Injection sclerotherapy is most effective for internal hemorrhoids, especially for patients with bleeding. However, traditional sclerotherapy via anoscope may cause iatrogenic risk and complications due to misplaced injections.[1] The flexible endoscopic sclerotherapy for internal hemorrhoids using a short needle without cap assistant was first reported in 1991 in the United States.[2] The flexible endoscopic injection using a short needle with cap assistant was reported in 2014 in Japan.[3] Cap-assisted endoscopic sclerotherapy (CAES) primarily using a long needle was reported in 2015[4] as an emerging flexible endoscopic therapy, and has been widely used for internal hemorrhoids and some prolapse in China. A panel of experts aimed to develop expert recommendations for CAES and derived guidelines on the key issues in hemorrhoidal disease, including rationale, new positioning methods for anus, indications, contraindications, techniques, post-procedure management, and core outcome set for evaluation [Figure 1].
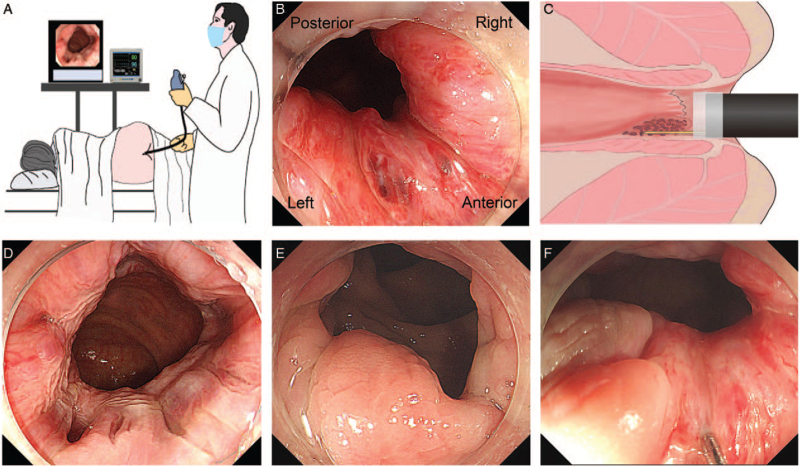
Figure 1.
CAES for internal hemorrhoids. (A) Colonoscopy in left lateral position. (B) Anus positioning methods under flexible endoscopy: along the clockwise direction, LPRA (with residual fluid or injected water). (C) The concept sketch of CAES. (D) The internal hemorrhoids under colonoscope, anterograde view, and proper insufflated air. (E) The small internal mucosal prolapse is located in the left-anterior anus. (F) Submucosal injection for internal hemorrhoids complicated with prolapse in the anterior anus. CAES: Cap-assisted endoscopic sclerotherapy; LPRA: Left anus, posterior anus, right anus, and anterior anus.
Methods and results for expert recommendations development: The modified three-round Delphi procedure was used for developing expert recommendations. Each invited expert did not know who else were invited before the third round. Each statement was accepted when ≥80% of the experts agreed. All statements were presented to 33 of 33 (100%) members on May 28, 2021, at the China Gut Conference, Nanjing, China. The full version of the Expert Recommendation is shown in [Supplementary File 1].
Rationale: The concept and value of CAES for hemorrhoidal disease mainly include: (1) Endoscope with cap and air delivery improves the endoscopic exposure for diagnosis and therapy, which should contribute to avoid iatrogenic injury due to ectopic injection; (2) CAES is an effective therapy for internal hemorrhoids bleeding, and an option for rectal mucosal prolapse; (3) Anorectal lesions differentiation, colon screening, and endoscopic therapy can be performed during the CAES procedure for better cost-efficacy.
Anus positioning methods: The residual fluid or injected water within the anus under endoscopy is the sign for determining the left anus under the left lateral decubitus position. Along the clockwise direction, left anus, posterior anus, right anus, and anterior anus (LPRA) is recommended to replace the typical lithotomy position for the precise direction description on the anal lesions and endoscopic therapy.
Based on the standard left lateral decubitus position for colonoscopy, the fluid accumulation is located on the left side of the anal canal [Figure 1A]. After confirming the position of the left side of the anus by the endoscopic injected water or the residual fluid, along the clockwise direction, the LPRA positioning method is practical, reliable, and a simple technique for physicians and patients to have direct and quick understanding. This LPRA four-direction description can be further divided into eight directions: left, left-posterior, posterior, right, right-posterior, anterior, right-anterior, and left-anterior. The LPRA positioning method for anal lesions and targeting therapy can improve the clinical workflow, scientific communications, and physician–patient communications [Figure 1B].
Indication 1: CAES for internal hemorrhoids. Patients with symptomatic Grade I or II internal hemorrhoids are considered for CAES when lifestyle intervention and conservative management are ineffective. CAES can be considered for patients with Grade III internal hemorrhoids unsuitable for surgery or those refusing surgery. Several studies have shown that flexible endoscopic sclerotherapy is effective minimally invasive therapy for Grades I–II internal hemorrhoids, with a relatively low occurrence of post-procedural pain and bleeding.[3,4] It has also been shown to be a safe and effective treatment for some Grade III hemorrhoids.[4,5]
Indication 2: CAES for internal mucosal prolapse. CAES is a therapeutic option for symptomatic small rectal mucosal prolapse. The most common symptoms of rectal mucosal prolapse are the protrusion itself, such as anal pendant expansion, obstruction feelings, and tenesmus. CAES with a long needle was reported as an effective therapy for small rectal mucosal prolapse,[4] however, more solid evidence is necessary.
Contraindications: The contraindications of CAES for hemorrhoids at least include patients with perianal abscess, stricture, fistula, anal malignancies, and pregnancy. CAES with conventional-dose injection is not recommended for patients with active proctitis, radiation enteritis, immune-related ulcer, or unexplained anal ulcer.
CAES can be considered as an option for bleeding hemorrhoids during an emergency in patients with cerebrovascular accidents, immunodeficiency, or hypercoagulability disorders after balancing potential risks and possible benefits from the interventional procedure. CAES is not recommended to treat thrombosed and strangulated hemorrhoids, Grade IV internal hemorrhoids, or external hemorrhoids. Psychiatric consultation should be recommended when a patient with hemorrhoid-like complaints has suspicious mental stability, such as hypochondriasis, hysterical reactions, and somatization of anal symptoms.[6]
Bowel preparation for CAES: Bowel preparation is recommended for meeting the criteria of the required colonoscopic diagnosis and therapy. Anesthesia assistance during CAES is helpful in improving physician–patient satisfaction.
Cap and air insufflation for CAES: Both conventional short-straight cap on the endoscope and the proper air insufflation are the key conditions for effective exposure and fluent therapy during the CAES procedure for the hemorrhoids and rectal prolapse [Figure 1C]. A conventional short-straight cap is recommended for maximizing visibility of the targeting field for diagnosis and injection [Figure 1D–F]. The colonoscope with the cap is helpful for preventing air leaking from the anus during injection of air for improving endoscopic exposure.
Choosing the needles and related consideration: The long or short injection needles should be considered according to the condition of hemorrhoidal disease.
The different techniques using long and short needles are shown in Supplementary Table 1. A long injection needle is defined as the length ≥10 mm. For patients only with bleeding hemorrhoids, both long and short needles can be selected for injection.[4,7] The long needle is recommended for the hemorrhoids combined with prolapse. The sclerosing agent is injected into the submucosal layer for about 5 s with 0.5 to 2.0 mL lauromacrogol per site.
Positioning and injection: The LPRA anus positioning method is helpful for the endoscopist to locate the injected and non-injected sites, thus avoiding the use of a tracer agent. The six o’clock position under endoscopic view is the recommended site for injection.[4] The sclerosing agents for treating internal hemorrhoids in China mainly include lauromacrogol, polidocanol, and traditional Chinese medicine (e.g., Xiaozhiling and Shaobei). Lauromacrogol is recommended to be injected with original fluid.
Post-CAES management 1: Patients post-CAES should remain in a supine position for at least 2 h to prevent prolapse and monitor potential short-term complications. Given the scarce literature, the supine position in bed for at least 2 h post-procedure is helpful for monitoring and managing the potential CAES-related complications in clinical practice.[4] Diets that might cause defecation during 6 to 12 h post-CAES should be avoided for patients.
Post-CAES management 2: Patients with chronic constipation or diarrhea should be treated with etiological treatment after CAES for preventing the recurrence of hemorrhoids. Both chronic constipation and diarrhea should be treated post-CAES.
Post-CAES management 3: Both antibiotics and hemostatics are not regularly required during and after the CAES procedure. No evidence supports the necessity of conventional use of antibiotics during or post-CAES. CAES has advantages in preventing iatrogenic risk from misplaced injections, which largely reduces the potential post-operative infections due to mucosal ulceration or necrosis, prostatic abscess, and others.[4]
Post-CAES management 4: CAES-associated complications mainly include difficulty in passing gas, bleeding, infection, ulcer, and chronic anal pain. The CAES procedure-associated complications were mainly reported from physicians who were in the early stage of CAES training.[7] Enema is the way to solve the difficulty in passing gas and defecation, and lower intestinal obstruction.[7]
Core outcome set for evaluation: The patient self-report based on both hemorrhoid-specific symptoms (pain, prolapse, blood loss, itching, and soiling) and life quality can be applied for efficacy evaluation of CAES in clinical practice and research. The patient-reported outcome measure based on both hemorrhoid-specific symptoms and patient quality of life has been widely applied to clinical practice and research of hemorrhoids. The primary outcome measurements, which included the core outcome, were sets of “pain”, “prolapse”, “blood loss”, “itching”, and “soiling”. Other additional domains, such as complications, recurrence, patient satisfaction, and others, were common sets of secondary outcomes.
To conclude, this expert opinion on the new anus positioning methods and the updated protocols of CAES will guide the research and practice of hemorrhoidal disease management.
Expert of CAES-LPRA Study Group
Fei-Hu Bai, Haikou; Shi-Yao Chen, Shanghai; Ye Chen, Shenzhen; Bo-Ta Cui, Nanjing; Ming-Ming Deng, Luzhou; Zhi-Ning Fan, Nanjing; Bai-Sui Feng, Zhengzhou; Xing-Xiang He, Guangzhou; Yun-Lian Hu, Wuhan; Xiao-Meng Jiang, Nanjing; Yan Jin, Wuxi; Jing-Nan Li, Beijing; Rong Lin, Wuhan; Tian-Yu Liu, Suining; Zhan-Guo Nie, Urumqi; Ying Song, Xi’an; Yang Sun, Kunming; Rong Wan, Shanghai; Fang-Yu Wang, Nanjing; Xin Wang, Xi’an; Wei Wei, Beijing; Yan-Ling Wei, Chongqing; Quan Wen, Nanjing; Kai-Chun Wu, Xi’an; Fang Xiao, Wuhan; Shi-Ming Yang, Chongqing; Ping Yao, Urumqi; Yu Yuan, Guangzhou; Hui-Hong Zhai, Beijing; Fa-Ming Zhang, Nanjing; Guo-Xin Zhang, Nanjing; Zhen-Yu Zhang, Nanjing; Yong-Jian Zhou, Guangzhou.
Funding
The development of the manuscript were funded by the Nanjing Medical University Fan Daiming Research Funds for Holistic Integrative Medicine. Unrestricted grants were provided by the Tianyu Pharmaceutical Co., Ltd and China Gut Conference for the meeting.
Conflicts of interest
None.
Supplementary Material
Supplementary Material
Footnotes
How to cite this article: Zhang FM, Wu KC, Li JN, Wang X, He XX, Wan R, Chen SY; CAES-LPRA Study Group. Rationale, new anus positioning methods, and updated protocols: Expert recommendations on cap-assisted endoscopic sclerotherapy for hemorrhoids from China Gut Conference. Chin Med J 2021;134:2675–2677. doi: 10.1097/CM9.0000000000001836
Supplemental digital content is available for this article.
References
- 1.Jacobs D. Clinical practice. Hemorrhoids. N Engl J Med 2014; 371:944–951. doi: 10.1056/NEJMcp1204188. [DOI] [PubMed] [Google Scholar]
- 2.Ponsky JL, Mellinger JD, Simon IB. Endoscopic retrograde hemorrhoidal sclerotherapy using 23.4% saline: a preliminary report. Gastrointest Endosc 1991; 37:155–158. doi: 10.1016/s0016-5107(91)70675-5. [DOI] [PubMed] [Google Scholar]
- 3.Tomiki Y, Ono S, Aoki J, Takahashi R, Sakamoto K. Endoscopic sclerotherapy with aluminum potassium sulfate and tannic acid for internal hemorrhoids. Endoscopy 2014; 46:E114.doi: 10.1055/s-0034-1364884. [DOI] [PubMed] [Google Scholar]
- 4.Zhang T, Xu LJ, Xiang J, He Z, Peng ZY, Huang GM, et al. Cap-assisted endoscopic sclerotherapy for hemorrhoids: methods, feasibility and efficacy. World J Gastrointest Endosc 2015; 7:1334–1340. doi: 10.4253/wjge.v7.i19.1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tomiki Y, Aoki J, Motegi S, Takahashi R, Hagiwara T, Okazawa Y, et al. Effectiveness of endoscopic sclerotherapy with aluminum potassium sulfate and tannic acid as a non-surgical treatment for internal hemorrhoids. Clin Endosc 2019; 52:581–587. doi: 10.5946/ce.2019.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van der Schans EM, Paulides TJC, Wijffels NA, Consten ECJ. Management of patients with rectal prolapse: the 2017 Dutch guidelines. Tech Coloproctol 2018; 22:589–596. doi: 10.1007/s10151-018-1830-1. [DOI] [PubMed] [Google Scholar]
- 7.Wu X, Wen Q, Cui B, Liu Y, Zhong M, Yuan Y, et al. Cap-assisted endoscopic sclerotherapy for internal hemorrhoids: technique protocol and study design for a multi-center randomized controlled trial. Ther Adv Gastrointest Endosc 2020; 13:2631774520925636.doi: 10.1177/2631774520925636. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.