Abstract
Background
The purpose of this systematic review was to (1) define the cumulative humerus fracture rate after BT and (2) compare how often fracture rate was reported compared to other complications.
Methods
A systematic review was performed using the PRISMA guidelines.
Results
39 studies reported complications and 30 reported no complications. Of the 39 studies that reported complications, 5 studies reported fracture after BT (n = 669, cumulative incidence of 0.53%). The overall non-fracture complication rate was 12.9%.
Discussion
Due to the relatively high incidence of fracture, surgeons should ensure that this complication is disclosed to patients undergoing BT.
Keywords: Biceps tenodesis, Humeral fracture, Adhesive capsulitis, Shoulder dislocation, Complications, Shoulder
1. Introduction
Biceps tenodesis (BT) is a commonly utilized procedure, with annual cases performed significantly increasing from 2007 to 2011.1, 2, 3 This procedure can be used to treat a variety of pathologies including biceps tenosynovitis, bicipital rupture, Superior Labral Anterior Posterior (SLAP) tears, and is often used in conjunction with other shoulder procedures, such as rotator cuff repairs (RCR).3 Complications after BT have been reported to occur in 2–13% of cases and include wound healing issues, wound infection, hematoma/seroma formation, nerve injury in addition to anterior shoulder pain, weakness, cramping.4, 5, 6 One potential rare but devastating complication after BT is humeral fracture, and this has been reported in the literature in both case reports7, 8, 9, 10 and larger studies.4,11
Prior biomechanical studies have suggested that the risk of fracture could be due to a decrease in humeral resistance secondary to torsional stress applied after a tenodesis hole is drilled. In a subpectoral approach, specifically, drilling in the metaphyseal-diaphyseal bone may act as a stress riser.12,13 An early study by Edergton et al. suggested that bone defects greater than 20% resulted in a 34% or greater reduction in torsional strength.14 Furthermore, more recent studies have found that drilling an 8-mm unicortical hole can reduce torsional strength by 20–30%.12,13 However, while increasing the size of the hole may result in torsional strength reduction, the type of fixation utilized likely has a minimal effect.15 A prior study by Euler et al. also suggested that laterally eccentric malpositioning of the tenodesis was associated with increased humeral fracture risk.16
Given the case reports on humeral fracture as a complication after BT in the literature, as well as the potential devastating sequelae including the necessity of revision surgery, the primary goals of this systematic review were to 1) determine the cumulative rate of fracture after BT and 2) define how frequently postoperative humeral fracture is reported as a complication compared to other complications after BT. A secondary goal was to qualitatively evaluate fracture rate and its relationship to intraoperative factors including BT approach (e.g., arthroscopic vs open, and subpectoral versus suprapectoral) and fixation (e.g., button, suture anchor, interference screw). Due to the scarcity of reports and low percentage reported in the literature, we hypothesized that fractures rarely occur after BT and are less frequent than many other complications including adhesive capsulitis, wound complications, dislocation, and Popeye deformity. In addition, we hypothesized that a subpectoral approach and advanced age may be associated with higher fracture rates.
2. Materials and methods
2.1. Search strategy
A systematic review was performed based on the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines. PubMed, Embase, and CINAHL were queried from the inception of databases to January 6, 2021 using the following search strategy: (“biceps tenodesis”) AND (“complications” OR “outcomes” OR “fracture”).
2.2. Study selection
Titles, abstracts, and full texts of studies were screened by 2 independent reviewers (*initials blinded for review*). Discussion between the reviewers took place to resolve conflicts. If no consensus was reached the decision was deferred to the senior author (WRA – blind). Articles were included if they were original studies reporting clinical outcomes and complications after a biceps tenodesis (BT). Studies with multiple cohorts (that included a BT cohort) and studies that reported on BT with concomitant procedures were included. If a study contained multiple cohorts, only the BT group was included in pooled analysis. Studies were excluded for the following causes: (1) non-clinical basic science studies; (2) cadaveric studies; (3) animal studies; (4) expert opinions or level V evidence; (5) systematic reviews or meta-analyses; (6) concomitant total shoulder arthroplasty (TSA); (7) preexisting humeral fracture; (8) Popeye deformities as the only complications reported; (9) studies with less than 5 patients; (10) revision studies; (11) non-English publications; (12) abstracts, comments, letters, or editorials; (13) non-osseous BT (e.g., fixation to the pectoralis major tendon); and (14) surgical technique articles without outcomes.
Some of the studies that met the inclusion and exclusion criteria were performed using large private and/or public databases.6,11,17, 18, 19, 20, 21, 22 The databases included American Board of Orthopaedic Surgery (ABOS),6,22 Military Health System Data Repository,11 American College of Surgeons National Surgical Quality Improvement Program (NSQIP),18 MarketScan (IBM, Armonk, NY, USA),19 Humana Patient Records Database queried through PearlDiver (Colorado Springs, CO, USA)),17,21 and Medicare queried through PearlDiver.20 Three sets of studies investigated sets of overlapping patients. Both Erickson et al. and Xiao et al. reported on complication rates in the Humana Patient Records Database.17,21 Xiao et al. included patients from 2007 to 2017, while Erickson et al. included patients from 2007 to 2014. Due to this overlap, only the study by Xiao et al. was included in our analysis because of its longer study timespan. Similarly, Shin et al. and Yeung et al. both reported on the ABOS database from the years 2012–2016.6,22 Due to overlap only one study could be included to prevent redundancy. Based on the methods employed, the study by Yeung et al. was included in final analysis. Lastly, two studies both by Werner et al. met all inclusion and exclusion criteria.23,24 However, due to overlapping time periods (2007–2011), only the study with the larger sample size was included.24
2.3. Data extraction
Data from the included studies were extracted using the DistillerSR platform (Evidence Partners, Ontario, Canada) and was performed by a single reviewer (*initials blinded for review*). Extracted data included study design, number of patients, diagnosis, type of BT, fixation technique, fixation location, concomitant procedures, complications, complication rates, fracture rates, BT failure rates, time of complication (intra- or post-operative), final follow-up duration, and level of evidence. The definition of failure after BT varied between studies but included: clinical observation of distal retraction of the muscle belly,25 loss of proximal fixation,26 residual anterior arm pain,27 partial slippage of the LHB tendon from the site of proximal fixation after a fall, failure of the proximal biceps at the musculotendinous junction,28 and bad tendon tissue quality and degenerative changes during refixation.29 Extracted data was tabulated and analyzed in Microsoft Excel (Microsoft, Redmond, WA, USA). The complication data was pooled to report fracture and other complication rates.
3. Results
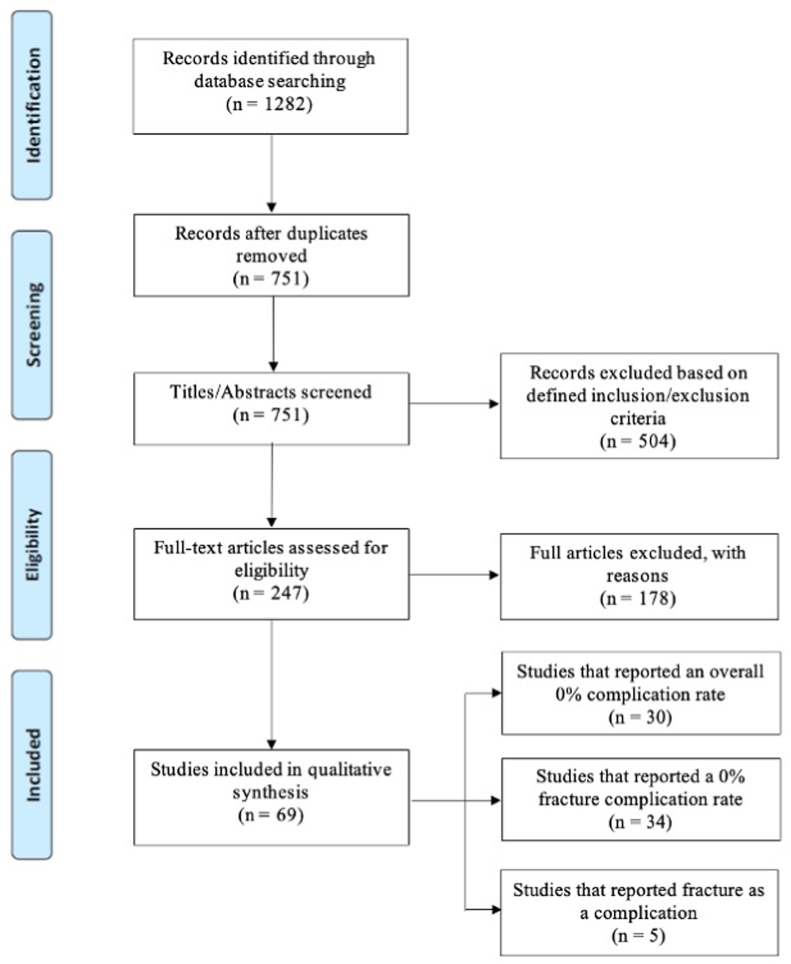
A search of PubMed, Embase, and CINAHL databases yielded 1282 studies (Fig. 1). After duplicates were removed, 751 studies underwent title and abstract review via DistillerSR software. Of these 504 were excluded and 247 studies underwent full text review. A total of 178 studies were excluded; thus, 69 studies with a total of n = 125,484 patients, were included in our assessment (Table 1).
Fig. 1.
PRISMA flow chart.
Table 1.
List of included studies including the rate of complications reported following biceps tenodesis.
| Author | Title | Complications (%) |
|---|---|---|
| Abtahi et al.30 | Complications after subpectoral biceps tenodesis using a dual suture anchor technique. | 7 (7%) |
| Baron et al.31 | Clinical Outcomes of Open Subpectoral Biceps Tenodesis with Cortical Button Fixation. | 2 (3.2%) |
| Baumgarten et al.32 | Patient-determined outcomes after arthroscopic rotator cuff repair with and without biceps tenodesis utilizing the PITT technique. | 1 (1.3%) |
| Belay et al.33 | Biceps tenotomy has earlier pain relief compared to biceps tenodesis: a randomized prospective study. | 3 (21%) |
| Berlemann et al.34 | Tenodesis of the long head of biceps brachii in the painful shoulder: improving results in the long term. | 3 (21%) |
| Boileau et al.35 | Arthroscopic treatment of isolated type II SLAP lesions: biceps tenodesis as an alternative to reinsertion. | 0 (0%) |
| Boileau et al.36 | Isolated arthroscopic biceps tenotomy or tenodesis improves symptoms in patients with massive irreparable rotator cuff tears. | 8 (24%) |
| Boileau et al.25 | Arthroscopic biceps tenodesis: a new technique using bioabsorbable interference screw fixation. | 2 (4.3%) |
| Brady et al.37 | Arthroscopic proximal biceps tenodesis at the articular margin: evaluation of outcomes, complications, and revision rate. | 42 (3.6%) |
| Castricini et al.38 | Tenodesis is not superior to tenotomy in the treatment of the long head of biceps tendon lesions. | 8 (12.5%) |
| Cook et al.39 | Low incidence of failure after proximal biceps tenodesis with unicortical suture button. | 7 (4.8%) |
| Denard et al.40 | Arthroscopic biceps tenodesis compared with repair of isolated type II SLAP lesions in patients older than 35 years. | 0 (0%) |
| Duchman et al.26 | Open Versus Arthroscopic Biceps Tenodesis: A Comparison of Functional Outcomes. | 1 (2.2%) |
| Duerr et al.41 | Clinical Evaluation of an Arthroscopic Knotless Suprapectoral Biceps Tenodesis Technique: Loop ‘n' Tack Tenodesis | 0 (0%) |
| Dunne et al.42 | Arthroscopic treatment of type II superior labral anterior to posterior (SLAP) lesions in a younger population: minimum 2-year outcomes are similar between SLAP repair and biceps tenodesis. | 1 (5%) |
| Ek et al.43 | Surgical treatment of isolated type II superior labrum anterior-posterior (SLAP) lesions: repair versus biceps tenodesis. | 1 (6.6%) |
| Euler et al.44 | Chronic rupture of the long head of the biceps tendon: comparison of 2-year results following primary versus revision open subpectoral biceps tenodesis. | 0 (0%) |
| Fang et al.45 | Lesions of the Long Head of the Biceps Tendon Concomitant with Rotator Cuff Tears: Tenotomy or Subpectoral Mini-open Tenodesis? A Comparative Short to Mid-term Follow-up Study. | 0 (0%) |
| Faruqui et al.27 | The modified Norwegian method of biceps tenodesis: how well does it work? | 5 (6.7%) |
| Forsythe et al.46 | Arthroscopic Suprapectoral and Open Subpectoral Biceps Tenodeses Produce Similar Outcomes: A Randomized Prospective Analysis. | 0 (0%) |
| Franceschetti et al.47 | The management of the long head of the biceps in rotator cuff repair: A comparative study of high vs. subpectoral tenodesis. | 0 (0%) |
| Franceschi et al.48 | To detach the long head of the biceps tendon after tenodesis or not: outcome analysis at the 4-year follow-up of two different techniques | 0 (0%) |
| Gombera et al.49 | All-arthroscopic suprapectoral versus open subpectoral tenodesis of the long head of the biceps brachii. | 2 (4.3%) |
| Gottschalk et al.50 | Subpectoral Biceps Tenodesis For the Treatment Of Type Two And Four Slap Lesions. | 5 (13%) |
| Gowd et al.18 | Open Biceps Tenodesis Associated with Slightly Greater Rate of 30-Day Complications Than Arthroscopic: A Propensity-Matched Analysis. | 80 (1.26%) |
| Gumina et al.51 | Rupture of the long head biceps tendon treated with tenodesis to the coracoid process. Results at more than 30 years. | 0 (0%) |
| Gupta et al.52 | Subpectoral biceps tenodesis for bicipital tendonitis with SLAP tear | 0 (0%) |
| Haidamous et al.53 | Arthroscopic Biceps Tenodesis Outcomes: A Comparison of Inlay and Onlay Techniques. | 4 (4.4%) |
| Hodgins et al.54 | Arthroscopic Suprapectoral and Open Subpectoral Biceps Tenodesis: Radiographic Characteristics. | 0 (0%) |
| Hufeland et al.55 | The influence of suprapectoral arthroscopic biceps tenodesis for isolated biceps lesions on elbow flexion force and clinical outcomes. | 0 (0%) |
| Jacxsens et al.56 | Clinical and sonographic evaluation of subpectoral biceps tenodesis with a dual suture anchor technique demonstrates improved outcomes and a low failure rate at a minimum 2-year follow-up. | 0 (0%) |
| Javed et al.57 | Subpectoral biceps tenodesis using a novel anterior cortical button technique. | 0 (0%) |
| Kany et al.58 | The keyhole technique for arthroscopic tenodesis of the long head of the biceps tendon. In vivo prospective study with a radio-opaque marker. | 0 (0%) |
| Kany et al.59 | Biceps tenodesis (long head): arthroscopic keyhole technique versus arthroscopic interference screw: a prospective comparative clinical and radiographic marker study. | 0 (0%) |
| Kathenberg et al.60 | Clinical and Biomechanical Evaluation of an All-Arthroscopic Suprapectoral Biceps Tenodesis. | 0 (0%) |
| Kim et al.61 | Long Head of the Biceps Tendon Tenotomy versus Subpectoral Tenodesis in Rotator Cuff Repair. | 0 (0%) |
| Kreines et al.62 | Outcomes of Arthroscopic Biceps Tenodesis for the Treatment of Failed Type II SLAP Repair: A Minimum 2-Year Follow-Up. | 2 (7.7%) |
| Liechti et al.28 | Immediate physical therapy without postoperative restrictions following open subpectoral biceps tenodesis: low failure rates and improved outcomes at a minimum 2-year follow-up. | 2 (2.2%) |
| Lim et al.63 | Comparison between SLAP Repair and Biceps Tenodesis with Concomitant Rotator Cuff Repair in Patients Older than 45 Years: Minimum 2-Year Clinical and Imaging Outcomes. | 3 (11.1%) |
| Lutton et al.64 | Where to tenodese the biceps: proximal or distal? | 0 (0%) |
| MacDonald et al.65 | Biceps Tenodesis Versus Tenotomy in the Treatment of Lesions of the Long Head of the Biceps Tendon in Patients Undergoing Arthroscopic Shoulder Surgery: A Prospective Double-Blinded Randomized Controlled Trial. | 0 (0%) |
| Maghpara et al.66 | Clinical Outcomes of an All-Arthroscopic Biceps Tenodesis Using the Anterolateral Anchor During Concomitant Double-Row Rotator Cuff Repair. | 0 (0%) |
| McCrum et al.4 | Complications of biceps tenodesis based on location, fixation, and indication: a review of 1526 shoulders. | 373 (24.4%) |
| McMahon et al.67 | Outcomes of tenodesis of the long head of the biceps tendon more than three months after rupture | 0 (0%) |
| Millett et al.68 | Interference screw vs. suture anchor fixation for open subpectoral biceps tenodesis: does it matter? | 0 (0%) |
| Ng et al.69 | Symptomatic chronic long head of biceps rupture: Surgical results. | 0 (0%) |
| Nho et al.5 | Complications associated with subpectoral biceps tenodesis: low rates of incidence following surgery. | 7 (2%) |
| Nho et al.70 | Arthroscopic repair of anterosuperior rotator cuff tears combined with open biceps tenodesis. | 0 (0%) |
| Overmann et al.11 | Incidence and Characteristics of Humeral Shaft Fractures After Subpectoral Biceps Tenodesis. | 12 (<0.1%) |
| Parisien et al.20 | Increased Risk of Humeral Fracture with Open Versus Arthroscopic Tenodesis of the Long Head of the Biceps Brachii. | 643 (1.19%) |
| Paulos et al.71 | A novel approach to arthroscopic biceps tenodesis | 0 (0%) |
| Peebles et al.72 | Conversion of Failed Proximal Long Head of the Biceps Tenodesis to Distal Subpectoral Tenodesis: Outcomes in an Active Population. | 0 (0%) |
| Perry et al.73 | Biceps Tenodesis and Intra-articular Decompression for Treatment of Superior Labral Tear from Anterior to Posterior and Associated Paralabral Cyst in Active Duty Military. | 0 (0%) |
| Provencher et al.74 | Outcomes of primary biceps sub-pectoral tenodesis in an active population: A prospective evaluation of 101 patients. | 8 (8%) |
| Rhee et al.75 | Double on-lay fixation using all suture-type anchor for subpectoral biceps tenodesis has favorable functional outcomes and leads to less cosmetic deformities than single on-lay fixation. | 0 (0%) |
| Sasaki et al.76 | Arthroscopic tenodesis using a bioabsorbable interference screw and soft anchor: A case series of 60 patients. | 0 (0%) |
| Schoch et al.29 | Suprapectoral biceps tenodesis using a suture plate: clinical results after 2 years. | 2 (4%) |
| Schrock et al.77 | Comparison of Clinical Failure Rates After 2 Techniques of Subpectoral Mini-Open Biceps Tenodesis: Sequence and Suture Passage Technique Matter | 16 (9.8%) |
| Schroder et al.78 | Sham surgery versus labral repair or biceps tenodesis for type II SLAP lesions of the shoulder: a three-armed randomised clinical trial | 10 (25.6%) |
| Shen et al.79 | Arthroscopic tenodesis through positioning portals to treat proximal lesions of the biceps tendon. | 1 (2%) |
| Tu et al.80 | Open subpectoral vs. arthroscopic proximal biceps tenodesis: A comparison study of clinical outcomes. | 14 (12%) |
| Varshneya et al.19 | Costs, Complications, and Reoperations Associated with Primary Arthroscopic Rotator Cuff Repair With or Without Acromioplasty and/or Biceps Tenodesis. | 4702 (16.1%) |
| Voss et al.81 | Open subpectoral biceps tenodesis in patients over 65 does not result in an increased rate of complications | 19 (5.6%) |
| Werner et al.24 | Increased incidence of postoperative stiffness after arthroscopic compared with open biceps tenodesis. | 27 (10.8%) |
| Xiao et al.21 | Increased reoperation rates among patients undergoing shoulder arthroscopy with concomitant biceps tenodesis | 885 (8.2%) |
| Yeung et al.6 | Complications of Arthroscopic Versus Open Biceps Tenodesis in the Setting of Arthroscopic Rotator Cuff Repairs: An Analysis of the American Board of Orthopaedic Surgery Database. | Arthroscopic (11.4%) |
| Open (13.1%) | ||
| Yi et al.82 | Small-incision open distal subpectoral vs. arthroscopic proximal biceps tenodesis for biceps long head tendon lesions with repair of rotator cuff tears. | 7 (9.8%) |
| Yi et al.83 | Arthroscopic proximal versus open subpectoral biceps tenodesis with arthroscopic repair of small- or medium-sized rotator cuff tears. | 5 (7.5%) |
| Zhang et al.84 | Tenotomy or tenodesis for long head biceps lesions in shoulders with reparable rotator cuff tears: a prospective randomised trial. | 7 (9.5%) |
Complication rates, postoperative follow-up times, type of fixation, approach, technique concomitant procedures and complication types are included in Table 2. Of the total of 69 papers (n = 125,484 patients), 39 studies reported complications following BT (total n = 124,144 patients; mean per study: 3183 ± 9980.4) and 30 studies (total n = 1340 patients; mean per study: 44.7 ± 44.4) reported a complication rate of 0% complications following BT. For the 39 studies that reported complications following BT, the average follow-up time was 26.2 ± 15.9 months. For the 69 included studies, the cumulative non-fracture complication rate was 12.9% (7257 complications in 56,315 patients). Of note, Xiao et al. did not report complication rates, but did report specific complications (acute kidney injury, UTI, capsulitis, nerve injury, and dislocation),21 and Yeung et al.’s database study did not include a follow-up period.6 In addition, two studies11,20 (n = 69,169 patients) only reported on fracture as a complication after BT. These large database studies, therefore, were included in calculating the cumulative rate of BT but were excluded from the pooled complication analysis as they did not report on any other complications and could significantly skew those findings.
Table 2.
Detailed table regarding studies included, specifically the list of complications.
| Author | Study Type | Pre-operative Diagnosis/Symptoms | N (Total Patients) | Total Complications | Postoperative F/U | Type of Fixation | Approach | Technique | Concomitant Procedures | Complications |
|---|---|---|---|---|---|---|---|---|---|---|
| Abtahi et al.30 | Level IV: Case Series | Biceps tendonitis, Superior labral tears, Biceps tendon subluxation, Biceps tendon partial tears | 103 | 7 (7%) | 7 months | Dual suture anchor | Subpectoral | Open | Arthroscopic subacromial/glenohumeral debridement arthroscopic RCR distal clavicle excision | Superficial wound infections (4) |
| Temporary nerve palsies from Interscalene block (2) | ||||||||||
| Pulmonary embolism (1) | ||||||||||
| Baron et al.31 | Level II: Retrospective | N/A | 61 | 2 (3.2%) | 42.2 months | Cortical button | Subpectoral | Open | Subacromial decompression | Transient sensory neuropathy (2) |
| Labral debridement | ||||||||||
| Distal clavicle resection | ||||||||||
| RCR | ||||||||||
| Labral repair Loose body removal | ||||||||||
| Baumgarten et al.32 | Level III: Retrospective | Partial long head Biceps tendon tear, Biceps instability/subluxation | 131 | 1 (1.3%) | 3.6 years | Intra-articular trans-tendon | Intra-articular | Arthroscopic | RCR | Revision RCR (1) |
| Lysis of adhesions (1) | ||||||||||
| Belay et al.335 | Level II: Prospective | Tendinopathy | 14 | 3 (21%) | 2 years | Interference screw | Humerus | Arthroscopic | RCR | Rupture (1), |
| Adhesive capsulitis (1) | ||||||||||
| Popeye (1) | ||||||||||
| Berlemann et al.34 | Level III: Case Series | Rupture, Impingement, Tendinitis | 14 | 3 (21%) | 7 years | N/A | Keyhole | N/A | Rotator cuff decompression | PE (1) |
| Rupture (2) | ||||||||||
| Boileau et al.36 | Level III: Retrospective | Rotator cuff tear, Tenosynovitis, Delamination, Pre-rupture | 33 | 8 (24%) | 35 months | Interference screw | Intra-articular | Arthroscopic | None | Pseudoparalysis of the shoulder (3) |
| Glenohumeral osteoarthritis (2) | ||||||||||
| Reflex sympathetic dystrophy (1) | ||||||||||
| Continued pain (2) | ||||||||||
| Boileau et al.25 | Level II Prospective | Tenosynovitis, Pre-rupture, Subluxation | 43 | 2 (4.3%) | 17 months | Interference Screw | Intra-articular | Arthroscopic | RCR | Failure (2) |
| Brady et al.37 | Level IV Case Series | Tendinopathy, Tear, Subluxation | 1083 | 42 (3.6%) | 136 weeks | Interference screw | Articular margin | Arthroscopic | Arthroscopic RCR Subacromial decompression Acromioplasty Labral repair Coracoplasty | Adhesive capsulitis (20) |
| Recurrent rotator cuff tears (13) | ||||||||||
| Biceps tendon ruptures (3) | ||||||||||
| Persistent pain (6) | ||||||||||
| Castricini et al.38 | Level I Prospective | Tenosynovitis, Subluxation, Dislocation, Partial rupture of the tendon | 24 | 8 (12.5%) | 24 months | Interference screw | N/A | Arthroscopic | Supraspinatus tear | Cramping (3) |
| Popeye deformity (5) | ||||||||||
| Cook et al.39 | Level III Retrospective | Longitudinal tear of the biceps tendon, SLAP | 145 | 7 (4.8%) | 6.9 months | Button | Subpectoral | Open | Labral repair Repair of the upper subscapularis tendon | Failure (1) |
| Mild asymmetry of the biceps (1) | ||||||||||
| Chronic pain in the posterior shoulder (2) | ||||||||||
| Postoperative hematoma (1) | ||||||||||
| Button found not to be fully flipped and seated on the intramedullary portion of the anterior humeral cortex (1) | ||||||||||
| Superficial wound infection (1) | ||||||||||
| Duchman et al.26 | Level IV Other | Biceps tendonitis, Tendinopathy, Instability, SLAP tear | 45 | 1 (2.2%) | 3.2 years | Interference screw | Arthroscopic Suprapectoral | Arthroscopic Suprapectoral | RCR | Failure (1) |
| Open Subpectoral | Open Subpectoral | Labral repair Subacromial decompression | ||||||||
| Dunne et al.42 | Level III Retrospective | SLAP | 20 | 1 (5%) | 3.4 years | Interference screw | Suprapectoral | Arthroscopic | Subacromial bursectomy Partial rotator cuff tears | Infection (1) |
| Ek et al.43 | Level III Retrospective | SLAP | 15 | 1 (6.6%) | 31 months | Anchor | Subpectoral | Arthroscopic | Subacromial decompression | Failure (1) |
| Faruqui et al.27 | Level IV Retrospective | Subluxation, SLAP | 75 | 5 (6.7%) | 3.9 years | Anchor | Intra-articular | Arthroscopic | Subscapularis, supraspinatus, and infraspinatus tendon repairs | Rupture (2) |
| Failure (3) | ||||||||||
| Gombera et al.49 | Level III Other | Tear of the biceps tendon, Subluxation | 46 | 2 (4.3%) | 30.1 months | Interference screw | Arthroscopic suprapectoral (23) | Arthroscopic suprapectoral (23) | None | Open: Plexopathy (1) |
| Open subpectoral (23) | Open subpectoral (23) | Superficial erythema scope (1) | ||||||||
| Gottschalk et al.50 | Level IV Case Series | SLAP | 23 | 5 (13%) | 40.2 months | Interference screw | Subpectoral | Arthroscopic | Subacromial decompression | Infection (2) |
| Acromioplasty Chondroplasty Arthroscopic Excision of the distal clavicle | Brachial plexus neurapraxia (1) Rupture (1) | |||||||||
| Debridement of the rotator cuff | Failure (1) | |||||||||
| Gowd et al.18 | Case Series Retrospective | 6330 | 80 (1.26%) | 1 month | N/A | N/A | Open Arthroscopic | Subacromial decompression Distal clavicle excision SLAP Debridement | Open (50): | |
| Dehiscence (3) | ||||||||||
| Sepsis (1) | ||||||||||
| PE (6) | ||||||||||
| Myocardial infarction (3) | ||||||||||
| Transfusion (11) | ||||||||||
| DVT (2) | ||||||||||
| UTI (4) | ||||||||||
| Pneumonia (7) | ||||||||||
| Unplanned intubation (3) | ||||||||||
| Infection (15) | ||||||||||
| Return to operating room (16) | ||||||||||
| Arthroscopic (30): | ||||||||||
| Dehiscence (1) | ||||||||||
| PE (6) | ||||||||||
| Myocardial infarction (3) | ||||||||||
| DVT (3) | ||||||||||
| UTI (4) | ||||||||||
| Pneumonia (5) | ||||||||||
| Unplanned intubation (2) | ||||||||||
| Infection (9) | ||||||||||
| Return to operating room (10) | ||||||||||
| Haidamous et al.53 | Level III Other | Bicep lesion | 90 | 4 (4.4%) | 15.7 months | Interference screw, Anchor | N/A | Arthroscopic | RCR | Popeye deformity (2) |
| Stiffness (2) | ||||||||||
| Kreines et al.62 | Level IV Other | Failure of SLAP repair | 26 | 2 (7.7%) | Min two years | Interference screw | Intra-articular | Arthroscopic | None | 2 revisions: |
| Acromial fracture that occurred after a fall (1) | ||||||||||
| Atraumatic arthritis due to chondrolysis (1) | ||||||||||
| Liechti et al.28 | Level IV Case Series | Tendinitis, Tenosynovitis, Proximal biceps tendon tears without distal retraction, Degenerative SLAP tears | 98 | 2 (2.2%) | 3.5 years | Bicortical suture button and Interference screw | Subpectoral | Open | Intra-articular debridement | Failure (2) |
| Subacromial decompression Acromioplasty Distal clavicle excision | ||||||||||
| Lim et al.63 | Level III Retrospective | SLAP | 18 | 3 (11.1%) | 29.4 months | Interference screw | N/A | Arthroscopic | RCR | Retear of rotator cuff (2) |
| Popeye (1) | ||||||||||
| McCrum et al.4 | Level III Retrospective | Partial tears, Subluxation, or Dislocation | 1526 | 373 (24.4%) | 10.8 months | Subpectoral (Out of Groove): Soft-tissue tenodesis (209) Anchor (96) Unicortical button (143) Bicortical button only (11) Bicortical button and screw (92) Tenodesis screw only (439) Keyhole (6) Suprapectoral (In Groove): Soft-tissue tenodesis (144) Anchor (239), Tenodesis screw only (143) Unicortical button (2) Bicortical button only (2) | Subpectoral (996) Suprapectoral (530) | Arthroscopic Open | RCR Labral repair SLAP repair | Soft tissue: |
| Cramping (6) | ||||||||||
| Popeye deformity (15) weakness (30) | ||||||||||
| Implant: | ||||||||||
| Cramping (26) | ||||||||||
| Popeye deformity (56) | ||||||||||
| Weakness (46) | ||||||||||
| Subpectoral (Out of Groove) | ||||||||||
| Cramping (23) | ||||||||||
| Popeye deformity (46) | ||||||||||
| Weakness (43) | ||||||||||
| Suprapectoral (In Groove) | ||||||||||
| Cramping (9) | ||||||||||
| Popeye deformity (25) | ||||||||||
| Weakness (33) | ||||||||||
| Nerve injury: | ||||||||||
| Subpectoral tenodesis screw (11) | ||||||||||
| Subpectoral bicortical button plus tenodesis screw (4) | ||||||||||
| Subpectoral unicortical button (2) | ||||||||||
| Anchor in rotator cuff repair (1) | ||||||||||
| Pulmonary emboli (2) | ||||||||||
| DVT (2) | ||||||||||
| Fracture (1) | ||||||||||
| Nho et al.5 | Level IV Case Series | Tenderness over the biceps and/or positive Speed's, O'Brien's, and Yergason's tests | 353 | 7 (2%) | 3 years | Interference screw | Subpectoral | Open | RCR | Pain (2) |
| Subacromial decompression | Infection (1) | |||||||||
| Capsular release Debridement Distal clavicle resection | Reflex sympathetic dystrophy (1) numbness (1) Popeye/failure (2) | |||||||||
| Overmann et al.11 | Level IV Case Series | SLAP teat | 15,085 | 12 (0.1%) | 9.4 months | Interference screw | Subpectoral | Arthroscopic Open | Distal clavicle excision | Humeral fracture (12) |
| Acromioclavicular joint arthritis | Bicortical button | Posterior labrum repair | ||||||||
| Posterior labrum tear | Suture anchor Unicortical button | Anterior labroligamentos periosteal sleeve avulsion | ||||||||
| Parisien et al.20 | Level III Retrospective | N/A | 54,084 | 643 (1.19%) | 12 months | N/A | N/A | N/A | N/A | Humeral fracture (643) |
| Provencher et al.74 | Level IV Case Series | Type II SLAP tear, Biceps tenosynovitis | 101 | 8 (8%) | 2.75 years | Interference screw | Subpectoral | Open | Partial rotator cuff tear | Infection (2) |
| Transient musculocutaneous neurapraxia (3) | ||||||||||
| Failure (3) | ||||||||||
| Schoch et al.29 | Level IV Case Series | Biceps tendinitis, Partial tears of the tendon, SLAP tears | 50 | 2 (4%) | 29.5 months | Button | Suprapectoral | Open | None | Failure (2) |
| Schrock et al.77 | Level III Other | N/A | 163 | 16 (9.8%) | 5.3 months | BirdBeak suture or free needle | Subpectoral | Open | RCR | Deformity (12) |
| Glenohumeral debridement | Pain (4) | |||||||||
| Schroder et al.78 | Level I Randomized Control Trial | SLAP | 39 | 10 (25.6%) | 2 years | Suture anchor | Low in the bicipital groove | Open | None | Capsulitis/stiffness (10) |
| Shen et al.79 | Level IV Case Series | Tendonitis, SLAP | 49 | 1 (2%) | 14 months | Suture anchor | Proximal | Arthroscopic | None | Persistent pain (1) |
| Tu et al.80 | Level III Retrospective | SLAP tears, Complete or partial tearing of the LHB, Tenosynovitis, LHB instability/subluxation, Associated small- or medium-sized rotator cuff tears | 117 | 14 (12%) | 20 months | Interference screw implant | Subpectoral, proximal | Arthroscopic Open | RCR | Open: |
| Open 3 (5.5%) | Stiffness (3) | |||||||||
| Arthroscopic | Arthroscopic: | |||||||||
| 11 (17.7%) | Stiffness (11) | |||||||||
| Varshneya et al.19 | Level IV Other | N/A | 29,203 | 4702 (16.1%) | 31.8 months | N/A | N/A | N/A | Acromioplasty | Capsulitis (4019) |
| Dislocation (568) | ||||||||||
| Infection (82) | ||||||||||
| Wound complication (33) | ||||||||||
| Hematoma (32) | ||||||||||
| Nerve injury (19) Thromboembolism (123) | ||||||||||
| Voss et al.81 | Level IV Case Series | N/A | 337 Over 65 y/o: (23) Under 65 y/o: (314) | 19 (5.6%) Over 65 y/o: 2 (8.7%) Under 65 y/o: 5.4% | 30 months | Interference screw | Subpectoral | Open | RCR | Over 65 y/o: |
| LHB tendonitis (1) | ||||||||||
| LHB rupture (1) | ||||||||||
| Under 65 y/o: | ||||||||||
| Hematoma, granuloma, infection, rupture, or pain over the tenodesis (17) | ||||||||||
| Fracture (12) | ||||||||||
| Werner et al.24 | Level III Case-Control | Biceps tendon degeneration/tear, Biceps subluxation | 249 | 27 (10.8%) | 9.9 months | Interference screw | Arthroscopic | Arthroscopic | RCR SLAP repair Anterior or posterior labral repair Acromioplasty | Arthroscopic: |
| Supra-pectoral | Suprapectoral | Postop stiffness (19) | ||||||||
| Open Subpectoral | Open Subpectoral | Open: Postop stiffness (8) | ||||||||
| Xiao et al.21 | Level III Retrospective | N/A | 10,688 | 885 (8.2%) | 30 days | N/A | N/A | Arthroscopic Open | Shoulder arthroscopy | Arthroscopic: |
| Capsulitis (489) | ||||||||||
| UTI (54) | ||||||||||
| Dislocation (28) | ||||||||||
| Acute kidney injury (15) | ||||||||||
| Infection (<11) | ||||||||||
| Hematoma(<11) | ||||||||||
| DVT or PE (<11) | ||||||||||
| Cardia arrest (<11) | ||||||||||
| Nerve injury (11) | ||||||||||
| Open: | ||||||||||
| Capsulitis (230) | ||||||||||
| UTI (28) | ||||||||||
| Dislocation (21) | ||||||||||
| Acute kidney injury (14) | ||||||||||
| Infection (<11) | ||||||||||
| Hematoma(<11) | ||||||||||
| Cardia arrest (<11) | ||||||||||
| Wound dehiscence (<11) | ||||||||||
| Yeung et al.6 | Level IV Case Series | N/A | 3362 | Arthroscopic (11.4%) Open (13.1%) | Database study (varies) | N/A | N/A | Arthroscopic Open | RCR | Bone Fracture (1) |
| Failure of Tendon Repair (51) | ||||||||||
| Infection (36) | ||||||||||
| Implant failure (23) | ||||||||||
| Fall (14) | ||||||||||
| Complex Regional Pain Syndrome (7) | ||||||||||
| Pain (58) | ||||||||||
| Nerve Injury/Palsy (30) | ||||||||||
| Stiffness/Arthrofibrosis (107) | ||||||||||
| Surgical Unspecified (45) | ||||||||||
| Surgical Procedure Intervention (1) | ||||||||||
| Wrong Side/Site (1) | ||||||||||
| Skin Ulcer/Blister (6) | ||||||||||
| Wound Healing Delay/Failure (15) | ||||||||||
| Tendon/Ligament Injury (7) | ||||||||||
| Hematoma/Seroma (11) | ||||||||||
| Vascular Injury (1) | ||||||||||
| Medical Complication Unspecified (43) | ||||||||||
| Medication Error/Reaction (8) | ||||||||||
| Patient Death (2) | ||||||||||
| Dermatologic Complaint (11) | ||||||||||
| Hypoxia/SOB (15) | ||||||||||
| PE (5) | ||||||||||
| Respiratory Failure (4) | ||||||||||
| UTI (3) | ||||||||||
| Pneumonia (5) | ||||||||||
| Renal Failure (2) | ||||||||||
| Urinary Retention (8) | ||||||||||
| DVT (10) | ||||||||||
| Anemia (1) | ||||||||||
| CVA (2) | ||||||||||
| Arrhythmia (1) | ||||||||||
| Unspecified Anesthetic Complications (2) | ||||||||||
| Block Anesthesia Complication (38) | ||||||||||
| General Anesthesia Complication (13) | ||||||||||
| Yi et al.82 | Level III Retrospective | LHBT lesions with RCR | 71 | 7 (9.8%) | 21 months | Interference screw | Subpectoral | Arthroscopic | RCR | Synovitis (3) |
| Open | Rotator cuff retear (4) | |||||||||
| Yi et al.83 | Level III Other | Rotator cuff tear | 66 | 5 (7.5%) | 26.8 months | Interference screw | Subpectoral | Arthroscopic | RCR | Rotator cuff retear (5) |
| Zhang et al.84 | Level I Prospective | Severe inflammation, Instability, Partial thickness tears, SLAP | 74 | 7 (9.5%) | 25 months | Suture anchor | N/A | Arthroscopic | RCR | Popeye deformity (2) |
| Acromioplasty Distal clavicle resection | Cramp/pain (5) |
3.1. Fracture after BT
Fracture rates, demographic information, type of fixation, approach, technique, and the time period of fractures are included in Table 3. Zhang et al. reported a post-operative fracture of the head of the humerus that was unrelated to surgery.84 This complication was excluded from our fracture rate. Five studies (n = 74,394 patients) reported fracture (n = 669) as a complication after BT with a mean fracture rate of 1.0% ± 1.6% (range = 0.1–3.6%) and cumulative fracture rate of 0.90%.4,6,11,20,81 Of note, Voss et al. combined tingling and postoperative fracture (n = 12) together into one complication group.81 Including the additional 64 studies that reported 0 fractures after BT, the cumulative fracture rate was 0.53%.
Table 3.
Studies that reported 1 or more fractures as a complication of biceps tenodesis.
| Author | Study Type | Pre-operative Diagnosis/Symptoms | N (Total Patients) | N (Fractures) | Fracture Rate (%) | Age | Male/Female/Unknown | Type of Fixation | Approach | Technique | Time Period of Fracture |
|---|---|---|---|---|---|---|---|---|---|---|---|
| McCrum et al.4 | LOE III: Retrospective review | Anterior shoulder pain, partial tears, subluxation, dislocation | 1526 | 1 | 0.09 | 53.7 (range: 18–91) | 1080/445 | Unicortical button | Subpectoral | Arthroscopic | Post-op, 10.8 months |
| Overmann et al.11 | LOE IV: Case series | SLAP tear, acromioclavicular joint arthritis, posterior labrum tear, anterior labroligamentous periosteal sleeve avulsion | 15,085 | 12 | 0.079 | 40 (range: 13–85) | 84%/16% | Unicortical button (n = 2) | Subpectoral | Open | Post-op (n = 11), 2.8 months Intra-op (n = 1) |
| Bicortical button (n = 1) | |||||||||||
| Suture anchor (n = 3) | |||||||||||
| Interference screw (n = 6) | |||||||||||
| Parisien et al.20 | LOE III: Retrospective | Not specified | 54,084 | 643 | 1.19 | 65–74 | 29,815/23,778/491 | Not specified | Not specified | Not specified | Post-op |
| Voss et al.81 | LOE IV: Case series | Chronic atrophic changes in the LHBT, tenosynovitis, | 337 | 12 | Total: 3.56 | 65+ group: | Not specified | Interference screw | Subpectoral | Open | Post-op |
| symptomatic intra-articular partial tears, pulley lesion with biceps instability (subluxation and luxation), SLAP lesion, | 65+ group: 0 | 69.7 (range 65–77) | |||||||||
| painful and hyperthrophic LHBT with secondary impingement, subpectoral biceps pain | Under 65 group: 3.80 | Under 65 group: 50 (29–64) | |||||||||
| Yeung et al.6 | LOE IV: Case series | Not specified | 3362 | 1 | 0.06 | 56.27 (Arthroscopic group) | 2282/1080 | Not specified | Not specified | Arthroscopic | Not specified |
| 53.91 (Open group) |
A total of 667 fractures occurred post-operatively, 1 fracture occurred intra-operatively, and the time of 1 fracture reported in Yeung et al.’s study was not specified.6 Of the 669 fractures, 643 were reported by Parisen et al.20 Parisien et al. (n = 643 fractures), and Yeung et al. (n = 1 fracture) did not specify fixation type nor BT approach (subpectoral versus suprapectoral).6,20 Unicortical button fixation was associated with 3 fractures, bicortical button fixation was associated with 1 fracture, suture anchor fixation was associated with 3 fractures, and interference screw fixation was associated with 13 fractures. Pooled results demonstrated that arthroscopic BT was associated with 243 fractures while open BT was associated with 304 fractures. The majority of these cases came from Parisien et al. who reported a significantly higher fracture risk in open BT (n = 280, 1.26%) versus arthroscopic BT (n = 232, 1.04%; P = 0.03, OR = 1.21).
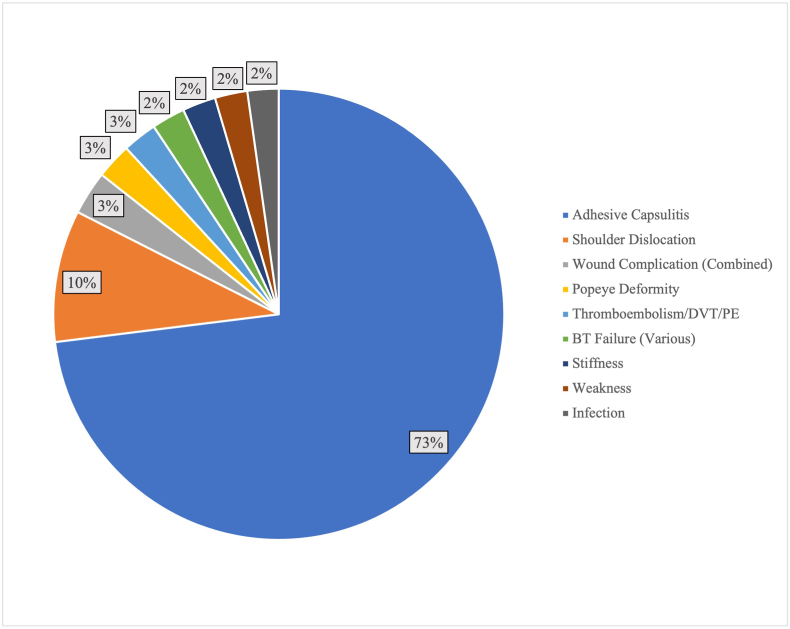
3.2. Non-fracture complication types
Complications besides humeral fracture that had greater than 100 cumulative occurrences (>0.18% of the 56,315 patients), included adhesive capsulitis (n = 4769; 8.47%), dislocation (n = 617; 1.10%), wound infections (total n = 205, superficial wound infection = 153, wound dehiscence = 4, not described = 48; overall 0.36%), Popeye deformity (n = 167; 0.30%), thromboembolism/deep venous thrombosis/pulmonary embolism (n = 161; 0.29%), BT failure (n = 157; 0.28%), stiffness (n = 156; 0.28%); weakness (n = 152; 0.27%), and unspecified infection (n = 146, 0.26%) (Fig. 2). All other complications had a cumulative rate <0.18% (n < 100, Table 4).
Fig. 2.
Non-fracture complications after BT (with an occurrence of n > 100 patients)
Rate is calculated based on the number of all complications with an occurrence >100 (n = 6530 patients). [DVT = deep vein thrombosis, PE = pulmonary embolism].
Table 4.
All reported non-fracture complications after BT.
| Complication | N | % of All Non-Fracture Complications | % of All Included Cases |
|---|---|---|---|
| Adhesive Capsulitis | 4769 | 65.72% | 8.47% |
| Shoulder Dislocation | 617 | 8.50% | 1.10% |
| Wound Complication (Combined) | 205 | 2.82% | 0.36% |
| Popeye Deformity | 167 | 2.30% | 0.30% |
| Thromboembolism/DVT/PE | 161 | 2.22% | 0.29% |
| BT Failure (Various) | 157 | 2.16% | 0.28% |
| Stiffness | 156 | 2.15% | 0.28% |
| Weakness | 152 | 2.09% | 0.27% |
| Infection | 146 | 2.01% | 0.26% |
| UTI | 93 | 1.28% | 0.17% |
| Cramping | 72 | 0.99% | 0.13% |
| Chronic Pain | 60 | 0.83% | 0.11% |
| Nerve Injury | 48 | 0.66% | 0.09% |
| Surgical Unspecified | 45 | 0.62% | 0.08% |
| Medical Complication Unspecified | 43 | 0.59% | 0.08% |
| Block Anesthesia Complication | 38 | 0.52% | 0.07% |
| AKI/Renal Failure | 31 | 0.43% | 0.06% |
| Nerve Injury/Palsy | 30 | 0.41% | 0.05% |
| Return to OR | 26 | 0.36% | 0.05% |
| Recurrent RC tears/RC retear | 24 | 0.33% | 0.04% |
| Implant failure | 23 | 0.32% | 0.04% |
| Unplanned Intubation | 17 | 0.23% | 0.03% |
| Pneumonia | 17 | 0.23% | 0.03% |
| Reflex Sympathetic Dystrophy | 15 | 0.21% | 0.03% |
| Hypoxia/SOB | 15 | 0.21% | 0.03% |
| Fall | 14 | 0.19% | 0.02% |
| General Anesthesia Complication | 13 | 0.18% | 0.02% |
| Postoperative Hematoma | 12 | 0.17% | 0.02% |
| Dermatologic Complaint | 11 | 0.15% | 0.02% |
| Medication Error/Reaction | 8 | 0.11% | 0.01% |
| Urinary Retention | 8 | 0.11% | 0.01% |
| Complex Regional Pain Syndrome | 7 | 0.10% | 0.01% |
| Tendon/Ligament Injury | 7 | 0.10% | 0.01% |
| MI | 6 | 0.08% | 0.01% |
| Transient Musculocutaneous Neuropraxia | 3 | 0.04% | 0.01% |
| Skin Ulcer/Blister | 6 | 0.08% | 0.01% |
| Respiratory Failure | 4 | 0.06% | 0.01% |
| Pseudoparalysis | 3 | 0.04% | 0.01% |
| Synovitis | 3 | 0.04% | 0.01% |
| Temporary Nerve Palsies from Interscalene Block | 2 | 0.03% | 0.00% |
| Transient Sensory Neuropathy | 2 | 0.03% | 0.00% |
| Glenohumeral OA | 2 | 0.03% | 0.00% |
| Patient Death | 2 | 0.03% | 0.00% |
| CVA | 2 | 0.03% | 0.00% |
| Unspecified Anesthetic Complications | 2 | 0.03% | 0.00% |
| Plexopathy | 1 | 0.01% | 0.00% |
| Superficial Erythema | 1 | 0.01% | 0.00% |
| Surgical Procedure Intervention | 1 | 0.01% | 0.00% |
| Wrong Side/Site | 1 | 0.01% | 0.00% |
| Vascular Injury | 1 | 0.01% | 0.00% |
| Anemia | 1 | 0.01% | 0.00% |
| Arryhythmia | 1 | 0.01% | 0.00% |
| Subsequent Lysis of Adhesions | 1 | 0.01% | 0.00% |
| Mild Asymmetry of the Biceps | 1 | 0.01% | 0.00% |
| Brachial Plexus Neuropraxia | 1 | 0.01% | 0.00% |
| Sepsis | 1 | 0.01% | 0.00% |
| Atraumatic Arthritis due to Chondrolysis | 1 | 0.01% | 0.00% |
| LHB tendonitis | 1 | 0.01% | 0.00% |
Rate is based on the cumulative number of included patients (n = 56,315 patients). [UTI = urinary tract infection, DVT = deep vein thrombosis, PE = pulmonary embolism, AKI = acute kidney injury, RCR = rotator cuff, MI = myocardial infarction, OA = osteoarthritis, LHB = long head of the biceps].
3.3. Non-fracture complications by approach, technique, and fixation
For the majority of included patients who suffered a non-fracture complication the approach, technique, and fixation type was not disclosed. For example, a total of 112 complications (1.54% of non-fracture complications) were associated with a subpectoral approach, 3 complications (0.04%) were associated with a suprapectoral approach, 18 complications (0.25%) were associated with an intra-articular approach, 1 complication was associated with a humoral approach (0.01%), 1 complication was associated with a keyhole approach (0.01%), 42 complications (0.58%) were associated with a total articular margin approach, 10 complications (0.18%) were associated with a “low in the bicipital groove” approach, and 1 complication was associated with a proximal approach (0.01%). It is important to note that fourteen studies4,6,18, 19, 20, 21, 22,24,26,38,49,53,63,84 did not include the BT approach and/or did not distinguish which approach was associated with a complication.
A total of 72 complications (0.99%) were associated with an open technique and a total of 106 complications (1.46%) were associated with an arthroscopic technique. However, fourteen studies4,6,11,18, 19, 20, 21, 22,24,26,34,49,80,82 did not include the BT technique and/or did not distinguish which technique was associated with a complication.
Suture anchor fixation was associated with 31 complications (0.43%), cortical button fixation was associated with 11 complications (0.15%), bicortical button with interference screw fixation was associated with 2 complications (0.03%), intra-articular trans-tendon fixation was associated with 1 complication (0.01%), interference screw fixation was associated with 158 complications (2.18%), and BirdBeak suture/free needle fixation was associated with 16 complications (0.22%). Ten studies4,6,11,18, 19, 20, 21, 22,34,53 did not include BT fixation type and/or did not distinguish which fixation type was associated with a complication.
4. Discussion
This systematic review found that the cumulative fracture risk was 0.5% in patients who underwent BT. The cumulative non-fracture complication rate was 12.9%. Fractures were the third most commonly reported complication after adhesive capsulitis and shoulder dislocation; adhesive capsulitis and shoulder dislocations occurred as a complication in 8.5% and 1.1% of cases, respectively, while fractures occurred after 0.5% of cases. This finding goes against our hypothesis; the fracture rate was higher than anticipated and higher than other complications, including wound complications, weakness, stiffness, and BT failure, in addition to medical complications such as unspecified infection and thromboembolism. The secondary purpose of this systematic review was to investigate the role of intraoperative variables on fracture after BT, including the role of fixation type and approach to provide clinical findings that corroborate recent biomechanical studies. The majority of studies included, however, did not include this information for the patients who suffered complications and thus no conclusion could be drawn.
Interestingly, the rate of postoperative adhesive capsulitis was relatively high at 8.5% of cases. This is likely due to the high rate of concomitant RCR. Varshneya et al., for example, only included BT patients who underwent a concomitant RCR with or without an acromioplasty.19 The authors reported a total of 4109 cases that were complicated by adhesive capsulitis. This number comprised 86.2% of the adhesive capsulitis cases included in this review. If the patients from the Varshneya et al. study were removed from the review, the cumulative rate of adhesive capsulitis would decrease from 8.5% to 1.3% and adhesive capsulitis would comprise only 21.0% of all non-fracture complications.19 This exercise demonstrates the high rate of adhesive capsulitis in patients undergoing BT with RCR and the relatively high rate of fracture when a complication, likely related to the RCR component of the surgery, is removed. This suggests that fracture may comprise a larger percent of complications in patients who undergo BT without a concomitant RCR.
Humeral fracture is a well-known complication after BT. Multiple case reports have reported on this topic, bringing this complication to light in the academic literature.7,9,85 Few studies, however, have been dedicated to investigating the rate of fracture after BTs in large sample sizes. It is often not even included in some systematic reviews reporting on complications after BT.86,87 This systematic review demonstrated that only 5 of 69 studies on outcomes after BT reported fracture as a complication.4,6,11,20,81 These 5 studies comprised 74,394 of the 125,484 (59.3%) included patients. The mean fracture rate of these studies was 1.0% (cumulative rate of 0.9%), while the cumulative fracture rate with all included studies was 0.5%, demonstrating how the inclusion of the other studies significantly deflated the cumulative fracture rate. Interestingly, these 5 studies were some of the largest included studies, and 3 of the 5 were database studies.6,11,20 In conjunction, these findings suggest that detection of fractures as a complication may be higher in studies of larger size, such as database studies.
The five studies reporting fracture as a complication utilized differing patient populations and inclusion/exclusion criteria, which may explain the large variation in fracture rate per study, ranging from 0.1%6 to 3.6%.81 Furthermore, the fracture number and rate was heavily skewed by the results of Parisien et al. (96% of all reported fractures).20 Other differences between these five studies may have influenced their reported fracture rate. Overmann et al., for example, reported on a specific cohort, the Military Health System, which includes active-duty service-members, dependents, and retirees.11 Despite these patients belonging to the military, suggesting a higher baseline level of activity, the range of included patients age was similar to the other studies (range: 13–85 years), although the mean age was slightly lower (40 years). Voss et al. used a mixed cohort that was mainly >65 years old (n = 314 of 337).81 Interestingly, all of their reported fractures (n = 12) occurred in the >65 years old, and this study had the highest reported fracture rate. Of note, however, the authors combined tingling and post-operative fracture into the same complication category, and it is unclear if anyone in this group did not actually sustain a fracture. The study by Parisien et al. was the largest included (n = 54,084) and had the highest number of fractures (n = 643) but not the highest rate (1.2%).20 Similar to the study by Voss et al., the authors limited their cohort to patients age 65–74 years old.81 Interestingly, these two studies that focused on assessing fracture rate in those >65 years old reported the highest fracture rate. This may be due to the higher rate of osteoporosis in this population, which has been shown to be a risk factor for periprosthetic fracture in other shoulder procedures such as total shoulder arthroplasty.20,81,88 This risk of fracture in the elderly population is particularly notable, as these patients may have higher rates of stiffness, morbidity, and mortality than younger patients. Unfortunately, while there some differences in the cohorts of these studies, as described, no conclusion could be drawn on the role of fixation, technique, or approach on fracture rate since this was not reported by Parisien et al. and Yeung et al.6,20
Prior studies have described a biomechanical basis for the increased fracture risk in BT. These studies demonstrated that drilling a unicortical tunnel creates a stress riser in the humerus, thus decreasing its torsional strength, and that torsional strength is more significantly lowered using a subpectoral approach versus a suprapectoral approach.12,89 In addition, Euler et al. demonstrated that lateral eccentric malpositioning of the BT socket significantly increases fracture risk.16 Furthermore, Khalid et al. demonstrated that a 6.25 mm interference screw significantly decrease the load needed to produce a humeral fracture.90 While fixation type may alter torsional strength, it has been demonstrated that absolute interference screw size may play a minimal role but relative defect size (drill hole relative to the humeral width at the level of insertion) significantly increases fracture risk.13,16 Since diameter and length of BT fixation does not significantly affect load to failure or stiffness of the construct,91 we recommend minimizing socket and screw diameter given their comparable strength and the increased risk of fracture in larger diameter screws.
In contrast to unicortical techniques, it is unclear what factors increase the risk of fracture when using a bicortical approach. One possible mechanism is the involvement and subsequent weakening of the adjacent cortical bone due excessively angled drilling. In addition to an aberrant angle of the drill, an eccentric drilling location, similar to what was described to Euler et al., could increase the likelihood of adjacent cortex involvement.16 Future studies are needed to investigate factors that may increase the risk of fracture in BTs performed with a bicortical technique.
4.1. Limitations
This study should be assessed in the context of the following limitations. First, the cumulative fracture and complication rate was based on the included 69 studies. These studies, however, demonstrated heterogeneity. For example, due to the scarcity of literature on isolated BT outcomes, concomitant procedures besides TSA and preexisting humeral fractures, were not excluded. Furthermore, our study was not able to assess the role of concomitant procedure and procedure type on fracture risk. Second, one of the goals of this study was to assess the role of fixation type and BT approach, but this was not possible due to the heterogeneity of the studies included and because the percent of studies that included this information was very low (<5% of patients who sustained a complication). It is unclear whether subgroup analysis based on fixation type and approach would yield different results. In addition, due to overlapping patient populations three studies had to be excluded from analysis.17,22,23 It is possible that some of the non-overlapping patients from these studies would slightly alter the fracture and complication rate. Lastly, many of the excluded studies reported on the rate of only Popeye deformity after BT but did not report on any other complication rate. If the complication rate was not explicitly stated or stated to be 0, then the study was excluded. It is possible, however, that these studies indeed did not have any other complications beyond Popeye deformities and their inclusion would lower both the fracture rate and overall complication rate.
5. Conclusion
Based on the current literature reporting on complications after a BT procedure, humeral fracture was the third most common complication after adhesive capsulitis and shoulder dislocation. The complication rate of adhesive capsulitis may be skewed by the high rate of concomitant rotator cuff repair. Due to the relatively high incidence of fracture, surgeons should ensure that this complication is disclosed to patients undergoing BT. It remains unclear what role, if any, fixation type and BT approach play in fracture risk.
Contributorship
HPH, JSK, SG, WA, and SMK have all made a substantial contributions to the concept and design of the work, and analysis and interpretation of data. HPH, JSK, SG, WA, and SMK have drafted the article and revised it critically for important intellectual content, approved the version to be published, and participated sufficiently in the work to take public responsibility for appropriate portions of the content.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Informed consent
N/A.
Ethical approval
N/A.
Declaration of competing interest
SMK is a committee member of the American Society for Surgery of the Hand (ASSH), a paid consultant and speaker for Integra LifeSciences, Inc, a paid consultant for Tissium, Inc., a stockholder and member of the medical advisory board for Reactiv, Inc., a member of the advisory board for Androes, LLC, and a speaker for TriMed, Inc. WA is a paid consultant for Exactech Inc. HPH, JSK, and SG declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Acknowledgements
N/A.
References
- 1.Vellios E.E., Nazemi A.K., Yeranosian M.G., et al. Demographic trends in arthroscopic and open biceps tenodesis across the United States. J Shoulder Elbow Surg. 2015;24:e279–e285. doi: 10.1016/j.jse.2015.04.021. [DOI] [PubMed] [Google Scholar]
- 2.Erickson B.J., Jain A., Cvetanovich G.L., et al. Biceps tenodesis: an evolution of treatment. Am J Orthop Belle Mead N J. 2017;46:E219–E223. [PubMed] [Google Scholar]
- 3.Werner B.C., Brockmeier S.F., Gwathmey F.W. Trends in long head biceps tenodesis. Am J Sports Medicine. 2015;43:570–578. doi: 10.1177/0363546514560155. [DOI] [PubMed] [Google Scholar]
- 4.McCrum C.L., Alluri R.K., Batech M., et al. Complications of biceps tenodesis based on location, fixation, and indication: a review of 1526 shoulders. J Shoulder Elbow Surg. 2019;28:461–469. doi: 10.1016/j.jse.2018.09.005. [DOI] [PubMed] [Google Scholar]
- 5.Nho S.J., Reiff S.N., Verma N.N., et al. Complications associated with subpectoral biceps tenodesis: low rates of incidence following surgery. J Shoulder Elbow Surg. 2010;19:764–768. doi: 10.1016/j.jse.2010.01.024. [DOI] [PubMed] [Google Scholar]
- 6.Yeung M., Shin J.J., Lesniak B.P., et al. Complications of arthroscopic versus open biceps tenodesis in the setting of arthroscopic rotator cuff repairs: an analysis of the American board of orthopaedic surgery database. J Am Acad Orthop Sur. 2020;28:113–120. doi: 10.5435/JAAOS-D-19-00252. [DOI] [PubMed] [Google Scholar]
- 7.Sears B.W., Spencer E.E., Getz C.L. Humeral fracture following subpectoral biceps tenodesis in 2 active, healthy patients. J Shoulder Elbow Surg. 2011;20:e7–e11. doi: 10.1016/j.jse.2011.02.020. [DOI] [PubMed] [Google Scholar]
- 8.Dein E.J., Huri G., Gordon J.C., et al. A humerus fracture in a baseball pitcher after biceps tenodesis. Am J Sports Medicine. 2014;42:877–879. doi: 10.1177/0363546513519218. [DOI] [PubMed] [Google Scholar]
- 9.Reiff S.N., Nho S.J., Romeo A.A. Proximal humerus fracture after keyhole biceps tenodesis. Am J Orthop Belle Mead N J. 2010;39:E61–E63. [PubMed] [Google Scholar]
- 10.Friedel R., Markgraf E., Schmidt I., et al. Die proximale Humerusschaftfraktur als Komplikation nach der Schlüssellochplastik: ein Fallbericht. Unfallchirurgie. 1995;21:198–201. doi: 10.1007/BF02588699. [DOI] [PubMed] [Google Scholar]
- 11.Overmann A.L., Colantonio D.F., Wheatley B.M., et al. Incidence and characteristics of humeral shaft fractures after subpectoral biceps tenodesis. Orthop J Sports Medicine. 2019;7 doi: 10.1177/2325967119833420. 2325967119833420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mellano C.R., Frank R.M., Shin J.J., et al. Subpectoral biceps tenodesis with peek interference screw: a biomechanical analysis of humeral fracture risk. Arthrosc J Arthrosc Relat Surg. 2018;34:806–813. doi: 10.1016/j.arthro.2017.09.012. [DOI] [PubMed] [Google Scholar]
- 13.Beason D.P., Shah J.P., Duckett J.W., et al. Torsional fracture of the humerus after subpectoral biceps tenodesis with an interference screw: a biomechanical cadaveric study. Clin Biomech. 2015;30:915–920. doi: 10.1016/j.clinbiomech.2015.07.009. [DOI] [PubMed] [Google Scholar]
- 14.Edgerton B.C., An K., Morrey B.F. Torsional strength reduction due to cortical defects in bone. J Orthop Res. 1990;8:851–855. doi: 10.1002/jor.1100080610. [DOI] [PubMed] [Google Scholar]
- 15.Frank R.M., Bernardoni E.D., Veera S.S., et al. Biomechanical analysis of all-suture suture anchor fixation compared with conventional suture anchors and interference screws for biceps tenodesis. Arthrosc J Arthrosc Relat Surg. 2019;35:1760–1768. doi: 10.1016/j.arthro.2019.01.026. [DOI] [PubMed] [Google Scholar]
- 16.Euler S.A., Smith S.D., Williams B.T., et al. Biomechanical analysis of subpectoral biceps tenodesis. Am J Sports Medicine. 2015;43:69–74. doi: 10.1177/0363546514554563. [DOI] [PubMed] [Google Scholar]
- 17.Erickson B.J., Basques B.A., Griffin J.W., et al. The effect of concomitant biceps tenodesis on reoperation rates after rotator cuff repair: a review of a large private-payer database from 2007 to 2014. Arthrosc J Arthrosc Relat Surg. 2017;33:1301–1307.e1. doi: 10.1016/j.arthro.2017.01.030. [DOI] [PubMed] [Google Scholar]
- 18.Gowd A.K., Liu J.N., Garcia G.H., et al. Open biceps tenodesis associated with slightly greater rate of 30-day complications than arthroscopic: a propensity-matched analysis. Arthrosc J Arthrosc Relat Surg. 2019;35:1044–1049. doi: 10.1016/j.arthro.2018.11.036. [DOI] [PubMed] [Google Scholar]
- 19.Varshneya K., Safran M.R., Sherman S.L., et al. Costs, complications, and reoperations associated with primary arthroscopic rotator cuff repair with or without acromioplasty and/or biceps tenodesis. Arthrosc Sports Medicine Rehabilitation. 2020;2:e369–e376. doi: 10.1016/j.asmr.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Parisien R.L., Trofa D.P., Kang H.P., et al. Increased risk of humeral fracture with open versus arthroscopic tenodesis of the long head of the biceps brachii. Arthrosc Sports Medicine Rehabilitation. 2020;2:e329–e332. doi: 10.1016/j.asmr.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xiao M., Abrams G.D. Increased reoperation rates among patients undergoing shoulder arthroscopy with concomitant biceps tenodesis. Jses Open Access. 2019;3:344–349. doi: 10.1016/j.jses.2019.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shin J.J., Popchak A.J., Musahl V., et al. Complications after arthroscopic shoulder surgery: a review of the American board of orthopaedic surgery database. Jaaos Global Res Rev. 2018;2:e093. doi: 10.5435/JAAOSGlobal-D-18-00093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Werner B.C., Evans C.L., Holzgrefe R.E., et al. Arthroscopic suprapectoral and open subpectoral biceps tenodesis: a comparison of minimum 2-year clinical outcomes. Am J Sports Medicine. 2014;42:2583–2590. doi: 10.1177/0363546514547226. [DOI] [PubMed] [Google Scholar]
- 24.Werner B.C., Pehlivan H.C., Hart J.M., et al. Increased incidence of postoperative stiffness after arthroscopic compared with open biceps tenodesis. Arthrosc J Arthrosc Relat Surg. 2014;30:1075–1084. doi: 10.1016/j.arthro.2014.03.024. [DOI] [PubMed] [Google Scholar]
- 25.Boileau P., Krishnan S.G., Coste J.-S., et al. Arthroscopic biceps tenodesis: a new technique using bioabsorbable interference screw fixation. Arthrosc J Arthrosc Relat Surg Official Publ Arthrosc Assoc North Am Int Arthrosc Assoc. 2002;18:1002–1012. doi: 10.1053/jars.2002.36488. [DOI] [PubMed] [Google Scholar]
- 26.Duchman K.R., DeMik D.E., Uribe B., et al. Open versus arthroscopic biceps tenodesis: a comparison of functional outcomes. Iowa Orthop J. 2016;36:79–87. [PMC free article] [PubMed] [Google Scholar]
- 27.Faruqui S., Kotob M.A., Hanna C.C., et al. The modified Norwegian method of biceps tenodesis: how well does it work? Knee Surg Sports Traumatol Arthrosc. 2017;25:3264–3269. doi: 10.1007/s00167-016-4145-7. [DOI] [PubMed] [Google Scholar]
- 28.Liechti D.J., Mitchell J.J., Menge T.J., et al. Immediate physical therapy without postoperative restrictions following open subpectoral biceps tenodesis: low failure rates and improved outcomes at a minimum 2-year follow-up. J Shoulder Elbow Surg. 2018;27:1891–1897. doi: 10.1016/j.jse.2018.02.061. [DOI] [PubMed] [Google Scholar]
- 29.Schoch C., Geyer M., Drews B. Suprapectoral biceps tenodesis using a suture plate: clinical results after 2 years. Arch Orthop Traum Su. 2017;137:829–835. doi: 10.1007/s00402-017-2664-4. [DOI] [PubMed] [Google Scholar]
- 30.Abtahi A.M., Granger E.K., Tashjian R.Z. Complications after subpectoral biceps tenodesis using a dual suture anchor technique. Int J Shoulder Surg. 2014;8:47–50. doi: 10.4103/0973-6042.137527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Baron S.L., Shamah S., McGee A.W., et al. Clinical outcomes of open subpectoral biceps tenodesis with cortical button fixation. Bull Hosp Jt Dis. 2013 2019;77:238–243. [PubMed] [Google Scholar]
- 32.Baumgarten K.M., Chang P.S., Foley E.K. Patient-determined outcomes after arthroscopic rotator cuff repair with and without biceps tenodesis utilizing the PITT technique. J Shoulder Elbow Surg. 2019;28:1049–1055. doi: 10.1016/j.jse.2019.01.024. [DOI] [PubMed] [Google Scholar]
- 33.Belay E.S., Wittstein J.R., Garrigues G.E., et al. Biceps tenotomy has earlier pain relief compared to biceps tenodesis: a randomized prospective study. Knee Surg Sports Traumatol Arthrosc. 2019;27:4032–4037. doi: 10.1007/s00167-019-05682-1. [DOI] [PubMed] [Google Scholar]
- 34.Berlemann U., Bayley I. Tenodesis of the long head of biceps brachii in the painful shoulder: improving results in the long term. J Shoulder Elbow Surg. 1995;4:429–435. doi: 10.1016/s1058-2746(05)80034-5. [DOI] [PubMed] [Google Scholar]
- 35.Boileau P., Parratte S., Chuinard C., et al. Arthroscopic treatment of isolated type II SLAP lesions. Am J Sports Medicine. 2009;37:929–936. doi: 10.1177/0363546508330127. [DOI] [PubMed] [Google Scholar]
- 36.Boileau P., Baqué F., Valerio L., et al. Isolated arthroscopic biceps tenotomy or tenodesis improves symptoms in patients with massive irreparable rotator cuff tears. J Bone Jt Surg. 2007;89:747–757. doi: 10.2106/JBJS.E.01097. [DOI] [PubMed] [Google Scholar]
- 37.Brady P.C., Narbona P., Adams C.R., et al. Arthroscopic proximal biceps tenodesis at the articular margin: evaluation of outcomes, complications, and revision rate. Arthrosc J Arthrosc Relat Surg. 2015;31:470–476. doi: 10.1016/j.arthro.2014.08.024. [DOI] [PubMed] [Google Scholar]
- 38.Castricini R., Familiari F., Gori M.D., et al. Tenodesis is not superior to tenotomy in the treatment of the long head of biceps tendon lesions. Knee Surg Sports Traumatol Arthrosc. 2018;26:169–175. doi: 10.1007/s00167-017-4609-4. [DOI] [PubMed] [Google Scholar]
- 39.Cook J.B., Sedory D.M., Freidl M.C., et al. Low incidence of failure after proximal biceps tenodesis with unicortical suture button. J Orthop. 2017;14:384–389. doi: 10.1016/j.jor.2017.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Denard P.J., Lädermann A., Parsley B.K., et al. Arthroscopic biceps tenodesis compared with repair of isolated type II SLAP lesions in patients older than 35 years. Orthopedics. 2014;37:e292–e297. doi: 10.3928/01477447-20140225-63. [DOI] [PubMed] [Google Scholar]
- 41.Duerr R.A., Nye D., Paci J.M., et al. Clinical evaluation of an arthroscopic knotless suprapectoral biceps tenodesis technique: loop ’n’ tack tenodesis. Orthop J Sports Medicine. 2018;6 doi: 10.1177/2325967118779786. 2325967118779786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dunne K.F., Knesek M., Tjong V.K., et al. Arthroscopic treatment of type II superior labral anterior to posterior (SLAP) lesions in a younger population: minimum 2-year outcomes are similar between SLAP repair and biceps tenodesis. Knee Surg Sports Traumatol Arthrosc. 2021;29:257–265. doi: 10.1007/s00167-020-05971-0. [DOI] [PubMed] [Google Scholar]
- 43.Ek E.T.H., Shi L.L., Tompson J.D., et al. Surgical treatment of isolated type II superior labrum anterior-posterior (SLAP) lesions: repair versus biceps tenodesis. J Shoulder Elbow Surg. 2014;23:1059–1065. doi: 10.1016/j.jse.2013.09.030. [DOI] [PubMed] [Google Scholar]
- 44.Euler S.A., Horan M.P., Ellman M.B., et al. Chronic rupture of the long head of the biceps tendon: comparison of 2-year results following primary versus revision open subpectoral biceps tenodesis. Arch Orthop Traum Su. 2016;136:657–663. doi: 10.1007/s00402-015-2393-5. [DOI] [PubMed] [Google Scholar]
- 45.Fang J., Dai X., Yu X., et al. Lesions of the long head of the biceps tendon concomitant with rotator cuff tears: tenotomy or subpectoral mini‐open tenodesis? A comparative short to mid‐term follow‐up study. Orthop Surg. 2019;11:857–863. doi: 10.1111/os.12536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Forsythe B., Zuke W.A., Agarwalla A., et al. Arthroscopic suprapectoral and open subpectoral biceps tenodeses produce similar outcomes: a randomized prospective analysis. Arthrosc J Arthrosc Relat Surg. 2020;36:23–32. doi: 10.1016/j.arthro.2019.07.009. [DOI] [PubMed] [Google Scholar]
- 47.Franceschetti E., Sanctis EG de, Palumbo A., et al. The management of the long head of the biceps in rotator cuff repair: a comparative study of high vs. subpectoral tenodesis. J Sport Health Sci. 2020 doi: 10.1016/j.jshs.2020.08.004. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Franceschi F., Longo U.G., Ruzzini L., et al. To detach the long head of the biceps tendon after tenodesis or not: outcome analysis at the 4-year follow-up of two different techniques. Int Orthop. 2007;31:537–545. doi: 10.1007/s00264-006-0206-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gombera M.M., Kahlenberg C.A., Nair R., et al. All-arthroscopic suprapectoral versus open subpectoral tenodesis of the long head of the biceps brachii. Am J Sports Medicine. 2015;43:1077–1083. doi: 10.1177/0363546515570024. [DOI] [PubMed] [Google Scholar]
- 50.Gottschalk M.B., Karas S.G., Ghattas T.N., et al. Subpectoral biceps tenodesis for the treatment of type two and four slap lesions. Orthop J Sports Medicine. 2014;2 doi: 10.1177/0363546514540273. 2325967114S00062. [DOI] [PubMed] [Google Scholar]
- 51.Gumina S., Carbone S., Perugia D., et al. Rupture of the long head biceps tendon treated with tenodesis to the coracoid process. Results at more than 30 years. Int Orthop. 2011;35:713–716. doi: 10.1007/s00264-010-1099-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gupta A.K., Chalmers P.N., Klosterman E.L., et al. Subpectoral biceps tenodesis for bicipital tendonitis with SLAP tear. Orthopedics. 2015;38:e48–e53. doi: 10.3928/01477447-20150105-60. [DOI] [PubMed] [Google Scholar]
- 53.Haidamous G., Noyes M.P., Denard P.J. Arthroscopic biceps tenodesis outcomes: a comparison of inlay and onlay techniques. Am J Sports Medicine. 2020;48:3051–3056. doi: 10.1177/0363546520952357. [DOI] [PubMed] [Google Scholar]
- 54.Hodgins J.L., Kovacevic D., Purcell S., et al. Arthroscopic suprapectoral and open subpectoral biceps tenodesis: radiographic characteristics. Arthrosc J Arthrosc Relat Surg. 2016;32:2234–2242. doi: 10.1016/j.arthro.2016.03.101. [DOI] [PubMed] [Google Scholar]
- 55.Hufeland M., Kolem C., Ziskoven C., et al. The influence of suprapectoral arthroscopic biceps tenodesis for isolated biceps lesions on elbow flexion force and clinical outcomes. Knee Surg Sports Traumatol Arthrosc. 2017;25:3220–3228. doi: 10.1007/s00167-015-3846-7. [DOI] [PubMed] [Google Scholar]
- 56.Jacxsens M., Granger E.K., Tashjian R.Z. Clinical and sonographic evaluation of subpectoral biceps tenodesis with a dual suture anchor technique demonstrates improved outcomes and a low failure rate at a minimum 2-year follow-up. Arch Orthop Traum Su. 2017;138:63–72. doi: 10.1007/s00402-017-2810-z. [DOI] [PubMed] [Google Scholar]
- 57.Javed S., Gheorghiu D., Walton M. Subpectoral biceps tenodesis using a novel anterior cortical button technique. Shoulder Elbow. 2018;10:292–295. doi: 10.1177/1758573218778799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kany J., Guinand R., Amaravathi R.S., et al. The keyhole technique for arthroscopic tenodesis of the long head of the biceps tendon. In vivo prospective study with a radio-opaque marker. Orthop Traumatology Surg Res. 2015;101:31–34. doi: 10.1016/j.otsr.2014.10.016. [DOI] [PubMed] [Google Scholar]
- 59.Kany J., Guinand R., Croutzet P., et al. Biceps tenodesis (long head): arthroscopic keyhole technique versus arthroscopic interference screw: a prospective comparative clinical and radiographic marker study. European J Orthop Surg Traumatology Orthopédie Traumatologie. 2016;26:77–84. doi: 10.1007/s00590-015-1714-2. [DOI] [PubMed] [Google Scholar]
- 60.Kahlenberg C.A., Patel R.M., Nair R., et al. Clinical and biomechanical evaluation of an all-arthroscopic suprapectoral biceps tenodesis. Orthop J Sports Medicine. 2014;2 doi: 10.1177/2325967114553558. 2325967114553558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kim J., Nam J.H., Kim Y., et al. Long head of the biceps tendon tenotomy versus subpectoral tenodesis in rotator cuff repair. Clin Orthop Surg. 2020;12:371–378. doi: 10.4055/cios19168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kreines A., Pontes M., Ford E., et al. Outcomes of arthroscopic biceps tenodesis for the treatment of failed type II SLAP repair: a minimum 2-year follow-up. Archives Bone Jt Surg. 2020;8:154–161. doi: 10.22038/abjs.2019.40449.2087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lim S., Kim S.K., Kim Y.-S. Comparison between SLAP repair and biceps tenodesis with concomitant rotator cuff repair in patients older than 45 Years: minimum 2-year clinical and imaging outcomes. Clin Orthop Surg. 2020;12:364–370. doi: 10.4055/cios19157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lutton D.M., Gruson K.I., Harrison A.K., et al. Where to tenodese the biceps: proximal or distal? Clin Orthop Relat Res. 2011;469:1050–1055. doi: 10.1007/s11999-010-1691-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.MacDonald P., Verhulst F., McRae S., et al. Biceps tenodesis versus tenotomy in the treatment of lesions of the long head of the biceps tendon in patients undergoing arthroscopic shoulder surgery: a prospective double-blinded randomized controlled trial. Am J Sports Medicine. 2020;48:1439–1449. doi: 10.1177/0363546520912212. [DOI] [PubMed] [Google Scholar]
- 66.Meghpara M.B., Schulz W., Buerba R.A., et al. Clinical outcomes of an all-arthroscopic biceps tenodesis using the anterolateral anchor during concomitant double-row rotator cuff repair. Orthop J Sports Medicine. 2020;8 doi: 10.1177/2325967120959142. 2325967120959142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.McMahon P.J., Speziali A. Outcomes of tenodesis of the long head of the biceps tendon more than three months after rupture. World J Orthoped. 2016;7:188–194. doi: 10.5312/wjo.v7.i3.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Millett P.J., Sanders B., Gobezie R., et al. Interference screw vs. Suture anchor fixation for open subpectoral biceps tenodesis: does it matter? Bmc Musculoskelet Di. 2008;9:121. doi: 10.1186/1471-2474-9-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ng C.Y., Funk L. Symptomatic chronic long head of biceps rupture: surgical results. Int J Shoulder Surg. 2012;6:108–111. doi: 10.4103/0973-6042.106222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Nho S.J., Frank R.M., Reiff S.N., et al. Arthroscopic repair of anterosuperior rotator cuff tears combined with open biceps tenodesis. Arthrosc J Arthrosc Relat Surg. 2010;26:1667–1674. doi: 10.1016/j.arthro.2010.04.008. [DOI] [PubMed] [Google Scholar]
- 71.Paulos L.E., Mendez K.T., Berg T. A novel approach to arthroscopic biceps tenodesis. Operat Tech Sports Med. 2007;15:27–34. [Google Scholar]
- 72.Peebles L.A., Midtgaard K.S., Aman Z.S., et al. Conversion of failed proximal long head of the biceps tenodesis to distal subpectoral tenodesis: outcomes in an active population. Arthrosc J Arthrosc Relat Surg. 2020;36:2975–2981. doi: 10.1016/j.arthro.2020.07.019. [DOI] [PubMed] [Google Scholar]
- 73.Perry N.P.J., Wolfe J.A., Nguyen-Ta K., et al. Biceps tenodesis and intra-articular decompression for treatment of superior labral tear from anterior to posterior and associated paralabral cyst in active duty military. Mil Med. 2018;183:e194–e200. doi: 10.1093/milmed/usx019. [DOI] [PubMed] [Google Scholar]
- 74.Provencher M.T., McCormick F., Peebles L.A., et al. Outcomes of primary biceps subpectoral tenodesis in an active population: a prospective evaluation of 101 patients. Arthrosc J Arthrosc Relat Surg. 2019;35:3205–3210. doi: 10.1016/j.arthro.2019.06.035. [DOI] [PubMed] [Google Scholar]
- 75.Rhee S.-M., Jeong H.Y., Ro K., et al. Double on-lay fixation using all suture-type anchor for subpectoral biceps tenodesis has favorable functional outcomes and leads to less cosmetic deformities than single on-lay fixation. Knee Surg Sports Traumatol Arthrosc. 2019;27:4005–4013. doi: 10.1007/s00167-019-05663-4. [DOI] [PubMed] [Google Scholar]
- 76.Sasaki Y., Ochiai N., Kenmoku T., et al. Arthroscopic tenodesis using a bioabsorbable interference screw and soft anchor: a case series of 60 patients. J Orthop Sci. 2020;25:410–415. doi: 10.1016/j.jos.2019.05.005. [DOI] [PubMed] [Google Scholar]
- 77.Schrock J.B., Kraeutler M.J., Bravman J.T. Comparison of clinical failure rates after 2 techniques of subpectoral mini-open biceps tenodesis: sequence and suture passage technique matter. Orthop J Sports Medicine. 2017;5 doi: 10.1177/2325967117729356. 2325967117729356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Schrøder C.P., Skare Ø., Reikerås O., et al. Sham surgery versus labral repair or biceps tenodesis for type II SLAP lesions of the shoulder: a three-armed randomised clinical trial. Br J Sports Med. 2017;51:1759. doi: 10.1136/bjsports-2016-097098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Shen J., Gao Q., Zhang Y., et al. Arthroscopic tenodesis through positioning portals to treat proximal lesions of the biceps tendon. Cell Biochem Biophys. 2014;70:1499–1506. doi: 10.1007/s12013-014-0071-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tu J., Xu B., Guo R. Open subpectoral vs. arthroscopic proximal biceps tenodesis: a comparison study of clinical outcomes. Exp Ther Med. 2020;19:428–434. doi: 10.3892/etm.2019.8232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Voss A., Cerciello S., DiVenere J., et al. Open subpectoral biceps tenodesis in patients over 65 does not result in an increased rate of complications. Bmc Musculoskelet Di. 2017;18:430. doi: 10.1186/s12891-017-1780-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Yi G., Yang J., Zhang L., et al. Small-incision open distal subpectoral vs. arthroscopic proximal biceps tenodesis for biceps long head tendon lesions with repair of rotator cuff tears. Exp Ther Med. 2020;19:861–870. doi: 10.3892/etm.2019.8284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Yi Y., Lee J.-M., Kwon S.H., et al. Arthroscopic proximal versus open subpectoral biceps tenodesis with arthroscopic repair of small- or medium-sized rotator cuff tears. Knee Surg Sports Traumatol Arthrosc. 2016;24:3772–3778. doi: 10.1007/s00167-015-3641-5. [DOI] [PubMed] [Google Scholar]
- 84.Zhang Q., Zhou J., Ge H., et al. Tenotomy or tenodesis for long head biceps lesions in shoulders with reparable rotator cuff tears: a prospective randomised trial. Knee Surg Sports Traumatol Arthrosc. 2015;23:464–469. doi: 10.1007/s00167-013-2587-8. [DOI] [PubMed] [Google Scholar]
- 85.Jacobs A.N., Umlauf J.A., Kniss J.R. Proximal humerus fracture following arthroscopic biceps tenodesis. J Orthop Sport Phys. 2020;50:649. doi: 10.2519/jospt.2020.9497. 649. [DOI] [PubMed] [Google Scholar]
- 86.Deng Z.J., Yin C., Cusano J., et al. Outcomes and complications after primary arthroscopic suprapectoral versus open subpectoral biceps tenodesis for superior labral anterior-posterior tears or biceps abnormalities: a systematic review and meta-analysis. Orthop J Sports Medicine. 2020;8 doi: 10.1177/2325967120945322. 2325967120945322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Frantz T.L., Shacklett A.G., Martin A.S., et al. Biceps tenodesis for superior labrum anterior-posterior tear in the overhead athlete: a systematic review. Am J Sports Medicine. 2020;49:522–528. doi: 10.1177/0363546520921177. [DOI] [PubMed] [Google Scholar]
- 88.Casp A.J., Montgomery S.R., Cancienne J.M., et al. Osteoporosis and implant-related complications after anatomic and reverse total shoulder arthroplasty. J Am Acad Orthop Sur. 2020;28:121–127. doi: 10.5435/JAAOS-D-18-00537. [DOI] [PubMed] [Google Scholar]
- 89.Dini A.A., Mizels J.E., Sadeghpour S., et al. Implant-free subpectoral biceps tenodesis is biomechanically at higher risk of spiral fracture of the humerus compared with implant-free suprapectoral biceps tenodesis. Arthrosc Sports Medicine Rehabilitation. 2021;3:e73–e78. doi: 10.1016/j.asmr.2020.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Khalid M.A., Morris R.P., Black N., et al. Biomechanical evaluation of humerus fracture after subpectoral biceps tenodesis with interference screw versus unicortical button. Arthrosc J Arthrosc Relat Surg. 2020;36:1253–1260. doi: 10.1016/j.arthro.2019.10.034. [DOI] [PubMed] [Google Scholar]
- 91.Slabaugh M.M.A., Frank R.M., Thiel G.S.V., et al. Biceps tenodesis with interference screw fixation: a biomechanical comparison of screw length and diameter. Arthrosc J Arthrosc Relat Surg. 2011;27:161–166. doi: 10.1016/j.arthro.2010.07.004. [DOI] [PubMed] [Google Scholar]