Abstract
Immune associated cells in the microenvironment have a significant impact on the development and progression of hepatocellular carcinoma (HCC) and have received more and more attention. Different types of immune-associated cells play different roles, including promoting/inhibiting HCC and several different types that are controversial. It is well known that immune escape of HCC has become a difficult problem in tumor therapy. Therefore, in recent years, a large number of studies have focused on the immune microenvironment of HCC, explored many mechanisms worth identifying tumor immunosuppression, and developed a variety of immunotherapy methods as targets, laying the foundation for the final victory in the fight against HCC. This paper reviews recent studies on the immune microenvironment of HCC that are more reliable and important, and provides a more comprehensive view of the investigation of the immune microenvironment of HCC and the development of more immunotherapeutic approaches based on the relevant summaries of different immune cells.
Keywords: HCC, TAM, NK cell, cancer immunotherapy, challenge, development
Introduction
Hepatocellular carcinoma (HCC) is the most common type of liver cancer, accounting for the sixth most common type of cancer and the second leading cause of death among all cancers (Ferlay et al., 2015). Due to changes in environmental factors, immunization and people’s lifestyle, the incidence of HCC and HCC-related mortality are increasing all over the world. The latest research indicates that HCC accounts for approximately 85% of patients diagnosed with liver cirrhosis. Its 5-year survival rate is only 18%, second only to pancreatic cancer (Asafo-Agyei and Samant, 2021). With the improvement of the treatment level for HCC, a variety of treatment options such as liver transplantation, surgical removal, systemic therapy and liver targeted therapy are constantly enhanced and created. At present, only surgical treatment is considered as a potential radical treatment for HCC. But only 15% of HCC patients have the opportunity to have surgery, most patients are found in the advanced stage (Roxburgh and Evans, 2008). Sorafenib is the only systemic medication approved by the FDA for advanced HCC. However, because of the overexpression of dihydropyrimine dehydrogenase, the multi-drug resistance gene MDR-1and p-glycoprotein gene products, HCC is regarded a chemotherapy-resistant tumour, and how to execute effective chemotherapy is still a major difficulty (Soini et al., 1996; Jiang et al., 1997; Kato et al., 2001).
Seven essential characteristics of cancer have been identified as crosstalk between cells and immune cells, self-sufficiency of signals for growth, unrestricted replication potential, apoptosis avoidance, growth signals insensitivity and continuous angiogenesis and invasion/metastasis of tissue (Hanahan and Weinberg, 2000; Hanahan and Weinberg, 2011). Tumor cells, immune cells, stromal cells, endothelial cells, and cancer-related fibroblasts are all found in the tumour microenvironment (TME), according to current research. Malignant tumour cells can evade immune monitoring and kill, as well as impair the human body, via a range of intricate ways (Hanahan and Weinberg, 2011). Due to the limitations of traditional chemotherapy regimens in the treatment of HCC, a variety of immunotherapy methods for HCC have been developed. Immunotherapy mostly employs immune cells within or outside of the TME to specifically target and assault cancer cells, with the benefits of high specificity and low side effects (Yost et al., 2019). More crucially, thanks to advances in tools such as mass spectrometry and single-cell RNA sequencing, We can map immunological cells in TMEs at the single-cell level (Spitzer and Nolan, 2016; Zheng et al., 2017; Papalexi and Satija, 2018; Wang et al., 2019a). We outline the significance of tumor-associated immune cells in the HCC tumour microenvironment and highlight their relevance in HCC cancer immunotherapy in this study.
The Immune Cells in TME
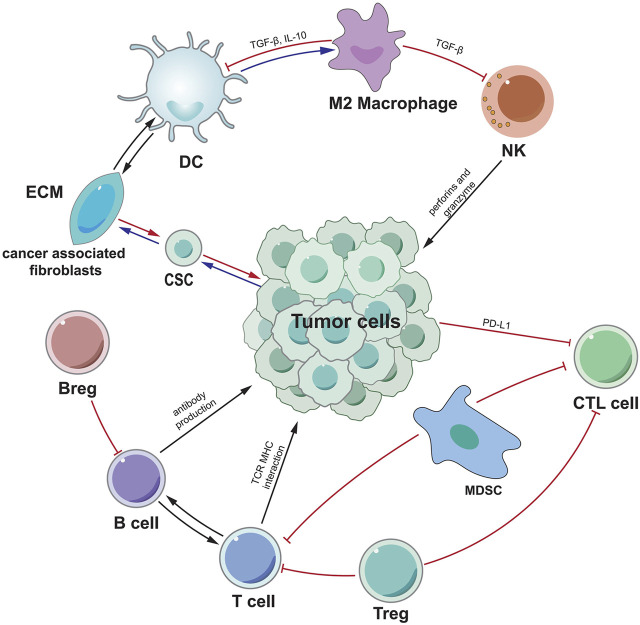
Tumor-associated immune cells are broadly classified into two types: tumor-promoting immune cells and tumor-antagonistic immune cells. At different stages of tumour formation, these two types of cells play different functions and impact each other (Figure 1). Because the significance of tumor-associated B cells in tumour growth is debatable, we shall introduce B cells additionally.
FIGURE 1.
A schematic overview of the most important mechanisms and interactions of the tumor microenvironment. Tumor cells interact with other cells in various ways. CSC indicates cancer stem cell, ECM indicates extracellular matrix, CTL indicates cytotoxic T lymphocytes.
Tumor-Antagonizing Immune Cells
Effector T Cells
Current studies suggest that CD8+ cytotoxic T cells (CTLs) are the main lymphocytes that kill cancer cells. When CD8+ T cells recognize antibodies on DC, CD80−CD86 and CD70 ligands on DC connect to CD27 and CD28 receptors on CD8+ T cells, and CD8+ T cells are modified to become cytotoxic effector CD8+ T cells (Tanaka et al., 1999; Farhood et al., 2019). Furthermore, CD4+ T cells can activate CD8+ T cells through CD40−CD40L interaction, and CD4+ T cells can produce IL-2 to enhance CD8+ T cell proliferation. CD4+ T cells are also important in the maturation of CD8+ T cells into memory cells (Bennett et al., 1997; Mackey et al., 1997; Bennett et al., 1998; Mackey et al., 1998; Schoenberger et al., 1998; Bourgeois et al., 2002; Cheng et al., 2002; Borst et al., 2018). CTL kills target cells through granular exocytosis and apoptotic induction mediated by FasL ligand (FasL) in working state. CTL can also produce interferon- (IFN-) and tumour necrosis factor (TNF-) to cause cancer cell cytotoxicity (Farhood et al., 2019). Activation and regulation of CTL requires signals from T cell receptors (TCR) and immune checkpoints (Rogler et al., 1999). For example, cancer cells inhibit CTL activity through the expression of a ligand that binds to an inhibitory checkpoint, such as PD-L1 (Iwai et al., 2002). A significant number of studies have established the function of CD8+ T cells and CD4+ T cells in the formation and progression of HCC, including diagnosis/treatment/prognosis, and so on.
Chang et al. 's study confirmed that NanoMnSor improves the effectiveness of anti-PD-1 antibodies and whole-cell cancer vaccine immunotherapy by encouraging macrophage polarization to an immunostimulating M1 phenotype, decreasing hypoxica-induced tumor infiltration of tumor-associated macrophages, and raising the number of CD8 cytotoxic T cells in tumors, thereby reprogramming immunosuppressive TME (Chang et al., 2020). Xie et al. 's research proposed that PD-L1 overexpression is mostly triggered by pre-existing activated CD8 (+) cytotoxic T cells in the HCC environment, rather than being produced constitutively by tumor cells, and that it is a good prognostic factor for HCC (Xie et al., 2016). The frequency of circulating PD-1 (+) CD8 (+) T cells increases as the illness develops from LC to HCC. PD-1 expression was shown to be much higher in tumor-infiltrating CD8 (+) T cells. In vitro, CD8 (+) T cells promoted the production of PD-L1 on HCC cells in an IFN-dependent way, increasing CD8 (+) T cell death, whereas inhibiting PD-L1 reversed this effect (Shi et al., 2011).
Both in vitro restimulation and in vivo depletion studies have indicated that CD4+ and CD8+ lymphocytes contribute to anticancer activity. ASPH activation resulted in considerable production of antigen-specific CD4+ T cells in PBMC from healthy volunteers and HCC patients (Shimoda et al., 2012). Lack of recovered CD19+, CD3+, CD4+, and especially CD8+ T cells is associated with poor survival in patients (Carr and Metes, 2012). Zhou et al. ‘s revealed that antibodies against CD274 (PD-L1), LAG3, or TIM3 boost CD4+ and CD8+ TIL proliferation and cytokine secretion in response to polyclonal antigens or TAA stimulation (Zhou et al., 2017). More research results on the effect of Effector T cells in HCC are summarized in Table 1. It is clear that Effector T cells play a critical role in the immunological milieu of HCC. Many studies have shown that targeting these cells is effective in patients with HCC.
TABLE 1.
The immune cells in TME: Effector T cells.
| Cells | The research direction | Result | Reference |
|---|---|---|---|
| CD8+ T cell | The immune mechanism | NanoMnSor enhances the efficacy of anti-PD-1 antibodies and whole cell cancer vaccine immunotherapy by reducing tumor invasion of hypoxia-induced tumor-associated macrophages, promoting macrophage polarization into an immune-stimulating M1 phenotype and increasing the number of CD8 cytotoxic T to reprogram the immunosuppressive TME. | Chang et al. (2020) |
| CD8+ T cell | immunotherapy | PVRL1 upregulated by HCC cells stabilizes PVR on the cell surface, which interacts with the inhibitory molecule TIGIT of CD8 effector memory T cells. It is possible to develop PVRL1/TIGIT inhibitors as well as anti-PD1 to treat HCC. | Chiu et al. (2020) |
| CD8+ T cell | Prognostic marker | PD1 or TIM3PD1 CD8 T cells were significantly associated with poor prognosis, and the latter were adjacent to PD-L1 tumor-associated macrophages. | Ma et al. (2019) |
| CD8+ T cell | immunotherapy | SFGL2 promotes HCC growth by reducing DC activity and subsequent cytotoxicity of CD8 T cells, suggesting that SFGL2 is a novel potential therapeutic target for HCC therapy. | Yang et al. (2019a) |
| CD8+ T cell | The immune mechanism | IL-35 inhibits the cytolytic and noncytolytic functions of CD8 T cells against non-viral hepatitis associated HCC, possibly inhibiting the expression of perforin. | Yang et al. (2019b) |
| CD8+ T cell | The immune mechanism | Suppression of the tumor immunosuppressive environment and immune escape is accompanied by proliferation of functional cytotoxic CD8 T cells as well as suppression of myeloid suppressor cells and regulatory T cells in the tumor environment. | Tao et al. (2019) |
| CD8+ T cell | The immune mechanism | A large number of TEM-1 positive (TEM-1) TAM in the late stage of HCC development indirectly impair the cytotoxic function of CD8 T cells and induce the apoptosis of CD8 T cells. | Wu et al. (2019a) |
| CD8+ T cell | immunotherapy | The Δ- catenin peptide vaccine stimulates the activation of cytotoxic T lymphocytes (CTL) and enhances the invasion of CD8+ T cells into the tumor. In addition, Δ- catenin peptide vaccine can enhance the secretion of IFN-γ and the killing effect of T cells on tumor cells. | Huang et al. (2018) |
| CD8+ T cell | The immune mechanism | Stat3-blocked lysates of whole HCC cells stimulated activation of T and natural killer (NK) cells and enhanced cytotoxic CD8 T cell infiltration in tumor tissues. | Han et al. (2017) |
| CD8+ T cell | The immune mechanism | Antibody against CD274(PD-ligand 1 [PD-L1]), TIM3, or LAG3 increases CD8 and CD4 TIL proliferation and cytokine production in response to stimulation by polyclonal antigens or TAA. | Zhou et al. (2017) |
| CD8+ T cell | immunotherapy | Tremelimumab in combination with tumor ablation is a potential new therapy for patients with advanced HCC, resulting in the accumulation of CD8 T cells in tumors. Positive clinical activity was observed and may replace HCV viral load. | Duffy et al. (2017) |
| CD8+ T cell | immunotherapy | PD-L1 upregulation is mainly induced by pre-existing activated CD8+ cytotoxic T cells in the HCC environment, rather than constitutively expressed by tumor cells, and is a favorable prognostic factor for HCC. | Xie et al. (2016) |
| CD8+ T cell | The immune mechanism | Expression of programmed death 1(PD-1) and programmed death ligand 1(PD-L1) correlated with CD3+ and CD8+ cell density and clinical outcome. High density of internal and peripheral CD3+ and CD8+ T cells and corresponding immune scores were significantly associated with lower recurrence rates and prolonged RFS. | Gabrielson et al. (2016) |
| CD8+ T cell | Prognostic marker | Crosstalk of NK and CD8 T cells in tumor microenvironment may benefit patient prognosis. The count of NK and CD8 T cells infiltrating in CRC tumors may provide useful prognostic information | Sconocchia et al. (2014) |
| CD8+ T cell | immunotherapy | In the tumor microenvironment of sorafenib treated mice, tumor-specific effector T cells were upregulated, while the ratio of CD8+ T cells expressing PD-1 and regulatory T cells (Tregs) was reduced. | Chen et al. (2014) |
| CD8+ T cell | The immune mechanism | In HLA-A2 transgenic mice, the CD8+ T cells producing IFN-γ and the cytolytic activity in vivo were significantly increased. | Chen et al. (2012) |
| CD8+ T cell | The immune mechanism | As the disease progresses from LC to HCC, the frequency of circulating PD-1 (+) CD8+ T cells increases. Tumor-infiltrating CD8+ T cells showed a dramatic increase in PD-1 expression. In vitro, CD8+ T cells induced PD-L1 expression on HCC cells in an IFN-γ dependent manner, thereby promoting APOPTOSIS of CD8+ T cells, while blocking PD-L1 reversed this effect. | Shi et al. (2011) |
| CD8+ T cell | immunotherapy | Strong TAA-specific CD8+ T cell response inhibited HCC recurrence. For patients with HCC following local therapy, induction of TAA-specific cytotoxic T lymphocytes should be considered with immunotherapy, such as peptide vaccine. | Hiroishi et al. (2010) |
| CD8+ T cell | Prognostic marker | Overexpression of HLA-G protein in HCC is an independent indicator of poor prognosis, especially in early disease. The combination of HLA-G expression and Tregs/CD8+ ratio increased the prognostic power of both variables. | Cai et al. (2009) |
| CD8+ T cell | immunotherapy | HCA661 peptides H110 and H246 are naturally processed in dendritic cells (DCs) and when applied to DCs, they are sufficient to induce autologous CD8+ T cells to initiate cytotoxic responses against HCA661(+) human cancer cells. | Pang et al. (2007) |
| CD8+ T cell | Prognostic marker | The combination of low intratumoral Tregs with high intratumoral activated CD8+ cytotoxic cells (CTL) is the balance of CTL and is an independent prognostic factor for improved DFS and OS. | Gao et al. (2007) |
| CD8+ T cell | Prognostic marker | Increased CD4 (+) CD25 (+) Foxp3 (+) Treg may impair effector function of CD8+ T cells, promote disease progression, and represent a potential prognostic marker and therapeutic target in HBV-associated HCC patients. | Fu et al. (2007) |
| CD8+ T cell | immunotherapy | The functionally detectable presence of M3 (271) specific CD8+ T cells in HCC patients makes M3 (271) a potential target for immunotherapy in these patients. CD8+ T cells that respond to both NY-ESO-1 and MAG-A3 antigens provide a theoretical basis for the use of a bivalent vaccine in HCC patients with tumors expressing both antigens. | Zhang et al. (2007) |
| CD8+ T cell | Prognostic marker | HCC patients showed significantly higher WT p53-specific memory CD8+ T cell frequency and stronger WT p53-specific CTL activity compared to healthy controls. Increased frequency and activity of P53 specific CD8+ T cells were associated with deletion of selective HLA-A2 alleles and decreased expression of co-stimulatory molecules in tumor cells. | Cicinnati et al. (2006) |
| CD8+ T cell | The immune mechanism | CD4+ CD25 + T cells in the peripheral region of HCC may play a key role in controlling the activity of CD8+ cytotoxic T cells, thus promoting the development of HCC. | Yang et al. (2006) |
| CD4+T cell | The immune mechanism | The C/eBPα/miR-7 axis negatively regulates CD4+T cell activation and function through MAPK4, thus orchestrating experimental AIH mice. | Zhao et al. (2020) |
| CD4+T cell | The immune mechanism | In vivo treatment with MYC ASO without control ASO reduced proliferation, induced apoptosis, increased senescence, and remodeled the tumor microenvironment by recruiting CD4+T cells | Dhanasekaran et al. (2020) |
| CD4+T cell | The immune mechanism | Tumor associated CD4/CD8 double positive T (DPT) cells were found to be rich in L region, with co-expression of PD-1/HLA-DR/ICOS/CD45RO, and showed high levels of IFN-, TNF- and -1 after PD stimulation. Enrichment of DPT and PD-1DPT in L region indicated a good prognosis. | Zheng et al. (2020a) |
| CD4+T cell | The immune mechanism | The recruitment of cytotoxic cells, namely terminally differentiated CD4+ and CD8+ T cells (TEFF), is impaired in the tumor, and the effector memory CD4+ T cells are more attracted in this region. | Chaoul et al. (2020) |
| CD4+T cell | The immune mechanism | Knockdown of DCR3 expression in HCC significantly restored the immunity of CD4+T cells. Inhibition of DCR3 expression may provide a novel immunotherapy approach to restore immunity in HCC patients | Zhu et al. (2019) |
| CD4+T cell | The immune mechanism | Activated CD4+T cells from HCC stimulate macrophages to produce C-X-C motif chemokine 10(CXCL10). CXCL10 binds to the CXC chemokine receptor 3 on B cells and signals them through extracellular signal-regulated kinases, making them plasma cells that produce IgG. | Wei et al. (2019) |
| CD4+T cell | The immune mechanism | In a study of mice with liver tumors, CXCR6 was found to mediate the removal of NKT cells and CD4+T cells from senescent liver cells. | Mossanen et al. (2019) |
| CD4+T cell | immunotherapy | Liver-specific MYC transgenic mice fed the MCD diet were induced. Blockage of CPT with the pharmacological inhibitor perhexiline reduced apoptosis of CD4+T cells in the liver and inhibited tumor formation in HCC. These results provide useful information for the potential targeting of the CPT family to salvage intrahepatic CD4+T cells and for immunotherapy to assist NAFLD-promoted HCC. | Brown et al. (2018) |
| CD4+T cell | immunotherapy | Tumor-infiltrating LY6G MDSCs from orthotopic liver tumors treated with sorafenib significantly induced CD4+T cells expressing IL-10 and TGF-β and down-regulated the cytotoxic activity of CD8 T cells. | Chang et al. (2018) |
| CD4+T cell | The immune mechanism | Antibody against CD274(PD-ligand 1 [PD-L1]), TIM3, or LAG3 increases CD8 and CD4 TIL proliferation and cytokine production in response to stimulation by polyclonal antigens or TAA. | Zhou et al. (2017) |
| CD4+T cell | The immune mechanism | Blockage of PD-L1 can restore IFNγ/TNF-α production in BTLAPD-1 tumor CD4+T cells, but partially inhibit the activation of BTLAPD-1 CD4+T cells. | Zhao et al. (2016) |
| CD4+T cell | The immune mechanism | CB2 inactivation reduces expression of T cell recruitment chemokines and inhibits liver T cell recruitment, including specific CD4+ T cells. | Suk et al. (2016) |
| CD4+T cell | immunotherapy | IFNγ enzym-linked immunodot assay demonstrated that they induced antigenicity of specific CD4+T cells in healthy donors or in HCC patients before and after GPC3-SP vaccine administration. The natural processing of these epitopes was demonstrated by the immune response of helper T cells to dendritic cells (DCs) loaded with GPC3. | Sayem et al. (2016) |
| CD4+T cell | The immune mechanism | TGF-β expression was upregulated in DEN induced HCC mouse model. TGF-β promotes the differentiation of Foxp3 (+) CD4 (+) T cells (Treg cells) in vitro. | Shen et al. (2015) |
| CD4+T cell | immunotherapy | Intra-tumor combined administration of SLC and anti-CD25 mAb significantly reduced the frequency of Treg and increased the number of CD8+ and CD4+ T cells in tumor sites, and also maximally inhibited the growth and invasion of HCC. | Chen et al. (2013) |
| CD4+T cell | Prognostic marker | The high expression of IL-17 and IL-17RE is a promising predictor of poor prognosis in HCC. The precursor capacity of the CD4+ T cells that produce IL-17 may be involved in cross-talk of different types of inflammatory/immune cells than in HCC. | Liao et al. (2013) |
| CD4+T cell | The immune mechanism | CD25-Foxp3-T cells with a CD127-IL-10 + phenotype can be induced in vitro from naive CD4 (+) T cells involving programmed cell death 1 ligand 1, immunoglobulin-like transcript4, and human leukocyte antigen G. | Kakita et al. (2012) |
| CD4+T cell | The immune mechanism | In vitro restimulation experiments and in vivo depletion studies have shown that both CD4+ and CD8+ cells contribute to antitumor activity. Using PBMC from healthy volunteers and patients with HCC, it was shown that ASPH stimulation led to significant development of antigen-specific CD4+ T cells. | Shimoda et al. (2012) |
| CD4+T cell | Prognostic marker | Lack of recovered CD19, CD3, CD8, and especially CD4+T cells is associated with poor survival in patients. | Carr and Metes, (2012) |
| CD4+T cell | immunotherapy | Tregs significantly increased the inhibition of CD8+ and CD4 (+) T cell proliferation and cytokine secretion, and increased numbers of circulating CD4 (+) CD25 (+) Foxp3 (+) Tregs and tumor-infiltrating Foxp3 (+) cells prior to cryoablation were associated with a higher risk of recurrence or progression in HCC patients after cryoablation. | Zhou et al. (2010) |
| CD4+T cell | The immune mechanism | MDSC exerts its immunosuppressive function by inducing CD4 (+) CD25 (+) Foxp3 (+) regulatory T cells in co-cultured CD4 (+) T cells. | Hoechst et al. (2008) |
| CD4+T cell | immunotherapy | CD4+ T cells killed gene-independent CT26 cells and even homologous HEPA1-6 cells. In mice treated with DC/BNL + IL-12, a large number of CD4+ T cells and MHC class II positive macrophages infiltrated the tumor tissue. | Homma et al. (2005) |
| CD4+T cell | The immune mechanism | TRAIL receptors on HCC cells were upregulated by 5-FU, and TRAIL on CD4 (+) T cells, CD14 (+) monocytes and CD56 (+) NK cells was induced by IFNα. | Yamamoto et al. (2004) |
| CD4+T cell | The immune mechanism | IFN-γ was produced by incubation with DC/MIH-2 from CD4 (+) T cells but not from CD8+ T cells of inoculated mice. Anti-IFN-γ antibody attenuated the cytotoxicity of spleen cells. Immunization of CD4 (+) T cells with DCs loaded with homologous HCC cells, which produce IFN-γ in response to HCC antigens, leads to activation of macrophages that kill liver tumor cells at an early stage. | Irie et al. (2004) |
NK Cells
NK cells are an essential anti-tumor immune cell that primarily mediates immune surveillance of malignancies. It performs a similar function as CD8+ T cells: NK cells regulate the killing response of tumor cells by releasing perforin and granulein, triggering apoptosis in target cells. In addition, to improve their anticancer activity, NK cells can produce proinflammatory cytokines and chemokines (Voskoboinik et al., 2006; Guillerey et al., 2016; Habif et al., 2019). Existing studies have confirmed the value of NK cells in the development, targeted therapy, prognosis of HCC. Sprinzl et al. 's research confirmed that Sorafenib can promote the pro-inflammatory response of tumor-associated macrophages in HCC, and then activate the anti-tumor NK cell response through the cytokine and NF-κB pathway (Sprinzl et al., 2013). Senescence monitoring necessitates the recruitment and maturation of CCR2 myeloid cells, and CCR2 deficiency promotes HCC growth. Conversely, HCC cells suppress the maturation of recruited myeloid progenitors, which promotes mice HCC growth and worsens prognosis and survival in human HCC patients via NK cell inhibition (Eggert et al., 2016). Kohga et al. 's revealed that natural killer (NK) cells had stronger cytolytic activity on ADAM9KD-HCC cells than on control cells, and that this cytotoxicity is enhanced by the MICA/B and NK group 2, D pathways. Sorafenib treatment resulted in a decrease in ADAM9 expression in HCC cells, an increase in membrane-bound MICA expression, and a decrease in the quantity of soluble MICA. Sorafenib increased HCC cell NK sensitivity by boosting the expression of membrane-bound MICA (Kohga et al., 2010a). Table 2 summarizes current research on NK cells in HCC, confirming the importance of NK cells in immune escape and anti-HCC therapy.
TABLE 2.
The immune cells in TME: NK cells.
| Cells | The research direction | Result | Reference |
|---|---|---|---|
| NK cells | immunotherapy | Sorafenib can promote the pro-inflammatory response of tumor-associated macrophages in HCC, and then activate the anti-tumor NK cell response through the cytokine and NF-κB pathway. | Sprinzl et al. (2013) |
| NK cells | The immune mechanism | NK cell activator Poly (I:C) promotes HCC in HBs-Tg mice. Poly (I:C) induces liver inflammation and liver cell damage in HBs-Tg mice. The increase of hepatocyte EMT depends on the presence of NK cells in HBs-Tg mice. IFN-γ derived from NK cells plays a key role in the development of HCC in HBs-Tg mice. | Chen et al. (2019) |
| NK cells | The immune mechanism | The phenotype of peripheral blood NK cells was biased towards the defect/fatigue immune pattern, and the frequency of cells expressing NKp30 and member D of natural killer group 2 decreased, and the proportion of cells expressing T cell immunoglobulin and mucin domain increased. In addition, nKP30-positive NK cells have reduced expression of NCR3 immunostimulated splicing variants and increased expression of inhibitory variants, leading to NKP30-mediated loss of function in patients with advanced tumors. | Mantovani et al. (2019) |
| NK cells | Prognostic marker | Blocking the CD96−CD155 interaction restores NK cell immunity to tumor by reversing NK cell depletion or TGF-β1 reversing NK cell depletion, suggesting that CD96 may have a therapeutic role in HCC. | Sun et al. (2019a) |
| NK cells | The immune mechanism | When co-cultured with sorafenib treated M φ, cytotoxic NK cells were activated, resulting in tumor cell death. In addition, sorafenib was found to down-regulate the expression of major histocompatibility complex I in tumor cells, which may reduce tumor response to immune checkpoint therapy and promote NK cell response. | Hage et al. (2019) |
| NK cells | immunotherapy | Serum cholesterol accumulates in NK cells and activates their effect on HCC cells, increases the anti-tumor function of natural killer cells, and reduces the growth of liver tumors in mice. | Qin et al. (2020) |
| NK cells | The immune mechanism | CD48 protein was strongly expressed in HCC tissues but not in tumor liver monocytes. This monocyte induced NK cell dysfunction was significantly attenuated by blocking CD48 receptor 2B4 on NK cells, but not by blocking NKG2D and NKp30. | Wu et al. (2013) |
| NK cells | The immune mechanism | The cytotoxicity of NK cells in patients with HCC is reduced. MDSCs inhibit NK cell cytotoxicity and IFN-γ release. MDSCs inhibit NK cells depending on cell contact. MDSCs inhibit NK cells for a long time. MDSCs use NKp30 receptors to inhibit NK cell function. | Hoechst et al. (2009) |
| NK cells | The immune mechanism | Compared with donor and recipient PB, donor liver NK cells showed the strongest cytotoxicity to HCC HepG2 after IL-2 stimulation. This may explain why liver natural killer (NK) cells have higher cytotoxic activity against tumor cells than peripheral blood (PB) NK cells. | Ishiyama et al. (2006) |
| NK cells | The immune mechanism | SMICA derived from advanced HCC is responsible for NKG2D expression and NK cell function. NK cells stimulate DC maturation induced by human hepatoma cells and enhance the excitatory stimulation ability of DC. When NK cells were pretreated with serum containing SMicas, DC maturation and activation were completely eliminated. | Jinushi et al. (2005) |
| NK cells | immunotherapy | Leptin can significantly inhibit human HCC. This effect is mediated by inducing the proliferation and activation of natural killer cells and directly inhibiting tumor growth. The decreased NK expression of inhibitory CIS and the overexpression of anti-proliferative STAT2 and SOCS1 proteins in HCC lines may emphasize the anticancer effect of leptin. | Elinav et al. (2006) |
| NK cells | The immune mechanism | Smoking is associated with a decrease in the frequency of natural killer (NK) cells in the peripheral blood, which is characterized by a reduction in NK function through systemic immunology. The combination of smoking and lowering the frequency of NK cells further increases the likelihood of viral load and ALT≥80 U/L. | Wang et al. (2019b) |
| NK cells | The immune mechanism | NKT and CD4+T cells promote the elimination of senescent liver cells to prevent the occurrence of HCC, and this process requires CXCR6. CXCR6 inhibits the occurrence of HCC by promoting natural killer T and CD4+T cell-dependent senescence control. | Mossanen et al. (2019) |
| NK cells | immunotherapy | Using CAR transduced T cells and NK cells that recognize the surface marker CD147 (also known as Basigin), various malignant HCC cell lines were effectively killed in vitro, as well as HCC tumors in transplanted and patient-derived mouse models of transplanted tumors. | Tseng et al. (2020) |
| NK cells | The immune mechanism | The liver gene delivery of high IL-15 makes CD8+ T cells and NK cells proliferate in large quantities, resulting in the accumulation of CD8+ T cells in the body (over 40 days), especially in the liver. Hyper-IL-15 therapy has significant therapeutic effects on established liver metastases and even autologous HCC induced by DEN. These effects can be depleted by CD8+ T cells instead of NK cells. | Cheng et al. (2014) |
| NK cells | immunotherapy | The cytolytic activity of natural killer (NK) cells on ADAM9KD-HCC cells is higher than that on control cells, and the enhancement of this cytotoxicity depends on the MICA/B and NK group 2, D pathways. Sorafenib treatment resulted in a decrease in the expression of ADAM9 in HCC cells, an increase in the expression of membrane-bound MICA and a decrease in the level of soluble MICA. The addition of sorafenib enhanced the NK sensitivity of HCC cells by increasing the expression of membrane-bound MICA. | Kohga et al. (2010a) |
| NK cells | The immune mechanism | ADAM9 protease plays a key role in the shedding of MHC class I related chain A (MICA) that regulates the sensitivity of tumor cells to natural killer cells (NK). The expression of ADAM9 in CD133si-PLC/PRF/5 cells and CD133-Huh7 cells decreased, membrane-bound MICA increased, and soluble MICA production decreased. CD133si-PLC/PRF/5 cells and CD133-Huh7 cells are both sensitive to NK activity, which depends on the expression level of membrane-bound MICA, while HCC cells expressing CD133 are not. | Kohga et al. (2010b) |
| NK cells | The immune mechanism | CD8+ T cells and NKT cells promote NASH and HCC by interacting with hepatocytes, but not myeloid cells. NKT cells mainly cause steatosis by secreting light, and CD8+ and NKT cells synergistically induce liver damage. Hepatocyte LTβR and typical NF-κB signals promote the transformation of NASH to HCC, indicating that different molecular mechanisms determine the development of NASH and HCC. | Wolf et al. (2014) |
| NK cells | The immune mechanism | In-depth studies of the immune landscape show that regulatory T cells(T) and CD8 resident memory T cells(T) are enriched in hbv-related HCC, while Tim-3CD8 T cells and CD244 natural killer cells are in non-virus-related HCC In the enrichment. | Lim et al. (2019) |
| NK cells | The immune mechanism | Senescence monitoring requires the recruitment and maturation of CCR2 bone marrow cells, while CCR2 ablation induces HCC growth. In contrast, HCC cells inhibit the maturation of recruited myeloid precursors, which promote mouse HCC growth and deteriorate the prognosis and survival of human HCC patients by inhibiting NK cells. | Eggert et al. (2016) |
| NK cells | The immune mechanism | β-glucosylceramide alleviates immunologically incongruent disease by altering the plasticity of NKT lymphocytes and may be involved in the “fine-tuning” of the immune response. | Zigmond et al. (2007) |
| NK cells | The immune mechanism | Proliferating immune cells, mainly NK cells and T cells, were present in the patient’s long-lived tumor and consisted only of tumor cells lacking proliferation in the region. The density of NK cells and CD8+T cells was positively correlated with tumor cell apoptosis and negative proliferation. | Chew et al. (2010) |
| NK cells | immunotherapy | GS-9620 treatment is associated with a reversible increase in serum liver enzymes and thrombocytopenia, and induction of intrahepatic CD8+ T cells, NK cells, B cells, and interferon response transcriptional signaling. | Menne et al. (2015) |
| NK cells | The immune mechanism | Fibrosis is a way to enhance the occurrence of HCC. Changes in fibrosis also regulate the activity of inflammatory cells in the liver and reduce natural killing, which is generally helpful for tumors to monitor the activity of natural killer T cells. These pathways work in conjunction with inflammatory signals, including telomerase activation and the release of reactive oxygen species, ultimately leading to cancer. | Zhang and Friedman, (2012) |
| NK cells | immunotherapy | AdCMVmCD40L therapy can induce strong lymphocyte infiltration in tumor tissues and increase the apoptosis of malignant cells. The observed anti-tumor effect is mediated by CD8+ T cells and is related to increased serum levels of interleukin (IL)-12 and enhanced natural killer (NK) activity. | Schmitz et al. (2001) |
| NK cells | The immune mechanism | The activation of β-catenin in hepatocytes can change the liver microenvironment and lead to the specific targeting of iNKT cells. The activation of β-catenin in hepatocytes triggers the pro-inflammatory process related to the activation of NF- κ B. In the process of liver inflammation induced by β-catenin, iNKT cells showed anti-inflammatory properties. In HCC induced by β-catenin, iNKTs and LECT2 are the key cellular and molecular effectors to control tumor progression. | Anson et al. (2012) |
| NK cells | The immune mechanism | AdCMVIL-12 can activate natural killer cells (NK) and inhibit angiogenesis. | Barajas et al. (2001) |
| NK cells | The immune mechanism | Gene transfer of angiostatin inhibited tumor angiogenesis and enhanced NK cell infiltration, while B7H3 therapy activated CD8+ and NK cells and increased their infiltration into the tumor, and enhanced circulating IFN-γ levels. | Ma et al. (2007) |
Dendritic cells
DC cells, as specialized antigen-presenting cells in the human body, can present antigens to T cells and produce costimulatory signals for T cell activation. According to the current study, mature DC cells can penetrate tumor cells and limit tumor incidence and progression. Under many severe conditions, this inhibition effect will be avoided by tumors through certain means. Therefore, targeting at DC cells, some studies have reported its role in the occurrence, development, immunotherapy, diagnosis and prognosis of HCC. For example, In mice, combining DC vaccination and PD-L1 inhibitor treatment can result in longer overall life, reduced tumor volume, and increased tumor cell apoptosis. As a new therapy method for HCC, combined treatment with DC vaccination and PD-L1 inhibitor may offer promising results (Teng et al., 2020). Ali et al. 's research clarified that the combination of PEI or RFTA with active antigen-specific immunotherapy using DCS is a promising approach to induce a sustained anti-tumor immune response aimed at reducing tumor recurrence and metastasis in patients with HCC. Table 3 summarizes the current role of DC cells in HCC.
TABLE 3.
The immune cells in TME: Dendritic cells.
| Cells | The research direction | Result | Reference |
|---|---|---|---|
| Dendritic cells | immunotherapy | The combination of DC vaccine and PD-L1 inhibitor resulted in longer overall survival, smaller tumor size, and higher tumor cell apoptosis rate in mice. The combination of DC vaccine and PD-L1 inhibitor may have broad prospects as a new therapeutic strategy for HCC. | Teng et al. (2020) |
| Dendritic cells | The immune mechanism | XCL1-GPC3 cells chemically attract murine XCR1CD8α dendritic cells (DCs) and human XCR1CD141 DCs, and promote their IL12 production. | Chen et al. (2020) |
| Dendritic cells | The immune mechanism | A more severe reduction in basal OCR was observed in tumor-derived DCs exposed to AFP due to down-regulation of cytochrome C oxidase. The expression of PGC1-α in circulating medullary DC in HCC patients was decreased, and the ability to stimulate the function of antigen-specific effector was impaired, indicating the negative effect of AFP on DC metabolism. | Santos et al. (2019) |
| Dendritic cells | The immune mechanism | AFP down-regulated CD1 on DC, but had little effect on NKT cell activation. | Li et al. (2019a) |
| Dendritic cells | The immune mechanism | DC-CIK cells can inhibit the growth of HCC and LCSC in vitro and in vivo, and the most successful DC-triggered cell killing activity can be achieved through their LCSC antigen loading. | Yang et al. (2018b) |
| Dendritic cells | The immune mechanism | MIP-10 enhances the antitumor activity of the DC/tumor fusion vaccine by alleviating the immunosuppressive tumor environment. | Hu et al. (2017) |
| Dendritic cells | immunotherapy | The use of nifurazine and DC-loaded TCL significantly increased the survival rate, inhibited tumor growth and promoted anti-tumor immune response in HCC mice implanted in situ. | Zhao et al. (2017b) |
| Dendritic cells | immunotherapy | Overexpression of IL-12 induced by adenovirus vector can effectively immunize DC. Intratumor but not systemic injection of activated IL-12-DC is essential for effective tumor regression. Improved immunotherapy with IL-12-DC represents a promising approach for the treatment of HCC. | Vogt et al. (2014) |
| Dendritic cells | immunotherapy | β-GC activated mouse liver NKT cells and enhanced the anti-tumor activity of PAD-HBsAg-DC. β-GC may act as an effective innate immune enhancer to enhance the antitumor effect of PAD-HBsAg-DC vaccine. | Long et al. (2013) |
| Dendritic cells | immunotherapy | Camory may play an important role in the development and progression of HCC through recruitment of DC and NK cells. | Lin et al. (2011) |
| Dendritic cells | The immune mechanism | Electroporation of GPC-3 mRNA is an effective method for antigen-carrying monocytes to generate DCs because they produce functional GPC-3 reactive T cells in vitro. | O'Beirne et al. (2010) |
| Dendritic cells | The immune mechanism | Immature DCs(IMDCs) derived from human monocytes were fully mature after effective phagocytosis of dying cells, and showed significant proliferation and cytotoxicity to HLA-matched HEPG (2) cells in autologous peripheral blood monocytes (PBMC). | Xing et al. (2009) |
| Dendritic cells | The immune mechanism | Secondary lymphoid tissue chemokines (SLC) are strongly expressed in secondary lymphoid organs. It has the ability to promote dendritic cell (DC) and T cell chemotaxis, making it a promising candidate for cancer therapy. | Liang et al. (2007) |
| Dendritic cells | immunotherapy | AdvHAFP-transduced DCs activate higher frequencies of Th1 CD4 responses to AFP in healthy donors and AFP positive HCC patients. Importantly, when activated by adenovirus-engineered DC, the cytokine expression profile of CD4+T cells was biased towards the production of interleukin-2 and interferon-γ, which has therapeutic implications for vaccination work. | Evdokimova et al. (2007) |
| Dendritic cells | immunotherapy | Dendritic cells transfected with total HCC mRNA stimulated an antigen-specific cytotoxic T cell response capable of recognizing and killing autologous tumor cells in vitro. | Peng et al. (2006) |
| Dendritic cells | The immune mechanism | Impairment of MDCs produced by IL-12 may result in impaired stimulation of naive T cells, suggesting that targeted IL-12 therapy may enhance tumor-specific immune responses in patients with HCC. | Ormandy et al. (2006) |
| Dendritic cells | immunotherapy | The combination of PEI or RFTA with active antigen-specific immunotherapy using DCS is a promising approach to induce a sustained anti-tumor immune response aimed at reducing tumor recurrence and metastasis in patients with HCC. | Ali et al. (2005) |
| Dendritic cells | The immune mechanism | The phenotypic and functional deficits of PBMC-derived DCs in LC and HCC patients may play a key role in HBV infection and HCC immune escape. After tumor is stimulated by antigen, DC function can be enhanced in LC patients. | Wong et al. (2005) |
| Dendritic cells | The immune mechanism | Ad-HBsAg-transduced DCs stimulated a strong cytotoxic T lymphocyte (CTL) response to HBsAg-expressing tumor cells and protected mice from lethal tumor attack. | Qiu et al. (2005) |
| Dendritic cells | immunotherapy | At concentrations up to 20 μg/mL, AFP did not alter the in vitro generation, maturation and T cell stimulation of DC. Higher AFP concentration ( >20 μg/ml) led to phenotypic changes in DC without impair its ability to stimulate CD4+ T cells. Independent of serum AFP levels, the frequency and function of DC and AFP-specific T cells did not decrease in HCC patients. | Ritter et al. (2004) |
| Dendritic cells | immunotherapy | Autologous DCs containing the HCA587 protein can induce specific T cell responses in healthy individuals by in vitro stimulation, and HCA587 is a good candidate for the development of a protein-based therapeutic DC tumor vaccine for the treatment of HCC patients. | Li et al. (2004) |
| Dendritic cells | immunotherapy | DCs transfected with MAGE-1 gene can induce higher cytotoxicity of SMMC7721 in vitro, suggesting that this transgenic DC may have the potential to induce specific antitumor activity and be used as a novel HCC vaccine. | Liu et al. (2001) |
| Dendritic cells | The immune mechanism | Decline in DC function and normal T cell response were observed in HBV-infected HCC patients, suggesting that the low function of DC is related to the pathogenesis of HBV or HCV-infected HCC. | Kakumu et al. (2000) |
M1-Polarized Macrophages
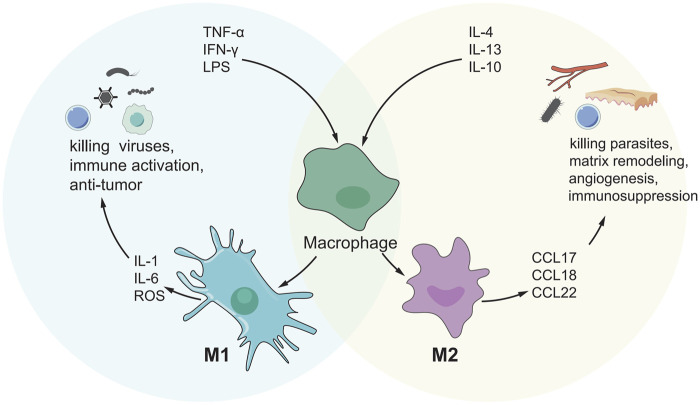
Another important type of immune cell in TME is macrophages derived from circulating monocytes, which can generally be divided into M2 polarization and M1 polarization (Figure 2). M1-polarized macrophages, for example, can create pro-inflammatory cytokines and reactive oxygen species/nitrogen to prevent the formation and progression of malignancies (Aras and Zaidi, 2017). There are limited investigations on the function of M1-polarized macrophages in HCC at the moment. Studies have shown that M1-polarized macrophages in the S3 subclass in HCC increased, and the prognosis was good. Memory B cells, Total B cells, M1 macrophages and T follicle helper cells, were linked with strong total immune cell infiltration into HCC, whereas resting mast cells, neutrophils, and NK cells were associated with poor infiltration (Rohr-Udilova et al., 2018). Table 4 summarizes the current role of M1-polarized macrophages in HCC.
FIGURE 2.
M1/M2 model of macrophage activation. M1 cells exert an inflammatory phenotype and are involved in killing bacteria, viruses and tumor cells, while M2 cells are involved in killing encapsulated parasites, immunosuppression, angiogenesis, etc.
TABLE 4.
The immune cells in TME: M1-polarized macrophages.
| Cells | The research direction | Result | Reference |
|---|---|---|---|
| M1-polarized macrophages | The immune mechanism | The number of M1-polarized macrophages in the S3 subclass in HCC was increased, and the prognosis was good. Strong total immune cell infiltration into HCC was associated with total B cells, memory B cells, T follicle helper cells, and M1 macrophages, while weak infiltration was associated with resting NK cells, neutrophils, and resting mast cells. | Rohr-Udilova et al. (2018) |
| M1-polarized macrophages | The immune mechanism | Conditionalized media from M1 macrophages promoted HCC cell migration and induced activation of NF-κB and FAK signal transduction. Activation of Bay 11-7,802 and NF-κB and FAK pathways eliminated HCC cell induced migration, suggesting that M1-like TAM has a metastatic role in HCC. | Wang et al. (2014) |
Tumor-Promoting Immune Cells
In the immune microenvironment of HCC, some cells could promote the occurrence and development of HCC, and we will review them one by one.
Regulatory T cells(Tregs)
Tregs play a vital role in immunological homeostasis and immune self-tolerance, and they can express the CD4+ marker and the Foxp3 marker (Samstein et al., 2012). Foxp3+ Treg acts as a switch for all levels of immune response, and its effects appear to be two-sided. First, Treg can inhibit harmful immune responses and thus inhibit the occurrence of autoimmune diseases (Berod et al., 2012). Second, Treg suppresses protective immune responses against invading pathogens or tumors, leading to further progression of the disease (Sakaguchi et al., 2010). How does Treg play a role in tumors, including how does Treg infiltrate and metastasize to tumor sites or how does Treg help tumors evade immune monitoring, has become a hot research topic in recent years. Many ideas have been put forward. Tregs were found in much higher numbers in HCC patients than in healthy controls. In addition, patients with high Treg(III) levels after TACE had a significantly lower progression-free survival than patients with low Treg(III) levels after TACE (Park et al., 2020). Other studies have shown that tumor Treg upregulated the expression of the glucocorticoid-induced tumor necrosis factor receptor (GITR). Treatment with soluble GITR ligand (GITRL) reduced inhibition caused by activated tumor infiltrating Treg and restored CD4+ CD25-T cell proliferation and cytokine production. (Pedroza-Gonzalez et al., 2013). In addition to that, the proportion of Tregs cells in HCC patients was significantly higher than that in healthy and cirrhosis controls, and was related to various clinical indicators of HCC patients. In HCC patients with BCLC stage C, the proportion of Treg cells was more pronounced than in BCLC stage B patients. One to 2 weeks after surgery, the fraction of Treg cells was much lower than before GSMS-TACE. Three to 5 weeks following surgery, the proportion of Treg cells continued to decline (Ren et al., 2021). Table 5 summarizes the most credible studies related to the role of Treg in HCC.
TABLE 5.
Tumor-promoting immune cells: Regulatory T cells.
| Cells | The research direction | Result | Reference |
|---|---|---|---|
| Treg | immunotherapy | The proportion of Treg cells in BCLC stage C HCC patients was higher than that in BCLC Stage B patients, and the proportion of Treg cells was significantly lower than that before GMS-TACE 1 ∼ 2 weeks after surgery. The percentage of Treg cells continued to decrease 3–5 weeks after surgery. | Ren et al. (2021) |
| Treg | The immune mechanism | Tumor progression is associated with the deep depletion of tumor antigen-specific CD8T cells and the accumulation of PD-1 CD8T cells and Treg cells. | Tipton et al. (2011) |
| Treg | The immune mechanism | At a non-cytotoxic concentration, resveratrol inhibited differentiation of CD8CD122 Treg from CD8CD122 T cells. | Zhang et al. (2020) |
| Treg | immunotherapy | The baseline reduction in the number or frequency of FOXP3Tregs, MDSCs, and exhausted T cells was significantly greater after tivozanib treatment. In addition, a larger increase in CD4T cells: Treg ratio after tivozanib treatment compared with sorafenib was associated with a significant improvement in OS. | Kalathil et al. (2020) |
| Treg | The immune mechanism | Long-term intake of ethanol can enrich HBV-enhanced abnormal lipid metabolism through HBx/Swaell1/arachidonic acid signaling and activate Treg in mice. | Liu et al. (2020a) |
| Treg | The immune mechanism | Lower CD8 T cell density and higher Foxp3 Tregs and immune checkpoint strength in intrahepatic cholangiocarcinoma (ICC) components compared to HCC components may indicate a stronger immune escape capability of ICC. | Zheng et al. (2020b) |
| Treg | Prognostic marker | The frequency of Tregs was significantly higher in HCC patients than in healthy controls. In addition, patients with high Treg (III) after TACE had a significantly reduced progression-free survival compared to patients with low Treg (III) after TACE. | Park et al. (2020) |
| Treg | The immune mechanism | Regulatory CD4/CD25/Foxp3 T cells (Tregs) were activated by transcriptional reprogramming of HCC parent cells in MacroH2A1 KD conditioned medium. Loss of MacroH2A1 in HCC cells drives proliferation and avoidance of immune surveillance by cancer stem cells. | Lo Re et al. (2020) |
| Treg | The immune mechanism | Treg-induced inhibition of IFN-γ secretion is partially prevented by neutralizing PD-1 and PD-L1 antibodies in HCC patients. In HCC, peripheral blood Tregs upregulate checkpoint inhibitors and promote systemic immune dysfunction and antitumor activity through several inhibitory pathways, presumably contributing to the development of tumors at a young age. | Langhans et al. (2019) |
| Treg | Prognostic marker | Patients with an increased T-effector/Treg ratio before treatment showed significant improvement in OS. | Kalathil et al. (2019) |
| Treg | The immune mechanism | Overexpression of lncRNA FENDRR and down-regulated miR-423-5p reduced cell proliferation and tumorigenicity, and promoted apoptosis of HCC cells, thereby regulating Treg-mediated immune escape of HCC. | Yu et al. (2019a) |
| Treg | immunotherapy | The hypoxic environment induces tumor immunosuppression by attracting TREM-1 TAMs of CCR6. Foxp3 Treg, and TREM-1 TAMs make HCC resistant to PD-L1 therapy | Wu et al. (2019a) |
| Treg | immunotherapy | After sorafenib alone and in combination, plasma SMet was elevated and TTP and OS shortening were associated with increased Tregs and CD56 natural killer (NK) cells. | Goyal et al. (2019) |
| Treg | immunotherapy | Sunitinib treatment induces an anti-tumor immune response by significantly reducing Treg frequency, TGF-β and IL-10 production by Treg, and protecting TAS CD8 T cells from HCC infection | Liu et al. (2017) |
| Treg | immunotherapy | Newly produced STAT3-blocked whole-cell HCC vaccines reduced production of Treg as well as production of TGF-β and IL-10. | Han et al. (2017) |
| Treg | The immune mechanism | LNC-EGFR specifically binds to EGFR and prevents its interaction with c-CBL and is ubiquitinated by c-CBL, which stabilizes and enhances the activation of its own and its downstream AP-1/NF-AT1 axis, thus causing EGFR expression. LNC-EGFR has been associated with immunosuppressive status and cancer by promoting Treg cell differentiation. | Jiang et al. (2017b) |
| Treg | The immune mechanism | Overexpression and activation of YAP-1 in HCC T cells can promote differentiation of Treg through enhanced transcription of TGFbR2, thereby inducing immunosuppression. | Fan et al. (2017) |
| Treg | Prognostic marker | CXCL10/CXCR3 signals were upregulated after liver graft injury, directly inducing the mobilization and recruitment of Tregs during transplantation, and further promoting the recurrence of HCC after transplantation. | Li et al. (2016) |
| Treg | immunotherapy | After treatment with sorafenib, the ratio of CD4CD127PD-1 T effector cells to CD4FoxP3PD-1 Treg was significantly increased. The increased frequency of CD4CD127 T effector cells in posttreated samples was significantly correlated with OS. | Kalathil et al. (2016) |
| Treg | immunotherapy | Sunitinib-mediated tumoricidal effect, Treg inhibition and antibody-mediated PD-1 blocking synergistic effect can effectively inhibit tumor growth and activate anti-tumor immunity. | Li et al. (2017) |
| Treg | The immune mechanism | The secreting of cancerous TGF-β1 may increase Tregs, while TGF-β1 knockdown may impair immunosuppression in the tumor microenvironment by decreasing Tregs. | Wang et al. (2016) |
| Treg | The immune mechanism | Intra-tumor combination of SLC and anti-CD25 mAb is an effective method for the treatment of HCC, which is related to the change of tumor microenvironment and the systematic optimization percentage of Treg, CD8+ T cells and CD4+ T cells in peripheral immune organs. | Chen et al. (2013) |
| Treg | immunotherapy | Sorafenib treatment can reduce the number of Treg by inhibiting the proliferation of Treg and inducing its apoptosis. In addition, sorafenib inhibits the function of Tregs, characterized by reduced expression of functionally important Treg-related molecules and impaired inhibition. Sorafenib treatment alleviated non-cellular autonomous inhibition of the tumor microenvironment mediated by Treg, leading to an effective anti-tumor immune response. | Chen et al. (2014) |
| Treg | immunotherapy | The subpharmacological doses of sorafenib had different effects on T cell subsets, selectively increasing Teff activation while blocking Treg function. | Cabrera et al. (2013) |
| Treg | The immune mechanism | Tumor Treg upregulated glucocorticoid-induced tumor necrosis factor receptor (GITR) expression. Treatment with soluble GITR ligand (GITRL) induced a reduction of inhibition mediated by activated tumor infiltrating Treg and restored the proliferation and cytokine production of CD4+ CD25-T cells. | Pedroza-Gonzalez et al. (2013) |
| Treg | The prognosis | Elevated FOXP3 (+) Tregs may represent a prognostic marker in patients with early HCC. The natural history of CHB influences the density of tumor infiltrate Treg in patients with chronic hepatitis B virus infection. | Wang et al. (2012) |
| Treg | The immune mechanism | The increased frequency of CD45Ro + subsets in CD4+ CD25(HIGH) Tregs in HCC patients may cooperate with the establishment of an immunosuppressive environment that induces tolerance of plasmocyte like DCs, thereby promoting the development of HCC. | Takata et al. (2011) |
| Treg | The immune mechanism | The tumor-associated MVARPHI may trigger an increase in the number of Foxp3 (+) Treg populations in tumors, thereby promoting the development of HCC. | Zhou et al. (2009) |
Myeloid-Derived Suppressor cells
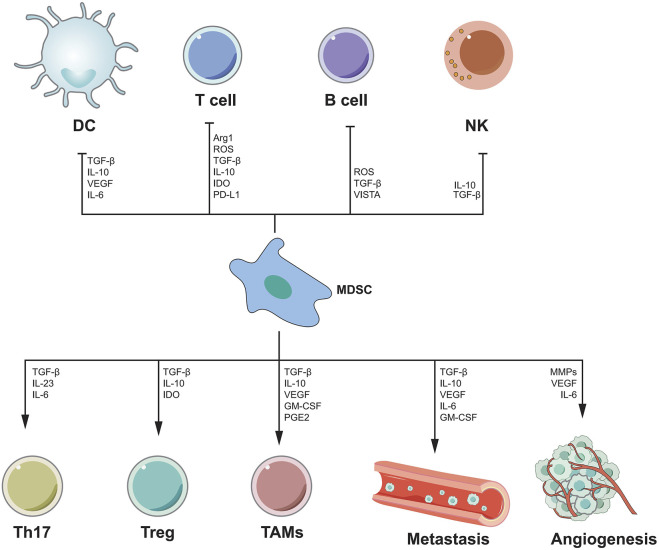
MDSC is thought to be a cancer-promoting immune cell in the HCC tumor microenvironment and was discovered a decade ago (Gabrilovich et al., 2007). MDSC is divided into granulocyte or multinuclear MDSC(PMN MDSC) and mononuclear MDSC(M-MDSC) (Veglia et al., 2018). MDSCs enhance angiogenesis by producing vascular endothelial growth factor (VEGF), actuator 2 and MMP9. They can also cause cancer cells to migrate to endothelial cells and encourage metastasis (Zhou et al., 2018a). MDSC also suppresses T cell activity by secreting immunosuppressive cytokines, inducible nitric oxide synthase, and argininase (Gabrilovich et al., 2012; Gabrilovich, 2017). MDSCs can have a dual influence on immune cells via distinct methods. B cells, T cells, DCs and NK cells, are all inhibited by MDSCs. MDSCs, on the other hand, can stimulate Th17 cells, Tregs, and TAMs, as well as tumor angiogenesis and metastasis (Figure 3). There has been a great deal of research on the processes through which MDSC supports the advancement of HCC, and many therapeutic pathways have been developed for MDSC as a target of HCC. For example, myeloid-derived suppressor cells (MDSCs) are drawn to the tumor microenvironment by PIWIL1-overexpressed HCC cells. MDSCs consumption reduced the proliferation and growth of PIWIL1-overexpressed HCC tumors. Complement C3 stimulates HCC cell secretion via PIWIL1 and mediates the contact between HCC cells and MDSC via p38 MAPK activation in MD38, and then initiates the expression of immunosuppressive cytokine IL10. PIWIL1, which is expressed by tumor cells, could be a viable target for the development of new HCC treatments (Wang et al., 2021a). Tumor-infiltrating LY6G MDSCs from orthotopic liver tumors treated with sorafenib dramatically increased CD4 T cells expressing IL-10 and TGF-and decreased CD8 T cell cytotoxicity. In vitro, IL-6 protects LY6G MDSC from sorafenib-induced cell death. Combining sorafenib and anti-IL-6 antibody or anti-LY6G antibody dramatically decreased the cell proportion of LY6G MDSCs in orthotopic liver tumors, synergistically boosted sorafenib’s therapeutic efficacy and increased T cell proliferation (Chang et al., 2018). Icaritin blocks MDSC production by blocking the attenuation of EMH, thereby inhibiting the immunosuppressive effect of the tumor, thereby triggering an anti-tumor immune response. Therefore, Icaritin can be used as a new adjuvant or even as an independent therapeutic agent for the effective treatment of HCC(Tao et al., 2021). In Table 6, we show the relevant role of MDSC in HCC immune microenvironment in recent years.
FIGURE 3.
The mechanism of MDSC-mediated immunosuppression. MDSC inhibits the functions of DC, T cells, B cells and NK cells by secreting various cytokines, while promoting the functions of Th17, Treg, TAMs cells, and can promote angiogenesis and metastasis.
TABLE 6.
Tumor-promoting immune cells: Myeloid-derived suppressor cells.
| Cells | The research direction | Result | References |
|---|---|---|---|
| MDSCs | The immune mechanism | The heterozygous loss of SPTBN1 significantly upregulated the liver expressions of IL-1α, IL-1β and IL-6, and increased the proportion of myeloid inhibitory cells (MDSC) and CD4CD25Foxp3 regulatory T cells (Foxp3Treg) in liver, which promoted the occurrence of HCC in DDC-fed mice. | Lin et al. (2021) |
| MDSCs | The immune mechanism | MDSCs contribute to tumor progression under psychological stress, chronic binding stress significantly promotes the growth of HCC, and MDSCs are mobilized from bone marrow to spleen and tumor sites. Also, the β-adrenergic signaling cascade plays a key role in the mobilization and recruitment of MDSC under chronic confinement stress. | Cao et al. (2021) |
| MDSCs | immunotherapy | Icaritin blocks MDSC production by blocking the attenuation of EMH, thereby inhibiting the immunosuppressive effect of the tumor, thereby triggering an anti-tumor immune response. Therefore, Icaritin can be used as a new adjuvant or even as an independent therapeutic agent for the effective treatment of HCC. | Tao et al. (2021) |
| MDSCs | immunotherapy | PIWIL1 overexpressed HCC cells attract myeloid suppressor cells (MDSCs) to the tumor microenvironment. MDSCs consumption reduced the proliferation and growth of HCC tumors overexpressed by PIWIL1. Complement C3 induces the secretion of HCC cells through PIWIL1, mediates the interaction between HCC cells and MDSC by activating the P38 MAPK signal in MD38, and then initiates the expression of the immunosuppressive cytokine IL10. | Wang et al. (2021a) |
| MDSCs | immunotherapy | After tivozanib treatment, the baseline number or frequency of FOXP3treg, MDSC, and exhausted T cells decreased significantly more. This may help identify patients who may benefit from c-kit/SCF antagonism and provide guidance for improving the efficacy of tivozanib in combination with immunotherapy. | Kalathil et al. (2020) |
| MDSCs | The immune mechanism | CD8+ T cells, MDSCs, and M2 macrophages were particularly increased in the tumorigenic liver of NCoA 5 ± male mice. NCoA5 deficiency promotes a unique hepatic tumorigenetic microenvironment through p21WAF1/CIP1 overexpression, which metformin reverses. | Williams et al. (2020) |
| MDSCs | immunotherapy/The immune mechanism | HSC promoted migration of MDSC through the SDF-1/CXCR4 axis. Pretreatment of MDSC with CXCR4 inhibitors or injection of SDF-1 knockout HSC inhibited migration of MDSC to the spleen and liver of tumor-bearing mice. | Xu et al. (2019) |
| MDSCs | Prognostic marker | Patients with an increased T-effector/Treg ratio before treatment showed significant improvement in OS. ERK + FLT-3+ Treg and MDSCs were significantly reduced after sorafenib treatment. An increase in baseline Flt-3+ p-ERK + MDSC was associated with a patient survival benefit. Conclusion High baseline CD4+ T effector/Treg ratio may be an important biomarker for prognosis in HCC. | Kalathil et al. (2019) |
| MDSCs | immunotherapy | CCR2 antagonists inhibited the infiltration of TAM and MDSC and delayed tumor growth in tumors of mice expressing A3b and A3b. Mechanically, upregulation of A3B in HCC inhibs the global abundance of H3K27me3 and reduces the presence of H3K27me3 on the chemokine Ccl2 promoter by interacting with the multicomb repressor complex 2(PRC2), thus recruiting large amounts of TAM and MDSC. | Wang et al. (2019c) |
| MDSCs | immunotherapy | Activated HSC induces mononuclear intrinsic p38 MAPK signaling, which triggers enhancer reprogramming for M-MDSC development and immunosuppression. Treatment with p38 MAPK inhibitors eliminated HSC-M-MDSC crosstalk to prevent HCC growth. Combined with I-BET762 suppressed patient-derived M-MDSC, combined with anti-PD-L1 therapy synergically enhanced TIL, resulting in tumor eradication and prolonged survival in a fibrotic HCC mouse model. | Liu et al. (2020b) |
| MDSCs | The immune mechanism | RIP3 knockdown results in an increase in MDSCs and a decrease in interferon Δ- positive (IFN-γ) clusters of tumor-infiltrating lymphocytes (CD8) differentiated into 8 positive (CD8) cells in HCC tissue, thus promoting immune escape and HCC growth in immunologically competent mice. | Li et al. (2019b) |
| MDSCs | The immune mechanism | By down-regulating the expression of IDO1, the HS donor induced T effector cells and inhibited MDSCs, and effectively restricted the tumor development of H22 HCC tumor-bearing mice. | Yang et al. (2019c) |
| MDSCs | The immune mechanism | March-derived suppressor cells (MDSCs) and tumor-associated macrophages (TAM) from the tumor microenvironment contribute to the suppression of the CD8 T cell response. | Liu et al. (2018a) |
| MDSCs | immunotherapy | Adoptive transfer of CIK to tumor-bearing mice induced an increase in inflammatory mediators (e.g., CX3CL1, IL-13) and tumor-infiltrating MDSC in the tumor microenvironment, and MDSCs effectively inhibited the cytotoxic activity of CIKs in vitro. In contrast, treatment with PDE5 inhibitors reversed MDSC inhibition by Arg1 and iNOS, while systemic treatment with PDE5 inhibitors prevented MDSC accumulation in the tumor microenvironment after CIK cell treatment and increased its anti-tumor efficacy. | Yu et al. (2019b) |
| MDSCs | The immune mechanism | RT/IL-12 significantly reduced the accumulation of tumor-infiltrating myeloid suppressor cells (MDSC) and its inhibitory function by reducing the production of reactive oxygen species | Wu et al. (2018) |
| MDSCs | immunotherapy | Tumor-infiltrating LY6G MDSCs from orthotopic liver tumors treated with sorafenib significantly induced CD4+T cells expressing IL-10 and TGF-β and down-regulated the cytotoxic activity of CD8 T cells. IL-6 protects LY6G MDSC against sorafenib induced cell death in vitro. The combination of anti-LY6G antibody or anti-IL-6 antibody and sorafenib significantly reduced the cell proportion of LY6G MDSCs in orthotopic liver tumors, enhanced the proliferation of T cells, and synergically improved the therapeutic effect of sorafenib. | Chang et al. (2018) |
| MDSCs | The immune mechanism | Tumor-infiltrating CD11BCD33HLA-DR MDSCs in HCC patients can effectively inhibit autologous CD8T cell proliferation. Concordant overexpression of CCRK and MDSC markers (CD11b/CD33) was positively associated with poorer survival. Hepatocyte CCRK stimulated the immunosuppressive CD11BCD33HLA-DR MDSC amplification of human peripheral blood mononuclear cells by up-regulating IL-6. | Zhou et al. (2018b) |
| MDSCs | The immune mechanism | In HCC, hypoxia induces the expression of ENTPD2 on cancer cells, leading to an increase in extracellular 5′-AMP, which in turn promotes MDSC maintenance by preventing its differentiation. | Chiu et al. (2017) |
| MDSCs | immunotherapy | The tumor suppressive effects of chemerin were associated with metastasis of tumor-infiltrating immune cells from myeloid suppressor cells (MDSC) to interferon-γ T cells and decreased tumor angiogenesis. | Lin et al. (2017) |
| MDSCs | The immune mechanism | TAF-derived cytokines (such as IL-6 and SDF-1A) can induce MDSC generation and activation, and then weaken the human anti-tumor immune response, thus creating favorable conditions for the development of HCC. | Deng et al. (2017) |
| MDSCs | immunotherapy | The frequency of MDSC before treatment is a prognostic factor for HAIC prevention of HCC. Patients with lower MDSC frequency also had significantly longer overall survival. | Mizukoshi et al. (2016) |
| MDSCs | immunotherapy | The frequency of MDSC increased significantly in HCC patients. It is associated with tumor progression, but not with liver fibrosis or inflammation. | Arihara et al. (2013) |
| MDSCs | The immune mechanism | The MDSC-mediated functional inhibition of NK cells mainly depends on NKP30 on NK cells. | Hoechst et al. (2009) |
Cancer-Associated fibroblasts
CAF is not an immune cell, but it plays an important role in the tumor microenvironment, so we will introduce it in detail here. CAF exists as a prominent component of the tumor stroma between various inflammatory cells and components in the tumor microenvironment (Kalluri, 2016). As a result, CAF possesses functions that normal fibroblasts do not. A vast number of prior studies have demonstrated that CAF plays a critical function in changing the tumor microenvironment and driving the development of a variety of cancers (Jiang et al., 2017a; Zhao et al., 2017a; Deng et al., 2017; Pistore et al., 2017). CAF is also significant in HCC. Many studies have revealed the great role of CAF in the pathogenesis, progression, prognosis, treatment and other aspects of HCC. CAF-derived cardioctonutrient-like cytokine 1 (CLCF1) has been found in studies to stimulate the release of TGF-β and CXCL6 in tumor cells, consequently increasing tumor stem cell development in HCC-TME (Song et al., 2021). Other research have found that CCN2, EMA, and FAP expression may be involved in the activation of CAF in HCC, resulting in aggressive behavior. The substantial association between EMA-expressing tumor cells and FAP-expressing CAF, as well as their topographical proximity, suggests that there may be interplay between tumor epithelial and stromal cells in the HCC tumor microenvironment (Kim et al., 2014). Table 7 summarizes the current role of CAF in HCC.
TABLE 7.
Tumor-promoting immune cells: cancer-associated fibroblasts.
| Cells | The research direction | Result | Reference |
|---|---|---|---|
| CAF | The immune mechanism | Sulf2 secreted by HCC cells induces THE differentiation of HSC into CAF through the TGFβ1/Smad3 signaling pathway. | Wang et al. (2021b) |
| CAF | immunotherapy | CNP inhibits the HCC promotion of CAF by inhibiting several HCC promoting cytokines secreted by CAF expressing GPR68. Further studies have shown that the combination of CNP and existing anticancer agents has some potential in the treatment of intractable HCC associated with the activation of CAF. | Yamanaka et al. (2021) |
| CAF | The immune mechanism | CAF-derived cytokines enhance the progression and metastasis of HCC by activating the circRNA-miRNA-mRNA axis in tumor cells. | Liu et al. (2021) |
| CAF | The immune mechanism | In HCC-TME, CAF-derived cardioctonutrient-like cytokine 1(CLCF1) increases the secretion of CXCL6 and TGF-β in tumor cells, thereby promoting tumor stem cell growth. | Song et al. (2021) |
| CAF | immunotherapy | Coptidine blocked the secretion of CAF exosome CIRCCCT3 and significantly inhibited tumor growth of HepG2 cells in immunodeficient mice. | Lv et al. (2020) |
| CAF | The immune mechanism | MiR-150-3p was significantly reduced in CAFS-derived exosomes and inhibited HCC migration and invasion. MiR-150-3p was transferred from miR-150-3p transfected CAF to HCC cells via exosomes and eliminated HCC migration and invasion. | Yugawa et al. (2021) |
| CAF | The immune mechanism | IL-6 and HGF are key EMT-stimulating cytokines secreted by H-CAF. | Jia et al. (2020) |
| CAF | The immune mechanism | The proportion of CAFs was positively correlated with the expression of CD73 in HCC cells. The c-Met and MEK-ERK1/2 pathways are activated by HGF from CAF, which upregulates CD73 expression in HCC cells. | Peng et al. (2020) |
| CAF | immunotherapy | Endothelial sialic acid protein expressed by CAF is the main regulator of macrophage recruitment and polarization, and inhibition of endothelial sialic acid protein inhibition is a potential therapeutic strategy for HCC. | Yang et al. (2020) |
| CAF | Prognostic marker | CAFs can produce plGFPLGF, which is associated with tumor angiogenesis markers and predicts poor prognosis in HCC patients. | Liu et al. (2020c) |
| CAF | immunotherapy | CAFs can promote the dryness and metastasis of HCC cells, and blocking autophagy can significantly reduce the enhanced dryness of CAFs, suggesting that targeting HCC autophagy may be an effective strategy for the treatment of HCC. | Zhao et al. (2019) |
| CAF | The immune mechanism | LXRα agonists limit TGFβ-dependent CAF differentiation and may limit the growth of primary HCC. | Morén et al. (2019) |
| CAF | immunotherapy | RVD1 inhibits the stem cell characterization of CAF-induced EMT and HCC cells by inhibiting the secretion of COMP. | Sun et al. (2019b) |
| CAF | The immune mechanism | Endogenous and exogenous BMP4 activates liver fibroblasts, acquires the ability to secrete cytokines, and enhances the aggressiveness of HCC cells. | Mano et al. (2019) |
| CAF | The immune mechanism | CAFs promote self-renewal, chemotherapy resistance, metastasis and tumorigenicity of CD24 HCC cells. CAFs secreted HGF and IL6 promote the dryness of CD24 HCC cells by phosphorylation of STAT3. | Li et al. (2019c) |
| CAF | The immune mechanism | HCC-CAFs regulate the survival, activation, and function of neutrophils in HCC through the IL6-STAT3-PDL1 signaling cascade. | Cheng et al. (2018) |
| CAF | The immune mechanism | IL-6 secreted by CAF promotes stem cell-like properties in HCC cells by enhancing STAT3/Notch signaling. | Xiong et al. (2018) |
| CAF | The immune mechanism | CAF-induced Notch3 expression is responsible for the activation of LSD1 in CSC, thereby promoting its self-renewal in HCC. | Liu et al. (2018b) |
| CAF | The immune mechanism | CAF-mediated tumor progression in HCC is associated with the deletion of anti-tumor miR-320a in CAF exosomes. | Zhang et al. (2017) |
| CAF | The immune mechanism | MiR-101 eliminated SDF1 signal transduction cells by inhibiting the expression of SDF1 in CAF and inhibiting the expression of VE-cadherin in tumors. | Yang et al. (2016) |
| CAF | The immune mechanism | CCL2, CCL5, CCL7 and CXCL16 secreted by CAF promote HCC metastasis through synergistic activation of HH and TGF-β pathways in HCC cells. | Liu et al. (2016) |
| CAF | immunotherapy | Targeting the CAF-derived, HGF-mediated c-Met/FRA1/Hey1 cascade may be a therapeutic strategy for the treatment of HCC. | Lau et al. (2016) |
| CAF | The immune mechanism | When stimulated, CAF shows the potential to differentiate into adipocytes, osteoblasts, and pancreatic cells. When co-cultured with human HCC cell lines, CAF upregulated the expression of TGFB1 and FAP genes in Huh-7 and JHH-6, thus having the ability to enter the circulation. | Sukowati et al. (2015) |
| CAF | The immune mechanism | The expression of CCN2, EMA and FAP may be involved in the activation of CAF in HCC, leading to aggressive behavior. The significant correlation between tumor cells expressing EMA and CAF expressing FAP and their terrain proximity suggests that there may be cross-talk between tumor epithelial cells and stromal cells in the HCC tumor microenvironment. | Kim et al. (2014) |
M2-Polarized Macrophages
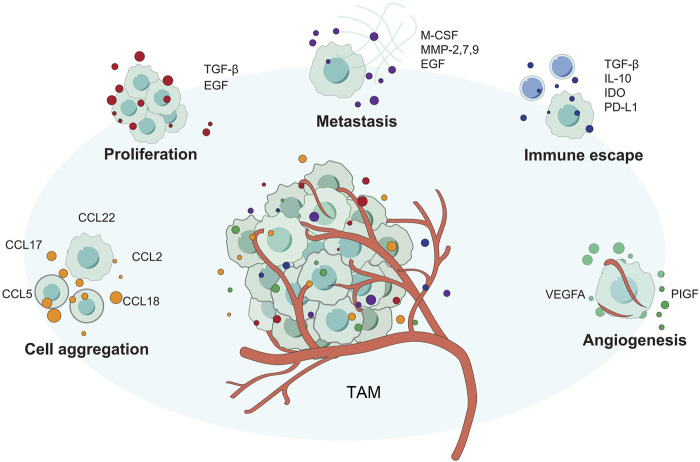
M2 polarized macrophages, as opposed to M1 polarized macrophages, have anti-inflammatory and pro-tumor actions (Figure 4). M2 macrophages are further differentiated into M2a, M2b, M2c, and M2d subsets. Th2 cytokines such as IL-13 and IL-4 can trigger macrophage transformation to the M2A phenotype, whereas TLR and immune complex activation induces M2B macrophages, the M2C subtype polarized by IL-10 (Hao et al., 2012; Sica and Mantovani, 2012). Despite the fact that there have been few research on M2-polarized macrophages in HCC, the function of them in the occurrence and development of HCC has been confirmed. According to several studies, arsenite raises miR-15b levels and causes M2 polarization in THP-1 cells. Increased miR-15b in Evs transfer from arsenite-treated THP-1 (AS-THP-1) cells to HCC cells via miR-15b. By targeting LATS1, it can reduce Hippo pathway activation while still accelerating the invasion and metastasis of growing HCC cells (Li et al., 2021). The potential therapeutic potential of M2 polarized macrophages has also been pointed out that Tumor cell-derived Wnt ligands induce M2-like polarization of TAM via traditional Wnt/-catenin signaling, resulting in tumor migration, development, immunosuppression and metastasis in HCC(Yang et al., 2018a). We summarize the current relevant research progress in Table 8.
FIGURE 4.
The different ways that TAM supports tumor growth. TAM promotes tumor proliferation, invasion, angiogenesis, and immune escape through various methods.
TABLE 8.
Tumor-promoting immune cells: M2-polarized macrophages.
| Cells | The research direction | Result | Reference |
|---|---|---|---|
| M2-polarized macrophages | The immune mechanism | MicroRNA (miR-17-92) clusters from the extracellular vesicles (EVs) of M2-polarized tumor-associated macrophages (M2-TAMs) stimulate the imbalance of the TGF-β1/BMP-7 pathway, TGF-β1/BMP-7 pathway imbalance significantly promotes HCC cell invasion and stem cells by increasing the expression of differentiation inhibitor 1(ID1). | Ning et al. (2021) |
| M2-polarized macrophages | The immune mechanism | Elevated levels of Mir-15B are transferred from arsenite-treated THP-1 (AS-THP-1) cells to HCC cells via Mir-15b in EVs, inhibit Hippo pathway activation by targeting LATS1, and participate in the migration and invasion of proliferation-promoting HCC cells. | Li et al. (2021) |
| M2-polarized macrophages | The immune mechanism | β2-AR promotes the occurrence and development of HCC by silencing GRK2 in M2 polarized macrophages. | Wu et al. (2019b) |
| M2-polarized macrophages | immunotherapy | Tumor cell-derived Wnt ligands stimulate M2-like polarization of TAM through classical Wnt/β-catenin signaling, which leads to tumor growth, migration, metastasis, and immunosuppression in HCC. | Yang et al. (2018a) |
| M2-polarized macrophages | immunotherapy | M2-polarized macrophages promote the migration and EMT of HCC cells through the TLR4/STAT3 signaling pathway, suggesting that TLR4 may be a new therapeutic target. | Yao et al. (2018) |
The Controversial Immune Cell Type in Cancer: B Cells
One type of immune cells that cannot be ignored in the HCC tumor microenvironment is B cells. According to the current relevant studies, it is not clear whether B cells are “good” or “bad”. Some studies have reported that B cells promote HCC, while others have reported the opposite effect. B cells, on the one hand, release cytokines that comport with CTL activity and serve as potent antigen-presenting cells (APCs). On the other hand, they may be tumorigenic due to the production of cytokines that attract MDSC and promote angiogenesis (de Visser et al., 2005; Tsou et al., 2016). Studies have shown that CCL20 derived from tumor cells interacts with CD19CD5 B cells overexpressed by CCR6 to promote the development of HCC, possibly through enhanced angiogenesis (He et al., 2017). Liu et al. 's study confirmed that Selective recruitment of CXCR3 (+) B cells Bridges the pro-inflammatory interleukin-17 response and the polarization of tumorigenic macrophages in the tumor environment, and blocking the migration or function of CXCR3+ B cells may help to overcome HCC (Liu et al., 2015). Therefore, B cells are involved in both the development and inhibition of HCC. Table 9 highlights the most recent reliable research on the involvement of B cells in HCC.
TABLE 9.
The controversial immune cell type in cancer: B cells.
| Cells | The research direction | Result | Reference |
|---|---|---|---|
| B cells | Prognostic marker | CD20 B cells, naive B cells, and CD27 isotypic transformed memory B cells are independent prognostic factors for survival in HCC. During the progression of HCC, intratumoral infiltration of B cells is significantly impaired. High density of tumor-infiltrating B cells means better clinical outcome. | Zhang et al. (2019) |
| B cells | The immune mechanism | In mice with HCC, B cell depletion blocked the production of these macrophages, increased anti-tumor T cell response, and reduced HCC growth. This pathway is involved in the increased expression of DNA methyltransferase 1 and EZH2 in HCC and HCC cells. | Wei et al. (2019) |
| B cells | Prognostic marker | Tumor derived exosome-activated B cells strongly express Tim-1 protein and have inhibitory activity against CD8 T cells. Exogenous HMGB1 activates B cells and promotes the expansion of Tim-1 Breg cells through Toll-like receptor (TLR) 2/4 and mitogen-activated protein kinase (MAPK) signaling pathways. Accumulation of TIM-1BREG cells in tumors is associated with advanced disease, early recurrence, and reduced survival in HCC patients. | Ye et al. (2018) |
| B cells | The immune mechanism | In MDR2 mice, CD20 B cell ablation promoted age-mediated fibrosis regression and inhibited the tumorigenic TNFα/NF-κB pathway. | Faggioli et al. (2018) |
| B cells | The immune mechanism | B cells and IgG2 may play an important role in the inhibition of liver tumorigenesis. Hepatocellular specific expression of ras oncogene may play a role in the inhibition of B cells, and B cells and T cells may be inhibited in developing liver tumors. | Wang et al. (2017) |
| B cells | The immune mechanism | CCL20 derived from tumor cells interacts with CD19CD5 B cells overexpressed by CCR6 to promote the development of HCC, possibly through enhanced angiogenesis. | He et al. (2017) |
| B cells | Prognostic marker | More than 50% of B cells in HCC exhibit FcγRII-activated phenotypes, and the production of FcγRII-activated B cells may represent a mechanism through which immune activation is associated with immune tolerance in the tumor environment. | Ouyang et al. (2016) |
| B cells | The immune mechanism | A novel oncogenic PD-1(HI) B cell subtype has been identified in human HCC that exhibits a phenotype distinct from that of surrounding regulatory B cells. TLR4-mediated upregulation of BCL6 is critical for inducing PD-1(HI) B cells, which act through an IL10-dependent pathway after interacting with PD-L1, thereby causing T cell dysfunction and promoting disease progression. | Xiao et al. (2016) |
| B cells | Prognostic marker | Tumor infiltrating T cells and B cells are in close contact with each other, and their density is associated with superior survival in patients with HCC. | Garnelo et al. (2017) |
| B cells | The immune mechanism | Selective recruitment of CXCR3 (+) B cells Bridges the pro-inflammatory interleukin-17 response and the polarization of tumorigenic macrophages in the tumor environment, and blocking the migration or function of CXCR3 (+) B cells may contribute to the defeat of HCC. | Liu et al. (2015) |
| B cells | The immune mechanism | After liver MET transfection, TUNEL (+) hepatocytes were increased in B cell-or macrophage-deficient mice, suggesting that these cells provide a protective effect against MET-induced hepatocyte apoptosis. | Subleski et al. (2015) |
| B cells | The immune mechanism | An increase in intrahepatic B cells at the edge of the tumor was positively associated with tumor invasion characteristics and more tumor recurrence. Bregs directly interact with HCC cells through the CD40/CD154 signaling pathway, thereby promoting the growth and aggressiveness of HCC. | Shao et al. (2014) |
| B cells | The immune mechanism | As a trans activator, HBx can regulate the activated B nuclear factor kappa-light chain enhancer (NF-κB) and transcription factor AP-2. HBx may cause the loss of apoptotic function, or directly contribute to carcinogenesis by realizing the transformation function, and accelerate the development of HCC. | Zhang et al. (2014) |
| B cells | The immune mechanism | Activation-induced cytidine deaminase (AID) acts as genomic mutants in activated B cells, and inappropriate expression of AID is associated with immunopathological phenotypes of human B cell malignancies. Abnormal activation of AID in hepatocytes leads to the accumulation of multiple genetic changes in the p53 gene, which may enhance genetic susceptibility to mutagenesis leading to HCC development. | Kou et al. (2007) |
Conclusions and Perspectives
With the development of single-cell sequencing and other technologies, we have the opportunity to further explore TME. Immunotherapy, a new tumor treatment method, also has a better and broader application prospect. However, at present, it is still too early for immunotherapy to replace traditional chemotherapeutic therapy, and there is still a long way to go in the process of clinical application. However, immunotherapy can be regarded as a good alternative therapy for patients with chemotherapy resistance. As mentioned in this paper, immunotherapies for tumor suppressor related immune cells, such as effect DCs, as well as tumor promoting immune cells, such as MDSC/Treg, are being developed one after another.
Compared with traditional chemotherapy, immunotherapy has many advantages. For example, immunotherapy has fewer overall side effects than chemotherapy and, once effective, may lead to long-term survival and even clinical cure. In addition, immunotherapy can be used as an important anti-tumor adjuvant therapy in addition to chemotherapy, radiotherapy and surgery. Appropriate immunotherapy can kill the tiny residual tumor cells after chemotherapy or some tumor cells resistant to chemotherapy. Immunotherapy should be considered for patients who are intolerant to chemotherapy or have extensive metastasis and cannot undergo surgery, radiotherapy or chemotherapy (Yang, 2015).
At present, the mainstream immunotherapy mainly includes CAR T therapy/immune checkpoint inhibitor therapy (PD-1, PD-L1, etc.)/tumor vaccine. CAR-T is the T cells, biological engineering, when the cancer has an immune deficiency, immune surveillance, give play to the role of the case, through the biological engineering to determine the targets of leukemia, it specifically chimeric in T cells, to attack the leukemia cells, the effect is significant, but easy to appear “storm” cells, serious and even cause death (Feins et al., 2019). Immune checkpoint inhibitor therapy has the advantage of long-term survival and relatively small adverse reactions. This therapy activates tumor-specific immune cells in the body by removing or attenuating the negative regulatory factors of immunoreactive cells, but it is not suitable for all patients. The higher the mutation load, the better the treatment response. Therefore, biomarkers should be used to screen the dominant population. The most common predictive indicators of PD-1/PD-L1 immune checkpoint inhibitors are microsatellite instability, PD-L1 and tumor mutation load (Pinato et al., 2019). The treatment of cancer vaccines is still incomplete.
Immunotherapy is not the end of tumor therapy; on the contrary, tumor immunotherapy represented by immune checkpoints has just opened a new chapter in tumor therapy. Combined with the basic and characteristics of immunotherapy, with the deepening of human understanding of tumors, tumors as a chronic disease that can be cured are no longer so far out of reach.
Acknowledgments
We would like to express our sincere thanks to Magdalens Klink, the author of the book “Interaction of immune and cancer cells.” Our pictures have been partially changed and repainted on the basis of this book. At the same time, this book has also given us a lot of writing inspiration.
Author Contributions
The manuscript had three first authors who made equal contributions to the project. XH, GS, and YZ were responsible for collecting information and design reviews of relevant studies. XK and DR are responsible for drawing the pictures. In addition, we have three corresponding authors in this manuscript. WT, JS, and XW contributed to the interpretation, editing and critical revision of the manuscript.
Funding
We are grateful for the grants from the National Natural Science Key Foundation of China (Grant No. 31930020) and National Natural Science Foundation of China (Grant No. 81771716).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, orclaim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- Ali M. Y., Grimm C. F., Ritter M., Mohr L., Allgaier H.-P., Weth R., et al. (2005). Activation of Dendritic Cells by Local Ablation of Hepatocellular Carcinoma. J. Hepatol. 43, 817–822. 10.1016/j.jhep.2005.04.016 [DOI] [PubMed] [Google Scholar]
- Anson M., Crain-Denoyelle A.-M., Baud V., Chereau F., Gougelet A., Terris B., et al. (2012). Oncogenic β-catenin Triggers an Inflammatory Response that Determines the Aggressiveness of Hepatocellular Carcinoma in Mice. J. Clin. Invest. 122, 586–599. 10.1172/jci43937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aras S., Zaidi M. R. (2017). TAMeless Traitors: Macrophages in Cancer Progression and Metastasis. Br. J. Cancer 117, 1583–1591. 10.1038/bjc.2017.356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arihara F., Mizukoshi E., Kitahara M., Takata Y., Arai K., Yamashita T., et al. (2013). Increase in CD14+HLA-DR−/low Myeloid-Derived Suppressor Cells in Hepatocellular Carcinoma Patients and its Impact on Prognosis. Cancer Immunol. Immunother. 62, 1421–1430. 10.1007/s00262-013-1447-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asafo-Agyei K. O., Samant H. (2021). HCC. Treasure Island(FL): StatPearls. [Google Scholar]
- Barajas M., Mazzolini G., Genove G., Bilbao R., Narvaiza I., Schmitz V., et al. (2001). Gene Therapy of Orthotopic Hepatocellular Carcinoma in Rats Using Adenovirus Coding for Interleukin 12. Hepatology 33, 52–61. 10.1053/jhep.2001.20796 [DOI] [PubMed] [Google Scholar]
- Bennett S. R. M., Carbone F. R., Karamalis F., Flavell R. A., Miller J. F. A. P., Heath W. R. (1998). Help for Cytotoxic-T-Cell Responses Is Mediated by CD40 Signalling. Nature 393, 478–480. 10.1038/30996 [DOI] [PubMed] [Google Scholar]
- Bennett S. R. M., Carbone F. R., Karamalis F., Miller J. F. A. P., Heath W. R. (1997). Induction of a CD8+ Cytotoxic T Lymphocyte Response by Cross-Priming Requires Cognate CD4+ T Cell Help. J. Exp. Med. 186, 65–70. 10.1084/jem.186.1.65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berod L., Puttur F., Huehn J., Sparwasser T. (2012). Tregs in Infection and Vaccinology: Heroes or Traitors? Microb. Biotechnol. 5, 260–269. 10.1111/j.1751-7915.2011.00299.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borst J., Ahrends T., Bąbała N., Melief C. J. M., Kastenmüller W. (2018). CD4+ T Cell Help in Cancer Immunology and Immunotherapy. Nat. Rev. Immunol. 18, 635–647. 10.1038/s41577-018-0044-0 [DOI] [PubMed] [Google Scholar]
- Bourgeois C., Rocha B., Tanchot C. (2002). A Role for CD40 Expression on CD8+ T Cells in the Generation of CD8+ T Cell Memory. Science 297, 2060–2063. 10.1126/science.1072615 [DOI] [PubMed] [Google Scholar]
- Brown Z. J., Fu Q., Ma C., Kruhlak M., Zhang H., Luo J., et al. (2018). Carnitine Palmitoyltransferase Gene Upregulation by Linoleic Acid Induces CD4+ T Cell Apoptosis Promoting HCC Development. Cell Death Dis 9, 620. 10.1038/s41419-018-0687-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cabrera R., Ararat M., Xu Y., Brusko T., Wasserfall C., Atkinson M. A., et al. (2013). Immune Modulation of Effector CD4+ and Regulatory T Cell Function by Sorafenib in Patients with Hepatocellular Carcinoma. Cancer Immunol. Immunother. 62, 737–746. 10.1007/s00262-012-1380-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai M.-Y., Xu Y.-F., Qiu S.-J., Ju M.-J., Gao Q., Li Y.-W., et al. (2009). Human Leukocyte Antigen-G Protein Expression Is an Unfavorable Prognostic Predictor of Hepatocellular Carcinoma Following Curative Resection. Clin. Cancer Res. 15, 4686–4693. 10.1158/1078-0432.ccr-09-0463 [DOI] [PubMed] [Google Scholar]
- Cao M., Huang W., Chen Y., Li G., Liu N., Wu Y., et al. (2021). Chronic Restraint Stress Promotes the Mobilization and Recruitment of Myeloid-Derived Suppressor Cells through Beta-Adrenergic-Activated CXCL5-CXCR2-Erk Signaling Cascades. Int. J. Cancer 1, 1. [DOI] [PubMed] [Google Scholar]
- Carr B. I., Metes D. M. (2012). Peripheral Blood Lymphocyte Depletion after Hepatic Arterial 90Yttrium Microsphere Therapy for Hepatocellular Carcinoma. Int. J. Radiat. Oncology*Biology*Physics 82, 1179–1184. 10.1016/j.ijrobp.2010.10.042 [DOI] [PubMed] [Google Scholar]
- Chang C.-C., Dinh T. K., Lee Y.-A., Wang F.-N., Sung Y.-C., Yu P.-L., et al. (2020). Nanoparticle Delivery of MnO2 and Antiangiogenic Therapy to Overcome Hypoxia-Driven Tumor Escape and Suppress Hepatocellular Carcinoma. ACS Appl. Mater. Inter. 12, 44407–44419. 10.1021/acsami.0c08473 [DOI] [PubMed] [Google Scholar]
- Chang C.-J., Yang Y.-H., Chiu C.-J., Lu L.-C., Liao C.-C., Liang C.-W., et al. (2018). Targeting Tumor-Infiltrating Ly6G+ Myeloid Cells Improves Sorafenib Efficacy in Mouse Orthotopic Hepatocellular Carcinoma. Int. J. Cancer 142, 1878–1889. 10.1002/ijc.31216 [DOI] [PubMed] [Google Scholar]
- Chaoul N., Mancarella S., Lupo L., Giannelli G., Dituri F. (2020). Impaired Anti-tumor T Cell Response in Hepatocellular Carcinoma. Cancers (Basel) 12, 1. 10.3390/cancers12030627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen K., Wu Z., Zhao H., Wang Y., Ge Y., Wang D., et al. (2020). XCL1/Glypican-3 Fusion Gene Immunization Generates Potent Antitumor Cellular Immunity and Enhances Anti-PD-1 Efficacy. Cancer Immunol. Res. 8, 81–93. 10.1158/2326-6066.cir-19-0210 [DOI] [PubMed] [Google Scholar]
- Chen L., Zhou S., Qin J., Hu H., Ma H., Liu B., et al. (2013). Combination of SLC Administration and Tregs Depletion Is an Attractive Strategy for Targeting Hepatocellular Carcinoma. Mol. Cancer 12, 153. 10.1186/1476-4598-12-153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen M.-L., Yan B.-S., Lu W.-C., Chen M.-H., Yu S.-L., Yang P.-C., et al. (2014). Sorafenib Relieves Cell-Intrinsic and Cell-Extrinsic Inhibitions of Effector T Cells in Tumor Microenvironment to Augment Antitumor Immunity. Int. J. Cancer 134, 319–331. 10.1002/ijc.28362 [DOI] [PubMed] [Google Scholar]
- Chen Y., Hao X., Sun R., Wei H., Tian Z. (2019). Natural Killer Cell-Derived Interferon‐Gamma Promotes Hepatocellular Carcinoma through the Epithelial Cell Adhesion Molecule-Epithelial‐to‐Mesenchymal Transition Axis in Hepatitis B Virus Transgenic Mice. Hepatology 69, 1735–1750. 10.1002/hep.30317 [DOI] [PubMed] [Google Scholar]
- Chen Y., Yang D., Li S., Gao Y., Jiang R., Deng L., et al. (2012). Development of a Listeria Monocytogenes-Based Vaccine against Hepatocellular Carcinoma. Oncogene 31, 2140–2152. 10.1038/onc.2011.395 [DOI] [PubMed] [Google Scholar]
- Cheng L., Du X., Wang Z., Ju J., Jia M., Huang Q., et al. (2014). Hyper-IL-15 Suppresses Metastatic and Autochthonous Liver Cancer by Promoting Tumour-specific CD8+ T Cell Responses. J. Hepatol. 61, 1297–1303. 10.1016/j.jhep.2014.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng L. E., Ohlen C., Nelson B. H., Greenberg P. D. (2002). Enhanced Signaling through the IL-2 Receptor in CD8+ T Cells Regulated by Antigen Recognition Results in Preferential Proliferation and Expansion of Responding CD8+ T Cells rather Than Promotion of Cell Death. Proc. Natl. Acad. Sci. 99, 3001–3006. 10.1073/pnas.052676899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng Y., Li H., Deng Y., Tai Y., Zeng K., Zhang Y., et al. (2018). Cancer-associated Fibroblasts Induce PDL1+ Neutrophils through the IL6-STAT3 Pathway that foster Immune Suppression in Hepatocellular Carcinoma. Cell Death Dis 9, 422. 10.1038/s41419-018-0458-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chew V., Tow C., Teo M., Wong H. L., Chan J., Gehring A., et al. (2010). Inflammatory Tumour Microenvironment Is Associated with superior Survival in Hepatocellular Carcinoma Patients. J. Hepatol. 52, 370–379. 10.1016/j.jhep.2009.07.013 [DOI] [PubMed] [Google Scholar]
- Chiu D. K.-C., Tse A. P.-W., Xu I. M.-J., Di Cui J., Lai R. K.-H., Li L. L., et al. (2017). Hypoxia Inducible Factor HIF-1 Promotes Myeloid-Derived Suppressor Cells Accumulation through ENTPD2/CD39L1 in Hepatocellular Carcinoma. Nat. Commun. 8, 517. 10.1038/s41467-017-00530-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiu D. K.-C., Yuen V. W.-H., Cheu J. W.-S., Wei L. L., Ting V., Fehlings M., et al. (2020). Hepatocellular Carcinoma Cells Up-Regulate PVRL1, Stabilizing PVR and Inhibiting the Cytotoxic T-Cell Response via TIGIT to Mediate Tumor Resistance to PD1 Inhibitors in Mice. Gastroenterology 159, 609–623. 10.1053/j.gastro.2020.03.074 [DOI] [PubMed] [Google Scholar]
- Cicinnati V. R., Zhang X., Yu Z., Ferencik S., Schmitz K. J., Dworacki G., et al. (2006). Increased Frequencies of CD8+ T Lymphocytes Recognizing Wild-type P53-Derived Epitopes in Peripheral Blood Correlate with Presence of Epitope Loss Tumor Variants in Patients with Hepatocellular Carcinoma. Int. J. Cancer 119, 2851–2860. 10.1002/ijc.22251 [DOI] [PubMed] [Google Scholar]
- de Visser K. E., Korets L. V., Coussens L. M. (2005). De Novo carcinogenesis Promoted by Chronic Inflammation Is B Lymphocyte Dependent. Cancer Cell 7, 411–423. 10.1016/j.ccr.2005.04.014 [DOI] [PubMed] [Google Scholar]
- Deng Y., Cheng J., Fu B., Liu W., Chen G., Zhang Q., et al. (2017). Hepatic Carcinoma-Associated Fibroblasts Enhance Immune Suppression by Facilitating the Generation of Myeloid-Derived Suppressor Cells. Oncogene 36, 1090–1101. 10.1038/onc.2016.273 [DOI] [PubMed] [Google Scholar]
- Dhanasekaran R., Park J., Yevtodiyenko A., Bellovin D. I., Adam S. J., Kd A. R., et al. (2020). MYC ASO Impedes Tumorigenesis and Elicits Oncogene Addiction in Autochthonous Transgenic Mouse Models of HCC and RCC. Mol. Ther. - Nucleic Acids 21, 850–859. 10.1016/j.omtn.2020.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duffy A. G., Ulahannan S. V., Makorova-Rusher O., Rahma O., Wedemeyer H., Pratt D., et al. (2017). Tremelimumab in Combination with Ablation in Patients with Advanced Hepatocellular Carcinoma. J. Hepatol. 66, 545–551. 10.1016/j.jhep.2016.10.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eggert T., Wolter K., Ji J., Ma C., Yevsa T., Klotz S., et al. (2016). Distinct Functions of Senescence-Associated Immune Responses in Liver Tumor Surveillance and Tumor Progression. Cancer Cell 30, 533–547. 10.1016/j.ccell.2016.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elinav E., Abd-Elnabi A., Pappo O., Bernstein I., Klein A., Engelhardt D., et al. (2006). Suppression of Hepatocellular Carcinoma Growth in Mice via Leptin, Is Associated with Inhibition of Tumor Cell Growth and Natural Killer Cell Activation. J. Hepatol. 44, 529–536. 10.1016/j.jhep.2005.08.013 [DOI] [PubMed] [Google Scholar]
- Evdokimova V. N., Liu Y., Potter D. M., Butterfield L. H. (2007). AFP-specific CD4+ Helper T-Cell Responses in Healthy Donors and HCC Patients. J. Immunother. 30, 425–437. 10.1097/cji.0b013e31802fd8e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faggioli F., Palagano E., Di Tommaso L., Donadon M., Marrella V., Recordati C., et al. (2018). B Lymphocytes Limit Senescence-Driven Fibrosis Resolution and Favor Hepatocarcinogenesis in Mouse Liver Injury. Hepatology 67, 1970–1985. 10.1002/hep.29636 [DOI] [PubMed] [Google Scholar]
- Fan Y., Gao Y., Rao J., Wang K., Zhang F., Zhang C. (2017). YAP-1 Promotes Tregs Differentiation in Hepatocellular Carcinoma by Enhancing TGFBR2 Transcription. Cell Physiol Biochem 41, 1189–1198. 10.1159/000464380 [DOI] [PubMed] [Google Scholar]
- Farhood B., Najafi M., Mortezaee K. (2019). CD8 + Cytotoxic T Lymphocytes in Cancer Immunotherapy: A Review. J. Cell Physiol 234, 8509–8521. 10.1002/jcp.27782 [DOI] [PubMed] [Google Scholar]
- Feins S., Kong W., Williams E. F., Milone M. C., Fraietta J. A. (2019). An Introduction to Chimeric Antigen Receptor (CAR) T‐cell Immunotherapy for Human Cancer. Am. J. Hematol. 94, S3–S9. 10.1002/ajh.25418 [DOI] [PubMed] [Google Scholar]
- Ferlay J., Soerjomataram I., Dikshit R., Eser S., Mathers C., Rebelo M., et al. (2015). Cancer Incidence and Mortality Worldwide: Sources, Methods and Major Patterns in GLOBOCAN 2012. Int. J. Cancer 136, E359–E386. 10.1002/ijc.29210 [DOI] [PubMed] [Google Scholar]
- Fu J., Xu D., Liu Z., Shi M., Zhao P., Fu B., et al. (2007). Increased Regulatory T Cells Correlate with CD8 T-Cell Impairment and Poor Survival in Hepatocellular Carcinoma Patients. Gastroenterology 132, 2328–2339. 10.1053/j.gastro.2007.03.102 [DOI] [PubMed] [Google Scholar]
- Gabrielson A., Wu Y., Wang H., Jiang J., Kallakury B., Gatalica Z., et al. (2016). Intratumoral CD3 and CD8 T-Cell Densities Associated with Relapse-free Survival in HCC. Cancer Immunol. Res. 4, 419–430. 10.1158/2326-6066.cir-15-0110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabrilovich D. I., Bronte V., Chen S.-H., Colombo M. P., Ochoa A., Ostrand-Rosenberg S., et al. (2007). The Terminology Issue for Myeloid-Derived Suppressor Cells. Cancer Res. 67, 425. 10.1158/0008-5472.can-06-3037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabrilovich D. I. (2017). Myeloid-Derived Suppressor Cells. Cancer Immunol. Res. 5, 3–8. 10.1158/2326-6066.cir-16-0297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabrilovich D. I., Ostrand-Rosenberg S., Bronte V. (2012). Coordinated Regulation of Myeloid Cells by Tumours. Nat. Rev. Immunol. 12, 253–268. 10.1038/nri3175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao Q., Qiu S.-J., Fan J., Zhou J., Wang X.-Y., Xiao Y.-S., et al. (2007). Intratumoral Balance of Regulatory and Cytotoxic T Cells Is Associated with Prognosis of Hepatocellular Carcinoma after Resection. Jco 25, 2586–2593. 10.1200/jco.2006.09.4565 [DOI] [PubMed] [Google Scholar]
- Garnelo M., Tan A., Her Z., Yeong J., Lim C. J., Chen J., et al. (2017). Interaction between Tumour-Infiltrating B Cells and T Cells Controls the Progression of Hepatocellular Carcinoma. Gut 66, 342–351. 10.1136/gutjnl-2015-310814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goyal L., Zheng H., Abrams T. A., Miksad R., Bullock A. J., Allen J. N., et al. (2019). A Phase II and Biomarker Study of Sorafenib Combined with Modified FOLFOX in Patients with Advanced Hepatocellular Carcinoma. Clin. Cancer Res. 25, 80–89. 10.1158/1078-0432.ccr-18-0847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guillerey C., Huntington N. D., Smyth M. J. (2016). Targeting Natural Killer Cells in Cancer Immunotherapy. Nat. Immunol. 17, 1025–1036. 10.1038/ni.3518 [DOI] [PubMed] [Google Scholar]
- Habif G., Crinier A., André P., Vivier E., Narni-Mancinelli E. (2019). Targeting Natural Killer Cells in Solid Tumors. Cell Mol Immunol 16, 415–422. 10.1038/s41423-019-0224-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hage C., Hoves S., Strauss L., Bissinger S., Prinz Y., Pöschinger T., et al. (2019). Sorafenib Induces Pyroptosis in Macrophages and Triggers Natural Killer Cell-Mediated Cytotoxicity against Hepatocellular Carcinoma. Hepatology 70, 1280–1297. 10.1002/hep.30666 [DOI] [PubMed] [Google Scholar]
- Han Q., Wang Y., Pang M., Zhang J. (2017). STAT3-blocked Whole-Cell Hepatoma Vaccine Induces Cellular and Humoral Immune Response against HCC. J. Exp. Clin. Cancer Res. 36, 156. 10.1186/s13046-017-0623-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanahan D., Weinberg R. A. (2011). Hallmarks of Cancer: the Next Generation. Cell 144, 646–674. 10.1016/j.cell.2011.02.013 [DOI] [PubMed] [Google Scholar]
- Hanahan D., Weinberg R. A. (2000). The Hallmarks of Cancer. Cell 100, 57–70. 10.1016/s0092-8674(00)81683-9 [DOI] [PubMed] [Google Scholar]
- Hao N. B., Lü M. H., Fan Y. H., Cao Y. L., Zhang Z. R., Yang S. M. (2012). Macrophages in Tumor Microenvironments and the Progression of Tumors. Clin. Dev. Immunol. 2012, 948098. 10.1155/2012/948098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- He H., Wu J., Zang M., Wang W., Chang X., Chen X., et al. (2017). CCR6+ B Lymphocytes Responding to Tumor Cell-Derived CCL20 Support Hepatocellular Carcinoma Progression via Enhancing Angiogenesis. Am. J. Cancer Res. 7, 1151–1163. [PMC free article] [PubMed] [Google Scholar]
- Hiroishi K., Eguchi J., Baba T., Shimazaki T., Ishii S., Hiraide A., et al. (2010). Strong CD8+ T-Cell Responses against Tumor-Associated Antigens Prolong the Recurrence-free Interval after Tumor Treatment in Patients with Hepatocellular Carcinoma. J. Gastroenterol. 45, 451–458. 10.1007/s00535-009-0155-2 [DOI] [PubMed] [Google Scholar]
- Hoechst B., Ormandy L. A., Ballmaier M., Lehner F., Krüger C., Manns M. P., et al. (2008). A New Population of Myeloid-Derived Suppressor Cells in Hepatocellular Carcinoma Patients Induces CD4+CD25+Foxp3+ T Cells. Gastroenterology 135, 234–243. 10.1053/j.gastro.2008.03.020 [DOI] [PubMed] [Google Scholar]
- Hoechst B., Voigtlaender T., Ormandy L., Gamrekelashvili J., Zhao F., Wedemeyer H., et al. (2009). Myeloid Derived Suppressor Cells Inhibit Natural Killer Cells in Patients with Hepatocellular Carcinoma via the NKp30 Receptor. Hepatology 50, 799–807. 10.1002/hep.23054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Homma S., Komita H., Sagawa Y., Ohno T., Toda G. (2005). Antitumour Activity Mediated by CD4+ Cytotoxic T Lymphocytes against MHC Class II-Negative Mouse Hepatocellular Carcinoma Induced by Dendritic Cell Vaccine and Interleukin-12. Immunology 115, 451–461. 10.1111/j.1365-2567.2005.02179.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu Z., Chen J., Zhou S., Yang N., Duan S., Zhang Z., et al. (2017). Mouse IP-10 Gene Delivered by Folate-Modified Chitosan Nanoparticles and Dendritic/tumor Cells Fusion Vaccine Effectively Inhibit the Growth of Hepatocellular Carcinoma in Mice. Theranostics 7, 1942–1952. 10.7150/thno.16236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang F., Chen J., Lan R., Wang Z., Chen R., Lin J., et al. (2018). δ-Catenin Peptide Vaccines Repress Hepatocellular Carcinoma Growth via CD8+ T Cell Activation. Oncoimmunology 7, e1450713. 10.1080/2162402x.2018.1450713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irie M., Homma S., Komita H., Zeniya M., Kufe D., Ohno T., et al. (2004). Inhibition of Spontaneous Development of Liver Tumors by Inoculation with Dendritic Cells Loaded with Hepatocellular Carcinoma Cells in C3H/HeNCRJ Mice. Int. J. Cancer 111, 238–245. 10.1002/ijc.20247 [DOI] [PubMed] [Google Scholar]
- Ishiyama K., Ohdan H., Ohira M., Mitsuta H., Arihiro K., Asahara T. (2006). Difference in Cytotoxicity against Hepatocellular Carcinoma between Liver and Periphery Natural Killer Cells in Humans. Hepatology 43, 362–372. 10.1002/hep.21035 [DOI] [PubMed] [Google Scholar]
- Iwai Y., Ishida M., Tanaka Y., Okazaki T., Honjo T., Minato N. (2002). Involvement of PD-L1 on Tumor Cells in the Escape from Host Immune System and Tumor Immunotherapy by PD-L1 Blockade. Proc. Natl. Acad. Sci. 99, 12293–12297. 10.1073/pnas.192461099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jia C., Wang G., Wang T., Fu B., Zhang Y., Huang L., et al. (2020). Cancer-associated Fibroblasts Induce Epithelial-Mesenchymal Transition via the Transglutaminase 2-dependent IL-6/IL6R/STAT3 axis in Hepatocellular Carcinoma. Int. J. Biol. Sci. 16, 2542–2558. 10.7150/ijbs.45446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang J., Ye F., Yang X., Zong C., Gao L., Yang Y., et al. (2017). Peri-tumor Associated Fibroblasts Promote Intrahepatic Metastasis of Hepatocellular Carcinoma by Recruiting Cancer Stem Cells. Cancer Lett. 404, 19–28. 10.1016/j.canlet.2017.07.006 [DOI] [PubMed] [Google Scholar]
- Jiang R., Tang J., Chen Y., Deng L., Ji J., Xie Y., et al. (2017). The Long Noncoding RNA Lnc-EGFR Stimulates T-Regulatory Cells Differentiation Thus Promoting Hepatocellular Carcinoma Immune Evasion. Nat. Commun. 8, 15129. 10.1038/ncomms15129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang W., Lu Z., He Y., Diasio R. B. (1997). Dihydropyrimidine Dehydrogenase Activity in Hepatocellular Carcinoma: Implication in 5-Fluorouracil-Based Chemotherapy. Clin. Cancer Res. 3, 395–399. [PubMed] [Google Scholar]
- Jinushi M., Takehara T., Tatsumi T., Hiramatsu N., Sakamori R., Yamaguchi S., et al. (2005). Impairment of Natural Killer Cell and Dendritic Cell Functions by the Soluble Form of MHC Class I-Related Chain A in Advanced Human Hepatocellular Carcinomas. J. Hepatol. 43, 1013–1020. 10.1016/j.jhep.2005.05.026 [DOI] [PubMed] [Google Scholar]
- Kakita N., Kanto T., Itose I., Kuroda S., Inoue M., Matsubara T., et al. (2012). Comparative Analyses of Regulatory T Cell Subsets in Patients with Hepatocellular Carcinoma: A Crucial Role of CD25−FOXP3−T Cells. Int. J. Cancer 131, 2573–2583. 10.1002/ijc.27535 [DOI] [PubMed] [Google Scholar]
- Kakumu S., Ito S., Ishikawa T., Mita Y., Tagaya T., Fukuzawa Y., et al. (2000). Decreased Function of Peripheral Blood Dendritic Cells in Patients with Hepatocellular Carcinoma with Hepatitis B and C Virus Infection. J. Gastroenterol. Hepatol. 15, 431–436. 10.1046/j.1440-1746.2000.02161.x [DOI] [PubMed] [Google Scholar]
- Kalathil S. G., Hutson A., Barbi J., Iyer R., Thanavala Y. (2019). Augmentation of IFN-Γ+ CD8+ T Cell Responses Correlates with Survival of HCC Patients on Sorafenib Therapy. JCI Insight 4. 10.1172/jci.insight.130116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalathil S. G., Lugade A. A., Miller A., Iyer R., Thanavala Y. (2016). PD-1+ and Foxp3+ T Cell Reduction Correlates with Survival of HCC Patients after Sorafenib Therapy. JCI Insight 1. 10.1172/jci.insight.86182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalathil S. G., Wang K., Hutson A., Iyer R., Thanavala Y. (2020). Tivozanib Mediated Inhibition of C-Kit/SCF Signaling on Tregs and MDSCs and Reversal of Tumor Induced Immune Suppression Correlates with Survival of HCC Patients. Oncoimmunology 9, 1824863. 10.1080/2162402x.2020.1824863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalluri R. (2016). The Biology and Function of Fibroblasts in Cancer. Nat. Rev. Cancer 16, 582–598. 10.1038/nrc.2016.73 [DOI] [PubMed] [Google Scholar]
- Kato A., Miyazaki M., Ambiru S., Yoshitomi H., Ito H., Nakagawa K., et al. (2001). Multidrug Resistance Gene (MDR-1) Expression as a Useful Prognostic Factor in Patients with Human Hepatocellular Carcinoma after Surgical Resection. J. Surg. Oncol. 78, 110–115. 10.1002/jso.1129 [DOI] [PubMed] [Google Scholar]
- Kim G. J., Rhee H., Yoo J. E., Ko J. E., Lee J. S., Kim H., et al. (2014). Increased Expression of CCN2, Epithelial Membrane Antigen, and Fibroblast Activation Protein in Hepatocellular Carcinoma with Fibrous Stroma Showing Aggressive Behavior. PLoS One 9, e105094. 10.1371/journal.pone.0105094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohga K., Takehara T., Tatsumi T., Ishida H., Miyagi T., Hosui A., et al. (2010). Sorafenib Inhibits the Shedding of Major Histocompatibility Complex Class I-Related Chain A on Hepatocellular Carcinoma Cells by Down-Regulating a Disintegrin and Metalloproteinase 9. Hepatology 51, 1264–1273. 10.1002/hep.23456 [DOI] [PubMed] [Google Scholar]
- Kohga K., Tatsumi T., Takehara T., Tsunematsu H., Shimizu S., Yamamoto M., et al. (2010). Expression of CD133 Confers Malignant Potential by Regulating Metalloproteinases in Human Hepatocellular Carcinoma. J. Hepatol. 52, 872–879. 10.1016/j.jhep.2009.12.030 [DOI] [PubMed] [Google Scholar]
- Kou T., Marusawa H., Kinoshita K., Endo Y., Okazaki I.-m., Ueda Y., et al. (2007). Expression of Activation-Induced Cytidine Deaminase in Human Hepatocytes during Hepatocarcinogenesis. Int. J. Cancer 120, 469–476. 10.1002/ijc.22292 [DOI] [PubMed] [Google Scholar]
- Langhans B., Nischalke H. D., Krämer B., Dold L., Lutz P., Mohr R., et al. (2019). Role of Regulatory T Cells and Checkpoint Inhibition in Hepatocellular Carcinoma. Cancer Immunol. Immunother. 68, 2055–2066. 10.1007/s00262-019-02427-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau E. Y. T., Lo J., Cheng B. Y. L., Ma M. K. F., Lee J. M. F., Ng J. K. Y., et al. (2016). Cancer-Associated Fibroblasts Regulate Tumor-Initiating Cell Plasticity in Hepatocellular Carcinoma through C-Met/FRA1/HEY1 Signaling. Cell Rep. 15, 1175–1189. 10.1016/j.celrep.2016.04.019 [DOI] [PubMed] [Google Scholar]
- Li B., He X., Pang X., Zhang H., Chen J., Chen W. (2004). Elicitation of Both CD4+ and CD8+ T-Cell-Mediated Specific Immune Responses to HCA587 Protein by Autologous Dendritic Cells. Scand. J. Immunol. 60, 506–513. 10.1111/j.0300-9475.2004.01503.x [DOI] [PubMed] [Google Scholar]
- Li C., Song B., Santos P. M., Butterfield L. H. (2019). Hepatocellular Cancer-Derived Alpha Fetoprotein Uptake Reduces CD1 Molecules on Monocyte-Derived Dendritic Cells. Cell Immunol. 335, 59–67. 10.1016/j.cellimm.2018.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li C. X., Ling C. C., Shao Y., Xu A., Li X. C., Ng K. T.-P., et al. (2016). CXCL10/CXCR3 Signaling Mobilized-Regulatory T Cells Promote Liver Tumor Recurrence after Transplantation. J. Hepatol. 65, 944–952. 10.1016/j.jhep.2016.05.032 [DOI] [PubMed] [Google Scholar]
- Li G., Liu D., Cooper T. K., Kimchi E. T., Qi X., Avella D. M., et al. (2017). Successful Chemoimmunotherapy against Hepatocellular Cancer in a Novel Murine Model. J. Hepatol. 66, 75–85. 10.1016/j.jhep.2016.07.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J., Xue J., Ling M., Sun J., Xiao T., Dai X., et al. (2021). MicroRNA-15b in Extracellular Vesicles from Arsenite-Treated Macrophages Promotes the Progression of Hepatocellular Carcinomas by Blocking the LATS1-Mediated Hippo Pathway. Cancer Lett. 497, 137–153. 10.1016/j.canlet.2020.10.023 [DOI] [PubMed] [Google Scholar]
- Li Y. M., Liu Z. Y., Wang J. C., Yu J. M., Li Z. C., Yang H. J., et al. (2019). Receptor‐Interacting Protein Kinase 3 Deficiency Recruits Myeloid‐Derived Suppressor Cells to Hepatocellular Carcinoma through the Chemokine (C‐X‐C Motif) Ligand 1-Chemokine (C‐X‐C Motif) Receptor 2 Axis. Hepatology 70, 1564–1581. 10.1002/hep.30676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Wang R., Xiong S., Wang X., Zhao Z., Bai S., et al. (2019). Cancer-associated Fibroblasts Promote the Stemness of CD24+ Liver Cells via Paracrine Signaling. J. Mol. Med. 97, 243–255. 10.1007/s00109-018-1731-9 [DOI] [PubMed] [Google Scholar]
- Liang C.-m., Ye S.-l., Zhong C.-p., Zheng N., Bian W., Sun R.-x., et al. (2007). More Than Chemotaxis: a New Anti-tumor DC Vaccine Modified by rAAV2-SLC. Mol. Immunol. 44, 3797–3804. 10.1016/j.molimm.2007.03.026 [DOI] [PubMed] [Google Scholar]
- Liao R., Sun J., Wu H., Yi Y., Wang J.-X., He H.-W., et al. (2013). High Expression of IL-17 and IL-17RE Associate with Poor Prognosis of Hepatocellular Carcinoma. J. Exp. Clin. Cancer Res. 32, 3. 10.1186/1756-9966-32-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim C. J., Lee Y. H., Pan L., Lai L., Chua C., Wasser M., et al. (2019). Multidimensional Analyses Reveal Distinct Immune Microenvironment in Hepatitis B Virus-Related Hepatocellular Carcinoma. Gut 68, 916–927. 10.1136/gutjnl-2018-316510 [DOI] [PubMed] [Google Scholar]
- Lin L., Chen S., Wang H., Gao B., Kallakury B., Bhuvaneshwar K., et al. (2021). SPTBN1 Inhibits Inflammatory Responses and Hepatocarcinogenesis via the Stabilization of SOCS1 and Downregulation of P65 in Hepatocellular Carcinoma. Theranostics 11, 4232–4250. 10.7150/thno.49819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin W., Chen Y. L., Jiang L., Chen J. K. (2011). Reduced Expression of Chemerin Is Associated with a Poor Prognosis and a Lowed Infiltration of Both Dendritic Cells and Natural Killer Cells in Human Hepatocellular Carcinoma. Clin. Lab. 57, 879–885. [PubMed] [Google Scholar]
- Lin Y., Yang X., Liu W., Li B., Yin W., Shi Y., et al. (2017). Chemerin Has a Protective Role in Hepatocellular Carcinoma by Inhibiting the Expression of IL-6 and GM-CSF and MDSC Accumulation. Oncogene 36, 3599–3608. 10.1038/onc.2016.516 [DOI] [PubMed] [Google Scholar]
- Liu B., Ye S., He P., Zheng N., Zhao Y., Sun R., et al. (2001). Study of the Cytotoxity against Human Hepatocellular Carcinoma Cells Induced by the MAGE-1 Gene Modified Dendritic Cells. Zhonghua Gan Zang Bing Za Zhi 9, 151–153. [PubMed] [Google Scholar]
- Liu C., Liu L., Chen X., Cheng J., Zhang H., Zhang C., et al. (2018). LSD1 Stimulates Cancer-Associated Fibroblasts to Drive Notch3-dependent Self-Renewal of Liver Cancer Stem-like Cells. Cancer Res. 78, 938–949. 10.1158/0008-5472.can-17-1236 [DOI] [PubMed] [Google Scholar]
- Liu D., Li G., Avella D. M., Kimchi E. T., Kaifi J. T., Rubinstein M. P., et al. (2017). Sunitinib Represses Regulatory T Cells to Overcome Immunotolerance in a Murine Model of Hepatocellular Cancer. Oncoimmunology 7, e1372079. 10.1080/2162402x.2017.1372079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu G., Sun J., Yang Z.-F., Zhou C., Zhou P.-Y., Guan R.-Y., et al. (2021). Cancer-associated Fibroblast-Derived CXCL11 Modulates Hepatocellular Carcinoma Cell Migration and Tumor Metastasis through the circUBAP2/miR-4756/IFIT1/3 axis. Cell Death Dis 12, 260. 10.1038/s41419-021-03545-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., Chen S., Wang W., Ning B.-F., Chen F., Shen W., et al. (2016). Cancer-associated Fibroblasts Promote Hepatocellular Carcinoma Metastasis through Chemokine-Activated Hedgehog and TGF-β Pathways. Cancer Lett. 379, 49–59. 10.1016/j.canlet.2016.05.022 [DOI] [PubMed] [Google Scholar]
- Liu M., Zhou J., Liu X., Feng Y., Yang W., Wu F., et al. (2020). Targeting Monocyte-Intrinsic Enhancer Reprogramming Improves Immunotherapy Efficacy in Hepatocellular Carcinoma. Gut 69, 365–379. 10.1136/gutjnl-2018-317257 [DOI] [PubMed] [Google Scholar]
- Liu R.-X., Wei Y., Zeng Q.-H., Chan K.-W., Xiao X., Zhao X.-Y., et al. (2015). Chemokine (C-X-C Motif) Receptor 3-positive B Cells Link Interleukin-17 Inflammation to Protumorigenic Macrophage Polarization in Human Hepatocellular Carcinoma. Hepatology 62, 1779–1790. 10.1002/hep.28020 [DOI] [PubMed] [Google Scholar]
- Liu Y.-T., Tseng T.-C., Soong R.-S., Peng C.-Y., Cheng Y.-H., Huang S.-F., et al. (2018). A Novel Spontaneous Hepatocellular Carcinoma Mouse Model for Studying T-Cell Exhaustion in the Tumor Microenvironment. J. Immunotherapy Cancer 6, 144. 10.1186/s40425-018-0462-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Z., Chen M., Zhao R., Huang Y., Liu F., Li B., et al. (2020). CAF-induced Placental Growth Factor Facilitates Neoangiogenesis in Hepatocellular Carcinoma. Acta Biochim. Biophys. Sin(shanghai). 52, 18–25. 10.1093/abbs/gmz134 [DOI] [PubMed] [Google Scholar]
- Liu Z., Wang J., Liu L., Yuan H., Bu Y., Feng J., et al. (2020). Chronic Ethanol Consumption and HBV Induce Abnormal Lipid Metabolism through HBx/SWELL1/arachidonic Acid Signaling and Activate Tregs in HBV-Tg Mice. Theranostics 10, 9249–9267. 10.7150/thno.46005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo Re O., Mazza T., Giallongo S., Sanna P., Rappa F., Vinh Luong T., et al. (2020). Loss of Histone macroH2A1 in Hepatocellular Carcinoma Cells Promotes Paracrine-Mediated Chemoresistance and CD4+CD25+FoxP3+ Regulatory T Cells Activation. Theranostics 10, 910–924. 10.7150/thno.35045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long J., Zhou B., Li H., Dai Q., Zhang B., Xing S., et al. (2013). Improvement of HBsAg Gene-Modified Dendritic Cell-Based Vaccine Efficacy by Optimizing Immunization Method or the Application of β-glucosylceramide. Immunological Invest. 42, 137–155. 10.3109/08820139.2012.744418 [DOI] [PubMed] [Google Scholar]
- Lv B., Zhu W., Feng C. (2020). Coptisine Blocks Secretion of Exosomal circCCT3 from Cancer-Associated Fibroblasts to Reprogram Glucose Metabolism in Hepatocellular Carcinoma. DNA Cell Biol 8, 1. 10.1089/dna.2020.6058 [DOI] [PubMed] [Google Scholar]
- Ma J., Zheng B., Goswami S., Meng L., Zhang D., Cao C., et al. (2019). PD1Hi CD8+ T Cells Correlate with Exhausted Signature and Poor Clinical Outcome in Hepatocellular Carcinoma. J. Immunotherapy Cancer 7, 331. 10.1186/s40425-019-0814-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma L., Luo L., Qiao H., Dong X., Pan S., Jiang H., et al. (2007). Complete Eradication of Hepatocellular Carcinomas by Combined Vasostatin Gene Therapy and B7H3-Mediated Immunotherapy. J. Hepatol. 46, 98–106. 10.1016/j.jhep.2006.07.031 [DOI] [PubMed] [Google Scholar]
- Mackey M. F., Gunn J. R., Ting P. P., Kikutani H., Dranoff G., Noelle R. J., et al. (1997). Protective Immunity Induced by Tumor Vaccines Requires Interaction between CD40 and its Ligand, CD154. Cancer Res. 57, 2569–2574. [PubMed] [Google Scholar]
- Mackey M. F., Barth R. J., Jr., Noelle R. J. (1998). The Role of CD40/CD154 Interactions in the Priming, Differentiation, and Effector Function of Helper and Cytotoxic T Cells. J. Leukoc. Biol. 63, 418–428. 10.1002/jlb.63.4.418 [DOI] [PubMed] [Google Scholar]
- Mano Y., Yoshio S., Shoji H., Tomonari S., Aoki Y., Aoyanagi N., et al. (2019). Bone Morphogenetic Protein 4 Provides Cancer-Supportive Phenotypes to Liver Fibroblasts in Patients with Hepatocellular Carcinoma. J. Gastroenterol. 54, 1007–1018. 10.1007/s00535-019-01579-5 [DOI] [PubMed] [Google Scholar]
- Mantovani S., Oliviero B., Lombardi A., Varchetta S., Mele D., Sangiovanni A., et al. (2019). Deficient Natural Killer Cell NKp30-Mediated Function and Altered NCR3 Splice Variants in Hepatocellular Carcinoma. Hepatology 69, 1165–1179. 10.1002/hep.30235 [DOI] [PubMed] [Google Scholar]
- Menne S., Tumas D. B., Liu K. H., Thampi L., AlDeghaither D., Baldwin B. H., et al. (2015). Sustained Efficacy and Seroconversion with the Toll-like Receptor 7 Agonist GS-9620 in the Woodchuck Model of Chronic Hepatitis B. J. Hepatol. 62, 1237–1245. 10.1016/j.jhep.2014.12.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mizukoshi E., Yamashita T., Arai K., Terashima T., Kitahara M., Nakagawa H., et al. (2016). Myeloid-derived Suppressor Cells Correlate with Patient Outcomes in Hepatic Arterial Infusion Chemotherapy for Hepatocellular Carcinoma. Cancer Immunol. Immunother. 65, 715–725. 10.1007/s00262-016-1837-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morén A., Bellomo C., Tsubakihara Y., Kardassis D., Mikulits W., Heldin C.-H., et al. (2019). LXRα Limits TGFβ-dependent Hepatocellular Carcinoma Associated Fibroblast Differentiation. Oncogenesis 8, 36. 10.1038/s41389-019-0140-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mossanen J. C., Kohlhepp M., Wehr A., Krenkel O., Liepelt A., Roeth A. A., et al. (2019). CXCR6 Inhibits Hepatocarcinogenesis by Promoting Natural Killer T- and CD4+ T-cell-dependent Control of Senescence. Gastroenterology 156, 1877–1889. 10.1053/j.gastro.2019.01.247 [DOI] [PubMed] [Google Scholar]
- Ning J., Ye Y., Bu D., Zhao G., Song T., Liu P., et al. (2021). Imbalance of TGF-Β1/bmp-7 Pathways Induced by M2-Polarized Macrophages Promotes Hepatocellular Carcinoma Aggressiveness. Mol. Ther. 29, 2067–2087. 10.1016/j.ymthe.2021.02.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Beirne J., Farzaneh F., Harrison P. M. (2010). Generation of Functional CD8+ T Cells by Human Dendritic Cells Expressing Glypican-3 Epitopes. J. Exp. Clin. Cancer Res. 29, 48. 10.1186/1756-9966-29-48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ormandy L. A., Farber A., Cantz T., Petrykowska S., Wedemeyer H., Horning M., et al. (2006). Direct Ex Vivo Analysis of Dendritic Cells in Patients with Hepatocellular Carcinoma. Wjg 12, 3275–3282. 10.3748/wjg.v12.i20.3275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouyang F.-Z., Wu R.-Q., Wei Y., Liu R.-X., Yang D., Xiao X., et al. (2016). Dendritic Cell-Elicited B-Cell Activation Fosters Immune Privilege via IL-10 Signals in Hepatocellular Carcinoma. Nat. Commun. 7, 13453. 10.1038/ncomms13453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pang P. H.-S., Chan K.-T., Tse L. Y.-W., Chan R. C.-F., Cheung Y.-K., Sin F. W.-Y., et al. (2007). Induction of Cytotoxic T Cell Response against HCA661 Positive Cancer Cells through Activation with Novel HLA-A∗0201 Restricted Epitopes. Cancer Lett. 256, 178–185. 10.1016/j.canlet.2007.06.002 [DOI] [PubMed] [Google Scholar]
- Papalexi E., Satija R. (2018). Single-cell RNA Sequencing to Explore Immune Cell Heterogeneity. Nat. Rev. Immunol. 18, 35–45. 10.1038/nri.2017.76 [DOI] [PubMed] [Google Scholar]
- Park H., Jung J. H., Jung M. K., Shin E.-C., Ro S. W., Park J. H., et al. (2020). Effects of Transarterial Chemoembolization on Regulatory T Cell and its Subpopulations in Patients with Hepatocellular Carcinoma. Hepatol. Int. 14, 249–258. 10.1007/s12072-020-10014-4 [DOI] [PubMed] [Google Scholar]
- Pedroza-Gonzalez A., Verhoef C., Ijzermans J. N. M., Peppelenbosch M. P., Kwekkeboom J., Verheij J., et al. (2013). Activated Tumor-Infiltrating CD4+ Regulatory T Cells Restrain Antitumor Immunity in Patients with Primary or Metastatic Liver Cancer. Hepatology 57, 183–194. 10.1002/hep.26013 [DOI] [PubMed] [Google Scholar]
- Peng B. G., He Q., Liang L. I., Xie B. H., Hua Y. P., Chen Z. B., et al. (2006). Induction of Cytotoxic T-Lymphocyte Responses Using Dendritic Cells Transfected with Hepatocellular Carcinoma mRNA. Br. J. Biomed. Sci. 63, 123–128. 10.1080/09674845.2006.11732731 [DOI] [PubMed] [Google Scholar]
- Peng H., Xue R., Ju Z., Qiu J., Wang J., Yan W., et al. (2020). Cancer-associated Fibroblasts Enhance the Chemoresistance of CD73+ Hepatocellular Carcinoma Cancer Cells via HGF-Met-Erk1/2 Pathway. Ann. Transl Med. 8, 856. 10.21037/atm-20-1038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinato D. J., Howlett S., Ottaviani D., Urus H., Patel A., Mineo T., et al. (2019). Association of Prior Antibiotic Treatment with Survival and Response to Immune Checkpoint Inhibitor Therapy in Patients with Cancer. JAMA Oncol. 5, 1774–1778. 10.1001/jamaoncol.2019.2785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pistore C., Giannoni E., Colangelo T., Rizzo F., Magnani E., Muccillo L., et al. (2017). DNA Methylation Variations Are Required for Epithelial-To-Mesenchymal Transition Induced by Cancer-Associated Fibroblasts in Prostate Cancer Cells. Oncogene 36, 5551–5566. 10.1038/onc.2017.159 [DOI] [PubMed] [Google Scholar]
- Qin W.-H., Yang Z.-S., Li M., Chen Y., Zhao X.-F., Qin Y.-Y., et al. (2020). High Serum Levels of Cholesterol Increase Antitumor Functions of Nature Killer Cells and Reduce Growth of Liver Tumors in Mice. Gastroenterology 158, 1713–1727. 10.1053/j.gastro.2020.01.028 [DOI] [PubMed] [Google Scholar]
- Qiu S.-J., Lu L., Qiao C., Wang L., Wang Z., Xiao X., et al. (2005). Induction of Tumor Immunity and Cytotoxic T Lymphocyte Responses Using Dendritic Cells Transduced by Adenoviral Vectors Encoding HBsAg: Comparison to Protein Immunization. J. Cancer Res. Clin. Oncol. 131, 429–438. 10.1007/s00432-004-0616-1 [DOI] [PubMed] [Google Scholar]
- Ren Z., Yue Y., Zhang Y., Dong J., Liu Y., Yang X., et al. (2021). Changes in the Peripheral Blood Treg Cell Proportion in Hepatocellular Carcinoma Patients after Transarterial Chemoembolization with Microparticles. Front. Immunol. 12, 624789. 10.3389/fimmu.2021.624789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritter M., Ali M. Y., Grimm C. F., Weth R., Mohr L., Bocher W. O., et al. (2004). Immunoregulation of Dendritic and T Cells by Alpha-Fetoprotein in Patients with Hepatocellular Carcinoma. J. Hepatol. 41, 999–1007. 10.1016/j.jhep.2004.08.013 [DOI] [PubMed] [Google Scholar]
- Rogler G., Hausmann M., Spöttl T., Vogl D., Aschenbrenner E., Andus T., et al. (1999). T-cell Co-stimulatory Molecules Are Upregulated on Intestinal Macrophages from Inflammatory Bowel Disease Mucosa. Eur. J. Gastroenterol. Hepatol. 11, 1105–1112. 10.1097/00042737-199910000-00006 [DOI] [PubMed] [Google Scholar]
- Rohr-Udilova N., Klinglmüller F., Schulte-Hermann R., Stift J., Herac M., Salzmann M., et al. (2018). Deviations of the Immune Cell Landscape between Healthy Liver and Hepatocellular Carcinoma. Sci. Rep. 8, 6220. 10.1038/s41598-018-24437-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roxburgh P., Evans T. R. J. (2008). Systemic Therapy of Hepatocellular Carcinoma: Are We Making Progress? Adv. Ther. 25, 1089–1104. 10.1007/s12325-008-0113-z [DOI] [PubMed] [Google Scholar]
- Sakaguchi S., Miyara M., Costantino C. M., Hafler D. A. (2010). FOXP3+ Regulatory T Cells in the Human Immune System. Nat. Rev. Immunol. 10, 490–500. 10.1038/nri2785 [DOI] [PubMed] [Google Scholar]
- Samstein R. M., Arvey A., Josefowicz S. Z., Peng X., Reynolds A., Sandstrom R., et al. (2012). Foxp3 Exploits a Pre-existent Enhancer Landscape for Regulatory T Cell Lineage Specification. Cell 151, 153–166. 10.1016/j.cell.2012.06.053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos P. M., Menk A. V., Shi J., Tsung A., Delgoffe G. M., Butterfield L. H. (2019). Tumor-Derived α-Fetoprotein Suppresses Fatty Acid Metabolism and Oxidative Phosphorylation in Dendritic Cells. Cancer Immunol. Res. 7, 1001–1012. 10.1158/2326-6066.cir-18-0513 [DOI] [PubMed] [Google Scholar]
- Sayem M. A., Tomita Y., Yuno A., Hirayama M., Irie A., Tsukamoto H., et al. (2016). Identification of Glypican-3-Derived Long Peptides Activating Both CD8+and CD4+T Cells; Prolonged Overall Survival in Cancer Patients with Th Cell Response. Oncoimmunology 5, e1062209. 10.1080/2162402x.2015.1062209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmitz V., Barajas M., Wang L., Peng D., Duarte M., Prieto J., et al. (2001). Adenovirus-mediated CD40 Ligand Gene Therapy in a Rat Model of Orthotopic Hepatocellular Carcinoma. Hepatology 34, 72–81. 10.1053/jhep.2001.25757 [DOI] [PubMed] [Google Scholar]
- Schoenberger S. P., Toes R. E. M., van der Voort E. I. H., Offringa R., Melief C. J. M. (1998). T-cell Help for Cytotoxic T Lymphocytes Is Mediated by CD40-Cd40l Interactions. Nature 393, 480–483. 10.1038/31002 [DOI] [PubMed] [Google Scholar]
- Sconocchia G., Eppenberger S., Spagnoli G. C., Tornillo L., Droeser R., Caratelli S., et al. (2014). NK Cells and T Cells Cooperate during the Clinical Course of Colorectal Cancer. Oncoimmunology 3, e952197. 10.4161/21624011.2014.952197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shao Y., Lo C. M., Ling C. C., Liu X. B., Ng K. T.-P., Chu A. C. Y., et al. (2014). Regulatory B Cells Accelerate Hepatocellular Carcinoma Progression via CD40/CD154 Signaling Pathway. Cancer Lett. 355, 264–272. 10.1016/j.canlet.2014.09.026 [DOI] [PubMed] [Google Scholar]
- Shen Y., Wei Y., Wang Z., Jing Y., He H., Yuan J., et al. (2015). TGF-β Regulates Hepatocellular Carcinoma Progression by Inducing Treg Cell Polarization. Cell Physiol Biochem 35, 1623–1632. 10.1159/000373976 [DOI] [PubMed] [Google Scholar]
- Shi F., Shi M., Zeng Z., Qi R.-Z., Liu Z.-W., Zhang J.-Y., et al. (2011). PD-1 and PD-L1 Upregulation Promotes CD8+ T-Cell Apoptosis and Postoperative Recurrence in Hepatocellular Carcinoma Patients. Int. J. Cancer 128, 887–896. 10.1002/ijc.25397 [DOI] [PubMed] [Google Scholar]
- Shimoda M., Tomimaru Y., Charpentier K. P., Safran H., Carlson R. I., Wands J. (2012). Tumor Progression-Related Transmembrane Protein Aspartate-β-Hydroxylase Is a Target for Immunotherapy of Hepatocellular Carcinoma. J. Hepatol. 56, 1129–1135. 10.1016/j.jhep.2011.12.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sica A., Mantovani A. (2012). Macrophage Plasticity and Polarization: In Vivo Veritas. J. Clin. Invest. 122, 787–795. 10.1172/jci59643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soini Y., Virkajarvi N., Raunio H., Paakko P. (1996). Expression of P-Glycoprotein in Hepatocellular Carcinoma: a Potential Marker of Prognosis. J. Clin. Pathol. 49, 470–473. 10.1136/jcp.49.6.470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song M., He J., Pan Q. Z., Yang J., Zhao J., Zhang Y. J., et al. (2021). Cancer‐Associated Fibroblast‐Mediated Cellular Crosstalk Supports Hepatocellular Carcinoma Progression. Hepatology 73, 1717–1735. 10.1002/hep.31792 [DOI] [PubMed] [Google Scholar]
- Spitzer M. H., Nolan G. P. (2016). Mass Cytometry: Single Cells, Many Features. Cell 165, 780–791. 10.1016/j.cell.2016.04.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sprinzl M. F., Reisinger F., Puschnik A., Ringelhan M., Ackermann K., Hartmann D., et al. (2013). Sorafenib Perpetuates Cellular Anticancer Effector Functions by Modulating the Crosstalk between Macrophages and Natural Killer Cells. Hepatology 57, 2358–2368. 10.1002/hep.26328 [DOI] [PubMed] [Google Scholar]
- Subleski J. J., Scarzello A. J., Alvord W. G., Jiang Q., Stauffer J. K., Kronfli A., et al. (2015). Serum-based Tracking of De Novo Initiated Liver Cancer Progression Reveals Early Immunoregulation and Response to Therapy. J. Hepatol. 63, 1181–1189. 10.1016/j.jhep.2015.06.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suk K.-T., Mederacke I., Gwak G.-Y., Cho S. W., Adeyemi A., Friedman R., et al. (2016). Opposite Roles of Cannabinoid Receptors 1 and 2 in Hepatocarcinogenesis. Gut 65, 1721–1732. 10.1136/gutjnl-2015-310212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sukowati C. H. C., Anfuso B., Crocé L. S., Tiribelli C. (2015). The Role of Multipotent Cancer Associated Fibroblasts in Hepatocarcinogenesis. BMC Cancer 15, 188. 10.1186/s12885-015-1196-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun H., Huang Q., Huang M., Wen H., Lin R., Zheng M., et al. (2019). Human CD96 Correlates to Natural Killer Cell Exhaustion and Predicts the Prognosis of Human Hepatocellular Carcinoma. Hepatology 70, 168–183. 10.1002/hep.30347 [DOI] [PubMed] [Google Scholar]
- Sun L., Wang Y., Wang L., Yao B., Chen T., Li Q., et al. (2019). Resolvin D1 Prevents Epithelial-Mesenchymal Transition and Reduces the Stemness Features of Hepatocellular Carcinoma by Inhibiting Paracrine of Cancer-Associated Fibroblast-Derived COMP. J. Exp. Clin. Cancer Res. 38, 170. 10.1186/s13046-019-1163-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takata Y., Nakamoto Y., Nakada A., Terashima T., Arihara F., Kitahara M., et al. (2011). Frequency of CD45RO+ Subset in CD4+CD25high Regulatory T Cells Associated with Progression of Hepatocellular Carcinoma. Cancer Lett. 307, 165–173. 10.1016/j.canlet.2011.03.029 [DOI] [PubMed] [Google Scholar]
- Tanaka H., Yoshizawa H., Yamaguchi Y., Ito K., Kagamu H., Suzuki E., et al. (1999). Successful Adoptive Immunotherapy of Murine Poorly Immunogenic Tumor with Specific Effector Cells Generated from Gene-Modified Tumor-Primed Lymph Node Cells. J. Immunol. 162, 3574–3582. [PubMed] [Google Scholar]
- Tao H., Liu M., Wang Y., Luo S., Xu Y., Ye B., et al. (2021). Icaritin Induces Anti-tumor Immune Responses in Hepatocellular Carcinoma by Inhibiting Splenic Myeloid-Derived Suppressor Cell Generation. Front. Immunol. 12, 609295. 10.3389/fimmu.2021.609295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tao Z., Ruan H., Sun L., Kuang D., Song Y., Wang Q., et al. (2019). Targeting the YB-1/pd-L1 Axis to Enhance Chemotherapy and Antitumor Immunity. Cancer Immunol. Res. 7, 1135–1147. 10.1158/2326-6066.cir-18-0648 [DOI] [PubMed] [Google Scholar]
- Teng C. F., Wang T., Wu T. H., Lin J. H., Shih F. Y., Shyu W. C., et al. (2020). Combination Therapy with Dendritic Cell Vaccine and Programmed Death Ligand 1 Immune Checkpoint Inhibitor for Hepatocellular Carcinoma in an Orthotopic Mouse Model. Ther. Adv. Med. Oncol. 12, 1758835920922034. 10.1177/1758835920922034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tipton K. N., Sullivan N., Bruening W., Inamdar R., Launders J., Uhl S., et al. (2011). Stereotactic Body Radiation Therapy. Rockville(MD): Mayo Foundation for Medical Education and Research. [PubMed] [Google Scholar]
- Tseng H.-c., Xiong W., Badeti S., Yang Y., Ma M., Liu T., et al. (2020). Efficacy of Anti-cd147 Chimeric Antigen Receptors Targeting Hepatocellular Carcinoma. Nat. Commun. 11, 4810. 10.1038/s41467-020-18444-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsou P., Katayama H., Ostrin E. J., Hanash S. M. (2016). The Emerging Role of B Cells in Tumor Immunity. Cancer Res. 76, 5597–5601. 10.1158/0008-5472.can-16-0431 [DOI] [PubMed] [Google Scholar]
- Veglia F., Perego M., Gabrilovich D. (2018). Myeloid-derived Suppressor Cells Coming of Age. Nat. Immunol. 19, 108–119. 10.1038/s41590-017-0022-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogt A., Sievers E., Lukacs-Kornek V., Decker G., Raskopf E., Meumann N., et al. (2014). Improving Immunotherapy of Hepatocellular Carcinoma (HCC) Using Dendritic Cells (DC) Engineered to Express IL-12 In Vivo . Liver Int. 34, 447–461. 10.1111/liv.12284 [DOI] [PubMed] [Google Scholar]
- Voskoboinik I., Smyth M. J., Trapani J. A. (2006). Perforin-mediated Target-Cell Death and Immune Homeostasis. Nat. Rev. Immunol. 6, 940–952. 10.1038/nri1983 [DOI] [PubMed] [Google Scholar]
- Wang C., Shang C., Gai X., Song T., Han S., Liu Q., et al. (2021). Sulfatase 2-Induced Cancer-Associated Fibroblasts Promote Hepatocellular Carcinoma Progression via Inhibition of Apoptosis and Induction of Epithelial-To-Mesenchymal Transition. Front. Cell Dev. Biol. 9, 631931. 10.3389/fcell.2021.631931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang D., Li X., Li J., Lu Y., Zhao S., Tang X., et al. (2019). APOBEC3B Interaction with PRC2 Modulates Microenvironment to Promote HCC Progression. Gut 68, 1846–1857. 10.1136/gutjnl-2018-317601 [DOI] [PubMed] [Google Scholar]
- Wang F., Jing X., Li G., Wang T., Yang B., Zhu Z., et al. (2012). Foxp3+ Regulatory T Cells Are Associated with the Natural History of Chronic Hepatitis B and Poor Prognosis of Hepatocellular Carcinoma. Liver Int. 32, 644–655. 10.1111/j.1478-3231.2011.02675.x [DOI] [PubMed] [Google Scholar]
- Wang H., Wang X., Li X., Fan Y., Li G., Guo C., et al. (2014). CD68+HLA-DR+ M1-like Macrophages Promote Motility of HCC Cells via NF-Κb/FAK Pathway. Cancer Lett. 345, 91–99. 10.1016/j.canlet.2013.11.013 [DOI] [PubMed] [Google Scholar]
- Wang J., Sanmamed M. F., Datar I., Su T. T., Ji L., Sun J., et al. (2019). Fibrinogen-like Protein 1 Is a Major Immune Inhibitory Ligand of LAG-3. Cell 176, 334–347. 10.1016/j.cell.2018.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang K., Nie X., Rong Z., Fan T., Li J., Wang X., et al. (2017). B Lymphocytes Repress Hepatic Tumorigenesis but Not Development in Hras12V Transgenic Mice. Int. J. Cancer 141, 1201–1214. 10.1002/ijc.30823 [DOI] [PubMed] [Google Scholar]
- Wang N., Tan H.-Y., Lu Y., Chan Y.-T., Wang D., Guo W., et al. (2021). PIWIL1 Governs the Crosstalk of Cancer Cell Metabolism and Immunosuppressive Microenvironment in Hepatocellular Carcinoma. Sig Transduct Target. Ther. 6, 86. 10.1038/s41392-021-00485-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y. H., Chuang Y. H., Wu C. F., Jan M. C., Wu W. J., Lin C. L., et al. (2019). Smoking and Hepatitis B Virus-Related Hepatocellular Carcinoma Risk: The Mediating Roles of Viral Load and Alanine Aminotransferase. Hepatology 69, 1412–1425. 10.1002/hep.30339 [DOI] [PubMed] [Google Scholar]
- Wang Y., Liu T., Tang W., Deng B., Chen Y., Zhu J., et al. (2016). Hepatocellular Carcinoma Cells Induce Regulatory T Cells and Lead to Poor Prognosis via Production of Transforming Growth Factor-Β1. Cell Physiol Biochem 38, 306–318. 10.1159/000438631 [DOI] [PubMed] [Google Scholar]
- Wei Y., Lao X.-M., Xiao X., Wang X.-Y., Wu Z.-J., Zeng Q.-H., et al. (2019). Plasma Cell Polarization to the Immunoglobulin G Phenotype in Hepatocellular Carcinomas Involves Epigenetic Alterations and Promotes Hepatoma Progression in Mice. Gastroenterology 156, 1890–1904. e16. 10.1053/j.gastro.2019.01.250 [DOI] [PubMed] [Google Scholar]
- Williams M., Liu X., Zhang Y., Reske J., Bahal D., Gohl T. G., et al. (2020). NCOA5 Deficiency Promotes a Unique Liver Protumorigenic Microenvironment through p21WAF1/CIP1 Overexpression, Which Is Reversed by Metformin. Oncogene 39, 3821–3836. 10.1038/s41388-020-1256-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf M. J., Adili A., Piotrowitz K., Abdullah Z., Boege Y., Stemmer K., et al. (2014). Metabolic Activation of Intrahepatic CD8+ T Cells and NKT Cells Causes Nonalcoholic Steatohepatitis and Liver Cancer via Cross-Talk with Hepatocytes. Cancer Cell 26, 549–564. 10.1016/j.ccell.2014.09.003 [DOI] [PubMed] [Google Scholar]
- Wong Y. Q., Qiu S. J., Tang Z. Y., Ye S. L., Liu Y. K., Fan J., et al. (2005). Changes in the Immune Function of Dendritic Cells (DC) Derived from HBV-Related Hepatocellular Carcinoma (HCC) Patient's Peripheral Blood Monocytes (PBMC) Pulsed with Tumor Antigen. Zhonghua Gan Zang Bing Za Zhi 13, 339–342. [PubMed] [Google Scholar]
- Wu C.-J., Tsai Y.-T., Lee I.-J., Wu P.-Y., Lu L.-S., Tsao W.-S., et al. (2018). Combination of Radiation and Interleukin 12 Eradicates Large Orthotopic Hepatocellular Carcinoma through Immunomodulation of Tumor Microenvironment. Oncoimmunology 7, e1477459. 10.1080/2162402x.2018.1477459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu J.-J., Yang Y., Peng W.-T., Sun J.-C., Sun W.-Y., Wei W. (2019). G Protein-Coupled Receptor Kinase 2 Regulating β2-adrenergic Receptor Signaling in M2-Polarized Macrophages Contributes to Hepatocellular Carcinoma Progression. Ott 12, 5499–5513. 10.2147/ott.s209291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Q., Zhou W., Yin S., Zhou Y., Chen T., Qian J., et al. (2019). Blocking Triggering Receptor Expressed on Myeloid Cells‐1‐Positive Tumor‐Associated Macrophages Induced by Hypoxia Reverses Immunosuppression and Anti‐Programmed Cell Death Ligand 1 Resistance in Liver Cancer. Hepatology 70, 198–214. 10.1002/hep.30593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y., Kuang D.-M., Pan W.-D., Wan Y.-L., Lao X.-M., Wang D., et al. (2013). Monocyte/macrophage-elicited Natural Killer Cell Dysfunction in Hepatocellular Carcinoma Is Mediated by CD48/2B4 Interactions. Hepatology 57, 1107–1116. 10.1002/hep.26192 [DOI] [PubMed] [Google Scholar]
- Xiao X., Lao X.-M., Chen M.-M., Liu R.-X., Wei Y., Ouyang F.-Z., et al. (2016). PD-1hi Identifies a Novel Regulatory B-Cell Population in Human Hepatoma that Promotes Disease Progression. Cancer Discov. 6, 546–559. 10.1158/2159-8290.cd-15-1408 [DOI] [PubMed] [Google Scholar]
- Xie Q.-K., Zhao Y.-J., Pan T., Lyu N., Mu L.-W., Li S.-L., et al. (2016). Programmed Death Ligand 1 as an Indicator of Pre-existing Adaptive Immune Responses in Human Hepatocellular Carcinoma. Oncoimmunology 5, e1181252. 10.1080/2162402x.2016.1181252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xing W., Wu S., Yuan X., Chen Q., Shen X., He F., et al. (2009). The Anti-tumor Effect of Human Monocyte-Derived Dendritic Cells Loaded with HSV-TK/GCV Induced Dying Cells. Cell Immunol. 254, 135–141. 10.1016/j.cellimm.2008.08.004 [DOI] [PubMed] [Google Scholar]
- Xiong S., Wang R., Chen Q., Luo J., Wang J., Zhao Z., et al. (2018). Cancer-associated Fibroblasts Promote Stem Cell-like Properties of Hepatocellular Carcinoma Cells through IL-6/STAT3/Notch Signaling. Am. J. Cancer Res. 8, 302–316. [PMC free article] [PubMed] [Google Scholar]
- Xu Y., Fang F., Jiao H., Zheng X., Huang L., Yi X., et al. (2019). Activated Hepatic Stellate Cells Regulate MDSC Migration through the SDF-1/CXCR4 axis in an Orthotopic Mouse Model of Hepatocellular Carcinoma. Cancer Immunol. Immunother. 68, 1959–1969. 10.1007/s00262-019-02414-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamamoto T., Nagano H., Sakon M., Wada H., Eguchi H., Kondo M., et al. (2004). Partial Contribution of Tumor Necrosis Factor-Related Apoptosis-Inducing Ligand (TRAIL)/TRAIL Receptor Pathway to Antitumor Effects of Interferon-Α/5-Fluorouracil against Hepatocellular Carcinoma. Clin. Cancer Res. 10, 7884–7895. 10.1158/1078-0432.ccr-04-0794 [DOI] [PubMed] [Google Scholar]
- Yamanaka T., Harimoto N., Yokobori T., Muranushi R., Hoshino K., Hagiwara K., et al. (2021). Conophylline Inhibits HCC by Inhibiting Activated Cancer-Associated Fibroblasts through Suppression of G Protein-Coupled Receptor 68. Mol. Cancer Ther. 20, 1019–1028. 10.1158/1535-7163 [DOI] [PubMed] [Google Scholar]
- Yang D., Li T., Li Y., Zhang S., Li W., Liang H., et al. (2019). H2S Suppresses Indoleamine 2, 3-dioxygenase 1 and Exhibits Immunotherapeutic Efficacy in Murine Hepatocellular Carcinoma. J. Exp. Clin. Cancer Res. 38, 88. 10.1186/s13046-019-1083-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang F., Wei Y., Han D., Li Y., Shi S., Jiao D., et al. (2020). Interaction with CD68 and Regulation of GAS6 Expression by Endosialin in Fibroblasts Drives Recruitment and Polarization of Macrophages in Hepatocellular Carcinoma. Cancer Res. 80, 3892–3905. 10.1158/0008-5472.CAN-19-2691 [DOI] [PubMed] [Google Scholar]
- Yang J., Lu Y., Lin Y.-Y., Zheng Z.-Y., Fang J.-H., He S., et al. (2016). Vascular Mimicry Formation Is Promoted by Paracrine TGF-β and SDF1 of Cancer-Associated Fibroblasts and Inhibited by miR-101 in Hepatocellular Carcinoma. Cancer Lett. 383, 18–27. 10.1016/j.canlet.2016.09.012 [DOI] [PubMed] [Google Scholar]
- Yang L., Shao X., Jia S., Zhang Q., Jin Z. (2019). Interleukin-35 Dampens CD8+ T Cells Activity in Patients with Non-viral Hepatitis-Related Hepatocellular Carcinoma. Front. Immunol. 10, 1032. 10.3389/fimmu.2019.01032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang M., Zhang Z., Chen J., Xu M., Huang J., Wang M., et al. (2019). Soluble Fibrinogen-like Protein 2 Promotes the Growth of Hepatocellular Carcinoma via Attenuating Dendritic Cell-Mediated Cytotoxic T Cell Activity. J. Exp. Clin. Cancer Res. 38, 351. 10.1186/s13046-019-1326-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang T., Zhang W., Wang L., Xiao C., Wang L., Gong Y., et al. (2018). Co-culture of Dendritic Cells and Cytokine-Induced Killer Cells Effectively Suppresses Liver Cancer Stem Cell Growth by Inhibiting Pathways in the Immune System. BMC Cancer 18, 984. 10.1186/s12885-018-4871-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang X. H., Yamagiwa S., Ichida T., Matsuda Y., Sugahara S., Watanabe H., et al. (2006). Increase of CD4+CD25+ Regulatory T-Cells in the Liver of Patients with Hepatocellular Carcinoma. J. Hepatol. 45, 254–262. 10.1016/j.jhep.2006.01.036 [DOI] [PubMed] [Google Scholar]
- Yang Y. (2015). Cancer Immunotherapy: Harnessing the Immune System to Battle Cancer. J. Clin. Invest. 125, 3335–3337. 10.1172/jci83871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y., Ye Y.-C., Chen Y., Zhao J.-L., Gao C.-C., Han H., et al. (2018). Crosstalk between Hepatic Tumor Cells and Macrophages via Wnt/β-Catenin Signaling Promotes M2-like Macrophage Polarization and Reinforces Tumor Malignant Behaviors. Cell Death Dis 9, 793. 10.1038/s41419-018-0818-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao R.-R., Li J.-H., Zhang R., Chen R.-X., Wang Y.-H. (2018). M2-polarized Tumor-Associated Macrophages Facilitated Migration and Epithelial-Mesenchymal Transition of HCC Cells via the TLR4/STAT3 Signaling Pathway. World J. Surg. Onc 16, 9. 10.1186/s12957-018-1312-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye L., Zhang Q., Cheng Y., Chen X., Wang G., Shi M., et al. (2018). Tumor-derived Exosomal HMGB1 Fosters Hepatocellular Carcinoma Immune Evasion by Promoting TIM-1+ Regulatory B Cell Expansion. J. Immunotherapy Cancer 6, 145. 10.1186/s40425-018-0451-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yost K. E., Satpathy A. T., Wells D. K., Qi Y., Wang C., Kageyama R., et al. (2019). Clonal Replacement of Tumor-specific T Cells Following PD-1 Blockade. Nat. Med. 25, 1251–1259. 10.1038/s41591-019-0522-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu S. J., Ma C., Heinrich B., Brown Z. J., Sandhu M., Zhang Q., et al. (2019). Targeting the Crosstalk between Cytokine-Induced Killer Cells and Myeloid-Derived Suppressor Cells in Hepatocellular Carcinoma. J. Hepatol. 70, 449–457. 10.1016/j.jhep.2018.10.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu Z., Zhao H., Feng X., Li H., Qiu C., Yi X., et al. (2019). Long Non-coding RNA FENDRR Acts as a miR-423-5p Sponge to Suppress the Treg-Mediated Immune Escape of Hepatocellular Carcinoma Cells. Mol. Ther. - Nucleic Acids 17, 516–529. 10.1016/j.omtn.2019.05.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yugawa K., Yoshizumi T., Mano Y., Itoh S., Harada N., Ikegami T., et al. (2021). Cancer-associated Fibroblasts Promote Hepatocellular Carcinoma Progression through Downregulation of Exosomal miR-150-3p. Eur. J. Surg. Oncol. 47, 384–393. 10.1016/j.ejso.2020.08.002 [DOI] [PubMed] [Google Scholar]
- Zhang D. Y., Friedman S. L. (2012). Fibrosis-dependent Mechanisms of Hepatocarcinogenesis. Hepatology 56, 769–775. 10.1002/hep.25670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang H.-G., Chen H.-S., Peng J.-R., Shang X.-Y., Zhang J., Xing Q., et al. (2007). Specific CD8+ T Cell Responses to HLA-A2 Restricted MAGE-A3 P271-279 Peptide in Hepatocellular Carcinoma Patients without Vaccination. Cancer Immunol. Immunother. 56, 1945–1954. 10.1007/s00262-007-0338-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Q., Huang H., Zheng F., Liu H., Qiu F., Chen Y., et al. (2020). Resveratrol Exerts Antitumor Effects by Downregulating CD8+CD122+ Tregs in Murine Hepatocellular Carcinoma. Oncoimmunology 9, 1829346. 10.1080/2162402x.2020.1829346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X. D., Wang Y., Ye L. H. (2014). Hepatitis B Virus X Protein Accelerates the Development of Hepatoma. Cancer Biol. Med. 11, 182–190. 10.7497/j.issn.2095-3941.2014.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z., Li X., Sun W., Yue S., Yang J., Li J., et al. (2017). Loss of Exosomal miR-320a from Cancer-Associated Fibroblasts Contributes to HCC Proliferation and Metastasis. Cancer Lett. 397, 33–42. 10.1016/j.canlet.2017.03.004 [DOI] [PubMed] [Google Scholar]
- Zhang Z., Ma L., Goswami S., Ma J., Zheng B., Duan M., et al. (2019). Landscape of Infiltrating B Cells and Their Clinical Significance in Human Hepatocellular Carcinoma. Oncoimmunology 8, e1571388. 10.1080/2162402x.2019.1571388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao J., Chu F., Xu H., Guo M., Shan S., Zheng W., et al. (2020). C/EBPα/miR-7 Controls CD4+ T Cell Activation and Function and Orchestrates Experimental Autoimmune Hepatitis in Mice. Hepatology 1, 1. 10.1002/hep.31607 [DOI] [PubMed] [Google Scholar]
- Zhao Q., Huang Z.-L., He M., Gao Z., Kuang D.-M. (2016). BTLA Identifies Dysfunctional PD-1-Expressing CD4+ T Cells in Human Hepatocellular Carcinoma. Oncoimmunology 5, e1254855. 10.1080/2162402x.2016.1254855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao T., Jia H., Cheng Q., Xiao Y., Li M., Ren W., et al. (2017). Nifuroxazide Prompts Antitumor Immune Response of TCL-Loaded DC in Mice with Orthotopically-Implanted Hepatocarcinoma. Oncol. Rep. 37, 3405–3414. 10.3892/or.2017.5629 [DOI] [PubMed] [Google Scholar]
- Zhao X.-L., Lin Y., Jiang J., Tang Z., Yang S., Lu L., et al. (2017). High-mobility Group Box 1 Released by Autophagic Cancer-Associated Fibroblasts Maintains the Stemness of Luminal Breast Cancer Cells. J. Pathol. 243, 376–389. 10.1002/path.4958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Z., Bai S., Wang R., Xiong S., Li Y., Wang X., et al. (2019). Cancer-associated Fibroblasts Endow Stem-like Qualities to Liver Cancer Cells by Modulating Autophagy. Cmar 11, 5737–5744. 10.2147/cmar.s197634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng B. H., Ma J. Q., Tian L. Y., Dong L. Q., Song G. H., Pan J. M., et al. (2020). The Distribution of Immune Cells within Combined Hepatocellular Carcinoma and Cholangiocarcinoma Predicts Clinical Outcome. Clin. Translational Med. 10, 45–56. 10.1002/ctm2.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng B., Wang D., Qiu X., Luo G., Wu T., Yang S., et al. (2020). Trajectory and Functional Analysis of PD‐1 High CD4 + CD8 + T Cells in Hepatocellular Carcinoma by Single‐Cell Cytometry and Transcriptome Sequencing. Adv. Sci. 7, 2000224. 10.1002/advs.202000224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng C., Zheng L., Yoo J.-K., Guo H., Zhang Y., Guo X., et al. (2017). Landscape of Infiltrating T Cells in Liver Cancer Revealed by Single-Cell Sequencing. Cell 169, 1342–1356. 10.1016/j.cell.2017.05.035 [DOI] [PubMed] [Google Scholar]
- Zhou G., Sprengers D., Boor P. P. C., Doukas M., Schutz H., Mancham S., et al. (2017). Antibodies against Immune Checkpoint Molecules Restore Functions of Tumor-Infiltrating T Cells in Hepatocellular Carcinomas. Gastroenterology 153, 1107–1119. 10.1053/j.gastro.2017.06.017 [DOI] [PubMed] [Google Scholar]
- Zhou J., Ding T., Pan W., Zhu L.-y., Li L., Zheng L. (2009). Increased Intratumoral Regulatory T Cells Are Related to Intratumoral Macrophages and Poor Prognosis in Hepatocellular Carcinoma Patients. Int. J. Cancer 125, 1640–1648. 10.1002/ijc.24556 [DOI] [PubMed] [Google Scholar]
- Zhou J., Liu M., Sun H., Feng Y., Xu L., Chan A. W. H., et al. (2018). Hepatoma-intrinsic CCRK Inhibition Diminishes Myeloid-Derived Suppressor Cell Immunosuppression and Enhances Immune-Checkpoint Blockade Efficacy. Gut 67, 931–944. 10.1136/gutjnl-2017-314032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou J., Nefedova Y., Lei A., Gabrilovich D. (2018). Neutrophils and PMN-MDSC: Their Biological Role and Interaction with Stromal Cells. Semin. Immunol. 35, 19–28. 10.1016/j.smim.2017.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou L., Fu J.-L., Lu Y.-Y., Fu B.-Y., Wang C.-P., An L.-J., et al. (2010). Regulatory T Cells Are Associated with post-cryoablation Prognosis in Patients with Hepatitis B Virus-Related Hepatocellular Carcinoma. J. Gastroenterol. 45, 968–978. 10.1007/s00535-010-0243-3 [DOI] [PubMed] [Google Scholar]
- Zhu H.-f., Liu Y.-p., Liu D.-l., Ma Y.-d., Hu Z.-y., Wang X.-y., et al. (2019). Role of TGFβ3-Smads-Sp1 axis in DcR3-Mediated Immune Escape of Hepatocellular Carcinoma. Oncogenesis 8, 43. 10.1038/s41389-019-0152-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zigmond E., Preston S., Pappo O., Lalazar G., Margalit M., Shalev Z., et al. (2007). -Glucosylceramide: a Novel Method for Enhancement of Natural Killer T Lymphoycte Plasticity in Murine Models of Immune-Mediated Disorders. Gut 56, 82–89. 10.1136/gut.2006.095497 [DOI] [PMC free article] [PubMed] [Google Scholar]