ABSTRACT
Meralgia paresthetica (MP) is a condition characterised by abnormal sensations on the anterolateral aspect of the thigh due to the dysfunction of the lateral femoral cutaneous nerve. Here, I present a case of a 64-year-old female cook who attended the General Medicine clinic with 2 months of persistent numbness and ‘burning’ sensation over the right anterolateral thigh. Subsequent physical examination revealed the diagnosis of meralgia paresthetica. The significance of good history taking and thorough physical examination in reaching the diagnosis of meralgia paresthetica cannot be overemphasized. In most typical presentations, advanced imaging and neurodiagnostic testing do not add value to confirm the diagnosis. If the clinical diagnosis is doubtful, nerve conduction study and magnetic resonance imaging may still be performed to exclude other mimicking pathologies. Increasing awareness of MP among doctors unfamiliar with this condition will prevent the ordering of excessive investigations.
INTRODUCTION
Meralgia paresthetica (MP) is a disorder characterized by abnormal sensations such as tingling, burning pain or numbness on the anterolateral aspect of the thigh due to the dysfunction of the lateral femoral cutaneous nerve (LFCN). The LFCN is a sensory branch of the lumbar plexus derived from the posterior divisions of the L2 and L3 spinal nerves. After emerging from under the lateral border of the psoas major muscle, the nerve courses inferolateral around the iliac fossa into a tunnel formed by the lateral attachment of the inguinal ligament and the anterior superior iliac spine. At the level of the inguinal ligament, the LFCN is susceptible to trauma and entrapment. As the nerve exits from the pelvis, it bifurcates into anterior and posterior branches, which provide sensation to the anterior and lateral thigh, respectively (see Fig. 1).
Figure 1.
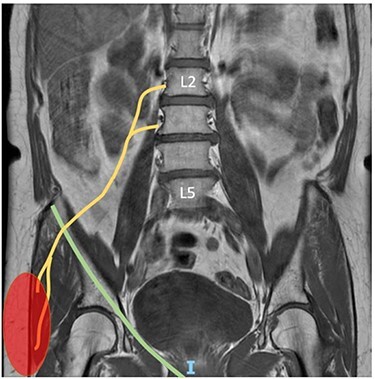
The yellow line is the right LFCN. The green line is the inguinal ligament. The red shaded area is the area innervated by LFCN.
CASE REPORT
A 64-year-old female cook at a childcare centre attended the General Medicine clinic with 2 months of persistent numbness and ‘burning’ sensation over the right anterolateral thigh. The symptoms were not aggravated by movement of the lower limb, and there were no relieving factors. She had no trauma to her back, right groin or thigh before the onset of symptoms. She had no backache, muscle ache or limb weakness. The bladder and bowel function were normal.
She had a history of minor back trauma > 30 years previously from which she made an uneventful recovery. She had well-controlled asthma on regular Seretide inhalers. She was a non-smoker and a teetotaller. Her general practitioner prescribed pregabalin 75-mg nocte and naproxen 275-mg twice daily to control the paraesthesia, but this offered her no relief.
Given the presenting complaint, a full neurological examination of the lower limbs was performed. She had no muscle wasting, and no deficits were elicited in tone, reflexes, power and coordination. The patient was able to demarcate a distinct area of paraesthesia on the anterolateral part of her right thigh. There were no overlying skin lesions on the paraesthetic area. Abdominal, inguinal and spine examinations were also unremarkable. She weighed 47.4 kg, and her body mass index was 23.3 kg/m2.
The clinical presentation and findings led to a diagnosis of meralgia paresthetica. A nerve conduction study of both the right and left LFCNs showed similar values in the latency, amplitude and conduction velocity (see Table 1). Value differences of >50% from side to side is considered significant [1]. A magnetic resonance imaging (MRI) of the lumbosacral plexus using the routine lumbar plexus protocol revealed mild focal swelling in the right LFCN proximal to the foramen beneath the inguinal ligament adjacent to the anterior superior iliac spine, compatible with underlying meralgia paresthetica (see Fig. 2). The rest of its length on the MRI showed no abnormality. There were no bony or soft tissue abnormalities within the pelvic cavity. Further investigations revealed a normal full blood count, renal function, thyroid function, vitamin B12 level and HbA1c of 5.5% (Normal < 6.4%). When the patient was reviewed in the clinic 4 months after the onset of symptom, she reported the paraesthesia had resolved completely and spontaneously.
Table 1.
Lateral femoral cutaneous sensory nerve conduction studies
| Nerve tested | Latency (ms) | Amplitude (μV) | Conduction velocity (m/s) |
|---|---|---|---|
| Right LFCN (lateral thigh) | 3.0 | 9.9 | 60 |
| Left LFCN (lateral thigh) | 2.6 | 8.8 | 65 |
Figure 2.
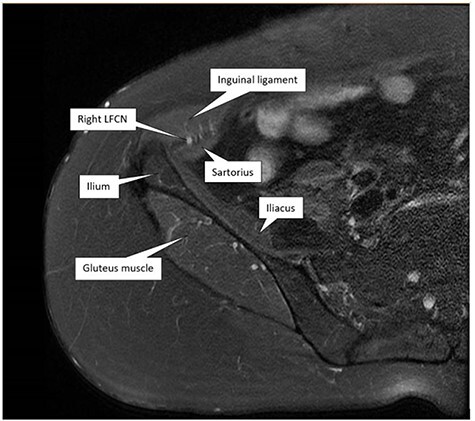
Axial T2 FS image shoes mild focal swelling in the right LFCN underneath the inguinal ligament adjacent to the anterior superior iliac spine.
DISCUSSION
Meralgia paresthetica (MP) is a condition commonly seen in primary care, orthopaedic surgery, bariatric surgery, obstetrics and intensive care settings. It is less frequently encountered in a General Medicine clinic.
There are many causes of MP. Some mechanical causes include obesity, pregnancy, pelvic masses, wearing tight belts or trousers and orthopaedic procedures causing direct damage to the LFCN. Metabolic factors such as lead poisoning, alcoholism, diabetes mellitus and hypothyroidism are also associated with MP. In a series of 67 patients with MP, 10 patients (15%) had no associated condition, making idiopathic cause the second most frequent finding after obesity [2]. Although there was no apparent cause in our patient, the presence of focal swelling in the LFCN raises the possibility that recurrent microtrauma in her occupational role as a cook may have caused damage to the nerve pain fibres.
In this patient, the nerve conduction study (NCS) was reported as within normal limits. This finding is unsurprising because the NCS of the LFCN is often technically challenging to perform due to its anatomical position, the variations in its course, the presence of increased adipose tissue and the lack of a standard NCS protocol [3, 4]. In a retrospective, cross-sectional study from Korea, 26.9% of the patients with MP were found to have normal LFCN conduction study [4]. This study suggests that NCS of the LFCN has a fairly low sensitivity in the diagnosis of MP and cannot be used as a substitute for a good history and appropriate physical examination. Nevertheless, an electrophysiological study may still be performed to rule out other mimicking diagnoses such as lumbar disk herniation and radiculopathy, especially if there is uncertainty about the clinical diagnosis [3].
Traditional MRI is not routinely used to assess LFCN as signal intensity changes of small peripheral nerves are usually challenging to evaluate. It may be performed to exclude other conditions that may mimic MP such as metastasis in the iliac crest, lumbar disk herniation, lumbar radiculopathy and chronic appendicitis [5–8], and to identify other bony abnormalities that may cause compression along the course of the nerve [9]. With advancing technology, magnetic resonance neurography is increasingly being utilized to diagnose or exclude a neuropathy, assess the degree of nerve injury, characterize the culprit lesion causing nerve entrapment and aid radiological-guided injection of perineural medication [10]. In the presence of neuropathy, the signal intensity of the injured nerve increases and is similar to the fluid-like signal intensity of the neighbouring vessels on T2 weighted imaging, as demonstrated in Fig. 2 [10].
In conclusion, this case has highlighted the importance of good history taking and thorough physical examination in reaching the diagnosis of meralgia paresthetica. In most cases, advanced imaging and neurodiagnostic testing do not help make the diagnosis. Raising awareness of meralgia paresthetica among physicians unfamiliar with the condition will prevent the overuse of investigations.
ACKNOWLEDGEMENTS
I thank Professor C. Rajasoorya from the Department of General Medicine for proofreading the article and Dr Wong Bak Siew Steven from the Department of Radiology for the MR images.
CONFLICT OF INTEREST
No conflict of interest.
FUNDING
None declared.
ETHICAL APPROVAL
No ethical approval is required.
CONSENT
Written informed consent was obtained from the patient.
GUARANTOR
I, Dr Wai Lun Moy, am the author and the guarantor of the paper. I confirm that the manuscript represents original work that has not been published, accepted or is currently being considered for publication elsewhere.
REFERENCES
- 1. Laughlin RS, Dyck PJB. Electrodiagnostic testing in lumbosacral plexopathies. Phys Med Rehabil Clin N Am 2013;24:93–105. [DOI] [PubMed] [Google Scholar]
- 2. Kitchen C, Simpson J. Meralgia paresthetica. A review of 67 patients. Acta Neurol Scand 1972;48:547–55. [DOI] [PubMed] [Google Scholar]
- 3. Lo YL, Pavanni R. Electrophysiological features in the Management of Meralgia Paraesthetica. Ann Acad Med Singapore 1998;27:530–2. [PubMed] [Google Scholar]
- 4. Choi MH, Park H, Eom YI, Joo IS. Clinical and electrophysiological characteristics of Meralgia Paresthetica. Korean J Clin Neurophysiol 2013;15:48. [Google Scholar]
- 5. Tharion G, Bhattacharji S. Malignant secondary deposit in the iliac crest masquerading as meralgia paresthetica. Arch Phys Med Rehabil 1997;78:1010–1. [DOI] [PubMed] [Google Scholar]
- 6. Trummer M, Flaschka G, Unger F, Eustacchio S. Lumbar disc herniation mimicking meralgia paresthetica: case report. Surg Neurol 2000;54:80–1. [DOI] [PubMed] [Google Scholar]
- 7. Kallgren MA, Tingle LJ. Meralgia paresthetica mimicking lumbar radiculopathy. Anesth Analg 1993;76:1367–8. [DOI] [PubMed] [Google Scholar]
- 8. Ghavanini MRA, Ghavanini AA. Meralgia paresthetica as the presenting feature of chronic appendicitis. Am J Phys Med Rehabil 2001;80:703–5. [DOI] [PubMed] [Google Scholar]
- 9. Petchprapa CN, Rosenberg ZS, Sconfienza LM, Cavalcanti CFA, la Rocca Vieira R, Zember JS. MR imaging of entrapment neuropathies of the lower extremity: part 1. The pelvis and hip. Radiographics 2010;30:983–1000. [DOI] [PubMed] [Google Scholar]
- 10. Chhabra A, Andreisek G, Soldatos T, Wang KC, Flammang AJ, Belzberg AJ, et al. MR Neurography: past, present, and future. Am J Roentgenol 2011;197:583–91. [DOI] [PubMed] [Google Scholar]


