Abstract
Scholarship linking social contextual measures to health outcomes has grown in recent decades, but the role of individuals’ intersecting identities in structuring social contexts to influence health remains unclear. Building on an existing intersectionality framework, we conceptualize how this may occur through social relationships. Then, we apply this framework to analyze whether adolescent peer social contextual disadvantage influences life-course obesity heterogeneously by individual gender, race, and early-life income. We take a life course approach as adolescence is a sensitive period for both social development and adult obesity development. In our analysis, we use cohort data from the National Longitudinal Study of Adolescent to Adult Health and leverage quasi-experimental variation in adolescent peers to addresses common sources of bias in prior observational studies. We find that among Black men from lower-income households in adolescence, there is a strong negative relationship between adolescent peer economic disadvantage and adult obesity that strengthens over time. By contrast, among Black women across adolescent household income levels, we find a strong positive relationship between adolescent peer economic disadvantage and obesity that emerges as women leave high school and endures into mid-adulthood. Among non-Black women, a more modest positive relationship appears between peer disadvantage and obesity. Among non-Black men, we find no relationship. These diverging patterns suggest that the pathways through which adolescent peer economic disadvantage influences health may differ or produce differential effects based on intersecting race, gender, and socioeconomic identities. Such heterogenous effects offer new insights, and future directions, for better understanding social life-course determinants of adult health and addressing inequities.
Keywords: Contextual disadvantage, obesity, intersectionality, life course, health disparities
Introduction
Scholarship on the relationship between social contexts, such as schools and neighborhoods, and health has grown in recent decades (Oakes et al. 2015). Various social contextual measures, such as school disadvantage, neighborhood poverty, and residential segregation, predict wide-ranging health outcomes, such as cancer, obesity, and birth outcomes (Kershaw, Albrecht and Carnethon 2013b; Mehra, Boyd and Ickovics 2017; Sheehan et al. 2017; Zahnd and McLafferty 2017). Social contextual effects models have been used to examine a combination of group-level and individual-level effects on individual-level outcomes, including interactive effects (Blalock 1984; Fletcher et al. 2019). However, most frequently, these models measure a contextual effect as a mean characteristic of a reference group while controlling for individual-level characteristics (Arcaya et al. 2016) rather than integrating these characteristics to potentially generate further understanding of health inequities.
In this paper, we have three aims. First, we extend an intersectionality framework to theorize how individual intersecting identities structure relationships within social contexts that result in health inequities. Second, we apply this framework to the early life contextual disadvantage and life course obesity literature. We use data from the National Longitudinal Study of Adolescent to Adult Health (Add Health) to measure heterogeneous impacts of school grade-mate peer socioeconomic disadvantage, namely peer lower-income status, on obesity by individual race, class, and gender identities. Finally, we employ a quasi-experimental design to overcome inherent biases in prior contextual effects research that approximates random assignment of adolescent peer social contexts within schools (Fletcher 2012; Gaviria and Raphael 2001).
We find that in response to increases in the proportion of grade-mate peers that are lower income during adolescence, obesity development through early-mid adulthood is heterogeneous by individual race, class, and gender identities. Most striking, we find large, positive effects for Black women and large, negative effects for lower-income Black men. Overall, we provide evidence that intersecting individual identities are likely to shape the social relationships that comprise social contexts, and can contribute to health inequities over the life course. Moreover, our findings point to the experience of school peer economic disadvantage in adolescence as particularly important in the development of life course obesity.
Background
Social Contexts, Social Relationships, and Health
An early criticism of social contextual effects models was that mean group-level characteristics cannot directly affect health outcomes (Erbring and Young 1979). Indeed, social contextual effects measured as mean group-level characteristics are better conceptualized as the sum of various indirect effects operating through social relationships and interactions within a particular context. Understanding the total effect of social contextual measures on health outcomes is important to identifying which social contexts influence health disparities, before narrowing down which social relationships within those contexts may be moderating the effects and how they are operating.
Social relationships influence health behaviors and human physiology through multiple mechanisms (Umberson, Crosnoe and Reczek 2010). For instance, within contexts, certain norms (e.g., drinking) may prevail or certain behaviors may have symbolic meaning and be viewed as higher status (e.g., risky behavior is considered “cool” among adolescents). Social control is another mechanism through which social ties monitor, remind, or threaten individuals to engage in healthy behaviors (e.g., parents monitor adolescents’ risky behavior). Moreover, social ties can provide social support, such as emotional support, information, or assistance with tasks, which can promote positive health behaviors and reduce physiological distress. Finally, stress can arise from negative social ties and lead to both negative health behaviors that may be employed as coping mechanisms as well as physiologic dysregulation (Umberson, Crosnoe and Reczek 2010).
Intersectionality Applied to Social Relationships in Contexts
Conceptualizing social contextual effects as sums across many social interactive pathways suggests that individuals and social ties relationally contribute to health behaviors and physiological changes. This implies a need to integrate into models, rather than control for, important individual-level characteristics, including race, class, and gender identities that may structure relationships, and thus health. We apply the concept of intersectionality to social relationships research to theorize how identities may relate to social ties in contexts.
The meanings of individual identities as micro-level measures or group measures are predicated on group location in interwoven systems of domination, i.e. where the group fits into the hierarchy of power and inequality (Andersen and Collins 2007). In particular, race, class, and gender remain important systems of inequality that give meaning to individual identities and structure individuals’ experiences in the U.S. (Andersen and Collins 2007). Intersectionality as a concept asserts that individuals may have multiple marginalized identities – e.g., race, class and gender – that interact to produce an experience or outcome that is different than the sum of the effect of each singular identity (Crenshaw 1989). Hulko (2009) builds on this concept to argue that the meaning and consequences of interacting identities, in terms of oppressions or privileges, should be understood in terms of context-dependent social location. This suggests that while identities may be assigned by macro-systems of inequality (e.g., U.S. socioeconomic systems), an individual’s experience of privilege or marginalization based on those identities is dependent on one’s relative position within meso-level contexts (e.g., schools).
The experience of privilege or marginalization at the individual level relies upon social interactions. Using an intersectional framework, it follows that the nature of social interactions within a social context will also depend on one’s relative position in that context, and thus the nature of social interactions can change as one’s social context changes. Indeed, sociological work on social interactions, particularly status organizing process work, provides additional theory and evidence that an individual’s external status—e.g. age, race, and sex—organizes social interactions within groups (Berger, Cohen and Zelditch 1972). The social interactive pathways that determine health, then, are influenced by the interaction of individual identity and peer context.
Thus, intersecting race, class, and gender identities may structure social relationships and social interactive pathways that connect individual privilege or marginalization to health outcomes in ways that are social context dependent. For example, Goosby and Walsemann (2012) found that Black students in predominantly white schools have poorer health outcomes in adulthood relative to Black students in schools with lower percentages of white students, with teacher discrimination as a potential pathway. In other words, the many social interactive pathways that determine individual health may differ or produce differential effects depending on the relative position of an individual’s status within the distribution of status characteristics of a group, where status may be based on multiple intersecting identities.
In this paper, we sum across all potentially competing social interactive mechanisms to measure the total effect of quasi-random changes in grade-mate peer economic context on obesity outcomes for race, SES, and gender subgroups. By narrowing social context to that of grade-mate peer economic disadvantage, we can use a quasi-experimental design that increases confidence that we are measuring heterogeneity in health outcomes due to the structuring of social interactive pathways by individual identities, and that this heterogeneity is not attributable to factors such as physical environment or homophily among peers. This provides a more credible demonstration of our intersectional approach than would an observational analysis.
Obesity and Social Contextual Disadvantage
We apply this intersectionality in social relationships framework to understand heterogeneity in the relationship between peer contextual economic disadvantage and obesity. We examine whether a measure of school, grade-mate peer economic disadvantage experienced in adolescence interacts with individual race, class, and gender identities to contribute to race, SES, and gender inequities in obesity in adulthood. Obesity is an ongoing public health concern due to its association with a variety of chronic conditions, including diabetes, hypertension, high cholesterol, and heart disease, as well as all-cause mortality (Flegal et al. 2013; Paeratakul et al. 2002). Adolescent and adult obesity rates have increased in recent decades, from around 13.9% of adolescents aged 12-19 labeled as obese in 1999-2000 to over 20% of adolescents in 2015-16, and from 30.5% of adults labeled as obese in 1999-2000 to 42.4% in 2017-18 (Fryar, Carroll and Ogden 2018; Hales et al. 2020). Like many other chronic conditions, inequities in obesity differ depending on individual identity characteristics, including socioeconomic status (SES), gender, and race. For example, non-Hispanic Black women are at significantly increased risk of obesity as compared to women belonging to other racial/ethnic categories (Hales et al. 2020). Moreover, women’s rates of obesity decline as their income levels increase, whereas men’s obesity rates increase with income (Carroll et al. 2010).
Obesity is also associated with contextual-level disadvantage in childhood and adulthood, measured at the level of peers, schools, and neighborhoods (Alvarado 2019; Fletcher and McLaughlin 2015; Kershaw, Albrecht and Carnethon 2013a; Kivimäki et al. 2018; Lee, Harris and Lee 2013; Sheehan et al. 2017). Evidence suggests that the association between obesity and social context depends upon individual identities, including race and gender (Yang and South 2018). For example, higher income inequality measured at the level of metropolitan statistical area is associated with lower overweight and obesity in white women, but not in white men, Black women, or Black men (Chang and Christakis 2005). Race and gender can influence obesity through various mechanisms. For instance, coping with perceived racism and racial segregation has the potential to alter stress responses and cortisol reactivity to increase BMI (Cozier et al. 2014). However, few studies have sought to measure how multiple intersecting identities interact with social context to determine life course obesity outcomes. Moreover, much of the work linking social contextual disadvantage, social relationships and obesity uses methods that inadequately control for common sources of bias in observational studies.
Adolescence as a Sensitive Period in Life Course Health and Obesity
There is a growing body of evidence that suggests social context and peer influence in adolescence are important in shaping life course health trajectories, particularly those related to BMI. Adolescence is a developmental period during which individuals are particularly vulnerable to stress, with consequences for metabolic dysregulation later in life (Pervanidou and Chrousos 2012). For example, Alvarado (2019) finds that neighborhood disadvantage during adolescence is more influential on adult obesity than during childhood, with social stress as a likely pathway. Furthermore, social contextual and peer influences on health lifestyles tend to emerge in adolescence, when individuals’ agency increases and parental monitoring declines (Mollborn and Lawrence 2018). Indeed, Lee, Harris and Lee (2013) find that school-level peer disadvantage in adolescence significantly explains obesity in adolescence and young adulthood.
Moreover, cumulative disadvantage theory suggests that exposure to disadvantage in early life can alter long-term obesity trajectories and differentiate cohort health outcomes through exposure to cascading health risks and feedback cycles (Ferraro and Kelley-Moore 2003). For instance, stress is one mechanism through which the process of cumulative disadvantage has been shown to operate. Regarding obesity, childhood stress exposure predicts stress exposure in adulthood. Both stress exposures are linked with obesity in women, but not men, and childhood stress is a more impactful predictor (Liu and Umberson 2015). Other social interactive mechanisms experienced in adolescence, such as social support, have also been demonstrated to influence health behaviors into early adulthood (Frech 2012). We incorporate a life course approach in our analysis to investigate whether peer social contextual disadvantage contributes to heterogeneity in obesity as it unfolds through early to middle adulthood.
Bias in Measuring Social Contextual Effects
From a causal standpoint, measurement of social contextual effects is a challenge as many sources of potential bias can impede estimation. First, the measurement of social context can reflect both characteristics of a shared environment and the social interactions that take place within an environment. For instance, in schools, both peer social interactions and school environment (e.g., school organized sports programs, school lunch programs, etc.) may influence obesity outcomes. To focus on social interaction effects, shared environment must be controlled, or coefficients could be biased upward or downward depending on the environmental characteristic.
Second, social contextual effects may reflect endogenous selection bias, such as homophily bias, wherein similar individuals are more likely to form social ties (Elwert and Winship 2014). For example, individuals that enjoy exercise may be inclined to join a sports team, through which they form social ties. However, to infer that teammate peers influence obesity, enjoyment of exercise would need to be controlled. Failure to adequately address homophily can contribute to a spurious associations, such as those between peer obesity and individual obesity (Cohen-Cole and Fletcher 2008). Third, confounding may occur if an unobserved variable links the average peer characteristic of interest with changes in individual outcomes. For example, neighborhoods frequently define school catchment areas, and hence peer groups. Neighborhoods also may determine obesity outcomes via access to grocery stores and safe outdoor spaces in which to exercise. Neighborhood therefore confounds the relationship between peer characteristics and individual obesity when uncontrolled, potentially inflating effect size estimates as neighborhood disadvantage is also associated with increased obesity in some groups (Alvarado 2016). We employ quasi-experimental methods to address these forms of bias.
Methods
In this study, we ask whether exposure to school grade-mate peer disadvantage in adolescence increases obesity risk across the life course. We seek to approximate a random experiment in which school grade-mate peers are randomly assigned to individuals, thus minimizing bias. We compare students within schools that are exposed to different sets of grade-mate peers, controlling for school fixed effects, grade fixed effects, whether students skipped grades or were held back grades, and age fixed effects. These controls help to isolate quasi-random variation in peer social context through the following logic. School fixed effects control for the various mechanisms that select students into schools, such as economic and racial segregation, as well as fixed characteristics of the school environment. Within schools, students are unlikely to select into grades, except by skipping a grade or being held back, which we further control. This leaves an individual’s grade-mate peers primarily determined by their birth dates in relation to school start dates. This peer variation is idiosyncratic and thus should be unrelated to individual background characteristics, approximating an experiment. Moreover, by measuring exposure to grade-mate peers rather than individually identified friendships we control for homophily bias, making the analysis like an intent-to-treat design.
Overall, this approach helps to ensure that we are measuring the effects of social relationships within school grade-mate peer contexts and how they are structured by individual identities. Without adequately controlling for selection mechanisms, environmental confounders and homophily among peers, the role of individual identities in generating heterogeneity in health outcomes would remain unclear.
Data and Measures
This study uses data from the National Longitudinal Study of Adolescent to Adult Health (Add Health), a nationally representative study of health and its social, biological, and behavioral correlates. Add Health’s longitudinal design, information on school-based peers, and focus on health in adolescence to early mid adulthood make it an ideal survey for our research question. Add Health began with a school-based survey of 90,118 students in grades 7-12, fielded in 1994-1995, from which 20,745 were randomly sampled for additional in-home and parent surveys in the same years (Wave 1). This included oversamples of some groups, such as Black students with at least one college-educated parent. Subsequent surveys followed Wave 1 into early-mid adulthood, with Waves II-V conducted in 1996, 2001, 2008, and 2016, respectively (although participants in grade 12 in Wave I were missing in Wave II only) (Harris 2013). We base our peer disadvantage measure on available income data from the Wave I survey for which school, grade and individual identifiers were available (N=14,620). However, we limit our main analysis of obesity outcomes to the longitudinal sample of individuals present in Waves I-V of the survey to examine relative differences in obesity between subgroups comprising the same individuals across waves. The initial sample size of the longitudinal dataset for which weights are available is 7,027, reduced to 5,553 with available data on income, race, and gender and controls. Then the final sample fluctuates between around 5,247 and 5,482 by wave, based on missingness in obesity data in each wave.
Our outcome of interest is individual-level obesity, which was defined in two ways in this study, depending on the age of participants in each wave. In Waves I and II, when study participants were adolescents, obesity was defined as being in the 95th BMI percentile or above compared to peers of the same gender and age, based on the recommendations of the American Academy of Pediatrics (Barlow and Dietz 1998) and calculated from CDC BMI-for-age charts (Centers for Disease Control and Prevention 2000). In Waves III-V, obesity was defined as having a BMI greater than or equal to 30 (the cut-off value used for adults). Obesity was calculated based on self-reported height and weight in Waves I, II and V, and measured height and weight in Waves III and IV. Height and weight were recorded using different measurement systems, i.e., metric or imperial, depending on survey wave. We calculated BMI as follows based on which measurement system was used in each wave:
Our predictors of interest are Wave 1 social contextual disadvantage and individual-level race, gender, and economic disadvantage, which are interacted in our model. We measure individual-level socioeconomic disadvantage as a dichotomous indicator of lower income, defined as having a household income in the lowest two quintiles of the distribution of household income in the sample, which equates to $30,000 per year or less. We do not account for family size in our household income measure due to a high degree of missingness in the measure of household size among those with available income data. For reference, the median household size in the sample is four and for a family of this size in 1995, $30,000 was approximately 200% of the federal poverty guidelines (U.S. Federal Register 1995). We use a dichotomous measure of self-reported Black or African American race, which includes individuals that identify as more than one race. We consider race to be an ascribed social status and not a biological construct, making race a proxy for differential racialized experiences and processes (Lee 2009). We use a dichotomous measure of gender, based on the Wave 1 interviewer confirmation of self-reported “male” or “female” sex in the In-School Survey. This measure captures the influences of gender as a social status as well as potential biological differences by sex in obesity (e.g. sex hormone effects on adiposity (Chang, Varghese and Singer 2018)). The social and biological components of gender cannot be distinguished in this study, meaning gendered outcomes may be attributable to both social and biological mechanisms.
We define social contextual disadvantage as concentrated peer economic disadvantage, measured as the percentage of grade-mate peers that are lower income based on the individual-level dichotomous lower-income variable. To calculate the percentage of grade-mate peers that are lower income, we sum the number of lower-income peers (excluding the individual in question) and divide by the number of students in that school-grade with income data available, minus one. Prevalence of peer disadvantage is based on the sample of peers for whom income data is present in the Wave I Parent Survey, not for the full sample of peers in school-level or administrative data samples. Additionally, of the 20,745 students captured in Wave 1 of the survey, over 5,158 were missing necessary data from the Parent Survey to calculate lower income. This suggests that our peer income measure includes two sources of error, one due to sampling design and one due to missingness.
Regarding sampling design, students from the Core Wave I Sample were stratified by grade and gender and randomly sampled, suggesting income measures, on average, should not be biased in this sample. However, we include the oversample of students to gain predictive power. To ensure the oversample of students does not bias our measure of peer mean lower income, we conduct an analysis using only the grade and sex-stratified random core sample to calculate the measure. This test and its results are described in Table S1 of the Online Supplement and suggest that inclusion of the oversample does not change our main conclusions.
Regarding missingness, we first check for bias in our income measure due to differential missingness in income data by sex and race by determining whether interacting sex and race variables predict lower income status, accounting for our control variables. The tests and results are described in Tables S2-S3 of the Online Supplement and demonstrate that differential missingness in income data by sex and racial subgroups is unlikely a concern for our conclusions. Then, in tests not presented, we assess whether missingness affects our results by conducting a “best-worse” and “worst-best” case sensitivity analysis. We impute missing lower income and obesity values with zero and one and rerun our analysis to generate bounds for scenarios in which all missing data are from lower income individuals and lead to poorer (or better) outcomes or all missing data are for higher income individuals and lead to better (or poorer) outcomes. We find that, qualitatively, our conclusions remain the same, suggesting additional imputation or sensitivity analyses are unnecessary (Jakobsen et al. 2017).
In addition to missingness in family income data, the sample used in this study is limited by attrition. Survey attrition differs by gender, race, and socioeconomic status, but attrition bias in outcomes generally has been minimal (Harris et al. 2019). Attrition could bias our results if related to our measure of peer disadvantage. In Table S4 of the Online Supplement, we check whether selective attrition is related to peer disadvantage by regressing a binary indicator of nonresponse through Wave 5 on peer disadvantage, including our controls for lower income, gender, and race, repeating, or skipping a grade, the proportion of peers that repeated or skipped a grade, grade fixed effects and school fixed effects. We find a modest, but not statistically significant relationship, suggesting attrition is unlikely to be a substantial concern. Still, we include longitudinal survey weights in the models presented in Table 3 to address any survey non-response bias (Chen and Chantala 2014). Finally, in Supplement Table S5 we show that small cell sizes generated by the clustered nature of our design do not qualitatively affect our findings.
In our main analysis, we introduce several controls to reduce endogeneity bias and isolate quasi-experimental variation in prevalence of grade-mate peers that are lower-income, such as variance in peers determined by birth date, which determines initial grade enrollment. First, we control for school fixed effects to adjust for student selection into schools based on background characteristics, such as income, ability, or neighborhood. Then, we control for individual-level characteristics that select students into grades, including whether a student repeated a grade or skipped grade, the proportion of peers that repeated a grade, and the proportion of peers that skipped a grade. We further introduce individual-level grade fixed effects to make students across different grades more comparable. Finally, we include individual-level age (in months) fixed effects, as age determines both an individual’s grade level and likelihood of obesity.
Approach
In our empirical strategy, we measure whether individual obesity across adolescent and adult life stages is affected by adolescent social contextual disadvantage differently by individual-level racial, class, and gender identities. We use a linear probability model to measure the effect of the interaction between grade-mate peer economic disadvantage and individual identities on obesity outcomes across waves. We build in individual controls and school and grade fixed effects according to the following specification:
| (1), |
where Obesityist is a binary indicator of obesity for individual i at time t who was a member of school s at the time of the Wave I survey. Xis is a vector of the individual-level adolescent lower-income, gender, and Black race identifiers. is grade-level peer disadvantage minus the individual in question, in each school. We also include wave, Ww. Our primary interest in this study is a term interacting individual-level lower-income, gender and race identifiers with grade-level peer disadvantage and wave, , making this a five-way interaction. We also include all other two-way, three-way, and four-way interactions among these variables. Cis is a vector of individual-level control variables, including age fixed effects, grade fixed effects, whether a participant skipped a grade, and whether a participant repeated a grade. In our preferred models, we introduce school fixed effects, Ss, to control for fixed characteristics of the school environment as well as to control for student selection into schools, based on such things as neighborhood and parental education. Errors terms are clustered at the school-level.
Descriptive Statistics
Table 1 presents unweighted summary statistics by race, gender, and income subgroup, including sample sizes, mean, standard deviation, and value ranges, for obesity across all waves, as well as additional Wave I measures. Higher income individuals have lower percentages of peers that are lower income, as do non-Black individuals. However, the variation in peer mean lower income by subgroup suggests overlap in subgroup exposure to levels of peer mean lower income. In Wave I, obesity prevalence ranges from 5.5% to 14.1% by subgroup, increasing steadily to between 32.7% and 60.3% by Wave V, when participants are ages 33 to 42 years old. Additional summary statistics for the full sample are in Supplement Table S6.
Table 1.
Summary Statistics
| Non-Black | Black | |||||||
|---|---|---|---|---|---|---|---|---|
| Females | Males | Females | Males | |||||
| Higher- Income |
Lower- Income |
Higher- Income |
Lower- Income |
Higher- Income |
Lower- Income |
Higher- Income |
Lower- Income |
|
| Mean Income | 67.950 | 18.331 | 65.929 | 18.148 | 60.556 | 15.675 | 59.982 | 15.681 |
| SD Income | 62.893 | 8.242 | 60.926 | 8.516 | 46.739 | 8.449 | 51.148 | 8.360 |
| Mean Peer Lower Income | 0.323 | 0.479 | 0.322 | 0.475 | 0.439 | 0.561 | 0.464 | 0.561 |
| SD Mean Peer Lower Income | 0.192 | 0.208 | 0.187 | 0.207 | 0.194 | 0.199 | 0.200 | 0.198 |
| N (Predictors) | 3566 | 2078 | 3764 | 2098 | 703 | 964 | 665 | 855 |
| Mean Obesity W1 | 0.055 | 0.087 | 0.122 | 0.141 | 0.131 | 0.137 | 0.123 | 0.128 |
| Mean Obesity W2 | 0.087 | 0.139 | 0.147 | 0.176 | 0.159 | 0.178 | 0.151 | 0.159 |
| Mean Obesity W3 | 0.178 | 0.257 | 0.194 | 0.223 | 0.272 | 0.323 | 0.204 | 0.226 |
| Mean Obesity W4 | 0.289 | 0.402 | 0.334 | 0.401 | 0.465 | 0.520 | 0.359 | 0.341 |
| Mean Obesity W5 | 0.327 | 0.454 | 0.352 | 0.457 | 0.553 | 0.603 | 0.398 | 0.420 |
| N (Obese W1) | 3460 | 1999 | 3734 | 2064 | 687 | 901 | 659 | 834 |
| N (Obese W2) | 2607 | 1536 | 2708 | 1531 | 527 | 653 | 469 | 605 |
| N (Obese W3) | 2725 | 1458 | 2620 | 1412 | 508 | 681 | 441 | 540 |
| N (Obese W4) | 2899 | 1645 | 2840 | 1502 | 578 | 760 | 476 | 574 |
| N (Obese W5) | 2584 | 1333 | 2264 | 1061 | 445 | 610 | 322 | 333 |
Notes: Initial summary statistics for Wave 1 predictors by race, gender, and adolescent family income status, as well as obesity statistics for Waves 1 – 5.
Source: Authors’ calculations from Add Health Data Waves 1 – 5.
Balancing Tests
An important concern in the literature on social contextual effects, e.g., in studies involving neighborhood and peer effects, is that the reference group is non-randomly determined. We address this issue through our use of quasi-random variation in grade-mate peer disadvantage. Interpreting this variation as quasi-random requires us to assume that the prevalence of grade-mate peer disadvantage is uncorrelated with individual background characteristics, such as income, race, and gender, after adjusting for fixed effects and controls. This assumption can be tested with several balancing tests.
The logic behind these tests is that if the variation in peer disadvantage is quasi-randomly distributed after the introduction of our controls, it should be unrelated to individual characteristics that are determined prior to exposure to grade-mate peers. In other words, if peer disadvantage does not predict pre-determined individual-level observables, this gives us some confidence that it also does not predict individual-level unobservables that could otherwise bias our results (Altonji, Elder and Taber 2005).
In these tests, we regress peer disadvantage on various student background characteristics, including our controls, and present results in Table S7 of the Supplement. These background characteristics include whether a student is white, Asian, Native American, or other race, Hispanic ethnicity, was born in the U.S., is living in the same residence in which they lived in 1990, whether English is spoken at home, the highest education of parents, and whether parents were married, happy, religious or a member of a parent-teacher organization. All outcomes except Hispanic ethnicity pass the test. While the modest and statistically significant coefficient could reflect Type 1 error, it is possible that Hispanic ethnicity is intertwined with our other predictor variables. Thus, we control for Hispanic ethnicity in Model 2 of our balancing tests and find that variation in peer disadvantage is unrelated to individual-level observables, supporting our assumption of quasi-random variation.
As a further test that our variation is quasi-experimental, we add the pre-determined characteristics from Model 2 of our balancing tests to Model 4 of our main results. Building on the idea that if our predictor variable, peer mean lower income, is quasi-randomly determined, it should be unrelated to these controls and adding these terms to the model should not alter our coefficients of interest.
Results
Table 2 presents results of differently specified models, each examining the effect of peer disadvantage on life course obesity by intersecting individual identities based on race, gender, and lower-income status, as outlined in Equation 1. These results are for the longitudinal sample of individuals present in each wave. The results shown are marginal effect sizes within each subgroup defined by the three-way interaction term calculated using marginal standardization in Stata 16.1. Model 1 includes grade fixed effects and all other controls, except school fixed effects. The results of Model 1 demonstrate large, positive, and statistically significant relationships between grade-mate peer disadvantage and obesity across the early-to-mid-adult life course for non-Black women and men, Black women, and Black higher-income men. In contrast, the results also show a negative, increasingly large, and statistically significant relationship between grade-mate peer disadvantage and obesity across the life course for Black, lower-income men. However, Model 1 still includes between-school variation, i.e., school selection mechanisms, in addition to the quasi-experimental variation in grade-mate peer disadvantage.
Table 2.
Results for the Longitudinal Sample across Waves 1-5
| VARIABLES | (1) Model 1 |
(2) Model 2 |
(3) Model 3 |
(4) Model 4 |
|---|---|---|---|---|
| Female, Non-Black, Higher-income | ||||
| Wave 1 | 0.025 (0.041) | −0.124 (0.079) | −0.128 (0.079) | −0.141 (0.093) |
| Wave 2 | 0.083 (0.059) | −0.068 (0.086) | −0.070 (0.086) | −0.074 (0.094) |
| Wave 3 | 0.230*** (0.086) | 0.089 (0.099) | 0.090 (0.100) | 0.087 (0.133) |
| Wave 4 | 0.367*** (0.086) | 0.220** (0.105) | 0.222** (0.105) | 0.216* (0.118) |
| Wave 5 | 0.318*** (0.086) | 0.172 (0.108) | 0.173 (0.109) | 0.211 * (0.126) |
| Female, Non-Black, Lower-income | ||||
| Wave 1 | 0.101 (0.065) | −0.019 (0.105) | −0.016 (0.106) | −0.014 (0.133) |
| Wave 2 | 0.076 (0.088) | −0.040 (0.125) | −0.037 (0.125) | −0.004 (0.152) |
| Wave 3 | 0.269** (0.116) | 0.156 (0.123) | 0.156 (0.123) | 0.181 (0.141) |
| Wave 4 | 0.272** (0.116) | 0.155 (0.122) | 0.157 (0.123) | 0.182 (0.139) |
| Wave 5 | 0.227* (0.120) | 0.110 (0.137) | 0.113 (0.138) | 0.166 (0.158) |
| Female, Black, Higher-income | ||||
| Wave 1 | −0.006 (0.150) | −0.060 (0.160) | −0.055 (0.160) | 0.146 (0.183) |
| Wave 2 | 0.164 (0.147) | 0.109 (0.159) | 0.113 (0.159) | 0.165 (0.188) |
| Wave 3 | 0.367* (0.203) | 0.321 (0.233) | 0.326 (0.233) | 0.313 (0.255) |
| Wave 4 | 0.461** (0.190) | 0.411* (0.230) | 0.404* (0.230) | 0.533** (0.233) |
| Wave 5 | 0.384** (0.190) | 0.337 (0.209) | 0.329 (0.209) | 0.362 (0.237) |
| Female, Black, Lower-income | ||||
| Wave 1 | 0.223 (0.208) | 0.128 (0.200) | 0.137 (0.201) | −0.048 (0.210) |
| Wave 2 | 0.472** (0.211) | 0.381* (0.202) | 0.390* (0.203) | 0.217 (0.228) |
| Wave 3 | 0.560*** (0.197) | 0.446** (0.192) | 0.455** (0.192) | 0.486*** (0.176) |
| Wave 4 | 0.459** (0.198) | 0.367 (0.249) | 0.377 (0.249) | 0.300 (0.297) |
| Wave 5 | 0.540*** (0.190) | 0.448* (0.247) | 0.458* (0.246) | 0.390 (0.299) |
| Male, Non-Black, Higher-income | ||||
| Wave 1 | 0.135* (0.073) | −0.039 (0.095) | −0.034 (0.095) | −0.052 (0.112) |
| Wave 2 | 0.136* (0.079) | −0.036 (0.098) | −0.031 (0.097) | −0.037 (0.108) |
| Wave 3 | 0.240*** (0.088) | 0.063 (0.114) | 0.069 (0.114) | 0.073 (0.132) |
| Wave 4 | 0.183* (0.100) | 0.009 (0.118) | 0.017 (0.118) | 0.043 (0.143) |
| Wave 5 | 0.086 (0.101) | −0.085 (0.118) | −0.088 (0.118) | −0.061 (0.143) |
| Male, Non-Black, Lower-income | ||||
| Wave 1 | 0.200** (0.099) | 0.070 (0.113) | 0.070 (0.114) | 0.061 (0.130) |
| Wave 2 | 0.125 (0.098) | −0.002 (0.120) | 0.012 (0.120) | −0.036 (0.142) |
| Wave 3 | 0.079 (0.109) | −0.042 (0.121) | −0.029 (0.122) | −0.097 (0.146) |
| Wave 4 | 0.142 (0.133) | 0.017 (0.164) | 0.028 (0.164) | −0.025 (0.182) |
| Wave 5 | 0.059 (0.132) | −0.070 (0.186) | −0.060 (0.187) | −0.065 (0.198) |
| Male, Black, Higher-income | ||||
| Wave 1 | 0.201 (0.165) | 0.253 (0.195) | 0.253 (0.195) | 0.165 (0.206) |
| Wave 2 | 0.239 (0.191) | 0.284 (0.197) | 0.283 (0.197) | 0.166 (0.244) |
| Wave 3 | 0.136 (0.206) | 0.169 (0.246) | 0.169 (0.245) | −0.013 (0.251) |
| Wave 4 | 0.064 (0.272) | 0.110 (0.288) | 0.111 (0.289) | −0.094 (0.366) |
| Wave 5 | 0.087 (0.265) | 0.132 (0.337) | 0.132 (0.339) | 0.077 (0.367) |
| Male, Black, Lower-income | ||||
| Wave 1 | 0.071 (0.125) | −0.02 (0.141) | −0.011 (0.141) | −0.104 (0.147) |
| Wave 2 | −0.064 (0.151) | −0.156 (0.149) | −0.146 (0.149) | −0.282 (0.184) |
| Wave 3 | −0.170 (0.213) | −0.262 (0.210) | −0.252 (0.211) | −0.404* (0.211) |
| Wave 4 | −0.317 (0.230) | −0.403* (0.237) | −0.393 (0.238) | −0.555*** (0.210) |
| Wave 5 | −0.625*** (0.239) | −0.722*** (0.237) | −0.711*** (0.236) | −0.920*** (0.210) |
| Observations | 26,994 | 26,994 | 26,912 | 20,671 |
| Controls | Yes | Yes | Yes | Yes |
| School Fixed Effects | No | Yes | Yes | Yes |
Standard errors in parentheses.
p<0.01
p<0.05
p<0.1
Notes: All models report marginal effects based on regression results of Equation 1, the effect of the prevalence of peer economic disadvantage interacted with gender, race, and individual lower income status on obesity across 5 waves. Each specification includes controls for age fixed effects, grade fixed effects, repeated grade, skipped grade, peer mean repeated grade, and peer mean skipped grade. Model 2 includes school fixed effects. Model 3 includes school fixed effects and controls for Hispanic ethnicity. Model 4 includes school fixed effects and controls for all variables examined in Table 2. All models use the longitudinal sample with data across Waves I-V for which longitudinal grand survey weights were available and include these weights (gsw12345). Observations are the total observations in each wave. Cluster robust standard errors are reported for Models 2-4.
Source: Authors’ calculations from Add Health Data Waves 1 – 5.
In Model 2 (Table 2), our preferred specification, we introduce school fixed effects, and results are notably altered for some groups. This suggests that mechanisms that select students into schools and other fixed aspects of school environment likely confound peer social contextual effect estimates. Specifically, marginal effect estimates are attenuated for non-Black women and lose statistical significance in most waves and move toward the null and lose all statistical significance for non-Black men. Among Black women, effect sizes are slightly attenuated but remain large and, in the lower-income group, significant in several waves. For example, among lower-income Black women, predicted obesity is 45 percentage points higher by Wave 5 when peer disadvantage is one (100%) relative to zero. Marginal peer effects for higher-income Black men appear to widen over subsequent waves but remain statistically insignificant. Finally, among low-income Black men, the effect of peer disadvantage becomes slightly more negative and gains statistical significance at Wave 4. For this group, predicted obesity by Wave 5 is 72 percentage points lower when peer disadvantage is one, relative to zero. Among low-income Black men, the relationship between peer disadvantage and obesity grows across waves, whereas for Black women, the relationship appears by Wave 3 and remains steady as obesity levels increase in Waves 4 and 5.
To test the robustness of our results to the assumption of quasi-experimental variation, we control for Hispanic ethnicity in Model 3, and further control for student background characteristics in Model 4 of our main results in Table 3. There is little change to the strength of the effect sizes or to patterns of statistical significance, suggesting we are capturing quasi-experimental variation and that selection related to these added factors is not a significant problem. Only among low-income Black males is there a strengthening of the coefficients and statistical significance. This could be a function of diminishing sample size due to the inclusion of more controls. If instead these variables control for additional selection mechanisms, this would suggest that the results of our preferred model may underestimate the true effect size.
Figures 1a and 1b present the results of Model 2 graphically as the predicted probability of obesity across changing levels of peer disadvantage. Each line represents a survey wave, with the ages of respondents at each wave in parentheses. Level changes in the lines suggest changes in obesity over time not attributable to peer contextual disadvantage. Slope changes in lines suggest a strengthening or weakening of the relationship between grade-mate peer economic disadvantage and obesity over time. Apparent is a strong positive relationship (slope) between peer disadvantage and obesity outcomes among Black females that establishes itself in earlier waves and remains steady across waves. This is in striking contrast to the pattern among lower-income Black males, where the negative relationship (slope) between peer disadvantage and obesity grows in magnitude across waves. There is also suggestive evidence of a positive relationship between peer disadvantage and obesity in early waves among higher-income Black men that dissipates over time, whereas the reverse is observed among non-Black women. There is no apparent relationship between peer disadvantage and obesity in non-Black males.
Figure 1a. Predicted Probability of Obesity across Levels of Peer Disadvantage, Females.
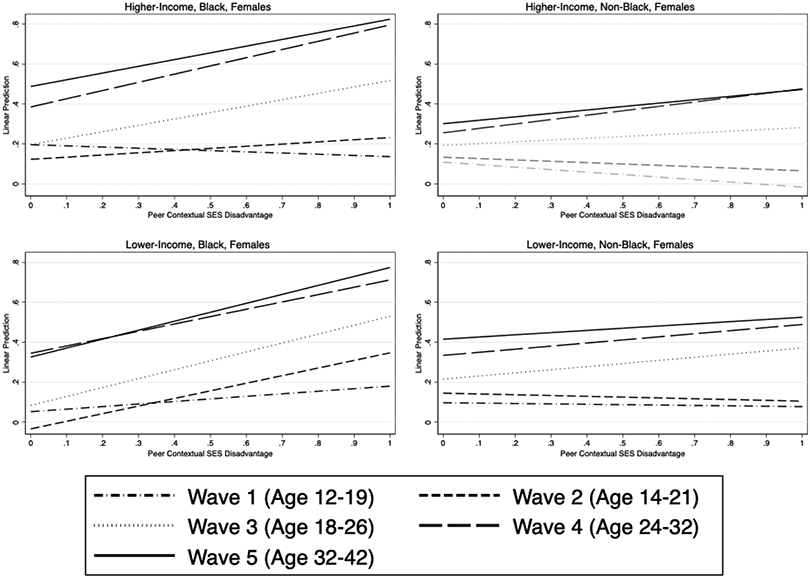
Notes: Figure 1a reflects the predicted probability of obesity based on Model 3 in Table 3, which report marginal effects from the regression of obesity across waves on peer disadvantage interacted with gender, race, and individual lower income status. The figure reflects longitudinal sample with data across Waves I-V for which longitudinal grand survey weights were available and include these weights (gsw12345). The approximate age range of individuals within each wave is reflected in parentheses. Source: Authors’ calculations from Add Health Data Waves 1 – 5.
Figure 1b. Predicted Probability of Obesity across Levels of Peer Disadvantage, Males.
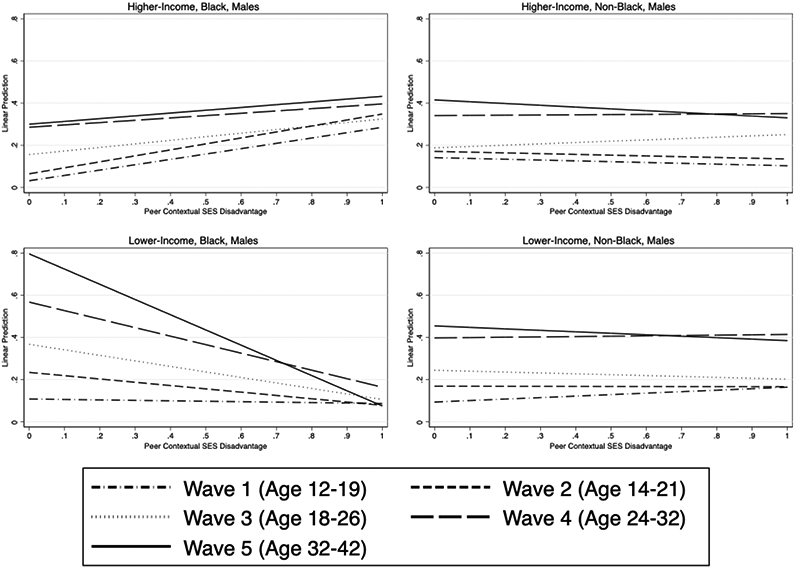
Notes as for Figure 1a.
Specification Tests and Robustness Checks
We also test how our results change with alternative specifications of peer socioeconomic disadvantage or with the addition of further controls, and if our results are robust in cross-sectional samples. First, we examine whether our results change based on our definition of lower income. In Table S8 of the Online Supplement, we test an alternative definition of lower income, defined as being in the first quintile of the income distribution in the sample. Under this definition, our effect sizes change somewhat, but remain qualitatively similar, except for higher-income, Black males for whom the relationship between peer low income and obesity directionally changes. This makes sense given that some lower-income Black men, who had very strong negative coefficients in the original results, are recategorized as higher income in these analyses. This also gives a sense of how severity in disadvantage can alter results. In Table S9, we control for peer mean parental education and average percent peers that are Black. Results of these analyses do not qualitatively change our conclusions.
In Table S10 of the Online Supplement, we also present results of Model 3 using cross-sectional rather than longitudinal data. The cross-sectional data examines the relationship between peer disadvantage and obesity for individuals present by wave. Individuals move in and out of the sample across waves, so although a cross-sectional analysis might increase our sample size in any given wave, the individuals in the cross-section change over time, making any changes in the relationship between peer disadvantage and obesity less clear. Results are qualitatively similar.
Discussion
This paper introduces and tests an intersectional approach to social contextual effects models to illuminate the complex dynamics that shape obesity trajectories across the life course. It also extends work on social contextual disadvantage and obesity by introducing a quasi-experimental design. Our findings uncover interesting heterogeneity in the effects of social context on obesity by race, gender, and income. Most notably, high concentrations of peer socioeconomic disadvantage predict dramatically diverging patterns of obesity for lower income Black men as compared to Black women. However, peer contextual economic disadvantage has a less extreme positive influence on obesity in white women and no influence on obesity in white men. These results demonstrate that the structuring of social relationships by intersecting identities may contribute to patterns of health inequity. They also underscore work demonstrating that adolescence is a sensitive period in the development of life course health, as peer contextual disadvantage has a lasting, and sometimes accumulating relationship with obesity across waves. Our results contribute novel findings to literatures on intersecting identities and health, social contextual effects and health, and adolescence as a sensitive period in the development of life course health. Moreover, our results suggest that using an intersectional approach in the analysis of relationships among social contexts, social interactive mechanisms and health is a promising avenue for future work.
First, our findings put in perspective how the relationship between identity and health may change depending on meso-level social contexts. Our results are partly in line with prior work that demonstrates that Black women have the highest BMIs in adolescence and steepest BMI trajectories across adulthood (Hargrove 2018), while we further demonstrate that heterogeneity in this group by peer socioeconomic context may help to explain this pattern. Moreover, we find meso-level social contextual disadvantage, in this case grade-mate peer economic disadvantage, interacts with individual race, gender, and class identities to structure health outcomes.
Our analyses contrast with previous work that finds higher levels of obesity among both male and female students with greater school or neighborhood disadvantage (Lee, Harris and Lee 2013). We find that peer social contextual disadvantage predicts obesity heterogeneously in magnitude and direction by economic status, race, and gender. This heterogeneity implies that social contextual disadvantage, measured as school peer economic disadvantage, affects individual obesity through different pathways based on intersecting race, class, and gender identities. This has implications for potential policy prescriptions, as our results suggest that blanket policies aimed at reducing school-level contextual disadvantage through, for instance, school-level economic desegregation, may not benefit all disadvantaged groups. An important next question to ask is how intersecting identities organize social interactions in peer contexts.
The intersectionality in social contexts framework can be further applied to answer this question. For instance, intersecting identities, rooted in larger systems of oppression, may carry shared experiences, meanings, or learned roles that structure interactions in context dependent ways. For example, if Black women take on additional responsibility for community well-being, as some scholars suggest (Lekan 2009), then it may be that in contexts with high peer disadvantage, Black girls experience additional social stress than they do in contexts with low peer disadvantage. Exploring subgroup heterogeneity in social interactive mechanisms operating in contexts demands that scholars recognize the larger systems of marginalization to which identities are linked in formulating hypotheses around how identities and social contexts impact health outcomes. In so doing, scholarship can move toward better accounting for, rather than controlling for, structural inequalities in the relationship between social contexts and health.
This study is not without limitations. First, while we estimate a total effect of peer disadvantage on individual obesity outcomes, we do not measure the mechanisms linking these two variables, which remain an area for future research. Second, while our falsification tests suggest we have controlled for important factors that confound the relationship between peer disadvantage and individual characteristics, we cannot fully rule out that some confounders continue to influence our results. Also, given that this is a quasi-experimental design at the school-peer contextual level, our results may not be generalizable outside of this context.
Another limitation is that we measure peer disadvantage as exposure to a sample of grade-mate peers. In so doing, we ignore underlying heterogeneity in peer influence, where friends may have a greater impact on obesity than other grade-mate peers, for instance. This suggests our results may underestimate the effects of peers on obesity outcomes. While measuring the influence of friends could offer more precision in our estimates, individuals select into friendships, meaning this approach could yield biased effect sizes, whereas our approach controls for this type of bias. In addition, since we are unable to measure income for all grade-mate peers, we must assume that variation in our sample represents the variation in the full peer group or we risk biased estimates. The tests of our assumptions suggest that income missingness and the student oversample are unlikely to bias our results. Finally, we recognize that obesity is an imperfect indicator of health risk and that the differences in obesity outcomes we find in this study may not be generalizable to other health risks.
Conclusion
In closing, the patterns we uncover partly uphold aspects of existing health disparities research, but also reveal additional heterogeneity in the influence of peer social contextual economic disadvantage on obesity by identity subgroup. The finding that peer economic disadvantage leads to heterogenous obesity patterns highlights the importance of using intersectional and quasi-experimental approaches jointly in research on social relationships and health. Moving forward, applying an intersectional framework to understanding how additional forms of contextual disadvantage influence health is warranted, as are investigations of the social interactive mechanisms linking contexts to health. Such work may generate new hypotheses for understanding existing health disparities.
Supplementary Material
Social contexts are comprised of social relationships and matter for health.
Intersecting identities (race/SES/gender) structure relationships in contexts.
The relationship between social context and health differs by individual identities.
The study quasi-experimentally measures adolescent peer economic contexts.
Peer disadvantage impacts life course obesity differently by individual identities.
Acknowledgements
Research reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health under Award Number R21HD101757. Stephanie Koning additionally received support from NIH Award Number F32 HD102152.The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Add Health is directed by Robert A. Hummer and funded by the National Institute on Aging cooperative agreements U01 AG071448 (Hummer) and U01AG071450 (Aiello and Hummer) at the University of North Carolina at Chapel Hill. Waves I-V data are from the Add Health Program Project, grant P01 HD31921 (Harris) from Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), with cooperative funding from 23 other federal agencies and foundations. Add Health was designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill. The authors thank Kathleen Cagney and Jason Fletcher for their helpful comments on this manuscript.
Footnotes
Polos conceptualized the study, developed the methodology, implemented statistical analysis, and drafted and edited the manuscript. McDade secured funding, facilitated access to the data and reviewed and edited the manuscript. Koning reviewed and edited the manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Altonji Joseph G, Elder Todd E, and Taber Christopher R. 2005. "Selection on Observed and Unobserved Variables: Assessing the Effectiveness of Catholic Schools." Journal of Political Economy 113(1):151–84. [Google Scholar]
- Alvarado Steven Elías. 2016. "Neighborhood disadvantage and obesity across childhood and adolescence: Evidence from the NLSY children and young adults cohort (1986–2010)." Social Science Research 57:80–98. [DOI] [PubMed] [Google Scholar]
- —. 2019. "The indelible weight of place: Childhood neighborhood disadvantage, timing of exposure, and obesity across adulthood." Health & Place 58:102159. [DOI] [PubMed] [Google Scholar]
- Andersen Margaret L, and Collins Patricia Hill. 2007. "Systems of Power and Inequality." Pp. 61–90 in Race, Class, & Gender: An Anthology, edited by Andersen Margaret L and Collins Patricia Hill: Thomson Wadsworth [Google Scholar]
- Arcaya Mariana C., Tucker-Seeley Reginald D., Kim Rockli, Schnake-Mahl Alina, So Marvin, and Subramanian SV. 2016. "Research on neighborhood effects on health in the United States: A systematic review of study characteristics." Social Science & Medicine 168:16–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow Sarah E., and Dietz William H.. 1998. "Obesity Evaluation and Treatment: Expert Committee Recommendations." Pediatrics 102(3):e29. [DOI] [PubMed] [Google Scholar]
- Berger Joseph, Cohen Bernard P., and Zelditch Morris. 1972. "Status Characteristics and Social Interaction." American Sociological Review 37(3):241–55. [Google Scholar]
- Blalock Hubert M. 1984. "Contextual-effects models: theoretical and methodological issues." Annual Review of Sociology 10(1):353–72. [Google Scholar]
- Carroll Margaret D., Flegal Katherine M., Lamb Molly M., and Ogden Cynthia L.. 2010. "Obesity and socioeconomic status in adults; United States, 2005-2008." [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. 2000. "BMI-for-age charts, 2 to 20 years, LMS parameters and selected smoothed BMI (kilograms/meters squared) percentiles, by sex and age." in Percentile Data Files with LMS Values, edited by National Center for Health Statistics. [Google Scholar]
- Chang Eric, Varghese Mita, and Singer Kanakadurga. 2018. "Gender and Sex Differences in Adipose Tissue." Current diabetes reports 18(9):69–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang Virginia W., and Christakis Nicholas A.. 2005. "Income inequality and weight status in US metropolitan areas." Social Science & Medicine 61(1):83–96. [DOI] [PubMed] [Google Scholar]
- Chen Ping, and Chantala Kim. 2014. "Guidelines for Analyzing Add Health Data." edited by Carolina Population Center. University of North Carolina at Chapel Hill. [Google Scholar]
- Cohen-Cole Ethan, and Fletcher Jason M.. 2008. "Is obesity contagious? Social networks vs. environmental factors in the obesity epidemic." Journal of Health Economics 27(5):1382–87. [DOI] [PubMed] [Google Scholar]
- Cozier Yvette C., Yu Jeffrey, Coogan Patricia F., Bethea Traci N., Rosenberg Lynn, and Palmer Julie R.. 2014. "Racism, Segregation, and Risk of Obesity in the Black Women's Health Study." American Journal of Epidemiology 179(7):875–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crenshaw Kimberle. 1989. "Demarginalizing the Intersection of Race and Sex: A Black Feminist Critique of Antidiscrimination Doctrine, Feminist Theory and Antiracist Politics." Pp. 8 in University of Chicago Legal Forum. [Google Scholar]
- Elwert Felix, and Winship Christopher. 2014. "Endogenous Selection Bias: The Problem of Conditioning on a Collider Variable." Annual Review of Sociology 40(1):31–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erbring Lutz, and Young Alice A.. 1979. "Individuals and Social Structure: Contextual Effects as Endogenous Feedback." Sociological Methods & Research 7(4):396–430. [Google Scholar]
- Ferraro Kenneth F., and Kelley-Moore Jessica A.. 2003. "Cumulative Disadvantage and Health: Long-Term Consequences of Obesity?" American Sociological Review 68(5):707–29. [PMC free article] [PubMed] [Google Scholar]
- Flegal Katherine M., Kit Brian K., Orpana Heather, and Graubard Barry I.. 2013. "Association of All-Cause Mortality With Overweight and Obesity Using Standard Body Mass Index Categories: A Systematic Review and Meta-analysis." JAMA 309(1):71–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fletcher Jason, Jinho Kim, Jenna Nobles, Ross Stephen, and Shaorshadze Irina. 2019. "The Effects of Foreign-Born Peers in US High Schools and Middle Schools." National Bureau of Economic Research. [Google Scholar]
- Fletcher Jason M. 2012. "Peer influences on adolescent alcohol consumption: evidence using an instrumental variables/fixed effect approach." Journal of Population Economics 25(4):1265–86. [Google Scholar]
- Fletcher Jason M., and McLaughlin Stephen M.. 2015. "Neighborhood Factors During Adolescence: Modest Effects On Cardiovascular Risk, Small Impact On Obesity And Depression." Health Affairs 34(9):1472–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frech Adrianne. 2012. "Healthy behavior trajectories between adolescence and young adulthood." Advances in Life Course Research 17(2):59–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fryar Cheryl D, Carroll Margaret D, and Ogden Cynthia L. 2018. "Prevalence of overweight, obesity, and severe obesity among children and adolescents aged 2–19 years: United States, 1963–1965 through 2015–2016." [Google Scholar]
- Gaviria Alejandro, and Raphael Steven. 2001. "School-Based Peer Effects and Juvenile Behavior." The Review of Economics and Statistics 83(2):257–68. [Google Scholar]
- Goosby Bridget J., and Walsemann Katrina M.. 2012. "School racial composition and race/ethnic differences in early adulthood health." Health & Place 18(2):296–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hales Craig M., Carroll Margaret D., Fryar Cheryl D., and Ogden Cynthia L.. 2020. "Prevalence of obesity and severe obesity among adults : United States, 2017–2018." [PubMed] [Google Scholar]
- Hargrove Taylor W. 2018. "Intersecting Social Inequalities and Body Mass Index Trajectories from Adolescence to Early Adulthood." Journal of Health and Social Behavior 59(1):56–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris Kathleen Mullan. 2013. "The add health study: Design and accomplishments." Chapel Hill: Carolina Population Center, University of North Carolina at Chapel Hill:1–22. [Google Scholar]
- Harris Kathleen Mullan, Halpern Carolyn Tucker, Whitsel Eric A., Hussey Jon M., Killeya-Jones Ley A., Tabor Joyce, and Dean Sarah C.. 2019. "Cohort Profile: The National Longitudinal Study of Adolescent to Adult Health (Add Health)." International Journal of Epidemiology 48(5):1415–15k. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hulko Wendy. 2009. "The time-and context-contingent nature of intersectionality and interlocking oppressions." Affilia 24(1):44–55. [Google Scholar]
- Jakobsen Janus Christian, Gluud Christian, Wetterslev Jørn, and Winkel Per. 2017. "When and how should multiple imputation be used for handling missing data in randomised clinical trials - a practical guide with flowcharts." BMC medical research methodology 17(1):162–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kershaw KN, Albrecht SS, and Carnethon MR. 2013a. "Racial and ethnic residential segregation, the neighborhood socioeconomic environment, and obesity among Blacks and Mexican Americans." Am J Epidemiol 177(4):299–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kershaw Kiarri N., Albrecht Sandra S., and Carnethon Mercedes R.. 2013b. "Racial and Ethnic Residential Segregation, the Neighborhood Socioeconomic Environment, and Obesity Among Blacks and Mexican Americans." American Journal of Epidemiology 177(4):299–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kivimäki Mika, Vahtera Jussi, Tabák Adam G., Halonen Jaana I., Vineis Paolo, Jaana Pentti Katja Pahkala, Rovio Suvi, Viikari Jorma, Kähönen Mika, Juonala Markus, Feme Jane E., Stringhini Silvia, and Raitakari Olli T.. 2018. "Neighbourhood socioeconomic disadvantage, risk factors, and diabetes from childhood to middle age in the Young Finns Study: a cohort study." The Lancet Public Health 3(8):e365–e73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Catherine. 2009. " “Race” and “ethnicity” in biomedical research: How do scientists construct and explain differences in health?" Social Science & Medicine 68(6):1183–90. [DOI] [PubMed] [Google Scholar]
- Lee Hedwig, Harris Kathleen M., and Lee Joyce. 2013. "Multiple Levels of Social Disadvantage and Links to Obesity in Adolescence and Young Adulthood." Journal of School Health 83(3):139–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lekan Deborah. 2009. "Sojourner Syndrome and Health Disparities in African American Women." Advances in Nursing Science 32(4). [DOI] [PubMed] [Google Scholar]
- Liu Hui, and Umberson Debra. 2015. "Gender, stress in childhood and adulthood, and trajectories of change in body mass." Social science & medicine (1982) 139:61–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehra Renee, Boyd Lisa M., and Ickovics Jeannette R.. 2017. "Racial residential segregation and adverse birth outcomes: A systematic review and meta-analysis." Social Science & Medicine 191:237–50. [DOI] [PubMed] [Google Scholar]
- Mollborn Stefanie, and Lawrence Elizabeth. 2018. "Family, Peer, and School Influences on Children’s Developing Health Lifestyles." Journal of Health and Social Behavior 59(1):133–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oakes J. Michael, Andrade Kate E., Biyoow Ifrah M., and Cowan Logan T.. 2015. "Twenty Years of Neighborhood Effect Research: An Assessment." Current Epidemiology Reports 2(1):80–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paeratakul S, Lovejoy JC, Ryan DH, and Bray GA. 2002. "The relation of gender, race and socioeconomic status to obesity and obesity comorbidities in a sample of US adults." International Journal of Obesity 26(9):1205–10. [DOI] [PubMed] [Google Scholar]
- Pervanidou Panagiota, and Chrousos George P.. 2012. "Metabolic consequences of stress during childhood and adolescence." Metabolism 61(5):611–19. [DOI] [PubMed] [Google Scholar]
- Sheehan Connor M., Cantu Phillip A., Powers Daniel A., Margerison-Zilko Claire E., and Cubbin Catherine. 2017. "Long-term neighborhood poverty trajectories and obesity in a sample of california mothers." Health & Place 46:49–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Federal Register. 1995. Pp. 7697–884. Washington, D.C. [Google Scholar]
- Umberson Debra, Crosnoe Robert, and Reczek Corinne. 2010. "Social Relationships and Health Behavior Across the Life Course." Annual Review of Sociology 36(1):139–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Tse-Chuan, and South Scott J.. 2018. "Neighborhood effects on body mass: Temporal and spatial dimensions." Social Science & Medicine 217:45–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahnd Whitney E., and McLafferty Sara L.. 2017. "Contextual effects and cancer outcomes in the United States: a systematic review of characteristics in multilevel analyses." Annals of Epidemiology 27(11):739–48.e3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


