Abstract
Background:
Trauma patients may present with non-survivable injuries, which could be resuscitated for future organ transplantation. Trauma surgeons face an ethical dilemma of deciding whether, when, and how to resuscitate a patient who will not directly benefit from it. As there are no established guidelines to follow, we aim to describe resuscitation practices for organ transplantation; we hypothesize that resuscitation practices vary regionally.
Study Design:
Over a 3-month period, we surveyed trauma surgeons practicing in Level I and II trauma centers within a single state using an instrument to measure resuscitation attitudes and practices for organ preservation. Descriptive statistics were calculated for practice patterns.
Results:
Survey response rate was 51% (31/60). Many (81%) had experience with resuscitations where the primary goal was to preserve potential for organ transplantation. Many (90%) said they encountered this dilemma at least monthly. All respondents were willing to intubate; most were willing to start vasopressors (94%) and to transfuse blood (84%) (range 1 unit to >10 units). Of respondents, 29% would resuscitate for ≥24 hours, and 6% would perform a resuscitative thoracotomy. Respect for patients’ dying process and future organ quality were the factors most frequently considered very important or important when deciding to stop or forgo resuscitation, followed closely by concerns about excessive resource utilization.
Conclusion:
Trauma surgeons’ regional resuscitation practices vary widely for this patient population. This variation implies a lack of professional consensus regarding initiation and extent of resuscitations in this setting. These data suggest this is a common clinical challenge, which would benefit from further study to determine national variability, areas of equipoise, and features amenable to practice guidelines.
Keywords: trauma surgery, trauma resuscitation, transplantation, organ preservation, organ donation, ethics
There is wide variation in trauma surgeons’ regional practice patterns when resuscitating patients with non-survivable injuries to preserve organs for future transplantation, implying a lack of professional consensus in this setting.
We conducted a statewide survey of trauma surgeons currently practicing in a level 1 or 2 trauma center regarding their resuscitation practices for patients with lethal injuries, who cannot directly benefit from resuscitation, but who are potential organ donors.
Introduction:
Trauma patients that present to the hospital with non-survivable injuries have the potential to progress to organ donation. These patients pose a unique resuscitative challenge for trauma surgeons. Resuscitation has no direct benefit to the dying trauma patient but may benefit many patients awaiting transplantation. There is no professional consensus on when, how, or even whether to resuscitate trauma patients in these circumstances. Organ donation as after trauma resuscitation has been proposed as an important secondary outcome and costs associated with resuscitations have also been shown to be mitigated by organ donation [[add 26881486 & 22000116]].Trauma surgeons’ practice patterns are not well understood or described in these ethical scenarios pitting patient non-maleficence against societal beneficence.
There is no published literature to describe trauma surgeons’ resuscitative practice patterns or the factors influencing the decision in cases of non-survivable injuries with the potential for organ donation, although one study1 evaluated organ donation as a retrospective outcome measure after Emergency Department (ED) thoracotomy. The American College of Surgeons (ACS) Committee on Trauma requires integration of trauma centers with organ donation by creating an established relationship with the local Organ Procurement Organization (OPO), implementing mechanisms to identify and monitor organ donation rates, and mandating a trauma surgeon representative on institutional donor councils. However, the scope of these requirements are limited to the level of the institution, have not been shown to have a measurable effect on solid organ donor outcomes, and do not provide clinical recommendations.2
To better understand the approach to resuscitation in the lethally injured patient with potential for organ donation, we surveyed the regional practice patterns of trauma surgeons. Our specific aims were to determine individual practice patterns and perspectives on ethical challenges and resource allocations. Our hypothesis was that there would be wide variation in attitudes and practice patterns amongst trauma surgeons when the goal of resuscitation is organ preservation for future transplantation.
Methods:
Over a 3-month period, we conducted a survey of trauma surgeons at ACS-verified Level I and Level II trauma centers in Tennessee to identify individual practice patterns during acute trauma resuscitation. Participants were eligible if they were trauma surgeons practicing in a trauma center in the state of Tennessee designated as Level I or Level II (8 total trauma centers). The survey instrument was developed in collaboration with trauma surgeons, biomedical ethicists, health policy experts, and survey design experts. Survey items assessed personal demographics, hospital demographics, level of surgeon’s training and experience. Resuscitation practice patterns were assessed with a list of possible therapeutic options. Decision making factors for resuscitation decisions were assessed using a Likert Scale ranging from 1=not important to 5=very important. Extent and limitations of resuscitation therapies which individual surgeons were willing to employ were evaluated using a hypothetical case example and prompting respondents to select Yes or No to a list of resuscitation options. Participants were asked questions regarding resuscitation decisions after being presented with the following theoretical survey scenario: “A 22-year-old man presents after a gunshot wound to the head that appears to be transtentorial. He was previously healthy and was a former school athlete but is now hypotensive and bleeding profusely from his wounds. You do not believe his injuries are survivable. His organ donor wishes are unknown.”
The survey instrument was distributed electronically utilizing the REDCap (Research Electronic Data Capture) application using email requests. No monetary incentives were provided. This study was approved by the Vanderbilt Human Research Protections Program Social and Behavioral Sciences Committee for exemption from review by the Institutional Review Board.
Anonymized survey results from completed surveys from individual surgeons were directly input into the REDCap database which was then queried. Descriptive statistics were calculated to characterize distributions of trauma surgeons’ practice patterns.
Results:
Surgeon Characteristics:
Survey response rate was 51% (31/60). The majority of respondents (71%) were men, the average age of respondents was 45 years, and 94% had completed a fellowship in surgical critical care or trauma or both. All respondents were board certified and 67% reported five or more years of clinical practice. (Complete demographic data are available in Table 1.)
TABLE 1:
Respondent Characteristics for Survey of Trauma Surgeon Resuscitation Ethics for Organ Transplantation after a Non-Survivable Injury (n=31)
| Age | 44.00 (36.33–51.00) |
| Gender | |
| Male | 22 (71) |
| Female | 9 (29) |
| Hospital Characteristics | |
| Level I Trauma Center | 29 (94) |
| Fellowships Completed | |
| Surgical Critical Care | 24 (77) |
| Acute Care Surgery or Trauma Surgery | 15 (48) |
| Neither | 2 (6) |
| Years in Practice | |
| <5 Years | 10 (32) |
| 5–9 Years | 4 (13) |
| 10–14 Years | 5 (16) |
| 15–20 Years | 6 (19) |
| >20 Years | 6 (19) |
Abbreviations: Median (IQR) for continuous variables. n (%) for categorical variables.
Over a 3-month period, we conducted a survey of trauma surgeons at ACS-verified Level I and Level II trauma centers in Tennessee to identify individual practice patterns during acute trauma resuscitation. The survey instrument was developed in collaboration with trauma surgeons, biomedical ethicists, health policy experts, and survey design experts. Survey items assessed personal demographics, level of surgeon’s experience, and hospital demographics.
Most respondents (81%) reported having personal experience resuscitating a trauma patient with the primary goal of preserving organs for donation, with 26% of participants reporting doing so on a weekly basis, while 90% reported no less frequently than monthly. When deciding to initiate resuscitation for organ preservation, respondents most frequently identified the patient’s potential for organ donation (e.g., young, healthy) as the most important factor.
Institutional Setting of Survey Respondents:
All 31 participants reported practicing in a hospital where organ procurements occur. Most (71%) worked in institutions that also have a transplant surgery service. All 31 respondents indicated that their institution had a protocol in place for determination of brain death, however a small minority (10%) responded that brain death testing was only available during daytime hours in their institutions. Most (71%) reported that their institution had a protocol in place for care of organ donors, while another 10% did not know if such a protocol existed in their hospital.
Factors Influencing Forgoing or Stopping Resuscitation Efforts in a Potential Organ Donor:
When we asked respondents about our hypothetical scenario, respect for the dying process and concerns about organ quality were prominent considerations in forgoing or stopping resuscitation efforts. A substantial majority (84% and 83%, respectively) characterized these factors as important or very important (Figure 1). These factors were followed closely by concerns about excessive resource utilization (81%). Many (74%) endorsed having ethical concerns about resuscitating a patient with low likelihood of survival. Less important factors in resuscitation practices were unknown donor status and a general sentiment that resuscitation in that setting felt wrong. When determining a patient’s organ donor wishes, 90% agreed or strongly agreed that indication on a patient’s driver’s license was sufficient confirmation of their organ donor status, however 90% also disagreed or strongly disagreed with using the absence of that indication on the license as a way to confirm that a patient does not wish to be an organ donor.
FIGURE 1:
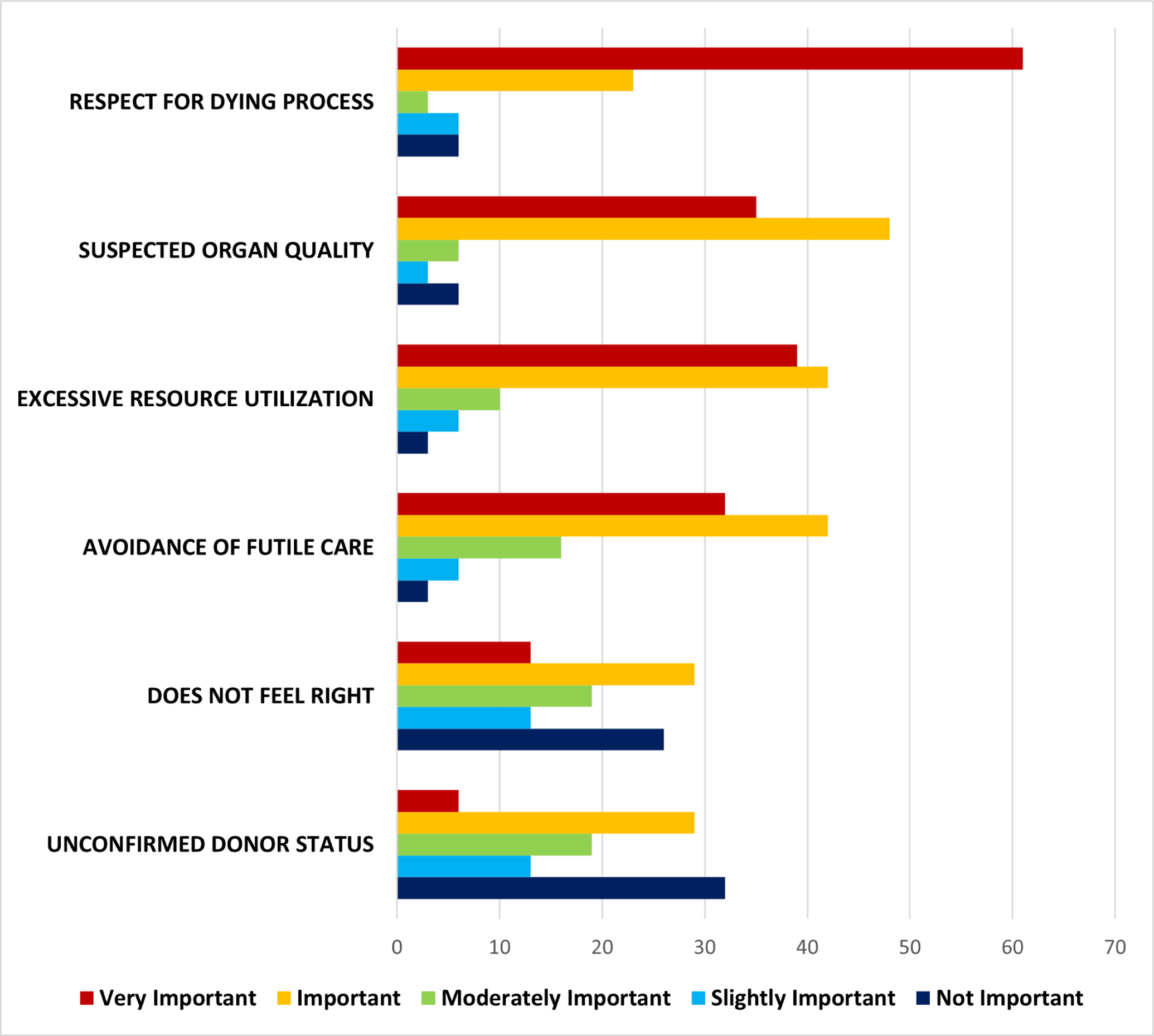
Ethical Factors Considered by Trauma Surgeons in Resuscitating a Non-Survivable Injury for Transplantation
Over a 3-month period, we conducted a survey of trauma surgeons at ACS-verified Level I and Level II trauma centers in Tennessee to identify individual practice patterns during acute trauma resuscitation. Ethical concerns about resuscitating with a goal of preserving organ donation and transplantation potential in cases of non-survivable injury were assessed using a hypothetical sample patient scenario of a 22-year-old previously healthy man who presents after a gunshot wound to the head which appears to be transtentorial.
Extent of Resuscitation Measures:
All respondents were willing to perform endotracheal intubation, with a slight majority (61%) also willing to perform a surgical airway. Most would initiate at least one vasopressor (94%) and would transfuse blood products (84%). Typically, participants were willing to give up to 3–6 units of blood, but ranged from limiting to one unit to willingness to initiate massive transfusion (>10 units). In contrast, a large majority of respondents (90%) were not willing to perform a resuscitative thoracotomy to preserve organ donation potential.
Discussion:
This is the first study examining practices and priorities of trauma surgeons in the setting of treating patients of uncertain organ donor status suffering from non-survivable injuries with potential for organ donation. These findings suggest a high degree of variability in practice when determining whether, when, and how to resuscitate these patients to preserve organs for possible transplantation when donor status is unknown. The range of acute resuscitation measures with which surveyed trauma surgeons were comfortable was wide, with some willing to employ very few interventions or resources to attempt organ preservation (and actively unwilling to do more), while other surgeons were inclined to spend significant resources (e.g., >10 units of blood) or to perform heroic procedures (e.g., resuscitative thoracotomy) to meet this outcome. Ethical issues considered important in acute resuscitation decision making also varied, however most surgeons agreed on the importance of a few key factors including respect for the patient’s dying process, likely organ quality, and excessive resource utilization when deciding to forgo or to stop resuscitative efforts.
We are not aware of other regional or national data on trauma surgeons’ practice patterns in this setting. However, in 2018, a case commentary3 considered a similar hypothetical resuscitation for organ donation scenario of a fatal 90 percent total body surface area burn. The authors described several potential ethical tensions, like supporting the patient’s death in a dignified, comfortable manner; avoiding futile care4 which could cause suffering; elucidating the patient’s organ donor status from family in a timely fashion, out of respect for autonomous wishes to donate or not to donate; and balancing professional and ethical duties and obligations to individual trauma patients and to populations in need of organ transplantation. After identifying imminent death, they highlight how the trauma team must make a well-timed and definitive decision to shift efforts to determining organ donor status. In so doing, they cite the importance of timely, evidence-based determination of physiologic futility, after which organ preservation can be pursued in an ethical manner which maximizes likelihood of graft survival5.
Our results show notable surgeon-to-surgeon variability in ethical approaches to patients at the individual physician level. Among this regional sample, respect for the patient’s dying process was a primary factor influencing resuscitative decisions for most trauma surgeons, however resource allocation issues were equally important for many. In the absence of specific evidence-based guidelines for the resuscitation of these patients after determination of non-survivability, our findings suggest that when the intent of resuscitation shifts from saving the patient’s life to a primary goal of preserving organ donor potential, trauma surgeons’ practices may encompass a wide range of resuscitative interventions, all while in keeping with institutional-, regional-, and association-level guidance8–10. These may include intubation, blood transfusions, vascular access procedures, thoracostomy tubes, resuscitative thoracotomies, and extracorporeal membrane oxygenation6,7. The cause for variation in practice is not clear, but divergent views on ethical priorities along with differing local resource constraints may partially explain this phenomenon. The results highlight the need for further research to direct organ donor resuscitation in the immediate post-trauma period and, by describing current practice patterns, could represent a step toward future standardization. Empirical research will need to inform the development of future standards and, given the complex nature of the issue, should include qualitative methods analysis to further understand the ethical issues and implications for future policy.
These findings should be interpreted in the setting of several important limitations. First, the nonresponse rate of 49% may represent the nonresponse bias of trauma surgeons who did not complete the survey and may differ significantly in their practice patterns, ethical perspectives, or resource considerations compared with those who did. Second, our small sample size may not capture the complete range of practices, of attitudes (e.g., patient, family, lay public11), and of disciplines (e.g., emergency medicine, nursing, blood bank). Our study suggests practice variation with the potential for significant effects on resource utilization and organ donor potential, but larger studies will need to be done to delineate the regional and cultural factors more clearly. Additionally, the clinical scenario we used to test our hypothesis of clinical variability does not explicitly state whether the resultant potential donation is after brain death (DBD) or donation after cardiac death (DCD). We believe parsing out the differences in practice and perceptions regarding these two modalities will be an important for future studies but was outside the scope of this current study. The state of Tennessee consists of five Level 1 trauma centers and two Level two trauma centers. In general, the Level 1 trauma centers consisted of a larger staff of trauma surgeons than did the level 2 trauma centers. Therefore, the only a small minority of those who were invited to take part in the survey were from one of the two Level 2 trauma centers. Due to limitations from the IRB regarding number of email solicitations we were unable to attract larger numbers from Level 2 trauma centers and hope that future studies will be able to expand on variations in practice at Level 2 and Level 3 centers. We also acknowledge that there may be additional variation that our results from a single region do not reflect, suggesting the need for a broader survey of practice patterns at the national level. Finally, while our survey was developed with the representation of the spectrum of resuscitation possibilities in mind, we recognize the risk of the oversimplification of reality, which is inherent in survey research.
Conclusions:
The wide variations found in a regional study of trauma surgeons’ practice patterns when resuscitating trauma patients with non-survivable injuries for potential for organ donation may imply a lack of professional consensus regarding initiation and extent of resuscitation in this setting. Our data suggest this is a common challenge for practicing trauma surgeons. To fully understand the breadth of this issue, surgeons and policy makers may benefit from further study to determine national variability, regional influences, areas of equipoise, and features amenable to practice guidelines.
Funding/Support
Dr. Peetz is supported by Vanderbilt Institute for Clinical and Translational Research (VICTR) based on funded by National Center for Advancing Translational Sciences (NCATS) Clinical Translational Science Award (CTSA) Program, Award Number UL1TR002243, Dr. Patel is supported by federal grants (NIH/NIA R01GM120484, NIH/NIGMS R01AG058639, VA ORD/RR&D I01RX002992), Dr. Beskow is supported by Vanderbilt Institute for Clinical and Translational Research (VICTR) based on funded by National Center for Advancing Translational Sciences (NCATS) Clinical Translational Science Award (CTSA) Program. REDCap was used to support this project (NCATS/NIH UL1 TR000445).
Abbreviations:
- ACS
American College of Surgeons
- ECMO
Extracorporeal Membrane Oxygenation
- ED
Emergency Department
- OPO
Organ Procurement Organization
- REDCap
Research Electronic Data Capture Application
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Meeting Presentation: This work was presented at the Ethics Track in the Owen H. Wangensteen Scientific Forum of the American College of Surgeons Clinical Congress on October 28, 2019, in San Francisco, CA.
Conflict of interest/Disclosure
The authors have no related conflicts of interest to declare.
References
- 1.Schnüriger B, Inaba K, Branco BC, et al. Organ donation: an important outcome after resuscitative thoracotomy. J Am Coll Surg 2010;211(4):450–455. [DOI] [PubMed] [Google Scholar]
- 2.Malinoski DJ, Patel MS, Lush S, et al. Impact of compliance with the American College of Surgeons trauma center verification requirements on organ donation-related outcomes. J Am Coll Surg 2012;215(2):186–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.DiBrito SR, Henderson ML. Should trauma physicians treat a severely injured patient for the sake of elucidating preferences about organ donation? AMA J Ethics 2018;20(5):447–454. [DOI] [PubMed] [Google Scholar]
- 4.Veatch RM, Spicer CM. Medically futile care: the role of the physician in setting limits. Am J Law Med 1992;18(1–2):15–36. [PubMed] [Google Scholar]
- 5.Wall SP, Goldfrank LR. Death on the waiting list: a failure in public health. Ann Emerg Med 2012;60(4):492–494. [DOI] [PubMed] [Google Scholar]
- 6.Arlt M, Philipp A, Voelkel S, et al. Extracorporeal membrane oxygenation in severe trauma patients with bleeding shock. Resuscitation 2010;81(7):804–809. [DOI] [PubMed] [Google Scholar]
- 7.Bonacchi M, Spina R, Torracchi L, Harmelin G. Extracorporeal life support in patients with severe trauma: an advanced treatment strategy for refractory clinical settings. J Thorac Cardiovasc Surg 2013;145(6):1617–1626. [DOI] [PubMed] [Google Scholar]
- 8.American College of Surgeons. Resources for Optimal Care of the Injured Patient. 6th ed. Chicago: 2014. [Google Scholar]
- 9.Organ Procurement and Transplantation Network. Ethics of Deceased Organ Donor Recovery. 2016.
- 10.American Medical Association. Opinion 6.2.1: Guidelines for Organ Transplantation. Code of Medical Ethics. [Google Scholar]
- 11.Wilson J, Shinall M, Leath T, et al. Worse than death: survey of public perceptions of disability outcomes after hypothetical traumatic brain injury. Ann Surg 2020; [DOI] [PMC free article] [PubMed] [Google Scholar]


