Abstract
Fractures of the femoral head are rare injuries, which typically occur after posterior hip dislocation.
The Pipkin classification, developed in 1957, is the most commonly used classification scheme to date.
The injury is mostly caused by high-energy trauma, such as motor vehicle accidents or falls from a significant height.
Emergency treatment consists of urgent closed reduction of the hip joint, followed by non-operative or operative treatment of the femoral head fracture and any associated injuries.
There is an ongoing controversy about the suitable surgical approach (anterior vs. posterior) for addressing fractures of the femoral head. Fracture location, degree of displacement, joint congruity and the presence of loose fragments, as well as concomitant injuries are crucial factors in choosing the adequate surgical approach.
Long-term complications such as osteonecrosis of the femoral head, posttraumatic osteoarthritis and heterotopic ossification can lead to a relatively poor functional outcome.
Cite this article: EFORT Open Rev 2021;6:1122-1131. DOI: 10.1302/2058-5241.6.210034
Keywords: classification, femoral head, fracture, Pipkin, surgical approach
Introduction
Fractures of the femoral head are severe, but uncommon, injuries of the proximal femur, which typically occur after posterior dislocation of the hip joint.1–3 In 1869, Birkett was the first to discover and document femoral head fractures while performing a post mortem dissection.4 The infrequency of these fractures has made the study of large patient populations difficult, as most of the available literature comprises small studies and case series. However, the incidence of this rare injury has increased steadily in recent years, most likely due to the occurrence of a higher number of motor vehicle accidents in combination with an enhanced survival of polytraumatized patients due to improved safety features in modern vehicles.5 Since fractures of the femoral head are usually high-energy, intra-articular injuries, they pose unique challenges for the treating surgeon. Treatment of this injury ranges from simple closed reduction to a surgical approach, which involves either open reduction and internal fixation of the injured femoral head, or the removal of the fractured segment. In addition, associated injuries such as femoral neck or acetabular fractures may have to be addressed.6–8
Serious long-term complications including osteonecrosis of the femoral head, posttraumatic osteoarthritis and heterotopic ossification may impair the natural course of post-injury healing and rehabilitation, often leading to a poor functional outcome and unsatisfactory clinical results.9–11 Moreover, the lack of a reliable uniform classification system with a prognostic value as well as the ongoing controversies about the optimal surgical approach and fixation treatment8,12 make this injury even more challenging. Therefore, this review is intended to provide an overview of mechanisms of injury, common classification systems, diagnostic modalities, treatment options and recent clinical studies, in order to facilitate decision making for the treating surgeon.
Mechanism of injury
Fractures of the femoral head almost exclusively occur after posterior hip dislocations or fractures of the acetabulum.13 The largest series of posterior hip dislocations reported an incidence rate of associated femoral head fractures of approximately 5–15%.1–3,14–16 The injury is caused by shear forces along the femoral axis against the acetabular rim, as the femoral head exits the acetabulum.17 Impression fractures caused by anterior or central hip dislocation or isolated fractures without accompanying dislocation are less frequent.18–20
Due to the intrinsic stability of the hip joint, fractures of the femoral head occur mostly after high-energy trauma, typically in the form of motor vehicle accidents (e.g. the knee of a passenger striking the dashboard of a motor vehicle (‘dashboard injury’)) or falls from a significant height. Approximately two thirds of patients are young adults, and associated injuries such as acetabular fractures are extremely common.21 In addition, anatomic variations of the proximal femur, e.g. a decreased femoral anteversion, represent a risk factor for posterior hip dislocation and, hence, for femoral head fractures.22
Classification systems
In 1954, Stewart and Milford described four grades of hip joint dislocation. Dislocations with a concomitant fracture of the femoral head or neck of the proximal femur were classified as grade IV.23 In 1957, Gerard Pipkin further subclassified Stewart and Milford grade IV injuries in order to gain a better understanding in the sequalae of these kinds of injuries. He developed the classification system based on 24 patients, of whom 22 had injuries caused by motor vehicle accidents. Although not primarily intended, the classification system also provided a management scheme for these fractures.24
Pipkin classified fractures by their location in the femoral head and the presence of any associated fractures as one of four types: type I is defined as fracture inferior to the capitis femoris; type II is defined as fracture extended superior to the capitis femoris; type III is a type I or type IIfracture associated with a femoral neck fracture; and type IV is a type I or type II fracture associated with an acetabular fracture (Fig. 1). Pipkin used the fovea capitis as a landmark between type I and type II fractures. The ligamentum capitis femoris remains attached to the inferior fragment in type II injuries, which often results in substantial rotation of this fragment. As a result, the rotated caudal segment with its attached ligamentum may prevent a reduction of the cranial head segment.24
Fig. 1.
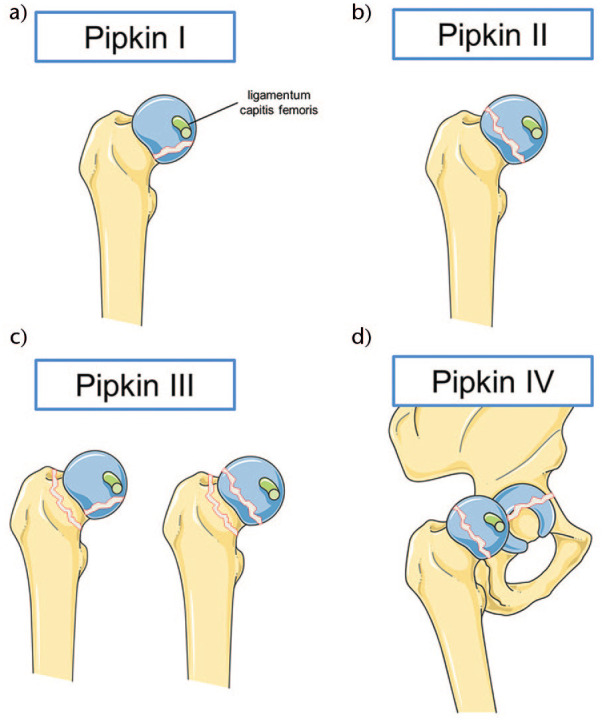
The Pipkin classification. (A) Type I: femoral head fracture inferior to the fovea centralis. The ligamentum capitis femoris inserting in the fovea centralis is shown. (B) Type II: femoral head fracture superior to the fovea centralis. (C) Type III: femoral head fracture inferior or superior to the fovea centrals with an associated femoral neck fracture. (D) Type IV: femoral head fracture inferior or superior to the fovea centrals with an associated acetabular fracture.
The Pipkin classification became the most frequently used classification system for fractures of the femoral head. Several studies evaluated the prognosis after surgical and non-surgical treatment of femoral head fractures classified using the Pipkin classification. The results indicate a better outcome with Pipkin type I and type II fractures when compared to Pipkin III and IV fractures, providing a crude validity to the classification system.25 However, no studies have reported on the inter-observer and intra-observer reliability, which is most likely due to the infrequency of these injuries, with data only limited to small case series. Some authors regard the Brumback classification as more accurate and clinically valid, when compared to the Pipkin classification.26 Indeed, the classification system of Brumback et al27 also considers the direction of the dislocation, joint stability and severity of the acetabular fracture (Table 1). In addition, the Brumback classification provides a prognostic value, with patients suffering from type 3B and type 5 injuries faring the worst, and patients with type 2B fractures having the best physical outcomes.9 However, Brumback’s classification has only recently been applied to a few published case series and is not as readily performed in clinical practice. Therefore, this classification system should be used and evaluated in future publications to truly determine its advantage over the well-established Pipkin classification.
Table 1.
Brumback classification of dorsal hip luxations and fractures of the femoral head
| Type 1A | Fracture of the inferiomedial aspect of the femoral head with minimal or no acetabular rim fracture; stable hip |
| Type 1B | Type 1A and significant acetabular rim fracture; unstable hip |
| Type 2A | Fracture of the supermedial aspect of the femoral head with minimal or no acetabular rim fracture; stable hip |
| Type 2B | Type 2A and significant acetabular rim fracture; unstable hip |
| Type 3A | Anterior or dorsal hip dislocation with femoral neck fracture |
| Type 3B | Anterior or dorsal hip dislocation with femoral neck fracture with associated femoral head fracture |
| Type 4A | Anterior hip dislocation and femoral head fracture; indentation type |
| Type 4B | Anterior hip dislocation and femoral head fracture; transchondral shear type |
| Type 5 | Central hip dislocation with acetabulum and femoral head fracture |
Evaluation and diagnosis
As these injuries are most commonly encountered during high-energy trauma, a thorough patient history and physical examination are necessary to diagnose the femoral head fracture and any associated injuries. Since the patient may be unconscious or uncooperative, detailed information from the emergency medical team can assist in understanding the mechanism of injury and determining potential concomitant injuries.
The posterior hip dislocation as the major cause of femoral head fractures usually presents with a shortened limb, in flexed, adducted and internally rotated position. However, this classical limb position may not be present with an accompanying fracture of the femoral neck or head. After evaluation of the limb position, a rapid neurovascular examination on this leg should be performed, including pulses, capillary refill and skin temperature. The neurological status of the limb should be assessed meticulously, as the sciatic nerve is commonly injured in this kind of trauma.2 The physician should be aware of any motor or sensory deficits of the affected limb. No attempt at reduction of the hip joint should be performed in a conscious patient until the physical examination and conventional X-rays are completed.
An appropriate radiographic assessment is crucial for determination of the injury management. Fracture dislocation is often evident on an anterior-posterior (AP) pelvic radiograph. If additional computed tomography (CT) imaging of the pelvis is performed as part of the polytrauma diagnostics, appropriate reconstructions can provide all the essential information for the diagnosis of a femoral head fracture. For patients with an isolated injury of the hip, AP radiographs of the pelvis reveal all the information needed to determine which additional radiographic assessment is necessary. The radiograph should be systematically reviewed on the representation of the femoral heads in size and location, a symmetrical joint gap, assessment of the rotational position of the femur and associated femoral neck, pelvic ring and acetabular fractures. If a posterior dislocation of the femoral head is present, an AP pelvic radiograph will usually show a superiorly displaced femoral head, a void in the acetabular socket and an obvious disruption of Shenton’s line. The femoral defect, however, is not obvious until the X-ray beam catches the plane of the femoral head fracture in profile.28 In the AP pelvic radiograph, the posteriorly femoral head will appear smaller than the contralateral side, as it is closer to the film and thus subject to less magnification effect. If in doubt, additional pelvic inlet and outlet views and 45° oblique views, as described by Judet and Letournel29, should be obtained, after the reduction manoeuvre. X-rays for follow-up examination should include plain radiograph of the pelvis and radiographs of the hip in two planes. If concomitant injuries, such as acetabular fractures, are diagnosed, additional iliac and obturator oblique views should be performed.
A CT scan should be performed routinely both after the successful closed reduction and after open reduction surgery. The CT scan provides essential information about the structure of the femoral head fracture, fracture displacement, potential fracture fragments in the joint gap and the overall condition of the hip joint. Subsequently, magnetic resonance imaging (MRI) may be obtained to detect an avulsion of the acetabular labrum, inexplicable widening of the hip joint and the early diagnosis of femoral head necrosis.5
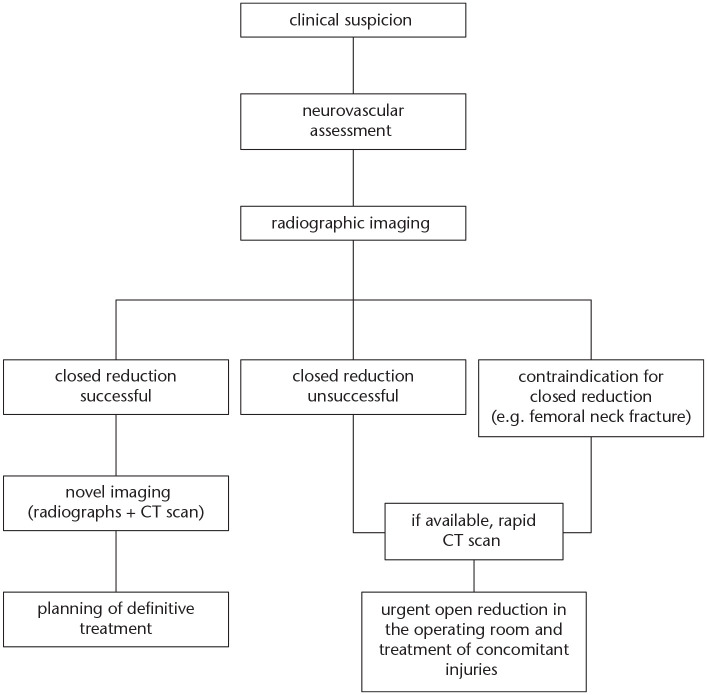
Emergency treatment
Fracture-dislocation of the hip joint is a surgical emergency condition. An immediate closed reduction is indicated regardless of the presence of a femoral head fracture. In the emergency department, reduction should be performed under sedation of the patient as soon as possible. Delay of the reduction must be avoided under all circumstances, in order to minimize the risk of osteonecrosis of the femoral head.30 After successful reduction, new radiographs and a CT scan of the hip should be obtained to evaluate the femoral head and associated injuries. If there is a contraindication for closed reduction (e.g. concomitant femoral neck fracture) or the dislocation remains irreducible due to a rotation of the fracture fragment around the ligament of the head of the femur, impaction of soft tissues or an osteochondral fragment,24 urgent open reduction in the operating room is indicated. A preoperative CT scan should be performed if possible; however, a substantial delay must not be accepted due to an increasing risk of femoral head osteonecrosis (Fig. 2).5
Fig. 2.
Treatment algorithm in the emergency phase. Upon clinical suspicion of a femoral head fracture after posterior hip dislocation, thorough neurovascular assessment has to be performed. Afterwards, radiographs of the hip and pelvis can confirm the diagnosis. Rapid closed reduction should be performed as soon as possible. If closed reduction is successful, novel imaging by means of radiographs and CT scans must be performed to evaluate the definitive treatment approach. If closed reduction is unsuccessful or contraindications for closed reduction are present (e.g. femoral neck fractures), urgent open reduction in the operating room is indicated. CT scans for completing diagnostics should performed if possible; however, they must not hinder rapid surgical treatment.
Note. CT, computed tomography.
Definitive treatment
Non-surgical treatment
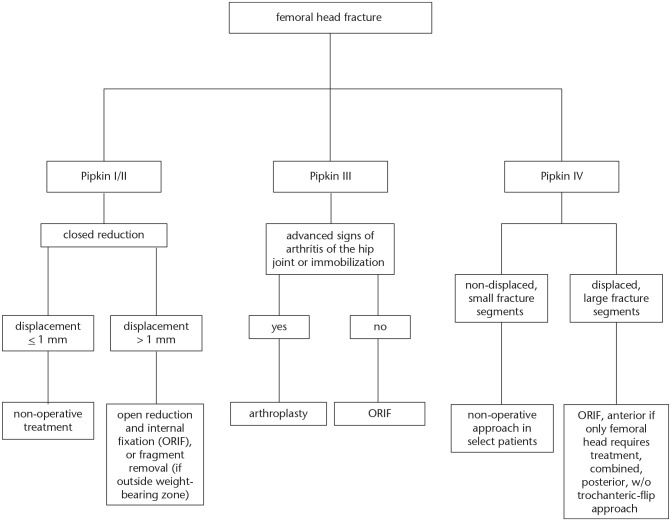
The Pipkin classification may assist in choosing the appropriate treatment approach (Fig. 3). A non-surgical approach of femoral head fractures may be considered in Pipkin I and II fractures, if a closed reduction achieves a residual displacement of 1 mm or less and an anatomically congruent hip joint without fragment interposition. In the past, most femoral head fractures were treated with prolonged bed rest and axial traction following closed reduction.24,31 However, fairly poor results have been reported with this treatment approach.14 Therefore, partial weight-bearing with crutches for a minimum of six weeks is recommended nowadays.27,32 Adduction and internal rotation above neutral should be restricted for approximately two months.5 Regular repeated radiographs should be obtained to evaluate maintenance of reduction and hip joint congruency. At our institution we perform control radiographs regularly after one, three and six weeks, as well as three months. If there is any doubt about secondary dislocation, as well as femoral head vascularity, repeat CT or MRI diagnostics are performed as required.
Fig. 3.
Treatment algorithm according to the Pipkin classification. In Pipkin type I and type II fractures, the treatment depends on the degree of displacement after closed reduction. For fractures with a displacement of less than 1 mm a non-operative approach should be considered. Fractures with a displacement of more than 1 mm should be addressed with open reduction and internal fixation (ORIF) or fragment removal. In Pipkin type III fractures, surgical treatment depends on signs of arthritis in the hip joint and the physical demands of the patient. If advanced signs of arthritis or immobilization are evident, a bipolar endoprosthesis or total hip arthroplasty are advised. If not, ORIF with surgical hip dislocation is suggested, attempting to preserve the femoral head, especially in younger patients. In Pipkin type IV fractures with non-displaced and small fracture segments, a non-operative approach with weight-bearing of the hip joint is recommended. Displaced and large fracture segments are usually treated with ORIF by the Kocher-Langenbeck approach with or without trochanteric-flip osteotomy.
Surgical treatment
In case an adequate closed reduction of less than 1 mm displacement cannot be achieved, a surgical approach is indicated. In Pipkin type I and type II fractures open reduction and internal fixation (ORIF) is recommended (Fig. 3). This is most commonly done with countersunk screws, or headless compression screws. In these cases, headless compression screws have the advantage that they can be placed subchondrally, without causing additional damage to the articular cartilage in the process.8,33 Additionally, Hermus et al34 and Prokop et al35 reported on the fixation of femoral head fractures with bio-absorbable screws. These bio-degradable implants provide fewer artifacts during magnetic resonance imaging. In smaller Pipkin type I injuries, outside the weight-bearing zone removal of the fractured fragment can also be an option.
Pipkin type III injuries have a poor prognosis in general.26 Closed reduction in this injury is not feasible as the femur is disconnected from the femoral head. Hence, immediate ORIF through an anteromedial Smith-Peterson, or in some cases an anterolateral Watson-Jones approach should be undertaken.36 ORIF of the femoral neck and head fracture should be performed in younger patients. A bipolar endoprosthesis or total hip arthroplasty, on the other hand, should be preferred in senescent patients with signs of advanced arthritis and low physical demands (THA) (Fig. 3).37
Pipkin IV fractures must be addressed in tandem with the associated acetabular fracture, with the latter determining a surgical approach. If the femoral head and acetabular fracture are non-displaced, a non-operative approach with restricted weight-bearing of the hip joint is usually recommended. If the fractures are displaced, ORIF of the acetabular and femoral head fracture should be performed. A posterior wall fracture of the acetabulum is often associated with fractures of the femoral head. The Kocher-Langenbeck approach allows the management of both types of fracture.5 In case of an injury to the anterior column, an ilioinguinal or a modified Stoppa approach with Smith-Peterson extension is usually chosen.5
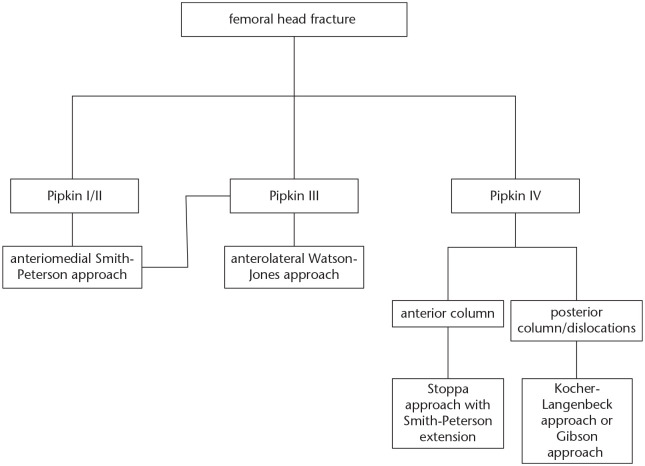
Surgical approaches
For most Pipkin type I and II injuries, the distal part of the anteromedial Smith-Peterson approach represents the preferred surgical exposure. This approach uses the intermuscular plane between the sartorius and tensor fascia latae muscles38 to allow the direct visualization and internal fixation of femoral head fragments, which are often located anterior and medially.9 Moreover, the Smith-Peterson approach is associated with a reduced surgery duration and blood loss,10 as well as a decreased rate of avascular necrosis of the femoral head,9 when compared to posterior approaches. On the other hand, however, heterotopic ossifications have been demonstrated to be more frequent in anterior approaches,39 especially if the more proximal extended part is utilized.
In addition to the Smith-Peterson approach, the anterolateral Watson-Jones approach is particularly suitable for the treatment of Pipkin type III fractures. The latter approach uses the interval between the gluteus medius and tensor fasciae latae muscles to address the femoral neck and femoral head fracture at the same time.
For posterior dislocations, as well as cases with associated acetabular fractures of the posterior column and posterior wall (Pipkin type IV), the Kocher-Langenbeck approach is recommended.40 This approach provides excellent exposure of the posterior wall of the acetabulum. However, it is limited by an insufficient visualization of the femoral head and can therefore hinder internal fixation of the femoral head fracture fragments, especially if the hip joint has been successfully reduced in the emergency room. Treatment of the femoral head then either requires a separate anterior exposure or, more elegantly, an extension of the posterior approach via trochanteric-flip osteotomy. Various authors have reported on this technique.41-43 In fact, in a previous study, Mostafa et al44 demonstrated that an additional trochanteric-flip osteotomy was associated with less operative time, reduced blood loss and improved visualization, thus facilitating direct screw fixation of the femoral head fracture. However, there was no significant difference in the final clinical and radiological outcome. Notably, the Gibson interval, between the gluteus maximus and tensor fasciae latae muscles, may be favourable when performing the trochanteric-flip osteotomy in order to preserve the integrity of the gluteus maximus muscle. In conclusion, choosing the most suitable approach for surgical treatment of femoral head fractures requires careful evaluation, including the fracture pattern and location, concomitant injures and, maybe most importantly, the preference of the surgeon himself (Fig. 4).
Fig. 4.
Algorithm for surgical approaches. For Pipkin type I and II fractures, the anteromedial Smith-Peterson approach represents the preferred surgical exposure. For Pipkin III fractures the Smith-Peterson and the anterolateral Watson-Jones approach is recommended. Pipkin IV injuries with concomitant acetabular fractures of the anterior column should be addressed using the Stoppa approach with Smith-Peterson extension. Pipkin IV fractures with injuries of the posterior column or posterior fragment dislocation should be treated with the Kocher-Langenbeck approach or the modified Gibson approach in combination with trochanter osteotomy.
Irreducible femoral head fractures
Femoral head fractures are rare injuries, and irreducible cases are even less frequent. However, they represent a critical surgical emergency, due to a high risk of osteonecrosis of the femoral head. Irreducible dislocation should be distinguished from incomplete reductions, which may be caused by a rotation of the fracture fragment around the capitis femoris ligament, impaction of soft tissue or an osteochondral fragment.24 Irreducible dislocations, however, are due to a button-hole effect associated with capsulolabral incarceration in the acetabulum and the femoral head indented on the posterior acetabular rim.45 Uzel et al45 reported about two cases of irreducible Pipkin II femoral head fractures, which occurred after road accidents. In both cases, closed reduction failed and the fracture dislocation was treated using a transgluteal approach.45 A femoral head extractor was introduced into the femoral neck via the greater trochanter to disengage the femoral head under muscle relaxation. The interposing soft tissue was freed manually and instrumentally. Subsequently surgical reduction was stabilized by screw osteosynthesis.45 Damage to the acetabular labrum can be a potential source of irreducibility of the femoral head fracture. In that case, care should be taken to fixate and reconstruct the labrum, in order to avoid future incarceration and damage to the articular surface of the hip joint. Moreover, the acetabular labrum is of crucial importance for hip joint stability and an equal distribution of forces during loading, reducing the demand on cartilage and compression in the main loading area.46,47 A posterior approach with a trochanteric-flip osteotomy may be best used to address such an injury to clearly identify all osteochondral lesions.
Fragment removal
There is ongoing controversy regarding the treatment of fragments in femoral head injuries. Earlier literature advocates the removal of all fragments, provided that the fragment constitutes of less than one third of the femoral head.3,14 However, the bio-mechanical consequences of removal of femoral head fragments remain unclear. Previous studies demonstrate similar outcomes between patients treated with fragment removal and those treated with internal fixation.5,48 In a case series focusing on the medium- and long-term outcomes of femoral head fractures, Kokubo et al49 suggest that fragments measuring less than 1 cm could be removed, while larger fragments should be fixed in all types of femoral head fractures. In general, factors influencing the treatment decision are fragment size, degree of comminution and the location of the fragment in relation to the weight-bearing area.5 Fragments which are large enough for stable internal fixation should be fixed. On the other hand, small or comminuted fragments that are not located within the weight-bearing portion of the head can be removed without compromising outcome.5
Role of hip arthroscopy
Hip arthroscopy has gained increasing popularity for the management of various hip disorders, in particular femora-acetabular impingement, in recent years.50 Its role in the management of fractures of the femoral head, however, is largely unexplored, with only a few case reports in the literature and no long-term follow-up results.51,52 In a technical note, Kekatpure et al50 provided a stepwise description for the arthroscopic reduction and internal fixation of Pipkin type I femoral head fractures. This technique showed acceptable reduction with maintained joint space, and may thus represent an alternative to the usually performed open reduction with the advantages of minimal surgical soft tissue injury and early rehabilitation in posttraumatic cases.50 Nonetheless, it requires reliable and multi-centric follow-up studies to truly evaluate the potential of minimally invasive hip arthroscopy for the treatment of fractures of the femoral head.
Traumatic hip dislocation in children and adolescents
Traumatic hip dislocation in children and adolescents is a particularly rare event.53 This injury is typically the result of a high-energy trauma, but can also occur after minor trauma, due to the laxity of capsular ligament structures in this age group.54 Similar to adults, traumatic hip dislocations can ultimately lead to fractures of the femoral head and acetabulum. Accordingly, the algorithm for diagnosis and treatment of concomitant injuries should in general follow the recommendations which are applied in adults. However, MRI diagnostics play a greater role in children and adolescents, not only for the evaluation long-term complications but also for further diagnosis during the acute phase after trauma. Concomitant injuries to the labrum, osteochondral defects and lesions of the ligamentum capitis femoris are not uncommon among children and adolescents and can only be reliably detected by MRI. Therefore, MRI diagnostics in juvenile and adolescent patients should be performed as soon as possible after reduction, in order to detected all potential injuries and initiate the necessary treatment to avoid long-term complications.55
Rehabilitation
Early mobilization demonstrated equivalent or superior results, when compared to prolonged bed rest and extension treatment in cases of both non-surgical and surgical treatment of femoral head fractures, provided that the hip joint is stable.16 Hence, early functional treatment with 20 kg partial weight-bearing with crutches is recommended for a minimum of six weeks postoperatively. Continuous passive motion devices may be used in the early postoperative period but it has not been confirmed to improve clinical outcome.56 Moreover, in selected cases hip flexion of more than 70 degrees can be avoided to reduce shear forces on the structurally weak part of the posterior acetabular rim. Patients should be assisted through physical therapy to work on passive, active-assisted, and active range of motion (ROM) of the hip to regain range of motion. If radiographic signs of fracture healing are evident after six weeks postoperatively, patients can wean off crutches and gentle strengthening can be started. In general, full weight-bearing is achieved approximately three months postoperatively.
Complications and prognosis
Since fractures of the femoral head are usually caused by high-energy trauma, the prognosis depends to a large degree on associated injuries including traumatic brain injury, thoracic and abdominal trauma, as well as unstable pelvic injuries. However, isolated fractures of the femoral head also carry the risk of a variety of complications, which require special attention during clinical examination and postoperative follow-up. The most frequent early complications in surgical cases of femoral head fractures represent postoperative infections with a rate of 3.2%. Moreover, sciatic nerve injury occurs in 4.0% of all fracture dislocations.26 Major late complications include avascular necrosis with an incidence rate of 11.8%, posttraumatic arthritis with 20% and heterotopic ossification with 16.8%.26 Of note, Mehlman et al54 performed a long-term follow-up of children suffering hip dislocation and found a comparable rate of 12% of cases with avascular head necrosis. Another common complication represented coxa magna in 27% of all cases with radiographic follow-up averaging two years and six months.54
Two significant problems are evident when attempting to analyse the prognosis of femoral head fractures: (1) inadequate follow-up in the percentage of patients within the study series and (2) the lack of a uniform classification system with a satisfactory inter-observer and intra-observer reliability.57 However, a reliable and standardized system for analysing end results is necessary to evaluate the correlation between injury classification, surgical treatment approach and clinical outcome. The most commonly used criteria for functional assessment after fractures of the femoral head were established by Thompson and Epstein,13 which include the radiographic outcome as well as remaining pain and range of motion of the hip joint. In a previously published systematic review by Giannoudis et al,26 the authors evaluated the outcome of femoral head fractures using Thompson and Epstein’s criteria. The overall results, regardless of fracture classification or treatment, showed excellent results in 14.3%, good results in 39.8%, fair results in 19.3% and poor results in 26.5% of all cases. Interestingly, the authors found no statistical difference in the outcome among Pipkin subtypes. Nonetheless, the analysis revealed a tendency towards a superior outcome in Pipkin type I and II fractures, when compared to Pipkin type III and IV fractures.26 Moreover, fractured segment removal showed better results in Pipkin type I injuries, when compared to ORIF, whereas in Pipkin type II fractures the principles of anatomic reduction and internal fixation should be applied.26 It is noteworthy that the data published by Giannoudis et al26 are based on rather a small number of patients and are compromised by the absence of a validated outcome instrument and the lack of high-quality randomized control (prospective or retrospective) studies. Hence, there is an urgent need for reliable, multi-centric, prospective clinical trials as well as large-scale retrospective register studies based on an uniform classification and outcome system to elucidate prognostic factors determining the functional outcome for each subtype of this injury independently.
Conclusion
Fractures of the femoral head represent a relatively uncommon but severe injury that often occurs after posterior hip dislocation in the context of a high-energy trauma. Treatment options are conservative in cases of non-displaced fractures with intact joint congruity and surgical treatment in displaced fractures. Surgical treatment involves open reduction and internal fixation of the fractured segments, fragment removal, as well as minimally invasive approaches using hip arthroscopy. Depending on fracture morphology and associated injuries of the femoral neck or acetabulum, a suitable anterior, anterolateral or posterior approach has to be chosen. However, due to a lack of clinical trials, definite treatment recommendations for specific fracture subtypes are currently hard to determine. Accordingly, the major challenge for the future will be to evaluate and compare the results of these different surgical approaches and internal fixation techniques for each fracture subtype individually. If this succeeds, specific treatment recommendations for each fracture subtype may be developed to finally facilitate decision making for the treating surgeon.
Acknowledgments
The authors thank Servier Medical Art for providing access to designed medical elements (https://smart.servier.com/), supporting the generation of graphical items in this publication.
Footnotes
ICMJE Conflict of interest statement: The authors declare no conflict of interest relevant to this work.
OA licence text: This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Funding statement
The author or one or more of the authors have received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Hougaard K, Thomsen PB. Traumatic posterior fracture-dislocation of the hip with fracture of the femoral head or neck, or both. J Bone Joint Surg [Am] 1988;70-A:233–239. [PubMed] [Google Scholar]
- 2. Roeder LF, Jr, DeLee JC. Femoral head fractures associated with posterior hip dislocation. Clin Orthop Relat Res 1980;147:121–130. [PubMed] [Google Scholar]
- 3. Epstein HC, Wiss DA, Cozen L. Posterior fracture dislocation of the hip with fractures of the femoral head. Clin Orthop Relat Res 1985;201:9–17. [PubMed] [Google Scholar]
- 4. Birkett J. Description of a dislocation of the head of the femur, complicated with its fracture; with remarks. 1869. Clin Orthop Relat Res 2007;458:10–11. [DOI] [PubMed] [Google Scholar]
- 5. Droll KP, Broekhuyse H, O’Brien P. Fracture of the femoral head. J Am Acad Orthop Surg 2007;15:716–727. [DOI] [PubMed] [Google Scholar]
- 6. Jukkala-Partio K, Partio EK, Hirvensalo E, Rokkanen P. Absorbable fixation of femoral head fractures: a prospective study of six cases. Ann Chir Gynaecol 1998;87:44–48. [PubMed] [Google Scholar]
- 7. Kelly PJ, Lipscomb PR. Primary vitallium-mold arthroplasty for posterior dislocation of the hip with fracture of the femoral head. J Bone Joint Surg [Am] 1958;40-A:675–680. [PubMed] [Google Scholar]
- 8. Murray P, McGee HM, Mulvihill N. Fixation of femoral head fractures using the Herbert screw. Injury 1988;19:220–221. [DOI] [PubMed] [Google Scholar]
- 9. Stannard JP, Harris HW, Volgas DA, Alonso JE. Functional outcome of patients with femoral head fractures associated with hip dislocations. Clin Orthop Relat Res 2000;377:44–56. [DOI] [PubMed] [Google Scholar]
- 10. Swiontkowski MF, Thorpe M, Seiler JG, Hansen ST. Operative management of displaced femoral head fractures: case-matched comparison of anterior versus posterior approaches for Pipkin I and Pipkin II fractures. J Orthop Trauma 1992;6:437–442. [PubMed] [Google Scholar]
- 11. Marchetti ME, Steinberg GG, Coumas JM. Intermediate-term experience of Pipkin fracture-dislocations of the hip. J Orthop Trauma 1996;10:455–461. [DOI] [PubMed] [Google Scholar]
- 12. Gardner MJ, Suk M, Pearle A, Buly RL, Helfet DL, Lorich DG. Surgical dislocation of the hip for fractures of the femoral head. J Orthop Trauma 2005;19:334–342. [PubMed] [Google Scholar]
- 13. Thompson VP, Epstein HC. Traumatic dislocation of the hip: a survey of two hundred and four cases covering a period of twenty-one years. J Bone Joint Surg [Am] 1951;33-A:746–778. [PubMed] [Google Scholar]
- 14. Epstein HC. Posterior fracture-dislocations of the hip; long-term follow-up. J Bone Joint Surg [Am] 1974;56-A:1103–1127. [PubMed] [Google Scholar]
- 15. Sahin V, Karakaş ES, Aksu S, Atlihan D, Turk CY, Halici M. Traumatic dislocation and fracture-dislocation of the hip: a long-term follow-up study. J Trauma 2003;54:520–529. [DOI] [PubMed] [Google Scholar]
- 16. Lang-Stevenson A, Getty CJ. The Pipkin fracture-dislocation of the hip. Injury 1987;18:264–269. [DOI] [PubMed] [Google Scholar]
- 17. Davis JB. Simultaneous femoral head fracture and traumatic hip dislocation. Am J Surg 1950;80:893–895. [DOI] [PubMed] [Google Scholar]
- 18. Richards BS, Howe DJ. Anterior perineal dislocation of the hip with fracture of the femoral head: a case report. Clin Orthop Relat Res 1988;228:194–201. [PubMed] [Google Scholar]
- 19. DeLee JC, Evans JA, Thomas J. Anterior dislocation of the hip and associated femoral-head fractures. J Bone Joint Surg [Am] 1980;62-A:960–964. [PubMed] [Google Scholar]
- 20. Mody BS, Wainwright AM. Fracture of the femoral head without associated hip dislocation following low-energy trauma: a report of two cases. Arch Orthop Trauma Surg 1996;115:300–302. [DOI] [PubMed] [Google Scholar]
- 21. Alonso JE, Volgas DA, Giordano V, Stannard JP. A review of the treatment of hip dislocations associated with acetabular fractures. Clin Orthop Relat Res 2000;377:32–43. [DOI] [PubMed] [Google Scholar]
- 22. Upadhyay SS, Moulton A, Burwell RG. Biological factors predisposing to traumatic posterior dislocation of the hip: a selection process in the mechanism of injury. J Bone Joint Surg [Br] 1985;67-B:232–236. [DOI] [PubMed] [Google Scholar]
- 23. Stewart MJ, Milford LW. Fracture-dislocation of the hip: an end-result study. J Bone Joint Surg [Am] 1954;36-A:315–342. [PubMed] [Google Scholar]
- 24. Pipkin G. Treatment of grade IV fracture-dislocation of the hip. J Bone Joint Surg [Am] 1957;39-A:1027–1042, passim. [PubMed] [Google Scholar]
- 25. Romeo NM, Firoozabadi R. Classifications in brief: the Pipkin classification of femoral head fractures. Clin Orthop Relat Res 2018;476:1114–1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Giannoudis PV, Kontakis G, Christoforakis Z, Akula M, Tosounidis T, Koutras C. Management, complications and clinical results of femoral head fractures. Injury 2009;40:1245–1251. [DOI] [PubMed] [Google Scholar]
- 27. Brumback RJ, Kenzora JE, Levitt LE, Burgess AR, Poka A. Fractures of the femoral head. Hip 1987;••:181–206. [PubMed] [Google Scholar]
- 28. Rizzo PF, Gould ES, Lyden JP, Asnis SE. Diagnosis of occult fractures about the hip: magnetic resonance imaging compared with bone-scanning. J Bone Joint Surg [Am] 1993;75-A:395–401. [DOI] [PubMed] [Google Scholar]
- 29. Judet R, Judet J, Letournel E. Fractures Of The Acetabulum: Classification And Surgical Approaches For Open Reduction. PRELIMINARY REPORT. J Bone Joint Surg Am 1964;46:1615–1646. [PubMed] [Google Scholar]
- 30. Hougaard K, Thomsen PB. Coxarthrosis following traumatic posterior dislocation of the hip. J Bone Joint Surg [Am] 1987;69-A:679–683. [PubMed] [Google Scholar]
- 31. Butler JE. Pipkin type-II fractures of the femoral head. J Bone Joint Surg [Am] 1981;63-A:1292–1296. [PubMed] [Google Scholar]
- 32. Leenen LP, van der Werken C. Traumatic posterior luxation of the hip. Neth J Surg 1990;42:136–139. [PubMed] [Google Scholar]
- 33. Lange RH, Engber WD, Clancy WG. Expanding applications for the Herbert scaphoid screw. Orthopedics 1986;9:1393–1397. [DOI] [PubMed] [Google Scholar]
- 34. Hermus JP, Laan CA, Hogervorst M, Rhemrev SJ. Fixation of a Pipkin fracture with bio-absorbable screws: case report and a review of the literature. Injury 2005;36:458–461. [DOI] [PubMed] [Google Scholar]
- 35. Prokop A, Helling HJ, Hahn U, Udomkaewkanjana C, Rehm KE. Biodegradable implants for Pipkin fractures. Clin Orthop Relat Res 2005;432:226–233. [DOI] [PubMed] [Google Scholar]
- 36. Tosounidis T, Aderinto J, Giannoudis PV. Pipkin type-III fractures of the femoral head: fix it or replace it? Injury 2017;48:2375–2378. [DOI] [PubMed] [Google Scholar]
- 37. Tannast M, Mack PW, Klaeser B, Siebenrock KA. Hip dislocation and femoral neck fracture: decision-making for head preservation. Injury 2009;40:1118–1124. [DOI] [PubMed] [Google Scholar]
- 38. Ricci WM, McAndrew CM, Miller AN, Avery MC. Open reduction and internal fixation of the femoral head via the Smith-Petersen approach. J Orthop Trauma 2018;32:S16–S17. [DOI] [PubMed] [Google Scholar]
- 39. Wang CG, Li YM, Zhang HF, Li H, Li ZJ. Anterior approach versus posterior approach for Pipkin I and II femoral head fractures: a systemic review and meta-analysis. Int J Surg 2016;27:176–181. [DOI] [PubMed] [Google Scholar]
- 40. Johnson EE. Irreducible fracture-dislocation of the hip: a severe injury with a poor prognosis. J Orthop Trauma 1999;13:228–229. [DOI] [PubMed] [Google Scholar]
- 41. Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg [Br] 2001;83-B:1119–1124. [DOI] [PubMed] [Google Scholar]
- 42. Henle P, Kloen P, Siebenrock KA. Femoral head injuries: which treatment strategy can be recommended? Injury 2007;38:478–488. [DOI] [PubMed] [Google Scholar]
- 43. Massè A, Aprato A, Alluto C, Favuto M, Ganz R. Surgical hip dislocation is a reliable approach for treatment of femoral head fractures. Clin Orthop Relat Res 2015;473:3744–3751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Mostafa MF, El-Adl W, El-Sayed MA. Operative treatment of displaced Pipkin type I and II femoral head fractures. Arch Orthop Trauma Surg 2014;134:637–644. [DOI] [PubMed] [Google Scholar]
- 45. Uzel AP, Laflamme GY, Rouvillain JL. Irreducible Pipkin II femoral head fractures: is transgluteal approach the best strategy? Orthop Traumatol Surg Res 2010;96:695–701. [DOI] [PubMed] [Google Scholar]
- 46. Audretsch CK, Schmidutz F, Kuper MA. Asymptomatic and unnoticed intra-articular screw over 18 years after fracture of the posterior wall of the acetabulum: a question of stability? Z Orthop Unfall 2021;159:298–303. [DOI] [PubMed] [Google Scholar]
- 47. Ferguson SJ, Bryant JT, Ganz R, Ito K. The influence of the acetabular labrum on hip joint cartilage consolidation: a poroelastic finite element model. J Biomech 2000;33:953–960. [DOI] [PubMed] [Google Scholar]
- 48. Chen ZW, Zhai WL, Ding ZQ, et al. Operative versus nonoperative management of Pipkin type-II fractures associated with posterior hip dislocation. Orthopedics 2011;34:350. [DOI] [PubMed] [Google Scholar]
- 49. Kokubo Y, Uchida K, Takeno K, et al. Dislocated intra-articular femoral head fracture associated with fracture-dislocation of the hip and acetabulum: report of 12 cases and technical notes on surgical intervention. Eur J Orthop Surg Traumatol 2013;23:557–564. [DOI] [PubMed] [Google Scholar]
- 50. Kekatpure A, Ahn T, Lee SJ, Jeong MY, Chang JS, Yoon PW. Arthroscopic reduction and internal fixation for Pipkin type I femoral head fracture: technical note. Arthrosc Tech 2016;5:e997–e1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Park MS, Yoon SJ, Choi SM. Hip arthroscopic management for femoral head fractures and posterior acetabular wall fractures (Pipkin type IV). Arthrosc Tech 2013;2:e221–e225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Park MS, Her IS, Cho HM, Chung YY. Internal fixation of femoral head fractures (Pipkin I) using hip arthroscopy. Knee Surg Sports Traumatol Arthrosc 2014;22:898–901. [DOI] [PubMed] [Google Scholar]
- 53. Macnicol MF. The Scottish incidence of traumatic dislocation of the hip in childhood. J Pediatr Orthop B 2000;9:122–124. [DOI] [PubMed] [Google Scholar]
- 54. Mehlman CT, Hubbard GW, Crawford AH, Roy DR, Wall EJ. Traumatic hip dislocation in children: long-term followup of 42 patients. Clin Orthop Relat Res 2000;376:68–79. [PubMed] [Google Scholar]
- 55. Strüwind CM, von Rüden C, Thannheimer A, Bühren V, Schneidmueller D. [Relevance of MRI after closed reduction of traumatic hip dislocation in children]. Z Orthop Unfall 2018;156:586–591. [DOI] [PubMed] [Google Scholar]
- 56. Salter RB, Simmonds DF, Malcolm BW, Rumble EJ, MacMichael D, Clements ND. The biological effect of continuous passive motion on the healing of full-thickness defects in articular cartilage: an experimental investigation in the rabbit. J Bone Joint Surg [Am] 1980;62-A:1232–1251. [PubMed] [Google Scholar]
- 57. Albrechtsen J, Hede J, Jurik AG. Pelvic fractures: assessment by conventional radiography and CT. Acta Radiol 1994;35:420–425. [PubMed] [Google Scholar]