Abstract
Objectives
Infectious diseases are the most common cause of disease stigmatisation, which can lead to a denial of healthcare, education, housing and employment as well as physical violence. Such stigmatisation is common during pandemics. This study aimed to examine the social stigmatisation of COVID-19 among residents of Riyadh, Saudi Arabia.
Methods
A cross-sectional descriptive study was conducted in Riyadh in May 2020. Non-probability convenient sampling was used to recruit 847 participants through social media platforms, including WhatsApp. The data were analysed using descriptive statistics, the Pearson correlation coefficient and the chi-squared test were used along with a multiple linear regression model.
Results
There was a high level of stigma among 21% of the participants and an intermediate level in almost 49% of the participants. Low stigma was indicated among 30% of the study’s sample. A highly significant association existed between stigma, on the one hand, and older age groups, being married and lower levels of education, on the other.
Conclusion
Future awareness programmes should educate patients and their families about stigma as well as the consequences of stigmatising COVID-19. Stigma eradication policies and interventions should be implemented to avoid potentially harmful consequences for public health.
Keywords: Social stigma, COVID-19, Pandemic, Saudi Arabia
Advances in Knowledge
- This study found that COVID-19-related stigmatisation exists at moderate to high levels among more than two-thirds of the residents of Riyadh, Saudi Arabia.
- General knowledge about COVID-19 was not found to be associated with social stigma.
- The factors significantly associated with the high stigma scores among the studied sample were the following: old age, being married, low educational level, not working in the healthcare field, not being exposed to infection previously, high level of knowledge about preventive measures, low perceived susceptibility and high perceived severity of the disease.
Applications to Patient Care
- The findings of this study might guide health educators in designing educational campaigns that focus on perceived susceptibility, which was found to be significantly associated with low stigma towards COVID-19. Specifically, such campaigns should raise people’s awareness about the likelihood of becoming infected with COVID-19.
- Stigma eradication policies and interventions should be implemented to avoid potentially harmful public health consequences.
Stigma is defined as “a simplified, standardised image of the disgrace of certain people that is held in common by a community at large”.1 Stigmatisation of diseases is considered the foremost barrier deterring people from seeking treatment.2,3 In many instances, this is caused by the perceived risk of stigma outweighing the perceived benefit of healthcare-seeking behaviour.2 Infectious diseases have been considered the most common cause of disease stigmatisation.4
Historically, many infectious diseases have been stigmatised.5 A review of major studies in this area confirmed that there is a statistically significant relationship between newly emerging infectious diseases and stigma.5–8 The involved stigmatisation leads not only to denial of healthcare, education, housing and employment but also to physical violence.9 For example, the severe acute respiratory syndrome (SARS) epidemic resulted in a significant reduction in the public’s healthcare-seeking behaviour.10 After the Ebola and SARS outbreaks, social stigma was attached to healthcare workers, as people feared being infected by them. If a person is infected, the social stigma attached to the individual and those who live around them continues even after the quarantine period when there is no further risk of spreading the virus.8 Moreover, stigma has been commonly recorded during pandemic outbreaks.4
The COVID-19 pandemic has caused individual fear and community panic.11,12 This is considered a natural response to the rapidly changing and uncertain conditions in which people find themselves.9,13 This is particularly true for people who are more vulnerable to COVID-19, namely older people, immunocompromised people, family members of infected patients and residents of high-incidence areas as well as those with severe underlying medical conditions.14,15 Moreover, people’s fear of and anxiety about unknown/unexpected diseases provide a rationale for exclusion and rejection.14 For instance, the fear of COVID-19 gave rise to mutual discrimination in China (i.e. discrimination within the Asian/Chinese communities).15 All of this could lead to ‘social stigmatisation’ that makes an individual hide the disease to avoid discrimination, inhibits them from adopting healthy behaviours and prevents them from seeking healthcare.5,7,8 Some people who face social stigma as a result of COVID-19 are those of Asian descent, those who have travelled and healthcare practitioners.15
A health stigma and discrimination framework developed by Stangl et al. provided an approach for planning for and responding to health-related stigma.13 Their framework is comprehensive and applicable to a broad range of health conditions; it highlights how stigma feeds upon socio-ecological factors related to health and national economic status. The process can be divided into a series of phases, including drivers and facilitators, stigma ‘making’ and stigma manifestations, which affect the outcomes of health in society.13 Evidence has shown that the fear and stigmatisation related to previous epidemics, namely SARS and Ebola, led to negative consequences; this may also be the case if COVID-19 is similarly stigmatised.8
Stangl et al. recommended early intervention to reduce the public stigma of health conditions to reach optimal health and quality healthcare.13 It is extremely important to increase people’s knowledge about the disease, its prevention and its treatment to prevent social exclusion and reduce stigma.5 In addition to facilitating support by family and healthcare teams, knowledge improves the commitment to healthcare.3 This highlights the role of public health practitioners and health educators who need to intensify their efforts and use rapid and effective ways to raise community awareness.5 This is highly important during a pandemic in which stigmatisation can also affect healthcare practitioners and public health workers, undermining their efforts.4
With the ultimate aim of helping to minimise the public health consequences of stigmatisation during the latest pandemic, this study was conducted to examine the social stigmatisation of COVID-19 among Riyadh’s residents and the factors affecting it. Riyadh was chosen as the first location in a series of studies to assess and compare stigmatisation of COVID-19 across the country. It was chosen due to its status as the capital of Saudi Arabia, the country’s largest and most diverse city with more than seven million residents. The findings of this study are expected to help in understanding the stigma around COVID-19 to inform public health research and practices to eradicate it.
Methods
This research is part of a project to study the stigmatisation of COVID-19. In the first part of the project, a cross-sectional descriptive study was conducted in Riyadh, Saudi Arabia, in May 2020. Non-probability convenience sampling was used to recruit residents.
An electronic survey created with the help of Microsoft Forms (Microsoft Corp., Redmond, Washington, USA) was distributed via social media and WhatsApp groups. Only respondents who were residents of Riyadh and over 18 years of age were included, regardless of their gender, race or nationality. The study sample was estimated to consist of a minimum of 385 participants out of the total of more than five million adult residents of Riyadh.16 This number was estimated to have a confidence level of 95% and a real value within ±5%. On the whole, 886 people participated in the survey. Of these, 39 participants were excluded for being under 18 years old. Thus, the sample size was 847, raising the confidence level to 98% and ensuring a real value within ±4%.
The research instrument consisted of five sections: socio-demographic characteristics, knowledge, attitude, practice and stigmatisation. This article is focused on stigmatisation; the findings on knowledge, attitudes and preventive practices regarding COVID-19 have been published separately.17 However, data concerned with knowledge (symptoms, risk groups and preventive measures) and participants’ perceptions of severity and susceptibility were used to examine their correlations with stigma.
The socio-demographic characteristics and general data of the participants included age, gender, level of education, workplace, the existence of chronic diseases and personal experience(s) with COVID-19. Questions about public stigma towards COVID-19 patients were adopted from an unpublished stigmatisation tool developed by the team that worked on this research. The questions included in the questionnaire were intended to measure public attitudes towards stigma. Seven questions were included in this section, which asked about participant perceptions of the following: (1) whether people with COVID-19 have low personal hygiene; (2) whether people with COVID-19 deserve to get infected because of their lifestyle during the pandemic; (3) whether a person with COVID-19 is not as responsible as others; (4) whether people who have had COVID-19 previously are obligated to disclose this information; (5) whether the participant keeps a physical distance from people who have recovered from COVID-19; (6) whether the participant avoids socialising with people who have had COVID-19 even after the latter’s recovery; and (7) whether low-income individuals are the reason the infection is spreading. Questions were evaluated based on a five-point Likert scale ranging from 1–5, where 5 represented ‘strongly agree’ and 1 represented ‘strongly disagree’.18 The total possible score was 35 and was interpreted based on quartiles as follows: ≤18 = low stigma, 19–24 = intermediate stigma and >24 = high stigma.
The questionnaire was developed based on an extensive review of relevant literature and guidelines. It was translated from English to Arabic using the forward-backward method. The final Arabic questionnaire was tested for face validity by experts in the field of community medicine and public health which resulted in some minor modifications. Reliability and validity tests were run and two questions were removed. After removal of the two questions, all of the questions had a significant positive correlation with the total stigma score; the r-value was above 0.4 and Cronbach’s α was 0.73.
The data were analysed using JMP, Version 14.2 (SAS Institute Inc., Cary, North Carolina, USA). Descriptive statistics were used to represent socio-demographic characteristics, exposure to COVID-19 and stigmatisation of COVID-19. The Pearson correlation coefficient and Chi-squared test were used to assess the correlation between stigma and socio-demographic factors, exposure to COVID-19, perception and knowledge. A multiple linear regression model was performed to determine stigma predictors.
Ethical approval (IRB Number: 20-0176) was obtained from Princess Nourah Bint Abdulrahman University. An informed consent statement was displayed at the start of the survey, which briefed the participants on the aim of the study and the confidentiality of the data. The statement also informed them that the data about them would only be used for research purposes.
Results
A total of 847 adults in Riyadh were included in this study with 79% of the participants being female. The participants in the >35–45 years category formed the largest component (32%); 62% of the study sample were married and 68% had a college degree. Moreover, 54% were employed and only 26% worked in the healthcare field [Table 1]. The questions concerned with exposure revealed that 10% of the participants had been infected or knew someone who had been infected with COVID-19. Meanwhile, 3% of the participants knew someone who had died as a result of COVID-19. Only 5% of the participants had been in contact with a COVID-19 patient.
Table 1.
Socio-demographic characteristics of residents from the city of Riyadh, Saudi Arabia (N = 847)
| Characteristic | n (%) |
|---|---|
| Gender | |
| Female | 673 (79) |
| Male | 174 (21) |
| Age group in years | |
| 18–25 | 207 (24) |
| >25–35 | 219 (26) |
| >35–45 | 270 (32) |
| >45–60 | 131 (15) |
| >60 | 20 (2) |
| Marital status | |
| Married | 524 (62) |
| Not married | 323 (38) |
| Education | |
| Less than a college degree | 121 (14) |
| College degree | 577 (68) |
| Postgraduate degree | 149 (18) |
| Working status | |
| Working | 457 (54) |
| Not working | 338 (40) |
| Retired | 52 (6) |
| Are you a health practitioner? | |
| Yes | 217 (26) |
| No | 630 (74) |
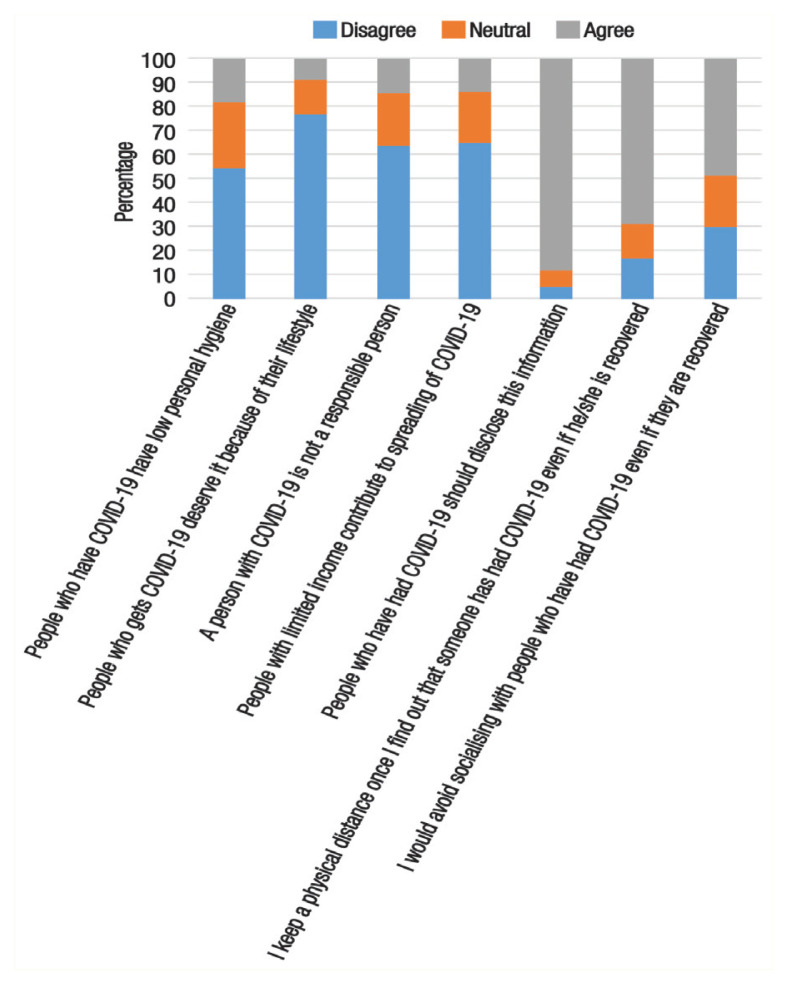
The study revealed a high level of stigma among 21% of the participants and an intermediate level in 49%of the participants. Low stigma was indicated among 30% of the study sample. The majority of the sample (69%) maintained a physical distance from people who had recovered from COVID-19 infection and 88% agreed that people who have had COVID-19 should disclose this information. Almost half of the participants would avoid socialising with people who have had COVID-19 even if the latter had recovered (49%) [Figure 1].
Figure 1.
Percentage of the responses of residents in Riyadh, Saudi Arabia, to statements regarding COVID-19 stigmatisation (N = 847).
Strong associations were found between stigma towards COVID-19 and many of the included factors. There was a highly significant association between stigma and older age groups. None of those aged 60 years or above had low stigma scores and 30% of them had a high level of stigma (P <0.001). Stigmatisation scores were significantly higher among individuals who were married than among those who were not (26% versus 12%, respectively; P <0.001). Stigmatisation was also higher among participants with lower education levels than those with higher education levels (35% versus 18%, respectively; P <0.003) and among those who did not work as health practitioners than those who did (23% versus 15%, respectively; P <0.001). Low stigma was found to be significantly more prevalent among those who had been infected or knew someone who had been infected by COVID-19 (41% versus 29%, respectively; P <0.010) [Table 2].
Table 2.
Factors influencing COVID-19 stigmatisation among residents in Riyadh, Saudi Arabia (N = 847)
| Characteristic | Level of stigmatisation n (%) | P value | ||
|---|---|---|---|---|
| High stigma | Intermediate stigma | Low stigma | ||
| Gender | 0.900 | |||
| Female | 140 (21) | 331 (49) | 202 (30) | |
| Male | 37 (21) | 83 (48) | 54 (31) | |
| Age group in years | <0.001 | |||
| 18–25 | 26 (13) | 98 (47) | 83 (40) | |
| >25–35 | 41 (19) | 93 (42) | 85 (39) | |
| >35–45 | 67 (25) | 144 (53) | 59 (22) | |
| >45–60 | 37 (28) | 65 (50) | 29 (22) | |
| >60 | 6 (30) | 14 (70) | 0 (0) | |
| Marital status | <0.001 | |||
| Married | 138 (26) | 259 (49) | 127 (24) | |
| Not married | 39 (12) | 155 (48) | 129 (40) | |
| Education | <0.003 | |||
| Less than a college degree | 42 (35) | 53 (44) | 26 (21) | |
| College degree | 108 (19) | 288 (50) | 181 (31) | |
| Postgraduate degree | 27 (18) | 73 (49) | 49 (33) | |
| Working status | 0.100 | |||
| Working | 86 (19) | 218 (48) | 153 (33) | |
| Not working | 77 (23) | 168 (50) | 93 (28) | |
| Retired | 14 (27) | 28 (54) | 10 (19) | |
| Are you a health practitioner? | <0.001 | |||
| Yes | 34 (15) | 92 (42) | 91 (42) | |
| No | 143 (23) | 322 (51) | 165 (26) | |
| Have you or anyone you know been infected with COVID-19? | <0.010 | |||
| Yes | 9 (11) | 39 (48) | 34 (41) | |
| No | 168 (22) | 375 (49) | 222 (29) | |
Moreover, a weak significant positive correlation was found between COVID-19 stigma and both perceived severity and knowledge about prevention and control measures (r = 0.247 and 0.131, respectively; P <0.001). On the contrary, a weak significant negative correlation between COVID-19 stigma and perceived susceptibility was found (r = −0.080; P = 0.021). However, the total knowledge score, which includes symptoms, risk groups and preventive measures, was not correlated with stigma [Table 3].
Table 3.
Correlation between COVID-19 stigmatisation and perception and knowledge about the disease among residents in Riyadh, Saudi Arabia (N = 847)
| Variable | Correlation with stigma | P value |
|---|---|---|
| Perceived susceptibility | −0.080 | 0.021 |
| Perceived severity | 0.247 | <0.001 |
| Knowledge about prevention and control measures | 0.131 | <0.001 |
| Total knowledge | 0.009 | 0.789 |
To find predictors of stigma, a multiple linear regression model was applied. The variables entered into the model were age, marital status, educational level, whether the respondent was a health practitioner, whether they had been exposed to infection, knowledge about preventive measures, perceived susceptibility and perceived severity of the disease. All of these variables significantly predicted the stigma score, except being a health practitioner. The probability was <0.010 for all of them and the whole model. The variables with the strongest regression weight on stigma were perceived severity of the disease, knowledge about preventive measures, not having previous exposure to the disease and low education level [Table 4].
Table 4.
Multiple linear regression predicting stigma against COVID-19 infection among 847 residents from the city of Riyadh, Saudi Arabia
| Variable | Estimate | SE | t ratio | Prob>|t| |
|---|---|---|---|---|
| Intercept | 12.173 | 1.408 | 8.65 | <0.001 |
| Age | 0.052 | 0.016 | 3.21 | <0.001 |
| Marital status [married] | 0.490 | 0.189 | 2.60 | <0.010 |
| Educational level [college degree or higher] | −0.628 | 0.221 | −2.85 | <0.005 |
| Are you a health practitioner? [no] | 0.255 | 0.184 | 1.39 | 0.166 |
| Have you or anyone you know been infected with COVID-19? [no] | 0.701 | 0.255 | 2.74 | 0.006 |
| Total knowledge about measures for prevention and control | 0.721 | 0.217 | 3.33 | <0.001 |
| Perceived susceptibility | −0.600 | 0.140 | −4.25 | <0.001 |
| Perceived severity | 1.037 | 0.148 | 7.02 | <0.001 |
SE = standard error; Prob>|t| = two sample t-test.
Discussion
The study found that stigma exists in moderate to high levels among more than two-thirds of Riyadh’s residents. This supports the findings of previous studies that reported a statistically significant positive correlation between many infectious diseases, including those caused by the influenza A virus (H1N1/H3N1/H5N1) and social stigma.2 Notably, there is limited literature concerning stigmatisation of infectious diseases in Saudi Arabia. However, several studies have indicated that HIV/AIDS has been stigmatised.19,20 A qualitative study involving patients who recovered from the Middle East respiratory syndrome coronavirus in Saudi Arabia revealed that they experienced social stigmatisation, alienation and rejection.21 The high rate of stigmatisation among the study participants highlights the importance of apt interventions to avoid the potentially harmful consequences of healthcare avoidance and healthy behaviours.
To the best of the authors’ knowledge, this is the first study that assesses public stigmatisation towards COVID-19 in Saudi Arabia. In addition, the current investigation was carried out during the time of the pandemic thereby providing more accurate insight into the phenomenon being studied. It must be stated here that a full COVID-19 stigma scale is under development by the present research team. For this study, the part of the scale concerned with public stigmatisation was used and it showed good reliability and validity.
Several studies have identified a strong relationship between the stigma of infectious disease and education, profession, income, health status, age and perceived risk factors such as residential location.2 The present study found the stigma towards COVID-19 to be strongly associated with older age, lower education levels, being married and not being a healthcare professional. Thus, the interventions to reduce COVID-19 stigma should suitably target these groups.
The present study also found that general knowledge about COVID-19 was not associated with stigma. The lack of a relationship between stigma and knowledge is common in infectious diseases; however, a rational explanation for this is still elusive.2 Notably, this study did find a correlation between stigma and specific knowledge about preventive measures and practices. This could be related to the nature of preventive behaviours which involve, to a large extent, personal hygiene, perhaps causing people to consider this infection to be a consequence of poor hygiene. On the other hand, it must be noted that these findings contradict those regarding the stigmatisation of HIV/AIDS in Saudi Arabia; the studies concerning the latter have found a negative correlation between knowledge and stigma.19,20 This contradiction could be because of the differences concerning the nature of these diseases and the different attitudes towards their respective causative behaviours.
Stigma was also higher among those who had not been exposed to COVID-19 infection previously. A similar finding was reported in cases of other newly emerging diseases—especially when quarantine was required—where, despite having recovered, those who had been quarantined were stigmatised.7 Stigma was low among people with high perceived susceptibility, which could be because they expect to become infected themselves. On the other hand, stigmatisation was high among people with high perceived severity which could be attributed to their heightened fear of becoming infected. The findings reported for HIV/AIDS have been similar.22 However, a study of another respiratory infectious pandemic—namely the H1N1 virus—did not find an association between perceived severity and stigma.4
Thus, it is important to intervene early to eradicate disease stigma and promote healthcare access.13 While education can improve preventive practices, the accompanying study conducted by the current team shows that on its own, education could increase stigma.17 Consequently, educational campaigns should focus on perceived susceptibility which was found to be significantly associated with low stigma towards COVID-19. Specifically, campaigns should raise people’s awareness of the likelihood of getting infected with COVID-19. Relevant literature has shown that stigmatisation of an infectious disease leads to abstention from testing and healthcare and this would certainly have a substantial impact on the quality of life of the individual concerned.
As suggested by Mahajan et al. concerning HIV/AIDS stigma, it is recommended to develop and reinforce a social and legal framework to reduce the consequences of stigmatisation.23 There is a need for an in-depth qualitative study to explore the experience of stigma among COVID-19 patients and healthcare workers who come in contact with COVID-19 patients. As part of the larger research project, a COVID-19 stigma scale is being developed. It is recommended to be used for future research on this subject to explore not only the experiences of patients and healthcare practitioners as carriers of stigma but also the consequences of stigmatising COVID-19 in various contexts.
Convenience nonprobability sampling that was used for this study was a limitation in as much as it prevented generalisability of this study’s findings. However, the large sample size increased the confidence level to 98% and the real value was within ±4% of the surveyed value.
Conclusion
The present study revealed that the prevalence of stigma against the COVID-19 infection is high among 21% of Riyadh’s adult population. The factors that were significantly associated with the high stigma scores generated among the studied sample were old age, being married, low educational level, not working in the healthcare field, not being exposed to the infection previously, high knowledge about preventive measures, low perceived susceptibility and high perceived severity of the disease. All of these factors, except working in the healthcare field, could significantly predict stigma against COVID-19. The Saudi health authorities need to direct educational campaigns towards increasing the perception of susceptibility and awareness regarding the high chance of getting infected. It is also recommended that stigma eradication policies and interventions be implemented to avoid public health consequences.
Footnotes
CONFLICT OF INTEREST
The authors report no conflicts of interest.
FUNDING
This research was funded by the Deanship of Scientific Research at Princess Nourah bint Abdulrahman University through the Fast-track Research Funding Program.
AUTHORS’ CONTRIBUTION
All authors (FA, SM, LAB, AlA, AnA) have substantially contributed to the design of the study, data collection, drafting the manuscript and approved the final version for submission. FA, LAB, AnA contributed in the literature review and discussing the results. SM, AlA contributed to data analysis and interpretation.
References
- 1.Neuberg SL, Smith DM, Asher T. Why people stigmatize: Toward a biocultural framework. In: Heatherton TF, Kleck RE, Hebl MR, Hull JG, editors. The social psychology of stigma. New York, USA: Guilford Press; 2000. pp. 31–61. [Google Scholar]
- 2.Williams J, Gonzalez-Medina D, Le Q. Infectious diseases and social stigma. Med Health Sci J. 2011;4:58–70. doi: 10.15208/mhsj.2011.127. [DOI] [Google Scholar]
- 3.de Vries SG, Cremers AL, Heuvelings CC, Greve PF, Visser BJ, Bélard S, et al. Barriers and facilitators to the uptake of tuberculosis diagnostic and treatment services by hard-to-reach populations in countries of low and medium tuberculosis incidence: a systematic review of qualitative literature. Lancet Infect Dis. 2017;17:E128–43. doi: 10.1016/S1473-3099(16)30531-X. [DOI] [PubMed] [Google Scholar]
- 4.McCauley M, Minsky S, Viswanath K. The H1N1 pandemic: Media frames, stigmatization and coping. BMC Public Health. 2013;13:1116. doi: 10.1186/1471-2458-13-1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet. 2020;395:912–20. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chew NW, Lee GK, Tan BY, Jing M, Goh Y, Ngiam NJ, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. 2020;88:559–65. doi: 10.1016/j.bbi.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Des Jarlais DC, Galea S, Tracy M, Tross S, Vlahov D. Stigmatization of newly emerging infectious diseases: AIDS and SARS. Am J Public Health. 2006;96:561–7. doi: 10.2105/AJPH.2004.054742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Person B, Sy F, Holton K, Govert B, Liang A, Garza B, et al. Fear and stigma: The epidemic within the SARS outbreak. Emerg Infect Dis. 2004;10:358–63. doi: 10.3201/eid1002.030750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health. 2013;103:813–21. doi: 10.2105/AJPH.2012.301069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chang HJ, Huang N, Lee CH, Hsu YJ, Hsieh CJ, Chou YJ. The impact of the SARS epidemic on the utilization of medical services: SARS and the fear of SARS. Am J Public Health. 2004;94:562–4. doi: 10.2105/ajph.94.4.562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization. Coronavirus. [Accessed: May 2020]. From https://www.who.int/health-topics/coronavirus.
- 12.World Health Organization. Mental health and psychological resilience during the COVID-19 pandemic. [Accessed: May 2020.]. From: http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/mental-health-and-psychological-resilience-during-the-covid-19-pandemic.
- 13.Stangl AL, Earnshaw VA, Logie CH, van Brakel W, Simbayi LC, Barré I, et al. The Health Stigma and Discrimination Framework: A global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Medicine. 2019;17:31. doi: 10.1186/s12916-019-1271-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Center for Disease Control and Prevention. Reducing stigma. [Accessed May 2020]. From: https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/reducing-stigma.html.
- 15.Lin CY. Social reaction toward the 2019 novel coronavirus (COVID-19) Soc Health Behav. 2020;3:1–2. doi: 10.4103/SHB.SHB_11_20. [DOI] [Google Scholar]
- 16.General Authority for Statistics. Annual Yearbook 2015. Saudi Statistical Yearbook 51. 2015. [Accessed May 2020]. From: https://www.stats.gov.sa/en/411.
- 17.Almoayad FA, Bin-Amer LA, Mahboub S, Alrabiah AM, Alhashem AM. Preventive practices against COVID-19 among residents of Riyadh, Saudi Arabia. J Infect Dev Ctries. 2021;15:780–6. doi: 10.3855/jidc.13175. [DOI] [PubMed] [Google Scholar]
- 18.Likert R. A technique for measurement of attitudes. Arch Psychol. 1932;140:5–55. [Google Scholar]
- 19.Badahdah AM. Stigmatization of persons with HIV/AIDS in Saudi Arabia. J Transcult Nurs. 2010;21:386–92. doi: 10.1177/1043659609360873. [DOI] [PubMed] [Google Scholar]
- 20.Raheel H. Stigma towards people living with HIV/AIDS (PLWAs) among adolescents of Riyadh, Kingdom of Saudi Arabia. J AIDS Clin Res. 2016;7:612. doi: 10.4172/2155-6113.1000612. [DOI] [Google Scholar]
- 21.Almutairi AF, Adlan AA, Balkhy HH, Abbas OA, Clark AMJ. “It feels like I’m the dirtiest person in the world.”: Exploring the experiences of healthcare providers who survived MERS-CoV in Saudi Arabia”. J Infect Public Health. 2017;11:187–91. doi: 10.1016/j.jiph.2017.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Limage-Pierre M. PhD Thesis. Walden University; Columbia, USA: 2016. Stigma and HIV testing among African American women in New Jersey. [Google Scholar]
- 23.Mahajan AP, Sayles JN, Patel VA, Remien RH, Ortiz D, Szekeres G, et al. Stigma in the HIV/AIDS epidemic: A review of the literature and recommendations for the way forward. AIDS. 2008;22:S67–79. doi: 10.1097/01.aids.0000327438.13291.62. [DOI] [PMC free article] [PubMed] [Google Scholar]