Abstract
Background/Objectives
The coronavirus disease 2019 (COVID‐19) pandemic has taken a disproportionate toll on long‐term care facility residents and staff. Our objective was to review the empirical evidence on facility characteristics associated with COVID‐19 cases and deaths.
Design
Systematic review.
Setting
Long‐term care facilities (nursing homes and assisted living communities).
Participants
Thirty‐six empirical studies of factors associated with COVID‐19 cases and deaths in long‐term care facilities published between January 1, 2020 and June 15, 2021.
Measurements
Outcomes included the probability of at least one case or death (or other defined threshold); numbers of cases and deaths, measured variably.
Results
Larger, more rigorous studies were fairly consistent in their assessment of risk factors for COVID‐19 outcomes in long‐term care facilities. Larger bed size and location in an area with high COVID‐19 prevalence were the strongest and most consistent predictors of facilities having more COVID‐19 cases and deaths. Outcomes varied by facility racial composition, differences that were partially explained by facility size and community COVID‐19 prevalence. More staff members were associated with a higher probability of any outbreak; however, in facilities with known cases, higher staffing was associated with fewer deaths. Other characteristics, such as Nursing Home Compare 5‐star ratings, ownership, and prior infection control citations, did not have consistent associations with COVID‐19 outcomes.
Conclusion
Given the importance of community COVID‐19 prevalence and facility size, studies that failed to control for these factors were likely confounded. Better control of community COVID‐19 spread would have been critical for mitigating much of the morbidity and mortality long‐term care residents and staff experienced during the pandemic. Traditional quality measures such as Nursing Home Compare 5‐Star ratings and past deficiencies were not consistent indicators of pandemic preparedness, likely because COVID‐19 presented a novel problem requiring extensive adaptation by both long‐term care providers and policymakers.
Keywords: assisted living, COVID‐19, long‐term care, nursing homes
Key Point
Larger size and location in an area with high COVID‐19 rates were the strongest and most consistent predictors of COVID‐19 outcomes.
Outcomes varied by facility racial composition.
More staff members increased outbreaks but more staff hours may have prevented deaths.
Why Does this Paper Matter?
Our results inform which policies might work; for example, large facilities in virus hotspots may benefit most from technical assistance and resources.
INTRODUCTION
The coronavirus disease 2019 (COVID‐19) pandemic has taken a disproportionate toll on long‐term care facility residents and staff, who have accounted for roughly 1.4 million cases and 183,000 deaths—almost 40% of all U.S. deaths—as of mid‐May 2021. 1 By early 2021, almost all U.S. nursing homes had experienced at least one COVID‐19 case, and most (more than 80%) had experienced at least one death. 2
The context of this tragedy, often referred to as a “perfect storm,” 3 stems from the confluence of attributes of the virus, of long‐term care residents, and of the setting. The SARS‐CoV‐2 virus that causes COVID‐19 is airborne, can be spread asymptomatically, and is particularly lethal for frail, older adults. 4 A congregate setting exacerbates this risk. Nursing homes and assisted living communities (ALCs) house large numbers of residents, often in shared rooms, who need hours of intimate care that precludes social distancing. That the virus spreads asymptomatically means that residents and staff can unwittingly serve as vectors of infection, triggering outbreaks that can quickly overwhelm a facility. 5 This was especially problematic early in the pandemic when there was less known about asymptomatic transmission and testing resources were severely limited.
From the outset, policymakers and researchers have sought to identify actionable correlates of COVID‐19 outbreaks and deaths in nursing homes and ALCs in order to find ways to mitigate the harm. Prior to the pandemic, 40% of nursing homes were cited with deficiencies in their infection control practices, making it the most frequently cited regulatory deficiency. 6 However, whether these baseline measures of infection control practices and traditional quality indicators like the Nursing Home Compare 5‐Star ratings correlate with a facility's success in preventing and controlling COVID‐19 outbreaks has been uncertain. A flurry of empirical research has emerged to explore those correlations. In the absence of a systematic review, media reports have drawn mixed conclusions and have been unable to reconcile seemingly inconsistent findings. Indeed, one media story provocatively suggested that the explanation for why some facilities had better COVID outcomes “depends who you ask.” 7
We fill this critical knowledge gap by systematically examining the evidence base on factors associated with COVID‐19 cases and deaths in long‐term care facilities. Our goal is to better inform practice and policy moving forward, both in this and future pandemics.
METHODS
We used PubMed to systematically search the literature for studies of factors associated with COVID‐19 cases and deaths in long‐term care facilities published between January 1, 2020 and June 15, 2021. Search terms included “SARS‐CoV‐2,” “COVID,” “coronavirus,” “nursing home,” “assisted living,” “long‐term care,” and “skilled nursing.” Given the rapidly evolving nature of this literature, we supplemented our PubMed search with additional journal articles, preprints, and gray literature found as of July 15, 2021 through a combination of citation mining of existing papers, review of COVID‐19 sections of key journals, and referral from content experts. We included all U.S. English language studies that empirically examined COVID‐19 cases or deaths in long‐term care facilities as an outcome and any area‐, facility‐, or unit‐level factor as an independent variable. We excluded studies that did not contain quantitative empirical analysis, were not in English, or did not directly examine COVID‐19 cases or deaths. Because our focus was the long‐term care environment and provider actions, we also excluded studies that solely examined resident‐level predictors of COVID‐19 outcomes.
Figure 1 summarizes the search process. During the PubMed search, two authors independently conducted all title, abstract, and full‐text reviews, then discussed and agreed upon which studies to exclude at each stage. The initial PubMed search yielded 793 articles. Of these, 745 were excluded after title review, 14 after abstract review, and eight after full‐text review, resulting in 26 articles for analysis. An additional 10 articles were identified through the secondary methods described above, yielding a total of 36 studies included for analysis. Only minor discrepancies among authors arose in terms of inclusions and exclusions, which were resolved through discussion.
FIGURE 1.
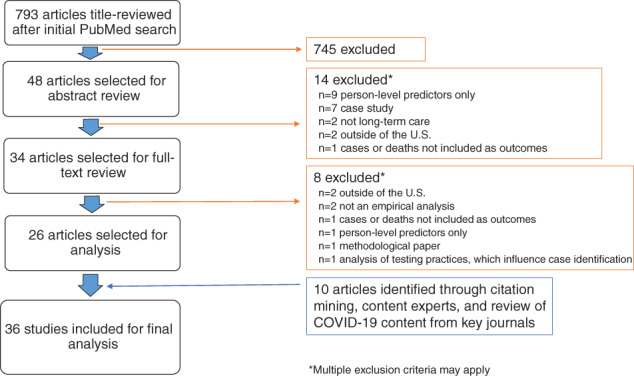
Summary of articles identified, included, and excluded during literature search
To evaluate the quality of included studies, we examined key features of each study design. Due to limitations of available data and the need for rapid results as the pandemic unfolded, randomized trials or strong quasi‐experimental designs enabling causal inference were not expected. Thus, quality was judged in terms of other aspects of internal validity (measurement of key variables, rigor of the statistical model and controls for key confounders, and underlying data quality) and external validity (whether the study was national, multi‐state, single‐state).
RESULTS
Table S1 summarizes the 36 studies that met our inclusion criteria. 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 With one exception, 27 all studies used facility‐level data and did not control for resident‐level risk factors. Thirty‐four studies examined nursing homes only, 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 one study included nursing homes and ALCs, 29 and one study examined ALCs only. 30 Nine were single‐state studies; 11 , 15 , 18 , 21 , 22 , 23 , 25 , 27 , 29 14 were national studies; 10 , 14 , 17 , 19 , 20 , 24 , 31 , 36 , 37 , 38 , 40 , 41 , 42 , 43 and the remainder were multi‐state studies including between 3 and 30 states.
For data on COVID‐19 cases and deaths in nursing homes, the vast majority of studies used one or both of two main data sources: the National Healthcare Safety Network (NHSN) data collected by the Centers for Disease Control and Prevention (CDC) and the Centers for Medicare and Medicaid Services (CMS) starting in May 2020 (with optional reporting of cases and deaths up to that point); and reports obtained from state websites. Five studies used data reported directly from nursing homes or ALCs. 23 , 27 , 29 , 33 , 34 Most studies used data on COVID‐19 cases reported prior to July 2020; 16 used data past this time period, 10 , 13 , 14 , 20 , 23 , 26 , 29 , 31 , 34 , 37 , 38 , 39 , 40 , 41 , 42 , 43 with the latest study using data through April, 2021. 37 , 38 As such, most of the studies do not take into account the widespread deployment of vaccines to facilities nationwide which began in mid‐December 2020.
For other independent variables, LTCFocus, Nursing Home Compare, and Payroll‐Based Journal staffing data were the most commonly used data sources for pre‐pandemic measures of facility characteristics. The most common sources for area‐level characteristics were census data, the Area Health Resources File, and the American Community Survey. County‐level COVID‐19 prevalence was drawn from statistics compiled by the New York Times, USAFacts.org, or the Johns Hopkins Coronavirus Resource Center.
Outcomes related to COVID‐19 cases and deaths were measured in four main ways: (1) the probability of at least one case (an “outbreak”); (2) the probability of at least one death; (3) cumulative or weekly case counts or rates; and (4) cumulative or weekly death counts or rates. Earlier studies tended to use the probability of at least one case as the primary outcome, given skepticism about the accuracy of data on numbers of cases or deaths in the absence of widespread testing. Conceptually, this outcome emphasizes the ability to keep the virus from entering the facility, but became less interesting by fall 2020 when the vast majority of nursing homes had had at least one case. Later studies tended to examine multiple outcomes, including the number of deaths, with improved trust in the numbers due to increased testing. These additional outcomes provided a conceptually distinct perspective on a facility's ability to contain the virus once introduced. Most studies that examined counts of cases or deaths used cumulative measures. Six studies examined incident cases within a specific time window or stratified by time, 11 , 20 , 24 , 38 , 39 , 43 and only four studies examined temporal variation. 35 , 37 , 38 , 43
Overall quality of the literature
The most robust studies either used national or multi‐state data or collected rich primary data from a smaller number of facilities. Additionally, stronger studies controlled for geography and adjusted for multiple facility‐ and area‐level covariates. Methodologically weaker studies were limited to a single state or a subset of facilities within one state (except for those involving primary data collection), presented only unadjusted analyses, and did not account for geographic variation. Table 1 summarizes the key quality‐related attributes of each study.
TABLE 1.
Summary of key evaluation criteria
| Study | States (n) | NH or ALC sample size (n) | Time period for COVID‐19 cases | COVID‐19 data sources | Key outcomes | Adjusted analysis | Area‐level control | Nursing home compare measures | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Probability of outbreak | Cases | Deaths | ||||||||
| Konetzka 46 | 12 | 5527 NHs | Through May 13, 2020 | State reports | X | X | X | |||
| Abrams et al. 9 | 30 | 9395 NHs | Through May 11, 2020 | State reports | X | X | X | X | X | |
| White et al. 33 | 26 | 341 NHs/3016 NHs | Through May 4, 2020 | State reports & provider data | X | X | X | X | X | X |
| Chatterjee et al. 12 | 23 + DC | 8943 NHs | Through April 29, 2020 | State reports | X | X | ||||
| Gorges et al. 19 | 50 + DC | 13,167 NHs | Through June 25, 2020 | NHSN | X | X | X | X | X | X |
| Figueroa et al. 16 | 8 | 4254 NHs | Through June 30, 2020 | State reports | X | X | X | X | ||
| He et al. 22 | 1 (CA) | 1223 NHs | Through June 2, 2020 | State reports | X | X | X | X | X | |
| Harrington et al. 21 | 1 (CA) | 1091 NHs | Through May 4, 2010 | State, county, and media reports | X | X | X | |||
| Li, Temkin‐Greener et al. 25 | 1 (CT) | 215 NHs | Through April 16, 2020 | State reports | X | X | X | X | X | X |
| Dean et al. 15 | 1 (NY) | 355 NHs | Through May 31, 2020 | State reports | X | X | X | X | X | |
| Gandhi et al. 17 | 49 | 13,398 NHs | Through May 24, 2020 | NHSN | X | X | X | X | ||
| Shi et al. 27 | 1 (MA) | 1 NH | Mar 16 to May 8, 2020 | NH testing data | Resident‐level outcome: incident COVID‐19 | X | N/A (1 NH) | |||
| Shen et al. 26 | 18 | 7154 NHs | Through July 10, 2020 | State reports | X | X | X | X | ||
| Temkin‐Greener et al. 30 | 7 | 3994 ALCs | Through May 29, 2020 | State reports | X | X | X | X | X | N/A |
| Cronin et al. 14 | 50 + DC | 15,115 NHs | Through September 13, 2020 | NHSN and state reports | X | X | X | X | X | |
| Li, Cen, et al. 24 | 50 + DC | 12,576 NHs | May 25 to May 31, 2020 | NHSN | X | X | X | X | X | X |
| Unruh et al. 32 | 3 (CT, NJ, NY) | 1162 NHs | Through mid‐April, 2020 | State reports | X | X | ||||
| Bui et al. 11 | 1 (WV) | 123 NHs | Through June 11, 2020 | State reports | X | X | X | X | ||
| Sun et al. 28 | 3 (MA, GA, NJ)/1 (CA) | 1146 NHs / 1021 NHs | Through late April/ early May, 2020 | State and local reports | X | X | X | X | ||
| Chen, Chevalier, et al. 35 | 21 + DC/50 + DC | 6337 NHs / 13,165 NHs | Mar 13 to May 31, 2020 | NHSN and state reports | X | X | X | X | ||
| Gopal et al. 18 | 1 (CA) | 713 NHs | Through May 1, 2020 | State report | X | X | X | X | X | |
| Telford et al. 45 | 1 (GA) | 17 NHs, 7 ALCs | Through July, 29, 2020 | NH testing data | X |
N/A (1 county) |
||||
| LeRose et al. 23 | 1 (MI) | 103 NHs | Through August 2020 | State report | X | X | ||||
| Braun et al. 10 | 50 + DC | 11,470 NHs | Through July 2, 2020 | NHSN | X | X | X | X | ||
| Sugg et al. 36 | 50 + DC | 13,709 NHs | Through June 30, 2020 | NHSN | X | X | X | X | ||
| Zimmerman et al. 34 | 20 | 219 NHs / 177 NHs / 215 NHs | January 20, 2020 to July 31, 2020 | NHSN and primary data | X | X | X | X | ||
| Gorges et al. 20 | 50 + DC | 13,312 NHs | Through September 13, 2020 | NHSN | X | X | X | X | ||
| Chen, Yun, et al. 13 | NR | 3008 NHs | Through October 11, 2020 | NHSN | X | X | X | |||
| Kumar et al. 37 | 50 + DC | 11,718 NHs | June 1, 2020 to December 27, 2020 | NHSN | X | X | X | X | ||
| Travers et al. 31 | 50 + DC | 11,587 NHs | Through July 19, 2020 | NHSN | X | X | X | X | ||
| Williams et al. 42 | 50 + DC | 14,693 NHs | Through January 10, 2021 | NHSN | X | X | X | X | X | |
| Weech‐Maldonado et al. 41 | 50 + DC | 12,914 | Through October 25, 2020 | NHSN | X | X | X | |||
| Ryskina et al. 40 | 50 + DC | 11,585 | Through August 2020 | NHSN | X | X | X | |||
| Gilman and Bassett 38 | 50 + DC | 13,820 | May 25, 2020 to April 18, 2021 | NHSN | X | X | X | X | ||
| McGarry et al., 202139 | NR | 7154 | June 1, 2020 to September 27, 2020 | NHSN | X | X | X | X | X | |
| Cai et al. 43 | 50+ DC | 13,123 | June 7, 2020 to August 23, 2020 | NHSN | X | X | X | X | X | X |
Note: Studies using national data that did not explicitly report number of states are assumed to represent 50 states plus Washington, D.C.
Abbreviations: ALC, assisted living community; NH, nursing home; NHSN, National Healthcare Safety Network COVID‐19 module for long‐term care facilities; NR, not reported.
The importance of community spread, facility size, and racial distribution
Across all studies, two findings stand out as most consistent and significant in magnitude. First, nursing homes located in areas (usually counties) with higher virus prevalence were at significantly higher risk for COVID‐19 cases and deaths. None of the larger, more rigorous studies that included a direct measure of community COVID‐19 prevalence or an area fixed effect failed to find a significant relationship, and usually their effects were substantially stronger than other variables in adjusted models. 9 , 10 , 12 , 14 , 16 , 17 , 19 , 20 , 24 , 26 , 27 , 28 , 30 , 31 , 33 , 35 , 36 , 40 , 42 , 43 Second, almost as consistent was the finding that larger facilities had a higher probability of any outbreak and more cases than smaller facilities. 9 , 11 , 12 , 18 , 19 , 20 , 21 , 26 , 28 , 30 , 31 , 32 , 33 , 34 , 35 , 43
Sixteen studies examined whether the racial composition of a facility's resident population was related to COVID‐19 outcomes. Fourteen of those used data from spring 2020 to early fall 2020 8 , 9 , 13 , 20 , 22 , 24 , 26 , 28 , 30 , 31 , 33 , 35 , 41 , 43 and all found that facilities with a higher proportion of Black and Hispanic residents had higher rates of adverse outcomes. Two studies examined mortality rates using later data and found distinct temporal variation: nursing homes with a high proportion of Black and Hispanic residents had more deaths through summer 2020, but predominantly White nursing homes had more deaths in late 2020 and early 2021 when COVID‐19 rates surged in the upper Midwest and rural states of the West. 37 , 38 Facility size and community characteristics including virus prevalence, population density, urbanicity, and social vulnerability index explained much of the variation by race. 20 , 23 , 26 , 31 , 43
The relationship between COVID‐19 outcomes and quality measures
Many of the studies (n = 16) directly examined the relationship between the Nursing Home Compare overall 5‐Star rating and COVID‐19 outcomes. 8 , 9 , 11 , 12 , 14 , 15 , 16 , 19 , 20 , 22 , 24 , 25 , 26 , 35 , 42 , 43 Across the vast majority of these studies, including all but one of the larger studies, using multiple data sources, no practically meaningful or statistically significant relationship was found between the overall 5‐Star rating and COVID‐19 outcomes. In contrast, only five studies found that higher star ratings were significantly associated with fewer COVID‐19 cases, and four of these were single‐state studies with limited generalizability, 11 , 18 , 22 , 24 finding small effect sizes that could be attributable to inadequate controls for confounding. Most importantly, two California‐only studies 18 , 22 did not control for community virus prevalence, and a West Virginia study 11 included only 14 facilities with outbreaks, one of which had no 5‐Star rating.
The remaining study that found an association between 5‐Star ratings and COVID‐19 outcomes, conducted by CMS and its team that developed the 5‐star ratings, used national data and controlled for key confounders, but used an unusual denominator for their outcome measures: cumulative resident incidence and mortality and the number of weeks in the top decile of resident incidence. 42 The denominator for the cumulative measures was the resident census as of January 2021 rather than the typical baseline measure, with an offset term to account for average resident census starting only in May 2020. Thus, the incidence and mortality rates were likely inflated in exactly those nursing homes that experienced a larger drop in occupancy due to COVID‐19 deaths or decreased admissions, particularly those that experienced their worst outbreaks in March and April 2020, before NHSN data collection began. Despite this likely inflation, the magnitudes of the associations were small. Similarly, the star ratings measures were from January 2021, meaning that outcomes during COVID were likely predicting star ratings and not the other way around.
Some studies examined 5‐Star ratings for one or more of the overall rating's three domains: inspections, staffing, and quality measures. 8 , 12 , 14 , 16 , 18 , 19 , 21 , 33 , 36 Only one study found a significant relationship between higher quality measures rating and fewer cases, 42 and the majority of studies found no association or inconsistent relationships between COVID‐19 outcomes and the staffing or inspections ratings. 8 , 12 , 33 , 36 The CMS study described above found significant relationships for both staffing and inspections, with the same caveats noted above. 42 One California study without geographic controls found that nursing homes with a 5‐star staffing rating were less likely to have any COVID‐19 cases, 21 and another small study based on early data found that nursing homes with 4 or 5 Stars in staffing had a lower probability of having at least 30 cases, 16 but the majority of studies with adequate controls found no association between COVID‐19 outcomes and the staffing star ratings. Similarly, although one study found that more stars in the inspection rating was associated with fewer deaths, 14 most studies found no association.
Four studies examined prior infection control inspection citations specifically, 9 , 13 , 26 , 33 given their direct relevance. However, none of the four studies found that these prior citations were predictive of COVID‐19 cases or deaths. One small study from 1 Georgia county found that facilities with fewer cases had better practices related to personal protective equipment (PPE) and social distancing, but no differences in other infection control practices, though the sample was subject to selection bias since facilities with low case counts were not included. 29
The relationship between COVID‐19 outcomes and staffing
Several studies examined staffing hours per resident‐day, measured just prior to the pandemic, as a predictor of COVID‐19 outcomes. 13 , 15 , 19 , 25 , 36 A national study found that, conditional on having any outbreak, nursing homes with more CNAs and total nurse staffing had fewer cases and deaths; 19 a Connecticut study found the same for RNs. 25 These effects were small in magnitude relative to the effect of facility size or county virus prevalence. A New York study found higher CNA staffing, regardless of outbreak status, and the presence of labor unions, to be associated with fewer deaths. 15 Other studies confirmed the protective effect of higher total nurse staffing once an outbreak occurred, with some inconsistencies by staff type. 13 , 36
In contrast, there is no evidence that having more staff prevented an initial outbreak. Indeed, several studies underscored the role that staff played in inadvertently bringing the virus in to the facility. One study found that nursing homes with a larger number of unique staff members—even when controlling for hours of care per day—had more COVID‐19 cases. 39 Other studies found that units of a nursing home whose staff lived in ZIP Codes with higher COVID‐19 prevalence were more likely to have an outbreak; 27 that characteristics of staff neighborhoods were more predictive of nursing home deaths than nursing home location characteristics; 26 and that staff movement between facilities was highly predictive of resident COVID‐19 cases. 35
The relationship between COVID‐19 outcomes and nursing home organizational factors
Given longstanding policy and research interest in nursing home ownership structures and payer mix, many studies included characteristics, such as for‐profit status and Medicaid census. Most studies did not find these factors to be significant or meaningful in magnitude.
Two studies directly examined the association between private equity ownership and COVID‐19 outcomes. 10 , 17 Neither found that nursing homes owned by private equity firms had worse COVID‐19 outcomes; in fact, results of the more rigorous study suggested that private‐equity‐owned nursing homes had fewer cases as well as better access to PPE and testing. 17 One study found that “Greenhouse” facilities had lower rates of both cases and deaths relative to facilities in the same area, consistent with the fact that Greenhouse facilities are small and tend to use staff for multiple purposes, limiting the number of staff entering and exiting a facility daily. 34 Finally, one study found that nursing homes in areas of high social deprivation were more at risk for COVID‐19 cases and deaths; however, this study did not control for other key risk factors. 23
DISCUSSION
We reviewed the evidence from 36 studies of nursing home and ALC attributes associated with COVID‐19 cases and deaths. We found the largest and most consistent predictors of COVID‐19 cases and deaths to be community prevalence of COVID‐19 and larger facility size, which relates to the amount of foot traffic coming and going from that community as well as ease of transmission within a facility. Studies that failed to control for these two factors were therefore likely confounded. Outcomes were disparate by the racial composition of the resident population, with facilities serving predominantly Black and Hispanic residents being hit hardest in the spring and summer of 2020, and predominantly White facilities subject to surges in the late fall and early winter of 2020. Facility size and community characteristics including virus prevalence partially explained the variation by race. Baseline nurse staffing levels were not consistently associated with the probability of having any outbreak, though more robust studies found that better‐staffed facilities had fewer deaths and smaller case counts once an outbreak occurred. Other nursing home characteristics, such as Nursing Home Compare 5‐Star ratings, ownership, and prior infection control citations did not have consistent, meaningful associations with COVID‐19 outcomes.
The current evidence base is subject to several limitations. First, most studies to date have examined risk factors and outcomes at the facility and community levels. Although studies examining resident‐level risk factors have begun to emerge, 4 , 27 , 44 those data are still limited, and it will be important in future work to examine resident‐ and staff‐level risk factors in conjunction with facility‐level factors. Second, each of the data sets used in the included studies has limitations; the NHSN data, for example, are missing many cases prior to May 2020, and LTCFocus data are several years old—but our conclusions hold across studies using varied data sources. Third, the vast majority of studies used data only through early fall 2020, missing the November–December 2020 surge that triggered some of the worst outbreaks of the pandemic. 2 Finally, almost all of the studies in the review were cross‐sectional. More work is needed to establish causal connections and assess temporal trends.
The results of our review have direct implications for policy and practice. The overwhelming importance of community COVID‐19 prevalence in predicting long‐term care cases and deaths suggests that mitigation policies should not solely focus on facility actions. Prior to the existence of effective vaccines, the single most important thing that policymakers could have done to mitigate the crisis in long‐term care would have been to effectively use public health measures to stem community spread. At the same time, policymakers could have prioritized the highest‐risk facilities for PPE distribution, access to early surveillance testing to identify outbreaks, 45 and assistance with coordinating emergency staffing reserves. Well into the pandemic, nursing homes were reporting widespread shortages of these critical resources. 46 , 47 , 48 The US Government Accountability Office concluded that CMS largely ignored a September 2020 report by their own Coronavirus Nursing Home Commission that recommended further investment in system‐based measures such as PPE, workforce, and rapid testing. 49
Unfortunately, in spring and summer of 2020, CMS pushed policies such as emergency inspections for infection control violations, predicated on the assumption that facilities could control outbreaks independent of community prevalence. CMS cited its earlier analysis of NHSN data that COVID‐19 cases were associated with the 5‐Star ratings, an analysis that was never released. 50 Subsequently, CMS implemented a program to financially reward or fine facilities based on their COVID‐19 cases and deaths. 51 Our review suggests that such policies were misguided, given that the strongest predictor of COVID‐19 outcomes was facility location. Anecdotal and qualitative evidence suggests that such polices may have had the inadvertent effects of diverting critical resources away from facilities most in need, 52 and shouldering administrators with undue administrative and regulatory burden at a time when they needed to focus on crisis management. 53
The lack of consistent relationships between COVID‐19 outcomes and ownership structure departs from past research which has found these factors to be associated with quality. Although for‐profit providers have been shown to employ fewer nursing staff, they also have organizational attributes which may have positioned them better than small, independently owned facilities to respond to the pandemic. Larger chains could centralize decision‐making to help reduce administrative burden for local facility leaders, streamline responses to changing guidance and regulations, maintain tracking systems, leverage connections for procurement of PPE and testing supplies, and facilitate communication with federal, state, and local health entities.
One exception to the lack of effective strategies by facilities themselves is staffing. A large literature links the levels of direct‐care staffing to nursing home quality, especially in the case of registered nurse (RN) staffing. 54 , 55 Staffing may have taken on even greater importance under pandemic conditions, as having adequate staff is a prerequisite for implementing the measures now considered best practices in trying to control an outbreak. The evidence from our review supports a positive (if small/inconsistent) role of staffing in handling an outbreak once it occurred.
Our results do not exonerate long‐term care providers from implementing rigorous infection control practices or imply that there are not concerns regarding care quality. Rather, the evidence suggests a widespread and unique challenge, especially in the face of inadequate supply chains for PPE and rapid testing. COVID‐19 has been a devastating, once‐in‐a‐generation problem requiring new organizational and clinical processes to contain an airborne, asymptomatically spread virus that is particularly lethal to the population nursing homes and ALCs serve. These new processes include implementing complex isolation and quarantine protocols; time‐ and resource‐intensive testing procedures; daily screenings of staff, residents, and visitors; new admission procedures; PPE procurement and management; restructuring of the physical environment to allow for social distancing; new communication processes with families; and a massive vaccination campaign. They also involved adherence to rapidly evolving local, state, and national guidance. The challenges with adapting to these new tasks likely reflect lack of flexibility in the current structure of the industry as well as the unprecedented nature of the pandemic.
Studies of the tragedy of the past year have provided critical evidence to inform future emergency preparedness in long‐term care. For the rest of this pandemic, and for future public health emergencies, long‐term care facilities must be recognized as integral components of the health care system and prioritized for assistance and resources as needed. Despite the need for long‐term care providers to improve, our review revealed little that providers could have done to prevent an outbreak when in a hotspot. The fate of residents and staff of long‐term care facilities is inextricably linked to the fate of the communities in which they are located. Policies to address future crises need to recognize these linkages and provide a more integrated response.
CONFLICT OF INTEREST
The authors declare no conflicts of interest with the work.
AUTHOR CONTRIBUTIONS
All authors contributed significantly to the work, in initiating the project (R. Tamara Konetzka, Vincent Mor, David C. Grabowski); conducting the search (Elizabeth M. White, Alexander Pralea); drafting the manuscript (R. Tamara Konetzka); and critical revision of the manuscript (Elizabeth M. White, David C. Grabowski, Vincent Mor).
SPONSOR'S ROLE
None.
Supporting information
Table S1 Table of Evidence Summarizing Studies of COVID‐19 Outcomes in U.S. Nursing Homes and Assisted Living Communities
Konetzka RT, White EM, Pralea A, Grabowski DC, Mor V. A systematic review of long‐term care facility characteristics associated with COVID‐19 outcomes. J Am Geriatr Soc. 2021;69(10):2766-2777. doi: 10.1111/jgs.17434
[Correction added after first online publication on September 24, 2021. Keypoints have been changed.]
Funding information For three of the authors (White, Grabowski, Mor), funding is acknowledged from National Institute on Aging under 3U54AG063546‐02S2 (MPI V. Mor, S. Berry).
REFERENCES
- 1. Kaiser Family Foundation . State Reports of Long‐Term Care Facility Cases and Deaths Related to COVID‐19. 2021. https://www.kff.org/health-costs/issue-brief/state-data-and-policy-actions-to-address-coronavirus/. Accessed July 26, 2021.
- 2. Nursing Home COVID‐19 Public File . Centers for Disease Control and Prevention National Healthcare Safety Network; 2021. https://data.cms.gov/stories/s/bkwz-xpvg. Accessed June 30.
- 3. Ouslander JG, Grabowski DC. COVID‐19 in nursing homes: calming the perfect storm. J Am Geriatr Soc. 2020;68:2153‐2162. [DOI] [PubMed] [Google Scholar]
- 4. Panagiotou OA, Kosar CM, White EM, et al. Risk factors associated with all‐cause 30‐day mortality in nursing home residents with COVID‐19. JAMA Intern Med. 2021;181(4):439‐448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Blackman C, Farber S, Feifer RA, Mor V, White EM. An illustration of SARS‐CoV‐2 dissemination within a skilled nursing facility using heat maps. J Am Geriatr Soc. 2020;68:2174‐2178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kaiser Family Foundation . Percent of Certified Nursing Facilities with Top Ten Deficiencies. 2020. https://www.kff.org/other/state-indicator/percent-of-certified-nursing-facilities-with-top-ten-deficiencies-2014. Accessed May 17, 2020.
- 7. Jaffe I. Why Were Some Nursing Homes Spared the Devastation of COVID‐19? Depends Who You Ask. Washington, D.C.: NPR. 2020; https://www.npr.org/2020/06/26/881935246/why-were-some-nursing-homes-spared-the-devastation-of-covid-19-depends-who-you-a. Accessed May 24, 2021. [Google Scholar]
- 8. Testimony of R. Tamara Konetzka, PhD: Caring for Seniors amid the COVID‐19 Crisis. Special Committee on Aging, U.S. Senate. 116th Congress, 2nd Session. 2020. https://www.aging.senate.gov/imo/media/doc/SCA_Konetzka_05_21_20.pdf
- 9. Abrams HR, Loomer L, Gandhi A, Grabowski DC. Characteristics of U.S. nursing homes with COVID‐19 cases. J Am Geriatr Soc. 2020;68(8):1653‐1656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Braun RT, Yun H, Casalino LP, et al. Comparative performance of private equity‐owned US nursing homes during the COVID‐19 pandemic. JAMA Netw Open. 2020;3(10):e2026702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bui DP, See I, Hesse EM, et al. Association between CMS quality ratings and COVID‐19 outbreaks in nursing homes—West Virginia, March 17–June 11, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(37):1300‐1304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chatterjee P, Kelly S, Qi M, Werner RM. Characteristics and quality of US nursing homes reporting cases of coronavirus disease 2019 (COVID‐19). JAMA Netw Open. 2020;3(7):e2016930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chen AT, Yun H, Ryskina KL, Jung HY. Nursing home characteristics associated with resident COVID‐19 morbidity in communities with high infection rates. JAMA Netw Open. 2021;4(3):e211555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cronin CJ, Evans WN. Nursing Home Quality, COVID‐19 Deaths, and Excess Mortality. Cambridge, MA: National Bureau of Economic Research. 2020, No. 28012. [Working Paper]. http://www.nber.org/papers/w28012. [Google Scholar]
- 15. Dean A, Venkataramani A, Kimmel S. Mortality rates from COVID‐19 are lower in unionized nursing homes. Health Aff (Millwood). 2020;39(11):1993‐2001. [DOI] [PubMed] [Google Scholar]
- 16. Figueroa JF, Wadhera RK, Papanicolas I, et al. Association of nursing home ratings on health inspections, quality of care, and nurse staffing with COVID‐19 cases. JAMA. 2020;324(11):1103‐1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gandhi A, Song YJ, Upadrashta P. Have Private Equity Owned Nursing Homes Fared Worse Under COVID‐19? SSRN. 2020. 10.2139/ssrn.3682892. [DOI]
- 18. Gopal R, Han X, Yaraghi N. Compress the curve: a cross‐sectional study of variations in COVID‐19 infections across California nursing homes. BMJ Open. 2021;11(1):e042804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gorges RJ, Konetzka RT. Staffing levels and COVID‐19 cases and outbreaks in U.S. nursing homes. J Am Geriatr Soc. 2020;68(11):2462‐2466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gorges RJ, Konetzka RT. Factors associated with racial differences in deaths among nursing home residents with COVID‐19 infection in the US. JAMA Netw Open. 2021;4(2):e2037431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Harrington C, Ross L, Chapman S, Halifax E, Spurlock B, Bakerjian D. Nurse staffing and coronavirus infections in California nursing homes. Policy Polit Nurs Pract. 2020;21(3):174‐186. [DOI] [PubMed] [Google Scholar]
- 22. He M, Li Y, Fang F. Is there a link between nursing home reported quality and COVID‐19 cases? Evidence from California skilled nursing facilities. J Am Med Dir Assoc. 2020;21(7):905‐908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. LeRose JJ, Merlo C, Duong P, et al. The role of the social vulnerability index in personal protective equipment shortages, number of cases, and associated mortality during the coronavirus disease 2019 (COVID‐19) pandemic in Michigan skilled nursing facilities. Infect Control Hosp Epidemiol. 2021;42(7):877‐880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Li Y, Cen X, Cai X, Temkin‐Greener H. Racial and ethnic disparities in COVID‐19 infections and deaths across U.S. nursing homes. J Am Geriatr Soc. 2020;68(11):2454‐2461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Li Y, Temkin‐Greener H, Shan G, Cai X. COVID‐19 infections and deaths among Connecticut nursing home residents: facility correlates. J Am Geriatr Soc. 2020;68(9):1899‐1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Shen K. Relationship between nursing home COVID‐19 outbreaks and staff neighborhood characteristics. medRxiv. 2020. https://www.medrxiv.org/content/10.1101/2020.09.10.20192203v2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Shi SM, Bakaev I, Chen H, Travison TG, Berry SD. Risk factors, presentation, and course of coronavirus disease 2019 in a large, academic long‐term care facility. J Am Med Dir Assoc. 2020;21(10):1378‐1383. e1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Sun CLF, Zuccarelli E, Zerhouni EGA, et al. Predicting coronavirus disease 2019 infection risk and related risk drivers in nursing homes: a machine learning approach. J Am Med Dir Assoc. 2020;21(11):1533‐1538. e1536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Telford CT, Bystrom C, Fox T, et al. COVID‐19 infection prevention and control adherence in long‐term care facilities, Atlanta, Georgia. J Am Geriatr Soc. 2021;69(3):581‐586. [DOI] [PubMed] [Google Scholar]
- 30. Temkin‐Greener H, Guo W, Mao Y, Cai X, Li Y. COVID‐19 pandemic in assisted living communities: results from seven states. J Am Geriatr Soc. 2020;68(12):2727‐2734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Travers JL, Agarwal M, Estrada LV, et al. Assessment of coronavirus disease 2019 infection and mortality rates among nursing homes with different proportions of black residents. J Am Med Dir Assoc. 2021;22(4):893‐898. e892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Unruh MA, Yun H, Zhang Y, Braun RT, Jung HY. Nursing home characteristics associated with COVID‐19 deaths in Connecticut, New Jersey, and New York. J Am Med Dir Assoc. 2020;21(7):1001‐1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. White EM, Kosar CM, Feifer RA, et al. Variation in SARS‐CoV‐2 prevalence in U.S. skilled nursing facilities. J Am Geriatr Soc. 2020;68(10):2167‐2173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Zimmerman S, Dumond‐Stryker C, Tandan M, et al. Nontraditional small house nursing homes have fewer COVID‐19 cases and deaths. J Am Med Dir Assoc. 2021;22(3):489‐493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Chen MK, Chevalier JA, Long EF. Nursing home staff networks and COVID‐19. Proc Natl Acad Sci U S A. 2021;118(1):e2015455118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Sugg MM, Spaulding TJ, Lane SJ, et al. Mapping community‐level determinants of COVID‐19 transmission in nursing homes: a multi‐scale approach. Sci Total Environ. 2021;752:141946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kumar A, Roy I, Karmarkar AM, et al. Shifting US patterns of COVID‐19 mortality by race and ethnicity from June–December 2020. J Am Med Dir Assoc. 2021;22(5):966‐970.e963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Gilman M, Bassett MT. Trends in COVID‐19 death rates by racial composition of nursing homes. J Am Geriatr Soc. 2021. 10.1111/jgs.17289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. McGarry BE, Gandhi AD, Grabowski DC, Barnett ML. Larger nursing home staff size linked to higher number of COVID‐19 cases in 2020. Health Aff (Millwood). 2021;40(8):1261‐1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Ryskina KL, Yun H, Wang H, Chen AT, Jung HY. Characteristics of nursing homes by COVID‐19 cases among staff: March to August 2020. J Am Med Dir Assoc. 2021;22(5):960‐965. e961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Weech‐Maldonado R, Lord J, Davlyatov G, Ghiasi A, Orewa G. High‐minority nursing homes disproportionately affected by COVID‐19 deaths. Front Public Health. 2021;9(246):606364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Williams CS, Zheng Q, White AJ, et al. The association of nursing home quality ratings and spread of COVID‐19. J Am Geriatr Soc. 2021;69(8):2070‐2078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Cai S, Yan D, Intrator O. COVID‐19 cases and death in nursing homes: the role of racial and ethnic composition of facilities and their communities. J Am Med Dir Assoc. 2021;22(7):1345‐1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Mehta HB, Li S, Goodwin JS. Risk factors associated with SARS‐CoV‐2 infections, hospitalization, and mortality among US nursing home residents. JAMA Netw Open. 2021;4(3):e216315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Telford CT, Onwubiko U, Holland DP, et al. Preventing COVID‐19 outbreaks in long‐term care facilities through preemptive testing of residents and staff members—Fulton County, Georgia, March–May 2020. MMWR Morb Mortal Wkly Rep. 2020;69(37):1296‐1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Konetzka RT, Gorges RJ. Nothing much has changed: COVID‐19 nursing home cases and deaths follow fall surges. J Am Geriatr Soc. 2021;69(1):46‐47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. McGarry BE, Grabowski DC, Barnett ML. Severe staffing and personal protective equipment shortages faced by nursing homes during the COVID‐19 pandemic. Health Aff (Millwood). 2020;39(10):1812‐1821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. McGarry BE, SteelFisher GK, Grabowski DC, Barnett ML. COVID‐19 test result turnaround time for residents and staff in US nursing homes. JAMA Intern Med. 2021;181(4):556‐559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. United States Government Accountability Office . Covid‐19 In Nursing Homes: HHS Has Taken Steps in Response to Pandemic, but Several GAO Recommendations Have Not Been Implemented . 2021. GAO‐21‐402T:. https://www.gao.gov/products/gao-21-402t
- 50. Centers for Medicare & Medicaid Services . Trump Administration Unveils Enhanced Enforcement Actions Based on Nursing Home COVID‐19 Data and Inspection Results 2020; https://www.cms.gov/newsroom/press-releases/trump-administration-unveils-enhanced-enforcement-actions-based-nursing-home-covid-19-data-and. Accessed May 8, 2021.
- 51. U.S. Department of Health and Human Services . Trump Administration Announces $2 Billion Provider Relief Fund Nursing Home Incentive Payment Plans. 2020; https://www.hhs.gov/about/news/2020/09/03/trump-administration-announces-2-billion-provider-relief-fund-nursing-home-incentive-payment-plans.html. Accessed May 8, 2021.
- 52. Berklan JM. Nursing homes criticize CMS chest‐thumping about $15.5M pandemic fines, severe citations McKnight's Long‐Term Care News , 2020.
- 53. White EM, Wetle TF, Reddy A, Baier RR. Front‐line nursing home staff experiences during the COVID‐19 pandemic. J Am Med Dir Assoc. 2021;22(1):199‐203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Bostick JE, Rantz MJ, Flesner MK, Riggs CJ. Systematic review of studies of staffing and quality in nursing homes. J Am Med Dir Assoc. 2006;7(6):366‐376. [DOI] [PubMed] [Google Scholar]
- 55. Castle NG. Nursing home caregiver staffing levels and quality of care—a literature review. J Appl Gerontol. 2008;27(4):375‐405. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Table of Evidence Summarizing Studies of COVID‐19 Outcomes in U.S. Nursing Homes and Assisted Living Communities


