Abstract
Background: The COVID-19 pandemic brought about great transformation to medical education mode. Although mobile communication devices played a crucial role in online learning among quarantined university students, the potential smartphone addition problems, negative health behaviors, and psychological symptoms need considerable attention. This study examined the relationship of problematic smartphone use (PSU), sleep quality, and daytime fatigue among medical students.
Methods: A web-based survey was conducted in six polyclinic hospitals in Beijing between February and May 2020. 1016 participants (26.01 ± 2.46 years, 65.16% female) completed self-report measurements including Short Version Smartphone Addiction Scale (SAS-SV), Athens Insomnia Scale (AIS), and Subjective Fatigue Scale (FS). Spearman correlation coefficients and multiple regression models were used to analyze the association among PSU, sleep quality, and daytime fatigue. We used structural equation modeling to test the mediating effect of sleep quality between PSU and daytime fatigue.
Results: 49.70% of the participants had PSU. Significant positive correlations were found among SAS-SV, AIS, and FS scores (r = 0.35–0.61, PS < 0.001). Subjects with PSU were more likely to report sleep disturbance (β = 1.07, P < 0.001, OR = 2.91, 95%CI = 2.17–3.91), physical fatigue (β = 1.16, P < 0.001, OR = 3.18, 95%CI = 2.45–4.15), and mental fatigue (β = 0.88, P < 0.001, OR = 2.42, 95%CI = 1.86–3.14). The indirect effect of PSU on physical fatigue and mental fatigue mediated by sleep quality accounted for 50.03 and 45.43% of the total effect, respectively.
Conclusions: PSU was significantly associated with sleep disturbance and fatigue among medical students during the COVID-19 pandemic. Sleep quality mediated the relationship between PSU and daytime fatigue. Our results provide valuable information for maintaining medical students' health status and constructing online education structures.
Keywords: problematic smartphone use, sleep quality, fatigue, mediating effect, COVID-19
Introduction
Since December 2019, an acute respiratory infectious disease caused by a novel coronavirus (SARS-CoV-2) broke out in Wuhan, China. The World Health Organization named it Coronavirus Disease 2019 (COVID-19) and declared on March 11 that the COVID-19 outbreak was a global pandemic (1). Recently emerged SARS-CoV-2 delta variants spreading in China and worldwide gave rise to a new wave of pandemics (2). The COVID-19 pandemic, a public health emergency, has had significant impacts on China's healthcare and medical education system (3), as governments adopted strict control measurements to require people to stay at home for social distancing (4). Many scholars have expressed their concerns about the online medical education in current and future pandemics (5, 6). One critical issue is that with the rapid development of communication technology, smartphone addiction and related clinical symptoms may surge among student populations. A cross-sectional online survey conducted by Chen and colleagues showed that primary school children who had psychological distress during the COVID-19 outbreak might spend longer time on Internet-related activities (7). The relationship between PSU and psychological distress has been influenced by the COVID-19, which has been confirmed by Chen's another longitudinal Study (8). Some scholars identified the overuse of smartphones as a hidden crisis during the pandemic (9), and this issue has been highlighted by recent literatures in China. A recent national survey among 746, 217 Chinese college students showed that the risks of developing depression and anxiety disorders increased with the exposure time to electronic devices (10). Another cross-sectional study showed that the level of COVID-19 related anxiety symptoms was correlated with the severity of problematic smartphone use (PSU) among Chinese adults (11). Many studies indicated that smartphone overuse directly impacts daytime functions and sleep quality (12–14), while the relationship has not been identified under the influence of the COVID-19 pandemic among medical students.
During the pandemic, medical students under quarantine relied heavily on the Internet and smartphone technology to complete heavy academic tasks and obtain the COVID-19 related information. Since medical students are more sensitive when tracking the pandemic information using smart deceives, their psychological patterns may differ from those of the general population (15). Thus, more studies about medical students are needed to cope with the transformation of the health care and education system. Colleges in Beijing have implemented measures to delay college students' return to school and required them to stay at home or in dormitories since January 2020. During an extended period of home isolation, university students' various living habits might change, among which the overuse of smartphones along with the resulting physical and mental health problems needs to be considered. Problematic smartphone use has been previously defined as excessive use of a smartphone that is accompanied by functional impairments in daily living, and substance addiction-like symptoms (16). PSU can cause many detrimental physical and psychological disorders and it has become a mental health threat to university students (17). A longitudinal study showed that the initial level of problematic use of smartphone/internet increased the psychological distress among university students in Hong Kong (18). Fatigue, defined as a subjective feeling of tiredness, weakness and discomfort, is now widely recognized as a premorbid state and causative factor (19). In clinical practice, physical fatigue and mental fatigue have specific symptoms.
Recent studies revealed that the intensity and time of electronic devices usage were relatively high during the COVID-19 pandemic, along with the increased incidence of smartphone addiction (20, 21), which could induce adverse behavioral and health outcomes (22, 23). Several studies have discussed the psychological and clinical mechanisms of the smartphone addiction issues, which are beneficial to support our hypotheses. In Billieux's pathway models, psychological, biological, social, and environmental factors play multiple roles in predicting PSU and are associated with various dysfunction symptoms (24). According to the Person-Affect-Cognition-Execution Model (I-PACE) of Internet addiction, individual factors such as physiology, personality, emotion, cognition, and executive function can significantly predict Internet addiction (25). In a study on undergraduate students, a combination of alexithymia, dissociative experiences, low self-esteem, and impulse dysregulation was confirmed to be a potential risk factor for Internet Addiction (26). As the Compensatory Internet Use Theory (CIUT) described, if individuals are in a negative situation, they may escape reality by surfing the internet, thus increasing the chance of addiction symptoms (27). The COVID-19 pandemic can be regarded as an unanticipated hostile incident, and people's mental health has been adversely affected, which further aggravates the possibility of dependence on smartphones (28). In addition to the above psychological models, clinical mechanisms are beneficial to support our theoretical model regarding the relationship of PSU, sleep quality, and daytime fatigue. Blue light and electromagnetic radiation emitted by smartphones directly cause harm to users' eyesight, neck, and spine (14, 29). Suppression of melatonin secretion caused by light stimulation at night is also a commonly recognized physiological pathway that results in sleep deprivation (30). As the skeletal muscle is a peripheral clock organ closely related to circadian rhythm, sleep disturbance may cause daytime physical symptoms by inhibiting mitochondrial activity (31). Besides, abnormal cortisol and hypothalamic-pituitary-adrenal cortex (HPA) axis functions have been confirmed as neuroendocrinology pathways of the association between sleep quality and mental fatigue (32). Based on the above mechanisms, we hypothesize that sleep disturbance is not only a direct adverse outcome of PSU, but also an important mediator of the relationship between PSU and daytime fatigue. Previous studies also showed that sleep quality played an intermediary role between smartphone overuse and various health issues (33–35). Thus, we built a theoretical partial mediation model and the following four hypotheses will be tested in the current study.
Hypothesis 01 (H01): PSU level is positively correlated with sleep disturbance.
Hypothesis 02 (H02): PSU level is positively correlated with daytime fatigue.
Hypothesis 03 (H03): Sleep quality is negatively correlated with daytime fatigue.
Hypothesis 04 (H04): Sleep quality mediate the relationship between PSU and daytime fatigue.
Materials and Methods
Participants and Ethics
Participants were 1,016 full-time medical postgraduates from six polyclinic hospitals affiliated to Peking University Health Science Center or Peking Union Medical College in Beijing. Data was collected from the Beijing Hospital (n = 208), the First Hospital of Peking University (n = 112), the People's Hospital of Peking University (n = 148), the Third Hospital of Peking University (n = 189), the Peking Union Medical College Hospital (n = 251), and the Cancer Hospital of the Chinese Academy of Medical Sciences (108). In each hospital, more than 50% of the total graduate students were recruited. The Ethics Committee of Beijing Hospital approved the study protocol (2020BJYEC-231-01).
Procedures
Since college students in Beijing were quarantined at home or at school until July 2020, a cross-sectional online questionnaire survey was conducted between February and May 2020 through a widely used social network application, “WeChat.” Data was collected by hospital administrators. The background and purpose of the survey, as well as the data consent were explained on the first page of the questionnaire. Each respondent could receive the feedback report via email and get compensation ranging from 3 to 10 yuan after submission. 1108 questionnaires were collected, and questionnaires with one of the following conditions were considered invalid: the response time was less than 5 min (n = 28); the individual's demographic information could not be identified (n = 8); all questions in the three scales used in this study were all answered repeatedly (n = 56). A total of 92 invalid questionnaires were excluded, and 1016 valid questionnaires were included in the final analysis, with an effective recovery rate of 91.70%. The education level was divided into master's and doctoral; the degree type was divided into academic and professional. An annual household income of <100,000 yuan was considered poor. The specialties were clinical medicine and others (including biology, preventive medicine, nursing, etc.). The student's relationship with the tutors was collected using a positive likert-5 single question (1–3 points = “bad”; 4–5 points = “good”). If the subjects self-reported regular exercise, they were defined as having exercise habits; and those who self-reported occasional exercise or no exercise were defined as having no exercise habit.
Measurements
Short Version Smartphone Addiction Scale
The 10-item Short Version Smartphone Addiction Scale (SAS-SV) developed by Kwon et al. was used to measure PSU (36). The scale consists of ten positive 6-point Likert questions describing the usage of smartphones, and the summed score ranges from 10 to 60. An example question was “Having my smartphone in my mind even when I am not using it.” The subjects were asked how much they agreed with each question (1 point = “disagree”; 6 points = “agree”). According to the threshold recommended for student populations, males with a summed score ≥ 31 and females with a summed score ≥ 33 were identified with PSU. The SAS-SV is the most widely used instrument to assess PSU and has been proved to have good reliability and validity in the Chinese population (37). In this study, the Cronbach's α coefficient of the scale is 0.91.
Athens Insomnia Scale
Sleep quality was measured with the Athens Insomnia Scale (AIS), a self-assessment psychometric instrument including eight 6-point Likert items with a total score of 0–24. Eight items in the AIS are related to sleep induction, awakenings during the night, final awakening, total sleep duration, sleep quality, well-being, functioning capacity, and sleepiness during the daytime. The Chinese version of AIS has been confirmed to be reliable and valid among adolescents and adults (38). As previous studies suggested, individuals with a summed AIS score ≥ 6 were classified as having sleep disturbance (39). In this study, the Cronbach's α coefficient of AIS was 0.87.
Subjective Fatigue Scale
Daytime fatigue was measured with a 14-item subjective fatigue scale (FS) developed by Chalder et al. (40). The FS consists of 14 two-category fatigue symptom self-assessment items and the scale showed appropriate validity for Chinese populations (41). The answer “yes” is counted as 1 point, the answer “no” is counted as 0, and the total score ranges from 0 to 14. Higher summed FS scores indicate a higher risk of daytime fatigue. Considering the lack of consensus on the cutoff value of the FS, we regard a summed score higher than or equal to 7 as a threshold of daytime fatigue. In the FS, 8 items reflected physical fatigue, and subscale score ≥4 was used as a cutoff; the last 6 items reflected mental fatigue, and subscale score ≥3 was used as a cutoff. In this study, the Cronbach's α coefficient of the FS was 0.84.
Statistical Analysis
Continuous variables were described as the mean ± standard deviation (M ± SD), and categorical variables were described as numbers with percentage [n (%)]. Student's t-test and χ2 test were used to compare the differences of SAS-SV scores across subgroups. Spearman correlation coefficient was used to analyze the association among SAS-SV, AIS, and FS scores. Multiple logistic regressions were used to analyze the association between PSU and the risk of fatigue and sleep disturbance. Subjects without PSU were used as the reference group and potential confounders were adjusted. We conducted a structural equation model (SEM) with robust weighted least squares estimation to test the mediating effect of sleep quality between PSU and daytime fatigue. A bias-corrected bootstrap method was used to test the significance of effect values in the SEM, and 1,000 random samples were put back from the original sample to calculate the 95% confidence intervals. Effect values were statistically significant if the 95% confidence interval did not include 0. Statistical analyses were performed using SPSS 24.0 version and Mplus 8.0 version. Statistical significance was accepted at the two-sided 0.05 level.
Results
Demographic Characteristics
A total of 1016 graduate students completed the questionnaire with an average age of 26.01 ± 2.46 years. Among the participants, 65.16% were female, 61.81% were master's students, 55.02% had a professional degree type, 77.46% majored in clinical medicine, 31.69% were first-year graduate students, and 34.55% lived in rural areas.
Problematic Smartphone use Status
The mean SAS-SV score of the participants was 32.73 ± 9.85, and 49.70% had PSU. As Table 1 showed, participants who had PSU were more likely to be male, have professional degree type, non-clinical medicine major, lower household income, live in rural areas, have a bad relationship with tutors, and have no exercise habits (Ps < 0.05).
Table 1.
Characteristics and PSU status of 1,016 medical students.
| Characteristics | N |
PSU (n = 505) |
Non-PSU (n = 511) |
t/χ2 | P-value | |
|---|---|---|---|---|---|---|
| Age (mean ± SD) | 1016 | 25.75 ± 2.35 | 26.25 ± 2.54 | 3.244 | 0.001 | |
| Gender [n (%)] | Male | 354 | 191(53.95) | 163(46.05) | 3.929 | 0.048 |
| Female | 662 | 314(47.43) | 348(52.57) | |||
| Education [n (%)] | Master | 628 | 316(50.32) | 312(49.68) | 0.248 | 0.618 |
| Doctoral | 388 | 189(48.71) | 199(51.29) | |||
| Degree [n (%)] | Academic | 457 | 201(43.98) | 256(56.02) | 10.901 | 0.001 |
| Professional | 559 | 304(54.38) | 255(45.62) | |||
| Residence [n (%)] | Rural | 351 | 194(55.27) | 157(44.73) | 6.654 | 0.009 |
| Urban | 665 | 311(46.77) | 354(53.23) | |||
| Household Income [n (%)] | Poverty | 523 | 287(54.88) | 236(45.12) | 11.551 | <0.001 |
| Non-poverty | 493 | 218(44.22) | 275(55.78) | |||
| Major [n (%)] | Clinical medicine | 787 | 370(47.01) | 417(52.99) | 10.153 | 0.001 |
| Others | 229 | 135(58.95) | 94(41.05) | |||
| Relationship with tutors [n (%)] | Good | 860 | 415(48.26) | 445(51.74) | 4.718 | 0.029 |
| Bad | 156 | 90(57.69) | 66(42.31) | |||
| Exercise habits [n (%)] | Yes | 392 | 157(40.05) | 235(59.95) | 6.315 | 0.007 |
| No | 624 | 393(62.98) | 231(37.02) | |||
| Sleep disturbance [n (%)] | Yes | 717 | 411(57.32) | 306(42.68) | 57.607 | <0.001 |
| No | 299 | 94(31.44) | 205(68.56) | |||
| Daytime fatigue [n (%)] | Yes | 407 | 268(65.85) | 139(34.15) | 71.741 | <0.001 |
| No | 609 | 237(38.92) | 372(61.08) | |||
| Physical fatigue [n (%)] | Yes | 568 | 354(62.32) | 214(37.68) | 83.291 | <0.001 |
| No | 448 | 151(33.71) | 297(66.29) | |||
| Mental fatigue [n (%)] | Yes | 443 | 278(62.75) | 165(37.25) | 54.004 | <0.001 |
| No | 573 | 227(39.62) | 346(60.38) |
PSU, problematic smartphone use; SD, standard deviation.
Associations Among SAS-SV, AIS, and FS Scores
The mean score of AIS was 8.09 ± 4.59, and 70.57% of the subjects had sleep disturbance. The mean score of FS was 6.42 ± 3.74, and 40.06% had daytime fatigue. Specifically, 55.91% of the subjects had physical fatigue, and 43.60% had mental fatigue, respectively. As Table 2 showed, the SAS-SV score was positively correlated with the AIS score (r = 0.38, P < 0.001) and fatigue scores (r = 0.35–0.41, P < 0.001). The AIS scores were positively correlated with fatigue scores (r = 0.48–0.61, P < 0.001).
Table 2.
Correlation coefficients among SAS-SV, AIS, and FS scores.
| Measurement | α | Mean | SD | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|---|---|---|
| 1. Problematic smartphone use | 0.91 | 32.73 | 9.85 | 1.00 | ||||
| 2. Sleep disturbance | 0.87 | 8.09 | 4.59 | 0.38*** (0.34***) | 1.00 | |||
| 3. Daytime fatigue | 0.84 | 6.42 | 3.74 | 0.41*** (0.39***) | 0.61*** (0.55***) | 1.00 | ||
| 4. Physical fatigue | 0.81 | 4.16 | 2.45 | 0.37*** (0.35***) | 0.58*** (0.54***) | 0.92*** (0.90***) | 1.00 | |
| 5. Mental fatigue | 0.72 | 2.26 | 1.77 | 0.35*** (0.39***) | 0.48*** (0.51***) | 0.84*** (0.81***) | 0.56*** (0.52***) | 1.00 |
P < 0.001.
α: Cronbach's alpha coefficient.
Partial correlation coefficients are shown in parentheses, controlling for age, gender, degree type, household income, major, residence, relationship with tutors, and exercise habits.
SAS-SV, Short Version Smartphone Addiction Scale; AIS, Athens Insomnia Scale; FS, Subjective Fatigue Scale; SD, standard deviation.
In the multiple logistic regression analyses (Table 3), SAS-SV, AIS, and FS scores were involved as dichotomous variables according to corresponding cutoffs. Gender, degree type, household income, major, residence, relationship with tutors, and exercise habits were involved as co-variables. After adjusting for potential confounders, subjects with PSU were more likely to report sleep disturbance (β = 1.07, P < 0.001, OR = 2.91, 95%CI = 2.17–3.91), daytime fatigue (β = 1.10, P < 0.001, OR = 2.99, 95%CI = 2.29–3.90), physical fatigue (β = 1.16, P < 0.001, OR = 3.18, 95%CI = 2.45–4.15), and mental fatigue (β = 0.88, P < 0.001, OR = 2.42, 95%CI = 1.86–3.14) than those without PSU.
Table 3.
Logistic regression analyses of PSU on sleep disturbance and fatigue.
| Models | Crude model | Adjusted modelΔ | |||||||
|---|---|---|---|---|---|---|---|---|---|
| β | SE | OR | 95%CI | β | SE | OR | 95%CI | ||
| Sleep disturbance | PSU | 1.47 | 0.11 | 2.92 | 2.21–3.89 | 1.07 | 0.15 | 2.91 | 2.17–3.91 |
| Non-PSU | Ref. | 1 | Ref. | 1 | |||||
| Daytime fatigue | PSU | 0.12 | 0.09 | 3.02 | 2.32–3.93 | 1.1 | 0.14 | 2.99 | 2.29–3.90 |
| Non-PSU | Ref. | 1 | Ref. | 1 | |||||
| Physical fatigue | PSU | 0.85 | 0.09 | 3.25 | 2.51–4.21 | 1.16 | 0.13 | 3.18 | 2.45–4.15 |
| Non-PSU | Ref. | 1 | Ref. | 1 | |||||
| Mental fatigue | PSU | 0.21 | 0.08 | 2.56 | 1.98–3.31 | 0.88 | 0.12 | 2.42 | 1.86–3.14 |
| Non-PSU | Ref. | 1 | Ref. | 1 | |||||
Adjusted model was adjusted for age, gender, degree type, household income, major, residence, relationship with tutors, and exercise habits.
β: Standardized regression coefficient.
Ref: Participants with non-PSU were reference category.
PSU, problematic smartphone use; SE, standard error; OR, odds ratio; CI: confidence interval.
Mediation Effect of Sleep Disturbance Between PSU and Fatigue
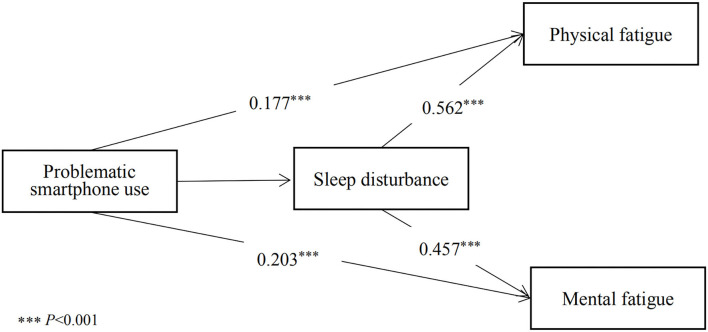
According to the theoretical hypothesis, a partial mediation model of sleep disturbance between PSU and daytime fatigue was built (Figure 1). Since the ordinal SAS, AIS, and FS scores did not meet the multivariate normal distribution, the path coefficients in the model were estimated by a robust weighted least square method. In the SEM, all the measurement variables were involved as manifest variables. As described in Table 4, all the standardized path coefficients were statistically significant (Ps < 0.001). The effect value of PSU on sleep disturbance was 0.370. The total effect of PSU on physical fatigue was 0.385 including a direct effect of 0.177, and the indirect effect mediated by sleep disturbance was 0.208, which accounted for 54.03% of the total effect. The total effect of PSU on mental fatigue was 0.372 including a direct effect of 0.203, and the indirect effect mediated by sleep disturbance was 0.169, which accounted for 45.43% of the total effect. The bias-corrected bootstrap methods showed that all the 95% confidence intervals of the effect values did not include 0 indicating statistical significance. To test the stability of the mediating mode, we also involved the measurement variables as dichotomous scores according corresponding cutoffs and re-calculated the pathway coefficients. The parameter estimation results are summarized in Supplementary Table 1, and effect values were proved to be statistically significant.
Figure 1.
Mediation models of problematic smartphone use, sleep disturbance, physical fatigue, and mental fatigue.
Table 4.
Path coefficients and effect values of PSU on sleep disturbance, physical fatigue, and mental fatigue.
| Pathway | β | SE | P-value | Total effect (95% CI) | Direct effect (95% CI) | Indirect effect (95% CI) |
|---|---|---|---|---|---|---|
| PSU → sleep disturbance | 0.37 | 0.014 | <0.001 | 0.370 (0.315, 0.420) | 0.370 (0.315, 0.420) | – |
| PSU → physical fatigue | 0.177 | 0.008 | <0.001 | 0.385 (0.331, 0.435) | 0.177 (0.127, 0.228) | 0.208 (0.174, 0.238) |
| PSU → mental fatigue | 0.203 | 0.006 | <0.001 | 0.372 (0.322, 0.429) | 0.203 (0.148, 0.259) | 0.169 (0.143, 0.198) |
| Sleep disturbance → physical fatigue | 0.562 | 0.018 | <0.001 | 0.562 (0.514, 0.604) | 0.562 (0.514, 0.604) | – |
| Sleep disturbance → mental fatigue | 0.457 | 0.014 | <0.001 | 0.457 (0.410, 0.505) | 0.457 (0.410, 0.505) | – |
β: standardized regression coefficient.
PSU, problematic smartphone use; SE, standard error; CI: confidence interval.
Discussion
In the current study, we identified the relationship of PSU, sleep quality, and daytime fatigue among medical university students during the COVID-19 pandemic. We obtained an unoptimistic incidence of PSU (49.70%) among quarantined medical students, which was higher than that of Chinese senior students (16.4%) from an online survey conducted on February 2020 (8). Consistent with our results, a cross-sectional study revealed a PSU prevalence of 59.42% in medical students from two provinces in China (42), and in another study the prevalence was 43.3% among Chinese adults (43). According to the I-PACE model and CIUT, the high prevalence of PSU among quarantined medical students was related to various factors (44). Firstly, Beijing has initiated a top-level response to major public health emergencies at the time of investigation and adopted social isolation policies. University students mainly relied on the Internet to communicate with the outside world, including social networking, shopping, learning, etc., which might aggravate smartphone overuse. Secondly, medical students had heavy academic burden during the pandemic. They needed to complete various learning and research objectives through virtual education platforms. In addition, when in-person communication with tutors became less frequent, the pressure and anxiety level would also increase, which might be incentives of PSU. Researches have revealed that smartphone overuse was closely related to depression, anxiety, and other psychological disorders (12, 45), and these correlations have also been confirmed in several investigations conducted during the pandemic (11). Thirdly, with the continuous unfolding of the COVID-19 pandemic, college students are worried about the social stability and health status of their family and friends; thus, they have increased demand to browse online information through smartphones daily. A longitudinal ecological study from the United States showed that along with the unfold of COVID-19, college students used more smartphones, had less physical activity, and visited fewer outdoor places (20). In this study, we identified several types of college students who were more susceptible to have PSU during the pandemic, which was supported by the CIUT. Male, professional degree type, low income, living in rural, poor relationship with tutors and inactivity were potential risk factors. Among quarantined medical students, daytime fatigue was commonly observed (40.06%), of which the prevalence of physical and mental fatigue was 55.91 and 46.60%, respectively. In another cross-sectional study, the prevalence of fatigue was 67.3% among Chinese nursing students in post-COVID-19 era (46). We also found a high prevalence of sleep disturbance (70.57%) in this sample. A recent review study including 12,682 respondents showed that the pooled prevalence of insomnia was 30% in Chinese frontline healthcare workers during the COVID-19 pandemic (47). Several studies also reported various physical and mental health outcomes were associated with the pandemic among healthcare workers, adolescents, and adults (48–50). Similarly to this study, a recent web-based survey showed that Indian undergraduate and postgraduate medical students had high level of perceived stress and anxiety during the COVID-19 pandemic (51).
SAS-SV score was significantly correlated with AIS score (r = 0.38) and medical students with PSU were more likely to report sleep disturbance (OR = 2.91). Lateef and colleagues also found a statistically significant positive correlation between Internet addiction and insomnia among clinical medical students in Africa (52). We confirmed the H-01 and the role of melatonin could account for the relationship between smartphone overuse and sleep deprivation, which has been confirmed by animal and human studies (29). Melatonin is one of the hormones secreted by the pineal gland, which helps sleep and regulates the circadian clock (53). The secretion of melatonin has an obvious circadian rhythm. Light stimulation during smartphone using at night will inhibit the activity of melatonin synthesis enzymes in the pineal gland, thus inhibiting the secretion of melatonin. We obtained significant correlations between SAS-SV score and FS score (r = 0.41), and H-02 was supported. Subjects with PSU were more likely to experience physical fatigue (OR = 3.18) and mental fatigue (OR = 2.42). Compared with the previous review studies, we have obtained larger odds ratios in this study (16, 54), suggesting that the pandemic might exaggerate the excessive use of smartphones and the corresponding daytime fatigue and sleep disturbance. Overuse of smartphones can lead to worsen upper limb pain (14). People who have smartphone addiction are more susceptible to blurred vision, back pain, wrist pain, stiff neck, and other health issues (14, 55). A recent systemic review reported that excessive and frequent smartphone usage increases the risk of headaches by 38% (56). Previous studies have also confirmed that PSU is associated with fatigue and physical dysfunction in student and adult samples (37, 57). In addition, factors such as introversion personality and negative emotions highlighted by the I-PACE model also contribute to the association between Internet addiction behaviors and daytime dysfunction. We found sleep quality was significantly associated with both physical fatigue and mental fatigue, and H-03 was supported. Firstly, although fatigue and sleep disturbance are defined as two independent, non-motor symptoms, they often overlap in clinical settings (58). People with fatigue often have difficulty in falling asleep and experience daytime sleepiness. In addition, the AIS and Pittsburgh Sleep Quality Index (PSQI), two most widely used sleep assessment scales, both contain components of daytime dysfunction, thus H-03 was conceptually supported. Secondly, the AIS score was significantly correlated with physical fatigue (r = 0.58). Skeletal muscle is not only one of the most important motor organs, but also the peripheral clock organ closely related to circadian rhythm. More than 2300 genes in skeletal muscle are expressed with circadian rhythm (31). Laboratory studies have shown that when circadian rhythm is disrupted, skeletal muscle fiber type displacement, sarcomere structure changes, and mitochondrial dysfunction are observed (59). In particular, reduced mitochondrial biosynthesis ability is a key regulatory process leading to skeletal muscle dysfunction and reduced human endurance (60). Thirdly, abnormal cortisol and melatonin function might be the main physiological mechanism of the correlation between AIS score and mental fatigue (r = 0.48). Cortisol is a neuroendocrine hormone regulated by the hypothalamic-pituitary-adrenal cortex (HPA) axis, which can participate in body metabolism, activate the vitality of the nervous system, and regulate the function of the cardiovascular system (32). Circadian rhythm disorders can disrupt the secretion of cortisol, thereby weakening the body's ability to regulate the nervous system, leading to mental fatigue symptoms such as decreased daytime excitability, neurasthenia, and memory loss. Furthermore, H-04 was confirmed in our SEM analysis. In the relationship of PSU and daytime fatigue, sleep quality mediated 50.03 and 45.43% of the total effect on physical and mental symptoms, respectively. The significance of path coefficients in the SEM model demonstrated the vital mediating role of sleep quality. The indirect effect of sleep quality in our hypothetical model could be supported by the above physiological mechanisms such as circadian rhythm and neurohormone secretion. Previous studies have also shown that sleep quality plays an intermediary role in PSU and physical and psychological illness such as eye symptoms, body dysfunction, and emotional problems in student samples (33, 61). Our findings have explored potential mechanisms of PSU on daytime function and are beneficial for health intervention among college students.
The emergence of new SARS-CoV-2 variants has dramatically increased the potential risk of future pandemics (62). Therefore, the government and colleges should alert to the adverse effects of excessive smartphone use on clinical health symptoms during the pandemic, and accessible psychological counseling services are necessary for quarantined university students. Tutors should strengthen the interaction with students, establishing timely and effective guidance on students' academic progress. While improving the virtual learning platforms, it is also feasible to monitor students' smartphone usage frequency during the lockdown. Establishing a monitoring network system that can send out reminders of smartphone overuse would benefit students' mental and physical wellness. Several limitations should be acknowledged. Firstly, the results did not indicate any causal inferences due to the cross-sectional design, and longitudinal studies are needed to further explore the COVID-19 pandemics' influence. Secondly, although the web-based survey and convenient sampling mode was the best option to reach subjects during the lockdown period, it inevitably led to selection bias and response bias. Thirdly, although we used standard measurements to identify the problematic use of smartphones, our data were not sufficient to discuss the duration and specific purpose of smartphones usage, which might overestimate the true incidence of PSU. Health-related information was collected from self-reports, which were less reliable than clinical diagnoses. Fourthly, the subjects of this study were exclusively from one city, and the extrapolation of the results needs to be treated with caution. However, Beijing can be regarded as a representative city of outbreak prevention and control in China, which to some extent reflects the trend of the whole country.
Conclusions
In conclusion, during the pandemic of COVID-19, medical students in Beijing had serious smartphone overuse problems, which were associated with sleep disturbance, physical fatigue, and mental fatigue. Our study provided insights into the mechanism that sleep quality mediated the relationship between PSU and daytime fatigue, which was valuable evidence to suggest actions for maintaining university students' health status and constructing online education structures.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by The Ethics Committee of Beijing Hospital. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
CZ, PZ, DL, and JJ proposed the concept and design. CZ analyzed and interpreted the data and wrote the manuscript. JT, SS, MZ, JC, and GZ drafted and edited the manuscript. CZ, DL, and JJ supervised the study and obtained funding. All authors read and approved the final version of the manuscript.
Funding
This study was supported by the National Key R&D Program of China (Grant No. 2020YFC2002700), the Education and Teaching Research Project of Peking University Health Science Center (Grant No. 2020YB42), the Fundamental Research Funds for the Central University (Grant No. 3332021077), and Research Subject of Chinese Society for Academic Degree and Graduate Education (Grant No. A1-YX20180201-02).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We sincerely thank all investigators and students who participated in this study, for their joint effort and cooperation.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.755059/full#supplementary-material
References
- 1.Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. (2020) 395:470–3. 10.1016/S0140-6736(20)30185-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mallapaty S. COVID. Vaccines slash viral spread—but delta is an unknown. Nature. (2021) 596:17–8. 10.1038/D41586-021-02054-Z [DOI] [PubMed] [Google Scholar]
- 3.Smith CA. Covid-19: Healthcare students face unique mental health challenges. BMJ. (2020) 369:M2491. 10.1136/bmj.M2491 [DOI] [PubMed] [Google Scholar]
- 4.Lee Y, Lui LMW, Chen-Li D, Liao Y, Mansur RB, Brietzke E, et al. Government response moderates the mental health impact of COVID-19: a systematic review and meta-analysis of depression outcomes across countries. J Affect Disord. (2021) 290:364–77. 10.1016/j.jad.2021.04.050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rose S. Medical student education in the time of COVID-19. JAMA. (2020) 323:2131–2. 10.1001/Jama.2020.5227 [DOI] [PubMed] [Google Scholar]
- 6.Kaul V, Gallo de. Moraes A. Khateeb D, Greenstein Y, Winter G, Chae J, et al. Medical education during the COVID-19 pandemic. Chest. (2021) 159:1949–60. 10.1016/j.Chest.2020.12.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen C. Y., Chen I. H., Pakpour A. H., Lin C. Y, Griffiths M. D. Internet-related behaviors and psychological distress among schoolchildren during the COVID-19 school hiatus. Cyberpsychol Behav Soc Netw. (2021) 20:497. 10.1089/Cyber.2020.0497 [DOI] [PubMed] [Google Scholar]
- 8.Hu T, Wang Y, Lin L, Tang W. The mediating role of daytime sleepiness between problematic smartphone use and post-traumatic symptoms in COVID-19 home-refined adolescents child youth. Serv Rev. (2021) 126:106012. 10.1016/j.Childyouth.2021.106012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ratan ZA, Zaman SB, Islam SMS, Hosseinzadeh H. Smartphone overuse: a hidden crisis in COVID-19 health. Policy Technol. (2021) 10:21–2. 10.1016/j.Hlpt.2021.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ma Z, Zhao J, Li Y, Chen D, Wang T, Zhang Z, et al. Mental health problems and correlates among 746217 college students during the coronavirus disease 2019 outbreak in China. Epidemiol Psychiatr Sci. (2020) 29:E181. 10.1017/S2045796020000931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elhai JD, Yang H, McKay D, Asmundson G. COVID-19 anxiety symptoms associated with problematic smartphone use severity in Chinese adults. J Affect Disord. (2020) 274:576–82. 10.1016/j.jad.2020.05.080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Demirci K, Akgönül M, Akpinar A. Relationship of smartphone use severity with sleep quality, depression, and anxiety in university students. J Behav Addict. (2015) 4:85–92. 10.1556/2006.4.2015.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lemola S, Perkinson-Gloor N, Brand S, Dewald-Kaufmann JF, Grob A. Adolescents' electronic media use at night, sleep disturbance, and depressive symptoms in the smartphone age. J Youth Adolesc. (2015) 44:405–18. 10.1007/S10964-014-0176-X [DOI] [PubMed] [Google Scholar]
- 14.Lee M, Hong Y, Lee S, Won J, Yang J, Park S, et al. The effects of smartphone use on upper extremity muscle activity and pain threshold. J Phys Ther Sci. (2015) 27:1743–5. 10.1589/Jpts.27.1743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baker DM, Bhatia S, Browm S, Cambridge W, Kamarajah K, McLean KA. Medical student involvement in the COVID-19 response. Lancet. (2020) 395:1254. 10.1016/S0140-6736(20)30795-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Elhai JD, Dvorak RD, Levine JC, Hall B. Problematic smartphone use: a conceptual overview and systematic review of relations with anxiety and depression psychopathology. J Affect Disord. (2017) 207:251–9. 10.1016/j.jad.2016.08.030 [DOI] [PubMed] [Google Scholar]
- 17.Li Y, Li GX, Yu ML, Liu CL, Qu YT, Wu H. Association between anxiety symptoms and problematic smartphone use among chinese university students: the mediating/moderating role of self-efficacy. Front Psychiatry. (2021) 12:581367. 10.3389/Fpsyt.2021.581367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen IH, Pakpour AH, Leung H, Potenza MN, Su JA, Lin CY, et al. Comparing generalized and specific problematic smartphone/internet use: longitudinal relationships between smartphone application-based addiction and social media addiction and psychological distress. J Behav Addict. (2020) 9:410–9. 10.1556/2006.2020.00023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Smets EM, Garssen B, Bonke B, De Haes J. The multidimensional fatigue inventory (MFI) psychometric qualities of an instrument to assess fatigue. J Psychosom Res. (1995) 39:315–25. 10.1016/0022-3999(94)00125-O [DOI] [PubMed] [Google Scholar]
- 20.Huckins JF, DaSilva AW, Wang W, Hedlund E, Rogers C, Nepal SK, et al. Mental health and behavior of college students during the early phases of the COVID-19 pandemic: longitudinal smartphone and ecological momentary assessment study. J Med Internet Res. (2020) 22:E20185. 10.2196/20185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bilal, Latif F., Bashir M. F., Komal B, Tan D. Role of electronic media in mitigating the psychological impacts of novel coronavirus (COVID-19). Psychiatry Res. (2020) 289: 113041. 10.1016/j.Psychres.2020.113041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gottlieb M, Dyer S. Information and disinformation: social media in the COVID-19 crisis. Acad Emerg Med. (2020) 27:640–1. 10.1111/Acem.14036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hossain MT, Ahammed B, Chanda SK, Jahan N, Ela MZ, Islam M. Social and electronic media exposure and generalized anxiety disorder among people during COVID-19 outbreak in bangladesh: a preliminary observation. PLoS ONE. (2020) 15:E0238974. 10.1371/Journal.Pone.0238974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Billieux J. Problematic use of the mobile phone: a literature review and a pathways model. Curr Psychiatry Rev. (2012) 8:299–307. 10.2174/157340012803520522 [DOI] [Google Scholar]
- 25.Brand M, Wegmann E, Stark R, Müller A, Wölfling K, Robbins TW, et al. The interaction of person-affect-cognition-execution (I-PACE) model for addictive behaviors: update, generalization to addictive behaviors beyond internet-use disorders, and specification of the process character of addictive behaviors. Neurosci Biobehav Rev. (2019) 104:1–10. 10.1016/j.Neubiorev.2019.06.032 [DOI] [PubMed] [Google Scholar]
- 26.De Berardis D, D'Albenzio A, Gambi F, Sepede G, Valchera A, Conti CM, et al. Alexithymia and its relationships with dissociative experiences and internet addiction in a nonclinical sample. Cyberpsychol Behav. (2009) 12:67–9. 10.1089/cpb.2008.0108 [DOI] [PubMed] [Google Scholar]
- 27.Mo A, Xiao CA, Yy A, Pan ZA, Ye CB, Xw C, et al. Student-student relationship and adolescent problematic smartphone use: the mediating role of materialism and the moderating role of narcissism. Child Youth Serv Rev. (2020) 110:104766. 10.1016/j.Childyouth.2020.104766 [DOI] [Google Scholar]
- 28.Xia Y, Fan Y, Liu TH, Ma Z. Problematic internet use among residential college students during the COVID-19 lockdown: a social network analysis approach. J Behav Addict. (2021) 10:253–62. 10.1556/2006.2021.00028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu L, Deng H, Tang X, Lu Y, Zhou J, Wang X, et al. Specific electromagnetic radiation in the wireless signal range increases wakefulness in mice. Proc Natl Acad Sci U S A. (2021) 118:1–6. 10.1073/Pnas.2105838118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fonken LK, Nelson R. The effects of light at night on circadian clocks and metabolism. Endocr Rev. (2014) 35:648–70. 10.1210/er.2013-1051 [DOI] [PubMed] [Google Scholar]
- 31.Mayeuf-Louchart A, Staels B, Duez H. Skeletal MUSCLE FUNCTIONS AROUND THE CLOCK DIABETES. Obes Metab. (2015) 17 Suppl 1:39–46. 10.1111/dom.12517 [DOI] [PubMed] [Google Scholar]
- 32.Cleare AJ. The neuroendocrinology of chronic fatigue syndrome. Endocr Rev. (2003) 24:236–52. 10.1210/er.2002-0014 [DOI] [PubMed] [Google Scholar]
- 33.Xie X, Dong Y, Wang J. Sleep quality as a mediator of problematic smartphone use and clinical health symptoms. J Behav Addict. (2018) 7:466–72. 10.1556/2006.7.2018.40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hong W, Liu RD, Ding Y, Sheng X, Zhen R. Mobile phone addiction and cognitive failures in daily life: the mediating roles of sleep duration and quality and the moderating role of trait self-regulation. Addict Behav. (2020) 107:106383. 10.1016/j.Addbeh.2020.106383 [DOI] [PubMed] [Google Scholar]
- 35.Spagnoli P, Balducci C, Fabbri M, Molinaro D, Barbato G. Workaholism, intensive smartphone use, and the sleep-wake cycle: a multiple mediation analysis. Int J Environ Res Public Health. (2019) 16:1–13. 10.3390/Ijerph16193517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kwon M, Kim DJ, Cho H, Yang S. The smartphone addiction scale: development and validation of a short version for adolescents. PLoS ONE. (2013) 8:E83558. 10.1371/Journal.Pone.0083558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Luk TT, Wang MP, Shen C, Wan A, Chau PH, Oliffe J, et al. Short version of the smartphone addiction scale in chinese adults: psychometric properties, sociodemographic, and health behavioral correlates. J Behav Addict. (2018) 7:1157–65. 10.1556/2006.7.2018.105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chung KF, Kan KK, Yeung W. Assessing insomnia in adolescents: comparison of insomnia severity index, athens insomnia scale and sleep quality index. Sleep Med. (2011) 12:463–70. 10.1016/j.Sleep.2010.09.019 [DOI] [PubMed] [Google Scholar]
- 39.Soldatos CR, Dikeos DG, Paparrigopoulos T. The diagnostic validity of the athens insomnia scale. J Psychosom Res. (2003) 55:263–7. 10.1016/S0022-3999(02)00604-9 [DOI] [PubMed] [Google Scholar]
- 40.Chalder T, Berelowitz G, Pawlikowska T, Watts L, Wessely S, Wright D, et al. Development of a fatigue scale. J Psychosom Res. (1993) 37:147–53. 10.1016/0022-3999(93)90081-P [DOI] [PubMed] [Google Scholar]
- 41.Zhan YX, Zhao SY, Yuan J, Liu H, Liu YF, Gui LL, et al. Prevalence and influencing factors on fatigue of first-line nurses combating with COVID-19 in China: a descriptive cross-sectional study. Curr Med Sci. (2020) 40:625–35. 10.1007/S11596-020-2226-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Huang J, Tan Z, Xu H, Huang B, Chen Q, Li Z, et al. Association of smartphone addiction with daily behaviors and mental health during the COVID-19 pandemic among medical college students. Chin J Sch Health. (2021) 42: 713–718. 10.16835/j.Cnki.1000-9817.2021.05.018 [DOI] [Google Scholar]
- 43.Zhang MX, Chen JH, Tong KK, Yu EW, Wu A. M S Problematic smartphone use during the COVID-19 pandemic: its association with pandemic-related and generalized beliefs. Int J Environ Res Public Health. (2021) 18:1–11. 10.3390/Ijerph18115724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Arrivillaga C, Rey L, Extremera N. Psychological distress, rumination and problematic smartphone use among spanish adolescents: an emotional intelligence-based conditional process analysis. J Affect Disord. (2021) 296:1–8. 10.1016/j.jad.2021.09.021 [DOI] [PubMed] [Google Scholar]
- 45.Rathbone AL, Prescott J. The use of mobile apps and sms messaging as physical and mental health interventions: systematic review. J Med Internet Res. (2017) 19:E295. 10.2196/Jmir.7740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Liu S, Xi HT, Zhu QQ, Ji M, Zhang H, Yang BX, et al. The prevalence of fatigue among chinese nursing students in Post-COVID-19 era. PeerJ. (2021) 9:E11154. 10.7717/Peerj.11154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Xia L, Chen C, Liu Z, Luo X, Guo C, Liu Z, et al. Prevalence of sleep disturbances and sleep quality in chinese healthcare workers during the COVID-19 Pandemic: a systematic review and meta-analysis. Front Psychiatry. (2021) 12:646342. 10.3389/Fpsyt.2021.646342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kang L, Li Y, Hu S, Chen M, Yang C, Yang BX, et al. the mental health of medical workers in wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. (2020) 7:e14. 10.1016/S2215-0366(20)30047-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shi L, Lu ZA, Que JY, Huang XL, Liu L, Ran MS, et al. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw Open. (2020) 3:E2014053. 10.1001/Jamanetworkopen.2020.14053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. (2020) 88:901–7. 10.1016/j.bbi.2020.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sharma R, Bansal P, Chhabra M, Bansal C, Arora M. Severe acute respiratory syndrome coronavirus-2-associated perceived stress and anxiety among indian medical students: a cross-sectional study. Asian J Soc Health Behav. (2021) 4:98–104. 10.4103/shb.shb_9_21 [DOI] [Google Scholar]
- 52.Oluwole L, Obadeji A, Dada M. Surfing over masked distress: internet addiction and psychological well-being among a population of medical students. Asian J Soc Health Behav. (2021) 4:56–61. 10.4103/shb.shb_76_20 [DOI] [Google Scholar]
- 53.Arendt J, Skene D. Melatonin as a chronobiotic. Sleep Med Rev. (2005) 9:25–39. 10.1016/j.Smrv.2004.05.002 [DOI] [PubMed] [Google Scholar]
- 54.Sohn SY, Rees P, Wildridge B, Kalk NJ, Carter B. Prevalence of problematic smartphone usage and associated mental health outcomes amongst children and young people: a systematic review, meta-analysis and grade of the evidence. BMC Psychiatry. (2019) 19:1–10. 10.1186/S12888-019-2350-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Choi SW, Kim DJ, Choi JS, Ahn H, Choi EJ, Song WY, et al. Comparison of risk and protective factors associated with smartphone addiction and internet addiction. J Behav Addict. (2015) 4:308–14. 10.1556/2006.4.2015.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wang J, Su H, Xie W, Yu S. Mobile phone use and the risk of headache: a systematic review and meta-analysis of cross-sectional studies. Sci Rep. (2017) 7:12595. 10.1038/S41598-017-12802-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Park N, Lee H. Social implications of smartphone use: korean college students' smartphone use and psychological well-being. Cyberpsychol Behav Soc Netw. (2012) 15:491–7. 10.1089/Cyber.2011.0580 [DOI] [PubMed] [Google Scholar]
- 58.Hossain JL, Ahmad P, Reinish LW, Kayumov L, Hossain NK, Shapiro C. Subjective fatigue and subjective sleepiness: two independent consequences of sleep disorders? J Sleep Res. (2005) 14:245–53. 10.1111/j.1365-2869.2005.00466.x [DOI] [PubMed] [Google Scholar]
- 59.Gabriel BM, Zierath J. Circadian rhythms and exercise—re-setting the clock in metabolic disease. Nat Rev Endocrinol. (2019) 15:197–206. 10.1038/S41574-018-0150-X [DOI] [PubMed] [Google Scholar]
- 60.Gupta NJ. Lifestyle and circadian health: where the challenges lie? Nutr Metab Insights. (2019) 12:1178638819869024. 10.1177/1178638819869024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zou L, Wu X, Tao S, Xu H, Xie Y, Yang Y, et al. Mediating effect of sleep quality on the relationship between problematic mobile phone use and depressive symptoms in college students. Front Psychiatry. (2019) 10:1–7. 10.3389/Fpsyt.2019.00822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lopez Bernal J, Andrews N, Gower C, Gallagher E, Simmons R, Thelwall S, et al. Effectiveness of Covid-19 Vaccines Against the B.1.617.2 (Delta) Variant. N Engl J Med. (2021) 21:1–10. 10.1056/NEJMoa2108891 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.