study was limited to younger patients, especially those without significant preexisting conditions. But televisual education may offer additional benefits for older patients who do have relevant preexisting conditions. Re-admissions caused by missing results are inconvenient for all parties involved. However, they are sometimes necessary when examination findings that are indispensable for risk assessment are missing, an avoidable problem in many cases.
For unambiguous patient identification, government-issued photo identity (ID) in conjunction with the individual's date of birth is widely considered sufficient. IP address tracking is inferior to photo ID, as operating out of a local network might result in one joint public IP address. Using the patient's personal e-mail address added an additional safety layer to the identification process.
Patients signed declarations of interest via mouse or digital pen, and those documents were then time stamped to avoid later alterations. Furthermore, if a change was necessary, both patient and doctor, in the same consultation, were required to amend the document, preventing unilateral changes. Previously published studies from the United States did not include the patient's signature.
According to German law (Federal Code of Law § 630 h paragraph 2, sentence 1 in conjunction with § 630 e), the burden of proof for properly conveying risk information and for obtaining informed consent lies with the physician. After patients have been informed, their consent can be collected in writing, orally, or through conclusive behaviour. As a signed consent form includes written information about the content of the preoperative evaluation, written consent has the greatest evidential value and is the best proof the consultation was conducted properly.
There are limitations to be considered with regard to generalisability of our findings. First, no control group was surveyed. Noninferiority of telepreoperative evaluation compared with on-site evaluation needs to be investigated in further research. For this purpose, we propose a randomised controlled trial, allocating patients to either an in-person or a telepreoperative evaluation with subsequent comparison of those two groups. Second, the study used a desktop application that runs exclusively on Windows 10 computers, which excluded some patients and caused problems because of the software installation. A future version of TARA should be web-based and platform-independent. Without the prerequisite of a specific operating system or the installation of a desktop application, together with the abovementioned option for testing camera and microphone on the patient's device prior to the consultation, we expect the technical feasibility to be above 95%. In our study, patient information included only text and pictures. In the future, inclusion of videos and animations might reduce anxiety18–21 and save time.19 In addition, telemedicine may add the additional benefit of electronic patient records and streamlined workflows in places where electronic records have not yet been implemented, resulting in time saving for the physician.
We conducted this trial from an anaesthesiological perspective but the system could be easily transferred into other settings. As the patient's consent is documented by signature on both sides, high legal demands are met. Therefore, surgeons as well as interventionists will have the opportunity to employ the infrastructure established by our group to acquire legally binding informed consent from their patients remotely. For this purpose, the anamnestic questionnaire with information concerning the anaesthesiological procedure, embedded in the software, could be easily replaced by any other PDF.
Implementing telepreoperative evaluations may have a profound impact on anaesthetists’ response to the COVID-19 pandemic. Given the nature of this infectious virus, the most effective means of limiting its spread is reducing physical contact to an absolute minimum. Due to the remote nature of the consultation, asymptomatic physicians that have tested positive for SARS-CoV-2 are still able to support their colleagues while quarantined.22 In addition, patients’ exposure and infection risk are minimised (Supplemental Table).
Conclusion
We have shown that telepreoperative education and risk assessment are feasible, do not require compromise in terms of its legal certainty and meet high data privacy standards. The individual perioperative risk could be assessed and informed consent obtained in most cases. In addition, no procedure-associated adverse medical events were attributed to the technical implementation. For the patient, the televisual approach resulted in a reduced time burden and high satisfaction rates were reported on both sides. As we included only ASA I and II patients, further studies should address whether telepreoperative evaluation is also suitable for ASA III and IV patients and for patients for whom a thorough physical examination is indispensable.
Supplementary Material
Supplementary Material
Acknowledgements relating to this article
Assistance with the study: none.
Financial support and sponsorship: support was provided solely from institutional and departmental sources.
Conflicts of interest: MC is shareholder and CEO of Docs in Clouds Telecare GmbH, Aachen, Germany. RR is shareholder of Docs in Clouds Telecare GmbH, Aachen, Germany. AF is CMO of Docs in Clouds Telecare GmbH, Aachen, Germany. LM has a 25% position at Docs in Clouds Telecare GmbH, Aachen, Germany. All other authors declare they have no conflicts of interest.
Presentation: none.
Footnotes
Published online 19 October 2021
Supplemental digital content is available for this article.
References
- 1.Follmann A, Ohligs M, Hochhausen N, et al. Technical support by smart glasses during a mass casualty incident: a randomized controlled simulation trial on technically assisted triage and telemedical app use in disaster medicine. J Med Internet Res 2019; 21:e11939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Czaplik M, Bergrath S, Rossaint R, et al. Employment of telemedicine in emergency medicine. Clinical requirement analysis, system development and first test results. Methods Inf Med 2014; 53:99–107. [DOI] [PubMed] [Google Scholar]
- 3.Bergrath S, Czaplik M, Rossaint R, et al. Implementation phase of a multicentre prehospital telemedicine system to support paramedics: feasibility and possible limitations. Scand J Trauma Resusc Emerg Med 2013; 21:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marx GDM, Czaplik M, Balzer F, et al. Telemedicine in the four pillars of anaesthesiology - Position paper of The German Society of Anaesthesiology and Intensive Care Medicine (DGAI) and German Society of Telemedicine (DG Telemed). Anästh Intensiv Med 2019; 60:191–207. [Google Scholar]
- 5.De Hert S, Imberger G, Carlisle J, et al. Preoperative evaluation of the adult patient undergoing noncardiac surgery: guidelines from the European Society of Anaesthesiology. Eur J Anaesthesiol 2011; 28:684–722. [DOI] [PubMed] [Google Scholar]
- 6.Apfelbaum JL, Connis RT, et al. Committee on Standards and Practice Parameters. Practice advisory for preanesthesia evaluation: an updated report by the American Society of Anesthesiologists Task Force on Preanesthesia Evaluation. Anesthesiology 2012; 116:522–538. [DOI] [PubMed] [Google Scholar]
- 7.Eser A. Westerhäll L. Functions and requirements of informed consent in German law and practice. Patient's rights: informed consent, access and equality. Bern, Switzerland: Nerenius & Santérus Publishers; 1994. 235–253. [Google Scholar]
- 8.Kieninger M, Eissnert C, Seitz M, et al. Analyse und Möglichkeiten der Optimierung von Prämedikationsgesprächen an einem Universitätsklinikum. Der Anaesthesist 2018; 67:93–108. [DOI] [PubMed] [Google Scholar]
- 9.Wong DT, Kamming D, Salenieks ME, et al. Preadmission anesthesia consultation using telemedicine technology: a pilot study. Anesthesiology 2004; 100:1605–1607. [DOI] [PubMed] [Google Scholar]
- 10.Mullen-Fortino M, Rising KL, Duckworth J, et al. Presurgical assessment using telemedicine technology: impact on efficiency, effectiveness, and patient experience of care. Telemed J E Health 2019; 25:137–142. [DOI] [PubMed] [Google Scholar]
- 11.Kamdar NV, Huverserian A, Jalilian L, et al. Development, implementation, and evaluation of a telemedicine preoperative evaluation initiative at a major academic medical center. Anesth Analg 2020; 131:1647–1656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. American College of Surgeons ASoA, Association of periOperative Registered Nurses, American Hospital Association. Joint Statement Roadmap for Resuming Elective Surgery after COVID-19 Pandemic. In, 2020. Available at: https://www.asahq.org/about-asa/newsroom/news-releases/2020/04/jointstatement-on-elective-surgery-after-covid-19-pandemic. (Accessed 26 February 2021) [Google Scholar]
- 13.Pinnock H, Barwick M, Carpenter CR, et al. StaRI Group. Standards for reporting implementation studies (StaRI) statement. BMJ 2017; 356:i6795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.De Hert S, Staender S, Fritsch G, et al. Preoperative evaluation of adults undergoing elective noncardiac surgery: updated guideline from the European Society of Anaesthesiology. Eur J Anaesthesiol 2018; 35:407–465. [DOI] [PubMed] [Google Scholar]
- 15.Viechtbauer W, Smits L, Kotz D, et al. A simple formula for the calculation of sample size in pilot studies. J Clin Epidemiol 2015; 68:1375–1379. [DOI] [PubMed] [Google Scholar]
- 16.Phillips MB, Bendel RE, Crook JE, Diehl NN. Global health implications of preanesthesia medical examination for ophthalmic surgery. Anesthesiology 2013; 118:1038–1045. [DOI] [PubMed] [Google Scholar]
- 17.Applegate RL, 2nd, Gildea B, Patchin R, et al. Telemedicine preanesthesia evaluation: a randomized pilot trial. Telemed J E Health 2013; 19:211–216. [DOI] [PubMed] [Google Scholar]
- 18.Jlala HA, French JL, Foxall GL, et al. Effect of preoperative multimedia information on perioperative anxiety in patients undergoing procedures under regional anaesthesia. Br J Anaesth 2010; 104:369–374. [DOI] [PubMed] [Google Scholar]
- 19.Vogel H, Schaaf W, Jacob M. Video-assisted patient education in anesthesia: how do medical users assess the procedure? Anaesthesist 2018; 67:829–836. [DOI] [PubMed] [Google Scholar]
- 20.Lee A, Chui PT, Gin T. Educating patients about anesthesia: a systematic review of randomized controlled trials of media-based interventions. Anesth Analg 2003; 96:1424–1431. [DOI] [PubMed] [Google Scholar]
- 21.Roth-Isigkeit A, Ocklitz E, Brückner S, et al. Development and evaluation of a video program for presentation prior to elective cardiac surgery. Acta Anaesthesiol Scand 2002; 46:415–423. [DOI] [PubMed] [Google Scholar]
- 22.Hollander JE, Carr BG. Virtually perfect? Telemedicine for covid-19. N Engl J Med 2020; 382:1679–1681. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.