Abstract
Vitiligo is the most common depigmenting disorder characterized by white patches in the skin. The pathogenetic origin of vitiligo revolves around autoimmune destruction of melanocytes in which, for instance, oxidative stress is responsible for melanocyte molecular, organelle dysfunction and melanocyte specific antigen exposure as well as melanocyte cell death and thus serves as an important contributor for vitiligo progression. In recent years, natural products have shown a wide range of pharmacological bioactivities against many skin diseases, and this review focuses on the effects and mechanisms of natural compounds against vitiligo models. It is showed that some natural compounds such as flavonoids, phenols, glycosides and coumarins have a protective role in melanocytes and thereby arrest the depigmentation, and, additionally, Nrf2/HO-1, MAPK, JAK/STAT, cAMP/PKA, and Wnt/β-catenin signaling pathways were reported to be implicated in these protective effects. This review discusses the great potential of plant derived natural products as anti-vitiligo agents, as well as the future directions to explore.
Keywords: vitiligo, oxidative stress, natural product, melanocytes, flavonoids, phenols, glycosides
Introduction
Pathogenesis of Vitiligo
Vitiligo is a chronic autoimmune destruction of melanocytes, leading to the pigment loss on the surface of skin and mucosa and then the gradual expansion of decolorized skin plaque (Seneschal et al., 2021). The severity of the disease affects about 1% of humans (Whitton et al., 2015). Clinically, vitiligo is divided into segmental vitiligo (SV), non-segmental vitiligo (NSV) and mixed vitiligo (MV) (Ezzedine et al., 2015). NSV is the most common type of vitiligo. Its clinical features are clear boundary, reticular, different size, different distribution, depigmentation and milky white. SV is a piece or several pieces, along the skin area dominated by a certain cutaneous ganglion segment, generally unilateral, accounting for 5–16% of all vitiligo cases (Speeckaert et al., 2020). MV includes the combination of SV and then bilateral NSV plaque after a period of time (Ezzedine et al., 2015). The debilitating nature of vitiligo leads to poor quality of life and mental health (Patel et al., 2017). Dermal exposure to UV light from depigmented skin increases the risk of skin irritation and cancer (Ahluwalia et al., 2017).
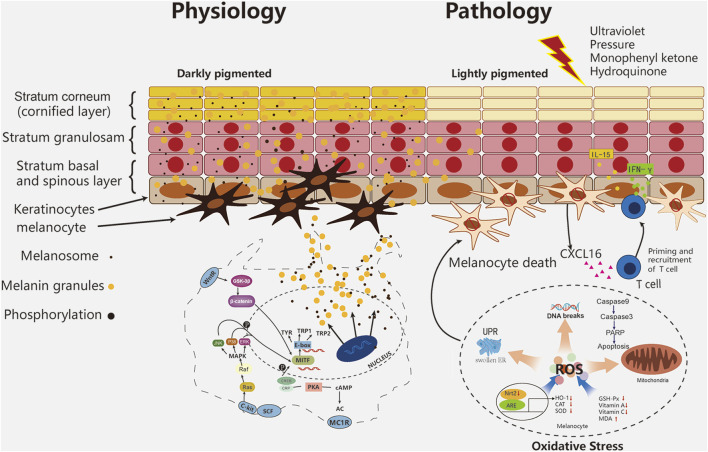
The main theories of the pathogenesis of vitiligo are: 1) oxidative stress theory, 2) autoimmune theory, 3) neural theory and 4) biochemical theory. The autoimmune theory is the most accepted one (Rodrigues et al., 2017). More than half of the 40 susceptibility genes revealed by genome-wide analysis are involved in immunoregulatory activities (Jin et al., 2016). Strong evidence shows that oxidative stress is a key factor in the occurrence and development of diseases (Denat et al., 2014). Several endogenous and exogenous stimuli are related to the occurrence of diseases. Endogenous factors include melanin synthesis, proliferation, differentiation, cell metabolism, immune response and apoptosis (Al-Shobaili and Rasheed 2015). Exogenous stimuli include exposure to the environment (e.g., cytotoxic chemicals, trauma, UV exposure, monophenones and other phenolics), other diseases (severe infections, neurological disorders, malignancies, calcium imbalance), and pharmaceutical applications (e.g., certain hormones, vaccination, drugs) (Xie et al., 2016). These all induce oxidative stress in melanocytes, which may be important in activating autoimmune responses associated with vitiligo (Abdel-Malek et al., 2020; Chen X. et al., 2019; Xie et al., 2016). The decrease of the level and activity of antioxidant enzymes (such as catalase and glutathione peroxidase) and the imbalance of Pro oxidation/anti oxidation balance are also the reasons for the production and accumulation of ROS (Wang Y. et al., 2019). Nrf2-ARE regulates cellular protective genes related to oxidative stress (Jian et al., 2011). In vitiligo melanocytes, Nrf2 has nuclear translocation and decreased transcriptional activity, resulting in decreased HO-1 expression and abnormal redox balance (Jian et al., 2014). Due to the deficiency of antioxidant function, melanocytes in vitiligo are particularly sensitive to ROS accumulation, which leads to DNA damage, protein oxidation/breakage, mitochondrial dysfunction, endoplasmic reticulum abnormalities and lipid peroxidation (Bickers and Athar 2006; Chen J. et al., 2021). Increased ROS levels even modified tyrosinase (Tyr) and other melanin proteins into new antigens (Rodrigues et al., 2017). Oxidative stress leads to the accumulation of misfolded proteins in the lumen of the endoplasmic reticulum (ER), which in turn activates the unfolded protein response (UPR) to restore cellular homeostasis and maintain cell survival. The disturbance of endoplasmic reticulum Ca2+ triggered by oxidative stress may also induce UPR and apoptosis (Carreras-Sureda et al., 2018). Under continuous cell pressure, UPR promotes autoimmune response through apoptosis cascade, and then activates CD8+ T cells to produce adaptive immune response, and T cells release interferon-γ (INF-γ), It binds to receptors on keratinocytes, further releases and presents inflammatory cytokines such as CXC-L16 and IL-15, and further recruits T cells to the skin through a positive feedback loop (Bergqvist and Ezzedine 2021). The recruitment of CD8+and T cells induced by cytokines and chemokines ensure the final destruction of epidermal melanocytes (Figure 1). After naive T cells are activated by antigen-presenting cells, a small subset of these precursor cells eventually develop into several subsets of memory T cells, including effector memory T (TEM) cells, tissue resident memory T (TRM) cells and central memory T (TCM) cells. TRM play a major role in vitiligo recurrence (Chen and Shen 2020). In the process, melanocytes, fibroblasts, innate lymphoid cells, natural killer cells, and keratinocytes collectively contribute to the pathogenesis of vitiligo (Seneschal et al., 2021).
FIGURE 1.
Melanocyte pathophysiology in vitiligo.
Vitiligo Therapy
However, there is no clear treatment for local and systemic vitiligo. The most widely used therapy is local steroid and narrowband ultraviolet B monotherapy (Grimes and Nashawati 2017), they are not effective in all patients and are expensive, not easily accepted, and are associated with side effects (Huo et al., 2014). Local corticosteroids, calcineurin inhibitors and phototherapy are still the basis of treatment, and long-term use of steroids can lead to decreased immunity (Whitton et al., 2016). Among the numerous treatments currently available, including medical, physical, or surgical approaches, each modality has its disadvantages and side effects (Yamaguchi et al., 2007).
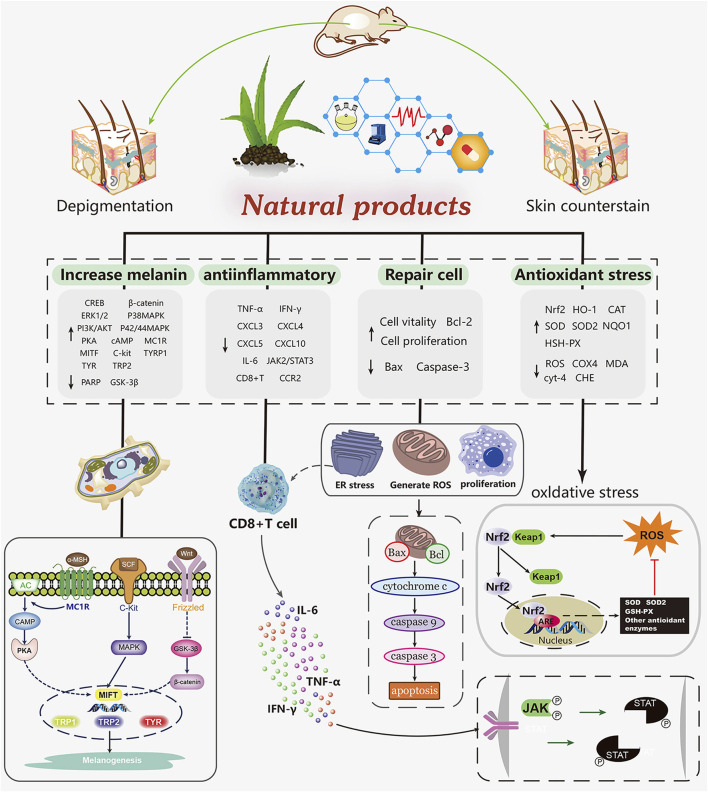
In vivo and in vitro experiments, natural products have been shown to promote melanin production and prevent melanin from being destroyed in a network way. It mainly includes scavenging free radicals (NOS) to alleviate the damage of melanocytes caused by oxidative stress, activating melanogenesis related pathways, increasing the expression of tyrosinase gene, reducing the expression of chemokines and inflammatory cytokines, preventing the migration of CD8 + T cells. This paper reviews several natural drugs for the treatment of vitiligo. Among the natural products that we screened, 16 compounds (such as baicalein, quercetin, paeonol. etc) exert antioxidant effects to protect melanocytes by scavenging free radicals, activating the Nrf2/HO-1 pathway, while maintaining normal cell morphology, slowing down apoptosis and preventing injury. Four compounds (vitexin, baicalin, EGCG and berberine) achieved repigmentation of vitiligo skin lesions via anti-inflammatory effects, the process of which involved the activation of the JAK/STAT pathway as well as the inhibition of autoimmunity caused by the migration of immune cells such as CD8 + T. In mammals, there are three major melanocyte specific enzymes catalyzing melanin biosynthesis: tyrosinase (TYR), tyrosinase associated protein 1 (TRP-1) and TRP-2. TRP-1 and Trp-2 are downstream functional proteins of TYR (Yin et al., 2018). Microphthalmia associated transcription factor (MITF) is a transcription factor important for melanogenesis genes (Hearing 1999). Previous studies summarized three main pathways of melanin biosynthesis regulated by tyrosinase: MAPK, cAMP/PKA, Wnt/β - catenin signaling pathway, and reviewed the effects of several natural products on melanin synthesis and tyrosinase activity (Niu and Aisa 2017; Pillaiyar et al., 2017). Among the compounds we screened, 37 compounds (such as quercetin, afzelin, puerarin, geniposide, etc) promote melanocyte generation through the above pathways (Figure 2).
FIGURE 2.
Mechanism of natural products in the treatment of vitiligo.
Flavonoids
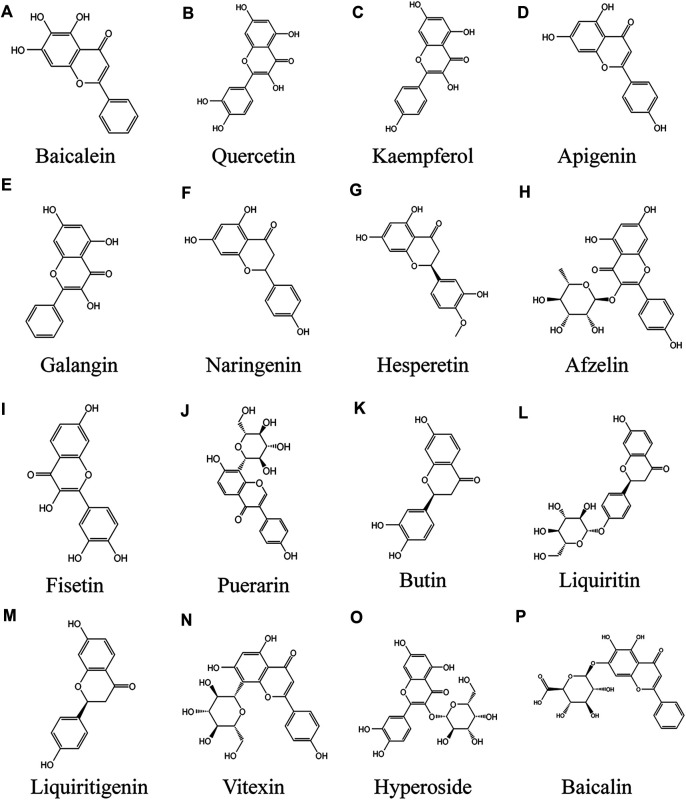
Baicalein
Baicalein is a flavonoid extracted from the roots of Scutellaria baicalensis Georgi that has been extensively applied in Traditional Medicine in Asia (Figure 3A) (Kim et al., 2014). It has been reported to have anti-cytotoxic, anti-inflammatory, and anti-tumor effects (Huang et al., 2005; Hwang et al., 2005; Yarla et al., 2016). In addition, the antioxidant effects of baicalein have received special attention during the past decades, including reducing the levels of reactive oxygen species (ROS) generated by chemical agents (Chiu et al., 2010; Choi et al., 2016; Zhao et al., 2018) or ultraviolet radiation (Wang et al., 2018). Baicalein has strong antioxidant properties, partly because compounds scavenge ROS by oxidative consumption of the three 5, 6, 7-position OH–groups in its structure (de Oliveira et al., 2015), and it form stable semiquinone radicals, which also underlie its powerful antioxidant activity (Gao et al., 1999). The apoptosis of PIG1 cells induced by H2O2 may be mediated by mitochondrial pathway. In the in vitro model of H2O2-induced oxidative stress of PIG1, baicalein protected PIG1 cells from H2O2-induced oxidative stress and apoptosis, maintained mitochondrial membrane potential, released cytochrome c, and decreased the Bax/Bcl-2 ratio. The mechanism mainly involves the activation of mitochondrial dependent caspase and the regulation of p38MAPK pathway. Baicalein at the concentration of 40 µM had the strongest protective effect on melanocytes (Liu et al., 2012). In human vitiligo melanocytes (PIG3V) induced by hydrogen peroxide, baicalein increased the expression of Nrf2 and its downstream gene HO-1 in PIG3V cells, promoted the translocation of Nrf2 from cytoplasm to nucleus, indicating that the protective effect of baicalein on melanocytes depends on Nrf2 signaling pathway (Ma et al., 2018). Baicalein also has antioxidant effect on keratinocytes (Wang et al., 2018), therefore, the development of baicalein topical preparation for the treatment of vitiligo may be a feasible method.
FIGURE 3.
Anti vitiligo flavonoids (A) Baicalein, (B) Quercetin, (C) Kaempferol, (D) Apigenin, (E) Galangin, (F) Naringenin, (G) Hesperetin, (H) Afzelin, (I) Fisetin, (J) Puerarin, (K) Butin, (L) Liquiritin, (M) Liquiritigenin, (N) Vitexin, (O) Hyperoside, (P) Baicalin.
Quercetin
Quercetin is a kind of polyhydroxy flavonoid, which is chemically named 3,3,4,5,7-pentahydroxyflavone (Figure 3B). It has high content in apple, onion and green tea, and also exists in Asparagus racemosus Willd., Ficus ingens (Miq.) Miq., Coriandrum sativum L. and Capparis spinosa L. It is one of the most consumed flavonoids in people's daily diet (Alvarez-Arellano et al., 2020). Quercetin has a variety of biological activities, such as antioxidant and scavenging free radicals (Wang et al., 2021e), anti-cancer, anti-aging (Zhu et al., 2015), anti-inflammatory (Rauf et al., 2018; Cui et al., 2019) anti-virus and immune regulation (Zhu et al., 2015; Alvarez-Arellano et al., 2020). It has a very important clinical significance in the treatment of bacterial infection, viral infection, hyperlipidemia and immune system diseases, especially for those caused by increased oxidative stress Cell damage and even mitochondrial dysfunction related diseases have potential therapeutic effects. Quercetin treatment of cultured melanoma cells or NHEM promote melanin synthesis and tyrosinase activity. In cell experiment, treatment of HMVII cells with quercetin at different doses (1, 5, 10, 20 μm) and for different times (1, 3, 5, 7 days) resulted in a dose and time-dependent increase in melanin content. The mechanism of action may be reflected by the genomic mechanism of new messenger RNA and protein synthesis (Nagata et al., 2004). Interestingly, the triple combination of GT extract/quercetin/folic acid prevented H2O2-induced cell damage in a synergistic manner, suggesting that effective antioxidant combinations should be studied to combat ROS types. Among them, quercetin and GT extract had strong protective effect on H2O2 induced cell death, and 100 μm quercetin had the most significant protective effect (Jeong et al., 2005). Cuiping Guan et al. observed endoplasmic reticulum expansion and configuration changes in cells treated with H2O2 and NaOH/H2O2. Quercetin alleviated the increase of ROS level induced by H2O2, and weakened the inhibition of tyrosinase expression by hydrogen peroxide. The mechanism may be to prevent oxidative stress damage, and tyrosinase is effectively exported from endoplasmic reticulum (Guan et al., 2015). Different nanoparticles, such as transporter, solid lipid nanoparticles, nanostructured lipid carriers, liposomes, nano emulsions and polymer nanoparticles, maximize the ideal properties and/or therapeutic activity of quercetin (Nasr and Al-Karaki 2020), which provides a feasibility for the external treatment of vitiligo with quercetin.
Kaempferol
Kaempferol (Figure 3C) is a kind of flavonoids, which mainly comes from the rhizome of Kaempferia galanga L. (Liu Z. Q. et al., 2021). It widely exists in all kinds of fruits, vegetables and beverages, hazelnut, tea, propolis, broccoli and grapefruit (Calderón-Montaño et al., 2011). Kaempferol can be used to combat cardiovascular disease, cancer outbreak, immune dysfunction, diabetes, oxidative stress and other diseases (Imran et al., 2019). Kaempferol has no obvious cytotoxic effect on B16F10 cells at the concentration of 16–32 μm for 24 h (Wang et al., 2017). Kaliziri is an extract from Baccharoides anthelmintica (L.) Moench, which has showed relatively good therapeutic effects for vitiligo (Maimaiti et al., 2017). Kaempferol is one of the main active components of Baccharoides anthelmintica (L.) Moench extract (Tuerxuntayi et al., 2014). After treatment with 1, 5, 10 and 20 μm kaempferol for 7 days, melanin content in hmvii cells increased significantly. It enhanced tyrosinase activity in HMVII cells and mouse buccal hair follicles by inducing tyrosinase protein expression (Takekoshi et al., 2014). Based on the SDTNBI method and experimental verification, kaempferol markedly increased tyrosinase activity and melanin biosynthesis gene expression in B16F10 cells, and effectively promoted melanin synthesis (Wang et al., 2017).
Apigenin
Apigenin (4′, 5,7-trihydroxyflavone; (Figure 3D) natural plant flavone, widely exists in common fruits and vegetables. It is considered to be a flavonoid with biological activity (Liu et al., 2017). Compared with other flavonoids, apigenin is relatively non-toxic and non-mutagenic, and has significant effects on normal cells and cancer cells (Patel et al., 2007). It has demonstrated a variety of pharmacological effects, including antidepressant (Li et al., 2015; Zhang X. et al., 2019), anti-inflammatory, liver protection, antithrombotic, anticancer, anti-aging (Lim et al., 2015), anti-oxidant (Wang J. et al., 2020). Apigenin significantly increased the activities of glutathione peroxidase (GSH PX), catalase (CAT) and superoxide dismutase (SOD), in a dose-dependent manner, and significantly inhibited the level of malondialdehyde (MDA), a biomarker of oxidative stress, in a H2O2 induced cell line PIG3V. Interestingly, apigenin markedly increased protein expression levels of Nrf2 and its downstream NQO1 and HO-1 in a dose-dependent manner, but had no effect on Nrf2 knockout cells. The results showed that apigenin protects melanocytes from oxidative damage dependent Nrf2 pathway (Zhang et al., 2020). In the dopamine (DA)—induced melanocyte model, 10 μm apigenin treatment significantly reduced ROS aggregation, reduced Da induced melanocyte apoptosis, and inhibited caspase-3 and PARP activities, which may be involved in the anti-apoptotic effect of apigenin. The mechanisms include inhibition of JNK, p38MAPK and Akt (Lin M. et al., 2011). In vitro, HMVII cells were treated with apigenin at 1, 5, 10 and 20 μm for 7 days, and the melanin content increased significantly (Takekoshi et al., 2014). So far, there is little evidence that apigenin promote adverse metabolic reactions in vivo when ingesting nutrition related amounts (Shukla and Gupta 2010; Takekoshi et al., 2014; Weng et al., 2016). Apigenin's local drug delivery system transports apigenin to local skin tissue instead of penetrating into blood circulation (Li et al., 1996). Therefore, apigenin may be a relatively safe method for the treatment of vitiligo.
Galangin
Galangin (GA, 3,5,7-trihydroxyflavone; Figure 3E) is an important natural active flavone, which is mainly extracted from the roots of Alpinia officinarum Hance, it has long been used as herbs and spices in South Africa and Asia (Yang et al., 2018). GA has been reported to possess a variety of biological activities, including antibacterial (Skiba et al., 2016), antiviral, anti-inflammatory (Cushnie et al., 2007), anti-obesity (Ma et al., 2019) and antioxidant (Sinha et al., 2014), it is reported that these effects are exerted by regulating NF - κ B, Nrf2 and cAMP/CREB signaling pathways (Yang C.-C. et al., 2020). 4.25 mg/kg GA significantly increased the number of basal melanocytes and melanoepidermal cells in shaving area of mice with hydroquinone induced vitiligo, and promote the melanin hair follicles to increase, the mechanism is to prevent oxidative stress by reducing cholinesterase (CHE) activity and MDA content and increase the expression of TYR protein. Malondialdehyde (MDA) is the final product of lipid peroxidation, which is considered as a specific indicator of oxidative stress (Huo et al., 2014). However, GA metabolism is fast and its bioavailability is low. 90% of GA is metabolized in 1 h and is metabolized in 2 h in hepatocytes. Therefore, it is necessary to modify GA by methylation to slow down its metabolism and improve its bioavailability (Fang et al., 2019).
Naringenin and Hesperetin
Naringenin (Figure 2F) and hesperetin (Figure 3G) are two main flavonoids identified from Citrus × limon (L.) Osbeck extract (Singh et al., 2020). The flavonoids in sweet orange peel include flavonoid glycosides, flavones and flavonols, among which flavanones exist in the form of glycosides (hesperidin and naringenin) or aglycones (hesperidin and naringenin) (Ramful et al., 2010). Citrus flavonoids have many biological activities, such as anti-tumor, anti-oxidation and anti-inflammatory (Salehi et al., 2019). It was found that flavonoids from navel orange peel extract had antioxidant activity (Long et al., 2021). Citrus products stimulate cell melanin production and tyrosinase expression, thereby preventing skin damage caused by ultraviolet light (Chiang et al., 2011). Huang et al. (2012) used 20 μg/ml citrus extract for melanin synthesis experiment. Citrus are rich in hesperidin, neohesperidin or naringin, and acid hydrolytic extracts of these three species of Citrus promote melanin synthesis. In this experiment, 50 μm hesperetin increased the expression of β-catenin, induced the rapid phosphorylation of p38MAPK, ERK and Akt, and activated the downstream transcription factor CREB phosphorylation in less than 1 h. Hesperidin stimulates melanogenesis by activating CREB and MAPKs in Wnt/β-catenin pathway (Huang et al., 2012). Naringenin enhanced tyrosinase activity of B16 mouse melanocytes in a time-dependent manner and increased melanin content in a concentration dependent manner, reaching the maximum at 100 μM. The mechanism included increasing the expression level of melanin producing enzyme (TYRP1 and DCT) and MITF (Ohguchi et al., 2006). Another study also confirmed that naringenin up-regulated tyrosinase activity of B16-F10 cells in a concentration dependent manner. Naringenin up regulated the expression of MITF by increasing the expression of β-catenin and the phosphorylation of Akt or GSK3, and then increased the activity of tyrosinase, so as to improve the melanin synthesis of B16-F10 cells, rather than through cAMP pathway (Huang et al., 2011). These results suggest that hesperetin induced melanogenesis in cell models may contribute to the development of topical beauty agents.
Afzelin
Afzelin (3-O-α-l-rhamnopyranoside; Figure 3H) is a flavonoid isolated from Thesium chinense Turcz. and widely distributed in Korea and China (Li G.-H. et al., 2021). Previous studies have shown that afzelin has antibacterial, anticancer and anti-inflammatory effects (Satthakarn et al., 2015). Afzelin markedly alleviated ultraviolet induced oxidative stress in human skin, damage of mitochondrial membrane potential and mitochondrial permeability (Shin et al., 2013). Afzelin showed strong anti-oxidant activity in DPPH radical scavenging experiment (Kim et al., 2008). Many studies have shown that afzelin could effectively treat skin diseases (Lee et al., 2014). In the experiment of melanogenesis induced by afzelin in human epidermal melanocytes, 100 μm afzelin increased the protein levels of TRP-1 and TYR by up regulating MITF, but did not increase the protein levels of TRP-2. The mechanism is p38MAPK phosphorylation, which up regulates MITF, and is independent of cAMP/PKA pathway (Jung et al., 2016).
Fisetin
Fisetin (3,30,40,7-tetrahydroxyflavone; Figure 3I) is a dietary flavone, which exists in a variety of vegetables and fruits, including apples, strawberries, grapes, cucumbers and onions (Khan et al., 2018). Studies have found that fisetin has anti allergic, anti-arthritis and neuroprotective effects (Ahmad et al., 2017; Ahmad et al., 2019). New data also showed that fisetin had anti-cancer activity (Jie et al., 2015; Khan and Mukhtar 2015; Ding et al., 2020). In particular, it has recently been found that it inhibited inflammation and antioxidant stress (Silva et al., 2007; Ahmad et al., 2019). Interestingly, fisetin has a two-way regulatory effect on melanin production. Takekoshi et al. first reported that fisetin could promote Tyr activity and melanin content of human melanoma cells (Takekoshi et al., 2014). However, Shon et al. found that fisetin inhibited the melanin content in and out of mouse B16F10 melanoma cells mediated by α - MSH(Shon et al., 2016). A recent study found that the difference of dual effects of fisetin was related to its concentration, because high concentration of fisetin inhibited the synthesis of melanin in zebrafish larvae (400 μm) and B16F10 melanoma cells (40 μm). When the concentration of fisetin exceeded 25 μm, the inhibitory activity increased slightly, and 200 μ m had the highest inhibitory rate on mushroom tyrosinase activity in vitro. Surprisingly, 5 μm fisetin slightly increased the content of spontaneous melanin and extracellular melanin, fisetin (at 20 μm) markedly increased the content and release of melanin in B16F10 cells by up regulating the expression of TYR and MITF, and promoted the melanin synthesis of zebrafish larvae. The mechanism is that fistein inhibits GSK-3 β, which activates β - Catenin, which leads to melanogenesis by activating MITF and tyrosinase (Molagoda et al., 2020). Therefore, low dose of fisetin may be an effective drug in the treatment of vitiligo.
Puerarin
Puerarin (7,40-dihydroxyisoflavone-8b-glucopyranoside; Figure 3J) is an isoflavonoid derivative isolated from the root of the traditional Chinese medicine Pueraria lobata (Willd.) Ohwi (Zhang 2019). Puerarin exhibits a wide range of antioxidant activities in cardiovascular diseases, diabetes, obesity, osteoporosis, and other diseases (Xu et al., 2021; Chang et al., 2021; Liu Y. et al., 2021; Xiao et al., 2020). In addition, puerarin has anti-inflammatory, anti-viral and other pharmacological activities (Wang Z.-K. et al., 2020; Wang H. X. et al., 2021). Puerarin exhibited obvious pharmacological activities against vitiligo in vitro and in vivo. Park et al. found that puerarin could increase the melanin content of melanocytes in vitro, and topical application could improve the melanin content of mouse skin tissue, the mechanism is via activation of the cAMP pathway, followed by elevation of MITF, tyrosinase, Trp-2, and Bcl-2 to increase melanocyte survival and melanin content (Park et al., 2014). In the 4-benzyloxyphenol-induced vitiligo mouse model, after one week of Puerarin Treatment, HE staining of the skin at the depigmented sites showed increased hair follicles, which were surrounded by a large number of melanocytes. Puerarin at 40 μmol/L significantly increased the melanin content of human melanocytes by decreasing the phosphorylation of ERK in the cells to promote TRP-1 and MITF expression, which led to an increase in melanin content (Ding et al., 2019).
Butin
Butin (7, 30, 40-trihydroxydihydroflavone, BUT; (Figure 3K) flavonoid with antioxidant activity, isolated from Alpinia officinarum Hance, Dalbergia odorifera T.C.Chen (Duan et al., 2017). BUT exhibited a wide range of pharmacological activities for the treatment of aging, diabetes, liver diseases, and cancer (Zhang et al., 2011). In the hydroquinone-induced vitiligo mouse model, (4.25, 42.5 mg/kg) butin increased the melanin content in the skin lesions by increasing the expression of Tyr and TRP-1 protein, reducing the serum cholinesterase activity and malondialdehyde content. Besides, BUT promoted the proliferation of basal melanocytes (Huo et al., 2017). A recent study found that butin induced melanin production both in vivo and in vitro when the concentration was 40 μmol/L, while tyrosinase activity peaked. Meanwhile, in a H2O2-induced zebrafish model, butin reduced the levels of reactive oxygen species in vivo (Lai et al., 2021).
Liquiritin and Liquiritigenin
Liquiritigenin (LQ; Figure 3L) and liquiritigenin (LQG; Figure 3M) are flavonoids extracted from Glycyrrhiza uralensis Fisch. ex DC. (Du et al., 2021; Mou et al., 2021). They have many biological activities, such as antiviral, anti-inflammatory, anti-oxidation, anti-tumor and so on (Pastorino et al., 2018). LQ and LQG were used to treat mouse melanoma B16-F1 cells and human melanoma hmvii cells with different doses for 72 h. The results showed that both natural drugs significantly increased the content of melanin in melanocytes in a dose-dependent manner, and had no effect on cell viability. Interestingly, both LQ and LQG could significantly up regulate tyrosinase activity and the expression of MITF and its downstream TRP-1 and Trp-2. Further studies have found that 50 μm LQ and LQG trigger melanin synthesis through p38 phosphorylation and activation of PKA/CREB signaling pathway (Uto et al., 2019).
Vitexin
Vitexin (apigenin-8-C-β-D-glucopyranoside; Figure 3N) is a natural flavonoid present in various medicinal plants such as: Crataegus L., Vigna Savi, Passiflora cristalina Vanderpl. & Zappi, Mimosa L., bamboo, etc (He et al., 2016). It has many pharmacological activities, anti-inflammatory, antiviral, anticancer, antihypertensive (Ding et al., 2021; Chen Y. et al., 2021). At the same time, Vitexin is an antioxidant (Ożarowski and Karpiński 2020). In H2O2-induced human melanocyte PIG1, Vitexin inhibited hydrogen peroxide induced apoptosis and promoted cell proliferation by activating the MAPK-Nrf2/ARE pathway, including decreasing IL-1β. The expression of IL-17A, Bax, caspase-3 and ROS, up-regulated the expression of p53, Bcl-2, Nrf2, HO-1, NQO-1, SOD (Li et al., 2020).
Hyperoside
Hyperoside (quercetin-3-O-galactoside, Hyp; Figure 3O) belongs to flavonol glycosides isolated from Rhododendron brachycarpum D. Don ex g. don, Abelmoschus manihot (L.) Medik. Rhododendron L.(Zhou et al., 2021). Studies have shown that Hyp possesses antioxidant, anticancer, antifibrotic, antiallergic, anti-inflammatory and other pharmacological activities (Huang et al., 2020). Hyperoside markly increased the proliferation of melanocytes in a dose - and time-dependent manner in vitro. In the H2O2-induced melanocyte model, Hyp protected melanocytes from oxidative damage by regulating the PI3K/Akt pathway, inhibiting p38 phosphorylation and suppressing mitochondrial apoptotic signaling, which included upregulation of the Bcl-2/Bax ratio and expression of Akt, and downregulation of caspase 3, p38 (Yang et al., 2016).
Baicalin
Baicalin (7-glucuronic acid-5,6-dihydroxy-flavone, BA; Figure 3P) is a kind of small molecular flavonoids extracted from Scutellaria baicalensis Georgi (Fan et al., 2021). BA has a variety of pharmacological activities, such as antioxidant stress, regulation of immunity, regulation of lipid metabolism disorders, anti-inflammatory and improve cell apoptosis (Xin et al., 2020). Recent studies have found that baicalin mediates antioxidant stress by activating Nrf2 signaling pathway (Wang X. et al., 2021). In the 40% monobenzone cream-induced vitiligo model, BA intraperitoneal injection inhibited the infiltration of leukocytes and CD8 + T cells in vitiligo lesions, increased the tyrosinase activity in the lesion area, reduced the expression of chemokine CXCL10 and its receptor CXCR3, and reduced the expression of inflammatory factors in serum samples, including IL-6 and TNF- α, IFN- γ And IL-13 (Zhu et al., 2019). The results of this study are obviously exciting. The infiltration of active CD8 + T cells occurs around the lesions of vitiligo, which is an important reason for the immune destruction of melanocytes (Wu et al., 2013). In vivo experiments, BA could inhibit the infiltration of immune T cells, remove inflammatory factors to slow down the appearance of leukoplakia, and reduce the area of decolorized spots. So it is a potential drug for the treatment of vitiligo.
Polyphenol
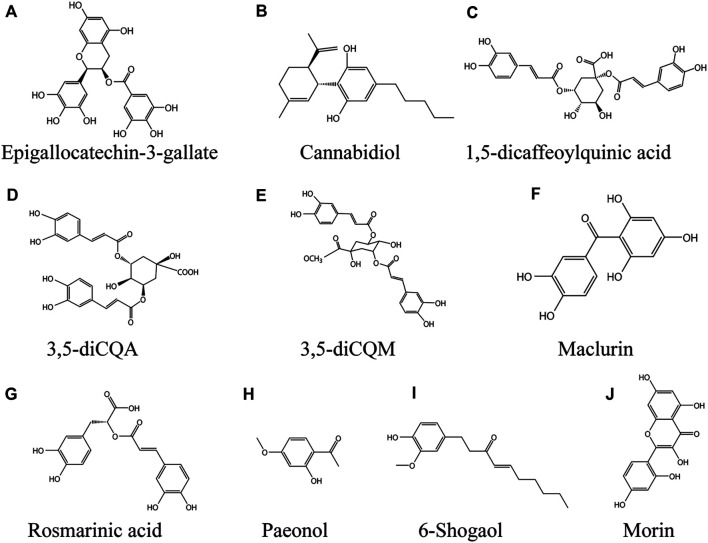
Epigallocatechin-3-Gallate
Epigallocatechin-3-gallate (EGCG, Figure 4A) belongs to catechin polyphenols and is one of the main bioactive substances in Camellia sinensis (L.) Kuntze (Huang et al., 2021). It has many pharmacological effects, including anti-inflammatory, anti-atherosclerotic and anti-cancer effects (Mereles and Hunstein 2011), it's also an antioxidant (Kalaiselvi et al., 2013). Katiyar et al. suggested that EGCG could be a topical preparation to resist UVB-induced ROS-related inflammatory skin diseases, photocarcinogenesis and photoaging (Katiyar et al., 1999). In a model of monobenzone-stimulated vitiligo in mice, EGCG delayed the time to depigmentation, the area of depigmentation and reduced the incidence of hyperpigmentation in the dorsal skin of mice. The underlying mechanism was the inhibition of CD8 + T cell migration and inflammatory cytokine expression. Meanwhile, EGCG decreased the expression of IFN-γ, TNF-α, and IL-6 in serum. 5%EGCG cream is the optimal concentration for the treatment of vitiligo (Zhu et al., 2014). IFN - γ, which plays a key role in vitiligo pathogenesis, feedback through crosstalk to promote CD8 + T cell recruitment to the skin (Harris et al., 2012). High levels of CXC chemokines induced by IFN - γ such as CXCL9, CXCL10 and CXCL11 were also found in patient serum, being the most highly expressed genes in the transcriptional profile of skin lesions from vitiligo patients (Rashighi et al., 2014). Excitingly, EGCG inhibited IFN - γ - induced phosphorylation activation of JAK2, STAT1 and STAT3 in human melanocytes and significantly suppressed the levels of ICAM-1, CXCL10 and MCP-1 in a dose-dependent manner. In primary cultured human melanocytes. EGCG reduced the expression of CXCR3, CCR2, and CD11a in purified CD8 + T cells derived from the CD4 + T leukemia cell line Jurkat and peripheral blood monoclonal cells (PBMCs) in a dose-dependent character (Ning et al., 2015).
FIGURE 4.
Phenolic compounds against vitiligo (A) EGCG, (B) Cannabidiol, (C) 1,5-dicQA, (D) 3,5-diCQA, (E) 3,5-diCQM, (F) Maclurin, (G) Rosmarinic acid, (H) Paeonol, (I) 6-Shogaol, (J) Morin.
Cannabidiol
Cannabinediol (CBD; (Figure 4B) non-psychoactive compound extracted from Cannabis sativa L., is an open pyran ring analogue. CBD has anti-inflammatory, antioxidant and anti-apoptotic effects (Iuvone et al., 2009). In addition, it has immunomodulatory properties (Mechoulam and Hanus 2002). In recent years, it has attracted great attention due to its potential in the treatment of various pathological diseases, including skin and cosmetic diseases (Baswan et al., 2020). CBD increaseed melanin content by binding to CB1 receptor of human epidermal melanocytes. The mechanism is to up regulate the expression of MITF by activating p42/44MAPK and p38MAPK signaling pathways, and then promote melanogenesis (Hwang et al., 2017). The safety of CBD transdermal drug delivery system is also under development (Paudel et al., 2010).
1,5-Dicaffeoylquinic Acid
1,5-dicaffeoylquinic acid (1,5-dicQA; Figure 4C) is a natural polyphenol widely found in Baccharoides anthelmintica (L.) Moench and Helianthus annuus L. (Cheevarungnapakul et al., 2019; Dogra et al., 2020). 1, 5-diCQA has a wide range of pharmacological effects, such as antioxidant, neuroprotective, antifibrotic and other biological activities (Cao et al., 2010). Plant seeds containing 1, 5-diCQA are used in traditional medicine to treat vitiligo (Tuerxuntayi et al., 2014). A previous study found that 1,5-dicqa exerts antioxidant activity through reducing intracellular ROS level and Nrf2 dependent pathway (Cao et al., 2010). 1, 5-diCQA inhibited Aβ42-induced neurotoxicity by activating PI3K/Akt, decreasing GSK3 β level and regulating Bcl-2/Bax ratio (Xiao et al., 2011). B16 cells treated with 0, 5, 50 or 100 μM 1, 5-dicQA significantly up-regulated the transcription levels of MITF, TYR, TRP1 and TRP2 in a dose-dependent manner without cytotoxicity. The mechanism is to activate p38 MAPK, ERK MAPK and PKA signaling pathway to promote the melanin synthesis of B16 cells. In conclusion, these studies suggest that 1,5-dicQA may be an effective drug for the treatment of hypopigmented skin diseases (Mamat et al., 2018).
3,5-diCQA
3,5-caffeoylquinic acid (3,5-diCQA; Figure 4D) is a polyphenolic compound extracted from the root of Cichorium intybus L. (Legrand et al., 2016), it also accumulated in Achillea millefolium L. and Artemisia dracunculus L. 3,5-diCQA has high free radical scavenging activity (Bernard et al., 2020). Phenolic compounds are beneficial to human health, especially their anti-inflammatory and antioxidant properties (Miguel et al., 2020). Plant polyphenols help the skin resist the damage caused by sunlight (Perez-Sanchez et al., 2016). 3,5-diCQA increased the content of melanin in melanocytes in a dose-dependent manner, the possible mechanism is that 3,5-diCQA promoted the phosphorylation of Akt and GSK-3 β, leading to the accumulation of β - Catenin in the cytoplasm. Subsequently, β - Catenin transferred to the nucleus and bound to LEF, which increased the protein expression of downstream MITF, TYR, TRP1 and TRP2. Therefore, 3,5-diCQA may restore skin pigmentation under the loss of antioxidant enzymes or melanocyte dysfunction (Mamat et al., 2017).
3,5-diCQM
3,5-dicaffeoylquinic acids (3,5-diCQM; Figure 4E) is a sort of natural phenolic acids condensed from quinic acid and caffeic acid by esterification. It is widely found in plants such as Gloriosa superba L., Inula helenium L., Xanthium strumarium subsp. strumarium, Crataegus azarolus L. and other fruit trees (Bernard et al., 2020). Caffeoylquinic acid derivatives have been used in traditional medicine in the east to treat a variety of diseases and show a diversity of pharmacological effects, such as liver protection (Basnet et al., 1996), anti-microbial (Zhu et al., 2004), anti-inflammatory (Góngora et al., 2002). In addition, the antioxidant activity of caffeoylquinic acid derivatives has been reported (Lin Y.-L. et al., 2011; Jang and Koh 2019). In the experiment of B16F10 melanoma cells treated with 0–50 μm 3, 5-dicCQM, the results showed that 3,5-diCQM could induce pigmentation. 3,5-diCQM drives melanogenesis in a dose-dependent manner, and the molecular mechanism underlying its ability to induce pigmentation is through activation of the p38 signaling pathway, phosphorylation and activation of CREB, and a cAMP/PKA dependent signaling pathway, which in turn upregulates the transcription factor MITF, thereby activating tyrosinase activity (Kim et al., 2015).
Maclurin
Maclurin [(3,4-dihydroxyphenyl) -(2,4,6-trihydroxyphenyl; Figure 4F) methanone] is a natural phenolic compound that belongs to the benzophenone family and is found in Morus alba L., Garcinia mangostana L. Previous studies have found that maclurin has pharmacological activities such as anticancer, antioxidant and anti-skin aging (Lee 2018; Lee et al., 2018; Mi Moon et al., 2019). The content of melanin in melanocytes was increased by maclurin in a dose-dependent manner, by a mechanism involving the activation of the cAMP/PKA/CREB signaling pathway, which in turn increased tyrosinase, MITF and their downstream TRP-1 and Trp-2 protein content, while also involving the activation of p38 MAPK and p44/42 MAPK pathways. In vitro, maclurin significantly attenuated UVB induced ROS production, inhibited hydrogen peroxide induced reduction of melanin and decreased cell survival (Hwang et al., 2019).
Rosmarinic Acid
Rosmarinic acid (a-o-caffeoyl-3,4-dihydroxyphenyl lacticacid; Figure 4G) is a natural phenolic compound, which exists in many Labiatae plants, such as Perilla L., Rosmarinus officinalis L., Prunella vulgaris L. (Zhang et al., 2021). Rosmarinic acid has anti-inflammatory, anti-oxidation, anti-cancer and other pharmacological activities (Wang L. et al., 2019; Zhang et al., 2021). Incubation of 50 μm rosmarinic acid with B16 melanoma cells for 48 h resulted in a significant increase in melanin content and tyrosinase protein expression, the mechanism being that rosmarinic acid induces melanin synthesis by activating the PKA/CREB signaling pathway via phosphorylation (Shomirzoeva et al., 2019). Recently, ultradeformable liposomes (UL) have been developed by scientific researchers, which greatly increased the skin permeation ability of rosmarinic acid by UL containing oleic acid, exhibiting potential as a formulation for development for external use (Subongkot et al., 2021).
Paeonol
Paeonol (Pae; 2′-hydroxy-4-methoxyacetophenone; Figure 4H) is a natural phenolic compound extracted from the Paeonia × suffruticosa Andrews (Miao et al., 2021). Paeonol has been used in traditional Chinese medicine as an anti-inflammatory and antipyretic drug with cardiovascular, anti-inflammatory, neuroprotective, antitumour and other pharmacological activities (Zhang L. et al., 2019; Tsai et al., 2020). Paeonol alleviated UVB-induced skin photoaging by activating Nrf2 and the antioxidant response element (Sun et al., 2018). Paeonol exhibits anti-inflammatory, anti-allergic activity in animal models of atopic dermatitis and psoriasis (Meng et al., 2017; Meng et al., 2019). In H2O2-induced PIG1 oxidative stress model of normal human epidermal melanocytes, paeonol inhibited hydrogen peroxide induced decrease in cell viability in a dose-dependent manner. 20 μM paeonol increased the enzymatic activities of SOD, CAT, GSH-Px and the expression of HO-1, NQO1, and SOD2 by activating the Nrf2 signaling pathway, but paeonol was unable to affect melanogenesis in PIG1 cells and acted only as a protective agent (Guo and Zhang 2021).
6-Shogaol
6-shogaol (Figure 4I), a natural phenolic compound, is the major active ingredient in Zingiber officinale Roscoe. Studies have found that 6-shogao possesses antiemetic, anti-inflammatory, antioxidant, and anticancer activities, as well as cardiovascular and neuroprotective effects (Kou et al., 2018; Chen et al., 2020; Yadav and Jang 2020). Jin et al. found that 6-shogaol exerts cellular antioxidant activity by mediating Nrf2 signaling through activation of the JNK pathway (Kim and Jang 2016). Feng et al. found that 6-shogaol inhibited UVB induced inflammation and oxidative stress in keratinocytes (Chen F. et al., 2019). Pretreatment of HEMn-MPs with 5 µM 6-shogaol for 6 h protected melanocytes from rhododendrol-induced cytotoxicity and maintained their original cell viability. In the oxidative stress-induced HEMn-MPs model, cells pretreated with 6-shogao maintained the initial cellular morphology, and 6-shogao significantly attenuated H2O2 induced oxidative stress and death and melanogenesis inhibition in melanocytes (Yang L. et al., 2020).
Morin
Morin (2′,3,4′,5,7-pentahydroxyflavone; Figure 4J) is a natural polyphenol found in onion, fig, guava leaves, apple and other Moraceae families such as Psidium guajava L., Maclura pomifera (Raf.) C.K.Schneid., as well as the medicinal plant Alpinia officinarum Hance (Lotito and Frei 2006). Studies have found that Morin has antitumor, antihypertensive, antioxidant, anti-inflammatory, antidiabetic, neuroprotective, antibacterial and other pharmacological effects (Caselli et al., 2016; Heeba et al., 2021). 50 μM Morin significantly upregulated the expression of MITF, as well as its downstream TRP-1 and Trp-2 to increase melanin production in B16F10 mouse melanoma cells, and the mechanisms include the activation of ERK and p38 signaling pathways via the phosphorylated MAPK pathway (Shin et al., 2021). Excitingly, long-term doses of oral Morin did not exhibit any toxicity (Cho et al., 2006).
Glycosides
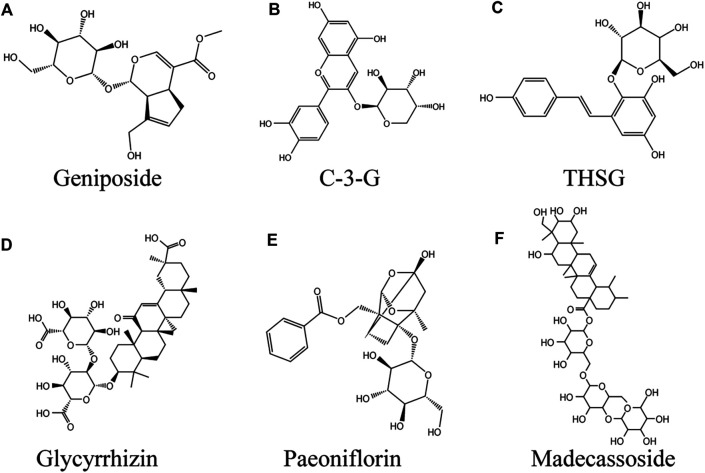
Geniposide
Geniposide (GP; Figure 5A) (C17H24O10) is a sort of iridoid glycoside extracted from Gardenia jasminoides J. Ellis fruits, which widely exists in nearly 40 species of plants in various families, especially Rubiaceae (Shan et al., 2017). In terms of biological activity, GP has been found to have a variety of pharmacological effects, such as anti-diabetes (Zhang et al., 2016), neuroprotective (Zhao et al., 2017), anti-inflammatory, antioxidant, etc (Zhou et al., 2019). GP is also an important component in many traditional Chinese herbal medicines for the treatment of vitiligo, such as Eucommia ulmoides Oliv. and Rehmannia glutinosa (Gaertn.) DC. (Zhou et al., 2019). In HEMn or HEKn models induced by norepinephrine (NE), GP significantly abolished the inhibitory effect of NE on HEMn melanogenesis in the presence of recombinant SCF. The binding of NE to α 1-adrenoceptor in melanocytes decreased cAMP level, resulting in decreased intracellular calcium uptake associated with c-kit production. The mechanism of GP promoting melanogenesis was through activating GLP-1R/c-kit receptor signal to enhance the expression of c-kit receptor, so as to eliminate the depigmentation caused by norepinephrine (Wen-Jun et al., 2008). In the melanocytes induced by H2O2, GP increased the activities of SOD and CAT, reduced the accumulation of ROS, thus increased the antioxidant capacity of melanocytes and inhibited melanocyte apoptosis by upregulating the Bcl-2/Bax ratio, while increasing cell viability. This process involves activation of PI3K/Akt signaling pathway (Zhou et al., 2019).
FIGURE 5.
Glycosides against vitiligo (A) Geniposide, (B) C-3-G, (C) THSG, (D) Glycyrrhizin, (E) Paeoniflorin, (F) Madecassoside.
Cyanidin-3-o-β-Glucopyranoside
Cyanidin-3-o-β-glucopyranoside (C-3-G; Figure 5B) is a kind of anthocyanin flavonoids widely found in vegetables and fruits. Chinese Myrica cerifera L. is a rich source of C-3-G, which is one of the most common anthocyanins (Sun et al., 2013). Anthocyanins are beneficial to human body. Known pharmacological actions include anti-inflammatory, anti-fatigue, anti-oxidation, anti-tumor and so on (Cui et al., 2018). In addition to the ability to significantly reduce ROS mediated oxidative damage, C-3-G inhibited UVA induced damage to primary human dermal fibroblasts (HDFS) by inducing autophagy (Wu et al., 2019). In one study, TVM-A12 human melanoma cells were incubated with 5 μm C-3-G, and the cells return to the differentiation state from the proliferation state. In addition, two human melanoma cell lines A-375 and M14 also obtained dendritic phenotypes after C-3-G treatment. At the concentration used, the cells treated with C-3-G showed no apoptosis or necrosis. At the same time, C-3-G significantly up-regulated the expression of tyrosinase, thereby inducing the content of melanin in TVM-A12 cells, which was mediated by up regulating cAMP pathway. It is particularly encouraging that the active concentration of C-3-G is comparable to food intake (range of μm) and has no toxicity. (Serafino et al., 2004).
2, 3, 5, 4′-Tetrahydroxystilbene-2-O-β-D-Glucoside
2, 3, 5, 4′-tetrahydroxystilbene-2-O-β-D-glucoside (THSG; Figure 5C) is a water-soluble active ingredient in Reynoutria multiflora (Thunb.) Moldenke (He et al., 2015). Numerous studies have found that THSG exerts antioxidant effects by protecting cells from oxidative damage caused by H2O2 through increasing SOD activity, reducing MDA content, and inhibiting ROS production (Yang et al., 2014; Wu et al., 2020). In hairless skin model, the extract of Reynoutria multiflora could up regulate SOD in a dose-dependent manner, thereby reducing UVB-induced oxidative damage, suggesting that the extract of Reynoutria multiflora contains anti skin photoaging agent (Hwang et al., 2006). At the first time, it was proved to be an effective tyramine Acid enzyme activators and melanogenesis stimulants (Guan et al., 2008). THSG increased tyrosinase activity in a dose-dependent manner at concentrations ranging from 1 to 10 μg/ml (Jiang et al., 2009). Guan et al. (2008) reached a similar conclusion. The mechanism was that THSG directly activated AC or inhibited PDE, increased cAMP level in cytoplasm, and mediated the activation of MITF/CREB. P38MAPK had a regulatory effect on melanin formation and the induced expression of tyrosinase and MITF in B16 cells induced by THSG (Jiang et al., 2009).
Glycyrrhizin
Glycyrrhizin (GLC; (Figure 5D) natural triterpene saponin, is one of the major chemical components extracted from Glycyrrhiza Tourn. ex L. and has been widely used in Asia, Europe, the Middle East (Cai et al., 2017). Studies have shown that GLC has antiallergic, immunomodulatory, antiulcer, anticancer, antioxidant, and antiviral effects (Wang G. et al., 2021). Jung et al. were the first to find that GLC induced melanin production in B16 melanoma cells in a dose-dependent manner by upregulating the tyrosinase and Trp-2 genes (Jung et al., 2001). Li et al. also verified this conclusion. Further studies revealed that GLC increases melanin production in melanocytes by three pathways, 1) activating activator protein-1 (AP-1) and CRE promoter to activate p42/44 MAPK signaling, 2) activating cAMP signaling, and 3) decreasing GSK3β phosphorylation while inducing CREB phosphorylation (Lee et al., 2005). Pretreatment with 1 mM GLC significantly inhibited H2O2-induced melanocyte apoptosis, and GR protected melanocytes from oxidative stress by reducing ROS production in cells via activation of the Nrf2/HO-1 pathway (Mou et al., 2019). Clinical study observations suggest that treatment with oral GLC in combination with UVB improves active generalized vitiligo (Mou et al., 2016).
Paeoniflorin
Paeoniflorin (C23H28O11, PF; (Figure 5E) monoterpene glycoside, is a major active ingredient isolated from the roots of Paeonia veitchii Lynch or Paeonia lactiflora Pall., which has been applied for 1,200 years in China (Li J. et al., 2021). In vivo and in vitro, paeoniflorin has a wide range of pharmacological activities, including anti-inflammatory, antioxidant, immunomodulatory, analgesic, anticonvulsant, antithrombotic, neuroprotective, cardioprotective, hepatoprotective, antitumor and antidepressant effects (Zhou Y.-X. et al., 2020). In the 40% monobenzone-induced vitiligo mouse model, the number of hair follicles and melanin content in the skin of paeoniflorin treated for 10 days were significantly higher than those of the model group. In vitro, 10 μg/ml paeoniflorin can stimulate the synthesis of melanin, and its mechanism is to increase the protein level of MITF and its downstream TRP-1 by promoting the phosphorylation of ERK and CREB (Hu M. et al., 2020). Interestingly, PF protected H2O2-induced PIG1 and PIG3V cells from oxidative stress by activating JNK/Nrf2/HO-1 signaling pathway, including decreased ROS level and increased SOD, CAT, Nrf2 and HO-1 expression. PF at a concentration of 50 μM, the cell viability was significantly increased (Yuan et al., 2020).
Cistanche deserticola Polysaccharide
Cistanche deserticola polysaccharide (CDP) is the main active component isolated from Cistanche deserticola Ma. It is widely used in anti-virus and anti-tumor in North Africa, Arab and Asian countries (Gu et al., 2016). In addition, CDP also has the pharmacological activities of liver injury protection, lipid balance, anti-aging, regulating immune function and antioxidant (Liu et al., 2018). CDP promoted the formation of melanin in vivo and in vitro. CDP promoted melanogenesis by activating MAPK signaling pathway and up regulating the expression of MITF and its downstream genes Tyr, TRP1 and Trp2, including increasing the phosphorylation levels of p38, JNK and ERK proteins. In vivo, CDP promotes melanin production in zebrafish. Notably, CDP protected HEM and B16F10 cells from oxidative stress induced by H2O2 and significantly inhibited apoptosis induced by oxidative stress (Hu Y. et al., 2020).
Madecassoside
Madecassoside (MADE; (Figure 5F) natural triterpenoid saponin, is isolated from Centella asiatica (L.) Urb (Zhou J. et al., 2020). Studies have found that asiatic acid has a wide range of pharmacological activities, such as anti-apoptotic, anti-inflammatory, and anti-oxidative (Peng et al., 2020). In the H2O2-induced oxidative stress model, MADE reduced the shrinkage of dendrites of melanocytes affected by oxidative stress in a dose-dependent manner, maintained cell morphology, improved mitochondrial swelling, and exerted antioxidant activity by increasing autophagy by upregulating the levels of LC3-II and LC3-I in melanocytes. Therefore, MADE is a promising natural product against vitiligo (Ling et al., 2017).
Coumarin
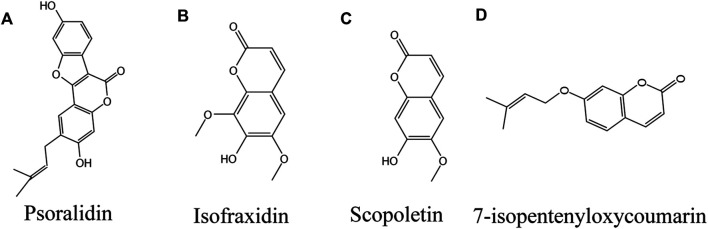
Psoralidin
Psoralidin (PL; Figure 6A), a natural coumarin isolated from Cullen corylifolium (L.) Medik. seeds, is structurally similar to coumestrol (Cao et al., 2019). It also exists naturally in various plants, such as lemon, lime and parsnip divaricata. PL is beneficial to diabetic complications, oxidative stress, obesity, osteoporosis, apoptosis, autophagy and cell proliferation (Sharifi-Rad et al., 2020). PL is used in the traditional Uyghur medicinal materials for color restoration (Wang et al., 2014; Niu et al., 2016; Pei et al., 2016), and several psoralen compounds, such as 8-MOP and 5-MOP, isolated from the same plant (Zang et al., 2019), are used in ultraviolet color restoration therapy (Dincer Rota et al., 2021). In vitro experiments showed that PL could improve the activity of tyrosinase (Shi et al., 2018). A recent clinical controlled study found that treatment of vitiligo lesions with psoralen in combination with NBUVB had higher efficacy compared with NBUVB alone, and there were no serious complications (Zabolinejad et al., 2020). The mechanism may provide an antioxidant effect by regulating the PI3K/Akt signaling pathway, affecting the downstream GSK3 β/β - Catenin, and the Nrf2/HO-1 axis (Zhai et al., 2018).
FIGURE 6.
Coumarins against vitiligo (A) Psoralidin, (B) Isofraxidin, (C) Scopoletin, (D) 7-isopentenyloxycoumarin.
Isofraxidin
Isofraxidin (Figure 6B) is a natural coumarin isolated from Artemisia capillaris Thunb. (Yim et al., 2017b). Isofraxidin related derivatives have been found to have anti-inflammatory, antioxidant, neuroprotective and other biological activities (Lau et al., 2019; Majnooni et al., 2020). Yim et al. emphasized that isofraxidin may be a new type of pigmentation agent. At the dose of 12.5 μm and 25 μm, zebrafish treated with isofraxidin showed higher melanin synthesis and tyrosinase activity in vivo experiments. In vitro, 25 μm isofraxidin significantly increased the melanin content in B16F10 cells by up regulating MITF and tyrosinase gene expression (Yim et al., 2017a).
Scopoletin
Scopoletin (SP; Figure 6C) is a phenolic coumarin isolated from Evolvulus alsinoides (L.) L., which has many pharmacological effects (Zhang F. et al., 2019). It has been isolated from Gramineae, Liliaceae, Musaceae, Compositae, Convolvulaceae and Leguminosae (Tal and Robeson 1986; Gnonlonfin et al., 2011). SP has been reported to have anti-inflammatory effect (Chaingam et al., 2020) and antioxidant effect (Usman et al., 2020), When B16F10 melanoma cells were treated with 0–50 μm SP, it was found that SP to induce melanin synthesis in a dose-dependent manner by increasing the expression of MITF and tyrosinase via increasing CREB phosphorylation (Ahn et al., 2014). When zebrafish embryos were exposed to the compound for 2 days, the increase of pigment was detected. In vitro, SP at concentrations of 0–50 μmol/L enhanced melanogenesis in vivo and in vitro by increasing melanin content and Tyr and MITF expression (Heriniaina et al., 2018).
7-Isopentenyloxycoumarin
7-isopentenoxycoumarin (Figure 6D), a natural pentenoxyumbelliferone derivative widely found in Rutaceae and umbelliferaceae, is a floral extract of Amaranthus retroflexus L., which is used as a food product in southern and central Italy (Fiorito et al., 2017). Studies have shown that 7-isopentenyloxycoumarins have antifungal, antioxidant, anticancer, neuroprotective, and anti-inflammatory properties (Preziuso et al., 2020). Fiorito et al. found that 7-isopentenoxycoumarin significantly induced melanogenesis at a dose of 40 μm, with the highest induction of melanin at 72 h, and excitingly the induction was 6-fold greater than that of the control group, and the mechanism of action was to increase melanogenesis by elevating MITF and its downstream genes tyrosinases, TRP-1 and Trp-2. Interestingly, 7-isopentenoxycoumarin interacted with the ERβ (ER-β) Binding may also be involved in melanin biosynthesis, as this receptor antagonist inhibited melanogenesis (Fiorito et al., 2018).
Other Compounds
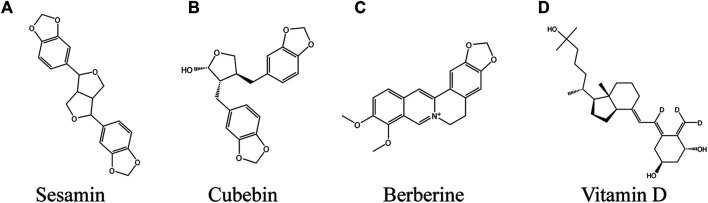
Sesamin
Sesamin (Figure 7A), a kind of lignan found in oil and Sesamum indicum L. seed, has been found to have a variety of biological activities and is beneficial to human body (Udomruk et al., 2020). The high antioxidant activity of sesamin has been reported (Pathak et al., 2014). In addition, its anti-nociceptive and anti-inflammatory activity was also reported (Jeng et al., 2005; Monteiro et al., 2014). It increased the content of tocotrienoll in the skin, so as to reduce sunburn and tumor incidence rate (Yamada et al., 2008), reduced the skin erythema caused by UVB, improved skin inflammation, protected skin from wrinkle formation and light damage (Lin et al., 2019). In the concentration range of 1–10 μM, sesamin increased melanin production in a dose-dependent manner. The mechanism is that sesamin up regulated CREB gene by activating cAMP/PKA signaling pathway, then up regulated the expression of tyrosinase and MITF, and finally induced melanin synthesis (Jiang et al., 2011). The currently developed transdermal drug delivery system will successfully transform lignin into an external preparation for the treatment of vitiligo in the future (Nguyen et al., 2015).
FIGURE 7.
Coumarins against vitiligo (A) Sesamin, (B) Cubebin, (C) Berberine, (D) Vitamin D.
TABLE 1.
Summary of natural products for the treatment of vitiligo in models.
| Natural compounds name | Models | Range of dosage | Targets/pathway/process/mechanism | References | |
|---|---|---|---|---|---|
| Flavonoids | Baicalein | H2O2-induced PIG3V (human cell) | 50 µM | Cell vitality and proliferation, Nrf2, HO-1, SOD2, NQO1, ERK1/2, PI3K/AKT | Ma et al. (2018) |
| H2O2-induced PIG1 (human cell) | 10, 20, and 40 µM | Cell viability, ROS, Bax, Bcl-2, caspase-3, β-actin, COX4, Cyt-4, p38 MAPK, ERK | Liu et al. (2012) | ||
| Quercetin | H2O2-induced epidermal melanocytes (human cell) | 25 µM | TYRe, Cell viability, ROS production, β-actin | Guan et al. (2015) | |
| Kaempferol | HMVII (human cell) | 1, 5, 10 and 20 µM | TYR activity, melanin content | Takekoshi et al. (2014) | |
| B16F10 | 8, 16, 32 μM | Viability, melanin melanin contents, Synthesis, TYR activity, MC1R, MITF, TYRP1, DCT | Wang et al. (2017) | ||
| Apigenin | H2O2-induced PIG3V (human cell) | 1, 5, 10 and 20 μM | Cell viability, SOD, CAT, GSH-PX, MDA, Nrf2, HO-1, NQO1, β-actin | Zhang et al. (2020) | |
| Dopamine-induced melanocytes (human cell) | 0.3–10 μM | Cell viability, ROS, JNK, p38MAPK, Akt, caspase-3, PARP | Lin et al. (2011a) | ||
| Galangin | Male C57BL/6 (mice) | 0.425 mg/kg, 4.25 m g/kg | Melanocytes, TYR activity, CHE activity, MDA | Huo et al. (2014) | |
| Naringenin | B16 melanocytes 4A5 (mice cell) | 0, 10, 25, 50, 100, 200 μM | Tyrp1, Dct, MITF, ERK, PI3K, GSK-3β, β-actin | Ohguchi et al. (2006) | |
| B16-F10 (mice cell) | 3–50 μM | Cell viability, melanin content, TYR, MITF, β-catenin, GSK-3β, Akt | Huang et al. (2011) | ||
| Hesperetin | B16-F10 (mice cell) | 3, 10, 30, 50 μM | Cell viability, melanin content, TYR, MITF, β-catenin, p38 MAPK, GSK-3β, p38MAPK, ERK, Akt, CREB | Huang et al. (2012) | |
| Afzelin | Epidermal melanocytes (human cell) | 0, 10, 50, 100 μM | TYR activity, Cell viability, MITF, TRP-1, TRP-2, p42/44MAPK, p38MAPK, JNK, CREB | Jung et al. (2016) | |
| Fisetin | B16F10 (mice cell), zebrafish model | 5, 20 µM | MITF, TYR, cell viability, melanin Content | Molagoda et al. (2020) | |
| Puerarin | Melan-a cell, zebrafish model, MITFvit/vit mice | 50 µM | MITF-M, Bcl-2, TRP-2, TYR, cAMP, melanin content cell viability, melanin content, TYR, TRP-1, MITF, GAPDH, ERK1/2, p38, JNK | Park et al. (2014) | |
| 40% monobenzone cream-induced emale C57BL/6 (mice), melanocytes from foreskins (human cell) | 1, 5, 10, 20, 40 μmol/L | Ding et al. (2019) | |||
| Butin | Hydroquinone-induced mice | 0.425, 4.25, 42.5 mg/kg | TYR, Trp-1, CHE, MDA | Huo et al. (2017) | |
| B16 cell, H2O2-induced zebrafish | 1, 10, 100 µM | ROS, melanin Content, TYR | Lai et al. (2021) | ||
| Liquiritin | B16-F1 (mice cell), HMVII (human cell) | 12.5, 25, 50 µM | Cell viability, melanin Content, TYR, TRP-1, TRP-2, p38, CREB, MITF, GAPDH | Uto et al. (2019) | |
| Liquiritigenin | B16-F1 (mice cell), HMVII (human cell) | 12.5, 25, 50 µM | Cell viability, melanin Content, TYR, TRP-1, TRP-2, p38, CREB, MITF, GAPDH | Uto et al. (2019) | |
| Vitexin | H2O2-induced PIG1 | 10, 20, 30, 40 µM | Cells viability, IL-1β, IL-17A, Nrf2, HO-1, NQO-1, SOD, cyt-C, ERK, ROS, p53, Bax, Bcl-2, β-actin, caspase-3 | Li et al. (2020) | |
| Hyperoside | H2O2-induced epidermal melanocytes (human cell) | 2, 10, 50 µg/ml | Cell viability, melanin amount, Bcl-2, Bax, caspase 3, GAPDH, AKT, p38 | Yang et al. (2016) | |
| Baicalin | 40% monobenzone-induced C57BL/6 (mice) | 20 mg/ml | CD8+T, CXCL10, CXCR3, IL-6, TNF-α, IFN-γ, IL-13 | Zhu et al. (2019) | |
| Polyphenol | EGCG | IFN-γ-induced (human cell), CD8+T | 0, 10, 20, 40 µM | ICAM-1, CXCL10, and MCP-1, JAK2/STATs, CD11a, CXCR3, CCR2 | Ning et al. (2015) |
| Female C57BL/6 (mice) | 2%, 5% and 10% EGCG cream | CD8+ T cells, TNF-α, IFN-γ, and IL-6, CXCl3, CXCL5, CXCR4, S100B, TGFBR2, c-fos, Rab27A, EGFR, PI3K | Zhu et al. (2014) | ||
| Cannabidiol | Epidermal melanocytes (human cell) | 1, 3, 6 µM | MITF, TYR, TRP-1, TRP-2, p38MAPK, p42/44 MAPK, TYR activity, cell viability | Hwang et al. (2017) | |
| 1,5-dicQA | B16 (mice cell) | 0–400 µM | Tyr activity, MITF, TYR, TRP-1, TRP-2, ERK, JNK, p38, PKA | Mamat et al. (2018) | |
| 3,5-diCQA | B16 (mice cell) | 0–200 µM | TYR activity, TYR, TRP1, TRP2, MITF, β-catenin | Mamat et al. (2017) | |
| 3,5-diCQM | B16F10 (mice cell) | 0–50 µM | TYR activity, melanin content, TRP-1, TRP-2, MITF, cAMP, ERK, p38MAPK, JNK, AKT | Kim et al. (2015) | |
| Maclurin | H2O2-induced epidermal melanocytes (human cell) | 1, 10, 50 µM | TRP-1, TRP-2, MITF, tyrosinase, cAMP, PKA, CREB, p38 MAPK, p44/42 MAPK, PKA | Hwang et al. (2019) | |
| Rosmarinic acid | B16 (mice cell) | 1, 10, 50, 100 µM | Melanin content, CREB, p38mapk, Akt, tyrosinase | Lee et al. (2007) | |
| Paeonol | H2O2-induced PIG1 (human cell) | 5, 10, 20, 40 µM | Cell viability, TYR, TRP-1, MITF, CAT, HO-1, NQO1, SOD2, Nrf2, GAPDH, SOD, GSH-Px | Guo and Zhang (2021) | |
| 6-Shogaol | H2O2-induced HEMn-MPs (human cell) | 5 µM | Cell viability, MITF, HO-1, NQO1, Nrf2, GAPDH | Yang et al. (2020b) | |
| Morin | B16F10 (mice cell) | 25, 50, 100, 250, 500 μM | MITF, TRP-1, TRP-2, GAPDH, ERK, p38 | Shin et al. (2021) | |
| Glycosides | Geniposide | NE-induced HEMn (human cell) | 0–100 µM | TYR activity, melanin, c-kit receptor, SCF ligand | Wen-Jun et al. (2008) |
| H2O2-induced primary melanocytes (human cell) | ROS, SOD, CAT, Akt, Bcl-2, Bax, caspase 3, caspase 9, β-actin | Lu et al. (2018) | |||
| C-3-G | TVM-A12,M14,A-375 (human cell) | 5, 10 μM | Cell viability, proliferation, NF-68 kDa, NF-160 kDa, NF-200 kDa, Melan-A/MART-1 | Serafino et al. (2004) | |
| THSG | B16F1 (mice cell) | 1–10 μg/ml | Melanin amount, TYR activity, MITF, ERK, p38 MAPK, JNK, cAMP | Jiang et al. (2009) | |
| B16 (mice cell) | 0.1–25 μg/ml | TYR activity, melanin content | Guan et al. (2008) | ||
| Glycyrrhizin | B16 (mice cell) | 0.2, 0.5, 1.0, 1.5 mM | Cell viability, melanin amount, AP-1, CREB, p42/44 MAPK, cAMP, GSK-3β, MITF | Lee et al. (2005) | |
| H2O2-induced NHEM (human cell) | 1 mM | Cell viability, ROS, β-actin, Nrf2, HO-1, GAPDH, NQO-1, GCLC, GCLM | Mou et al. (2019) | ||
| Paeoniflorin | Epidermal melanocytes (human cell), 40% monobenzone-inducedC57BL/6 (mice) | 0, 5, 10 μg/ml, 60 mg/kg in 20% propanediol | Cell vitality and proliferation, melanin amount, TRP-1, MITF, TYR, ERK, CREB, GAPDH cell viability, ROS, SOD, CAT, Nrf2, NQO1, HO-1 | Hu et al. (2020a) | |
| H2O2-induced PIG1, PIG3V (human cell) | 50–400 µM | Yuan et al. (2020) | |||
| Cistanche deserticola polysaccharide | H2O2-induced B16F10 (mice cell) and epidermal melanocytes (human cell), zebrafish | 20,40,80 μg/ml | Cell viability, melanin amount, TYR, ROS, MITF, TRP1, TRP2, RAB2 7A, FSCN1, GAPDH, ERK, JNK, p38, ROS, Nrf2, HO-1 | Hu et al. (2020b) | |
| Madecassoside | H2O2-induced B16F10 (mice cell), HEM (human cell), zebrafish | 20, 40, 80 µg/ml | Cell viability, melanin amount, TYR, MITF, TRP1, TRP2, RAB2 7A, FSCN1, GAPDH, ERK, JNK, p38, ROS, Nrf2, HO-1, MAPK | Ling et al. (2017) | |
| Coumarin | Psoralidin | In silico (no cell) | 0.125, 0.25, 0.5, 1 g/ml | TYR, a rate-limiting enzyme of melanogenesis | Shi et al. (2018) |
| isofraxidin | B16F10 (mice cell), zebrafish | 12.5, 25 µM | Melanocytes, TYR activity, melanin, MIFT, TRP-1 | Yim et al. (2017a) | |
| Scopoletin | B16F10 (mice cell) | 0–50 μM | TYR activity, melanin content, TYR, MITF, CREB, β-actin, melanin content, TYR activity, melanin content, Cell viability, ROS | Ahn et al. (2014), Heriniaina et al. (2018) | |
| B16F10 (mice cell), zebrafish | 10–25 μmol/L | ||||
| 7-Isopentenyloxycoumarin | Melan-a (mice cell) | 1, 10, 20, 40 µM | Cells viability, melanin content, tyrosinase, TRP-1, TRP-2, and MITF | Fiorito et al. (2018) | |
| Other compounds | Sesamin | B16F1 (mice cell) | 5, 10, 20 µM | Melanin amount, TYR activity, TYR, CREB, MITF, p38MAPK, PKA, cAMP | Heriniaina et al. (2018) |
| Cubebin | B16 (mice cell) | 0–20 µM | Melanin amount, cell proliferation, TYR activity, p38 MAPK, ERK1/2, p70 S6K1 | Hirata et al. (2007) | |
| Berberine | H2O2-induced PIG1 (human cell) | 0.1, 1.0, 5.0 μM | Cells viability, Bax, Bcl-2, PARP, HO-1, NQO1, SOD, Nrf2, Mitf, TYR, TYRP1, DCT, IL-6, IL-8, p65, ROS | Jiang et al. (2019) | |
| Vitamin D | H2O2-induced PIG1, PIG3V (human cell) | 1 nM | Cells viability, SOD, ROS, β-catenin, CDH3, GSK3β, Nrf2, MITF, caspase3, MDA, GAPDH, HO-1 | Tang et al. (2018) |
Cubebin
Cubebin (Figure 7B) is a compound extracted from the seeds of Piper cubeba L. f. (Godoy de Lima et al., 2018). It exhibits various pharmacological activities, such as trypanosomiasis, anti-Mycobacterium (Silva et al., 2007), analgesic, anti-inflammatory (Souza et al., 2004) and vasodilator (Somani et al., 2017). In vitro, cubebin showed a concentration time-dependent melanogenesis activity in B16 cells. The mechanism is to promote melanin synthesis by increasing the phosphorylation level of p38 MAPK, which in turn increases the expression of MITF and tyrosinase (Hirata et al., 2007).
Berberine
Berberine (BBR, (Figure 7C) natural isoquinoline alkaloid, is a major compound isolated from the Chinese herb Coptis chinensis Franch. (Wang et al., 2021d), and studies have found that BBR has pharmacological activities against cancer, hypolipidemic, cardiovascular, anti-inflammatory, and antioxidant stress (Zhao et al., 2021). Wei et al. studied the potential medicinal value of berberine in vitiligo. At 0.1–5.0 μM BBR induced melanocyte proliferation in a time-dependent manner. At the same time, BBR inhibited the oxidative damage induced by H2O2 by down regulating the activities of CAT and SOD and reducing the accumulation of ROS in PIG1 cells, 5 μM BBR inhibited the cleavage of PARP and the apoptosis of melanocytes induced by H2O2 by down regulating the ratio of Bax/Bcl-2. The antioxidant effect of BBR depends on Nrf2-ARE pathway, and the process involves up regulation of HO-1, SOD and NQO-1 protein expression, and the protective effect is obviously reduced after Nrf2 gene is knocked out. In addition, BBR enhanced the expression of MITF in melanocytes induced by oxidative stress, thereby increasing the production of melanin. Finally, BBR inhibited H2O2-induced upstream NF-κB activation and expression of IL-6 and IL-8 (Jiang et al., 2019). BBR could protect melanocytes from oxidative stress through anti-oxidation and anti-inflammatory. It is a potential natural drug against vitiligo.
Vitamin D
Vitamin D (1,25-dihy-droxyvitamin D3, Figure 7D) is a cyclopentane phenanthrene compound, which is an essential vitamin for human body, it mainly comes from daily meat (Dominguez et al., 2021). Vitamin D has been used in autoimmune diseases, cancer and osteoporosis (Sintov et al., 2014). Vitamin D deficiency leads to the excessive production of ROS in mitochondria and damages the antioxidant system (Latham et al., 2021). Previous studies have confirmed that vitamin D compounds regulate the proliferation, differentiation, migration and apoptosis of melanocytes and affect T-cell mediated peripheral immune response (Birlea et al., 2008; Kawakami et al., 2014). In H2O2-induced oxidative stress models in PIG1 and PIG3V cells, vitamin D activated WNT/β-Catenin signaling pathway exerted antioxidant activity, the mechanism included the promotion of GSK3β inactivation, increased β-catenin nuclear translocation and activation of the downstream Nrf2/ARE pathway. In addition, vitamin D passed through up regulation of MITF in a β-catenin pathway dependent manner promoted melanocyte proliferation and protected melanocytes from H2O2-induced apoptosis by suppressing caspase3 expression (Tang et al., 2018).
Conclusion and Prospective
In traditional medicine, there are many traditional herbal medicines (Kwon et al., 2018; Xu et al., 2017; Moreira et al., 2012) for the treatment of pigment deficiency. Their extracts significantly improved the activity of tyrosinase (Xu et al., 2017). However, their specific components and mechanism of action are still unclear. Vitiligo is an autoimmune skin disease in which melanocytes are destroyed by autoreactive CD8+ T cells, resulting in cutaneous leukoplakia. Depigmented mouse skin lesions with autoimmune features were fitted to a monobenzone-induced vitiligo model (Zhu et al., 2013). Unfortunately, among all natural drugs mentioned in this review, only four natural products (such as Vitexin, baicalin, EGCG and berberine) currently exhibit anti depigmenting pharmacological activity in this model. We mentioned earlier that oxidative stress may be a driver of autoimmune destruction and that intense and persistent oxidative stress leads to apoptosis, damage, and antigen exposure of melanocytes, which in turn trigger autoimmune destruction. Therefore, recently, researchers have paid more attention to the mechanism of action of natural products against oxidative stress in melanocytes. Some natural drugs (such as baicalein, Vitexin, maclurin, etc.) inhibited the damaging effects of H2O2-induced oxidative stress on melanocytes, even counterstaining depigmented mouse skin lesions. Therefore, it is reasonable to speculate that some of these members contribute to protection against autoimmune destruction. 37 natural products can elevate melanin expression by elevating tyrosinase activity in an in vitro melanocyte model in vivo, but their contribution to intervening in autoimmune destruction is similarly unknown. The above mentioned vitiligo models are all inducible and cannot fully replicate the disease characteristics of human vitiligo, thus increasing the difficulty of developing new drugs. Genetically edited mice have not been widely promoted (Riding et al., 2019). Several natural drugs have been reported for their use in the clinic. For example: observations from clinical studies have shown that oral Glycyrrhizin Combined with UVB therapy improves active systemic vitiligo, but also exposes minor side effects (Mou et al., 2016). In clinical studies, the overall recolor rate of PUVA (psoralen plus UVA) was only 44% (Bishnoi and Parsad 2018). However, due to the lack of large clinical research, they still have a long way to go before they can be promoted as anti-vitiligo agents (Maleš et al., 2019). A systematic review study showed that vitiligo does not generally produce benefi cial outcomes with the use of topical antioxidants, but the added effect of oral intake cannot be ignored (Speeckaert et al., 2018). Developing new natural products against autoimmune destruction will be a hotspot in the future and also provide a new direction to elucidate the pathogenesis of vitiligo. Vitiligo treatment serves two purposes: 1) Controlling vitiligo disease progression during the active phase and 2) increasing melanocyte production during the stationary phase. We propose the hypothesis that in the future natural drugs with anti-oxidant and anti-autoimmune properties are used in vitiligo progression phase and natural drugs with improved tyrosinase activity are used in stability phase.
In conclusion, strong evidence that natural products can prevent or treat vitiligo is still lacking. Appropriately designed clinical trials are needed to further understand the efficacy of natural products against vitiligo. As an auxiliary means of phototherapy, plant derived compounds with antioxidant properties are becoming an attractive choice for the treatment of vitiligo (Dell'Anna et al., 2007). Natural products (NPs) extracted from plants show the effect of increasing the expression of melanin, and have less side effects on human body, which is of great significance for us to continue to develop natural drugs (Yin et al., 2017).
Author Contributions
Concepts: YP. Wrote the paper: YP, SW, YH, and JL. Designed the figures: JZ, YP, and YY. Reviewed manuscript: JG and QN. All authors commented on the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the National Natural Science Foundation of China (Grant nos. 81804066, 82074443, 81873310), and by Xinglin Scholar Research Promotion Project of Chengdu University of TCM (Grant nos. QNXZ2019017, and QNXZ2020003) and “Hundred Talents Program” of the Hospital of Chengdu University of Traditional Chinese Medicine (Grant nos. 20-B01, 20-Q03, and 20-Q05).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Abbreviations
HO-1, heme oxygenase-1; Nrf2, The nuclear factor erythroid 2-like factor 2; NE, Norepinephrine; GCLM, g-glutamylcystine ligase modulatory subunit; GCLC, g-glutamylcystine ligase catalytic subunit; Cyt-4, cytochrome c; ROS, reactive oxygen species; TYR, tyrosinase; TRP-1, tyrosinase-related protein 1; TRP-2, tyrosinase-related protein 2; MITF, microphthalmia-associated transcription factor; MAPK, mitogen-activated protein kinase; ERK, extracellular signal-regulated kinase; JNK, c-Jun N-terminal kinase; cAMP, intracellular cyclic adenosine monophosphate; GSK-3β, glycogen synthase kinase 3β; cRE, cAMP-response element; cREB, cAMP-response element binding protein; PKA, protein kinase A; α-MSH, α melanocyte stimulating hormone; PI3K, phosphoinositide 3-kinase; Akt, protein kinase B; c-Kit, proto-oncogene; TNF-α, tumor necrosis factor alpha; IFN-γ, interferon-γ; ARE, antioxidant response element; SOD, Superoxide dismutase; CAT, catalase; HEMn, normal human epidermal melanocytes; HEKn, normal human epidermal keratinocytes
References
- Abdel-Malek Z. A., Jordan C., Ho T., Upadhyay P. R., Fleischer A., Hamzavi I. (2020). The enigma and Challenges of Vitiligo Pathophysiology and Treatment. Pigment Cel Melanoma Res 33 (6), 778–787. 10.1111/pcmr.12878 [DOI] [PubMed] [Google Scholar]
- Ahluwalia J., Correa-Selm L. M., Rao B. K. (2017). Vitiligo: Not Simply a Skin Disease. Skinmed 15 (2), 125–127. 10.1080/14725843.2017.1282416 [DOI] [PubMed] [Google Scholar]
- Ahmad A., Ali T., Park H. Y., Badshah H., Rehman S. U., Kim M. O. (2017). Neuroprotective Effect of Fisetin against Amyloid-Beta-Induced Cognitive/Synaptic Dysfunction, Neuroinflammation, and Neurodegeneration in Adult Mice. Mol. Neurobiol. 54 (3), 2269–2285. 10.1007/s12035-016-9795-4 [DOI] [PubMed] [Google Scholar]
- Ahmad A., Ali T., Rehman S. U., Kim M. O. (2019). Phytomedicine-Based Potent Antioxidant, Fisetin Protects CNS-Insult LPS-Induced Oxidative Stress-Mediated Neurodegeneration and Memory Impairment. J. Clin. Med. 8 (6). 10.3390/jcm8060850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahn M.-J., Hur S.-J., Kim E.-H., Lee S. H., Shin J. S., Kim M.-K., et al. (2014). Scopoletin fromCirsium setidensIncreases Melanin Synthesis via CREB Phosphorylation in B16F10 Cells. Korean J. Physiol. Pharmacol. 18 (4), 307–311. 10.4196/kjpp.2014.18.4.307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Shobaili H. A., Rasheed Z. (2015). Oxidized Tyrosinase: A Possible Antigenic Stimulus for Non-segmental Vitiligo Autoantibodies. J. Dermatol. Sci. 79 (3), 203–213. 10.1016/j.jdermsci.2015.06.009 [DOI] [PubMed] [Google Scholar]
- Alvarez-Arellano L., Salazar-García M., Corona J. C. (2020). Neuroprotective Effects of Quercetin in Pediatric Neurological Diseases. Molecules 25 (23). 10.3390/molecules25235597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basnet P., Matsushige K., Hase K., Kadota S., Namba T. (1996). Four Di-O-caffeoyl Quinic Acid Derivatives from Propolis. Potent Hepatoprotective Activity in Experimental Liver Injury Models. Biol. Pharm. Bull. 19 (11), 1479–1484. 10.1248/bpb.19.1479 [DOI] [PubMed] [Google Scholar]
- Baswan S. M., Klosner A. E., Glynn K., Rajgopal A., Malik K., Yim S., et al. (2020). Therapeutic Potential of Cannabidiol (CBD) for Skin Health and Disorders. Ccid 13, 927–942. 10.2147/ccid.s286411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergqvist C., Ezzedine K. (2021). Vitiligo: A Focus on Pathogenesis and its Therapeutic Implications. J. Dermatol. 48 (3), 252–270. 10.1111/1346-8138.15743 [DOI] [PubMed] [Google Scholar]
- Bernard G., Alves Dos Santos H., Etienne A., Samaillie J., Neut C., Sahpaz S., et al. (2020). MeJA Elicitation of Chicory Hairy Roots Promotes Efficient Increase of 3,5-diCQA Accumulation, a Potent Antioxidant and Antibacterial Molecule. Antibiotics (Basel) 9 (10). 10.3390/antibiotics9100659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickers D. R., Athar M. (2006). Oxidative Stress in the Pathogenesis of Skin Disease. J. Invest. Dermatol. 126 (12), 2565–2575. 10.1038/sj.jid.5700340 [DOI] [PubMed] [Google Scholar]
- Birlea S., Costin G.-E., Norris D. (2008). Cellular and Molecular Mechanisms Involved in the Action of Vitamin D Analogs Targeting Vitiligo Depigmentation. Cdt 9 (4), 345–359. 10.2174/138945008783954970 [DOI] [PubMed] [Google Scholar]
- Bishnoi A., Parsad D. (2018). Clinical and Molecular Aspects of Vitiligo Treatments. Int. J. Mol. Sci. 19 (5). 10.3390/ijms19051509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai X., Wang X., Li J., Chen S. (2017). Protective Effect of Glycyrrhizin on Myocardial Ischemia/reperfusion Injury-Induced Oxidative Stress, Inducible Nitric Oxide Synthase and Inflammatory Reactions through High-Mobility Group Box 1 and Mitogen-Activated Protein Kinase Expression. Exp. Ther. Med. 14 (2), 1219–1226. 10.3892/etm.2017.4617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calderón-Montaño J. M., Burgos-Morón E., Pérez-Guerrero C., López-Lázaro M. (2011). A Review on the Dietary Flavonoid Kaempferol. Mini Rev. Med. Chem. 11 (4), 298–344. [DOI] [PubMed] [Google Scholar]
- Cao H.-j., Li C.-r., Wang L.-y., Ziadlou R., Grad S., Zhang Y., et al. (2019). Effect and Mechanism of Psoralidin on Promoting Osteogenesis and Inhibiting Adipogenesis. Phytomedicine 61, 152860. 10.1016/j.phymed.2019.152860 [DOI] [PubMed] [Google Scholar]
- Cao X., Xiao H., Zhang Y., Zou L., Chu Y., Chu X. (2010). 1, 5-Dicaffeoylquinic Acid-Mediated Glutathione Synthesis through Activation of Nrf2 Protects against OGD/reperfusion-induced Oxidative Stress in Astrocytes. Brain Res. 1347, 142–148. 10.1016/j.brainres.2010.05.072 [DOI] [PubMed] [Google Scholar]
- Carreras-Sureda A., Pihán P., Hetz C. (2018). Calcium Signaling at the Endoplasmic Reticulum: fine-tuning Stress Responses. Cell Calcium 70, 24–31. 10.1016/j.ceca.2017.08.004 [DOI] [PubMed] [Google Scholar]
- Caselli A., Cirri P., Santi A., Paoli P. (2016). Morin: A Promising Natural Drug. Cmc 23 (8), 774–791. 10.2174/0929867323666160106150821 [DOI] [PubMed] [Google Scholar]
- Chaingam J., Juengwatanatrakul T., Yusakul G., Kanchanapoom T., Putalun W. (2020). HPLC-UV-based Simultaneous Determination of Canthin-6-One Alkaloids, Quassinoids,and Scopoletin: the Active Ingredients in Eurycoma Longifolia Jack and Eurycoma Harmandiana Pierre, and Their Anti-inflammatory Activities. J. AOAC Int. 104, 802–810. 10.1093/jaoacint/qsaa141 [DOI] [PubMed] [Google Scholar]
- Chang X., Zhang T., Liu D., Meng Q., Yan P., Luo D., et al. (2021). Puerarin Attenuates LPS-Induced Inflammatory Responses and Oxidative Stress Injury in Human Umbilical Vein Endothelial Cells through Mitochondrial Quality Control. Oxid Med. Cel Longev 2021, 6659240. 10.1155/2021/6659240 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Cheevarungnapakul K., Khaksar G., Panpetch P., Boonjing P., Sirikantaramas S. (2019). Identification and Functional Characterization of Genes Involved in the Biosynthesis of Caffeoylquinic Acids in Sunflower (Helianthus Annuus L.). Front. Plant Sci. 10, 968. 10.3389/fpls.2019.00968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen F., Tang Y., Sun Y., Veeraraghavan V. P., Mohan S. K., Cui C. (2019a). 6-shogaol, a Active Constiuents of Ginger Prevents UVB Radiation Mediated Inflammation and Oxidative Stress through Modulating NrF2 Signaling in Human Epidermal Keratinocytes (HaCaT Cells). J. Photochem. Photobiol. B: Biol. 197, 111518. 10.1016/j.jphotobiol.2019.111518 [DOI] [PubMed] [Google Scholar]
- Chen J., Li S., Li C. (2021a). Mechanisms of Melanocyte Death in Vitiligo. Med. Res. Rev. 41 (2), 1138–1166. 10.1002/med.21754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen L., Shen Z. (2020). Tissue-resident Memory T Cells and Their Biological Characteristics in the Recurrence of Inflammatory Skin Disorders. Cell Mol Immunol 17 (1), 64–75. 10.1038/s41423-019-0291-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen T. C., Yen C. K., Lu Y. C., Shi C. S., Hsieh R. Z., Chang S. F., et al. (2020). The Antagonism of 6-shogaol in High-Glucose-Activated NLRP3 Inflammasome and Consequent Calcification of Human Artery Smooth Muscle Cells. Cell Biosci 10, 5. 10.1186/s13578-019-0372-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X., Guo W., Chang Y., Chen J., Kang P., Yi X., et al. (2019b). Oxidative Stress-Induced IL-15 Trans-presentation in Keratinocytes Contributes to CD8+ T Cells Activation via JAK-STAT Pathway in Vitiligo. Free Radic. Biol. Med. 139, 80–91. 10.1016/j.freeradbiomed.2019.05.011 [DOI] [PubMed] [Google Scholar]
- Chen Y., Wang B., Yuan X., Lu Y., Hu J., Gao J., et al. (2021b). Vitexin Prevents Colitis-Associated Carcinogenesis in Mice through Regulating Macrophage Polarization. Phytomedicine 83, 153489. 10.1016/j.phymed.2021.153489 [DOI] [PubMed] [Google Scholar]
- Chiang H.-M., Lin J.-W., Hsiao P.-L., Tsai S.-Y., Wen K.-C. (2011). Hydrolysates of Citrus Plants Stimulate Melanogenesis Protecting against UV-Induced Dermal Damage. Phytother. Res. 25 (4), 569–576. 10.1002/ptr.3302 [DOI] [PubMed] [Google Scholar]
- Chiu W.-T., Shen S.-C., Chow J.-M., Lin C.-W., Shia L.-T., Chen Y.-C. (2010). Contribution of Reactive Oxygen Species to Migration/invasion of Human Glioblastoma Cells U87 via ERK-dependent COX-2/PGE2 Activation. Neurobiol. Dis. 37 (1), 118–129. 10.1016/j.nbd.2009.09.015 [DOI] [PubMed] [Google Scholar]
- Cho Y.-M., Onodera H., Ueda M., Imai T., Hirose M. (2006). A 13-week Subchronic Toxicity Study of Dietary Administered Morin in F344 Rats. Food Chem. Toxicol. 44 (6), 891–897. 10.1016/j.fct.2005.12.002 [DOI] [PubMed] [Google Scholar]
- Choi E.-O., Jeong J.-W., Park C., Hong S. H., Kim G.-Y., Hwang H.-J., et al. (2016). Baicalein Protects C6 Glial Cells against Hydrogen Peroxide-Induced Oxidative Stress and Apoptosis through Regulation of the Nrf2 Signaling Pathway. Int. J. Mol. Med. 37 (3), 798–806. 10.3892/ijmm.2016.2460 [DOI] [PubMed] [Google Scholar]
- Cui H. X., Chen J. H., Li J. W., Cheng F. R., Yuan K. (2018). Protection of Anthocyanin from Myrica Rubra against Cerebral Ischemia-Reperfusion Injury via Modulation of the TLR4/NF-Κb and NLRP3 Pathways. Molecules 23 (7). 10.3390/molecules23071788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui S., Wu Q., Wang J., Li M., Qian J., Li S. (2019). Quercetin Inhibits LPS-Induced Macrophage Migration by Suppressing the iNOS/FAK/paxillin Pathway and Modulating the Cytoskeleton. Cell Adhes. Migration 13 (1), 1–12. 10.1080/19336918.2018.1486142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cushnie T. P. T., Hamilton V. E. S., Chapman D. G., Taylor P. W., Lamb A. J. (2007). Aggregation of Staphylococcus aureus Following Treatment with the Antibacterial Flavonol Galangin. J. Appl. Microbiol. 103 (5), 1562–1567. 10.1111/j.1365-2672.2007.03393.x [DOI] [PubMed] [Google Scholar]
- de Oliveira M. R., Nabavi S. F., Habtemariam S., Erdogan Orhan I., Daglia M., Nabavi S. M. (2015). The Effects of Baicalein and Baicalin on Mitochondrial Function and Dynamics: A Review. Pharmacol. Res. 100, 296–308. 10.1016/j.phrs.2015.08.021 [DOI] [PubMed] [Google Scholar]
- Dell'Anna M. L., Mastrofrancesco A., Sala R., Venturini M., Ottaviani M., Vidolin A. P., et al. (2007). Antioxidants and Narrow Band-UVB in the Treatment of Vitiligo: a Double-Blind Placebo Controlled Trial. Clin. Exp. Dermatol. 32 (6), 631–636. 10.1111/j.1365-2230.2007.02514.x [DOI] [PubMed] [Google Scholar]
- Denat L., Kadekaro A. L., Marrot L., Leachman S. A., Abdel-Malek Z. A. (2014). Melanocytes as Instigators and Victims of Oxidative Stress. J. Invest. Dermatol. 134 (6), 1512–1518. 10.1038/jid.2014.65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dincer Rota D., Aksoy Sarac G., Arca E., Onder M. (2021). Comparison of the Efficacy of Broad-Band Targeted UVB Phototherapy and Topical Psoralen with Targeted UVA Phototherapy in Localized Vitiligo. Dermatol. Ther. 34 (1), e14562. 10.1111/dth.14562 [DOI] [PubMed] [Google Scholar]
- Ding G., Xu X., Li D., Chen Y., Wang W., Ping D., et al. (2020). Fisetin Inhibits Proliferation of Pancreatic Adenocarcinoma by Inducing DNA Damage via RFXAP/KDM4A-dependent Histone H3K36 Demethylation. Cell Death Dis 11 (10), 893. 10.1038/s41419-020-03019-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding T., Zhao T., Li Y., Liu Z., Ding J., Ji B., et al. (2021). Vitexin Exerts Protective Effects against Calcium Oxalate crystal-induced Kidney Pyroptosis In Vivo and In Vitro . Phytomedicine 86, 153562. 10.1016/j.phymed.2021.153562 [DOI] [PubMed] [Google Scholar]
- Ding X., Mei E., Hu M., Zhou C., Li X., Cai L., et al. (2019). Effect of Puerarin on Melanogenesis in Human Melanocytes and Vitiligo Mouse Models and the Underlying Mechanism. Phytotherapy Res. 33 (1), 205–213. 10.1002/ptr.6218 [DOI] [PubMed] [Google Scholar]
- Dogra N. K., Kumar S., Kumar D. (2020). Vernonia Anthelmintica (L.) Willd.: An Ethnomedicinal, Phytochemical, Pharmacological and Toxicological Review. J. Ethnopharmacology 256, 112777. 10.1016/j.jep.2020.112777 [DOI] [PubMed] [Google Scholar]
- Dominguez L. J., Farruggia M., Veronese N., Barbagallo M. (2021). Vitamin D Sources, Metabolism, and Deficiency: Available Compounds and Guidelines for its Treatment. Metabolites 11 (4), 255. 10.3390/metabo11040255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du Y., Luo M., Du Y., Xu M., Yao Q., Wang K., et al. (2021). Liquiritigenin Decreases Aβ Levels and Ameliorates Cognitive Decline by Regulating Microglia M1/M2 Transformation in AD Mice. Neurotox Res. 39 (2), 349–358. 10.1007/s12640-020-00284-z [DOI] [PubMed] [Google Scholar]
- Duan J., Guan Y., Mu F., Guo C., Zhang E., Yin Y., et al. (2017). Protective Effect of Butin against Ischemia/reperfusion-Induced Myocardial Injury in Diabetic Mice: Involvement of the AMPK/GSK-3β/Nrf2 Signaling Pathway. Sci. Rep. 7, 41491. 10.1038/srep41491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ezzedine K., Eleftheriadou V., Whitton M., van Geel N. (2015). Vitiligo. The Lancet 386 (9988), 74–84. 10.1016/s0140-6736(14)60763-7 [DOI] [PubMed] [Google Scholar]
- Fan Z., Cai L., Wang S., Wang J., Chen B. (2021). Baicalin Prevents Myocardial Ischemia/Reperfusion Injury through Inhibiting ACSL4 Mediated Ferroptosis. Front. Pharmacol. 12, 628988. 10.3389/fphar.2021.628988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang D., Xiong Z., Xu J., Yin J., Luo R. (2019). Chemopreventive Mechanisms of Galangin against Hepatocellular Carcinoma: A Review. Biomed. Pharmacother. 109, 2054–2061. 10.1016/j.biopha.2018.09.154 [DOI] [PubMed] [Google Scholar]
- Fiorito S., Epifano F., Palmisano R., Genovese S., Taddeo V. A. (2017). A Re-investigation of the Phytochemical Composition of the Edible Herb Amaranthus Retroflexus L. J. Pharm. Biomed. Anal. 143, 183–187. 10.1016/j.jpba.2017.05.051 [DOI] [PubMed] [Google Scholar]
- Fiorito S., Epifano F., Preziuso F., Cacciatore I., di Stefano A., Taddeo V. A., et al. (2018). Natural Oxyprenylated Coumarins Are Modulators of Melanogenesis. Eur. J. Med. Chem. 152, 274–282. 10.1016/j.ejmech.2018.04.051 [DOI] [PubMed] [Google Scholar]
- Gao Z., Huang K., Yang X., Xu H. (1999). Free Radical Scavenging and Antioxidant Activities of Flavonoids Extracted from the Radix of Scutellaria Baicalensis Georgi. Biochim. Biophys. Acta (Bba) - Gen. Subjects 1472 (3), 643–650. 10.1016/s0304-4165(99)00152-x [DOI] [PubMed] [Google Scholar]
- Gnonlonfin B. G., Gbaguidi F., Gbenou J. D., Sanni A., Brimer L. (2011). Changes in Scopoletin Concentration in Cassava Chips from Four Varieties during Storage. J. Sci. Food Agric. 91 (13), 2344–2347. 10.1002/jsfa.4465 [DOI] [PubMed] [Google Scholar]
- Godoy de Lima R., Barros M. T., da Silva Laurentiz R. (2018). Medicinal Attributes of Lignans Extracted from Piper Cubeba: Current Developments. ChemistryOpen 7 (2), 180–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Góngora L., Giner R. M., Máñez S., del Carmen Recio M., Schinella G., Rios J. L. (2002). Effects of Caffeoyl Conjugates of Isoprenyl-Hydroquinone Glucoside and Quinic Acid on Leukocyte Function. Life Sci. 71 (25), 2995–3004. 10.1016/s0024-3205(02)02167-7 [DOI] [PubMed] [Google Scholar]
- Grimes P. E., Nashawati R. (2017). Depigmentation Therapies for Vitiligo. Dermatol. Clin. 35 (2), 219–227. 10.1016/j.det.2016.11.010 [DOI] [PubMed] [Google Scholar]
- Gu C., Yang X., Huang L. (2016). Cistanches Herba: A Neuropharmacology Review. Front. Pharmacol. 7, 289. 10.3389/fphar.2016.00289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan C., Xu W., Hong W., Zhou M., Lin F., Fu L., et al. (2015). Quercetin Attenuates the Effects of H2O2 on Endoplasmic Reticulum Morphology and Tyrosinase export from the Endoplasmic Reticulum in Melanocytes. Mol. Med. Rep. 11 (6), 4285–4290. 10.3892/mmr.2015.3242 [DOI] [PubMed] [Google Scholar]
- Guan S., Su W., Wang N., Li P., Wang Y. (2008). A Potent Tyrosinase Activator from Radix Polygoni Multiflori and its Melanogenesis Stimulatory Effect in B16 Melanoma Cells. Phytother. Res. 22 (5), 660–663. 10.1002/ptr.2358 [DOI] [PubMed] [Google Scholar]
- Guo S., Zhang Q. (2021). Paeonol Protects Melanocytes against Hydrogen Peroxide-Induced Oxidative Stress through Activation of Nrf2 Signaling Pathway. Drug Dev. Res. 10.1002/ddr.21793 [DOI] [PubMed] [Google Scholar]
- Harris J. E., Harris T. H., Weninger W., John Wherry E., Hunter C. A., Turka L. A. (2012). A Mouse Model of Vitiligo with Focused Epidermal Depigmentation Requires IFN-γ for Autoreactive CD8+ T-Cell Accumulation in the Skin. J. Invest. Dermatol. 132 (7), 1869–1876. 10.1038/jid.2011.463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- He H., Wang S., Tian J., Chen L., Zhang W., Zhao J., et al. (2015). Protective Effects of 2,3,5,4′-Tetrahydroxystilbene-2-O-β-D-Glucoside in the MPTP-Induced Mouse Model of Parkinson's Disease: Involvement of Reactive Oxygen Species-Mediated JNK, P38 and Mitochondrial Pathways. Eur. J. Pharmacol. 767, 175–182. 10.1016/j.ejphar.2015.10.023 [DOI] [PubMed] [Google Scholar]
- He M., Min J.-W., Kong W.-L., He X.-H., Li J.-X., Peng B.-W. (2016). A Review on the Pharmacological Effects of Vitexin and Isovitexin. Fitoterapia 115, 74–85. 10.1016/j.fitote.2016.09.011 [DOI] [PubMed] [Google Scholar]
- Hearing V. J. (1999). Biochemical Control of Melanogenesis and Melanosomal Organization. J. Invest. Dermatol. Symp. Proc. 4 (1), 24–28. 10.1038/sj.jidsp.5640176 [DOI] [PubMed] [Google Scholar]
- Heeba G. H., Rabie E. M., Abuzeid M. M., Bekhit A. A., Khalifa M. M. (2021). Morin Alleviates Fructose-Induced Metabolic Syndrome in Rats via Ameliorating Oxidative Stress, Inflammatory and Fibrotic Markers. Korean J. Physiol. Pharmacol. 25 (3), 177–187. 10.4196/kjpp.2021.25.3.177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heriniaina R. M., Dong J., Kalavagunta P. K., Wu H.-L., Yan D.-S., Shang J. (2018). Effects of Six Compounds with Different Chemical Structures on Melanogenesis. Chin. J. Nat. Medicines 16 (10), 766–773. 10.1016/s1875-5364(18)30116-x [DOI] [PubMed] [Google Scholar]
- Hirata N., Naruto S., Ohguchi K., Akao Y., Nozawa Y., Iinuma M., et al. (2007). Mechanism of the Melanogenesis Stimulation Activity of (−)-cubebin in Murine B16 Melanoma Cells. Bioorg. Med. Chem. 15 (14), 4897–4902. 10.1016/j.bmc.2007.04.046 [DOI] [PubMed] [Google Scholar]
- Hu M., Chen C., Liu J., Cai L., Shao J., Chen Z., et al. (2020a). The Melanogenic Effects and Underlying Mechanism of Paeoniflorin in Human Melanocytes and Vitiligo Mice. Fitoterapia 140, 104416. 10.1016/j.fitote.2019.104416 [DOI] [PubMed] [Google Scholar]
- Hu Y., Huang J., Li Y., Jiang L., Ouyang Y., Li Y., et al. (2020b). Cistanche Deserticola Polysaccharide Induces Melanogenesis in Melanocytes and Reduces Oxidative Stress via Activating NRF2/HO‐1 Pathway. J. Cel Mol Med 24 (7), 4023–4035. 10.1111/jcmm.15038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang J., Tong X., Zhang L., Zhang Y., Wang L., Wang D., et al. (2020). Hyperoside Attenuates Bleomycin-Induced Pulmonary Fibrosis Development in Mice. Front. Pharmacol. 11, 550955. 10.3389/fphar.2020.550955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang K., Li C., Gao F., Fan Y., Zeng F., Meng L., et al. (2021). Epigallocatechin-3-Gallate Promotes the In Vitro Maturation and Embryo Development Following IVF of Porcine Oocytes. Dddt 15, 1013–1020. 10.2147/dddt.s295936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang W. H., Lee A. R., Chien P. Y., Chou T. C. (2005). Synthesis of Baicalein Derivatives as Potential Anti-aggregatory and Anti-inflammatory Agents. J. Pharm. Pharmacol. 57 (2), 219–225. 10.1211/0022357055371 [DOI] [PubMed] [Google Scholar]
- Huang Y.-C., Yang C.-H., Chiou Y.-L. (2011). Citrus Flavanone Naringenin Enhances Melanogenesis through the Activation of Wnt/β-Catenin Signalling in Mouse Melanoma Cells. Phytomedicine 18 (14), 1244–1249. 10.1016/j.phymed.2011.06.028 [DOI] [PubMed] [Google Scholar]
- Huang Y. C., Liu K. C., Chiou Y. L. (2012). Melanogenesis of Murine Melanoma Cells Induced by Hesperetin, a Citrus Hydrolysate-Derived Flavonoid. Food Chem. Toxicol. 50 (3-4), 653–659. 10.1016/j.fct.2012.01.012 [DOI] [PubMed] [Google Scholar]
- Huo S.-X., Liu X.-M., Ge C.-H., Gao L., Peng X.-M., Zhao P.-P., et al. (2014). The Effects of Galangin on a Mouse Model of Vitiligo Induced by Hydroquinone. Phytother. Res. 28 (10), 1533–1538. 10.1002/ptr.5161 [DOI] [PubMed] [Google Scholar]
- Huo S.-X., Wang Q., Liu X.-M., Ge C.-H., Gao L., Peng X.-M., et al. (2017). The Effect of Butin on the Vitiligo Mouse Model Induced by Hydroquinone. Phytother. Res. 31 (5), 740–746. 10.1002/ptr.5794 [DOI] [PubMed] [Google Scholar]
- Hwang I. K., Yoo K.-Y., Kim D. W., Jeong S. J., Won C.-K., Moon W.-K., et al. (2006). An Extract of Polygonum Multiflorum Protects against Free Radical Damage Induced by Ultraviolet B Irradiation of the Skin. Braz. J. Med. Biol. Res. 39 (9), 1181–1188. 10.1590/s0100-879x2006000900005 [DOI] [PubMed] [Google Scholar]
- Hwang J.-M., Tseng T.-H., Tsai Y.-Y., Lee H.-J., Chou F.-P., Wang C.-J., et al. (2005). Protective Effects of Baicalein on Tert-Butyl Hydroperoxide-Induced Hepatic Toxicity in Rat Hepatocytes. J. Biomed. Sci. 12 (2), 389–397. 10.1007/s11373-005-1572-8 [DOI] [PubMed] [Google Scholar]
- Hwang Y. S., Oh S. W., Park S. H., Lee J., Yoo J. A., Kwon K., et al. (2019). Melanogenic Effects of Maclurin Are Mediated through the Activation of cAMP/PKA/CREB and P38 MAPK/CREB Signaling Pathways. Oxid Med. Cel Longev 2019, 9827519. 10.1155/2019/9827519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang Y. S., Kim Y.-J., Kim M. O., Kang M., Oh S. W., Nho Y. H., et al. (2017). Cannabidiol Upregulates Melanogenesis through CB1 Dependent Pathway by Activating P38 MAPK and P42/44 MAPK. Chemico-Biological Interactions 273, 107–114. 10.1016/j.cbi.2017.06.005 [DOI] [PubMed] [Google Scholar]
- Imran M., Rauf A., Shah Z. A., Saeed F., Imran A., Arshad M. U., et al. (2019). Chemo-preventive and Therapeutic Effect of the Dietary Flavonoid Kaempferol: A Comprehensive Review. Phytotherapy Res. 33 (2), 263–275. 10.1002/ptr.6227 [DOI] [PubMed] [Google Scholar]
- Iuvone T., Esposito G., De Filippis D., Scuderi C., Steardo L. (2009). Cannabidiol: a Promising Drug for Neurodegenerative Disorders?. CNS Neurosci. Ther. 15 (1), 65–75. 10.1111/j.1755-5949.2008.00065.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang Y., Koh E. (2019). Antioxidant Content and Activity in Leaves and Petioles of Six Sweet Potato (Ipomoea Batatas L.) and Antioxidant Properties of Blanched Leaves. Food Sci. Biotechnol. 28 (2), 337–345. 10.1007/s10068-018-0481-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeng K.-C. G., Hou R. C. W., Wang J.-C., Ping L.-I. (2005). Sesamin Inhibits Lipopolysaccharide-Induced Cytokine Production by Suppression of P38 Mitogen-Activated Protein Kinase and Nuclear Factor-Κb. Immunol. Lett. 97 (1), 101–106. 10.1016/j.imlet.2004.10.004 [DOI] [PubMed] [Google Scholar]
- Jeong Y.-M., Choi Y.-G., Kim D.-S., Park S.-H., Yoon J.-A., Kwon S.-B., et al. (2005). Cytoprotective Effect of green tea Extract and Quercetin against Hydrogen Peroxide-Induced Oxidative Stress. Arch. Pharm. Res. 28 (11), 1251–1256. 10.1007/bf02978208 [DOI] [PubMed] [Google Scholar]
- Jian Z., Li K., Liu L., Zhang Y., Zhou Z., Li C., et al. (2011). Heme Oxygenase-1 Protects Human Melanocytes from H2O2-Induced Oxidative Stress via the Nrf2-ARE Pathway. J. Invest. Dermatol. 131 (7), 1420–1427. 10.1038/jid.2011.56 [DOI] [PubMed] [Google Scholar]
- Jian Z., Li K., Song P., Zhu G., Zhu L., Cui T., et al. (2014). Impaired Activation of the Nrf2-ARE Signaling Pathway Undermines H2O2-Induced Oxidative Stress Response: a Possible Mechanism for Melanocyte Degeneration in Vitiligo. J. Invest. Dermatol. 134 (8), 2221–2230. 10.1038/jid.2014.152 [DOI] [PubMed] [Google Scholar]
- Jiang W., Li S., Chen X., Zhang W., Chang Y., He Y., et al. (2019). Berberine Protects Immortalized Line of Human Melanocytes from H2O2-Induced Oxidative Stress via Activation of Nrf2 and Mitf Signaling Pathway. J. Dermatol. Sci. 94 (1), 236–243. 10.1016/j.jdermsci.2019.03.007 [DOI] [PubMed] [Google Scholar]
- Jiang Z., Li S., Liu Y., Deng P., Huang J., He G. (2011). Sesamin Induces Melanogenesis by Microphthalmia-Associated Transcription Factor and Tyrosinase Up-Regulation via cAMP Signaling Pathway. Acta Biochim. Biophys. Sinica 43 (10), 763–770. 10.1093/abbs/gmr078 [DOI] [PubMed] [Google Scholar]
- Jiang Z., Xu J., Long M., Tu Z., Yang G., He G. (2009). 2, 3, 5, 4'-Tetrahydroxystilbene-2-O-Beta-D-Glucoside (THSG) Induces Melanogenesis in B16 Cells by MAP Kinase Activation and Tyrosinase Upregulation. Life Sci. 85 (9-10), 345–350. 10.1016/j.lfs.2009.05.022 [DOI] [PubMed] [Google Scholar]
- Jie Q., Kodithuwakku N. D., Yuan X., He G., Chen M., Xu S., et al. (2015). Anti-allergic and Anti-inflammatory Properties of a Potent Histamine H1 Receptor Antagonist, Desloratadine Citrate Disodium Injection, and its Anti-inflammatory Mechanism on EA.Hy926 Endothelial Cells. Eur. J. Pharmacol. 754, 1–10. 10.1016/j.ejphar.2015.02.016 [DOI] [PubMed] [Google Scholar]
- Jin Y., Andersen G., Yorgov D., Ferrara T. M., Ben S., Brownson K. M., et al. (2016). Genome-wide Association Studies of Autoimmune Vitiligo Identify 23 New Risk Loci and Highlight Key Pathways and Regulatory Variants. Nat. Genet. 48 (11), 1418–1424. 10.1038/ng.3680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung E., Kim J. H., Kim M. O., Jang S., Kang M., Oh S. W., et al. (2016). Afzelin Positively Regulates Melanogenesis through the P38 MAPK Pathway. Chemico-Biological Interactions 254, 167–172. 10.1016/j.cbi.2016.06.010 [DOI] [PubMed] [Google Scholar]
- Jung G.-D., Yang J.-Y., Song E.-S., Park J.-W. (2001). Stimulation of Melanogenesis by Glycyrrhizin in B16 Melanoma Cells. Exp. Mol. Med. 33 (3), 131–135. 10.1038/emm.2001.23 [DOI] [PubMed] [Google Scholar]
- Kalaiselvi P., Rajashree K., Bharathi Priya L., Padma V. V. (2013). Cytoprotective Effect of Epigallocatechin-3-Gallate against Deoxynivalenol-Induced Toxicity through Anti-oxidative and Anti-inflammatory Mechanisms in HT-29 Cells. Food Chem. Toxicol. 56, 110–118. 10.1016/j.fct.2013.01.042 [DOI] [PubMed] [Google Scholar]
- Katiyar S. K., Matsui M. S., Elmets C. A., Mukhtar H. (1999). Polyphenolic Antioxidant (-)-Epigallocatechin-3-Gallate from Green Tea Reduces UVB-Lnduced Inflammatory Responses and Infiltration of Leukocytes in Human Skin. Photochem. Photobiol. 69 (2), 148–153. 10.1111/j.1751-1097.1999.tb03267.x [DOI] [PubMed] [Google Scholar]
- Kawakami T., Ohgushi A., Hirobe T., Soma Y. (2014). Effects of 1,25-dihydroxyvitamin D3 on Human Epidermal Melanocytes and Melanoblasts. J. Dermatol. Sci. 76 (1), 72–74. 10.1016/j.jdermsci.2014.07.005 [DOI] [PubMed] [Google Scholar]
- Khan H., Marya S., Amin S., Kamal M. A., Patel S. (2018). Flavonoids as Acetylcholinesterase Inhibitors: Current Therapeutic Standing and Future Prospects. Biomed. Pharmacother. 101, 860–870. 10.1016/j.biopha.2018.03.007 [DOI] [PubMed] [Google Scholar]
- Khan N., Mukhtar H. (2015). Dietary Agents for Prevention and Treatment of Lung Cancer. Cancer Lett. 359 (2), 155–164. 10.1016/j.canlet.2015.01.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H. J., Kim J. S., Woo J.-T., Lee I.-S., Cha B.-Y. (2015). Hyperpigmentation Mechanism of Methyl 3,5-Di-Caffeoylquinate through Activation of P38 and MITF Induction of Tyrosinase. Acta Biochim. Biophys. Sin 47 (7), 548–556. 10.1093/abbs/gmv040 [DOI] [PubMed] [Google Scholar]
- Kim J.-K., Jang H.-D. (2016). 6-shogaol Attenuates H2O2-Induced Oxidative Stress via Upregulation of Nrf2-Mediated γ-glutamylcysteine Synthetase and Heme Oxygenase Expression in HepG2 Cells. Food Sci. Biotechnol. 25 (1), 319–327. 10.1007/s10068-016-0045-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J. K., Kim Y. S., Kim Y., Uddin M. R., Kim Y. B., Kim H. H., et al. (2014). Comparative Analysis of Flavonoids and Polar Metabolites from Hairy Roots of Scutellaria Baicalensis and Scutellaria Lateriflora. World J. Microbiol. Biotechnol. 30 (3), 887–892. 10.1007/s11274-013-1498-7 [DOI] [PubMed] [Google Scholar]
- Kim S. K., Kim H. J., Choi S. E., Park K. H., Choi H. K., Lee M. W. (2008). Anti-oxidative and Inhibitory Activities on Nitric Oxide (NO) and Prostaglandin E2 (COX-2) Production of Flavonoids from Seeds of Prunus Tomentosa Thunberg. Arch. Pharm. Res. 31 (4), 424–428. 10.1007/s12272-001-1174-9 [DOI] [PubMed] [Google Scholar]
- Kou X., Wang X., Ji R., Liu L., Qiao Y., Lou Z., et al. (2018). Occurrence, Biological Activity and Metabolism of 6-shogaol. Food Funct. 9 (3), 1310–1327. 10.1039/c7fo01354j [DOI] [PubMed] [Google Scholar]
- Kwon S.-J., Kim Y.-M., Jang H.-J., Seo Y.-K. (2018). Synergistic Effect of rice Bran Extract and Extremely Low-Frequency Electromagnetic fields on Dermal Papilla/melanocytes in Melanogenesis. Bioelectromagnetics 39 (8), 595–603. 10.1002/bem.22151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai Y., Feng Q., Zhang R., Shang J., Zhong H. (2021). The Great Capacity on Promoting Melanogenesis of Three Compatible Components in Vernonia Anthelmintica (L.) Willd. Int. J. Mol. Sci. 22 (8). 10.3390/ijms22084073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latham C. M., Brightwell C. R., Keeble A. R., Munson B. D., Thomas N. T., Zagzoog A. M., et al. (2021). Vitamin D Promotes Skeletal Muscle Regeneration and Mitochondrial Health. Front. Physiol. 12, 660498. 10.3389/fphys.2021.660498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau K. M., Yue G. G., Chan Y. Y., Kwok H. F., Gao S., Wong C. W., et al. (2019). A Review on the Immunomodulatory Activity of Acanthopanax Senticosus and its Active Components. Chin. Med. 14, 25. 10.1186/s13020-019-0250-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J., Jung E., Park J., Jung K., Park E., Kim J., et al. (2005). Glycyrrhizin Induces Melanogenesis by Elevating a cAMP Level in B16 Melanoma Cells. J. Invest. Dermatol. 124 (2), 405–411. 10.1111/j.0022-202x.2004.23606.x [DOI] [PubMed] [Google Scholar]
- Lee J., Kim Y. S., Park D. (2007). Rosmarinic Acid Induces Melanogenesis through Protein Kinase A Activation Signaling. Biochem. Pharmacol. 74 (7), 960–968. 10.1016/j.bcp.2007.06.007 [DOI] [PubMed] [Google Scholar]
- Lee S., So Y.-J., Shin M., Cho J., Lee J. (2014). Antibacterial Effects of Afzelin Isolated from Cornus Macrophylla on Pseudomonas aeruginosa, a Leading Cause of Illness in Immunocompromised Individuals. Molecules 19 (3), 3173–3180. 10.3390/molecules19033173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S. Y. (2018). Synergistic Effect of Maclurin on Ginsenoside Compound K Induced Inhibition of the Transcriptional Expression of Matrix Metalloproteinase-1 in HaCaT Human Keratinocyte Cells. J. Ginseng Res. 42 (2), 229–232. 10.1016/j.jgr.2017.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Y. J., Jung O., Lee J., Son J., Cho J. Y., Ryou C., et al. (2018). Maclurin Exerts Anti-cancer Effects on PC3 Human Prostate Cancer Cells via Activation of P38 and Inhibitions of JNK, FAK, AKT, and C-Myc Signaling Pathways. Nutr. Res. 58, 62–71. 10.1016/j.nutres.2018.07.003 [DOI] [PubMed] [Google Scholar]
- Legrand G., Delporte M., Khelifi C., Harant A., Vuylsteker C., Mörchen M., et al. (2016). Identification and Characterization of Five BAHD Acyltransferases Involved in Hydroxycinnamoyl Ester Metabolism in Chicory. Front. Plant Sci. 7, 741. 10.3389/fpls.2016.00741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li B., Pinch H., Birt D. R. (1996). Influence of Vehicle, Distant Topical Delivery, and Biotransformation on the Chemopreventive Activity of Apigenin, a Plant Flavonoid, in Mouse Skin. Pharm. Res. 13 (10), 1530–1534. 10.1023/a:1016083613916 [DOI] [PubMed] [Google Scholar]
- Li G.-H., Fang K.-L., Yang K., Cheng X.-P., Wang X.-N., Shen T., et al. (2021a). Thesium Chinense Turcz.: An Ethnomedical, Phytochemical and Pharmacological Review. J. Ethnopharmacology 273, 113950. 10.1016/j.jep.2021.113950 [DOI] [PubMed] [Google Scholar]
- Li J., Ren S., Li M., Bi J., Yang G., Li E. (2021b). Paeoniflorin Protects against Dextran Sulfate Sodium (DSS)-induced Colitis in Mice through Inhibition of Inflammation and Eosinophil Infiltration. Int. Immunopharmacology 97, 107667. 10.1016/j.intimp.2021.107667 [DOI] [PubMed] [Google Scholar]
- Li R., Zhao D., Qu R., Fu Q., Ma S. (2015). The Effects of Apigenin on Lipopolysaccharide-Induced Depressive-like Behavior in Mice. Neurosci. Lett. 594, 17–22. 10.1016/j.neulet.2015.03.040 [DOI] [PubMed] [Google Scholar]
- Li X.-S., Tang X.-Y., Su W., Li X. (2020). Vitexin Protects Melanocytes from Oxidative Stress via Activating MAPK-Nrf2/ARE Pathway. Immunopharmacology and Immunotoxicology 42 (6), 594–603. 10.1080/08923973.2020.1835952 [DOI] [PubMed] [Google Scholar]
- Lim H., Park H., Kim H. P. (2015). Effects of Flavonoids on Senescence-Associated Secretory Phenotype Formation from Bleomycin-Induced Senescence in BJ Fibroblasts. Biochem. Pharmacol. 96 (4), 337–348. 10.1016/j.bcp.2015.06.013 [DOI] [PubMed] [Google Scholar]
- Lin M., Lu S.-s., Wang A.-x., Qi X.-y., Zhao D., Wang Z.-h., et al. (2011a). Apigenin Attenuates Dopamine-Induced Apoptosis in Melanocytes via Oxidative Stress-Related P38, C-Jun NH2-terminal Kinase and Akt Signaling. J. Dermatol. Sci. 63 (1), 10–16. 10.1016/j.jdermsci.2011.03.007 [DOI] [PubMed] [Google Scholar]
- Lin T. Y., Wu P. Y., Hou C. W., Chien T. Y., Chang Q. X., Wen K. C., et al. (2019). Protective Effects of Sesamin against UVB-Induced Skin Inflammation and Photodamage In Vitro and In Vivo . Biomolecules 9 (9). 10.3390/biom9090479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Y.-L., Lu C.-K., Huang Y.-J., Chen H.-J. (2011b). Antioxidative Caffeoylquinic Acids and Flavonoids from Hemerocallis Fulva Flowers. J. Agric. Food Chem. 59 (16), 8789–8795. 10.1021/jf201166b [DOI] [PubMed] [Google Scholar]
- Ling Y., Gong Q., Xiong X., Sun L., Zhao W., Zhu W., et al. (2017). Protective Effect of Madecassoside on H2O2-Induced Oxidative Stress and Autophagy Activation in Human Melanocytes. Oncotarget 8 (31), 51066–51075. 10.18632/oncotarget.17654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu B., Jian Z., Li Q., Li K., Wang Z., Liu L., et al. (2012). Baicalein Protects Human Melanocytes from H2O2-Induced Apoptosis via Inhibiting Mitochondria-dependent Caspase Activation and the P38 MAPK Pathway. Free Radic. Biol. Med. 53 (2), 183–193. 10.1016/j.freeradbiomed.2012.04.015 [DOI] [PubMed] [Google Scholar]
- Liu R., Ji P., Liu B., Qiao H., Wang X., Zhou L., et al. (2017). Apigenin Enhances the Cisplatin Cytotoxic Effect through P53-Modulated Apoptosis. Oncol. Lett. 13 (2), 1024–1030. 10.3892/ol.2016.5495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Qiu Y., Chen Q., Han X., Cai M., Hao L. (2021a). Puerarin Suppresses the Hepatic Gluconeogenesis via Activation of PI3K/Akt Signaling Pathway in Diabetic Rats and HepG2 Cells. Biomed. Pharmacother. 137, 111325. 10.1016/j.biopha.2021.111325 [DOI] [PubMed] [Google Scholar]
- Liu Y., Wang H., Yang M., Liu N., Zhao Y., Qi X., et al. (2018). Cistanche Deserticola Polysaccharides Protects PC12 Cells against OGD/RP-induced Injury. Biomed. Pharmacother. 99, 671–680. 10.1016/j.biopha.2018.01.114 [DOI] [PubMed] [Google Scholar]
- Liu Z. Q., Yao G. L., Zhai J. M., Hu D. W., Fan Y. G. (2021b). Kaempferol Suppresses Proliferation and Induces Apoptosis and DNA Damage in Human Gallbladder Cancer Cells through the CDK4/CDK6/cyclin D1 Pathway. Eur. Rev. Med. Pharmacol. Sci. 25 (3), 1311–1321. [DOI] [PubMed] [Google Scholar]
- Long X., Zeng X., Yan H., Xu M., Zeng Q., Xu C., et al. (2021). Flavonoids Composition and Antioxidant Potential Assessment of Extracts from Gannanzao Navel Orange (Citrus Sinensis Osbeck Cv. Gannanzao) Peel. Nat. Product. Res. 35 (4), 702–706. 10.1080/14786419.2019.1593162 [DOI] [PubMed] [Google Scholar]
- Lotito S., Frei B. (2006). Consumption of Flavonoid-Rich Foods and Increased Plasma Antioxidant Capacity in Humans: Cause, Consequence, or Epiphenomenon?. Free Radic. Biol. Med. 41 (12), 1727–1746. 10.1016/j.freeradbiomed.2006.04.033 [DOI] [PubMed] [Google Scholar]
- Lu W., Zhao Y., Kong Y., Zhang W., Ma W., Li W., et al. (2018). Geniposide Prevents H2 O2 -induced Oxidative Damage in Melanocytes by Activating the PI3K-Akt Signalling Pathway. Clin. Exp. Dermatol. 43 (6), 667–674. 10.1111/ced.13409 [DOI] [PubMed] [Google Scholar]
- Ma J., Li S., Zhu L., Guo S., Yi X., Cui T., et al. (2018). Baicalein Protects Human Vitiligo Melanocytes from Oxidative Stress through Activation of NF-E2-Related Factor2 (Nrf2) Signaling Pathway. Free Radic. Biol. Med. 129, 492–503. 10.1016/j.freeradbiomed.2018.10.421 [DOI] [PubMed] [Google Scholar]
- Ma Y. L., Zhao F., Yin J. T., Liang C. J., Niu X. L., Qiu Z. H., et al. (2019). Two Approaches for Evaluating the Effects of Galangin on the Activities and mRNA Expression of Seven CYP450. Molecules 24 (6), 1171. 10.3390/molecules24061171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maimaiti Z., Turak A., Aisa H. A. (2017). Two New Compounds from the Seeds of Vernonia Anthelmintica. J. Asian Nat. Prod. Res. 19 (9), 862–868. 10.1080/10286020.2016.1269760 [DOI] [PubMed] [Google Scholar]
- Majnooni M. B., Fakhri S., Shokoohinia Y., Mojarrab M., Kazemi-Afrakoti S., Farzaei M. H. (2020). Isofraxidin: Synthesis, Biosynthesis, Isolation, Pharmacokinetic and Pharmacological Properties. Molecules 25 (9), 2040. 10.3390/molecules25092040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maleš Ž., Drvar D. L., Duka I., Žužul K. (2019). Application of Medicinal Plants in Several Dermatovenerological Entities. Acta Pharm. 69 (4), 525–531. [DOI] [PubMed] [Google Scholar]
- Mamat N., Lu X. Y., Kabas M., Aisa H. A. (2018). Potential Anti-vitiligo Properties of Cynarine Extracted from Vernonia Anthelmintica (L.) Willd. Int. J. Mol. Med. 42 (5), 2665–2675. 10.3892/ijmm.2018.3861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamat N., Dou J., Lu X., Eblimit A., Haji Akber A. (2017). Isochlorogenic Acid A Promotes Melanin Synthesis in B16 Cell through the β-catenin Signal Pathway. Acta Biochim. Biophys. Sin (Shanghai) 49 (9), 800–807. 10.1093/abbs/gmx072 [DOI] [PubMed] [Google Scholar]
- Mechoulam R., Hanus L. (2002). Cannabidiol: an Overview of Some Chemical and Pharmacological Aspects. Part I: Chemical Aspects. Chem. Phys. Lipids 121 (1-2), 35–43. 10.1016/s0009-3084(02)00144-5 [DOI] [PubMed] [Google Scholar]
- Meng Y., Liu Z., Zhai C., Di T., Zhang L., Zhang L., et al. (2019). Paeonol Inhibits the Development of 1-chloro-2,4-dinitrobenzene-induced A-topic D-ermatitis via M-ast and T C-ells in BALB/c M-ice. Mol. Med. Rep. 19 (4), 3217–3229. 10.3892/mmr.2019.9985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng Y., Wang M., Xie X., Di T., Zhao J., Lin Y., et al. (2017). Paeonol Ameliorates Imiquimod-Induced Psoriasis-like Skin Lesions in BALB/c Mice by Inhibiting the Maturation and Activation of Dendritic Cells. Int. J. Mol. Med. 39 (5), 1101–1110. 10.3892/ijmm.2017.2930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mereles D., Hunstein W. (2011). Epigallocatechin-3-gallate (EGCG) for Clinical Trials: More Pitfalls Than Promises?. Ijms 12 (9), 5592–5603. 10.3390/ijms12095592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mi Moon K., Young Kim C., Yeul Ma J., Lee B. (2019). Xanthone-related Compounds as an Anti-browning and Antioxidant Food Additive. Food Chem. 274, 345–350. 10.1016/j.foodchem.2018.08.144 [DOI] [PubMed] [Google Scholar]
- Miao J., Zhong J., Lan J., Ye S., Ye P., Li S., et al. (2021). Paeonol Attenuates Inflammation by Confining HMGB1 to the Nucleus. J. Cel Mol Med 25 (6), 2885–2899. 10.1111/jcmm.16319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miguel S., Legrand G., Duriot L., Delporte M., Menin B., Michel C., et al. (2020). A GDSL Lipase-like from Ipomoea Batatas Catalyzes Efficient Production of 3,5-diCQA when Expressed in Pichia pastoris. Commun. Biol. 3 (1), 673. 10.1038/s42003-020-01488-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molagoda I. M. N., Karunarathne W., Park S. R., Choi Y. H., Park E. K., Jin C. Y., et al. (2020). GSK-3beta-Targeting Fisetin Promotes Melanogenesis in B16F10 Melanoma Cells and Zebrafish Larvae through Beta-Catenin Activation. Int. J. Mol. Sci. 21 (1). 10.3390/ijms21010312 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Monteiro É., Chibli L., Yamamoto C., Pereira M., Vilela F., Rodarte M., et al. (2014). Antinociceptive and Anti-inflammatory Activities of the Sesame Oil and Sesamin. Nutrients 6 (5), 1931–1944. 10.3390/nu6051931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreira C. G., Horinouchi C. D. S., Souza-Filho C. S., Campos F. R., Barison A., Cabrini D. A., et al. (2012). Hyperpigmentant Activity of Leaves and Flowers Extracts of Pyrostegia venusta on Murine B16F10 Melanoma. J. Ethnopharmacology 141 (3), 1005–1011. 10.1016/j.jep.2012.03.047 [DOI] [PubMed] [Google Scholar]
- Mou K., Pan W., Han D., Wen X., Cao F., Miao Y., et al. (2019). Glycyrrhizin Protects Human Melanocytes from H2O2-induced O-xidative D-amage via the Nrf2-dependent I-nduction of HO-1. Int. J. Mol. Med. 44 (1), 253–261. 10.3892/ijmm.2019.4200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mou K. H., Han D., Liu W. L., Li P. (2016). Combination Therapy of Orally Administered Glycyrrhizin and UVB Improved Active-Stage Generalized Vitiligo. Braz. J. Med. Biol. Res. 49 (8). 10.1590/1414-431x20165354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mou S. Q., Zhou Z. Y., Feng H., Zhang N., Lin Z., Aiyasiding X., et al. (2021). Liquiritin Attenuates Lipopolysaccharides-Induced Cardiomyocyte Injury via an AMP-Activated Protein Kinase-dependent Signaling Pathway. Front. Pharmacol. 12, 648688. 10.3389/fphar.2021.648688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagata H., Takekoshi S., Takeyama R., Homma T., Yoshiyuki Osamura R. (2004). Quercetin Enhances Melanogenesis by Increasing the Activity and Synthesis of Tyrosinase in Human Melanoma Cells and in normal Human Melanocytes. Pigment Cel Res 17 (1), 66–73. 10.1046/j.1600-0749.2003.00113.x [DOI] [PubMed] [Google Scholar]
- Nasr M., Al-Karaki R. (2020). Nanotechnological Innovations Enhancing the Topical Therapeutic Efficacy of Quercetin: A Succinct Review. Cdd 17 (4), 270–278. 10.2174/1567201817666200317123224 [DOI] [PubMed] [Google Scholar]
- Nguyen D.-V., Li F., Li H., Wong B. S., Low C. Y., Liu X.-Y., et al. (2015). Drug Permeation through Skin Is Inversely Correlated with Carrier Gel Rigidity. Mol. Pharmaceutics 12 (2), 444–452. 10.1021/mp500542a [DOI] [PubMed] [Google Scholar]
- Ning W., Wang S., Dong X., Liu D., Fu L., Jin R., et al. (2015). Epigallocatechin-3-gallate (EGCG) Suppresses the Trafficking of Lymphocytes to Epidermal Melanocytes via Inhibition of JAK2: Its Implication for Vitiligo Treatment. Biol. Pharm. Bull. 38 (11), 1700–1706. 10.1248/bpb.b15-00331 [DOI] [PubMed] [Google Scholar]
- Niu C., Aisa H. A. (2017). Upregulation of Melanogenesis and Tyrosinase Activity: Potential Agents for Vitiligo. Molecules 22 (8), 1303. 10.3390/molecules22081303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niu C., Pang G. X., Li G., Dou J., Nie L. F., Himit H., et al. (2016). Synthesis and Biological Evaluation of Furocoumarin Derivatives on Melanin Synthesis in Murine B16 Cells for the Treatment of Vitiligo. Bioorg. Med. Chem. 24 (22), 5960–5968. 10.1016/j.bmc.2016.09.056 [DOI] [PubMed] [Google Scholar]
- Ohguchi K., Akao Y., Nozawa Y. (2006). Stimulation of Melanogenesis by the Citrus Flavonoid Naringenin in Mouse B16 Melanoma Cells. Biosci. Biotechnol. Biochem. 70 (6), 1499–1501. 10.1271/bbb.50635 [DOI] [PubMed] [Google Scholar]
- Ożarowski M., Karpiński T. M. (2020). Extracts and Flavonoids of Passiflora Species as Promising Anti-inflammatory and Antioxidant Substances. Curr. Pharm. Des. 10.2174/1381612826666200526150113 [DOI] [PubMed] [Google Scholar]
- Park W.-s., Kwon O., Yoon T.-J., Chung J. H. (2014). Anti-graying Effect of the Extract of Pueraria Thunbergiana via Upregulation of cAMP/MITF-M Signaling Pathway. J. Dermatol. Sci. 75 (2), 153–155. 10.1016/j.jdermsci.2014.05.003 [DOI] [PubMed] [Google Scholar]
- Pastorino G., Cornara L., Soares S., Rodrigues F., Oliveira M. B. P. P. (2018). Liquorice (Glycyrrhiza Glabra ): A Phytochemical and Pharmacological Review. Phytotherapy Res. 32 (12), 2323–2339. 10.1002/ptr.6178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel D., Shukla S., Gupta S. (2007). Apigenin and Cancer Chemoprevention: Progress, Potential and Promise (Review). Int. J. Oncol. 30 (1), 233–245. 10.3892/ijo.30.1.233 [DOI] [PubMed] [Google Scholar]
- Patel S., Rauf A., Khan H., Meher B. R., Hassan S. S. U. (2017). A Holistic Review on the Autoimmune Disease Vitiligo with Emphasis on the Causal Factors. Biomed. Pharmacother. 92, 501–508. 10.1016/j.biopha.2017.05.095 [DOI] [PubMed] [Google Scholar]
- Pathak N., Rai A. K., Kumari R., Bhat K. V. (2014). Value Addition in Sesame: A Perspective on Bioactive Components for Enhancing Utility and Profitability. Pharmacogn Rev. 8 (16), 147–155. 10.4103/0973-7847.134249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paudel K. S., Hammell D. C., Agu R. U., Valiveti S., Stinchcomb A. L. (2010). Cannabidiol Bioavailability after Nasal and Transdermal Application: Effect of Permeation Enhancers. Drug Develop. Ind. Pharm. 36 (9), 1088–1097. 10.3109/03639041003657295 [DOI] [PubMed] [Google Scholar]
- Pei T., Zheng C., Huang C., Chen X., Guo Z., Fu Y., et al. (2016). Systematic Understanding the Mechanisms of Vitiligo Pathogenesis and its Treatment by Qubaibabuqi Formula. J. Ethnopharmacology 190, 272–287. 10.1016/j.jep.2016.06.001 [DOI] [PubMed] [Google Scholar]
- Peng L. Y., Shi H. T., Yuan M., Li J. H., Song K., Huang J. N., et al. (2020). Madecassoside Protects against LPS-Induced Acute Lung Injury via Inhibiting TLR4/NF-Κb Activation and Blood-Air Barrier Permeability. Front. Pharmacol. 11, 807. 10.3389/fphar.2020.00807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez-Sánchez A., Barrajón-Catalán E., Herranz-López M., Castillo J., Micol V. (2016). Lemon Balm Extract ( Melissa Officinalis , L.) Promotes Melanogenesis and Prevents UVB-Induced Oxidative Stress and DNA Damage in a Skin Cell Model. J. Dermatol. Sci. 84 (2), 169–177. 10.1016/j.jdermsci.2016.08.004 [DOI] [PubMed] [Google Scholar]
- Pillaiyar T., Manickam M., Jung S.-H. (2017). Recent Development of Signaling Pathways Inhibitors of Melanogenesis. Cell Signal. 40, 99–115. 10.1016/j.cellsig.2017.09.004 [DOI] [PubMed] [Google Scholar]
- Preziuso F., Genovese S., Marchetti L., Sharifi-Rad M., Palumbo L., Epifano F., et al. (2020). 7-Isopentenyloxycoumarin: What Is New across the Last Decade. Molecules 25 (24), 5923. 10.3390/molecules25245923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramful D., Bahorun T., Bourdon E., Tarnus E., Aruoma O. I. (2010). Bioactive Phenolics and Antioxidant Propensity of Flavedo Extracts of Mauritian Citrus Fruits: Potential Prophylactic Ingredients for Functional Foods Application. Toxicology 278 (1), 75–87. 10.1016/j.tox.2010.01.012 [DOI] [PubMed] [Google Scholar]
- Rashighi M., Agarwal P., Richmond J. M., Harris T. H., Dresser K., Su M.-W., et al. (2014). CXCL10 Is Critical for the Progression and Maintenance of Depigmentation in a Mouse Model of Vitiligo. Sci. Translational Med. 6 (223), 223ra23. 10.1126/scitranslmed.3007811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rauf A., Imran M., Khan I. A., Ur-Rehman M., Gilani S. A., Mehmood Z., et al. (2018). Anticancer Potential of Quercetin: A Comprehensive Review. Phytotherapy Res. 32 (11), 2109–2130. 10.1002/ptr.6155 [DOI] [PubMed] [Google Scholar]
- Riding R. L., Richmond J. M., Harris J. E. (2019). Mouse Model for Human Vitiligo. Curr. Protoc. Immunol. 124 (1), e63. 10.1002/cpim.63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodrigues M., Ezzedine K., Hamzavi I., Pandya A. G., Harris J. E. (2017). New Discoveries in the Pathogenesis and Classification of Vitiligo. J. Am. Acad. Dermatol. 77 (1), 1–13. 10.1016/j.jaad.2016.10.048 [DOI] [PubMed] [Google Scholar]
- Salehi B., Fokou P. V. T., Sharifi-Rad M., Zucca P., Pezzani R., Martins N., et al. (2019). The Therapeutic Potential of Naringenin: A Review of Clinical Trials. Pharmaceuticals (Basel) 12 (1), 11. 10.3390/ph12010011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satthakarn S., Hladik F., Promsong A., Nittayananta W. (2015). Vaginal Innate Immune Mediators Are Modulated by a Water Extract of Houttuynia Cordata Thunb. BMC Complement. Altern. Med. 15, 183. 10.1186/s12906-015-0701-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seneschal J., Boniface K., D’Arino A., Picardo M. (2021). An Update on Vitiligo Pathogenesis. Pigment Cel Melanoma Res. 34 (2), 236–243. 10.1111/pcmr.12949 [DOI] [PubMed] [Google Scholar]
- Serafino A., Sinibaldi Vallebona P., Lazzarino G., Tavazzi B., Rasi G., Pierimarchi P., et al. (2004). Differentiation of Human Melanoma Cells Induced by Cyanidin‐3‐ O ‐β‐glucopyranoside. FASEB j. 18 (15), 1940–1942. 10.1096/fj.04-1925fje [DOI] [PubMed] [Google Scholar]
- Shan M., Yu S., Yan H., Guo S., Xiao W., Wang Z., et al. (2017). A Review on the Phytochemistry, Pharmacology, Pharmacokinetics and Toxicology of Geniposide, a Natural Product. Molecules 22 (10), 1689. 10.3390/molecules22101689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharifi-Rad J., Kamiloglu S., Yeskaliyeva B., Beyatli A., Alfred M. A., Salehi B., et al. (2020). Pharmacological Activities of Psoralidin: A Comprehensive Review of the Molecular Mechanisms of Action. Front. Pharmacol. 11, 571459. 10.3389/fphar.2020.571459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi M., Zhang Y., Song M., Sun Y., Li C., Kang W. (2018). Screening the Marker Components in Psoralea Corylifolia L. With the Aids of Spectrum-Effect Relationship and Component Knock-Out by UPLC-MS(2). Int. J. Mol. Sci. 19 (11), 3439. 10.3390/ijms19113439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin S., Ko J., Kim M., Song N., Park K. (2021). Morin Induces Melanogenesis via Activation of MAPK Signaling Pathways in B16F10 Mouse Melanoma Cells. Molecules 26 (8), 2150. 10.3390/molecules26082150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin S. W., Jung E., Kim S., Kim J. H., Kim E. G., Lee J., et al. (2013). Antagonizing Effects and Mechanisms of Afzelin against UVB-Induced Cell Damage. PLoS One 8 (4), e61971. 10.1371/journal.pone.0061971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shomirzoeva O., Li J., Numonov S., Mamat N., Shataer D., Lu X., et al. (2019). Chemical Components of Hyssopus Seravshanicus: Antioxidant Activity, Activations of Melanogenesis and Tyrosinase, and Quantitative Determination by UPLC-DAD. Nat. Product. Res. 33 (6), 866–870. 10.1080/14786419.2017.1408105 [DOI] [PubMed] [Google Scholar]
- Shon M.-S., Kim R.-H., Kwon O. J., Roh S.-S., Kim G.-N. (2016). Beneficial Role and Function of Fisetin in Skin Health via Regulation of the CCN2/TGF-β Signaling Pathway. Food Sci. Biotechnol. 25 (S1), 133–141. 10.1007/s10068-016-0110-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shukla S., Gupta S. (2010). Apigenin: a Promising Molecule for Cancer Prevention. Pharm. Res. 27 (6), 962–978. 10.1007/s11095-010-0089-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva M. L. A., Coímbra H. S., Pereira A. C., Almeida V. A., Lima T. C., Costa E. S., et al. (2007). Evaluation of Piper Cubeba Extract, (-)-cubebin and its Semi-synthetic Derivatives against Oral Pathogens. Phytother. Res. 21 (5), 420–422. 10.1002/ptr.2088 [DOI] [PubMed] [Google Scholar]
- Singh B., Singh J. P., Kaur A., Singh N. (2020). Phenolic Composition, Antioxidant Potential and Health Benefits of Citrus Peel. Food Res. Int. 132, 109114. 10.1016/j.foodres.2020.109114 [DOI] [PubMed] [Google Scholar]
- Sinha R., Srivastava S., Joshi A., Joshi U. J., Govil G. (2014). In-vitro Anti-proliferative and Anti-oxidant Activity of Galangin, Fisetin and Quercetin: Role of Localization and Intermolecular Interaction in Model Membrane. Eur. J. Med. Chem. 79, 102–109. 10.1016/j.ejmech.2014.04.002 [DOI] [PubMed] [Google Scholar]
- Sintov A. C., Yarmolinsky L., Dahan A., Ben-Shabat S. (2014). Pharmacological Effects of Vitamin D and its Analogs: Recent Developments. Drug Discov. Today 19 (11), 1769–1774. 10.1016/j.drudis.2014.06.008 [DOI] [PubMed] [Google Scholar]
- Skiba M. A., Szendzielorz K., Mazur B., Król W. (2016). The Inhibitory Effect of Flavonoids on Interleukin-8 Release by Human Gastric Adenocarcinoma (AGS) Cells Infected with Cag PAI (+) Helicobacter pylori . cejoi 3 (3), 229–235. 10.5114/ceji.2016.63119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somani G. S., Nahire M. S., Parikh A. D., Mulik M. B., Ghumatkar P. J., Laddha K. S., et al. (2017). Neuroprotective Effect of Cubebin: A Dibenzylbutyrolactone Lignan on Scopolamine-Induced Amnesia in Mice. Indian J. Med. Res. 146 (2), 255–259. 10.4103/ijmr.IJMR_156_14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Souza G. H. B., da Silva Filho A. A., de Souza V. A., Pereira A. C., de A. Royo V., e Silva M. L. A., et al. (2004). Analgesic and Anti-inflammatory Activities Evaluation of (-)-O-Acetyl, (-)-O-Methyl, (-)-O-Dimethylethylamine Cubebin and Their Preparation from (-)-cubebin. Il Farmaco 59 (1), 55–61. 10.1016/j.farmac.2003.07.012 [DOI] [PubMed] [Google Scholar]
- Speeckaert R., Dugardin J., Lambert J., Lapeere H., Verhaeghe E., Speeckaert M. M., et al. (2018). Critical Appraisal of the Oxidative Stress Pathway in Vitiligo: a Systematic Review and Meta-Analysis. J. Eur. Acad. Dermatol. Venereol. 32 (7), 1089–1098. 10.1111/jdv.14792 [DOI] [PubMed] [Google Scholar]
- Speeckaert R., Lambert J., Bulat V., Belpaire A., Speeckaert M., van Geel N. (2020). Autoimmunity in Segmental Vitiligo. Front. Immunol. 11, 568447. 10.3389/fimmu.2020.568447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subongkot T., Ngawhirunpat T., Opanasopit P. (2021). Development of Ultradeformable Liposomes with Fatty Acids for Enhanced Dermal Rosmarinic Acid Delivery. Pharmaceutics 13 (3), 404. 10.3390/pharmaceutics13030404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun C., Huang H., Xu C., Li X., Chen K. (2013). Biological activities of extracts from Chinese bayberry (Myrica rubra Sieb. et Zucc.): a review. Plant Foods Hum. Nutr. 68 (2), 97–106. 10.1007/s11130-013-0349-x [DOI] [PubMed] [Google Scholar]
- Sun Z., Du J., Hwang E., Yi T.-H. (2018). Paeonol Extracted from Paeonia Suffruticosa Andr. Ameliorated UVB-Induced Skin Photoaging via DLD/Nrf2/ARE and MAPK/AP-1 Pathway. Phytotherapy Res. 32 (9), 1741–1749. 10.1002/ptr.6100 [DOI] [PubMed] [Google Scholar]
- Takekoshi S., Nagata H., Kitatani K. (2014). Flavonoids Enhance Melanogenesis in Human Melanoma Cells. Tokai J. Exp. Clin. Med. 39 (3), 116–121. [PubMed] [Google Scholar]
- Tal B., Robeson D. J. (1986). The Metabolism of Sunflower Phytoalexins Ayapin and Scopoletin. Plant Physiol. 82 (1), 167–172. 10.1104/pp.82.1.167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang L., Fang W., Lin J., Li J., Wu W., Xu J. (2018). Vitamin D Protects Human Melanocytes against Oxidative Damage by Activation of Wnt/β-Catenin Signaling. Lab. Invest. 98 (12), 1527–1537. 10.1038/s41374-018-0126-4 [DOI] [PubMed] [Google Scholar]
- Tsai C. F., Su H. H., Chen K. M., Liao J. M., Yao Y. T., Chen Y. H., et al. (2020). Paeonol Protects against Myocardial Ischemia/Reperfusion-Induced Injury by Mediating Apoptosis and Autophagy Crosstalk. Front. Pharmacol. 11, 586498. 10.3389/fphar.2020.586498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuerxuntayi A., Liu Y. Q., Tulake A., Kabas M., Eblimit A., Aisa H. A. (2014). Kaliziri Extract Upregulates Tyrosinase, TRP-1, TRP-2 and MITF Expression in Murine B16 Melanoma Cells. BMC Complement. Altern. Med. 14, 166. 10.1186/1472-6882-14-166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Udomruk S., Kaewmool C., Phitak T., Pothacharoen P., Kongtawelert P. (2020). Sesamin Promotes Neurite Outgrowth under Insufficient Nerve Growth Factor Condition in PC12 Cells through ERK1/2 Pathway and SIRT1 Modulation. Evid. Based Complement. Alternat Med. 2020, 9145458. 10.1155/2020/9145458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usman H., Ullah M. A., Jan H., Siddiquah A., Drouet S., Anjum S., et al. (2020). Interactive Effects of Wide-Spectrum Monochromatic Lights on Phytochemical Production, Antioxidant and Biological Activities of Solanum Xanthocarpum Callus Cultures. Molecules 25 (9), 2201. 10.3390/molecules25092201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uto T., Ohta T., Yamashita A., Fujii S., Shoyama Y. (2019). Liquiritin and Liquiritigenin Induce Melanogenesis via Enhancement of P38 and PKA Signaling Pathways. Medicines 6 (2), 68. 10.3390/medicines6020068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang G., Hiramoto K., Ma N., Yoshikawa N., Ohnishi S., Murata M., et al. (2021a). Glycyrrhizin Attenuates Carcinogenesis by Inhibiting the Inflammatory Response in a Murine Model of Colorectal Cancer. Int. J. Mol. Sci. 22 (5), 2609. 10.3390/ijms22052609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H. X., Zeng M. S., Ye Y., Liu J. Y., Xu P. P. (2021b). Antiviral Activity of Puerarin as Potent Inhibitor of Influenza Virus Neuraminidase. Phytotherapy Res. 35 (1), 324–336. 10.1002/ptr.6803 [DOI] [PubMed] [Google Scholar]
- Wang J., Wang S., Sun S., Lu Y., Gao K., Guo C., et al. (2020a). Apigenin-7-O-β-D-(-6"-p-coumaroyl)-glucopyranoside Treatment Elicits a Neuroprotective Effect through GSK-3β Phosphorylation-Mediated Nrf2 Activation. Aging 12 (23), 23872–23888. 10.18632/aging.104050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J. Y., Chen H., Wang Y. Y., Wang X. Q., Chen H. Y., Zhang M., et al. (2017). Network Pharmacological Mechanisms of Vernonia Anthelmintica (L.) in the Treatment of Vitiligo: Isorhamnetin Induction of Melanogenesis via Up-Regulation of Melanin-Biosynthetic Genes. BMC Syst. Biol. 11 (1), 103. 10.1186/s12918-017-0486-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L., Yang H., Wang C., Shi X., Li K. (2019a). Rosmarinic Acid Inhibits Proliferation and Invasion of Hepatocellular Carcinoma Cells SMMC 7721 via PI3K/AKT/mTOR Signal Pathway. Biomed. Pharmacother. 120, 109443. 10.1016/j.biopha.2019.109443 [DOI] [PubMed] [Google Scholar]
- Wang X., Yu J.-y., Sun Y., Wang H., Shan H., Wang S. (2021c). Baicalin Protects LPS-Induced Blood-Brain Barrier Damage and Activates Nrf2-Mediated Antioxidant Stress Pathway. Int. Immunopharmacology 96, 107725. 10.1016/j.intimp.2021.107725 [DOI] [PubMed] [Google Scholar]
- Wang Y.-F., Liu Y.-N., Xiong W., Yan D.-M., Zhu Y., Gao X.-M., et al. (2014). A UPLC-MS/MS Method for In Vivo and In Vitro Pharmacokinetic Studies of Psoralenoside, Isopsoralenoside, Psoralen and Isopsoralen from Psoralea Corylifolia Extract. J. Ethnopharmacology 151 (1), 609–617. 10.1016/j.jep.2013.11.013 [DOI] [PubMed] [Google Scholar]
- Wang Y.-s., Cho J.-G., Hwang E.-S., Yang J.-E., Gao W., Fang M.-z., et al. (2018). Enhancement of Protective Effects of Radix Scutellariae on UVB-Induced Photo Damage in Human HaCaT Keratinocytes. Appl. Biochem. Biotechnol. 184 (4), 1073–1093. 10.1007/s12010-017-2611-4 [DOI] [PubMed] [Google Scholar]
- Wang Y., Li S., Li C. (2019b). Perspectives of New Advances in the Pathogenesis of Vitiligo: From Oxidative Stress to Autoimmunity. Med. Sci. Monit. 25, 1017–1023. 10.12659/msm.914898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Liu H., Zheng M., Yang Y., Ren H., Kong Y., et al. (2021d). Berberine Slows the Progression of Prediabetes to Diabetes in Zucker Diabetic Fatty Rats by Enhancing Intestinal Secretion of Glucagon-like Peptide-2 and Improving the Gut Microbiota. Front. Endocrinol. (Lausanne) 12, 609134. 10.3389/fendo.2021.609134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Quan F., Cao Q., Lin Y., Yue C., Bi R., et al. (2021e). Quercetin Alleviates Acute Kidney Injury by Inhibiting Ferroptosis. J. Adv. Res. 28, 231–243. 10.1016/j.jare.2020.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z.-K., Chen R.-R., Li J.-H., Chen J.-Y., Li W., Niu X.-L., et al. (2020b). Puerarin Protects against Myocardial Ischemia/reperfusion Injury by Inhibiting Inflammation and the NLRP3 Inflammasome: The Role of the SIRT1/NF-Κb Pathway. Int. Immunopharmacology 89 (Pt B), 107086. 10.1016/j.intimp.2020.107086 [DOI] [PubMed] [Google Scholar]
- Wen-Jun L., Hai-Yan W., Wei L., Ke-Yu W., Rui-Ming W. (2008). Evidence that Geniposide Abrogates Norepinephrine-Induced Hypopigmentation by the Activation of GLP-1r-dependent C-Kit Receptor Signaling in Melanocyte. J. Ethnopharmacology 118 (1), 154–158. 10.1016/j.jep.2008.03.021 [DOI] [PubMed] [Google Scholar]
- Weng L., Guo X., Li Y., Yang X., Han Y. (2016). Apigenin Reverses Depression-like Behavior Induced by Chronic Corticosterone Treatment in Mice. Eur. J. Pharmacol. 774, 50–54. 10.1016/j.ejphar.2016.01.015 [DOI] [PubMed] [Google Scholar]
- Whitton M. E., Pinart M., Batchelor J., Leonardi-Bee J., González U., Jiyad Z., et al. (2015). Interventions for Vitiligo. Cochrane Database Syst. Rev., CD003263. 10.1002/14651858.cd003263.pub5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitton M., Pinart M., Batchelor J. M., Leonardi-Bee J., Gonzalez U., Jiyad Z., et al. (2016). Evidence-based Management of Vitiligo: Summary of a Cochrane Systematic Review. Br. J. Dermatol. 174 (5), 962–969. 10.1111/bjd.14356 [DOI] [PubMed] [Google Scholar]
- Wu J., Zhou M., Wan Y., Xu A. (2013). CD8+ T Cells from Vitiligo Perilesional Margins Induce Autologous Melanocyte Apoptosis. Mol. Med. Rep. 7 (1), 237–241. 10.3892/mmr.2012.1117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu S., Hu Y., Bai W., Zhao J., Huang C., Wen C., et al. (2019). Cyanidin‐3‐o‐glucoside Inhibits UVA‐induced Human Dermal Fibroblast Injury by Upregulating Autophagy. Photodermatol. Photoimmunol Photomed. 35 (5), 360–368. 10.1111/phpp.12493 [DOI] [PubMed] [Google Scholar]
- Wu T. Y., Lin J. N., Luo Z. Y., Hsu C. J., Wang J. S., Wu H. P. (2020). 2,3,4',5-Tetrahydroxystilbene-2-O-beta-D-Glucoside (THSG) Activates the Nrf2 Antioxidant Pathway and Attenuates Oxidative Stress-Induced Cell Death in Mouse Cochlear UB/OC-2 Cells. Biomolecules 10 (3), 465. 10.3390/biom10030465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao H. B., Cao X., Wang L., Run X. Q., Su Y., Tian C., et al. (2011). 1,5-dicaffeoylquinic Acid Protects Primary Neurons from Amyloid β 1-42-induced Apoptosis via PI3K/Akt Signaling Pathway. Chin. Med. J. (Engl) 124 (17), 2628–2635. 10.3760/cma.j.issn.0366-6999.2011.17.012 [DOI] [PubMed] [Google Scholar]
- Xiao L., Zhong M., Huang Y., Zhu J., Tang W., Li D., et al. (2020). Puerarin Alleviates Osteoporosis in the Ovariectomy-Induced Mice by Suppressing Osteoclastogenesis via Inhibition of TRAF6/ROS-dependent MAPK/NF-κB Signaling Pathways. Aging 12 (21), 21706–21729. 10.18632/aging.103976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie H., Zhou F., Liu L., Zhu G., Li Q., Li C., et al. (2016). Vitiligo: How Do Oxidative Stress-Induced Autoantigens Trigger Autoimmunity?. J. Dermatol. Sci. 81 (1), 3–9. 10.1016/j.jdermsci.2015.09.003 [DOI] [PubMed] [Google Scholar]
- Xin L., Gao J., Lin H., Qu Y., Shang C., Wang Y., et al. (2020). Regulatory Mechanisms of Baicalin in Cardiovascular Diseases: A Review. Front. Pharmacol. 11, 583200. 10.3389/fphar.2020.583200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu D.-X., Guo X.-X., Zeng Z., Wang Y., Qiu J. (2021). Puerarin Improves Hepatic Glucose and Lipid Homeostasis In Vitro and In Vivo by Regulating the AMPK Pathway. Food Funct. 12 (6), 2726–2740. 10.1039/d0fo02761h [DOI] [PubMed] [Google Scholar]
- Xu P., Su S., Tan C., Lai R.-S., Min Z.-S. (2017). Effects of Aqueous Extracts of Ecliptae Herba, Polygoni Multiflori Radix Praeparata and Rehmanniae Radix Praeparata on Melanogenesis and the Migration of Human Melanocytes. J. Ethnopharmacology 195, 89–95. 10.1016/j.jep.2016.11.045 [DOI] [PubMed] [Google Scholar]
- Yadav A. K., Jang B. C. (2020). Anti-Survival and Pro-apoptotic Effects of 6-Shogaol on SW872 Human Liposarcoma Cells via Control of the Intrinsic Caspase Pathway, STAT-3, AMPK, and ER Stress. Biomolecules 10 (10). 10.3390/biom10101380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamada Y., Obayashi M., Ishikawa T., Kiso Y., Ono Y., Yamashita K. (2008). Dietary Tocotrienol Reduces UVB-Induced Skin Damage and Sesamin Enhances Tocotrienol Effects in Hairless Mice. J. Nutr. Sci. Vitaminol 54 (2), 117–123. 10.3177/jnsv.54.117 [DOI] [PubMed] [Google Scholar]
- Yamaguchi Y., Brenner M., Hearing V. J. (2007). The Regulation of Skin Pigmentation. J. Biol. Chem. 282 (38), 27557–27561. 10.1074/jbc.r700026200 [DOI] [PubMed] [Google Scholar]
- Yang B., Yang Q., Yang X., Yan H.-B., Lu Q.-P. (2016). Hyperoside Protects Human Primary Melanocytes against H2O2-Induced Oxidative Damage. Mol. Med. Rep. 13 (6), 4613–4619. 10.3892/mmr.2016.5107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang C.-C., Hsiao L.-D., Yang C.-M. (2020a). Galangin Inhibits LPS-Induced MMP-9 Expression via Suppressing Protein Kinase-dependent AP-1 and FoxO1 Activation in Rat Brain Astrocytes. Jir 13, 945–960. 10.2147/jir.s276925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang C. C., Lin C. C., Hsiao L. D., Yang C. M. (2018). Galangin Inhibits Thrombin-Induced MMP-9 Expression in SK-N-SH Cells via Protein Kinase-dependent NF-Κb Phosphorylation. Int. J. Mol. Sci. 19 (12), 4084. 10.3390/ijms19124084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang L., Yang F., Teng L., Katayama I. (2020b). 6-Shogaol Protects Human Melanocytes against Oxidative Stress through Activation of the Nrf2-Antioxidant Response Element Signaling Pathway. Int. J. Mol. Sci. 21 (10), 3537. 10.3390/ijms21103537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang X.-P., Liu T.-Y., Qin X.-Y., Yu L.-C. (2014). Potential protection of 2,3,5,4′-Tetrahydroxystilbene-2-O-β-D-Glucoside against Staurosporine-Induced Toxicity on Cultured Rat hippocampus Neurons. Neurosci. Lett. 576, 79–83. 10.1016/j.neulet.2014.05.045 [DOI] [PubMed] [Google Scholar]
- Yarla N. S., Bishayee A., Sethi G., Reddanna P., Kalle A. M., Dhananjaya B. L., et al. (2016). Targeting Arachidonic Acid Pathway by Natural Products for Cancer Prevention and Therapy. Semin. Cancer Biol. 40-41, 48–81. 10.1016/j.semcancer.2016.02.001 [DOI] [PubMed] [Google Scholar]
- Yim S. H., Tabassum N., Kim W. H., Cho H., Lee J. H., Batkhuu G. J. (2017b). Isolation and Characterization of Isofraxidin 7-O-(6'-O-P-Coumaroyl)-β-Glucopyranoside from Artemisia Capillaris Thunberg: A Novel, Nontoxic Hyperpigmentation Agent that Is Effective In Vivo . Evid. Based Complement. Alternat Med. 2017, 1401279. 10.1155/2017/1401279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yim S. H., Tabassum N., Kim W. H., Cho H., Lee J. H., Batkhuu G. J., et al. (2017a). Isolation and Characterization of Isofraxidin 7-O-(6'-O-P-Coumaroyl)-β-Glucopyranoside from Artemisia Capillaris Thunberg: A Novel, Nontoxic Hyperpigmentation Agent that Is Effective In Vivo . Evid. Based Complement. Alternat Med. 2017, 1401279. 10.1155/2017/1401279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin L., Pang G., Niu C., Habasi M., Dou J., Aisa H. A. (2018). A Novel Psoralen Derivative-MPFC Enhances Melanogenesis via Activation of P38 MAPK and PKA Signaling Pathways in B16 Cells. Int. J. Mol. Med. 41 (6), 3727–3735. 10.3892/ijmm.2018.3529 [DOI] [PubMed] [Google Scholar]
- Yin L., Niu C., Liao L. X., Dou J., Habasi M., Aisa H. A. (2017). An Isoxazole Chalcone Derivative Enhances Melanogenesis in B16 Melanoma Cells via the Akt/GSK3β/β-Catenin Signaling Pathways. Molecules 22 (12), 2077. 10.3390/molecules22122077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan J., Lu Y., Wang H., Feng Y., Jiang S., Gao X. H., et al. (2020). Paeoniflorin Resists H(2)O(2)-Induced Oxidative Stress in Melanocytes by JNK/Nrf2/HO-1 Pathway. Front. Pharmacol. 11, 536. 10.3389/fphar.2020.00536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zabolinejad N., Maleki M., Salehi M., Ashrafi Z., Molkara S., Layegh P. (2020). Psoralen and Narrowband UVB Combination Provides Higher Efficacy in Treating Vitiligo Compared with Narrowband UVB Alone: A Randomised Clinical Trial. Australas. J. Dermatol. 61 (1), e65–e69. 10.1111/ajd.13184 [DOI] [PubMed] [Google Scholar]
- Zang D., Niu C., Aisa H. A. (2019). Amine Derivatives of Furocoumarin Induce Melanogenesis by Activating Akt/GSK-3β/β-Catenin Signal Pathway. Drug Des. Develop. Ther. 13, 623–632. 10.2147/DDDT.S180960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhai Y., Wang Q., Li Y., Cui J., Feng K., Kong X., et al. (2018). The Higher Osteoprotective Activity of Psoralidin In Vivo Than Coumestrol Is Attributed by its Presence of an Isopentenyl Group and through Activated PI3K/Akt axis. Biomed. Pharmacother. 102, 1015–1024. 10.1016/j.biopha.2018.03.166 [DOI] [PubMed] [Google Scholar]
- Zhang B., Wang J., Zhao G., Lin M., Lang Y., Zhang D., et al. (2020). Apigenin Protects Human Melanocytes against Oxidative Damage by Activation of the Nrf2 Pathway. Cell Stress and Chaperones 25 (2), 277–285. 10.1007/s12192-020-01071-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang F., Zhang Y., Yang T., Ye Z. Q., Tian J., Fang H. R., et al. (2019a). Scopoletin Suppresses Activation of Dendritic Cells and Pathogenesis of Experimental Autoimmune Encephalomyelitis by Inhibiting NF-Κb Signaling. Front. Pharmacol. 10, 863. 10.3389/fphar.2019.01037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L., Li D.-c., Liu L.-f. (2019b). Paeonol: Pharmacological Effects and Mechanisms of Action. Int. Immunopharmacology 72, 413–421. 10.1016/j.intimp.2019.04.033 [DOI] [PubMed] [Google Scholar]
- Zhang L. (2019). Pharmacokinetics and Drug Delivery Systems for Puerarin, a Bioactive Flavone from Traditional Chinese Medicine. Drug Deliv. 26 (1), 860–869. 10.1080/10717544.2019.1660732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang R., Lee I. K., Piao M. J., Kim K. C., Kim A. D., Kim H. S., et al. (2011). Butin (7,3′,4′-Trihydroxydihydroflavone) Reduces Oxidative Stress-Induced Cell Death via Inhibition of the Mitochondria-dependent Apoptotic Pathway. Ijms 12 (6), 3871–3887. 10.3390/ijms12063871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang W., Cheng C., Sha Z., Chen C., Yu C., Lv N., et al. (2021). Rosmarinic Acid Prevents Refractory Bacterial Pneumonia through Regulating Keap1/Nrf2-Mediated Autophagic Pathway and Mitochondrial Oxidative Stress. Free Radic. Biol. Med. 168, 247–257. 10.1016/j.freeradbiomed.2021.03.038 [DOI] [PubMed] [Google Scholar]
- Zhang X., Bu H., Jiang Y., Sun G., Jiang R., Huang X., et al. (2019c). The Antidepressant Effects of Apigenin Are Associated with the Promotion of Autophagy via the mTOR/AMPK/ULK1 Pathway. Mol. Med. Rep. 20 (3), 2867–2874. 10.3892/mmr.2019.10491 [DOI] [PubMed] [Google Scholar]
- Zhang Y., Ding Y., Zhong X., Guo Q., Wang H., Gao J., et al. (2016). Geniposide Acutely Stimulates Insulin Secretion in Pancreatic β-cells by Regulating GLP-1 receptor/cAMP Signaling and Ion Channels. Mol. Cell Endocrinol. 430, 89–96. 10.1016/j.mce.2016.04.020 [DOI] [PubMed] [Google Scholar]
- Zhao C., Zhang H., Li H., Lv C., Liu X., Li Z., et al. (2017). Geniposide Ameliorates Cognitive Deficits by Attenuating the Cholinergic Defect and Amyloidosis in Middle-Aged Alzheimer Model Mice. Neuropharmacology 116, 18–29. 10.1016/j.neuropharm.2016.12.002 [DOI] [PubMed] [Google Scholar]
- Zhao L., Li H., Gao Q., Xu J., Zhu Y., Zhai M., et al. (2021). Berberine Attenuates Cerebral Ischemia-Reperfusion Injury Induced Neuronal Apoptosis by Down-Regulating the CNPY2 Signaling Pathway. Front. Pharmacol. 12, 609693. 10.3389/fphar.2021.609693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao W.-Z., Wang H.-T., Huang H.-J., Lo Y.-L., Lin A. M.-Y. (2018). Neuroprotective Effects of Baicalein on Acrolein-Induced Neurotoxicity in the Nigrostriatal Dopaminergic System of Rat Brain. Mol. Neurobiol. 55 (1), 130–137. 10.1007/s12035-017-0725-x [DOI] [PubMed] [Google Scholar]
- Zhou J., Chen F., Yan A., Xia X. (2020a). Madecassoside Protects Retinal Pigment Epithelial Cells against Hydrogen Peroxide-Induced Oxidative Stress and Apoptosis through the Activation of Nrf2/HO-1 Pathway. Biosci. Rep. 40 (10), 4347. 10.1042/bsr20194347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou J., Zhang S., Sun X., Lou Y., Bao J., Yu J. (2021). Hyperoside Ameliorates Diabetic Nephropathy Induced by STZ via Targeting the miR-499-5p/APC axis. J. Pharmacol. Sci. 146 (1), 10–20. 10.1016/j.jphs.2021.02.005 [DOI] [PubMed] [Google Scholar]
- Zhou Y.-X., Gong X.-H., Zhang H., Peng C. (2020b). A Review on the Pharmacokinetics of Paeoniflorin and its Anti-inflammatory and Immunomodulatory Effects. Biomed. Pharmacother. 130, 110505. 10.1016/j.biopha.2020.110505 [DOI] [PubMed] [Google Scholar]
- Zhou Y. X., Zhang R. Q., Rahman K., Cao Z. X., Zhang H., Peng C. (2019). Diverse Pharmacological Activities and Potential Medicinal Benefits of Geniposide. Evid. Based Complement. Alternat Med. 2019, 4925682. 10.1155/2019/4925682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu X., Zhang H., Lo R. (2004). Phenolic Compounds from the Leaf Extract of Artichoke (Cynara scolymusL.) and Their Antimicrobial Activities. J. Agric. Food Chem. 52 (24), 7272–7278. 10.1021/jf0490192 [DOI] [PubMed] [Google Scholar]
- Zhu Y., Tchkonia T., Pirtskhalava T., Gower A. C., Ding H., Giorgadze N., et al. (2015). The Achilles' Heel of Senescent Cells: from Transcriptome to Senolytic Drugs. Aging Cell 14 (4), 644–658. 10.1111/acel.12344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y., Wang S., Lin F., Li Q., Xu A. (2014). The Therapeutic Effects of EGCG on Vitiligo. Fitoterapia 99, 243–251. 10.1016/j.fitote.2014.08.007 [DOI] [PubMed] [Google Scholar]
- Zhu Y., Wang S., Xu A. (2013). A Mouse Model of Vitiligo Induced by Monobenzone. Exp. Dermatol. 22 (7), 499–501. 10.1111/exd.12184 [DOI] [PubMed] [Google Scholar]
- Zhu Y., Zhong L., Peng J., Yuan Q., Xu A. (2019). The Therapeutic Effects of Baicalin on Vitiligo Mice. Biol. Pharm. Bull. 42 (9), 1450–1455. 10.1248/bpb.b19-00319 [DOI] [PubMed] [Google Scholar]