Abstract
The clinical utility of rapid genomic sequencing (rGS) for critically unwell infants and children has been well demonstrated. Parental capacity for informed consent has been questioned, yet limited empirical data exists to guide clinical service delivery. In an Australian nationwide clinical implementation project offering rGS for critically unwell infants and children, parents made a decision about testing in under a day on average. This study reports parents’ experiences of decision making for rGS within this rapid timeframe to inform pre-test counselling procedures for future practice. A nationwide sample of 30 parents, whose children were amongst the first to receive rGS, were interviewed. We found that framing and delivery of rGS require careful consideration to support autonomous decision making and avoid implicit coercion in a stressful intensive care setting. Many parents described feeling ‘special’ and ‘lucky’ that they were receiving access to expensive and typically time-consuming genomic sequencing. Thematic analysis revealed a spectrum of complexity for decision making about rGS. Some parents consented quickly and were resistant to pre-test counselling. Others had a range of concerns and described deliberating about their decision, which they felt rushed to make. This research identifies tensions between the medical imperative of rGS and parents’ decision making, which need to be addressed as rGS becomes routine clinical care.
Subject terms: Medical genomics, Genetic services, Paediatrics, Genetics research
Introduction
The clinical utility of rapid genomic sequencing (rGS) for critically unwell infants and children has been consistently demonstrated by multiple studies in different healthcare systems [1–7]. Simultaneously, concern has been expressed about parents’ ability to make informed decisions about rGS in this setting [8, 9]. In our previous study this concern was, however, not raised by genetic counsellors [10], emphasising the need for parents’ insights on this issue.
To date, research has largely focused on the acceptability of testing and post-test experience of parents, typically at a single NICU site [11–14]. This emerging research suggests a level of acceptability of rGS to parents as a diagnostic tool for their critically unwell child, and that most parents do not regret their decision to accept rGS in this setting [11, 12]. Nonetheless, parents of children undergoing rGS in acute care have been reported as having high rates of depression and anxiety relative to the general population [13] and describe themselves as being stressed and fatigued [14], highlighting the need for careful pre-test counselling to address these factors [14].
While genetic health professionals have identified challenges in providing pre-test counselling arising from the time pressure, intensive care environment and parents’ heightened emotional states [10, 14–16], parents’ experiences of pre-test counselling for rGS have not been reported. In a large Australian multi-site implementation feasibility programme of rGS delivery for critically unwell infants and children, there was less than a day on average between programme approval of a patient and parent consent for testing [17]. The swiftness of the pre-test counselling process in a stressful environment raises questions about potential impact on parents’ decision making.
The primary objective of this qualitative study was to explore parents’ experiences of rGS for their critically unwell infant or child at six sites around Australia. This paper focuses on parents’ experiences of pre-test counselling and decision making in this new setting to inform future practice and delivery of rGS.
Subjects and methods
Context
The protocol and clinical outcomes for the Acute Care Flagship study of the Australian Genomics Health Alliance have been described elsewhere [17]. Briefly, participants of the wider clinical study were critically unwell infants or children suspected of having a monogenic condition, and their families. Families were offered trio exome sequencing, with results returned approximately three to five days after consent. Pre-test counselling was conducted by either a genetic counsellor, clinical geneticist, or both. Almost all (96%) families approached agreed to participate in the wider clinical study, with just five (4%) declining rGS. The mean time from approval that a patient met the inclusion criteria to parents providing consent to participate was 0.9 days (range 0–6, 95% CI 0.7–1.1). Pathogenic and likely pathogenic variants related to the presenting phenotype were returned to families, as well as a limited number of variants of uncertain significance that were deemed to be of potentially high clinical significance. Incidental findings – findings unrelated to the clinical condition – were not returned.
Participants
Inclusion criteria for this study were all parents of children who participated in the Acute Care Flagship between March, 2018, and December, 2018. De-identified clinical data were exported from the study database for all families recruited to the Acute Care Flagship who had agreed to be contacted for further research, and who had received results at least six months prior. Participants were not required to speak English. Families were excluded if the treating team (including clinical geneticist or genetic counsellor) deemed them not currently appropriate to contact; this was decided on a case-by-case basis.
Recruitment
A recruitment email/letter, consent form and participant information statement were sent to eligible families. If no response was received within two weeks, FL made two follow-up telephone calls. If the parent agreed to interview, a mutually convenient time and place were agreed, including whether parents wished to interview separately or as a couple. For non-English-speaking parents, all documents were translated into their preferred language, and a trained medical interpreter was used for all interactions.
Data collection and analysis
FL conducted all qualitative semi-structured interviews by telephone, videoconference, or in-person, using an interpreter where required. Evidence suggests these modes provide comparable data quality [18, 19] so participants were given a choice to maximise recruitment of a geographically diverse population. The interview guide is included as Supplementary Material. Interviews were conducted with one or both parents, together or separately, depending on participant preference and availability. Interviews were audio-recorded and transcribed verbatim. For the interview involving an interpreter, only the English portions were transcribed (i.e. the interviewer and interpreter speaking). Pseudonyms were assigned to participants and their children to maintain anonymity.
Interviews were analysed concurrently with data collection using reflexive thematic analysis [20], involving familiarisation (becoming immersed in the data), generating codes (labelling sections of the transcript), constructing candidate themes (grouping codes and data into coherent themes), and revising and defining these themes through further coding and discussion. Initial codes were generated from topics in the interview guide and informed by the literature, with further codes generated inductively from transcripts. Data were also analysed for patterns related to participant characteristics including rGS outcome and whether the child was alive or deceased at the time of interview. All transcripts were coded and discussed by FL and BM to ensure rigour. Iterative data analysis was managed using NVivo 12 qualitative data analysis software [21].
In quotes presented in this paper, an ellipsis (…) reflects where a significant part of speech has been removed, and square brackets represent where a word has been replaced for clarity or to protect participant anonymity. We use words such as ‘some’ and ‘other’ to denote heterogeneity of participants’ experiences.
Ethics
This study was reviewed and approved by the Human Research Ethics Committee of The University of Melbourne (HREC ID 1853036). Participants provided voluntary, informed consent. The Australian Genomics Acute Care study received human research ethics committee approval from Melbourne Health (HREC/16/MH251).
Results
Sample
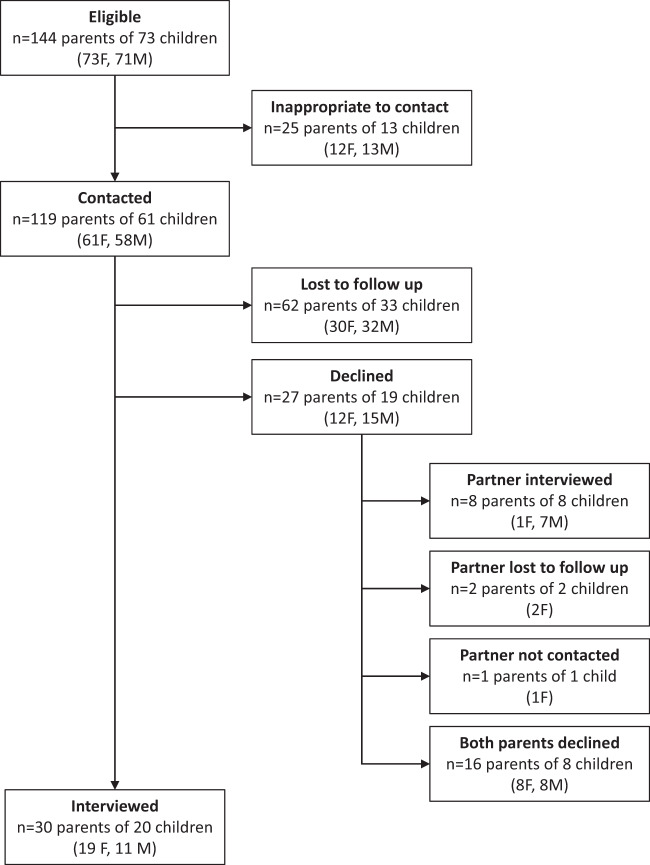
Figure 1 outlines the recruitment process and sample. Twenty-five families were considered inappropriate to contact for reasons including the child was critically unwell at the time; the child had recently died; the family were no longer in Australia; there were complex family circumstances; or the family requested no further contact from the clinical genetics service. Twenty-three interviews with 30 parents of 20 patients were conducted (June 2019–January 2020), six with both members of a couple. Sixteen were conducted by phone, five in person, and two by videoconference. One was conducted using a trained medical interpreter. Interviews averaged 53 min (range 20–98). A range of family circumstances and ethnicities were represented. A summary of patient and interviewee characteristics are provided in Tables 1 and 2.
Fig. 1. Recruitment and sample.
144 parents were eligible to participate in the study. Of these, 25 were deemed inappopriate to contact, 62 were lost to follow up, 27 declined, and 30 participated in an interview. Numbers show parents and the corresponding number of families they represent. The number of female (F) and male (M) participants are also shown for each recruitment stage.
Table 1.
Summary of case characteristics.
| Patients | Interviewees | |||
|---|---|---|---|---|
| n (%)a | Mothers | Fathers | Total n (%)a | |
| rGS outcome | ||||
| Diagnosis | 9 (45%) | 9 | 6 | 15 (50%) |
| No diagnosis | 7 (35%) | 6 | 2 | 8 (27%) |
| Uncertain result | 4 (20%) | 4 | 3 | 7 (23%) |
| Survival outcome | ||||
| Alive | 14 (70%) | 14 | 10 | 24 (80%) |
| Deceased | 6 (30%) | 5 | 1 | 6 (20%) |
| Referral source | ||||
| NICU | 13 (65%) | 12 | 9 | 21 (70%) |
| PICU | 5 (25%) | 5 | 2 | 7 (23%) |
| Ward | 2 (10%) | 2 | 0 | 2 (7%) |
| TOTAL | 20 | 19 | 11 | 30 |
aProportions are calculated within each column.
Table 2.
Summary of interviewee characteristics.
| n (%) | ||
|---|---|---|
| Gender | Female | 19 (63) |
| Male | 11 (37) | |
| Number of children | 1 | 12 (40) |
| 2 | 13 (43) | |
| 3+ | 5 (17) | |
| Language | English | 28 (93) |
| Other | 2 (7) | |
| Location | Metropolitan | 28 (93) |
| Regional | 2 (7) | |
| Ethnicity | Australian/New Zealander | 12 (40) |
| North African/Middle Eastern | 2 (7) | |
| European (Non-Finnish) | 4 (13) | |
| Asian | 2 (7) | |
| Aboriginal/Torres Strait Islander | 1 (3) | |
| Maori/Pacific Islander | 1 (3) | |
| Declined to specify/Unknown | 8 (27) | |
| TOTAL | 30 |
Of the 27 parents who declined, the partner of eight participated in an interview. The remaining 19 parents represent 11 patients; of these, seven received a diagnosis and four received no diagnosis. All were alive at the time of interview invitation.
Parental experiences
Interviews generated data on topics including parents’ experiences of searching for and understanding information about rGS and their child’s condition, accessing support, navigating relationships with health professionals, and communicating with family members and friends. The following describes the results of thematic analysis relating to the issue of decision making for rGS in intensive care.
“Mind-numbingly stressful”: the intensive care experience
The extreme stress of having a critically unwell child was evident.
“It’s literally the worst stress I’ve ever experienced in my whole life…Really, really just mind-numbingly stressful”. [Eleanor, mother of Edward, diagnosis]
Parents often hadn’t slept, eaten or showered. They were emotionally drained and overwhelmed. They described the impact on their ability to process information.
“Parents are so emotionally drained, particularly if their child is incredibly sick at the time that the testing is happening, that my only thoughts and concerns were on my baby”. [Jenny, mother of Jessica, no diagnosis, deceased]
Other stressors on the parents at the time of rapid genomic sequencing
Parents identified additional stressors beyond the hospital environment, such as caring for other children or managing work commitments.
“It was harder for Michael because he was at home with our son and I was living in hospital, so he felt very isolated ‘cause at least if I was in hospital I had access to the social worker, I had access to people around me…” [Miranda, mother of Matthew, diagnosis, deceased]
“…we’re extremely busy, we run our own business…” [Ian, father of Isaac, no diagnosis]
Families who needed to travel a long way to the hospital faced unique challenges including having to find and finance travel and accommodation.
“…the first 11 or 12 weeks, Brad was pretty much down in [city] with me the whole time. And then we did a slow transition, so he was…down in [city] for an extended weekend, type thing…And when we were discharged from the hospital…it was recommended that we didn’t go home, and so we rented an apartment…near the hospital…for five months”. [Bridget, mother of Bethany, diagnosis]
Getting ‘special access’ to rapid genomic sequencing
Parents were aware that genomic testing usually has a longer turnaround time, and that it was being expedited for their child.
“We knew that it normally takes a long process and it had been expedited”. [Ayden, father of Alex, diagnosis]
Parents used phrases such as having to have the ‘grant approved’, ‘getting on the trial’, ‘getting approval’ and ‘qualifying’ for the test, indicating they were aware that there were certain criteria to meet in order to gain access to the rapid test, and it was not automatically offered.
“They said, ‘Look, good news, you’ve been approved for the super fast-tracked one’”. [Drew, father of Declan, no diagnosis]
“Genetics came and approached us and said that…they applied for a grant for us and that it was approved, and if we’d like to go for it, then we can and then we did”. [Hannah, mother of Hilary, diagnosis]
Parents also understood that genomic testing is usually expensive, and some reported that they were pre-emptively offered the chance to self-fund should they not be eligible for the study. Parents recalled standard exome sequencing costing anywhere from $5,000 to $30,000, recognising that they would not have been able to afford it if they had had to pay for it themselves.
“…everything costs money, but to have a carrot dangled about…it was still hard to hear that there was a potential answer that was $5,000 away. If a bureaucratic process or a decision fell on the side of this costing us money, I think we would have been in a tough position to go through with it…” [Drew, father of Declan, no diagnosis]
Parents described being excited about being offered rGS, recognising the special circumstances of their participation in the research programme, and feeling grateful they received access to the technology.
“Having these options for exome sequencing and really cutting-edge research is amazing…it’s something that we’re really lucky to have even [been] offered”. [Drew, father of Declan, no diagnosis]
“…I was…really thankful, grateful that we were chosen…” [Quinn, mother of Quinton, uncertain result, deceased]
Some parents talked about how members of their treating team had to advocate for access to the test. Others described health professionals working outside usual work hours to receive results as quickly as possible.
“I think [the neonatologist] pulled some strings, or a few people went in to bat for us, which was amazing”. [Drew, father of Declan, no diagnosis]
“I think they worked weekends to sequence it all”. [Eric, father of Edward, diagnosis]
Perceptions of rapid genomic sequencing compared with other tests
Some parents felt that rGS was no different to any other test their child had had, that it was just another diagnostic tool, with the sample collected in the same way as other tests.
“It’s just a blood test, in my eyes”. [Sarah, mother of Samuel, diagnosis]
“…It was a bit lost in everything else that was happening at the time…she was getting heart tests, she was getting CTs…for us it was more or less, here’s another diagnostic route…This was one of many scenarios that they were just poking and prodding”. [Logan, father of Lyla, uncertain result]
Other parents perceived rGS as different, emphasising that the discussion surrounding rGS was more formal than other tests and that rGS could unveil information about their child’s prognosis.
“…With genetics, when it was more the overall, policies and all that…it seemed really formal…” [Quinn, mother of Quinton, uncertain result, deceased]
“It’s much different from other tests… [rGS] will come to know what will come in the future, whether in future he’ll be having this or whether he can be improving or whether he can’t be improving”. [Odette, mother of Oliver, diagnosis]
Overall, these parents felt other tests were more targeted, whereas rGS was more comprehensive, providing information about their child with both greater depth and breadth.
“I guess [rGS was] more in-depth, they said that they had their suspicions of where they were going to look, but if it wasn’t there, then they were going to go fishing somewhat…” [Bridget, mother of Bethany, diagnosis]
“…we were told that it was basically searching for everything…that medically is known…Whereas the other tests seemed to be quite specific or only looking for a range of things based on his symptoms”. [Natalie, mother of Nicholas, no diagnosis, deceased]
Approaches to decision making for rapid genomic sequencing
Parents consented to rGS within one day on average (range 0-3). Diverse approaches to decision making about rGS were evident. Some parents’ descriptions suggested a deliberative process of decision making, including consideration of a variety of concerns about the test, both for themselves and for their child. Concerns included the necessity of another blood draw, data privacy, and life insurance implications. Interviews also revealed parental concerns about the potential outcome of the test, discovering their child’s condition was genetic, and the potential for blame if the variant had been inherited from one or both parents.
In contrast, some parents described a different approach, preferring to consent to the test with little deliberative decision making, and were incredulous as to why parents would not consent. These parents were resistant to pre-test counselling, instead putting trust in the treating team to make the decision. Notably, parents did not necessarily describe the same approach to decision making as their partner. Quotes demonstrating these approaches to decision making are presented in Table 3.
Table 3.
Parents’ approaches to decision making for rapid genomic sequencing.
| Deliberative decision making |
|---|
| “…the benefits outweighed the risks”. [Eleanor, mother of Edward, diagnosis] |
| “The only concerns that I really had were taking the blood from Ryan when he just didn’t have that much to give at the time, and the distress that it caused him”. [Rachel, mother of Ryan, no diagnosis] |
| “One of the biggest concerns we had was the privacy of the data”. [Eric, father of Edward, diagnosis] |
| “I wish before we’d had the genetic testing done, that I’d gone and taken out life insurance, income protection, etcetera, because now, when we go and do that…we have to disclose that we’ve had genetic testing done…it’s something that not only impacts my son’s life, but it now impacts my life and my husband’s life…” [Eleanor, mother of Edward, diagnosis] |
| “I was just very worried because something related to the genetics make me some worried, but afterwards when they given [sic] us the final report, it was good, so I was just pleased that it’s not something wrong with our genes”. [Frances, mother of Freddie, no diagnosis] |
| “…‘cause they kept mentioning genetics…we were concerned that it was coming from one of us…no one wants to be blamed for that”. [Sarah, mother of Samuel, diagnosis] |
| Little deliberative decision making |
| “…we were in that mindset that we just wanted to get it done…” [Bridget, mother of Bethany, diagnosis] |
| “…I was just happy to sign…we were just so invested in helping George and getting to the bottom of what was going on…that I think someone probably could have slipped a contract under our nose to sell the house and we would have just signed it”. [Graham, father of George, uncertain result] |
| “I can’t comprehend why someone would say no to a test”. [Sarah, mother of Samuel, diagnosis] |
| “…it was just straight to the point, for me. Enough of the fluff, if you want to do this test, get it done. We wasted a day, probably, with the counsellor…we could have just authorised the test, ‘Yeah, no worries, go for it’. I don’t think it required the actual sit-down conversation and things that…we had. It was just…we do a test for Isaac, whatever we need to do, let’s get it done”. [Ian, father of Isaac, no diagnosis] |
| “I’m happy to have any kind of test you want…” [Tyler, father of Thomas, diagnosis] |
| “[The genetics team] had told us it would be a worthwhile thing to do, fine, let’s do it. I just had complete trust, and that came from the time and care given by the team…” [Graham, father of George, uncertain result] |
Perceptions of pressure on decision making
Parents mostly described making a decision about whether to have rGS without experiencing any pressure, and no parents described regretting their decision. Some parents were given time to themselves, away from health professionals, to read and process information, helping them to make the decision that was right for them.
“We weren’t forced into that at all, they gave us the option”. [Miranda, mother of Matthew, diagnosis, deceased]
“We were given time to digest it by ourselves and within our own space…We weren’t pushed in any one way or the other. We were given enough information to make informed decisions…” [Patrick, father of Parker, diagnosis, deceased]
However, some parents felt rushed in their decision whether to consent to rGS, explaining they felt they did not have time to adequately consider their decision.
“…it was quite rushed at the end…to be honest there wasn’t a lot of time to think about it”. [Eleanor, mother of Edward, diagnosis]
“The whole thing was quite rushed”. [Jenny, mother of Jessica, no diagnosis, deceased]
While some parents recognised the urgency of getting a result for their child as quickly as possible, others were confused.
“…they were really fast-tracking [the test] because it was a race against time”. [Quinn, mother of Quinton, uncertain result, deceased]
“I remember signing papers and it was all very, very urgent that we get my husband’s signature as well…I just remember quite a sense of urgency, so I don’t know whether the deadlines for the trial were pressing and that’s why it was so urgent for us to get paperwork signed…” [Carolyn, mother of Corey, no diagnosis, deceased]
“…[the clinical geneticist] literally ran down to take blood from my husband and I…[they] just grabbed the samples and ran, it was…almost like an emergency…It was really odd. We just thought, ‘Oh my god, what is this [person] doing? Is it that severe?’” [Kayla, mother of Kate, uncertain result]
No patterns emerged when potential relationships were considered between parental experience of decision making for rGS and elements including rGS outcome, whether the child was deceased or alive, the age of the child at time of rGS, the perceived likelihood of a suspected diagnosis, and parent characteristics.
Discussion
Our study provides novel findings that add to the limited, but growing evidence-base to guide implementation of rGS in intensive care settings, adding empirical evidence to concerns expressed by others about parents’ decision making [8, 9]. By studying a nationwide sample of 30 parents, including those whose children had died, we found greater heterogeneity in parents’ experiences than previously reported [11, 14]. Some parents found the decision to consent to rGS easy, whereas others described a more deliberative process of decision making. This diversity contrasts with the perspectives of health professionals providing care for these patients [10], whereas others have reported consistency between the experiences of parents and their health professionals [14]. Our study describes aspects of parents’ experiences that can impact on their decision making for rGS, including parental stress and perceptions of pressure to consent, raising questions about the processes around informed consent in this context. We suggest that framing and delivery of rGS requires careful consideration to support autonomous decision making and avoid implicit coercion in the stressful intensive care setting.
Approaches to decision making: no ‘one-size-fits-all’
A spectrum of complexity of decision making by parents was evident in this study, with some finding the decision to consent to rGS more straightforward than others. This may be reflected in the range of time taken to provide consent in the larger clinical study (0–6 days, with a median of one day) [17]. Further, there was diversity in the concerns and information needs of parents relating to their decision. This contrasts with previous early research suggesting that most parents find the decision to pursue rGS easy [11, 14]. Like parents in the non-urgent, outpatient setting [22], those parents who wanted to consent with little deliberative decision making were resistant to extensive pre-test counselling. In contrast, parents who required more time to decide sometimes felt rushed to consent to the test. That partners sometimes had different approaches to decision making further adds to the complexity of pre-test counselling in this setting. This diversity in decision-making needs emphasises the importance of individualised care for families offered rGS in intensive care, and the challenges for those providing pre-test counselling [10]. Nonetheless, there are aspects of parents’ experiences that can impact their decision-making ability.
Understanding choice architecture and decision making for rGS
The concept of ‘choice architecture’ refers to the context in which a decision is made, and includes factors such as the physical environment, the identity of the person (in this case, the health professional) presenting the choice, and the way in which this health professional frames the decision [23]. In the context of rGS, the health professional may be the intensive care clinician, clinical geneticist and/or genetic counsellor involved in the care of the patient. Choice architecture is inherent to a decision or choice being offered, and takes into account the many elements influencing an individual’s decision. Descriptions by parents in this study of the stressful environment of the intensive care setting, the complexity and uncertainty of genomic sequencing, and the ‘buzz’ surrounding new and exciting technology suggest the combination of these elements form part of the choice architecture of rGS in intensive care, impacting parents’ decisions to consent to or decline the test.
As also described by others, the physical environment in which parents are often asked to make such decisions further adds to the stress of having a critically unwell child [11]. However, while privacy and quiet are important to parents in intensive care [24], genetic counsellors working in this setting have reported challenges in finding a quiet space for pre-test counselling [10].
Irrespective of their approach to decision making, parents described feeling like they were getting ‘special access’ to rGS for their child. The consistency of this perception amongst participants suggests the influence of health professionals’ framing of the test or study participation. Although parents in this study felt they were free to consent to or decline rGS, feeling ‘special’ and ‘lucky’ may impact on parents’ willingness to decline. Moreover, the perception that discussions around rGS were more ‘formal’ than those for other investigations and that rGS has the ability to unveil unique, otherwise inaccessible information could further influence parents’ decisions. Add to this parents’ reports of health professionals advocating to get their child access to expensive rGS, and the possibility that some parents may not wish to appear ungrateful by declining must be entertained. Framing of the test and actions surrounding its delivery require careful consideration by health professionals to support parents’ autonomous decision making and avoid implicit coercion.
As this test is adopted as part of routine clinical practice, some elements of the choice architecture around the decision will be eliminated, such as the extensive research consent required and potential rationing of test availability. While the novelty and excitement of rGS may diminish over time, parental stress and the complexity of genomic sequencing are factors that will continue to impact parents’ decisions as part of the wider choice architecture surrounding rGS in intensive care.
Implications for practice: informed consent
Because of the many factors impacting parents’ decision making, some have proposed that there are limitations to how ‘informed’ consent can be in neonatal and paediatric intensive care settings [25], let alone for genomic sequencing [12, 14]. Aspects of rGS in intensive care that others have speculated may impact parents’ decision making [8, 9] were evident in our research. Despite suggestions that extrapolation of traditional approaches to informed consent for genetic testing may not be appropriate for genomic sequencing [9, 22, 26], few have provided comprehensive solutions to this problem. In neonatal and paediatric intensive care settings, it has been proposed that more directive counselling may be suitable for rGS [9].
Hill and colleagues report that health professionals’ and parents’ perspectives are consistent, with parents largely finding the decision to consent to rGS straightforward [14]. In contrast, our studies––with parents’ perspectives reported here and those of health professionals reported previously [10]––indicate a divergence in perceptions. Despite our findings that some parents feel rushed and pressured to consent to rGS, our previous research showed that health professionals did not raise concerns about parents’ informed decision making in intensive care. Although all parents in this study did make a decision about rGS and did not describe regretting their decision, this divergence suggests that some parents’ needs for additional time for deliberative decision making are not being recognised by health professionals in this setting.
Nevertheless, while some parents desired more time, others wanted to consent to rGS with little consideration. Helping patients to engage with the risks, as well as benefits, of testing is not a new challenge for genetic health professionals [27, 28]. While there is little evidence for successful strategies to facilitate engagement of clients who do not wish to deliberate or fully consider the potential implications of testing, genetic counsellors are experienced in pre-test counselling to facilitate this decision making.
Our research highlights the importance of a supportive, guided and considered approach to facilitating parents’ decision making, irrespective of their desired approach. Individualised pre-test counselling for rGS in intensive care is therefore needed to support a careful process that balances the medical imperative of rGS with parents’ diverse decision-making needs, including consideration for diversity in approaches between partners. As our previous research suggests, genetic counsellors can provide the necessary skills and expertise to deliver patient-centred pre-test counselling for rGS to address this diversity [10].
Study limitations and further research
The parents from the Acute Care Flagship who did not participate in this qualitative study (excluded, declined, or lost to follow up) may have had different experiences. The perspectives of those who declined rGS for their child would make an important contribution to informing pre-test counselling protocols for rGS. Unfortunately, those who declined rGS are not participants in the overarching study and so could not be approached for interview. Additionally, quotes presented from non-English-speaking participants are the interpreter’s words. While this interview did not raise different or additional concerns to those conducted in English, further research is needed to explore the experiences of those who are navigating rGS in an unfamiliar language. While no patterns emerged to suggest parental characteristics influenced their experiences of decision making for rGS, there may be benefit in testing this in a larger quantitative study. Some aspects of the choice architecture of rGS in intensive care could also be explored further. Recording of clinical consultations may shed light on factors such as the way the test is framed by health professionals, and how this impacts parents’ decisions. As health professionals’ experience grows over time, their practice and perspectives are likely to evolve [10, 14]. Exploration of the experiences of the variety of health professionals working in this setting as rGS moves from a research-funded offering into routine clinical care––and their impact on parents’ decision making––would provide valuable insights for those considering implementing or improving services.
Conclusion
Our study demonstrates both commonalities and variation in the experiences and needs of parents faced with deciding whether their critically unwell child should have rGS. Interestingly, the results of our study diverge from our previous study reporting on the views of health professionals, who did not raise concerns for parents’ informed decision making in this setting [10], despite some parents in this study describing feeling rushed and pressured to consent to rGS. We suggest this disparity reflects the novelty of practice in this setting, and indicates a clear need for the ongoing, iterative development of processes that acknowledge the views and experiences of both families and health professionals in this context. The challenge is of course to ensure pre-test counselling is sufficiently tailored to support parents’ diverse decision-making needs in this uniquely high-stress environment, while also meeting the imperative that genomic information is available to inform time-sensitive medical management decisions. As practice becomes more established in this setting, nuanced analysis of the impact of clinical presentation, test outcomes and turn-around times on clinical utility will determine the extent of flexibility afforded to parents in the decision-making process. As the clinical utility of rGS increases, so will the medical imperative for parents to consent, potentially further increasing pressure on decision making. This will further challenge parents’ ability to provide informed consent or dissent, making it essential that health professionals experienced in facilitating decision making within this rapid timeframe are involved in the process. The implementation of rGS in acute care is growing and changing rapidly; ongoing collaborative research on its implementation, parents’ perspectives, and clinical outcomes will be critical in informing service delivery as this test is adopted into routine clinical care.
Supplementary information
Acknowledgements
This study partially fulfils the requirements for FL’s Doctor of Philosophy from The University of Melbourne. The authors thank the participants for their involvement.
Funding
This work was supported by the Victorian Government’s Operational Infrastructure Support Programme and a grant from the Australian National Health & Medical Research Council (GNT1113531). FL is supported by a Melbourne Children’s Postgraduate Health Research Scholarship funded by the Royal Children’s Hospital Foundation. The Australian Genomics Health Alliance (Australian Genomics) project is funded by an NHMRC Targeted Call for Research grant (GNT1113531). The Acute Care flagship project was also supported by a Royal Children’s Hospital Foundation grant (2017-906), and Sydney Children’s Hospital Network, Channel 7 Children’s Research Foundation Grant.
Data availability
The datasets generated during the current study are available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Ethical approval
This study was reviewed and approved by the Human Research Ethics Committee of The University of Melbourne (HREC ID 1853036). Participants provided voluntary, informed consent. The Australian Genomics Acute Care study received human research ethics committee approval from Melbourne Health (HREC/16/MH251).
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s41431-021-00950-6.
References
- 1.Farnaes L, Hildreth A, Sweeney NM, Clark MM, Chowdhury S, Nahas S, et al. Rapid whole-genome sequencing decreases infant morbidity and cost of hospitalization. NPJ Genom Med. 2018;3:10. doi: 10.1038/s41525-018-0049-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kingsmore SF, Cakici JA, Clark MM, Gaughran M, Feddock M, Batalov S, et al. A randomized, controlled trial of the analytic and diagnostic performance of singleton and trio, rapid genome and exome sequencing in ill infants. Am J Hum Genet. 2019;105:719–33. doi: 10.1016/j.ajhg.2019.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meng L, Pammi M, Saronwala A, Magoulas P, Ghazi AR, Vetrini F, et al. Use of exome sequencing for infants in intensive care units: ascertainment of severe single-gene disorders and effect on medical management. JAMA Pediatr. 2017;171:e173438. doi: 10.1001/jamapediatrics.2017.3438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mestek-Boukhibar L, Clement E, Jones WD, Drury S, Ocaka L, Gagunashvili A, et al. Rapid Paediatric Sequencing (RaPS): comprehensive real-life workflow for rapid diagnosis of critically ill children. J Med Genet. 2018;55:721–8. doi: 10.1136/jmedgenet-2018-105396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sanford EF, Clark MM, Farnaes L, Williams MR, Perry JC, Ingulli EG, et al. Rapid whole genome sequencing has clinical utility in children in the PICU. Pediatr Crit Care Med. 2019;20:1007–20. doi: 10.1097/PCC.0000000000002056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stark Z, Lunke S, Brett GR, Tan NB, Stapleton R, Kumble S, et al. Meeting the challenges of implementing rapid genomic testing in acute pediatric care. Genet Med. 2018;20:1554–63. doi: 10.1038/gim.2018.37. [DOI] [PubMed] [Google Scholar]
- 7.Petrikin JE, Cakici JA, Clark MM, Willig LK, Sweeney NM, Farrow EG, et al. The NSIGHT1-randomized controlled trial: rapid whole-genome sequencing for accelerated etiologic diagnosis in critically ill infants. NPJ Genom Med. 2018;3:6. doi: 10.1038/s41525-018-0045-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Diamonstein CJ. Factors complicating the informed consent process for whole exome sequencing in neonatal and pediatic intensive care units. J Genet Couns. 2019;28:256–62. doi: 10.1002/jgc4.1097. [DOI] [PubMed] [Google Scholar]
- 9.Gyngell C, Newson AJ, Wilkinson D, Stark Z, Savulescu J. Rapid challenges: ethics and genomic neonatal intensive care. Pediatr. 2019;143:S14–S21. doi: 10.1542/peds.2018-1099D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lynch F, Nisselle A, Gaff CL, McClaren B. Rapid acute care genomics: challenges and opportunities for genetic counselors. J Genet Couns. 2020;30:30–41. doi: 10.1002/jgc4.1362. [DOI] [PubMed] [Google Scholar]
- 11.Aldridge CE, Osiovich H, Siden H, RAPIDOMICS Study, GenCOUNSEL Study, Elliott AM. Rapid genome-wide sequencing in a neonatal intensive care unit: A retrospective qualitative exploration of parental experiences. J Genet Couns 2021;30:616– 629. [DOI] [PubMed]
- 12.Brett GR, Martyn M, Lynch F, de Silva MG, Ayres S, Gallacher L, et al. Parental experiences of ultrarapid genomic testing for their critically unwell infants and children. Genet Med. 2020;22:1976–85. doi: 10.1038/s41436-020-0912-4. [DOI] [PubMed] [Google Scholar]
- 13.Smith EE, du Souich C, Dragojlovic N, Study C, Study R, Elliott AM. Genetic counseling considerations with rapid genome‐wide sequencing in a neonatal intensive care unit. J Genet Couns. 2019;28:263–72. doi: 10.1002/jgc4.1074. [DOI] [PubMed] [Google Scholar]
- 14.Hill M, Hammond J, Lewis C, Mellis R, Clement E, Chitty LS. Delivering genome sequencing for rapid genetic diagnosis in critically ill children: parent and professional views, experiences and challenges. Eur J Hum Genet. 2020;28:1529–40. doi: 10.1038/s41431-020-0667-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stark Z, Nisselle A, McClaren B, Lynch F, Best S, Long JC, et al. Attitudes of Australian health professionals towards rapid genomic testing in neonatal and paediatric intensive care. Eur J Hum Genet. 2019;27:1493–501. doi: 10.1038/s41431-019-0429-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ayres S, Gallacher L, Stark Z, Brett GR. Genetic counseling in pediatric acute care: Reflections on ultra‐rapid genomic diagnoses in neonates. J Genet Couns. 2019;28:273–82. doi: 10.1002/jgc4.1086. [DOI] [PubMed] [Google Scholar]
- 17.Australian Genomics Health Alliance Acute Care Flagship. Feasibility of ultra-rapid exome sequencing in critically ill infants and children with suspected monogenic conditions in the Australian public health care system. JAMA. 2020;323:2503–11. doi: 10.1001/jama.2020.7671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sturges JE, Hanrahan KJ. Comparing telephone and face-to-face qualitative interviewing: a research note. Qual Res. 2004;4:107–18. doi: 10.1177/1468794104041110. [DOI] [Google Scholar]
- 19.Novick G. Is there a bias against telephone interviews in qualitative research? Res Nurs Health. 2008;31:391–8. doi: 10.1002/nur.20259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Braun V, Clarke V, Hayfield N, Terry G Thematic Analysis. In: Liamputtong P (ed). Handbook of Research Methods in Health Social Sciences. Springer: Singapore; 2019: pp 843–60.
- 21.NVivo qualitative data analysis software [computer program]. Version 122018.
- 22.Tabor HK, Stock J, Brazg T, McMillin MJ, Dent KM, Yu J, et al. Informed consent for whole genome sequencing: a qualitative analysis of participant expectations and perceptions of risks, benefits, and harms. Am J Med Genet A. 2012;158A:1310–9. doi: 10.1002/ajmg.a.35328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Blumenthal‐Barby J, Opel DJ. Nudge or grudge? Choice architecture and parental decision‐making. Hastings Cent Report. 2018;48:33–39. doi: 10.1002/hast.837. [DOI] [PubMed] [Google Scholar]
- 24.Latour JM, van Goudoever JB, Schuurman BE, Albers MJIJ, van Dam NAM, Dullaart E, et al. A qualitative study exploring the experiences of parents of children admitted to seven Dutch pediatric intensive care units. Intensive Care Med. 2011;37:319–25. doi: 10.1007/s00134-010-2074-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Janvier A, Lantos J, Aschner J, Barrington K, Batton B, Batton D, et al. Stronger and more vulnerable: a balanced view of the impacts of the NICU experience on parents. Pediatr. 2016;138:e20160655. doi: 10.1542/peds.2016-0655. [DOI] [PubMed] [Google Scholar]
- 26.Rego S, Grove ME, Cho MK, Ormond KE. Informed consent in the genomics era. Cold Spring Harb Perspect Med. 2020;10:a036582. doi: 10.1101/cshperspect.a036582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Marteau TM. Towards informed decisions about prenatal testing: a review. Prenat Diagn. 1995;15:1215–26. doi: 10.1002/pd.1970151304. [DOI] [PubMed] [Google Scholar]
- 28.McAllister M. Predictive genetic testing and beyond: a theory of engagement. J Health Psych. 2002;7:491–508. doi: 10.1177/1359105302007005628. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during the current study are available from the corresponding author on reasonable request.