Abstract
This paper describes an Experience-based Co-design (EBCD) project that aimed to increase patient activity within an acute stroke unit. We apply the concept of liminality to explore ways in which the EBCD process, a form of Participatory Action Research, may dilute or even dissolve social hierarchies and challenge assumptions about practices and constraints in this care setting, thereby opening up possibilities for transformation that enhances the therapeutic value of the space for patients and care providers alike. By occasioning a liminal phase of possibility for change, the work of one co-design group explored in detail here suggests that, in this process, the sociomaterial interactions involving patients, family members, staff, and the physical space are refashioned and re-inscribed in transformed ‘emplaced’ relationships of care.
Keywords: Experience-based Co-Design, Stroke rehabilitation, Liminality, Ward environment, Therapeutic space
Highlights
-
•
EBCD improved an acute stroke unit environment to provide greater opportunity for social and therapeutic activity.
-
•
The structured EBCD approach provided a ‘liminal’ space within which collaborative change could be enabled.
-
•
Liminality facilitated trust and built a sense of community between participating patients, families and staff.
-
•
The different roles adopted by participants during the process challenged norms and effected change.
1. Introduction
Participatory Action Research (PAR) is an approach whereby participants become actively involved in the process of change, rather than being passive informants (Baum et al., 2006). Through cycles of reflection and action, the approach aims to enable understanding of an aspect of the social world and working to change it collaboratively (Baum et al., 2006). Informed by human-centred design, learning theory and narrative-based approaches to change (Robert, 2013), Experience-based Co-design (EBCD) is a form of PAR which was specifically developed to enable patients and frontline healthcare staff to work together to improve the quality of care and services. Adaptations and evaluations of the original approach -a pilot in a head and neck cancer service in 2004–05 (Bate and Robert, 2006)- have led to a structure for applying ‘design thinking’ to improving healthcare services driven by the priorities of patients, family members and staff (Sangiorgi and Prendiville, 2017). Focussing on experiences of both providers and users of a service, EBCD gives voice to both patients and staff and brings them together in co-design groups in which they prioritise and implement changes (Bate and Robert, 2006).
Drawing upon participatory design principles (Robert et al., 2021), the co-design element in EBCD seeks to recognise and benefit from forms of experiential knowledge which are typically neglected in healthcare improvement work (Donetto et al., 2015a); that is to say, patients (and often their relatives and informal carers) are invited to share their knowledge and participate as equals to staff in a structured organisational change process. As such, EBCD can be viewed as a small part of a much-discussed shift towards the co-creation of public services involving a wider set of resources and which views service users as vital to the design and delivery of services, working with professionals and front line staff to devise effective solutions (Cottam and Leadbeater, 2004) (Meroni and Sangiorgi, 2011). As we have argued elsewhere (Donetto et al., 2015), equality, equal contribution and mutual respect are central to co-design but challenging to establish in healthcare contexts given the traditional roles of ‘provider’ and ‘recipient’ of care ascribed to social actors. Some of those who have led EBCD projects highlight how specific configurations of power can have a significant impact upon the process of co-design and the implementation of changes (Bowen et al., 2013): 14). Nevertheless, co-design (in EBCD) has – in line with a ‘democratic’ model of service user participation –the potential to help form new discursive spaces and discourses that ‘traverse people's sociocultural, professional and personal boundaries' (Iedema et al., 2010) p.86 (Turner, 1977b).
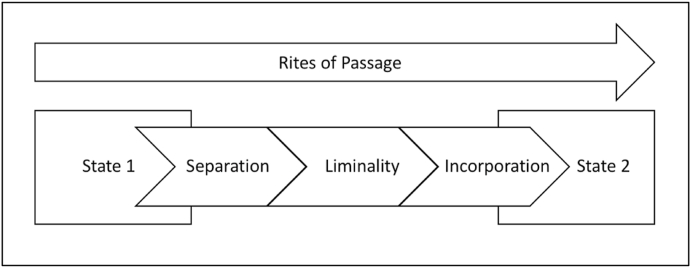
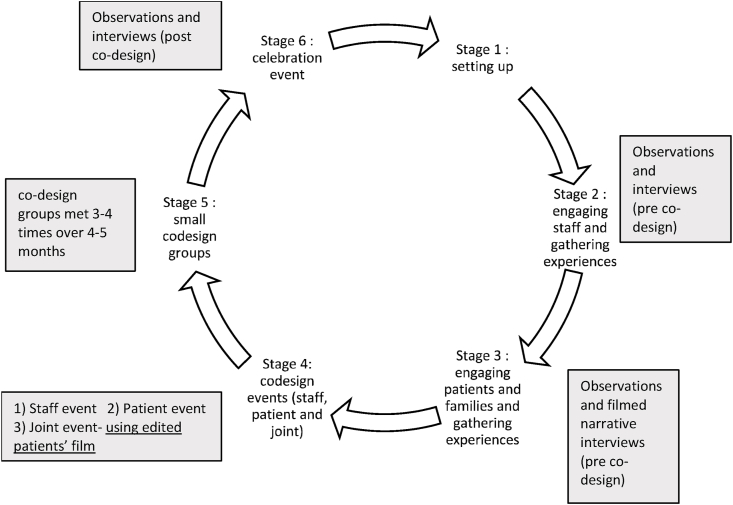
EBCD typically includes a structured, facilitated 6-stage process (Fig. 1) and takes between 9 and 12 months to complete. Central to the approach is the view that patients are equal partners in the co-design process. Despite increasing use of EBCD as a service improvement methodology across healthcare (Donetto et al., 2015b), there were few examples in stroke care and rehabilitation, and there has been little attention paid to understanding the social processes and dynamic context of EBCD within acute settings. This paper draws upon data generated for a study that aimed to assess the feasibility of co-designing more active rehabilitation environments for patients recovering from a stroke.
Fig. 1.
Schematic showing van Gennep's Rites of Passage sequence. (adapted from Söderlund and Borg, 2018).
Since the National Stroke Strategy was launched in 2007 to facilitate large-scale NHS stroke service improvement in England, more than nine out of 10 stroke patients are cared for on an acute stroke unit (Stroke Association, 2018), substantially improving clinical outcomes and reducing length of stay. Specialised stroke care is delivered by a multidisciplinary team typically consisting of doctors, nurses, therapists, psychologists, and dietitians that meet regularly to share updates and plan care based on patient needs and according to predetermined National Stroke guidelines (Intercollegiate Working Party for Stroke, 2012). These guidelines are based on a hierarchy of evidence and clinical consensus for example promoting independent patient activity in the acute phase of stroke is recommended as it is associated with improved outcomes such as personal independence (Askim et al., 2014; Intercollegiate and Stroke Working Party, 2016; Lohse et al., 2014). UK stroke units are currently required to submit data according to specified quality criteria including whether patients receive 45 min of appropriate therapy (Occupational Therapy, Physiotherapy and Speech and Language therapy) for a minimum of five days per week (Intercollegiate Working Party for Stroke, 2012). However, the impact of the guideline is built on three assumptions: first, that recommendations on rehabilitation intensity are interpreted and enacted consistently by therapists; second, that therapy is available over all 7 days of an inpatient week; and third, that rehabilitation is the responsibility of therapists alone and not that of the whole multidisciplinary team.
Despite the focus on delivering therapy according to guidelines, ethnographic studies on stroke units have shown that stroke units are dominated by routinised patterns of work focussed on tasks such as washing, dressing, mealtimes and ward rounds consisting of brief technical encounters between staff and patients, and limited opportunity for patient engagement and activity (Clarke et al., 2017; Costa et al., 2021; Taylor et al.). So, whilst staff are occupied in task completion through each day, between encounters with staff, patients are very often inactive and can ‘normalise’ to the absence of opportunity to engage with therapeutic activity (Costa et al., 2021). This paper draws on findings from the Collaborative Rehabilitation Environments in AcuTe strokE study (CREATE) (Jones et al., 2020) which applied an EBCD approach in an effort to transform the acute stroke environment to increase stroke patients' activity levels. It focuses on one of the sites taking part in the study and on one of the smaller co-design groups that sought to reconfigure the physical environment of a stroke rehabilitation unit.
We discuss here the extent to which liminality is a useful lens to understand and interpret the behaviours of and interactions between co-design participants in the context of their relationships with space and place in the stroke unit. We suggest that liminality can provide a fresh perspective on participants’ engagement with and experiences of EBCD in the context of the reconfiguration of places of care and the sociomaterial interactions of which they are part.
Empirical work by van Gennep described rites of passage and ritual forms in terms of three distinct phases of separation, liminality and incorporation when moving from one social status to another (Fig. 1) (Van Gennep, 1960). Anthropologist Victor Turner's work in the late 1960s and early 1970s elaborated upon the role of the liminal phase in rites of passage and other cultural rituals in enabling transformations in individuals moving from one social status to another (Turner, 1969, Turner, 1977a). Turner described those in the liminal (from the Latin limen, threshold) phase of the rite of passage as being “betwixt and between”, no longer of one status but not yet of another. This phase entails the dissolution of the known social order (‘structure’) and the possibility of new configurations and structures (‘anti-structure’), until a new status and social order is reached. As Turner put it: “The liminal is that which is neither this nor that, and yet is both” (Turner, 1967) p.59 In this liminal time-space, participants in the ritual are brought together in ‘communitas’. This is, Olaveson (2001) summarises:
an unstructured or rudimentarily structured and undifferentiated communion or community of equal individuals. […] … it is comprised of egalitarian, direct, non-rational bonds between concrete, historical, idiosyncratic individuals who are equal in terms of a shared humanity; it is a modality of human interrelatedness …) (Olaveson, 2001)p.104.
and is usually characterised by a strong, if not dominant, emotional dimension (Olaveson, 2001). Studies in healthcare that have used the concept of liminality to explore a place of ‘in-between’ at the core of participants' experiences (Atkinson and Robson, 2012; Little et al., 1998) stress the importance of understanding the phase of transition, for example after being diagnosed with serious chronic conditions that can have a significant impact on one's sense of identity and social location. However, we are not aware of studies that have previously used the concept of liminality to explore what happens during co-design or participatory research processes in a health care setting and suggest here that this may be a useful analytical lens to explore and understand the effects of participatory improvement work on ‘emplaced’ – i.e. grounded in the “interrelationship of body-mind-environment (Howes, 2005) p.7 - power relations.
2. Background – An EBCD case study in one acute stroke unit
Environmental enrichment studies in stroke services to date have largely been external-researcher driven but have made a contribution to increased activity levels in patients in acute stroke units (Janssen et al., 2014b; Rosbergen et al., 2017). The CREATE project adopted a participatory approach to enable groups of former patients, families, and staff to prioritise improvements and co-design solutions to address levels and forms of therapeutic activity in their stroke units. The CREATE EBCD approach (see Fig. 2 and text below) referred to in this paper was used in four participating units in acute hospitals in London and North England (Jones et al., 2020). For this paper, we refer only to Site 1 (S1) here, as it was one of the first units to complete a full EBCD cycle. S1 is a 600-bed district general hospital, in a socio-economically deprived area in London, and the stroke unit was not engaged in any existing research or improvement activity. Within this study site, we focus on the work undertaken by one of the three co-design groups that formed at this site, that is the ‘space’ group-which worked on the physical environment of the stroke rehabilitation unit.
Fig. 2.
EBCD
Stages 2 and 3 of the EBCD process involved exploration of participants’ experiences. This data collection included audio-recorded individual interviews with staff members, filmed narrative interviews with patients and non-participant observation of routine activities in the stroke unit (Table 1). The Health Research Authority and South East Coast Brighton & Sussex Research Ethics Committee (16/LO/0212) provided ethical approval.
Table 1.
Site 1: Participant numbers, BM observations, Observation hours.
| Staff interviews | patient interviews | carer interviews | BM Observations | Non-participant observation hours | |
|---|---|---|---|---|---|
| pre-stage 2 EBCD cycle | 13 | 9 | 4 | 702 | 50 |
| post-stage 6 EBCD | 8 | 5 | 5 | 949 | 46 |
Narrative interviews (i.e. minimally structured interviews allowing for a full account of the participant's experience of care in their own narrative) with patients and semi-structured individual interviews with staff explored stroke unit routines (e.g. timing of shifts, meals, ward rounds and other regular tasks) and experiences and perceptions of activity and inactivity (Jones et al., 2020) particularly outside any structured therapy provision, for example during evenings and weekends. Interviews were conducted by AC, FJ and STK, and typically lasted about 1 h. Interviews took place wherever convenient for participants, which was mostly at the hospital site for members of staff and at home for patients and family members.
Non-participant observation was conducted over 10 days at different times including evenings and weekends by one of the research team (AC, FJ and KG) and involved observation of organisational processes, context and interactions between staff and patients including instances of planned and unplanned activity. In addition, behavioural mapping was carried out at 10-min intervals on three separate days (weekdays and weekends). Behavioural mapping (BM) is a validated method of observing social, cognitive and physical activity of patients at 10 min intervals and generates 60 observations for each patient per day (Janssen et al., 2014a).
Not only did the observational fieldwork and interviews provide context and informed the participatory process that followed, but such activities also enabled involvement of patients and carers from the very start, providing occasions for the research team to listen and learn about their experiences and opportunities (or not) for activity. During subsequent joint staff, patient, and carer events (Stage 4), insights from this initial fieldwork (prompted by viewing and discussion of a composite film of the patient narratives) were reflected upon jointly by participants. Improvement priorities were discussed and, using facilitation techniques such as emotional mapping (walking through the emotional journey of a day and night in the life of a patient), ideas were taken forward into smaller co-design groups (stage 5). During a six-month period, several priorities and action points were addressed by each of these co-design groups. Following implementation of changes a joint celebratory event (Stage 6) was held as part of the EBCD cycle to recognise the range and extent of service improvements and the efforts of the co-design groups.
Data from observations, Behavioural Mapping (BM), and interviews with staff, patients and carers provided context for understanding the unit environment and getting a sense of the extent and nature of daily communications between different actors, unit routines, processes, and patient activity-see Table 1. Observation and interview data were analysed thematically using NVivo software by the research team (KG and FJ) taking an inductive approach, and then summarised and discussed iteratively with the wider research team (CM, AM, GR, RH, DC and SH). BM data were analysed using SPSS v22 software and reported as frequency counts for social, physical, and cognitive activity types. Throughout the research process, the researchers recorded reflective notes. Lead field researchers (KG and FJ) supported co-design groups, organised events, conducted interviews, ethnographic observations, and BM.
2.1. Engaging with staff, patients, families, and the environment
Behavioural mapping data were consistent with observations and confirmed very low levels of physical, social, and cognitive activity in the unit prior to the co-design work. These data provided important evidence for the experiences discussed in the separate staff and patient events and the joint event (stage 4 EBCD). Staff expressed the perception that efforts to change the environment had been made before and had often been held up by organisational barriers such as limited funding, lack of space, and health and safety policies. However, staff's resolve to change things was strengthened when they heard about the findings from the observation data, and the very low levels of activity and boredom reported by patients at weekends and evenings.
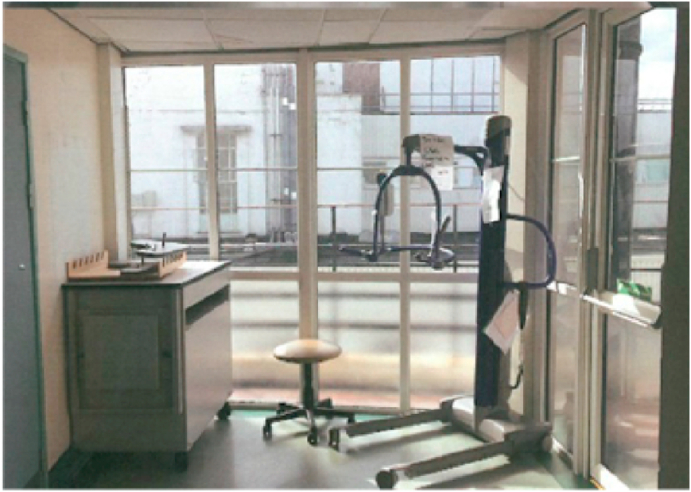
As well as confirming staff perceptions that the unit had low levels of activity and engagement, observations documented that the environment looked uniform and bland, all walls were beige and notice boards were populated with multiple health and safety posters. The corridors were dark, and the space often filled with large equipment; there was no visible welcoming for patients and families coming onto the unit (Fig. 3). Observations also revealed how frequently patients’ bedside areas were cluttered with clinical equipment such as sharps boxes, syringes, and dressings (Fig. 4). Typically, patients had very few personal items such as photographs in evidence, and no space for any personal activities such as jigsaws or drawing.
Fig. 3.
Cluttered and bland corridors.
Fig. 4.
Typical bed space and décor described by patients and staff as cluttered and uninspiring.
From our interviews, it became clear that patients and family members felt the “sterile” environment negatively contributed to their perception of being distant from their own home. One patient, for example, commented:
And it looks very much like a hospital environment, I think the colours are very hospital-y, I think the decor is a bit shabby and when you're spending months in this hospital sometimes it just feels like there's nothing that looks particularly homely. (Interview, Patient)
They added that a few familiar objects – “like photos and a radio, my own cushion and cup..”
would help with making the place more homely.
As well as the clutter in corridors and lack of personal items at bedsides, there was no shared social space -for example, a day room-for patients to access. This meant that all personal communication with relatives and visitors took place at the bedside in cramped conditions. A member of staff highlighted how a day room would constitute a space for patients to socialize away from the very institutionalised look of the unit's environment:
I keep going back to this idea of realistic day room thing, it would be nice for patients to go in there and socialise […], getting them off that unit environment because it is meant to be rehab and it is very, very hospitalised (Interview, Member of staff)
Patient participants also highlighted what a missed opportunity it was, for their rehabilitation, not being able to connect with other patients and visitors on the unit. Patient interviews pointed to ways in which socialising with other patients may be helpful: by helping pass the time, by mitigating feelings of isolation, by providing new ideas for their recovery:
[…] when you're talking with different people, it not only makes the time go, it also makes you feel better in yourself, because you feel, “I'm not alone”, […] because you hear about things that perhaps you hadn't thought of yourself.” (Interview, patient)
The interviews with patients, family members and members of staff signalled participants’ aspirations for physical changes in the environment, such as the introduction of new colour schemes for one family member and a brighter space for a member of staff:
[S]o you might have some apricots and peaches and whites sort of blended in soft tones and then maybe some pale blues and pinks, just make it more, but not just mono colour, actually sponge effects, that kind of thing. It just gives a more welcoming atmosphere, more healing atmosphere … (Interview, Family member)
On my wish list would be just to decorate the ward and have a brighter space … use the space we have but make it brighter and less shabby … that would be lovely (Interview, staff member)
It became clear from the interviews and observations that the cluttered clinical environment impacted on staff experiences as well as patients' and families, and through co-design events the idea of having a ‘bit of home in the unit’ and, ‘bringing the outside in’, began to emerge. Ideas voiced in interviews and informal discussions sometimes highlighted the potential symbolic value of imagined change, like this member of staff suggested:
It's about laying it out there and saying let's have a fresh start together … - how are we going to do the best for our patients, how can we look for all the opportunities to make life more enjoyable whilst they are on our ward (interview, staff member).
These ideas and perspectives were taken forward to events in stage 4 and generated excitement and a sense of possibility.
2.2. Staff, patient, and joint events
In stage 4, two separate facilitated events – one for staff and one for patients and carers-were held to discuss the findings from observations and interviews. In these events, participants were creative and wide-ranging in generating ideas in response to the findings around the extent to which the unit's environment was cramped, uninspiring and dull, until they reached a shared agreement within their groups on priorities for change. After these facilitated sessions, staff, patients, and family members came together for the first time at a joint event (also in Stage 4). Here, they viewed a 20-min composite film of patients' and family members' video interviews focussing on key aspects of participants' experiences of care in the unit. For example, in the film a patient highlighted the negative impact of restricted bed space and of small actions by members of staff on their ability to carry out simple activities and to feel autonomous:
With the handle [of the water jug] turned the other way round, …and the thing that goes across the bed, I used to have by the side of me and I had everything placed so that I could get a hold of it, and they used to come up and put the jug down right across the other side and with the handle pointing outward, not toward me. (Interview, Patient, S1)
Exposure to the patients' voices and sentiments in filmed interviews seemed to incentivise staff regarding the need for change. It is from this point onwards that we think the EBCD process has the potential to enable a degree of dissolution and/or ‘separation’ from the known order (‘structure’) (Fig. 2) and we will return later to why we think the liminal potentiality of EBCD may help us understand how it enables social transformation. The composite film triggered emotional responses from staff and made visible the importance of and need for change. Through a series of large group and small round table discussions, participants identified three main priorities for change: 1) the physical therapeutic and social space, (2) activity opportunities, and (3) unit communication and culture. During the joint event staff, patients and family members expressed preferences about the areas of change they felt most motivated to work on and volunteered to join the co-design group (stage 5 of EBCD) focussing on the priority area that was closest to this interest. For example, the co-design group which would work on the physical space of the unit included a family member who was also a local artist and a staff member who had an interest in craft and design.
2.3. Co-design groups and celebration event
Codesign groups were encouraged to meet regularly and to elect both a patient/family member and staff member to help facilitate and record actions. Groups were supported by one of the research team (KG), who updated participants on progress with action points, sent necessary information and arranged travel for patient and families to group meetings.
The group that focussed on the physical environment of the unit -or ‘Space’ group – is the focus of this paper. The group included four staff members, five patients and four patient family members. They met four times over a five-month period and had email exchanges and informal meetings e.g., one-to-one meetings on the ward to discuss specific items such as artwork or furniture in the intervening weeks. The formal meetings were based on debate and discussion about space with an emphasis on ‘what was possible’ within the co-design group. This focus freed staff from previous concerns about barriers to change and enabled a dialogue which generated enthusiasm about patients' ideas. The interviews with staff and patients after the implementation of the co-designed changes indicated that the co-design work had led to participants perceiving their status as having become much more equal. A family member, for example, stated:
… everybody was treated like equal […] respectfully and ideas from the patients were taken on board really well and the staff suggestions […] they didn't impose anything on anybody, it was all very well balanced […]. I think they appreciated the patients' feedback. I'm sure they learnt stuff from the patients that they didn't know about their relationship before […]. (Interview, Family member)
A member of staff highlighted how the direct involvement of users of the services in making changes towards care improvement, was ‘the best thing about the whole process’:
Well I think the most positive thing about it is often when we try and change things in healthcare it’s the wrong people making the changes, and actually part of this whole process is actually listening to what the patients had to say, […], I think that's the best thing about the whole process, is actually just using patient experience and staff experience to bring about change. (Interview, member of staff)
As we discuss in more detail later, the collaborative work carried out as part of the co-design process generates a sense of partnership and of unanticipated value (that of thinking ‘out of the box’) that resonate with features of ‘communitas’ as discussed by Turner (1969).
Finally, the EBCD celebration event (Stage 6) provided the opportunity to publicise service improvements to external stakeholders (local press, voluntary and community groups, and local artists) and for the co-design groups to highlight the potential use of EBCD as part of wider structural and organisational change. Discussions at this event also raised suggestions for further changes as managers and staff not involved in the CREATE study heard about the impact perceived by all participants and considered the added value of EBCD as an improvement approach.
3. Anti-structure, liminality and communitas
The joint event and codesign groups (stage 4 and 5 of EBCD) in which patients, families and, staff discussed ideas in a free-flowing way, resembled a liminal space that enabled the sharing of new views and emerging ideas. This locus of potentiality resonates with what Turner calls an ‘anti-structure’ to the ‘structure’, i.e. a transitional (and necessarily temporary) state in which communitas and the liberation from recognised identities and roles are possible (Turner, 1969).
Members of our ‘space’ co-design group recognised the blurring of social roles in group-work and the value of the coming together of different identities in the EBCD sessions:
What I realised is when you get people from different aspects of the unit, family members, patients, therapy members, staff, nurses, you get [ …] almost a multilayer of input and just […] a broader kind of view, and also the same goes for […] problem solving, so I would look at a certain situation but then somebody else will come in a totally different angle with different experiences and it's just so much easier to solve a problem […], so I think that was really powerful when the groups met, (Interview, member of staff)
Interview data suggested that the co-design groups provided a space which allowed not only for free thinking, but also for connecting and perceiving of each other in different roles, i.e., not as “patient” and “staff”, but as an ‘equal’ co-design group member. EBCD brokered the transition from then (the way things were when participants used to be inpatients) to now, from looking at barriers to change and at what is not happening to actively creating conditions for change to occur and be sustained. The experience of participating in the co-design groups and the wider EBCD project enabled this shift from existing professional roles to our interrelatedness as humans, that is, communitas:
I think it was very positive. People were very open and as therapists […] you don't see things in [through] the eyes of the patient or a family member and it just made me realise that [..] they're all humans and it's a horrible thing that happened to them, it's like a tragedy […], it's great to give them physiotherapy and OT and whatever, but there's so much more that we can do as humans, […] (Interview, member of staff)
As others have commented, in codesign participants propose solutions to the here and now but in a way that is inevitably connected to past experiences (Palmer et al., 2019), and staff in our study were directly confronted with fresh narratives about stroke survivors ‘inhabiting’ a stroke unit and managing their boredom and inactivity. They were required to listen rather than performing their more familiar roles of telling, advising, and directing others. In this research site, mutual trust, and a sense of communal action to change existing spaces and practices developed quickly. The tacit knowledge and skills of our participants, some of whom had been through the experience of stroke more than once, almost implicitly reinforced the need to change. Actual experience of a traumatic health issue legitimised the need to change; such powerful causes necessitated the need to enter the liminal space. This emergence of trust within the liminal space through EBCD processes and activities enabled a social relational ‘anti-structure’ rich of transformation possibilities. The bond of trust formed within the co-design groups built a social contract between the participants that members of staff felt obliged to fulfil in order to do justice to patients' and family members' involvement (Gilson, 2003). This social contract could be said to strengthen communitas.
The peculiarity and strength of EBCD is that it does offer a structure, thus avoiding excessive discomfort for participants who may otherwise be wary of plunging into a completely disorganised improvement effort, but at the same time highly flexible and fluid, which frees the participants from having to perform a specific prescribed role in the process. Participants' interviews supported the idea that the EBCD structure with its six clearly defined stages was important to build trust, as well as the ‘meaning’ the groups gave to the changes:
[I]t feels like we're about to make some meaningful change without changing anything too radically, […] lots of small improvements, […] adding up […] […], a bigger improvement overall, […], I think that's really pleasing. (Interview, member of staff)
The contained ‘not knowing’ at the start of the co-design stages (especially from the joint event onwards) provided space to reconsider actions and perspectives that are familiar and generally unquestioned, to reflect, in other words, on the status quo. In the rituals studied by Turner, people inhabiting this transition phase are ‘liminal personae’ or ‘threshold people’, temporarily liberated from their previous social role(s) and not yet stabilised into new ones (Turner, 1969). However, in the case of our EBCD work what was transformed via a process of redefinition, uncertainty and liminality was not the social status of participants but the assemblage of built environment of the unit, its spatiality, and the relationships between participants and between participants and the space. We now turn to examining this transformed network of sociomaterial relationships.
4. Transformed relationalities
Numerous visible changes to the environment (Fig. 5, Fig. 6, Fig. 7) were implemented, which included new artworks and colour schemes, digital clocks, coat hooks, photograph hangers for every bed, activity boxes giving access to cognitive games and materials, and a new therapeutic space for dining and activities such as art workshops. These changes were the product of collective action by members of staff, local artists, and family members as well as the research team which began after the first codesign group meeting and continued beyond the celebration event. A lot of structural changes e.g., wall painting-happened at weekends, which meant incremental changes were visible and provided motivation to participants. The project benefitted from the input of one of the participating patient's daughters, who was a local artist, and of a dietician. A mayoral visit marked the official closure of the 9-month EBCD project, when the new stroke unit ‘space’ was revealed to the mayor, senior management team, and local stakeholders including voluntary groups.
Fig. 5.
End of a corridor at site 1, previously used for storing chairs and hoists.
Fig. 6.
New space at site 1, now an area for patients and families to meet and socialize.
Fig. 7.
One of the new colour schemes in a four-bedded bay with a shelf for clinical equipment, photo hanger and space on the locker for personal items. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Navigating from the relative anti-structure of the co-design and ideas phase (Stages 4 and 5) through the more rigid organisational structure of estates, finance and unit processes was sometimes frustrating and challenging. Changes such as hanging original local artwork on the unit walls, new shelves for patients to de-clutter the bedside, coat hooks next to patient beds, and photo hangers were completed quickly and were used and appreciated. Making the toilet accessible for families so they would not have to leave their relative for too long or having a drinks station on the units at weekends, on the other hand, took much longer and required intervention at a relatively senior managerial to overcome perceived health and safety barriers. However, having the endpoint for the celebration event in sight accelerated those changes to happen so they could be presented to the patients and family members as well as senior management including the hospital chief executive.
The changes in the physical space were intended to enable inpatients to have a relationship of familiarity with the environment, which would support hope and motivation for the rehabilitation process. As one family member put it:
[…] but to just be in such a sterile area and they're all in there for quite a long time so it's nice to make it somewhere where they feel familiar and they feel there's home almost because, again, that gives them hope and gives them strength to keep going. (Interview, Family member)
They were also intended to enable different types of interactions. For example, the transformation of the end of a corridor into a space for meeting and socialising (see Fig. 5, Fig. 6) aimed to enable conversations and exchanges between inpatients/family members, and the space for photos and personal items in the bays aimed to generate exchanges between patients and between patients and staff that were based on the lives and experiences of patients outside of the stroke unit. In other words, the transformed spaces -born out of previous patients’ experiences of relating to the unit-were meant to occasion and support new, transformed interactions and relationships between social actors but also between social actors and the place in which care takes place. As one member of staff pointed out:
[T]he rooms […] feel more comfortable, they feel more secure, it feels less like a sterile, horrible hospital environment, and they're actually talking to one another more, and I think I told [anonymised] that one thing that will always stay in my mind is when we put up some of the pictures I think it was in bay, the last bay, the male bay, one of the patients never, ever opened his eyes or kind of showed any response, he opened his eyes and he looked at the picture and that kind of made my day, so I think that could have made a change in the overall feeling of the unit for patients, families and for people working there. (Interview, member of staff)
Staff who did not take part EBCD actively whilst lacking the agency to contribute directly began to see visible changes in their working environment and moved through a phase of uncertainty and adjustment to a new configuration of interactions and spatiality. In this sense, the transformed space-human interactions showed the potential to refashion perspectives and habits in the longer term.
5. Discussion and conclusions
It is a well-known idea in human geography that places “organize social space and therefore social relations and power, practice, resources, and knowledge” (Liaschenko, 1994)p19. More recent post humanist thinking proposes that “the meaning of place […] is not considered a product of individual cognitive processes but rather mind, discourse, and representation are understood to be locked together with physical materiality” (Kearns and Andrews, 2021) p306. We suggest that in the case of the stroke unit improvement work illustrated above, liminality was occasioned by the EBCD process but the transformations of relations of power were inscribed in the space and in the transformed relationships the space takes part in, rather than in the individual identities and social roles of participants. For the codesign group we have discussed here, implementation of change involved the management of a liminal space -in this case the assemblage of physical space, patients, family members, staff, researchers, sticky notes, journey maps, coffee cups and sketched ideas etc-in which relatively unbounded possibilities for transformation had room to surface. CREATE enabled a temporary dissolution -or at least dilution-of power asymmetries in acute stroke care whereby participants questioned current norms and orientated around new possibilities such as a personalised bed space and a more homely, therapeutic feel to the stroke unit, with additional space to form social connections.
EBCD offered the opportunity for people to get involved in the process flexibly, in keeping with experiences of co-production which Filipe et al. (2017) described as “generative processes that are less about delivering predictable impacts and outputs and more about developing new communities, interactions, practices, and different modes of knowledge and value production” (Filipe et al., 2017) p.5. This meant, participants could come to meetings when it suited, could join more than one group, or give feedback over the phone or email. However, the actual outcomes still mattered. Tangible improvements were still the main aim of the project and constituted an endpoint to the liminal space.
The process of co-designing a more social and therapeutic environment was a complex challenge in a stroke unit which serves a primary purpose as delivering clinical care. It highlighted the tension between ‘communitas’ and social actors and roles that continue to represent the existing social structure of the care environment. Whilst the social processes of CREATE and changes on the unit started to take shape, not everyone perceived this positively and some referred to higher external forces such as ‘they’ [other actors in the NHS Trust who were not taking part in the process]. For example, a member of staff pointed out that newly installed shelves may be too high to reach, and was attributed to someone ‘outside the unit’ making a decision that would impact on their everyday care tasks. As others have noted (Bridges et al., 2017), taking part in activities to bring about changes for the benefit of the patient can still be perceived as subordinate to providing direct patient care (Bridges et al., 2017).
Some scholars have argued that the input of people in a research or co-design project itself must be constantly questioned to reduce exploitation, i.e. unpaid service users doing the work of others (Farr, 2018). We had (ethical) checks and processes in place that made sure that patients and families were fully informed before they agreed to take part in the research and take part in EBCD. We were keen for co-design to be perceived as of value rather than being an additional burden for staff as well as patients and families. We encouraged flexible participation and groups with diverse skills and backgrounds, but many staff carried out additional work out of hours and patient and family participants sustained their involvement beyond the project, providing art groups at weekend and singing classes, well beyond the structure of the project.
We found that the actual physical space was important for change and was a central part of it. In our case, the identity of the unit changed with the participants' perceptions moving from a predominantly clinical environment and ethos towards a space in which patients and staff could be more creative, active, and connected with each other. For example, the co-design group decided they wanted “the outside in” and encouraged families to bring in familiar home items. Although the relatively slow pace of change through an EBCD cycle can be seen to be a limiting factor in the setting of acute stroke care, we learned that relatively ‘small changes’ -such as the photo hangers-could make a significant difference to care practice, both in terms of helping validate EBCD as important way of arriving at change and in terms of transforming the possibilities for care interactions that are more inclusive.
Apart from the changes to the physical environment-observational and interview data confirmed discernible changes in the nature and use of communal ward spaces and more group activity, e.g., breakfast and art groups and increased activity opportunities at bedsides for individual patients. Patients and families had access to new social spaces to meet and interact, and organized groups and community volunteers were available at weekends. Behavioural mapping data post implementation of codesigned changes, also confirmed the changes we saw in the space and environment of the units, with an increase in cognitive and social activity (Jones et al., 2020). Additionally we found that stroke unit staff communicated more consistently about activity opportunities through leaflets and posters, highlighting activities available outside of structured therapy provision for example at weekends and evenings (Jones et al., 2021).
This study has also confirmed the idea that the stroke unit is itself a space in between home and care home for some and between not knowing and learning how to come to terms with a new and serious health condition. In many ways, clinical spaces more broadly can be seen as liminal insofar as the patients experiencing them may also be experiencing some form of identity transition in relation to their condition. In this sense, it would be possible to examine liminality within liminality depending on the process we choose to focus on. Our data was limited to the EBCD process in the stroke unit described above and did not allow for this type of exploration. However, we suggest that examining what types of dissolution of structure are possible in specific clinical areas and how they relate to the wider care context in which they are situated would be a useful direction for healthcare research, alongside analyses of the extent to which the built environment of a service can be included in studies of collaborative approaches to the design of places of care (Curtis et al., 2007).
Finally and most significantly for our understanding of EBCD, we found that the co-design work of the ‘space’ group in one case study illuminated ways in which EBCD as a process occasions liminality for a more democratic reconfiguration of emplaced sociomaterial interactions in healthcare. We therefore suggest that the examination of EBCD as a transformative process of redefinition of relationships-in/and-space is a promising and exciting interdisciplinary trajectory for human geography and applied healthcare research.
Funding
This paper presents independent research funded by the National Institute for Health Research (NIHR) under its Health Services and Delivery Research (HS&DR) Programme (Grant Reference Number: NIHR –HS&DR Programme (13–11/495). The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Declaration of competing interest
GR teaches on the EBCD training courses run by ‘The Point of Care Foundation’ in London and is one of the originators of EBCD.
Acknowledgements
The authors acknowledge the contribution of the stroke survivors, family members, stroke unit staff, volunteers, hospital managers and local community groups and the support for the study in the participating NHS Foundation Trust. We also wish to acknowledge colleagues who supported elements of the CREATE study, these include Dr Tino Kulnik who conducted pre-implementation interviews, Dr Alessia Costa (AC), supported ethnographic fieldwork and Dr Carole Pound, supported co-design events.
References
- Askim T., Bernhardt J., Salvesen O., Indredavik B. Physical activity early after stroke and its association to functional outcome 3 months later. J. Stroke Cerebrovasc. Dis. 2014;23:e305–312. doi: 10.1016/j.jstrokecerebrovasdis.2013.12.011. [DOI] [PubMed] [Google Scholar]
- Atkinson S., Robson M. Arts and health as a practice of liminality: Managing the spaces of transformation for social and emotional wellbeing with primary school children. Health Place. 2012;18:1348–1355. doi: 10.1016/j.healthplace.2012.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bate P., Robert G. Experience-based design: from redesigning the system around the patient to co-designing services with the patient. Qual. Saf. Health Care. 2006;15:307–310. doi: 10.1136/qshc.2005.016527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baum F., MacDougall C., Smith D. Participatory action research. J. Epidemiol. Community Health. 2006;60:854–857. doi: 10.1136/jech.2004.028662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen S., McSeveny K., Lockley E., Wolstenholme D., Cobb M., Dearden A. How was it for you? Experiences of participatory design in the UK health service. CoDesign. 2013;9:230–246. doi: 10.1080/15710882.2013.846384. [DOI] [Google Scholar]
- Bridges J., May C., Fuller A., Griffiths P., Wigley W., Gould L., Barker H., Libberton P. Optimising impact and sustainability: a qualitative process evaluation of a complex intervention targeted at compassionate care. BMJ Qual. Saf. 2017;26:970–977. doi: 10.1136/bmjqs-2017-006702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke D., Jones F., Harris R., Robert G. What outcomes are associated with developing and implementing co-produced interventions in acute healthcare settings? A rapid evidence synthesis. BMJ Open. 2017;7 doi: 10.1136/bmjopen-2016-014650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa A., Jones F., Kulnik S.T., Clarke D., Honey S., Robert G. Doing nothing? An ethnography of patients' (In)activity on an acute stroke unit. Health (London) 1363459320969784. 2021. [DOI] [PMC free article] [PubMed]
- Cottam H., Leadbeater C. RED paper 01 – health: Co-creating services. London: Design council. 2004. http://www.hilarycottam.com/wp-content/uploads/2010/01/RED_Paper-01-Health_Co-creating_services.pdf [WWW Document]. URL Available at: accessed 8.26.2021.
- Curtis S., Gesler W., Fabian K., Francis S., Priebe S. Therapeutic landscapes in hospital design: A qualitative assessment by staff and service users of the design of a new mental health inpatient unit. Environ. Plann. C Govern. Pol. 2007;25:591–610. doi: 10.1068/c1312r. [DOI] [Google Scholar]
- Donetto S., Pierri P., Tsianakas V., Robert G. Experience-based Co-design and healthcare improvement: Realizing participatory design in the public sector. Des. J. 2015;18:227–248. doi: 10.2752/175630615X14212498964312. [DOI] [Google Scholar]
- Donetto S., Pierri P., Tsianakas V., Robert G. Experience-based Co-design and healthcare improvement: Realizing participatory design in the public sector. Des. J. 2015;18:227–248. doi: 10.2752/175630615X14212498964312. [DOI] [Google Scholar]
- Farr M. Power dynamics and collaborative mechanisms in co-production and co-design processes. Crit. Soc. Pol. 2018;38:623–644. doi: 10.1177/0261018317747444. [DOI] [Google Scholar]
- Filipe A., Renedo A., Marston C. The co-production of what? Knowledge, values, and social relations in health care. PLoS Biol. 2017;15 doi: 10.1371/journal.pbio.2001403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilson L. Trust and the development of health care as a social institution. Soc. Sci. Med. 2003;56:1453–1468. doi: 10.1016/s0277-9536(02)00142-9. [DOI] [PubMed] [Google Scholar]
- Howes D., editor. Empire of the Senses: the Sensual Culture Reader. Sensory formations series. Berg; Oxford ; New York: 2005. [Google Scholar]
- Iedema R., Merrick E., Piper D., Britton K., Gray J., Verma R., Manning N. Codesigning as a discursive practice in emergency health services: The architecture of deliberation. J. Appl. Behav. Sci. 2010;46(1):73–91. doi: 10.1177/0021886309357544. [DOI] [Google Scholar]
- Intercollegiate, Stroke Working Party . fifth ed. Royal College of Physicians; 2016. National Clinical Guideline for Stroke. [Google Scholar]
- Intercollegiate Working Party for Stroke . Royal College of Physicians; London: 2012. National Guidelines for Stroke. [Google Scholar]
- Janssen H., Ada L., Bernhardt J., McElduff P., Pollack M., Nilsson M., Spratt N. Physical, cognitive and social activity levels of stroke patients undergoing rehabilitation within a mixed rehabilitation unit. Clin. Rehabil. 2014;28:91–101. doi: 10.1177/0269215512466252. [DOI] [PubMed] [Google Scholar]
- Janssen H., Ada L., Bernhardt J., McElduff P., Pollack M., Nilsson M., Spratt N.J. An enriched environment increases activity in stroke patients undergoing rehabilitation in a mixed rehabilitation unit: a pilot non-randomized controlled trial. Disabil. Rehabil. 2014;36:255–262. doi: 10.3109/09638288.2013.788218. [DOI] [PubMed] [Google Scholar]
- Jones F., Gombert K., Honey S., Cloud G., Harris R., Macdonald A., McKevitt C., Robert G., Clarke D. Addressing inactivity after stroke: The collaborative rehabilitation in Acute stroke (CREATE) study. Int. J. Stroke. 2021;16:669–682. doi: 10.1177/1747493020969367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones F., Gombert-Waldron K., Honey S., Cloud G., Harris R., Macdonald A., McKevitt C., Robert G., Clarke D. NIHR Journals Library; Southampton (UK): 2020. Using Co-production to Increase Activity in Acute Stroke Units: the CREATE Mixed-Methods Study, Health Services and Delivery Research. [PubMed] [Google Scholar]
- Kearns R., Andrews G. Routledge International Handbook of Critical Issues in Health and Illness. Taylor and Francis; 2021. Place in health, illness and healthcare; p. 306. [Google Scholar]
- Liaschenko J. The moral geography of home care. Adv. Nurs. Sci. 1994;17:16–26. doi: 10.1097/00012272-199412000-00005. [DOI] [PubMed] [Google Scholar]
- Little M., Jordens C.F., Paul K., Montgomery K., Philipson B. Liminality: a major category of the experience of cancer illness. Soc. Sci. Med. 1998;47:1485–1494. doi: 10.1016/s0277-9536(98)00248-2. [DOI] [PubMed] [Google Scholar]
- Lohse K.R., Lang C.E., Boyd L.A. Is more better? Using metadata to explore dose-response relationships in stroke rehabilitation. Stroke. 2014;45:2053–2058. doi: 10.1161/STROKEAHA.114.004695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meroni A., Sangiorgi D. Gower; Farnham: 2011. Design for Services, Design for Social Responsibility Series. [Google Scholar]
- Olaveson T. Collective effervescence and communitas: Processual Models of ritual and society in emile durkheim and victor Turner. Dialect. Anthropol. 2001;26:89–124. doi: 10.1023/A:1020447706406. [DOI] [Google Scholar]
- Palmer V.J., Weavell W., Callander R., Piper D., Richard L., Maher L., Boyd H., Herrman H., Furler J., Gunn J., Iedema R., Robert G. The Participatory Zeitgeist: an explanatory theoretical model of change in an era of coproduction and codesign in healthcare improvement. Med. Humanit. 2019;45:247–257. doi: 10.1136/medhum-2017-011398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robert G. In: Understanding and Using Health Experiences. Ziebland S., Coulter A., Calabrese J.D., Locock L., editors. Oxford University Press; 2013. Participatory action research: using experience-based co-design to improve the quality of healthcare services; pp. 138–149. [DOI] [Google Scholar]
- Robert G., Donetto S., Williams O. In: The Palgrave Handbook of Co-production of Public Services and Outcomes. Loeffler E., Bovaird T., editors. Springer International Publishing; Cham: 2021. Co-designing healthcare services with patients; pp. 313–333. [DOI] [Google Scholar]
- Rosbergen I.C., Grimley R.S., Hayward K.S., Walker K.C., Rowley D., Campbell A.M., McGufficke S., Robertson S.T., Trinder J., Janssen H., Brauer S.G. Embedding an enriched environment in an acute stroke unit increases activity in people with stroke: a controlled before-after pilot study. Clin. Rehabil. 2017;31:1516–1528. doi: 10.1177/0269215517705181. [DOI] [PubMed] [Google Scholar]
- Sangiorgi D., Prendiville A., editors. Designing for Service: Key Issues and New Directions. Bloomsbury Publishing Plc; 2017. [DOI] [Google Scholar]
- Soderlund Jonas, Borg Elizabeth. Liminality in management and organization studies: process, position and place. Int. J. Manag. Rev. 2018;20(4):880–902. doi: 10.1111/ijmr.12168. [DOI] [Google Scholar]
- Stroke Association . Stroke Association; 2018. State of the Nation Stroke Statistics.https://www.stroke.org.uk/what-is-stroke/stroke-statistics [Google Scholar]
- Taylor, E., Jones, F., McKevitt, C., n.d. Influencing rehabilitation in inpatient stroke units in the UK? An ethnographic. BMJ Open 8. [DOI] [PMC free article] [PubMed]
- Turner V. Cornell University Press; Ithaca and London: 1967. The Forest of Symbols: Aspects of Ndembu Ritual. [Google Scholar]
- Turner V.W. Cornell University Press; Ithaca, N.Y: 1977. The Ritual Process: Structure and Anti-structure, Symbol, Myth, and Ritual Series. [Google Scholar]
- Turner V.W. Cornell University Press; Ithaca, N.Y: 1977. The Ritual Process: Structure and Anti-structure, Symbol, Myth, and Ritual Series. [Google Scholar]
- Turner V.W. Cornell University Press; Ithaca, N.Y: 1969. The Ritual Process: Structure and Anti-structure, Symbol, Myth, and Ritual Series. [Google Scholar]
- Van Gennep, Arnold . Routledge and Kegan Paul; London: 1960. The Rites of Passage. London. [Google Scholar]