Abstract
Purpose of the Study
Traditionally during labour woman is supported by another woman. However, in hospitals, continuous support during labour has often become the exception rather than the routine. Worldwide, there is a growing concern about the disrespect and abuse of women seeking maternity care. This prompted us to decide to change the obstetric care practices by providing a birth companion of her choice to women during labour and compare their maternal and newborn outcomes with the data from the same institute before intervention.
Methods
This was a quasi-experimental study conducted in the Department of OBGY, GMCH, Aurangabad for 20 months and compared with the previous data from the same institute before implementation of the birth companion policy. The impact of this intervention was evaluated by caesarean section rate, episiotomy rates and admission to neonatal intensive care units, and data was analysed by an appropriate statistical test.
Results
The rate of caesarean Section (20%) and episiotomy (8.57%) was significantly lower in the intervention group than in the control group. The rate of NICU admission and time required for initiation of breastfeeding was significantly lower in the intervention than in the control group. Around 86.6% of women from the intervention group were fully satisfied with the role of birth companion and 13.4% were partially satisfied.
Conclusion
Our study demonstrated that the use of an intrapartum birth companion of her choice helped us improve maternal and newborn outcomes without any harm. We recommend generalizing the policy of use of the trained birth companion of her choice in the private as well as the public sector.
Keywords: Birth companion, Respectful maternity care, Caesarean section rate, NICU admission, Episiotomy rate
Introduction
In every country and community worldwide, pregnancy and childbirth are momentous events in the lives of women and families and represent a time of intense vulnerability [1]. Almost all pregnant women desire a nurturing, supportive companion throughout labour to help them cope with the challenges of giving birth, including pain, fear, fatigue and uncertainty [2] Companion of choice at birth is defined as the continuous presence of a support person during labour and birth [3]. Traditionally during labour, a woman is supported by another woman. The “safe motherhood” concept is usually restricted to physical safety only. The notion of safe motherhood must be expanded beyond the prevention of morbidity or mortality to encompass respect for women’s basic human rights, including respect for women’s autonomy, dignity, feelings, choices and preferences, including companionship during maternity care [1]. Doula (from the Greek word for a female caregiver) can fulfil these needs, and the continuous labour support that the doula provides can improve labour and delivery outcomes [4]. Birth companions not only help in providing emotional support but also advice regarding coping techniques, comfort measures (comforting touch, massages, promoting adequate fluid intake and output) and advocacy (helping the woman articulate her wishes to the other). However, in public hospitals, continuous support during labour has often become the exception rather than the routine [5]. Even the birth companions allowed in private hospitals are not aware of their role during labour. Birth companion intervention has been recommended by the World Health Organization (WHO) to improve labour outcomes and women’s satisfaction with care [6, 7]. It has also been identified as a key element in the WHO vision of quality of care for pregnant women and newborn [2]. Worldwide, there is a growing concern about the disrespect and abuse of women seeking maternity care and requires urgent attention. White Ribbon Alliance (WRA) led a movement for reproductive, maternal and newborn health and rights through a charter of ten rights of a birthing woman, together termed as respectful maternity care (RMC). There is persuasive evidence that RMC gives better maternal and newborn outcomes, such as decreased medicalization and interventions and lower caesarean deliveries. The presence of a companion during labour is a low-cost intervention that might prove beneficial to the women in labour.
Pregnant women who enter into the labour room may find the hospital environment hostile and may get afraid. If a birth companion of her choice is available with her, due to the positive environment and support, oxytocin is naturally secreted. A birth companion provides the much-needed moral support to the mother and facilitates high-impact practices such as early initiation of breastfeeding. Government Medical College and Hospital, Aurangabad, is a tertiary hospital with a high caseload. There were growing concerns about disrespect and abuse to women during the birthing process, which prompted us to decide to institutionalize the practice of RMC, which is also one of the six quality improvement (QI) cycles in the LaQshya initiative. Keeping this in mind, we took an initiative in September 2016 to change obstetric care practices by providing the birth companion of her choice to a woman during labour and compare their maternal and newborn outcomes with the data from the same institute before intervention.
Objective(s)
To compare.
-
A.
Caesarean section rate in control and intervention group.
-
B.
Episiotomy rate
-
C.
NICU admission rate
-
D.
Timing of initiation of breastfeeding
Material and Method(s)
This was a Quasi trial (Nonrandomized trial) conducted in the Department of Obstetrics and Gynaecology, GMCH, Aurangabad for 20 months (September 2016 to May 2018) and compared with the previous data (control group) from the same institute before implementation of policy (January 2014 to August 2016).
Women participating after intervention were referred to as intervention group and those before the intervention were considered as the control group.
Inclusion Criteria
Intervention Group
Women with a singleton live foetus with cephalic presentation ≥ 37 weeks of gestational age and low risk at the time of enrolment and having plan to deliver in our hospital, women with a female friend or relative willing to stay with them through the process of labour and birth and who have undergone the process of childbirth herself.
Control Group
Same as in the intervention group except for the availability of birth companion.
Exclusion Criteria
Women who are mentally incapacitated or deaf and dumb, women requiring planned caesarean delivery, women agreed for participation but delivered in other facility, women requiring HDU/ICU admission, women without the birth companion of choice, women with multiple gestations, non-cephalic presentation, women with medical disorders, women who delivered before 37 weeks of gestational age, women with previous caesarean section, intrauterine foetal demise (IUFD), birth companion having cough, cold and fever or any other infectious disease.
After Institutional Ethics Committee permission, the women attending antenatal OPD with the plan to deliver in this hospital and willing to participate in the study were made aware of the birth companion policy of the hospital. The purpose of the study was explained to her and written consent for participation was obtained. Even though women were denied participation, the same care was offered to them. The women were treated as per the standard operating procedures of the department.
Sensitization of the doctors and supporting staff regarding the RMC practices and birth companion policy was done by arranging four workshops (one day each) at an interval of 12 months with an NGO- White Ribbon alliance and daily supervision by a motivated faculty with leadership qualities.
Intervention
During the first antenatal care (ANC) visit, the health care providers (HCPs) including doctors and nurses informed each expectant mother about the birth companion policy and encouraged her to provide the name and contact information of the birth companion of her choice in the following visit. A birth companion register was maintained in the antenatal OPD. Based on a pre-planned schedule, all birth companions were trained on their role during labour, delivery and childbirth. This training comprised of a minimum of two sessions, of which one was a theoretical session and the other was a site visit. Emphasis was laid on the importance of not interfering in medical procedures and respecting the privacy of other women. The birth companions were requested to accompany expectant mothers during subsequent antenatal visits and childbirth. The training was focussed on emotional and physical support; emotional support including being present, demonstrating a caring and positive attitude, saying calming verbal expressions, using humour, praise, encouraging and acknowledging efforts during the process of pushing the baby. Physical support including supporting her to change position favouring upright positions, walking with her, giving her drinks and food, massage, reminding her to go and pass urine, helping her find a comfortable position for pushing, wipe her face with a cool cloth and help her breastfeed. She was made aware of the warning signs and symptoms during pregnancy, labour and the post-partum period. All doubts were cleared, and questions were answered individually at the end of the group training for birth companions. Information, education and communication (IEC) material were developed in the local language and displayed in the labour room and OPD to reinforce information dissemination during the training.
The impact of this intervention was evaluated by caesarean section delivery rate, episiotomy rates, admission to neonatal intensive care units and time required for initiation of breastfeeding and data was compared with the control group.
At the time of discharge from the hospital every woman in the intervention group was interviewed regarding the perception of quality care received, ease of identifying the birth companion of her choice, ease of understanding the role by the birth companion, the problems encountered and satisfaction rate and the questions were analysed by using Likert scales with response ranging from 1 to 5.
Data were analysed by using SPSS software version 15 and a p-value < 0.05 was considered significant. For qualitative data, the Chi-square test was used and for quantitative data, a t-test was used.
Observation(s)
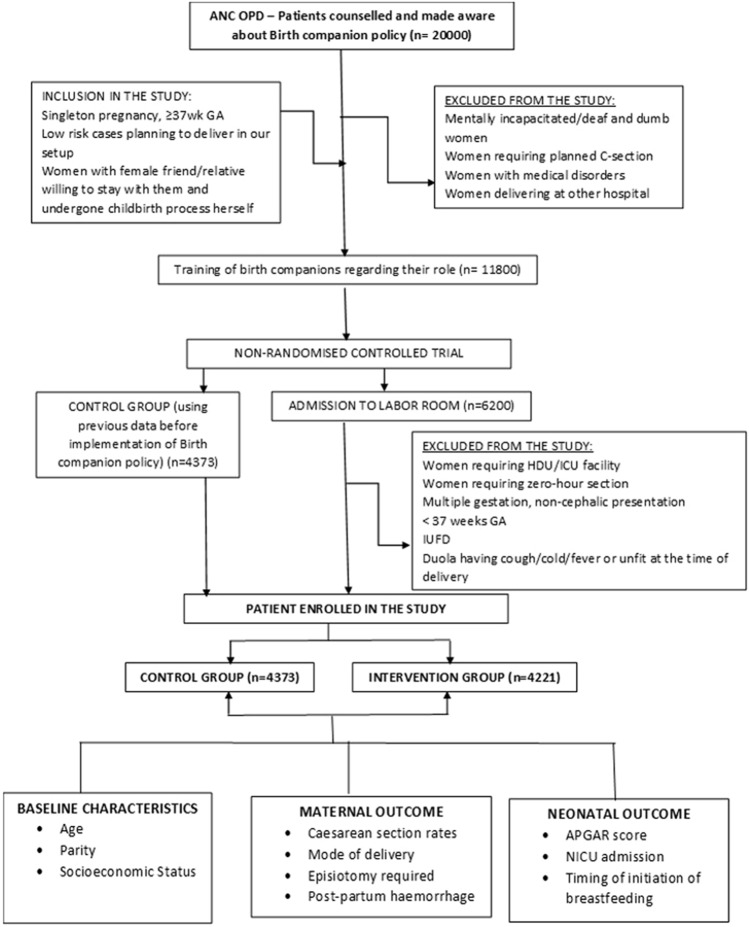
Around 20,000 women coming to the antenatal clinic were made aware of the birth companion policy. Out of them, around 11,800 women’s birth companions were trained regarding their role and at the time of delivery, around 4221 women were accompanied by a trained birth companion and enrolled in the study. Around 4373 women who delivered before the intervention were included as control group (Fig. 1).
Fig. 1.
The effect of intrapartum birth Companion of her choice on the maternal and newborn outcome at a tertiary care centre
Both groups were comparable with respect to age, parity and socioeconomic status (Table 1).
Table 1.
Baseline characteristics of Study Population
| Baseline characteristics | Control group (n = 4373) | Intervention group (n = 4221) | Statistical analysis | |
|---|---|---|---|---|
| Age | 24.86 ± 3.8 | 24.88 ± 3.6 |
t = − 0.434 p = 0.66 |
|
| Parity | Primigravida | 1875(43.04%) | 1809 (42.87%) |
X2 = 0.0003369 df = 1 p = 0.9854 |
| Multigravida | 2498 (56.96%) | 2412 (57.13%) | ||
| Socioeconomic status* | Class II (upper middle) | 214 (4.9%) | 211 (5%) |
X2 = 1.477 df = 3 p = 0.6875 |
| Class III (lower middle) | 869(19.88%) | 845(20%) | ||
| Class IV (upper lower) | 1496(34.22%) | 1393(33%) | ||
| Class V (lower) | 1794 (41%) | 1772 (42%) | ||
*Modified Kuppuswamy’s Scale
The rate of caesarean section was significantly reduced in the intervention group (20%) than in the control group (26%). There was no significant difference regarding PPH in both groups (Table 2).
Table 2.
Comparison of maternal outcome
| Characteristics | Control group (n = 4373) | Intervention group (n = 4221) | Statistical analysis | |
|---|---|---|---|---|
| Mode of delivery | Normal delivery | 3175 (72.6%) | 3318 (78.6%) |
X2 = 43.48 df = 2 p < 0.0000001 |
| Caesarean section (LSCS) | 1137 (26%) | 844 (20%) | ||
| Operative vaginal delivery (OVD) | 61 (1.4%) | 59 (1.4%) | ||
| Episiotomy | 681 (15.57%) | 362 (8.57%) |
X2 = 98.65 df = 1 p < 0.0000001 |
|
| Post-partum haemorrhage (PPH) | 109 (2.5%) | 101 (2.4%) |
X2 = 0.08969 df = 1 p = 0.7646 |
The rate of NICU admission and time required for initiation of breastfeeding was significantly lower in the intervention than in the control group (Table 3).
Table 3.
Comparison of neonatal outcomes
| Characteristics | Control group (n = 4373) | Intervention group (n = 4221) | Statistical analysis | |
|---|---|---|---|---|
| Apgar score At 5’ | ≤ 7 | 140 (3.2%) | 42 (1%) | X2 = 15.63 df = 1 p < 0.00007711 |
| > 7 | 4233(96.8%) | 4174(98.8%) | ||
| NICU admission | Neonatal jaundice | 66 (1.5%) | 63 (1.5%) | X2 = 69.22 df = 5 p < 0.0000001 |
| Prolonged PROM | 52 (1.2%) | 46(1.1%) | ||
| Baby weight > 4 kg | 66 (1.5%) | 63 (1.5%) | ||
| Refusal to feed | 109 (2.5%) | 34 (0.8%) | ||
| Convulsions | 101 (2.3%) | 25 (0.6%) | ||
| Asphyxia | 140 (3.2%) | 42 (1%) | ||
| Time required to initiate breastfeeding (in minutes) | 42 ± 6 | 26.84 ± 5.5 | t = 211.608 p < 0.0000001 | |
Out of 4221 women who received birth companion support, around 86.6% of women were fully satisfied with the role of birth companion. Around 13.4% of women were partially satisfied as they perceived companion’s role more in terms of assisting them with non-clinical tasks than providing emotional support.
Discussion
This was a history-controlled nonrandomized trial where data were analysed before and after intervention from the same institute to see the effect of using intrapartum birth companion policy on maternal and newborn outcomes. There are very few clinical trials on trained birth companion of her choice from developing countries. During implementation of the policy, there were several teething problems with birth companions, most of them were due to a lack of understanding about the birth companions role and mothers not identifying suitable birth companion. Sometimes, women brought their younger unmarried sister as a companion. In the rainy season, many birth companions came with common cold and/or fever, which adversely affected their ability to perform their roles. Most birth companions brought mobile phones to take pictures of the newborn, which not only hindered the maternal and newborn care process but also distracted the doulas from their roles. The facility, therefore, made a dress code for doulas and developed a system of identity cards, it was ensured that they did not carry mobile phones into the labour ward. The birth companions were also instructed strictly not to disclose any other woman’s condition to her family or those waiting outside the labour room.
During labour, women are exposed to unfamiliar environment, sometimes overmedicalization with high rates of intervention, unfamiliar personnel, lack of privacy and other conditions that might be experienced as harsh. These conditions might have an adverse impact on the progress of labour and the development of feelings of confidence and competence [5]. The support by a birth companion of her choice during labour may help her relieve stress and strain. Thus, helping her control the autonomic response that might negatively affect the progress of labour and alleviate anxiety. The encouragement provided by the companion to keep her mobile during labour and push during second stage would help her to utilize her efforts efficiently. Trained birth companion may provide soothing environment along with tangible assistance to help a woman cope with labour stress and labour pain.
In hostile environment of the hospital, labour may supress women's feelings of competence, confidence in adapting to parenthood and initiation of successful breastfeeding. These untoward effects might get reduced by the provision of additional companion during labour aimed to promote self-esteem. [8]. Only support from someone in a doula role or a member of woman’s social network seemed to have this effect [9].
The strength of the study was that despite such a high caseload, we could succeed in providing a birth companion of her choice to labouring women and got encouraging results which can be generalized for high-risk mothers also.
The limitation of the study was that the duration of labour, need for labour analgesia and the effect on post-partum depression were not included in the study.
The continuous support during labour might have improved outcomes for women and infants, including increased spontaneous vaginal birth, shorter duration of labour, and decreased caesarean birth, instrumental vaginal birth, low five-minute Apgar score and negative feelings about childbirth experiences. [5].
Support by doulas during labour was associated with a significant reduction in caesarean birth and oxytocin administration. The impact of a doula's presence during labour and birth is associated with positive outcomes that have physical, emotional and economic implications. [10]
Continuous labour support is a rare example of health care practice found to have many benefits and no known harm [9]. We observed that the intervention by using a birth companion of her choice reduced the caesarean section rate, episiotomy rate, NICU admission rate with no evidence of harm.
Conclusion
Our study has demonstrated the use of intrapartum birth companion of her choice policy helped us improve maternal and newborn outcomes without any harm. Labour support from a chosen family member or friend who has been trained for performing the role of birth companion increased women's satisfaction with the birthing experience. We recommend routine use of the trained birth companion policy of her choice in private as well as the public sector.
Shrinivas N. Gadappa
MBBS, MD is Professor & Head, Department of OBGY, Government Medical College & Hospital, Aurangabad. He has 25 years of clinical and teaching experience and has done 55 publications in indexed journals. He has authored a book on Standard Operating Procedure for PGs & consultants. He has been the State Nodal Officer for the course of Integrating Gender in Medical Education and contributed to a module on it. He has pioneered “RESPECTFUL MATERNITY CARE” in government set-up. He is the coordinator for the project by WHO on Violence against women. He is a Master Trainer for LaQshya by NHM GOI and many government programmes.
Funding
The project is not funded by any agency.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Study on Human Participants
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Dr. Shrinivas N. Gadappa, MBBS, MD OBGY, Professor and Head in Department of Obstetrics and Gynecology at Government Medical College and Hospital, Aurangabad, Maharashtra, India; Dr. Sonali S. Deshpande, MBBS, MD OBGY, Academic Professor in Department of Obstetrics and Gynecology at Government Medical College and Hospital, Aurangabad, Maharashtra, India.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Shrinivas N. Gadappa, Email: gadappashrinivas@gmail.com
Sonali S. Deshpande, Email: sonalissd97@gmail.com
References
- 1.Hodnett ED, Lowe NK, Hannah ME, Willan AR, Stevens B, Weston JA, Ohlsson A, Gafni A, Muir HA, Myhr TL, Stremler R. Nursing supportive care in labor trial group. Effectiveness of nurses as providers of birth labor support in North American hospitals: a randomized controlled trial. JAMA. 2002;288(11):1373–1381. doi: 10.1001/jama.288.11.1373. [DOI] [PubMed] [Google Scholar]
- 2.Bowser D, Hill K (2010) Exploring evidence for disrespect and abuse in facility‐based childbirth: report of a landscape analysis. Bethesda, MD: USAID‐TRAction Project, University Research Corporation, LLC, and Harvard School of Public Health. ii The Charter borrows heavily from the framework of the International Planned Parenthood Federation Charter on Sexual and Reproductive Rights, 1996.
- 3.American College of Obstetricians and Gynecologists (College); Society for Maternal-Fetal Medicine, Caughey AB, Cahill AG, Guise JM, Rouse DJ. Safe prevention of the primary cesarean delivery. Am J Obstet Gynecol. 2014 Mar;210(3):179–93. doi: 10.1016/j.ajog.2014.01.026. PMID: 24565430. [DOI] [PubMed]
- 4.Hodnett ED, Gates S, Hofmeyer GJ, Sakala C. Continuous support for women during childbirth. Cochrane Database Syst Rev. 2013 doi: 10.1002/14651858.CD003766.pub5. [DOI] [PubMed] [Google Scholar]
- 5.Bohren MA, Hofmeyr GJ, Sakala C, Fukuzawa RK, Cuthbert A. Continuous support for women during childbirth. Cochrane Database Syst Rev. 2017 doi: 10.1002/14651858.CD003766.pub6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.WHO recommendations for augmentation of labour. Geneva: World Health Organization; 2014. (http://www.who.int/reproductivehealth/publications/maternal_perinatal_health/augmentation-labour/en/). [PubMed]
- 7.WHO recommendations on health promotion interventions for maternal and newborn health. Geneva: World Health Organization; 2015. (http:// www.who.int/maternal_child_adolescent/documents/health-promotioninterventions/en/) [PubMed]
- 8.Hofmeyr GJ, Nikodem VC, Wolman WL, Chalmers BE, Kramer T. Companionship to modify the clinical birth environment: effects on progress and perceptions of labour, and breastfeeding. Br J Obstet Gynaecol. 1991;98(8):756–764. doi: 10.1111/j.1471-0528.1991.tb13479.x.PMID:1911582.). [DOI] [PubMed] [Google Scholar]
- 9.National Partnership for Women & Families Continuous support for women during childbirth: 2017 cochrane review update key takeaways. J Perinat Educ. 2018;27(4):193–197. doi: 10.1891/1058-1243.27.4.193.PMID:31073265;PMCID:PMC6491161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Trueba G, Contreras C, Velazco MT, Lara EG, Martínez HB. Alternative strategy to decrease cesarean section: support by doulas during labor. J Perinat Educ. 2000;9(2):8–13. doi: 10.1624/105812400X87608. [DOI] [PMC free article] [PubMed] [Google Scholar]