Abstract
Background
The exponential increase in SARS-CoV-2 infections during the first wave of the pandemic created an extraordinary overload and demand on hospitals, especially intensive care units (ICUs), across Europe. European countries have implemented different measures to address the surge ICU capacity, but little is known about the extent. The aim of this paper is to compare the rates of hospitalised COVID-19 patients in acute and ICU care and the levels of national surge capacity for intensive care beds across 16 European countries and Lombardy region during the first wave of the pandemic (28 February to 31 July).
Methods
For this country level analysis, we used data on SARS-CoV-2 cases, current and/or cumulative hospitalised COVID-19 patients and current and/or cumulative COVID-19 patients in ICU care. To analyse whether capacities were exceeded, we also retrieved information on the numbers of hospital beds, and on (surge) capacity of ICU beds during the first wave of the COVID-19 pandemic from the COVID-19 Health System Response Monitor (HSRM). Treatment days and mean length of hospital stay were calculated to assess hospital utilisation.
Results
Hospital and ICU capacity varied widely across countries. Our results show that utilisation of acute care bed capacity by patients with COVID-19 did not exceed 38.3% in any studied country. However, the Netherlands, Sweden, and Lombardy would not have been able to treat all patients with COVID-19 requiring intensive care during the first wave without an ICU surge capacity. Indicators of hospital utilisation were not consistently related to the number of SARS-CoV-2 infections. The mean number of hospital days associated with one SARS-CoV-2 case ranged from 1.3 (Norway) to 11.8 (France).
Conclusion
In many countries, the increase in ICU capacity was important to accommodate the high demand for intensive care during the first COVID-19 wave.
Keywords: COVID-19, Hospital capacity, Hospital utilisation, Intensive care, ICU surge capacity
Abbreviations: BE, Belgium; DE, Germany; DK, Denmark; GR, Greece; HSRM, Health System Response Monitor; ICU, Intensive Care Unit; IE, Ireland; IT, Italy; IT-25, Lombardy; NL, The Netherlands; NO, Norway; OWiD, Our World in Data; PPE, Personal Protective Equipment; UK, United Kingdom
1. Introduction
Health systems have faced substantial pressures related to the COVID-19 pandemic. The exponential increase in SARS-CoV-2 infections in March and April 2020 created an unprecedented demand for hospitals in many European countries. On March 11, the bed occupancy in some hospitals in Italy exceeded existing intensive care unit (ICU) capacities [1]. Shortly thereafter, in late March, many Spanish hospitals, especially in the capital city of Madrid, reported reaching their capacity limits of acute and/or intensive care beds to adequately treat all patients with COVID-19 requiring inpatient care [2]. Many hospitals in other European regions (e.g., the Dutch region of Brabant and Grand Est in France) were also overwhelmed with the influx of patients with COVID-19 and transferred critically ill patients to other hospitals across the country or even neighbouring countries to free up capacity [3]. Throughout Europe, hospitals were required to postpone elective treatments to free up hospital beds and to add beds to ICUs equipped with ventilators while maintaining essential services such as urgent consultations, necessary treatments (e.g., chemotherapy, dialysis), maternal services, and rehabilitation [4], [5].
While recognising that many health systems have at least partially been overburdened during the first wave, little is known about the extent of hospital surge capacity created in acute and intensive care units as a response to COVID-19 to accommodate the spike in the number of patients and the actual use of hospital capacities across European countries. However, information on capacities, both in terms of initial and reserve surge capacities, as well as resource utilisation by patients with COVID-19 is key to inform pandemic preparedness and contingency planning within the hospital setting [6]. At the time this article was written, existing studies only report on hospital surge capacities in single countries [7] or hospitals [8]; to the best of our knowledge, no cross-country overview of additional surge capacity for patients with COVID-19 is available. Furthermore, evidence on the length of stay of patients with COVID-19 in acute and intensive care units is available only for a few European countries [9], [10], [11].
This paper aims to analyse whether COVID-19 hospitalisations exceeded the national ICU surge capacity across 16 European countries and the Lombardy region during the first wave of the pandemic (28 February to 31 July, 2020). We complement this analysis with a comparison of the average length of stay and the cumulative number of days of hospitalisation for patients with COVID-19 across the countries. The latter parameter is additionally compared to the rate of SARS-CoV-2 infections. The findings aim to support health care decision makers in refining contingency plans and improving hospital preparedness for future health emergencies.
2. Materials and methods
2.1. Type of study and data collection
This cross-country analysis is based on a systematic data collection encompassing data from 18 European countries and two Italian regions of the following variables: number of SARS-CoV-2 cases; number of COVID-19 tests carried out or persons tested; number of current and/or cumulative hospitalised cases with COVID-19 and number of current and/or cumulative cases with COVID-19 in ICU care.
Countries were included in the collection of data from patients with COVID-19 hospitalised in acute and intensive care units, which began on 20 March 2020, once they reported at least five positive cases per 100,000 population. All data was manually retrieved from official online sources, such as websites of Ministries of Health, national research and public health institutes, official dashboards from national institutions and Our World in Data (OWiD) [12] that daily report numbers of all registered cases, tests and hospitalised patients in the respective countries. The resulting database is publicly available on the website of our institution [13] and the Harvard Dataverse repository [14]. The database was updated regularly to reflect values that some countries corrected retrospectively (e.g., Norway and the United Kingdom [UK]) (see supplemental Tables 1–18, appendix pp 1–23). Over time, some countries adjusted their data collection method, data reporting channel or the style of reporting (i.e., in Denmark the definition of COVID-19-related hospital admission was changed as of June 2020, see supplemental Table 4). If updated data were available retrospectively, we adjusted the collected data in our database accordingly. The ECDC started to provide similar data on current hospital and ICU occupancy for COVID-19 in several European countries as of summer 2020 [15].
We also retrieved information on the numbers of hospital beds prior to the pandemic from the OECD [16] and ICU beds prior to the pandemic from the OECD/European Union [17]. Information on the surge capacity of ICU beds during the first wave was obtained from the COVID-19 Health System Response Monitor (HSRM) [18], with some supplementary information available from national sources. The HSRM tool was established in March 2020 and designed in response to the COVID-19 outbreak to collect and disseminate up-to-date information on how countries, mainly those in the WHO European Region, are responding to the crisis with a primary focus on the responses of health systems.
For the analysis data on SARS-CoV-2 cases and currently and cumulative hospital and ICU admissions of patients with COVID-19 were used. Spain and Switzerland did not report on current numbers of patients in acute and intensive care units and were therefore excluded from the analysis. The Lombardy region was included because it had the highest number of cases of COVID-19 in Europe and in the world during the early months of 2020 [19]. Single missing values for currently hospitalised patients were imputed linearly to facilitate a comparative analysis of countries with incomplete daily reporting (e.g., no data were reported on weekends).
2.2. Data description
For the data collected on hospitalised patients and patients in intensive care units, definitions and reported units differ between countries due to different data collection methods used (see supplemental Tables 1–18, appendix pp 1–23). For most countries, information on whether hospitalised patients with COVID-19 represent confirmed cases only or confirmed and suspected cases combined is not available. When both confirmed and suspected cases were reported, we only retrieved data on confirmed cases. Furthermore, data collection varies in terms of the reason and trajectory of hospital admission, namely, whether patients were admitted only due to COVID-19 (and excluding other pathologies and transfers from other hospitals, i.e., in Belgium) or comprise all hospitalised patients who tested positive for COVID-19 (i.e., in Denmark and France). Moreover, some countries subsumed ICU patients in the total number of hospitalised patients, while others did not (e.g., the Netherlands). We added the numbers of inpatients treated in normal wards and in ICUs to calculate the total number of currently hospitalised patients. The definition of ICU cases is unclear in some countries, e.g., regarding the inclusion of patients in surveillance beds. A detailed description of the data collected, including sources, variable definitions (i.e. type of tests), first or last date of reporting, and collection method for each country (and region), is provided in supplemental Tables 1–18, appendix pp 1–23.
2.3. Analysis
The analysis presented here focuses on a subset of 16 European countries and one Italian region, for which information on current hospitalisations and/or ICU treatments of patients with COVID-19 was available for the period up to 31 July 2020, i.e., Austria, Belgium, Denmark, Estonia, Finland, France, Germany, Greece, Ireland, Italy (and the Lombardy region), Luxembourg, Netherlands, Norway, Portugal, Sweden, and the UK.
First, we present and compare hospital and ICU bed capacities prior to COVID-19 in 14 countries and the Lombardy region. In addition, we depict the additional ICU beds that were available during the surge for the COVID-19 pandemic in 11 countries, as reported in the HSRM and national sources.
Second, we plotted the number of currently hospitalised patients with COVID-19 per 100,000 population over time against the hospital bed capacities before the pandemic and grouped countries with similar capacity levels to analyse whether hospital capacities were exceeded. We used the same approach for ICU bed capacities, with an additional step of illustrating ICU surge capacity against the current hospitalisation rates of patients with COVID-19 in intensive care units. Due to limited data availability, 11 countries and the Lombardy region were included in the analysis of acute bed capacities, and nine countries and the Lombardy region were included in the analysis of ICU surge capacities.
Third, we calculated additional indicators to further illustrate COVID-19-related hospital utilisation. Cumulative days of hospitalisation and cumulative days of ICU stay were calculated by summing the respective daily numbers of current inpatients (representing the total number of bed occupancy days until 31 July 2020). For intensive care, this procedure was performed for all 16 countries plus the Lombardy region. With respect to acute care, Greece and Sweden were excluded due to a lack of data. The relation between bed occupancy days and burden of SARS-CoV-2 infections was reported as the mean numbers of hospital days and ICU days per infected case. The mean length of stay was approximated for hospital and ICU treatment by dividing the number of bed occupancy days by the cumulative number of hospital and ICU treatment cases, respectively; this approach was used for eight countries for acute care and for six countries for intensive care.
Finally, we calculated the proportion of cumulative patients infected with SARS-CoV-2 requiring hospital treatment and ICU treatment in the same countries.
We used Excel and the statistical programme R for data visualization. Supplemental Table 19 (appendix, p 24) provides an overview of the countries included in each step of the analysis.
3. Results
The pre-pandemic hospital and ICU capacities varied widely across the 14 countries, with data available ranging from 197 acute care beds per 100,000 in Sweden to 602 beds in Germany [16] and from 5.0 ICU beds per 100,000 in Ireland (2016) and Sweden [17] to 33.4 ICU beds in Germany (2018) [20] (see Table 1 ). Thus, a three-fold variation in the acute care capacity and even a seven-fold variation in the intensive care bed capacity were observed between the two ends of the spectrum in these countries prior to the COVID-19 pandemic. However, it must be noted that the number of ICU beds in Ireland only include those in the public sector.
Table 1.
Pre-pandemic hospital capacity, ICU capacity and ICU surge capacity during the first COVID-19 wave.
| Country/region | Acute care bed capacity prior to COVID-19 [16] |
ICU bed capacity prior to COVID-19 |
ICU bed surge capacity during the first COVID-19 wave |
Change of ICU bed capacity (in%) | |||||
| in total | per 100,000 | year | in total | per 100,000 | year | in total | per 100,000 | per 100,000 | |
| Austria | 47,276 | 535 | 2018 | 2547a | 28.9 [17] | 2018 | n/a | n/a | n/a |
| Belgium | 56,758 | 497 | 2018 | 1993a | 17.4 [17] | 2019 | ca. 2750 (early April)a | 24 [18] | 38% |
| Denmark | 13,659 | 236 | 2018 | 1078b | 18.6c | 2020 | 1242 (925 for patients with COVID-19) [21] | 21.4c | 15% |
| Estonia | 4444 | 336 | 2018 | 199a | 15.0 [17] | 2019 | 130 for patients with COVID-19d[18] | n/a | n/a |
| Finland | 15,667 | 284 | 2018 | 300a | 5.4 [17] | 2019 | n/a | n/a | n/a |
| France | 203,662 | 304 | 2018 | 10,882a | 16.3 [17]j | 2018 | n/a | n/a | n/a |
| Germany | 497,182 | 602 | 2018 | 27,463 [20]g | 33.4c | 2018 | 32,824 (early June) [22]h | 39.5c | 18% |
| Greece | 39,011 | 363 | 2018 | 565a | 5.3 [17] | 2019 | 1017 (350 for patients with COVID-19, end of April) [18] | 9.5c | 79% |
| Ireland | 13,560 | 279 | 2018 | 250a | 5.0 [17] | 2016 | 489 (end of May)/up to 800 [[23], [24] | 10.0/16.3c | 100/ 226% |
| Italy | 156,216 | 259 | 2018 | 5200a | 8.6 [17] | 2020 | 8550 [25] | 14.0c | 63% |
| Lombardy | 34,756 [26] | 346 [26] | 2018 | 724 [27] | 7.2c | 2019 | 1,347e[18] | 13.4c | 86% |
| Luxembourg | 2251 | 370 | 2018 | n/a | n/a | n/a | n/a | n/a | n/a |
| Netherlands | 46,323 | 269 | 2018 | 1150a | 6.7 [17] | 2018 | 2400 (1 900 for patients with COVID-19) [28] | 13.9 | 107% |
| Norway | 16,646 | 313 | 2018 | 450 | 8.5 [17] | 2018 | up to 925 (or even 1,200f) [18] | 17.4c (22.5c) | 105% |
| Portugal | 33,850 | 329 | 2018 | 587 [18]i | 5.7c | n/a | n/a | n/a | n/a |
| Sweden | 20,019 | 197 | 2018 | 526 [18] | 5.0c | 2020 | 1064 (mid-April) [18] | 10.4c | 108% |
| UK | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a |
Notes: a: own calculation based on ICU beds prior to COVID-19 per 100,000; b: including 645 ICU beds with ventilators usually reserved for patients with elective surgery; c: own calculation based on ICU beds prior to COVID-19 in total; d: we were unable to determine whether these beds were created additionally or reserved for patients with COVID-19; e: calculation based on information from HSRM that ICU bed capacity increased by 86%; f: on April 15th, the Regional Health Authorities provided detailed contingency plans on how to increase the ICU capacity to 1200 beds, but underlined that such a capacity can only be sustained for a short period of time; g: includes high-care and low-care ICU beds (for adults and children) but excludes post-surgery recovery beds; h: includes high-care and low-care ICU beds (for adults and children); i: includes general level 3 ICU beds for adults and children; j: includes resuscitation beds (lits de réanimation adulte) (except severe burns) and intensive care beds (lits de soins intensifs) (except neonatology) but excludes surveillance beds for adults and children (lits de surveillance) and resuscitation beds for children (lits de réanimation enfants).
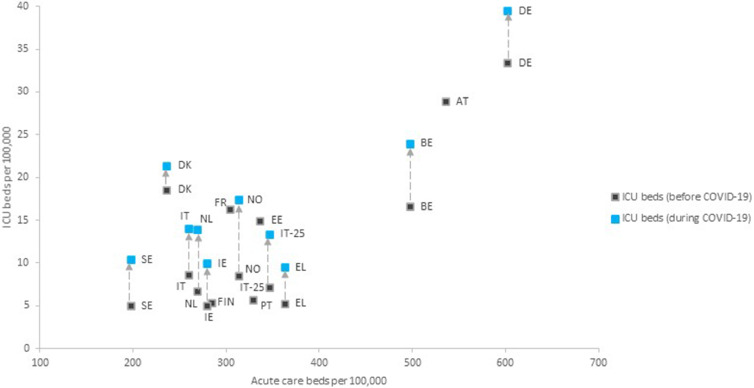
Fig. 1 further illustrates the association between acute care and ICU bed capacities in 14 countries and the Lombardy region; countries with a high acute bed capacity also tend to have a high ICU bed capacity. Denmark appears to be an exception, with relatively high ICU bed capacities compared to a lower acute hospital bed capacity.
Fig. 1.
Hospital and ICU capacities before COVID-19 and the ICU surge capacity created for COVID-19 (per 100,000). Sources: Acute care and ICU beds prior to the COVID-19 pandemic [14-15] and ICU beds during the COVID-19 pandemic [16]; see table 1 for more information. Notes: AT Austria, BE Belgium, DE Germany, DK Denmark, EE Estonia, FIN Finland, EL Greece, IE Ireland, IT Italy, IT-25 Lombardy, NL The Netherlands, NO Norway, PT Portugal, SE Sweden.
Fig. 1 further shows the number of ICU beds per 100,000 additionally created (or planned) during the first wave for nine countries and the Lombardy region based on information reported in the COVID-19 HSRM and national sources (see also Table 1). In Ireland, the Netherlands, Norway and Sweden – as well as in Italy's hard-hit Lombardy region (“IT-25″ in Fig. 1) –, the intensive care capacity has approximately doubled since the start of the COVID-19 crisis. The number of ICU beds also increased markedly in Belgium, Germany, Greece and Italy. According to Norway's contingency plan, the ICU capacity could more than double in an emergency situation. An increase in the number of beds likely occurred also in acute care units, but data were not consistently reported in the HSRM and country-specific sources.
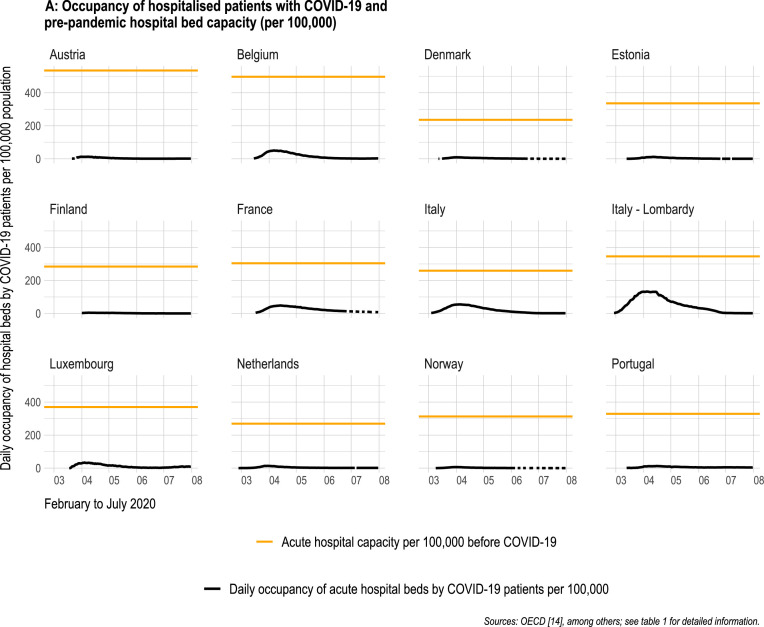
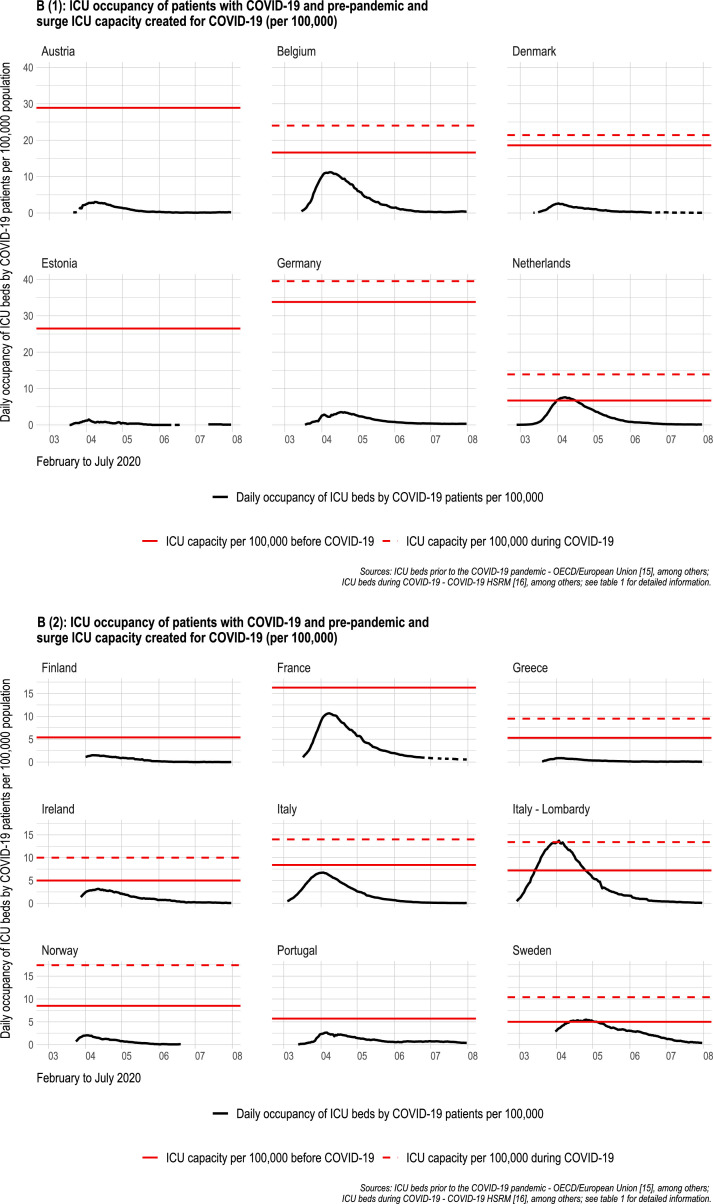
Fig. 2 shows that the pre-pandemic capacity of acute care beds was not exceeded by COVID-19 hospitalisations in any of the 11 countries. In the Lombardy region, the percentage of acute care beds occupied by patients with COVID-19 peaked at 38.3%, followed by Italy at 21.1%, while in Austria, the maximum percentage was 2.3%.
Fig. 2.
(A) Occupancy of hospitalised patients with COVID-19 and pre-pandemic hospital bed capacity (per 100,000. (B) (1 and 2): ( ICU occupancy of patients with COVID-19 and pre-pandemic and surge ICU capacity created for COVID-19 (per 100,000).
In contrast, Fig. 2B shows that the intensive care capacity prior to the pandemic was exceeded by COVID-19-necessitated admissions in the Netherlands, Sweden, and the Lombardy region and that capacities were nearly surpassed in Belgium and Italy. For approximately five weeks, the demand for intensive care by patients with COVID-19 exceeded pre-pandemic capacities in Lombardy and Sweden, while the shortage lasted approximately two weeks in the Netherlands. Only in the Lombardy region was the surge capacity fully exhausted and even exceeded for one day (on 3 April 2020).
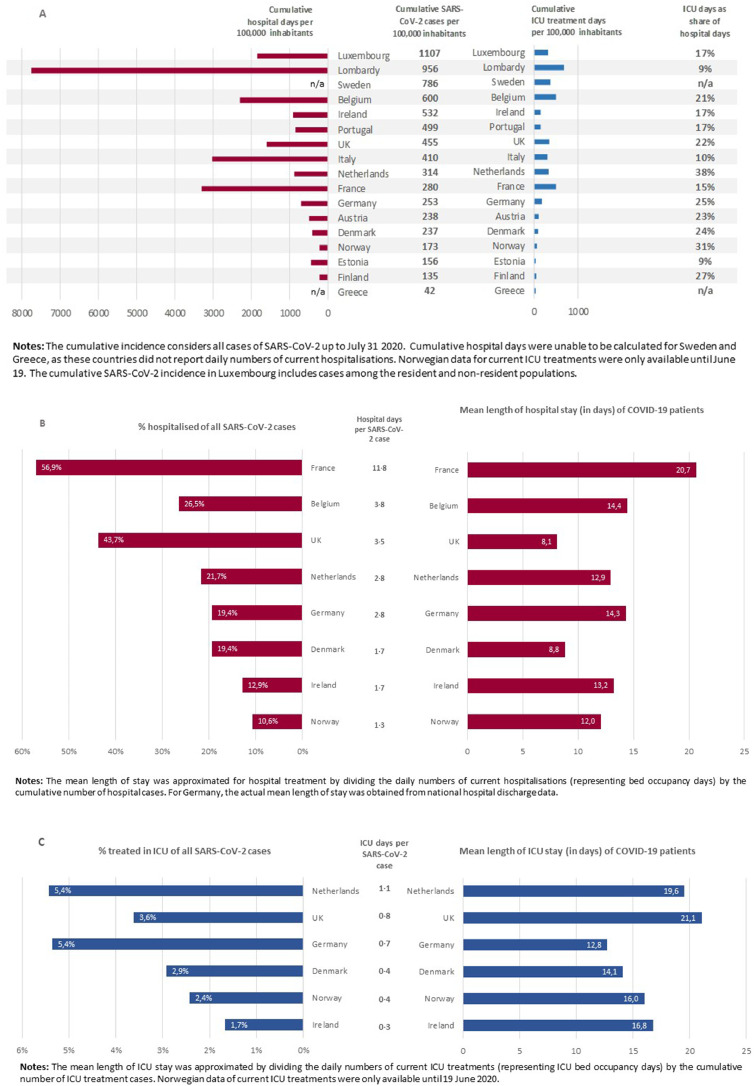
Fig. 3 reports the total number of days patients with COVID-19 spent in acute and intensive care units per 100,000 population (countries are sorted by cumulative COVID-19 incidence until 31 July 2020). The number of days patients with COVID-19 were treated in acute and intensive care settings varied widely across countries; until 31 July, the cumulative number of hospital days per 100,000 inhabitants ranged from 210 in Finland to 7762 in Lombardy (Italy), and the cumulative number of days in intensive care units ranged from 38 in Greece to 678 in Lombardy, followed by France, Italy, and Belgium. For France, high numbers of hospital and ICU treatment days were observed, while the reported overall SARS-CoV-2 incidence was comparatively low. Other countries, such as Ireland and Portugal, had a higher SARS-CoV-2 incidence but noticeably lower numbers of hospital and ICU treatment days. The proportion of cumulative days spent in intensive care units in relation to cumulative days spent in normal wards ranged from 9% in Lombardy and Estonia to 38% in the Netherlands.
Fig. 3.
(A): Cumulative hospital days and ICU days of patients with COVID-19 (per 100,000), (B) and (C): Indicators on hospital utilisation of COVID-19 patients in acute and intensive care units.
Figure 3B and 3C depict the percentages of patients with COVID-19 treated in acute and intensive care settings, the mean lengths of stay and the mean number of hospital and ICU treatment days per SARS-CoV-2 case, with the latter determining the order of countries in the figures. The left panel displays the number of patients with COVID-19 treated in hospitals and ICUs as a percentage of all SARS-CoV-2 cases until 31 July, and the right panel shows the mean lengths of hospital stay for patients with COVID-19.
The mean number of hospital days associated with one SARS-CoV-2 case ranged from 1.3 (Norway) to 11.8 (France). The proportion of all patients infected with SARS-CoV-2 who received inpatient treatment ranged from 11% (Norway) to 57% (France). The mean length of hospital stay ranged from 8 days (UK) to 21 days (France).
The mean number of ICU days associated with one SARS-CoV-2 case ranged from 0.3 (Ireland) to 1.1 (Netherlands). The proportion of patients infected with SARS-CoV-2 requiring ICU treatment ranged from 1.7% (Ireland) to 5.4% (Germany and the Netherlands). The mean length of ICU stay ranged from 13 days (Germany) to 21 days (UK).
4. Discussion
To the best of our knowledge, this study is the first cross-country overview of hospitalisations associated with COVID-19 and the creation of additional intensive care resources. Our results indicate that the pre-pandemic hospital capacities varied substantially between countries included in the analysis. Regardless of their starting point, countries have implemented several measures to increase the ICU capacity during the first wave of the pandemic and meet the spike in demand for hospital care, although to different extents. The highest increase in the number of ICU beds was achieved in Ireland, the Netherlands, and Sweden, where capacity at least doubled compared to pre-COVID levels. The Lombardy region and Greece also increased their initial capacity of ICU beds per 100,000 by 86% and 79%, and Italy and Belgium increased their initial capacity by 63% and 38%, respectively. In contrast, Germany increased its ICU capacity by only 18%, which is likely to be linked to its high initial capacity of ICU beds. From the sample of countries included in our analysis, countries with low pre-pandemic ICU bed rates (Sweden, Greece, Ireland and the Netherlands) increased ICU capacity stronger than countries with high initial ICU capacities such as Austria, Belgium and Germany.
In response to the rapidly increasing numbers of patients with COVID-19, countries have implemented different strategies. The most common strategies were the postponement of elective surgery, the re-configuration of hospital wards, the use of private hospitals or the setup of field hospitals, to rapidly create additional acute and ICU beds [4,29]. In the first wave, countries seemed to have used these various strategies to increase hospital capacities to highest possible levels. These strategies were increasingly aligned to real need throughout the pandemic as knowledge on expected admissions, treatment and length of stay proliferated. Some countries that did not see a critical increase in COVID-19 cases and hospitalisations in the first wave, such as Denmark, Estonia, and Norway, had contingency plans in place to reserve surge capacity for extreme situations.
While countries faced different numbers of confirmed SARS-CoV-2 infections, the available capacities of acute care beds were not exceeded by patients with COVID-19 in the included countries. Thus, in theory, these countries would have been able to manage more COVID-19 patients or non-COVID-19 patients requiring acute care, always provided that there are sufficient health professionals. However, based on our analysis, the Netherlands and Sweden would not have had sufficient capacity to treat all patients with COVID-19 requiring intensive care without the ICU surge capacity. In the Lombardy region, the ICU surge capacity was even exceeded.
Our calculations of hospital indicators showed that COVID-19-related hospital utilisation varied substantially across the countries included. We observed a large difference in the number of cumulative treatment days of patients with COVID-19 in acute and intensive care settings and were unable to reveal a consistent relation to the incidence of SARS-CoV-2. Thus, the SARS-CoV-2 incidence alone is not the driving force for the utilisation of acute and intensive care in the hospital, but many other factors, such as demographics and morbidity of patients infected with SARS-CoV-2 [30] testing strategies, treatment pathways, and service delivery patterns may play an important role and should be included in predictive models. For example, the true number of persons infected with SARS-CoV-2 might be underestimated, depending on the use of different testing strategies across countries [31].
Consequently, the mean number of hospital days per SARS-CoV-2 case ranged from 1.3 (Norway) to 11.8 (France), and the number of ICU days per case ranged from 0.3 (Ireland) to 1.1 (Netherlands). These figures may serve as basic landmarks for forecasting capacity requirements to meet the surge demand. In Belgium, for example, based on the data obtained from March to July 2020, 1000 additional infections would cause an average need for 3800 hospital bed days (mean days per case of 3.8) and 800 ICU bed days (mean days per case of 0.8).
The study has several limitations that should be acknowledged before discussing its usefulness, e.g., for forecasting hospital capacity requirements. First, information on the timing of surge capacity in a country, including when it started, how quickly it scaled up, and if/when it scaled down, is uncertain because the level of information reported in the HSRM is not systematically harmonised across countries. Second, some uncertainties in data quality and data completeness are noted within countries, both related to data on hospital utilisation and information reported on HSRM. Third, non-COVID-19 patients requiring acute or intensive care were not included in our analysis, which should be considered to comprehensively estimate the full burden on hospitals during the first wave. Fourth, with the exception of the Lombardy region, this study is a country-level analysis and does not consider the geographic distribution of hospital capacity, COVID-19 admissions and patterns of hospital utilisation; periods might have existed where ICUs were overloaded in certain regions within a country, which are not reflected in our data. For instance, ICUs were overloaded in Lombardy, but not in Italy as a whole. Similarly, our data do not allow us to identify whether the capacities of single hospitals were exceeded. For example, Mateen et al. [32] reported that the hospital capacities of one-third of all hospitals in England were exceeded during the first COVID-19 wave. Fifth, the focus of our study is on hospital bed capacities without considering the capacities of health professionals and medical equipment such as PPE (personal protective equipment) and ventilators that are necessary to ensure that surge capacities for patients with COVID-19 remain operational. Any decision on planning capacity should take these aspects into account [6]. Sixth, disaggregation of data related to both intensive care capacity and utilisation, i.e., low, high or intermediate care, was not performed due to limited information on type of ICU beds in international data. Hence, differences in the notion of intensive care influencing the comparability of the data may exist. A consistent and harmonised definition of ICU beds across countries would enhance comparability of capacities. Currently, there is no such definition by international organisation such as the OECD. Furthermore, the informative value of our data in regard to the length of hospital stay of patients with COVID-19 is limited, as we were only able to approximate the mean length of stay instead of calculating the median, which was reported in the majority of existing studies [9,10]. Finally, the comparability of data across countries is limited, e.g., due to the use of different data collection methods and definitions for variables, such as hospitalised patients with COVID-19, which in some countries also include unconfirmed cases or the numbers of SARS-CoV-2 cases (which were only confirmed by PCR tests in some countries, but also confirmed by antibody tests in other countries, see supplemental Tables 1–18, appendix pp 1–23).
However, when comparing our data to the published literature, our findings appear to be plausible. For example, the Norwegian ICU registry reported an average length of stay of 17 days in October 2020 [33], which is similar to our data from 19 June 2020 (latest available date in our database) showing that patients spent an average of 16 days in the ICU, with the variation likely related to the different time of measurement. Furthermore, data from the OECD/European Union [17] reported ICU occupancy levels of 78% in Italy at the height of the outbreak, which is comparable with our data, where this proportion was approximately 80%. However, they only relate the number of patients requiring intensive care to the initial number of ICU beds. Considering the surge capacity, the number of ICU beds occupied by patients with COVID-19 drops to 48%. This finding shows the importance of surge capacity, which is highlighted in our analysis.
Furthermore, the observed COVID-19-related hospital utilisation varied substantially. Indicators of hospital utilisation, such as the percentage of hospitalisations among patients infected with SARS-CoV-2 or cumulative treatment days, revealed no consistent relation with the number of persons infected with SARS-CoV-2. Thus, the SARS-CoV-2 incidence alone is not decisive for the utilisation of acute and intensive hospital care. The true number of persons infected with SARS-CoV-2 might be underestimated to a greater or lesser extent, depending on the use of different testing strategies across countries [31].
Data on available hospital resources combined with their utilisation are crucial to inform health care decision makers [34] over the course of the COVID-19 pandemic and for upcoming public health crises, e.g., by integrating indicators presented in this study into forecasting models. Finland, Norway, Sweden [35], the Netherlands, and the UK (England, Wales, Northern Ireland) have a long tradition of ICU registries [36] and were therefore able to strictly monitor the daily situation during the pandemic, which is key for reacting in a timely manner. Other countries, such as Germany [22], established ICU registries only after the pandemic had emerged.
Overall, European countries experienced hospital capacity utilisation differently. This result underlines the importance of data collection and monitoring for planning authorities. Generally, being overprepared in extreme situations might be preferable to risking overwhelmed capacities. This finding is substantiated by a recent study showing a higher mortality rate for patients with COVID-19 in an area without access to intensive care [37]. At the same time, in many countries hospital units were restructured with elective services being postponed and occupancy rates being low which had adverse effects on patient outcomes [38].
5. Conclusions
Our study indicates that the SARS-CoV-2 incidence is not the only aspect during the first COVID-19 wave that contributed to the burden of hospital care for patients with COVID-19, but rather the utilisation of hospital resources, as indicated by cumulative hospital days and mean length of stay, is also important. Hospital resource utilisation also depends on demographics and morbidity of infected population groups, treatment pathways, and service delivery patterns, including reimbursement policies, public health strategies and the number of hospital beds and ICU beds within a health system. The presented analysis on intensity and timing of COVID-19 related hospital admissions might contribute to preparedness (re-)planning for healthcare during emergency phases. In countries with low ICU capacities where pre-pandemic ICU capacities were exceeded, a potentially useful approach would be to consider strategies for reserving ICU beds for future health emergencies. Upcoming studies on hospital utilisation during the second wave of the pandemic might provide additional findings that will further contribute to preparedness activities, aiming to cope with future occurrences of unpredicted large-scale needs in acute health care.
Funding
This study was funded under the Excellence Strategy of the Federal Government and the Länder by the Berlin University Alliance (grant 112_PreEP_Corona). The funders of the study had no role in the study design, data collection, data analysis, data interpretation, writing of the report, or the decision to submit the paper for publication.
Authors’ contributions
EB, JW and RB conceived the study and were responsible for its design. UN, HE, DP, CR and TR contributed ideas and feedback to the conceptualisation of the study. EB, JW, HE and UN contributed to data analysis and wrote the main draft of the manuscript. EB, JW, HE UN, CR, TR and DP contributed to the acquisition and curation of data. RB and DP contributed to the critical revision of the report and study supervision. All authors critically revised and approved the manuscript.
Declaration of Competing Interest
EB, JW, HE, UN, CR, TR, DP and RB report grants from the Ministry of Education and Research (BMBF) and the federal state of Berlin during the conduct of the study. UN receives funding from the German Research Foundation. DP started working for the European Observatory on Health Systems and Policies on 1 October 2020, a partnership hosted by the World Health Organization. The submitted work is independent from this relationship. RB reports grants from the Federal Ministry of Research and Education, grants from the World Health Organization, grants and other funding from the Federal Ministry of Health, and grants from the Innovation Fund for projects outside the scope of the submitted work.
Acknowledgments
Institutional support and physical resources were provided by the Technische Universität Berlin. Erin Webb was responsible for language editing and proofreading.
Footnotes
Open Access for this article is made possible by a collaboration between Health Policy and The European Observatory on Health Systems and Policies.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.healthpol.2021.11.009.
Appendix. Supplementary materials
References
- 1.Verelst F., Kuylen E., Beutels P. Indications for healthcare surge capacity in European countries facing an exponential increase in coronavirus disease (COVID-19) cases. Euro Surveill. 2020 doi: 10.2807/1560-7917.ES.2020.25.13.2000323. March 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jones S. Spanish minister says older people found 'dead and abandoned': US scrambles to tackle coronavirus pandemic and Germany reports that new infections are levelling off. 23 March 2020. https://www.theguardian.com/world/2020/mar/23/spain-distributes-650000-testing-kits-as-coronavirus-deaths-rise-steeply. Accessed 24 Nov 2020.
- 3.Winkelmann J., Scarpetti G., Hernandez-Quevedo C., van Ginneken E. How do the worst-hit regions manage COVID-19 patients when they have no spare capacity left? Health Syst Response Monit. 2020 https://analysis.covid19healthsystem.org/index.php/2020/04/24/how-do-the-worst-hit-regions-manage-covid-19-patients-when-they-have-no-spare-capacity-left/ Accessed 8 Dec 2020. [Google Scholar]
- 4.Winkelmann J., Webb E., Williams G.A., Hernández-Quevedo C., Maier C.B., Panteli D. European countries' responses in ensuring sufficient physical infrastructure and workforce capacity during the first COVID-19 wave. Health Policy (New York) 2021 doi: 10.1016/j.healthpol.2021.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Webb E., Hernández-Quevedo C., Williams G., Scarpetti G., Reed S., Panteli D. Providing health services effectively during the first wave of COVID-19: a cross-country comparison on planning services, managing cases, and maintaining essential services. Health Policy (New York) 2021 doi: 10.1016/j.healthpol.2021.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. Beyond Containment: health systems responses to COVID-19 in the OECD; 2020.
- 7.McCabe R., Schmit N., Christen P., D'Aeth J.C., Løchen A., Rizmie D., et al. Adapting hospital capacity to meet changing demands during the COVID-19 pandemic. BMC Med. 2020;18:329. doi: 10.1186/s12916-020-01781-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carenzo L., Costantini E., Greco M., Barra F.L., Rendiniello V., Mainetti M., et al. Hospital surge capacity in a tertiary emergency referralcentre during the COVID-19 outbreak in Italy. Anaesthesia. 2020:928–934. doi: 10.1111/anae.15072. [DOI] [PubMed] [Google Scholar]
- 9.Lane E.A., Barrett D.J., Casey M., McAloon C.G., Collins Á.B., Hunt K., et al. Country differences in hospitalisation, length of stay and admission to Intensive Care Units due to SARS-CoV-2 infection: a rapid review of available literature (preprint) medRxiv. 2020 doi: 10.1101/2020.05.12.20099473. [DOI] [Google Scholar]
- 10.Rees E.M., Nightingale E.S., Jafari Y., Waterlow N.R., Clifford S., B Pearson C.A., et al. COVID-19 length of hospital stay: a systematic review and data synthesis. BMC Med. 2020;18:270. doi: 10.1186/s12916-020-01726-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Karagiannidis C., Mostert C., Hentschker C., Voshaar T., Malzahn J., Schillinger G., et al. Case characteristics, resource use, and outcomes of 10 021 patients with COVID-19 admitted to 920 German hospitals: an observational study. Lancet Respirat Med. 2020 doi: 10.1016/S2213-2600(20)30316-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Our World in Data (OWiD). Coronavirus Pandemic (COVID-19): statistics and Research. 2020. https://ourworldindata.org/coronavirus. Accessed 18 Dec 2020.
- 13.Department of Health Care Management (MiG). COVID-19-STATS. 2020. https://www.mig.tu-berlin.de/fileadmin/a38331600/sonstiges/COVID-19-STATS_2007_22.pdf. Accessed 18 Dec 2020.
- 14.Winkelmann J., Berger E., Busse R., Nimptsch U., Reichebner C., Eckhardt H., et al. COVID-19 Hospitalisation, cases and tests in 18 European countries. 2021. https://dataverse.harvard.edu/dataset.xhtml?persistentId=doi:10.7910/DVN/02CFBB. Accessed 28 Jan 2021.
- 15.European Centre for Disease Prevention and Control (ECDC). Data on hospital and ICU admission rates and current occupancy for COVID-19. 2021. https://www.ecdc.europa.eu/en/publications-data/download-data-hospital-and-icu-admission-rates-and-current-occupancy-covid-19. Accessed 26 Jan 2021.
- 16.OECD. Hospital beds; Curative (acute) care beds. 2020. https://stats.oecd.org/Index.aspx?ThemeTreeId=9#. Accessed 26 Nov 2020.
- 17.OECD/European Union . OECD; Paris: 2020. Health at a glance: Europe 2020: state of health in the EU cycle. [Google Scholar]
- 18.COVID-19 Health System Response Monitor (HSRM). COVID-19 health system response monitor: main page. 2020. https://www.covid19healthsystem.org/mainpage.aspx. Accessed 26 Nov 2020.
- 19.Cereda D., Tirani M., Rovida F., Demicheli V., Ajelli M., Poletti P., et al. The early phase of the COVID-19 outbreak in Lombardy, Italy. Lancet. 2020;396:e86–e87. doi: 10.1016/S0140-6736(20)32154-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Statistisches Bundesamt. Grunddaten der Krankenhäuser: 2018; 2020.
- 21.Sundhedsstyrelsen. Håndtering af COVID-19: Prognose og kapacitet i Danmark for intensiv terapi; 2020.
- 22.DIVI. Intensivregister. 2020. https://www.intensivregister.de/#/index. Accessed 8 Dec 2020.
- 23.HSE. COVID19 Daily Operations Update: Acute Hospitals. 2020. https://www.hse.ie/eng/services/news/newsfeatures/covid19-updates/covid19-daily-operations-update-2000-29-may-2020.pdf. Accessed 9 Dec 2020.
- 24.HSE. COVID-19 Committee Meeting Tuesday 2 June 2020. 2020. https://www.hse.ie/eng/services/news/media/pressrel/covid-19-committee-meeting-tuesday-2-june-2020.html. Accessed 9 Dec 2020.
- 25.Piantoni V. After years of cuts, Italy is set to double the number of ICU beds in response to Covid-19. 2020. https://www.lastampa.it/esteri/la-stampa-in-english/2020/05/07/news/after-years-of-cuts-italy-is-set-to-double-the-number-of-icu-beds-in-response-to-covid-19-1.38815375. Accessed 9 Dec 2020.
- 26.Eurostat. Hospital bed by NUTS2 regions. 2020. https://ec.europa.eu/eurostat/databrowser/view/hlth_rs_bdsrg/default/table?lang=en. Accessed 18 Dec 2020.
- 27.Ministero della Salute. Open data. 2019. http://www.dati.salute.gov.it/imgs/C_17_dataset_96_0_upFile.csv. Accessed 26 Nov 2020.
- 28.Lailor A. Number of ICU beds needed will decrease to normal levels by 1 May, OMT expects. 2020. Currently, the Netherlands has managed to double its total ICU capacity, with 2400 beds available nationally, of which 1900 are available to coronavirus patients. Accessed 9 Dec 2020.
- 29.Phua J., Weng L., Ling L., Egi M., Lim C.-.M., Divatia J.V., et al. Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Respirat Med. 2020;8:506–517. doi: 10.1016/S2213-2600(20)30161-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vahey G.M., McDonald E., Marshall K., Martin S.W., Chun H., Herlihy R., et al. Risk factors for hospitalization among persons with COVID-19-Colorado. PLoS One. 2021;16 doi: 10.1371/journal.pone.0256917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Raftery A.E., Currie J., Bassett M.T., Groves R. National Academies Press; Washington, D.C.: 2020. Evaluating data types: a guide for decision makers using data to understand the extent and spread of COVID-19. [Google Scholar]
- 32.Mateen B.A., Wilde H., Jm Dennis, Duncan A., Thomas N.J.M., McGovern A.P., et al. A geotemporal survey of hospital bed saturation across England during the first wave of the COVID-19 Pandemic (preprint) medRxiv. 2020 doi: 10.1101/2020.06.24.20139048. [DOI] [Google Scholar]
- 33.Borgan E. Norwegian COVID-19 patients: physicians surprised by length of stay on ventilators. 2020. https://sciencenorway.no/covid19-epidemic-medical-procedures/norwegian-covid-19-patients-physicians-surprised-by-length-of-stay-on-ventilators/1753844. Accessed 25 Nov 2020.
- 34.World Health Organization. Critical preparedness, readiness and response actions for COVID-19. 2020. https://apps.who.int/iris/rest/bitstreams/1283590/retrieve. Accessed 9 Dec 2020.
- 35.Strand K., Walther S.M., Reinikainen M., Ala-Kokko T., Nolin T., Martner J., et al. Variations in the length of stay of intensive care unit nonsurvivors in three Scandinavian countries. Crit Care. 2010;14:R175. doi: 10.1186/cc9279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Walther S.M., Karlström G. Quality management in intensive care: a practical guide. Cambridge University Press; 2016. National ICU registries; pp. 195–203. Guidet B, Valentin A, Flaatten H, editors. [Google Scholar]
- 37.Bauer J., Brüggmann D., Klingelhöfer D., Maier W., Schwettmann L., Weiss D.J., Groneberg D.A. Access to intensive care in 14 European countries: a spatial analysis of intensive care need and capacity in the light of COVID-19. Intensive Care Med. 2020 doi: 10.1007/s00134-020-06229-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stöß C., Steffani M., Kohlhaw K., Rudroff C., Staib L., Hartmann D., et al. The COVID-19 pandemic: impact on surgical departments of non-university hospitals. BMC Surg. 2020;20:313. doi: 10.1186/s12893-020-00970-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.