Abstract
Objective:
To compare and evaluate the stability of correction of anterior crossbite in the mixed dentition by fixed or removable appliance therapy.
Material and Methods:
The subjects were 64 consecutive patients who met the following inclusion criteria: early to late mixed dentition, anterior crossbite affecting one or more incisors, no inherent skeletal Class III discrepancy, moderate space deficiency, a nonextraction treatment plan, and no previous orthodontic treatment. The study was designed as a randomized controlled trial with two parallel arms. The patients were randomized for treatment with a removable appliance with protruding springs or with a fixed appliance with multibrackets. The outcome measures were success rates for crossbite correction, overjet, overbite, and arch length. Measurements were made on study casts before treatment (T0), at the end of the retention period (T1), and 2 years after retention (T2).
Results:
At T1 the anterior crossbite had been corrected in all patients in the fixed appliance group and all except one in the removable appliance group. At T2, almost all treatment results remained stable and equal in both groups. From T0 to T1, minor differences were observed between the fixed and removable appliance groups with respect to changes in overjet, overbite, and arch length measurements. These changes had no clinical implications and remained unaltered at T2.
Conclusions:
In the mixed dentition, anterior crossbite affecting one or more incisors can be successfully corrected by either fixed or removable appliances with similar long-term stability; thus, either type of appliance can be recommended.
Keywords: Orthodontics, Anterior crossbite, Stability, Randomized controlled trial
INTRODUCTION
The reported prevalence of anterior crossbites varies between 2.2% and 12%, depending on the age of the subjects, whether an edge-to-edge relationship is included in the data, and the ethnicity of the children studied.1–5 It has also been reported that 36% of subjects with anterior crossbite exhibit functional shift; that is, interincisal contact is possible when the mandible is in centric relationship, implying a pseudo Class III malocclusion with no inherent skeletal Class III discrepancy.5
Anterior crossbite is established in the mixed dentition. Early intervention is therefore recommended to prevent adverse effects on growth and development of the jaws and disturbance of temporal and masseter muscle activity, which would increase the risk of craniomandibular disorders during adolescence.2,4,6–8 Moreover, early treatment improves maxillary lip posture and facial appearance.9
A recent systematic review10 disclosed a wide variety of treatment modalities, more than 12 methods, in use for anterior crossbite correction. However, strong evidence in support of any one technique was lacking. Thus, the review highlighted the need for high-quality clinical trials to identify the most effective intervention for correcting anterior crossbites.
The fundamental goal of orthodontic treatment is to achieve a normal occlusion that is morphologically stable in the long term and functionally and esthetically acceptable. As early correction of anterior crossbite is undertaken in the growing child, it is also important to evaluate posttreatment changes in a long-term perspective. Very few studies, however, have analyzed the posttreatment effects of anterior crossbite correction and most are retrospective in design.11,12 Also lacking are prospective studies comparing the long-term effects of fixed or removable appliance therapy for correcting anterior crossbite in the mixed dentition.10
The aim of the present study, in the form of a randomized controlled trial (RCT), was to compare and evaluate the stability of outcome in patients who had undergone fixed or removable appliance therapy at the mixed dentition stage to correct crossbites affecting one or more incisors. The null hypothesis was that the two treatment methods achieve similar long-term outcomes.
MATERIALS AND METHODS
The original study sample comprised 62 subjects (25 girls and 37 boys) with one or more incisors in anterior crossbite with functional shift. The study was approved by the Ethics Committee of Lund University, Lund, Sweden (Dnr: 334/2004). All patients and parents were informed of the purpose of the trial. Written, informed consent was required before enrolment.
The patients were consecutively recruited between 2004 and 2009 from the Department of Orthodontics, Faculty of Odontology, Malmö University, Malmö, Sweden, and from one public dental health service clinic in Malmö, Skåne County Council, Sweden. All patients met the following inclusion criteria: early to late mixed dentition; anterior crossbite affecting one or more incisors; anterior crossbite with functional shift, that is, interincisal contact is possible when the mandibular is in the centric relation (1 to 3 mm sliding from centric relation to centric occlusion), no inherent skeletal Class III discrepancy (ANB angle > 0°), moderate space deficiency in the maxilla (up to 4 mm), a nonextraction treatment plan, and no previous orthodontic treatment.
Half of the subjects were randomly allocated to removable therapy and half to fixed appliance therapy. Two orthodontists and one postgraduate student undergoing specialist training in orthodontics and under the supervision of an orthodontist then treated the patients according to a pre-set concept. Study casts were made at pretreatment, that is, at baseline (T0); at postretention, that is, after treatment, including the retention period (T1); and at follow-up, that is, 2 years postretention (T2).
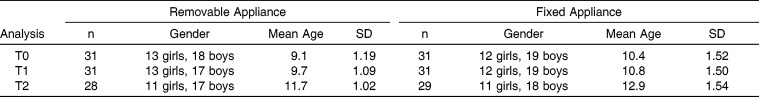
One subject in the removable appliance group withdrew from the study after noncompliance between T0 and T1. Another subject in the removable appliance group had a relapse between T1 and T2 and was retreated with a fixed appliance. Moreover, four subjects, two from each group, were excluded because they could not be contacted for the two-year follow-up. Thus, the study comprised 57 subjects, 28 treated with removable appliances and 29 with fixed appliances. The patient flow is illustrated in Figure 1. Table 1 presents the sample size, gender, and age distribution of the subjects at pretreatment/baseline (T0), at postretention (T1), and at follow-up 2 years postretention (T2).
Figure 1.
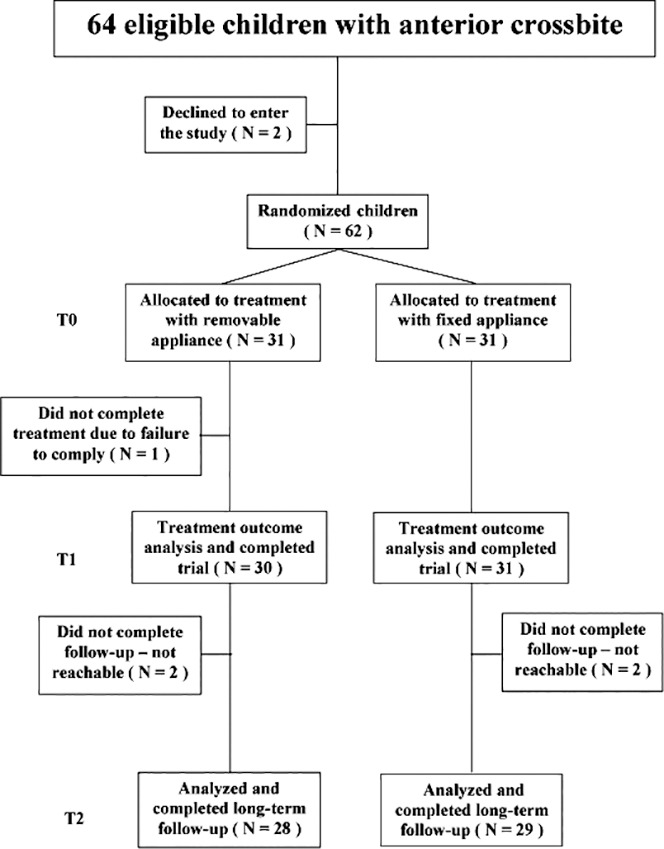
Flow chart of the patients in the study.
Table 1.
Gender, Mean Ages, and Standard Deviations (SDs) at Baseline (T0), at Posttreatment, Including the Retention Period (T1), and at the 2-Year Follow-up (T2)
The following outcome measures were assessed:
Success rate of anterior crossbite correction (yes or no);
Treatment duration in months, from insertion to date of appliance removal;
Overjet and overbite in millimeters;
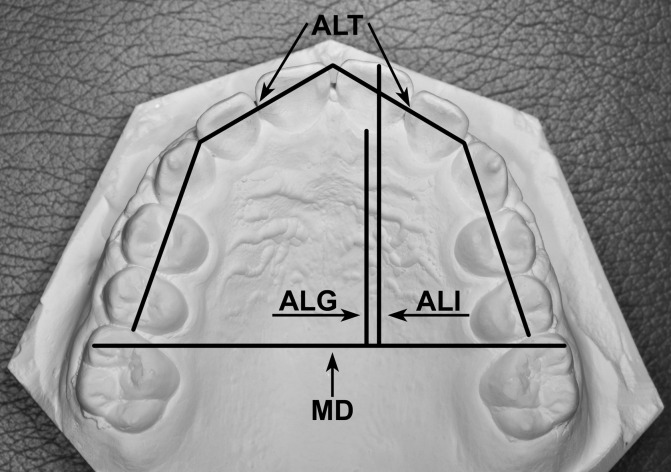
Arch length incisal: distance in millimeters from the incisal edge of the maxillary incisor in anterior crossbite to tangents of the mesiobuccal cusp tips of the maxillary first molar (Figure 2);
Arch length gingival: distance in millimeters from the gingival margin of the maxillary incisor in anterior crossbite to tangents of the mesiobuccal cusp tips of the maxillary first molar (Figure 2);
Maxillary dental arch length total: distance in millimeters at the alveolar crest between the mesial surface of the left and right maxillary first molars (Figure 2);
Transverse maxillary molar distance: transverse distance in millimeters between the mesiobuccal cusp tips of the maxillary first molars (Figure 2).
Figure 2.
Sagittal and transverse measurements made on the maxillary study casts. For definitions of the different variables, see the list of outcome measures in the Materials and Methods section.
Successful treatment was defined as positive overjet (normal interincisal relationship) for all incisors at T1 and T2.
The overjet, overbite, arch length, and transverse maxillary molar distance were measured with a digital sliding caliper (Digital 6, 8M007906, Mauser-Messzeug GmbH, Oberndorf/Neckar, Germany). All measurements were made to the nearest 0.1 mm by an orthodontist (Dr Wiedel). Changes in the different measures were calculated as the difference between T1 and T0, T2 and T1, and T2 and T0. All study cast measurements were blinded, that is, the examiner was unaware of the group to which the patient belonged. Furthermore, the T0, T1, and T2 casts were randomized for measurements. Finally, the duration of treatment was registered from the patient files.
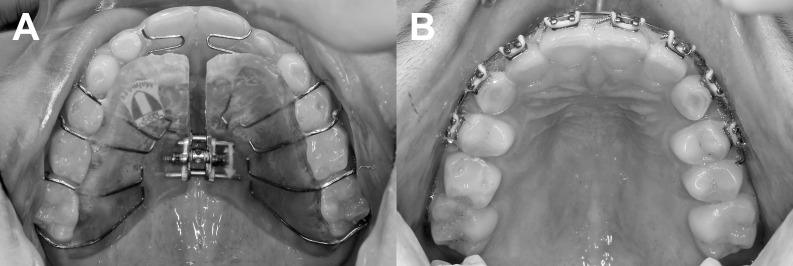
The removable appliance (Figure 3A) comprised an acrylic plate with protrusion springs for the incisors in anterior crossbite, bilateral occlusal coverage of the posterior teeth, an expansion screw, stainless steel clasps on either the first deciduous molars or the first premolars (if erupted) and the permanent molars. The protrusion springs were activated once a month until normal incisor overjet was achieved. Lateral occlusal coverage (1 to 2 mm of thickness) was used to avoid vertical interlock between the incisors in crossbite and the mandibular incisors and also to increase the retention of the appliance. The occlusal coverage was removed as soon as the anterior crossbite was corrected. An inactive expansion screw was inserted into the appliance. The screw was activated during the treatment period only if it was judged to comply with the natural transverse growth of the jaw.
Figure 3.
Occlusal view of (A) the removable orthodontic appliance and (B) the fixed orthodontic appliance. The lateral occlusal coverage of the removable appliance has just been removed because the maxillary incisors were the in correct position and the anterior crossbite was corrected. Also, the expansion screw has been activated during the treatment because it was judged to comply with the natural transverse growth of the jaw.
The dentist instructed the patient firmly to wear the appliance day and night, except for meals and tooth-brushing, that is, the appliance was to be worn at least 22 hours a day. Progress was evaluated every 4 weeks. The same appliance then served as a passive retainer for a retention period of 3 months.
The fixed appliance (Figure 3B) consisted of stainless steel brackets (Victory, slot 0.022″, 3M Unitek, Monrovia, Calif). Usually, eight brackets were bonded to the maxillary incisors, the deciduous canines, and either the first deciduous molars or the first premolars, if erupted. All patients were treated according to a standard straight-wire concept designed for light forces.13 The archwire sequence was: 0.016 heat-activated nickel-titanium, 0.019 × 0.025″ heat-activated nickel-titanium, and finally 0.019 × 0.025″ stainless steel wire. To raise the bite, composite (Point Four, 3M Unitek) was bonded to the occlusal surfaces of both the mandibular second deciduous molars. This prevented vertical interlock between the incisors in crossbite and the mandibular incisors. The composite was removed as soon as the anterior crossbite was corrected. Progress was evaluated every 4weeks. The same fixed appliance then served as a passive retainer for a retention period of 3 months.
Statistical Analysis
SPSS software (version 21.0, SPSS Statistics, Chicago, IL) was used for statistical analysis of the data. For categorical variables, the χ2 test was used. Arithmetic means and standard deviations were calculated for numerical variables. To compare active treatment time and treatment effects between the groups, an independent sample t-test was used for analysis of means. Differences with probabilities of less than 5% (P < .05) were considered statistically significant.
Ten randomly selected study casts were measured on two occasions, at an interval of at least 1 month.
RESULTS
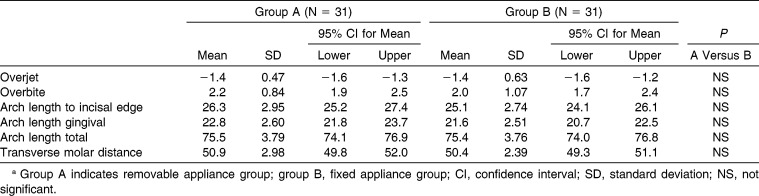
The baseline measurement variables before treatment are summarized in Table 2. No significant differences were found between the groups, except for age (P < .05) (Table 1). There was no significant intergroup difference in the number of maxillary incisors in anterior crossbite before treatment. No significant gender differences were found for any of the study variables; hence, the data for boys and girls were pooled for analysis. Paired t-tests disclosed no significant mean differences between the two series of records. The error of the method did not exceed 0.13 mm for any study variable.
Table 2.
Baseline Measurements (T0) (in Millimeters)a
The crossbites of all patients in the fixed appliance group, and all except one in the removable appliance group, were successfully corrected during the treatment period (T0–T1). Treatment duration was significantly shorter (mean, 1.4 months; P < .05) in the fixed appliance group (mean, 5.5 months; SD, 1.41) than in the removable group (mean, 6.9 months; SD, 2.8).
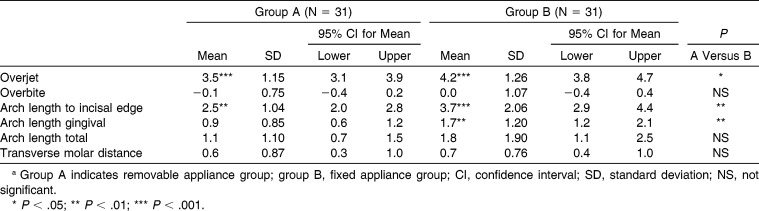
Overjet and incisal arch length increased significantly in both groups between T0 and T1 (Table 3). The fixed appliance group also showed a significant increase in gingival arch length (Table 3). The increase in overjet after treatment was significantly greater in the fixed appliance group (P < .05). This group also exhibited significantly greater increases in incisal and gingival arch lengths after treatment, as shown in Table 3. There were no intergroup differences with respect to overbite, total maxillary dental arch length and transverse maxillary molar distance (Table 3).
Table 3.
Changes in different Measures (in Millimeters) Within and Between Groups Calculated as the Difference Between T1 (Posttreatment, Including the Retention Period) and T0 (Pretreatment)a
At the 2-year follow-up, relapses had occurred in three subjects. Thus, 27 of 29 patients in the fixed apliance group and 27 of 28 patients in the removable appliance group had maintained normal interincisal relationships. It was also noted that, at follow-up, transition to the permanent dentition had occurred in most of the subjects in both groups.
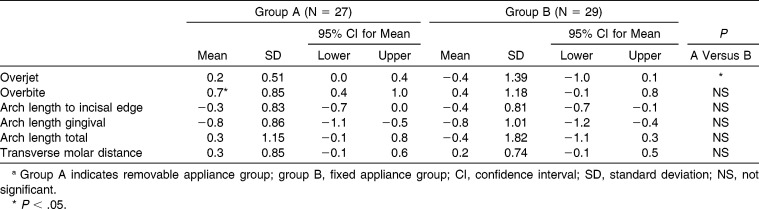
During the follow-up period (T1–T2), a small but significant increase in overbite occurred in the removable appliance group and a small, albeit significant, intergroup difference was found with respect to overjet. There were no other significant changes in the outcome variables (Table 4).
Table 4.
Changes in Measures (in Millimeters) Within and Between Groups Calculated as the Difference Between T2 (2-Year Follow-up) and T1 (Posttreatment, Including Retention Period)a
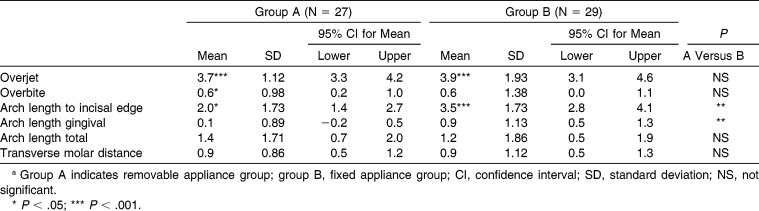
The overall changes during the study period (T0–T2) are shown in Table 5. Significant increases in overjet and incisal arch length were found in both groups. In the fixed appliance group, incisal arch length and gingival arch length increased significantly more than in the removable appliance group. No other significant intragroup or intergroup differences were observed.
Table 5.
Overall Changes in Measures (in Millimeters) Within and Between Groups Calculated as the Difference Between T2 (2-Year Follow-up) and T0 (Pretreatment)a
DISCUSSION
The results of this RCT confirm the initial hypothesis that at follow-up the outcomes in the two treatment groups were comparable: in the mixed dentition, anterior crossbite affecting one or more incisors can be successfully corrected by either fixed or removable appliances with similar stability and equally favorable prognoses. Thus, either type of appliance can be recommended to correct anterior crossbite affecting one or more incisors in the mixed dentition.
The success rate of both treatment methods was high at completion of treatment and at the 2-year follow-up. In the removable appliance group there was a significant increase in overbite during the follow-up period, which could also have contributed to the stable treatment results. In both groups there were minor decreases in arch length at the 2-year follow-up. These changes had no clinical implications. In all, three patients relapsed over the entire trial period, one in the removable appliance group and two in the fixed appliance group. Because of ethical regulations, lateral head radiographs was not assessed 2 years after retention, and therefore, we have no data to show whether unfavorable growth of the mandible may have occurred in these patients. Ideally, the study should have included an untreated control group of patients with anterior crossbite to evaluate the potential impact of the condition on long-term growth. However, postponement of a needed intervention for 3 years was regarded as ethically unacceptable. Nevertheless, the RCT design permits the reduction of the risk of normal growth bias between the groups.
In general, stability after orthodontic treatment is reported to vary, though most relapses occurring during the first 2 years after retention.14 Consequently, the follow-up period of 2 years used in this study was adequate for long-term conclusions, and at T2, transition to the permanent dentition had occurred in most of the subjects in both groups. Ideally, an even longer follow-up period than 2 years would have been preferable, but as it was found that at 2 years after retention almost all subjects had good Class I occlusion with normal overjet and overbite, the prognosis was favorable for the treatment and postretention results to be stable in the future. Moreover, analyses of retrospective data on patients with anterior crossbite and functional shift treated with 2 × 4 fixed appliances have disclosed stable results 511 and 10 years after treatment.12 These studies support a favorable long-term prognosis for correcting anterior crossbite affecting one or more incisors in the mixed dentition.
A recent systematic review disclosed the lack of RCTs comparing the effectiveness of fixed and removable appliances in correcting anterior crossbite and the lack of long-term evaluations.10 Thus, no comparison can be made with previous studies. Although not directly comparable, a multicenter RCT15 of early Class III orthopedic treatment with a protraction facemask versus untreated controls reported successful outcomes in 70% of the subjects. An RCT studying correction of unilateral posterior crossbite in the mixed dentition16 reported and confirmed that fixed appliance (Quad-helix) therapy was superior to removable appliance (expansion plate) therapy: one-third of the failures in the removable appliance group were attributed to poor patient compliance. This is in contrast to the high success rate in the present study. It is likely that patients with anterior crossbite are more aware of their malocclusion: unlike posterior crossbite, it is a very obvious and esthetically disturbing condition. Hence, our patients were obviously highly motivated and keen to comply with treatment.
The rationale for selecting an RCT design was to reduce the risk of error from such factors as selection bias, the clinician's preferred treatment method, and the differences in the skills of the operators with respect to the two treatment methods. Furthermore, random allocation of subjects reduces bias and confounding variables by ensuring that both known and unknown determinants of outcome are evenly distributed among the subjects. The prospective design also ensures that the baseline characteristics, treatment progression, and side effects can be strictly controlled and accurately observed. A drawback was that a significant mean difference in age was found between the groups; the explanation for this is unclear, even though the randomization should have avoided the age difference. In any event, the age difference was regarded to be of minor importance because all subjects followed all the inclusion criteria, and thus, for example, were in the same dental age, that is, early to late mixed dentition.
Moreover, to reduce the risk of bias, measurement of the study casts was blinded; the examiner was unaware of the patients' groups. Thus, the design and methodology ensured good external validity of the results.
In a long-term study, the effect on outcomes of subject dropout during the trial must be considered. However, in the present study the attrition rate was small, ensuring that the outcomes were not biased by loss of data.
The present study evaluated a relatively limited number of outcome measures. The primary aim was to compare long-term success rates of fixed and removable appliance therapy, but a further aim was to assess changes in overjet and maxillary arch length as well as tipping effects on the maxillary incisors. These outcome measures are highly relevant to the clinician.
Having established that the two treatment strategies are equally effective with respect to clinical outcomes, other aspects now warrant investigation. A comparative study of the cost-effectiveness of the two methods is currently in progress. Another important aspect of treatment that warrants investigation is that of patient perceptions of treatment by fixed or removable appliances.
CONCLUSIONS
In the mixed dentition, anterior crossbite affecting one or more incisors can be successfully corrected by either fixed or removable appliances with similar stability and equally favorable prognoses.
Either type of appliance can be recommended.
REFERENCES
- 1.Keski-Nisula K, Lehto R, Lusa V, Keski-Nisula L, Varrela J. Occurrence of malocclusion and need of orthodontic treatment in early mixed dentition. Am J Orthod Dentofacial Orthop. 2003;124:631–638. doi: 10.1016/j.ajodo.2003.02.001. [DOI] [PubMed] [Google Scholar]
- 2.Karaiskos N, Wiltshire WA, Odlum O, Brothwell D, Hassard TH. Preventive and interceptive orthodontic treatment needs of an inner-city group of 6- and 9-year-old Canadian children. J Canad Dent Assoc. 2005;71:649a–649e. [PubMed] [Google Scholar]
- 3.Lux CJ, Ducker B, Pritsch M, Komposch G, Niekusch U. Occlusal status and prevalence of occlusal malocclusion traits among 9-year-old schoolchildren. Eur J Orthod. 2009;31:294–299. doi: 10.1093/ejo/cjn116. [DOI] [PubMed] [Google Scholar]
- 4.Schopf P. Indication for and frequency of early orthodontic therapy or interceptive measures. J Orofacial Orthop. 2003;64:186–200. doi: 10.1007/s00056-003-0234-6. [DOI] [PubMed] [Google Scholar]
- 5.Thilander B, Myrberg N. The prevalence of malocclusion in Swedish schoolchildren. Scand J Dent Res. 1973;81:12–20. doi: 10.1111/j.1600-0722.1973.tb01489.x. [DOI] [PubMed] [Google Scholar]
- 6.Lee BD. Correction of cross-bite. Dent Clin North Am. 1978;22:647–668. [PubMed] [Google Scholar]
- 7.Ngan P, Hu AM, Fields HW., Jr Treatment of Class III problems begins with differential diagnosis of anterior crossbites. Pediatr Dent. 1997;19:386–395. [PubMed] [Google Scholar]
- 8.Vakiparta MK, Kerosuo HM, Nystrom ME, Heikinheimo KA. Orthodontic treatment need from eight to 12 years of age in an early treatment oriented public health care system: a prospective study. Angle Orthod. 2005;75:344–349. doi: 10.1043/0003-3219(2005)75[344:OTNFET]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 9.Croll TP, Riesenberger RE. Anterior crossbite correction in the primary dentition using fixed inclined planes. I. Technique and examples. Quint Int. 1987;18:847–853. [PubMed] [Google Scholar]
- 10.Borrie F, Bearn D. Early correction of anterior crossbites: a systematic review. J Orthod. 2011;38:175–184. doi: 10.1179/14653121141443. [DOI] [PubMed] [Google Scholar]
- 11.Hägg U, Tse A, Bendeus M, Rabie AB. A follow-up study of early treatment of pseudo Class III malocclusion. Angle Orthod. 2004;74:465–472. doi: 10.1043/0003-3219(2004)074<0465:AFSOET>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 12.Anderson I, Rabie AB, Wong RW. Early treatment of pseudo-class III malocclusion: a 10-year follow-up study. J Clin Orthod. 2009;43:692–698. [PubMed] [Google Scholar]
- 13.McLaughlin RP, Bennett J, Trevisi H. Systemized Orthodontic Treatment Mechanics. London: Mosby International Ltd; 2001. [Google Scholar]
- 14.Kuijpers-Jagtman AM, Al Yami EA, van't Hof MA. Long-term stability of orthodontic treatment. Ned Tijdschr Tandheelkd. 2000;107:178–181. [PubMed] [Google Scholar]
- 15.Mandall N, DiBiase A, Littlewood S, et al. Is early Class III protraction facemask treatment effective? A multicentre, randomized, controlled trial: 15-month follow-up. J Orthod. 2010;37:149–161. doi: 10.1179/14653121043056. [DOI] [PubMed] [Google Scholar]
- 16.Petrén S, Bjerklin K, Bondemark L. Stability of unilateral posterior crossbite correction in the mixed dentition: a randomized clinical trial with a 3-year follow-up. Am J Orthod Dentofacial Orthop. 2011;139:e73–e81. doi: 10.1016/j.ajodo.2010.06.018. [DOI] [PubMed] [Google Scholar]