Abstract
This report describes a case of an adult rhabdomyoma (ARM) occurring in the oral cavity. A 47-year-old man was referred for the diagnosis of a painless, well-circumscribed, submucous nodule located on the floor of the mouth, measuring approximately 6.0 cm in length. Computed tomography revealed a well-defined, solid, and hypodense mass. A benign salivary gland or mesenchymal tumor were the main diagnostic hypotheses. Under local anesthesia, the patient underwent surgical excision. Microscopically, the tumor comprised large polygonal well-defined cells with abundant, eosinophilic granular cytoplasm with cross striations. No atypia or mitosis was observed. The cells were positive for muscle-specific actin, desmin, and sarcomeric alpha-actin. Based on these features, a diagnosis of ARM was established. No recurrence was observed after 48 months. Although rare, ARM should be considered in the differential diagnosis of oral submucosal nodules, especially those located on the floor of the mouth.
Keywords: Benign neoplasms, Diagnosis, Differential, Immunohistochemistry, Mouth, Rhabdomyoma, Therapeutics
History and Clinical Findings
A 47-year-old man was referred for the evaluation of an oral, painless, slow-growing mass with approximately 2 years of evolution. The patient complained of dysphagia and discomfort during speech. Intraoral examination revealed a large, painless, well-circumscribed, and non-tender mass located on the right floor of the mouth, measuring approximately 6.0 cm in length (Fig. 1). The lesion was recovered by smooth, intact, and normal-colored mucosa. The tongue could not protrude normally due to the superior and posterior displacement of the lesion. Axial section computerized tomography images showed a well-delimited, solid, hypodense mass located on the floor of the mouth/submandibular region. The main hypotheses for diagnosis were a benign salivary gland tumor as a pleomorphic adenoma and a benign mesenchymal tumor. As the lesion was well delimited, it was surgically excised under local anesthesia.
Fig. 1.
Large, painless, well-circumscribed submucous nodule located at the right side of the floor of the mouth. The lesion was covered by smooth, intact, and normal-color mucosa
Diagnosis and Treatment
Gross examination revealed a bilobulated nodule with an irregular surface, brown coloring, and fibrous consistency, measuring 6.9 × 3.2 × 2.0 cm. Microscopically, at low magnification, the lesion appeared as a well-circumscribed and partially encapsulated nodule with irregular margins (Fig. 2A). The tumor comprised large polygonal cells with well-defined borders, with central or eccentric nuclei and prominent nucleoli (Fig. 2B–D). The cells exhibited abundant, eosinophilic, and granular cytoplasm, which often presented complete or partial vacuolization; so-called “spider cells” (Fig. 2B–D). Cross-striations in the cytoplasm were also observed, and there were no atypia or mitoses (Fig. 2D). In addition, hypocellular areas formed by fibrous connective tissue were also observed. Immunohistochemically, the tumor cells were positive for muscle-specific actin (HHF-35, 1:800; Dako, Glostrup, Denmark), desmin (D33, 1:800, Dako) (Fig. 3A), and sarcomeric alpha-actin (EP2529Y, 1:300, Abcam, Cambridge, England) (Fig. 3B). In contrast, the cells were negative for calponin (CALP, 1:600, Dako), H-caldesmon (h-CD, 1:400, Dako), and myogenin (F5D, 1:500, Dako). Thus, a diagnosis of ARM was established.
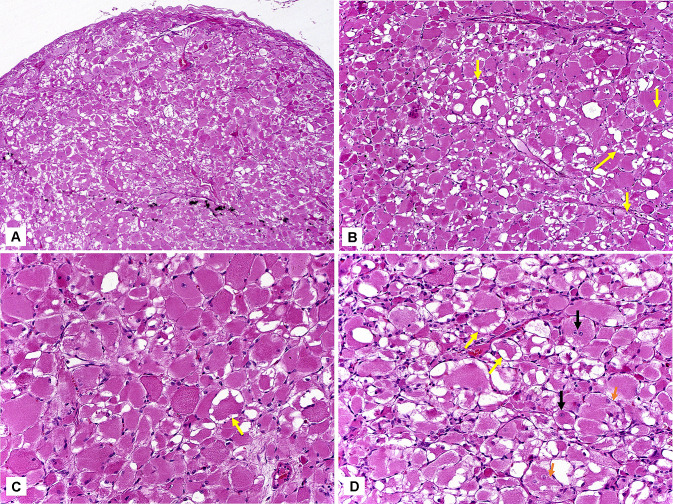
Fig. 2.
A Microscopically, at low magnification, the lesion appeared as a well-circumscribed and partially encapsulated nodule, with irregular margins (hematoxylin-eosin, 50x). B Large polygonal cells exhibited abundant, eosinophilic, and granular cytoplasm, which often presented complete or partial vacuolization; so-called “spider cells” (yellow arrows) (hematoxylin-eosin, 100x). C Large tumor cells with well-defined borders, and central or eccentric nuclei. Cytoplasmic vacuolization is also observed (“spider cells”—yellow arrows) (hematoxylin-eosin, 200x). D Most cells exhibiting granular cytoplasm, with complete or partial vacuolization (“spider cells”—yellow arrows). Prominent nucleoli (black arrows) and cross-striations (orange arrows) were also observed (hematoxylin-eosin, 200x)
Fig. 3.
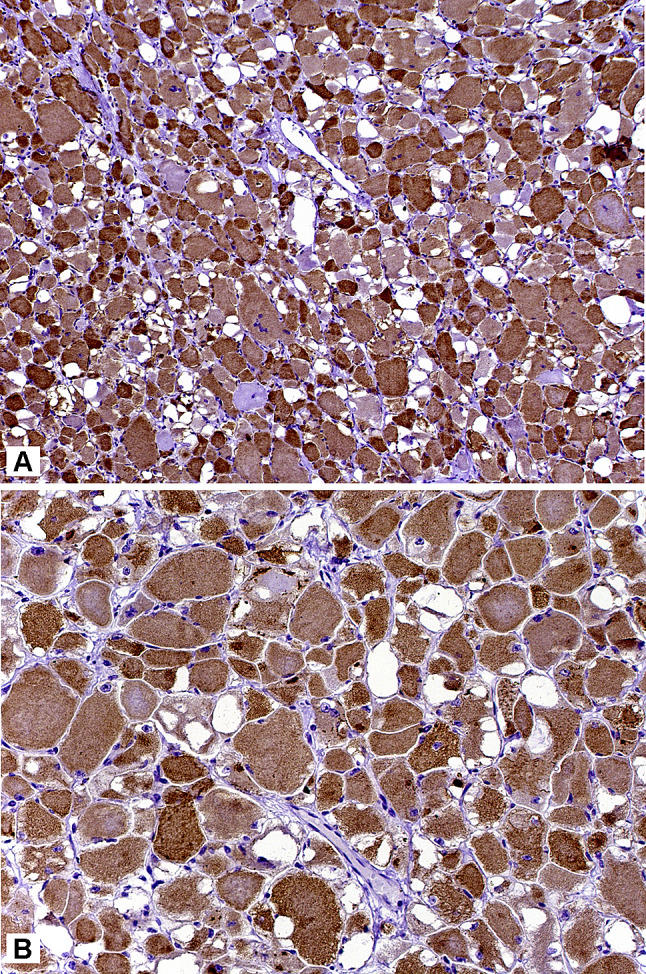
A Tumor cells presenting strong positivity for desmin (streptavidin-biotin-peroxidase method, 100x). B Tumor cells exhibiting strong positivity for sarcomeric alpha actin. Cross-striations are evident (streptavidin-biotin-peroxidase method, 400x)
The patient received clinical and imaging follow-up, with no signs of recurrence 48 months after treatment.
Discussion
Rhabdomyoma (RM) is an uncommon benign mesenchymal tumor that accounts for approximately 2% of all striated muscle tumors. It is usually classified into cardiac and extracardiac forms [1, 2]. Cardiac RM occurs more frequently in young children and is often associated with tuberous sclerosis, neurofibromatosis, and sebaceous adenomas [1, 3, 4]. Extracardiac RMs are rare and classified into adult and fetal types, depending on the degree of differentiation. RM also occurs as a genital type located in the vagina and vulva [1, 5].
Adult rhabdomyoma (ARM) is a rare benign neoplasm with differentiation of mature skeletal muscle. ARM is often solitary (70%) but may be multinodular (26%), and rarely multicentric (4%) [1, 3, 6, 7]. ARM occurs most commonly in men over 50 years of age, and shows a predilection for the head and neck region, followed by the extremities, esophagus, stomach, mediastinum, orbit, prostate, and intracranial regions. ARM is rare in the oral cavity and, to date, about 80 cases, including the present one, have been reported in the English-language literature (Table 1) [1–61]. The fetal type also typically involves the head and neck region, tends to occur at younger ages, and rarely affects adults, whereas the genital type is found in the vagina and vulva of young and middle-aged women [6, 8]. The present case fulfilled the ARM criteria.
Table 1.
Oral adult rhabdomyoma published in the English-language literature
| Authors | Year | Age (Years) | Sex | Site | Duration (months) | Follow-up |
|---|---|---|---|---|---|---|
| Beyer and Blair | 1948 | 52 | M | Floor of the mouth | 24 | No recurrence at 7 months |
| Mish | 1958 | 21 | F | Tongue | 36 | No recurrence at 48 months |
| Horn | 1960 | 65 | F | Floor of the mouth | 48 | NA |
| Sirsat and Vakil | 1962 | 42 | F | Soft Palate | 2 | NA |
| Tsukata and Pickren | 1965 | 81 | M | Floor of the mouth | 3 | No recurrence at 72 months |
| Kay et al. | 1969 | 64 | F | Floor of the mouth | 2 | NA |
| Assor and Thomas | 1969 | 59 | M | Submandibular region (multifocal) | 6 | NA |
| Wyatt et al. | 1970 | 54 | M | Tongue | 4 | No recurrence at 60 months |
| Tandler et al. | 1970 | 69 | M | Lip | NA | NA |
| Olofsson | 1972 | 36 | M | Floor of the mouth | 18 | No recurrence at 24 months |
| Albrechtensen et al. | 1974 | 62 | M | Floor of the mouth | NA | NA |
| Albrechtensen et al. | 1974 | 29 | – | Floor of the mouth | NA | NA |
| Ferracini et al. | 1977 | 40 | M | Floor of the mouth | NA | NA |
| Jones and Buntine | 1977 | 49 | M | Floor of the mouth | NA | NA |
| Caracta et al. | 1978 | 55 | M | Submandibular region | NA | NA |
| Everson and Merchant | 1978 | 59 | M | Floor of the mouth | 36 | NA |
| Heiden et al. | 1978 | 50 | F | Soft palate | NA | NA |
| Weitzner et al. | 1979 | 60 | M | Soft palate | 2 | No recurrence at 24 months |
| Solomon and Tolete-Velcek | 1979 | 11 | M | Tongue | NA | NA |
| Neville and McConnel | 1981 | 58 | M | Floor of the mouth (multifocal) | NA | NA |
| Warner et al. | 1981 | 66 | F | Submandibular region | NA | NA |
| Gardner and Corio | 1983 | 60 | M | Submandibular region (multifocal) | NA | NA |
| Schlossnagle et al. | 1983 | 65 | F | Submandibular region (multifocal) | NA | NA |
| Reid and Smith | 1985 | 39 | M | Floor of the mouth | NA | NA |
| Bock and Bock | 1987 | 72 | M | Soft palate | NA | No recurrence at 72 months |
| Bertholf et al. | 1988 | 65 | M | Floor of the mouth | 4 | No recurrence at 9 months |
| Nam et al. | 1990 | – | Base of the tongue | NA | NA | |
| Walker and Laszewski | 1990 | 76 | M | Tongue (multifocal) | NA | NA |
| Sangueza et al. | 1990 | 84 | M | Tongue | NA | NA |
| Garcia-Ruiz et al. | 1991 | 74 | M | Submandibular region | 60 | No recurrence at 12 months |
| Napier et al. | 1991 | 59 | M | Floor of the mouth | NA | No recurrence at 48 months |
| Gibas and Miettinen | 1992 | 34 | M | Soft palate | NA | NA |
| Horn et al. | 1992 | 52 | F | Floor of the mouth | NA | NA |
| Shemen et al. | 1992 | 53 | M | Floor of the mouth (multifocal) | NA | NA |
| Shemen et al. | 1992 | 75 | M | Floor of the mouth | NA | NA |
| Fortson et al. | 1993 | 71 | M | Submandibular region (multifocal) | NA | NA |
| Kapadia et al. | 1993 | 46 | M | Tongue | NA | Recurrence at 96 and 102 months |
| Kapadia et al. | 1993 | 81 | F | Floor of the mouth | NA | NA |
| Kapadia et al. | 1993 | 75 | F | Soft palate | NA | No recurrence at 221 months |
| Kapadia et al. | 1993 | 36 | M | Buccal mucosa | NA | Recurrence at 72 months |
| Kapadia et al. | 1993 | 51 | F | Soft palate | NA | No recurrence at 216 months |
| Kapadia et al. | 1993 | 59 | M | Base of the tongue | NA | Recurrence at 2 months |
| Kapadia et al. | 1993 | 60 | M | Submandibular region | NA | No recurrence 27 months |
| Kapadia et al. | 1993 | 55 | M | Floor of the mouth | NA | Recurrence at 79 and 91 mo. No recurrence at 75 months |
| Kapadia et al. | 1993 | 69 | F | Base of tongue | NA | Recurrence at 132 mo. No recurrence at 156 months |
| Kapadia et al. | 1993 | 49 | F | Soft palate | NA | NA |
| Zachariades et al. | 1994 | 49 | M | Buccal mucosa | NA | NA |
| Zbaren et al. | 1995 | 64 | M | Submandibular region | NA | NA |
| Bastian and Brocker | 1998 | 75 | M | Lip | NA | NA |
| Ballester et al. | 2000 | – | – | Tongue | NA | NA |
| Moriniere et al. | 2001 | – | – | Base of tongue | NA | NA |
| Fukuda et al. | 2003 | 51 | M | Base of tongue | NA | NA |
| Favia et al. | 2003 | 58 | M | Floor of the mouth | NA | No recurrence at 144 months |
| Favia et al.gil | 2003 | 63 | F | Submandibular region | NA | No recurrence at 168 months |
| McGregor et al. | 2003 | 78 | M | Floor of the mouth | 12 | NA |
| Delides et al. | 2005 | 59 | M | Tongue (multifocal) | NA | NA |
| Hansen et al. | 2005 | 82 | F | Floor of the mouth | NA | NA |
| Liess et al. | 2005 | 69 | M | Submandbular region (multifocal) | NA | NA |
| Bellis et al. | 2006 | 62 | M | Submandibular region | 24 | No recurrence at 72 months |
| De Medts et al. | 2007 | 65 | M | Submandibular region (multifocal) | NA | NA |
| Bizon et al. | 2008 | 65 | M | Submandibular region (multifocal) | NA | NA |
| Catalfamo et al. | 2010 | 52 | M | Submandibular region | 24 | No recurrence at 48 months |
| Etit et al. | 2010 | 67 | M | Base of tongue | NA | NA |
| Gupta et al. | 2010 | 43 | M | Floor of the mouth | NA | NA |
| Gupta et al. | 2010 | 37 | M | Bilateral submandibular region | NA | No recurrence at 2 months |
| Parara et al. | 2010 | 69 | M | Floor of the mouth | 3 | No recurrence at 24 months |
| Maglio et al. | 2012 | 72 | M | Submandibular region | NA | – |
| Sirera and Sempere | 2012 | 54 | M | Floor of the mouth | 12 | No recurrence at 36 months |
| Zhang et al. | 2012 | 78 | M | Floor of mouth (multifocal) | 2 | No recurrence at 24 months |
| Vera-Sirera and Vera-Sempere | 2012 | 54 | M | Floor of the mouth | 12 | No recurrence at 36 months |
| de Tray | 2013 | 55 | M | Submandibular region (multifocal) | NA | NA |
| Schlittenbauer et al. | 2013 | 38 | M | Buccal mucosa | 30 | No recurrence at 2 months |
| Amelia Souza et al. | 2013 | 40 | F | Floor of the mouth | 6 | No recurrence at 24 months |
| Mengoli et al. | 2016 | 48 | M | Lip | NA | NA |
| Mistry | 2017 | 60 | M | Bilateral submandibular region | NA | NA |
| Andrade | 2018 | 11 | F | Tongue | 4 | NA |
| Dau et al. | 2019 | 65 | M | Soft palate (multifocal) | 12 | No recurrence at 36 months |
| Yadav et al. | 2019 | 55 | F | Floor of the mouth | 2 | NA |
| Hakim et al. | 2020 | 56 | M | Floor of the mouth | 24 | No recurrence at 12 months |
| Present case | 2021 | 47 | M | Floor of the mouth | 24 | No recurrence at 48 months |
M male, F female, NA not available
According to previously published cases, oral ARM more commonly affects men (75%), with a male:female ratio of 3:1, and a mean age of 57 years, with a peak incidence between the sixth and seventh decades of life [1–9]. Most cases occur on the floor of the mouth/submandibular region (49–61.2%), followed by the tongue base (16–20%), soft palate (9–11.2%), buccal mucosa (3–3.8%), and lip (3–3.8%) [1–61]. Some patients (14 cases, 17.5%) present with multifocal lesions [6, 10, 22, 24, 25, 30, 36, 37, 47, 49, 51, 52, 57, 60]. The lesions vary in size from a few millimeters to 15 cm [1–61]. Similar features were observed in the present case.
Clinically, oral ARM usually presents as a painless, slow-growing, well-circumscribed, homogeneous, non-tender, and mobile submucosal nodule. However, depending on the size and site of occurrence, such as the floor of the mouth, displacement of the tongue, dysphagia, dyspnea and/or apnea, and facial asymmetry may occur [1–61]. In our case, the patient presented with dysphagia and difficulty during speech. The mean time of evolution is 16 months, ranging from 2 to 60 months [1–61]. The clinical differential diagnosis depends on the location and may include benign and malignant salivary gland tumors and benign mesenchymal tumors, as considered in the present case.
Histologically, ARM is characterized by polygonal cells of variable size with abundant eosinophilic and granular cytoplasm. Cross-striations are typically readily identifiable. Mitoses and necrosis are absent. Immunohistochemical reactions confirm skeletal muscle differentiation [3, 10]. Histopathological differential diagnoses include lesions consisting of cells with abundant eosinophilic cytoplasm, such as a granular cell tumor, hibernoma, and oncocytoma [11]. However, none of these tumors present with cross-striations or glycogen. In addition, paraganglioma and crystal storage histiocytosis should also be considered [1, 14].
Granular cell tumors are characterized by cells showing large and eosinophilic cells, with finely granular cytoplasm devoid of cross-striations and defined borders characteristics of ARM cells. Tumor cells are strongly positive for S-100 protein, and skeletal muscle markers are typically absent [1, 6]. Hibernomas consist of cells containing diverse intracytoplasmic lipid droplets tending to show centrally placed nuclei, while ARM cells have predominantly peripherally located nuclei. Immunohistochemically, cells display strong cytoplasmic positivity for S-100 [14]. Oncocytoma is a benign salivary gland neoplasm comprising polyhedral cells rich in mitochondria that show finely granular and eosinophilic cytoplasm. Tumor cells are positive for epithelial markers, whereas muscular markers are negative [2, 3]. Rhabdomyosarcomas may also be considered but are composed of spindle-shaped or rounded cells with atypical and pleomorphic nuclei, occasionally presenting cross-striations. Usually, obvious nuclear atypia and pleomorphism allow the distinction between rhabdomyosarcoma and rhabdomyoma [1, 12]. Moreover, rhabdomyosarcomas are ill-circumscribed and infiltrative tumors [12].
Cardiac RM is often associated with tuberous sclerosis complex, whereas extracardiac forms are usually not. Cases of fetal RM have been described in patients with nevoid basal cell carcinoma syndrome with homozygous inactivating mutations in the PTCH gene [62]. In addition, transcriptional activation of PTCH has been observed in all sporadic adult and fetal RMs. This finding suggests that dysregulation of Hedgehog signaling may play an important role in the pathogenesis of syndromic and sporadic RMs [62].
The treatment of ARM involves surgical excision with preservation of the surrounding tissues [6, 10]. Recurrence is uncommon in oral ARM but may occur, especially in cases with incomplete surgical excision or in which the tumor appears as a multinodular lesion [4, 10]. Only 32 (40%) cases reported clinical follow-up, 5 (15.6%) of which experienced relapse after treatment (ranging from 2 to 132 months) [1–61]. As recurrence may be observed after several years, periodic follow-up is essential [6].
In summary, although rare, ARM has a predilection for the head and neck region. This lesion should be considered in the differential diagnosis of submucosal nodules mainly affecting the floor of the mouth.
Author Contributions
Conceptualization: DECP; EJAC. Supervision: DECP; OPA. Visualization: EJAC. Writing—original draft: ACLSL; STS. Writing—review & editing: DECP; JFLC; OPA.
Funding
Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior, (CAPES), Finance Code 001, Brazil.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Mengoli MC, Jukna A, Cesinaro AM. Rhabdomyoma of the lip: a case report with review of the literature. Am J Dermatopathol. 2016;38(2):154–7. doi: 10.1097/DAD.0000000000000444. [DOI] [PubMed] [Google Scholar]
- 2.Mistry VN, Whitfield PH, Brown AN. Bilateral submandibular rhabdomyomas: case report. Br J Oral Maxillofacc Surg. 2017;55(6):653–4. doi: 10.1016/j.bjoms.2017.03.009. [DOI] [PubMed] [Google Scholar]
- 3.Vera-Sirera B, Vera-Sempere F. Adult rhabdomyoma with oncocytic changes affecting the floor of the mouth: optical, immunohistochemical, and ultrastructural study. J Craniofacc Surg. 2012;23(5):e412-5. doi: 10.1097/SCS.0b013e31825dace7. [DOI] [PubMed] [Google Scholar]
- 4.Schlittenbauer T, Rieker R, Amann K, Schmitt C, Wehrhan F, Mitsimponas K, Schlegel KA, Agaimy A. Recurrent adult-type rhabdomyoma: a rare differential diagnosis of “swellings in the masticatory muscle". J Craniofacc Surg. 2013;24(5):e504-7. doi: 10.1097/scs.0b013e31827c85ee. [DOI] [PubMed] [Google Scholar]
- 5.Etit D, Bayol U, Cumurcu S, Erdogan I, Tan A. Cytology of a giant adult-type rhabdomyoma of the tongue. Diagn Cytopathol. 2011;39(9):686–8. doi: 10.1002/dc.21530. [DOI] [PubMed] [Google Scholar]
- 6.Zhang GZ, Zhang GQ, Xiu JM, Wang XM. Intraoral multifocal and multinodular adult rhabdomyoma: report of a case. J Oral Maxillofacc Surg. 2012;70(10):2480–5. doi: 10.1016/j.joms.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 7.Yadav SK, Sood N. Multinodular adult rhabdomyoma in female: a rare case report. J Oral Maxillofacc Pathol. 2019;23(Suppl 1):54–7. doi: 10.4103/jomfp.JOMFP_4_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beyer TE, Blair JR. Sublingual rhabdomyoma. Arch Otolaryngol. 1948;47(5):678–80. doi: 10.1001/archotol.1948.00690030704012. [DOI] [PubMed] [Google Scholar]
- 9.Misch KA. Rhabdomyoma purum: a benign rhabdomyoma of tongue. J Pathol Bacteriol. 1958;75(1):105–8. doi: 10.1002/path.1700750112. [DOI] [PubMed] [Google Scholar]
- 10.Assor D, Thomas JR. Multifocal rhabdomyoma. Report of a case. Arch Otolaryngol. 1969;90(4):489–91. doi: 10.1001/archotol.1969.00770030491015. [DOI] [PubMed] [Google Scholar]
- 11.Wyatt RB, Schochet SS, Jr, McCormick WF, Rhabdomyoma Light and electron microscopic study of a case with intranuclear inclusions. Arch Otolaryngol. 1970;92(1):32–9. doi: 10.1001/archotol.1970.04310010058006. [DOI] [PubMed] [Google Scholar]
- 12.Tandler B, Rossi EP, Stein M, Matt MM. Rhabdomyoma of the lip. Light and electron microscopical observations. Arch Pathol. 1970;89(2):118–27. [PubMed] [Google Scholar]
- 13.Olofsson J. Extracardiac rhabdomyoma. Acta Otolaryngol. 1972;74(1):139–44. doi: 10.3109/00016487209128433. [DOI] [PubMed] [Google Scholar]
- 14.Albrechtsen R, Ebbesen F, Vang Pedersen S. Extracardiac rhabdomyoma. Light and electron microscopic studies of two cases in the mandibular area, with a review of previous reports. Acta Otolaryngol. 1974;78(5–6):458–64. doi: 10.3109/00016487409126380. [DOI] [PubMed] [Google Scholar]
- 15.Ferracini R, Cavina C, Morrone B. Rhabdomyoma (adult type) of the sublingual region. Tumori. 1977;63(1):43–8. doi: 10.1177/030089167706300106. [DOI] [PubMed] [Google Scholar]
- 16.Jones JK, Buntine DW. Benign rhabdomyoma of the submandibular region. J Otolaryngol. 1977;6(3):215–8. [PubMed] [Google Scholar]
- 17.Caracta PF, Guzman L, Wigger HJ, Hsu YH. Extracardiac rhabdomyoma: a rare entity. South Med J. 1978;71(5):538–540. doi: 10.1097/00007611-197805000-00017. [DOI] [PubMed] [Google Scholar]
- 18.Eveson JW, Merchant NE. Sublingual rhabdomyoma. Int J Oral Surg. 1978;7(1):27–31. doi: 10.1016/s0300-9785(78)80007-6. [DOI] [PubMed] [Google Scholar]
- 19.Heiden CL, Steuer G, Marquart KH. Ein rhabdomyom des weichen gaumens [Rhabdomyoma of the soft palate (author’s transl)] Laryngol Rhinol Otol. 1978;57(9):796–804. [PubMed] [Google Scholar]
- 20.Weitzner S, Lockey MW, Lockard VG. Adult rhabdomyoma of soft palate. Oral Surg Oral Med Oral Pathol. 1979;47(1):70–3. doi: 10.1016/0030-4220(79)90104-x. [DOI] [PubMed] [Google Scholar]
- 21.Solomon MP, Tolete-Velcek F. Lingual rhabdomyoma (adult variant) in a child. J Pediatr Surg. 1979;14(1):91–4. doi: 10.1016/s0022-3468(79)80586-2. [DOI] [PubMed] [Google Scholar]
- 22.Neville BW, McConnel FM. Multifocal adult rhabdomyoma. Report of a case and review of the literature. Arch Otolaryngol. 1981;107(3):175–8. doi: 10.1001/archotol.1981.00790390041012. [DOI] [PubMed] [Google Scholar]
- 23.Warner TF, Goell W, Sundharadas M, Falk VS. Adult rhabdomyoma: ultrastructure and immunocytochemistry. Arch Pathol Lab Med. 1981;105(11):608–11. [PubMed] [Google Scholar]
- 24.Gardner DG, Corio RL. Multifocal adult rhabdomyoma. Oral Surg Oral Med Oral Pathol. 1983;56(1):76–8. doi: 10.1016/0030-4220(83)90059-2. [DOI] [PubMed] [Google Scholar]
- 25.Schlosnagle DC, Kratochvil FJ, Weathers DR, McConnel FM, Campbell WG., Jr Intraoral multifocal adult rhabdomyoma. Report of a case and review of the literature. Arch Pathol Lab Med. 1983;107(12):638–42. [PubMed] [Google Scholar]
- 26.Reid CO, Smith CJ. Rhabdomyoma of the floor of the mouth: a new case and review of recently reported intra-oral rhabdomyomas. Br J Oral Maxillofacc Surg. 1985;23(4):284–91. doi: 10.1016/0266-4356(85)90046-4. [DOI] [PubMed] [Google Scholar]
- 27.Böck D, Böck P. Rhabdomyoma of the soft palate. Fine structural details of a highly differentiated muscle tumor. Histol Histopathol. 1987;2(3):285–9. [PubMed] [Google Scholar]
- 28.Bertholf MF, Frierson HF, Jr, Feldman PS. Fine-needle aspiration cytology of an adult rhabdomyoma of the head and neck. Diagn Cytopathol. 1988;4(2):152–5. doi: 10.1002/dc.2840040216. [DOI] [PubMed] [Google Scholar]
- 29.Nam HK, Mikhael MA, Wolff AP. Adult rhabdomyoma of the base of the tongue. Ann Otol Rhinol Laryngol. 1990;99(3 Pt 1):234–5. doi: 10.1177/000348949009900314. [DOI] [PubMed] [Google Scholar]
- 30.Walker WP, Laszewski MJ. Recurrent multifocal adult rhabdomyoma diagnosed by fine-needle aspiration cytology: report of a case and review of the literature. Diagn Cytopathol. 1990;6(5):354–8. doi: 10.1002/dc.2840060513. [DOI] [PubMed] [Google Scholar]
- 31.Sangueza O, Sangueza P, Jordan J, White CR., Jr Rhabdomyoma of the tongue. Am J Dermatopathol. 1990;12(5):492–5. doi: 10.1097/00000372-199010000-00010. [DOI] [PubMed] [Google Scholar]
- 32.Garcia-Ruiz JA, Sanchez-Aniceto G, De La Mata-Pages R, Gonzalez-Rex JA, Ballestin Carcavilla C. Submandibular rhabdomyoma: a case report. Br J Oral Maxillofacc Surg. 1991;29(2):123–6. doi: 10.1016/0266-4356(91)90099-q. [DOI] [PubMed] [Google Scholar]
- 33.Napier SS, Pagni CG, McGimpsey JG. Sublingual adult rhabdomyoma. Report of a case. Int J Oral Maxillofacc Surg. 1991;20(4):201–3. doi: 10.1016/s0901-5027(05)80174-2. [DOI] [PubMed] [Google Scholar]
- 34.Gibas Z, Miettinen M. Recurrent parapharyngeal rhabdomyoma. Evidence of neoplastic nature of the tumor from cytogenetic study. Am J Surg Pathol. 1992;16(7):721–8. doi: 10.1097/00000478-199207000-00011. [DOI] [PubMed] [Google Scholar]
- 35.Horn G, Werner JA, Schmidt D, Beigel A. Rhabdomyom des mundbodens–ein fallbericht [Rhabdomyoma of the mouth floor–a case report] HNO. 1992;40(8):322–4. [PubMed] [Google Scholar]
- 36.Shemen L, Spiro R, Tuazon R. Multifocal adult rhabdomyomas of the head and neck. Head Neck. 1992;14(5):395–400. doi: 10.1002/hed.2880140511. [DOI] [PubMed] [Google Scholar]
- 37.Fortson JK, Prunes FS, Lang AG. Adult multifocal extracardiac rhabdomyoma. J Natl Med Assoc. 1993;85(2):147–50. [PMC free article] [PubMed] [Google Scholar]
- 38.Kapadia SB, Meis JM, Frisman DM, Ellis GL, Heffner DK, Hyams VJ. Adult rhabdomyoma of the head and neck: a clinicopathologic and immunophenotypic study. Hum Pathol. 1993;24(6):608–17. doi: 10.1016/0046-8177(93)90240-h. [DOI] [PubMed] [Google Scholar]
- 39.Zachariades N, Skoura C, Sourmelis A, Liapi-Avgeri G. Recurrent twin adult rhabdomyoma of the cheek. J Oral Maxillofacc Surg. 1994;52(12):1324–8. doi: 10.1016/0278-2391(94)90058-2. [DOI] [PubMed] [Google Scholar]
- 40.Zbären P, Läng H, Becker M. Rare benign neoplasms of the larynx: rhabdomyoma and lipoma. ORL J Otorhinolaryngol Relat Spec. 1995;57(6):351–5. doi: 10.1159/000276780. [DOI] [PubMed] [Google Scholar]
- 41.Bastian BC, Bröcker EB. Adult rhabdomyoma of the lip. Am J Dermatopathol. 1998;20(1):61–4. doi: 10.1097/00000372-199802000-00012. [DOI] [PubMed] [Google Scholar]
- 42.Ballester F, Polo I, Papí M, Lafarga J, Espuch D, Niveiro M. Rabdomioma del adulto [Rhabdomyoma in the adult] Acta Otorrinolaringol Esp. 2000;51(4):361–3. [PubMed] [Google Scholar]
- 43.Morinière S, Sibel JP, Marlier F, Guerrier B. Rhabdomyome basi-lingual. A propos d’un cas traité par voie endoscopique [Basilingual rhabdomyoma treated by endoscopy] Ann Otolaryngol Chir Cervicofac. 2001;118(4):245–8. [PubMed] [Google Scholar]
- 44.Fukuda Y, Okamura HO, Nemoto T, Kishimoto S. Rhabdomyoma of the base of the tongue. J Laryngol Otol. 2003;117(6):503–7. doi: 10.1258/002221503321892415. [DOI] [PubMed] [Google Scholar]
- 45.Favia G, Lo Muzio L, Serpico R, Maiorano E. Rhabdomyoma of the head and neck: clinicopathologic features of two cases. Head Neck. 2003;25(8):700–4. doi: 10.1002/hed.10266. [DOI] [PubMed] [Google Scholar]
- 46.McGregor DK, Krishnan B, Green L. Fine-needle aspiration of adult rhabdomyoma: a case report with review of the literature. Diagn Cytopathol. 2003;28(2):92–5. doi: 10.1002/dc.10241. [DOI] [PubMed] [Google Scholar]
- 47.Delides A, Petrides N, Banis K. Multifocal adult rhabdomyoma of the head and neck: a case report and literature review. Eur Arch Otorhinolaryngol. 2005;262(6):504–6. doi: 10.1007/s00405-004-0840-y. [DOI] [PubMed] [Google Scholar]
- 48.Hansen T, Katenkamp D. Rhabdomyoma of the head and neck: morphology and differential diagnosis. Virchows Arch. 2005;447(5):849–54. doi: 10.1007/s00428-005-0038-8. [DOI] [PubMed] [Google Scholar]
- 49.Liess BD, Zitsch RP, 3rd, Lane R, Bickel JT. Multifocal adult rhabdomyoma: a case report and literature review. Am J Otolaryngol. 2005;26(3):214–7. doi: 10.1016/j.amjoto.2004.11.014. [DOI] [PubMed] [Google Scholar]
- 50.Bellis D, Torre V, Nunziata R, Demarchi A, Fornaseri V, Coverlizza S, Beatrice F. Submandibular rhabdomyoma: a case report. Acta Cytol. 2006;50(5):557–9. doi: 10.1159/000326015. [DOI] [PubMed] [Google Scholar]
- 51.De Medts J, Dick C, Casselman J, Van Den Berghe I. Intraoral multifocal adult rhabdomyoma: a case report. B-ENT. 2007;3(4):205–8. [PubMed] [Google Scholar]
- 52.Bizon A, Capitain O, Girault S, Charrot H, Laccourreye L. Rhabdomyome multifocal et tomographie par émission de positons [Multifocal adult rhabdomyoma and positron emission tomography] Ann Otolaryngol Chir Cervicofacc. 2008;125(4):213–217. doi: 10.1016/j.aorl.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 53.Catalfamo L, Lombardo G, Siniscalchi EN, Nava C, Familiari E, Francesco Sde P. Rhabdomyomas of the submandibular and sublingual glands. J Craniofac Surg. 2010;21(3):927–30. doi: 10.1097/SCS.0b013e3181d7f09c. [DOI] [PubMed] [Google Scholar]
- 54.Gupta N, Banik T, Rajwanshi A, Radotra BD, Panda N, Dey P, Srinivasan R, Nijhawan R. Fine needle aspiration cytology of oral and oropharyngeal lesions with an emphasis on the diagnostic utility and pitfalls. J Cancer Res Ther. 2012;8(4):626–9. doi: 10.4103/0973-1482.106581. [DOI] [PubMed] [Google Scholar]
- 55.Parara E, Christopoulos P, Tosios K, Paravalou I, Vourlakou C, Alexandridis K. A swelling of the floor of the mouth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109(1):12–6. doi: 10.1016/j.tripleo.2009.09.024. [DOI] [PubMed] [Google Scholar]
- 56.Maglio R, Francesco S, Paolo M, Stefano V, Francesco D, Giovanni R. Voluminous extracardiac adult rhabdomyoma of the neck: a case presentation. Case Rep Surg. 2012;2012:984789. doi: 10.1155/2012/984789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.de Trey LA, Schmid S, Huber GF. Multifocal adult rhabdomyoma of the head and neck manifestation in 7 locations and review of the literature. Case Rep Otolaryngol. 2013;2013:758416. doi: 10.1155/2013/758416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Amelia Souza A, de Araújo VC, Passador Santos F, Ferreira Martinez E, de Menezes Filho JF, de SoaresAraujo N, Soares AB. Intraoral adult rhabdomyoma: a case report. Case Rep Dent. 2013;2013:741548. doi: 10.1155/2013/741548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Andrade NN, Gandhewar T, Aggarwal N, Mathai P. Adult rhabdomyoma of the tongue in a child: report of a case and a literature appraisal. Contemp Clin Dent. 2018;9(1):2–4. doi: 10.4103/ccd.ccd_835_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Dau M, Kraeft SK, Kämmerer PW. Unique manifestation of a multifocal adult rhabdomyoma involving the soft palate-case report and review of literature. J Surg Case Rep. 2019;2019(4):rjz116. doi: 10.1093/jscr/rjz116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hakim I, Yunus MRM. Extracardiac rhabdomyoma mimicking plunging ranula. Medeni Med J. 2020;35(3):271–5. doi: 10.5222/MMJ.2020.88120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tostar U, Malm CJ, Meis-Kindblom JM, Kindblom LG, Toftgård R, Undén AB. Deregulation of the hedgehog signalling pathway: a possible role for the PTCH and SUFU genes in human rhabdomyoma and rhabdomyosarcoma development. J Pathol. 2006;208(1):17–25. doi: 10.1002/path.1882. [DOI] [PubMed] [Google Scholar]