Abstract
Background and rationale
Obesity is associated with the development and progression of many diseases. Understanding and management of obesity have become increasingly important; however, a knowledge gap remains between how healthcare providers (HCPs) consider weight‐loss treatment and the importance of weight loss for improving obesity‐related diseases.
Objective
The objective of this study was to investigate how HCPs assess obesity, how they interpret the relationship between obesity and 12 recognized co‐morbidities of obesity (excluding diabetes), and their view about the value of various weight‐loss therapies.
Methods
This was a cross‐sectional, non‐interventional, descriptive study. Participants were medical doctors (HCPs) from eight European countries.
Results
Eighty‐nine percent of the 197 HCPs that completed the survey considered obesity a disease. For most of the 12 obesity‐related diseases under consideration, a majority of HCPs agreed that weight loss could reverse the disease or prevent progression. Among HCPs who have recommended weight loss, lifestyle interventions were by far the most common recommendation. However, more than three out of four HCPs stated that they would be likely to prescribe anti‐obesity medications if available and reimbursed.
Conclusion
Most HCPs in this survey consider obesity a disease that needs to be treated. However, the majority of HCPs appear to prefer recommending lifestyle changes, although it is well documented that weight loss obtained by lifestyle changes is difficult to maintain. These results underscore the need for improved education of HCPs involved in the treatment of obesity‐related diseases.
Keywords: anti‐obesity medication, complications, HCP, obesity, survey
Visual Abstract
1. INTRODUCTION
Throughout Europe, the prevalence of obesity in the adult population has risen during the past decade and is expected to increase further unless significant interventions are made. By 2025, the level of people with obesity in Europe is expected to reach 20% or more. 1 If obesity rates continue to increase as projected, the cost of maintaining Europe's healthcare systems is likely to escalate dramatically. Research links obesity with as many as 236 other conditions and diseases, 2 and the duration of obesity alone increases the likelihood of several diseases worsening, requiring even more intense interventions. 3 Therefore, understanding and managing obesity is becoming increasingly important throughout entire healthcare systems, both in primary care and in the hospital sector.
Treating obesity could significantly improve the management of a broad range of diseases and reduce associated morbidity or mortality. For example, weight loss of different magnitudes has been shown to clinically improve or reverse the course of disease progression in several obesity‐related illnesses. Even moderate weight loss (i.e., 5%–10%) has been shown to avoid progression for selected complications, including osteoarthritis (OA), 4 , 5 infertility due to polycystic ovarian syndrome (PCOS), 6 , 7 obstructive sleep apnea (OSA), 8 , 9 , 10 and urinary incontinence (UI) in women. 11
Despite many clinicians across medical specialties being directly involved in the treatment of obesity‐related diseases, previous research surveys have shown that few among medical doctors (healthcare providers [HCPs]) diagnose or treat obesity. 12 , 13 It is unclear if this derives from inadequate recognition of obesity as a disease entity, from perceived access to treatment, or from inadequate appreciation of the benefits of treating obesity for the management of related diseases, or all three.
To investigate beliefs and attitudes about obesity and its treatment among HCPs in Europe, an online survey among medical doctors across multiple disciplines, not specialized in obesity care, was conducted. Specifically, this study aimed to understand how HCPs perceive the relationship between obesity and several well‐known complications of obesity (excluding diabetes) and their views about the value of various weight‐loss therapies to treat obesity‐related diseases.
2. METHODS
The study was a cross‐sectional, non‐interventional online survey among HCPs in eight European countries (United Kingdom, Germany, France, Spain, Italy, Sweden, Switzerland, and Denmark), conducted between February and March 2020. The HCPs were recruited through existing email panels, where they were selected at random from a pool of HCPs within the relevant countries and specialties. The participants did not know the subject of the survey before they chose to participate. Each HCP signed up to the panel, agreeing to participate anonymously in studies such as this one.
To understand the knowledge, experience, and attitudes surrounding the treatment of obesity‐related illnesses among HCPs within different medical specialties in Europe, the study included 12 diseases or conditions that are known to be associated with obesity. The diseases were selected from a comprehensive list of obesity‐related disorders from the systematic literature review by Yuen et al. 2 which identified a total of 236 conditions linked to obesity. The selection was designed to represent different types of well‐known obesity‐related diseases that are treated by clinicians across different medical specialties. A number of selection criteria were applied, including prevalence and incidence of the disease among people in Europe with a body mass index (BMI) ≥35, mortality, and disutility associated with the disease, and the extent to which weight loss has been scientifically documented to improve or reverse the course of the specific disease.
The selected diseases were heart failure with preserved ejection fraction (HFpEF), henceforth heart failure, OA (knee, hips), hypertension, PCOS, cirrhosis (obesity‐related) henceforth cirrhosis, depression, dyslipidemia, OSA, psoriasis, female UI, asthma, and chronic kidney disease/end‐stage renal failure (CKD/ESRF). Since the relationship between obesity and type 2 diabetes is well established 14 and weight reduction is already incorporated into international diabetes guidelines 15 , 16 , 17 for the management of diabetes, this survey did not include diabetes.
Eligible HCPs were medical practitioners in a participating country within the following specialties: cardiology, rheumatology, nephrology, endocrinology, gynecology, psychiatry, hepatology, otorhinolaryngology specializing in sleep medicine, dermatology, urology, pulmonology, and general medicine. The practitioners worked in clinics treating at least one of the selected diseases. The specialties had been selected to match the specialties of the 12 diseases.
All respondents provided electronic informed consent prior to initiation of the screening questions and survey. The survey is attached as Supplementary Material 1. The study complied with all laws and regulations regarding the management of personal information as required by the participant's country of residence and the European General Data Protection Regulation. Therefore, the authors did not have access to information regarding characteristics of the participants such as gender, age, etc. Moreover, the survey complied with the EphMRA code of conduct. 18
2.1. Survey design and testing
A questionnaire was developed in consultation with a multidisciplinary group including survey experts, health economists, public health experts, and medical doctors. A pretest was conducted to assess the clarity and relevance of the questions among HCPs in the target group. The survey was designed to facilitate comparisons across diseases.
2.2. Study subjects and procedure
All individuals could access the first part of the survey, and an initial set of screening questions determined eligibility based on whether the specific diseases were treated at the HCP's clinic. If so, respondents proceeded to the full survey. Respondents were compensated for their time and were recruited primarily via an existing online panel to which they had given permission to be contacted for research purposes. Respondents completed the survey in their native language. All respondents could suspend the survey at any time or point in the survey and for any reason. Respondents were allowed to complete the survey only once. To avoid bias, the study included carefully phrased questions presented in the same order for each respondent. To avoid survey fatigue, they were asked questions about a maximum of three diseases (the disease they mentioned as the disease they treated most often and two other diseases among their selected diseases, chosen at random). HCPs indicating that they treated just one or two of the diseases answered questions about only that/those disease(s).
2.3. Outcomes
Outcomes were measured by end‐anchored 5‐point Likert evaluation scales (to what extent the disease is related to obesity; to what extent weight loss can be used to reverse the disease; to what extent weight loss can be used to avoid progression of the disease; likelihood of using the listed therapy options; likelihood of using pharmacological treatment that targets weight loss, if it were available and reimbursed); numeric response (what percentage of weight loss is necessary to start showing clinical improvement or reversal of the disease); single‐item selection (whether the respondent has recommended/prescribed weight loss therapy [diet, exercise, pharmacotherapy, etc.] to patients with 1 of the 12 diseases in order to assist them in reducing the effects of the disease; whether the respondent considers obesity a disease; whether the respondent thinks obesity should be treated); multiple‐item selection (what weight loss therapy options the respondent has recommended/prescribed; how obesity should be treated); and free text (why the respondent was unlikely to use the therapy option). The full set of questions is available in Supplementary Material 1. Besides the results reported here, the questionnaire also contained a number of additional questions regarding treatment guidelines for the 12 diseases and obesity. The results of this subset of questions are beyond the scope of this report and will be published separately.
The sample target was set at two HCPs within each specialty for each country.
2.4. Analysis
Analysis of data was conducted using Microsoft Excel. Data were summarized using univariate descriptive statistics (means, medians, modes, and frequencies). Data were not weighted.
3. RESULTS
A total of 197 HCPs from eight countries completed the survey (Table S1). HCPs indicated that they each treated an average of 4.7 of the 12 diseases (ranging from 1 to 12 diseases). HCPs provided a total of 448 evaluations of the 12 diseases: 66 evaluations were collected for heart failure, 30 for OA, 51 for hypertension, 32 for PCOS, 31 for cirrhosis, 33 for depression, 40 for dyslipidemia, 43 for OSA, 34 for psoriasis, 31 for female UI, 28 for asthma, and 29 for CKD/ESRF.
The vast majority (89%) of the HCPs considered obesity a disease, ranging from 76% in the United Kingdom to 100% in Italy and Spain. Moreover, nearly all HCPs thought that obesity should be treated (96%), ranging from 88% in Switzerland to 100% in Spain, Italy, and Sweden.
The HCPs reported using a wide range of approaches to treat obesity and were most likely to recommend exercise (94% of HCPs), patient education regarding weight loss (92%), and nutritional counseling (92%). Recommended less often were counseling (therapy, psychologist, etc.) (75%), pharmacological treatment targeting weight loss (68%), and surgical treatment targeting weight loss (66%). These recommendations also varied among countries, with the lowest intent to recommend pharmacological treatment targeting weight loss in Denmark, Italy, and Germany (54%), and the highest in Sweden (79%) and Spain (94%). As the sample per country was relatively small, the country‐specific estimates should be interpreted with caution.
Across all 12 diseases included in this study, an average of 62% of HCPs indicated their belief that the diseases are related to obesity (shown in Figure 1). Specifically, for 8 of the 12 diseases, more than 50% of HCPs stated that the disease is related to obesity to a large or a very large extent. The diseases found to be most closely related to obesity by the HCPs were hypertension and OSA at 92% and 89%, respectively. Psoriasis, female UI, asthma, and CKD/ESRF were deemed least related to obesity (43%, 43%, 28%, and 35%, respectively).
FIGURE 1.
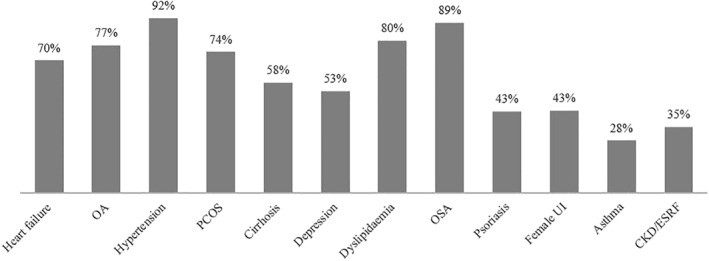
Percentage of healthcare providers who indicated that the disease is related to obesity to a large or a very large extent. HCPs were asked the following questions: Please indicate to what extent you think that the listed disease(s) is/are related to obesity. To what extent are people with obesity more likely to suffer from the following diseases? n = 197, heart failure: n = 66, OA: n = 30, hypertension: n = 51, PCOS: n = 32, cirrhosis: n = 31, depression: n = 33, dyslipidemia: n = 40, OSA: n = 43, psoriasis: n = 34, female UI: n = 31, asthma: n = 28, CKD/ESRF: n = 29. OA, osteoarthritis; PCOS, polycystic ovarian syndrome; OSA, obstructive sleep apnea; UI, urinary incontinence; CKD, chronic kidney disease; ESRF, end‐stage renal failure
Many HCPs indicated a belief that treating obesity can reverse or significantly prevent the progression of all 12 diseases. Specifically, between 66% and 85% of HCPs stated that weight loss could reverse or prevent the progression of hypertension, OSA, dyslipidemia, and OA (data shown in Figure 2). A smaller percentage of HCPs responded that weight loss could reverse the other diseases; nevertheless, at least one in four HCPs believed that all 12 diseases could be reversed by weight loss. Likewise, similar results were found for weight loss to prevent the progression of the diseases (shown in Figure 2); however, a higher percentage of HCPs treating heart failure, OA, PCOS, cirrhosis, dyslipidemia, OSA, female UI, and CKD/ESRF indicated a belief that weight loss can significantly prevent disease progression.
FIGURE 2.
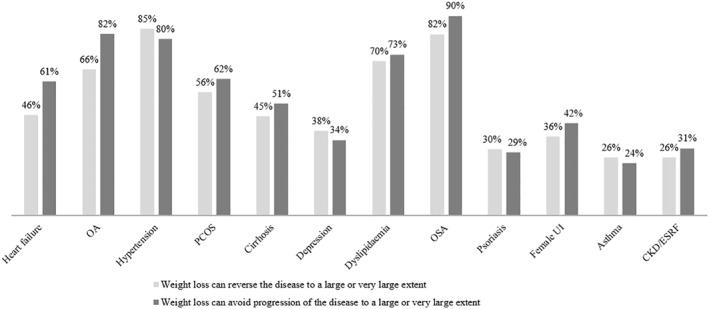
Percentage of healthcare providers (HCPs) who indicated their belief that weight loss can be used to a large or a very large extent to reverse or significantly avoid progression of the diseases. HCPs were asked the following questions: Please indicate to what extent you think that weight loss can be used to reverse the listed disease(s). That is, to what extent would weight loss lead to a remission of the disease? Please indicate to what extent you think that weight loss can be used to significantly avoid progression of the listed disease(s). n = 197, heart failure: n = 66, OA: n = 30, hypertension: n = 51, PCOS: n = 32, cirrhosis: n = 31, depression: n = 33, dyslipidemia: n = 40, OSA: n = 43, psoriasis: n = 34, female UI: n = 31, asthma: n = 28, CKD/ESRF: n = 29. OA, osteoarthritis; PCOS, polycystic ovarian syndrome; OSA, obstructive sleep apnea; UI, urinary incontinence; CKD, chronic kidney disease; ESRF, end‐stage renal failure
Most HCPs believed that patients with obesity must lose a considerable amount of body weight to start reversing any of the 12 diseases (shown in Table 1). For PCOS, depression, psoriasis, female UI, asthma, and CKD/ESRF, the HCPs who evaluated these diseases estimated that an average weight loss of 10% could start reversing the disease. According to the HCPs, OA, cirrhosis, and OSA require the largest weight loss to start reversing the disease (most HCPs stated a mode weight loss of 20%).
TABLE 1.
Percentage weight loss necessary according to the HCPs to start reversing the disease, that is, to show a clinically meaningful/acceptable improvement
| Heart failure | OA | Hypertension | PCOS | Cirrhosis | Depression | Dyslipidemia | OSA | Psoriasis | Female UI | Asthma | CKD/ESRF | Total | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Required weight loss in % according to the HCPs | <5% | 0% | 0% | 3% | 8% | 9% | 10% | 2% | 0% | 24% | 12% | 14% | 8% | 7% |
| 5%–10% | 39% | 32% | 39% | 46% | 28% | 42% | 39% | 27% | 37% | 40% | 46% | 50% | 39% | |
| 11%–20% | 34% | 35% | 30% | 22% | 39% | 26% | 28% | 40% | 25% | 28% | 28% | 28% | 31% | |
| 21%+ | 27% | 32% | 28% | 24% | 25% | 22% | 31% | 32% | 14% | 19% | 12% | 14% | 24% | |
| Calculations | Average | 19% | 23% | 21% | 18% | 18% | 17% | 21% | 23% | 14% | 16% | 13% | 15% | 19% |
| Range (mid‐50%) | 10%–25% | 10%–29% | 10%–25% | 8%–20% | 10%–20% | 8%–25% | 10%–26% | 10%–30% | 5%–25% | 9%–20% | 5%–20% | 10%–20% | 10%–20% | |
| Mode | 10% | 20% | 10% | 10% | 20% | 10% | 10% | 20% | 10% | 10% | 10% | 10% | 10% |
Notes: HCPs were asked the following question: Please indicate for each of the following diseases how large a weight loss in % you believe is necessary to start reversing the disease, that is, to show a clinically meaningful/acceptable improvement.
Please note that numbers are rounded and therefore may not add up to 100%.
n = 197, heart failure: n = 66, OA: n = 30, hypertension: n = 51, PCOS: n = 32, cirrhosis: n = 31, depression: n = 33, dyslipidemia: n = 40, OSA: n = 43, psoriasis: n = 34, female UI: n = 31, asthma: n = 28, CKD/ESRF: n = 29.
Abbreviations: CKD, chronic kidney disease; ESRF, end‐stage renal failure; HCPs, healthcare providers; OA, osteoarthritis; OSA, obstructive sleep apnea ; PCOS, polycystic ovarian syndrome; UI, urinary incontinence.
HCPs were asked about their experience prescribing weight‐loss therapy in relation to the treatment of the 12 diseases. Overall, 68% or more of HCPs have prescribed or recommended weight loss as a treatment to reduce the effects of the diseases (shown in Figure 3). Weight‐loss recommendation was most widely used in relation to OA, PCOS, and OSA, with 90% or more of HCPs having advised patients to lose weight. Sixty‐eight percent of HCPs responded that they have prescribed or recommended weight loss for reducing the effects of psoriasis.
FIGURE 3.
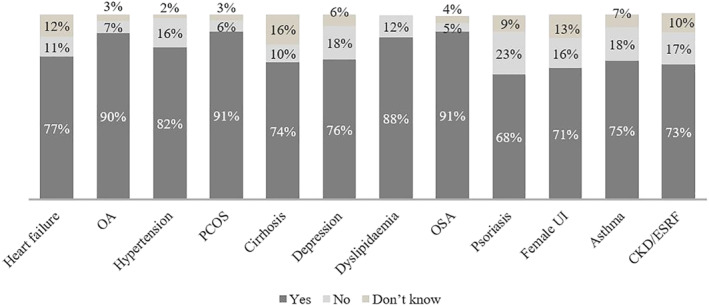
Percentage of healthcare providers (HCPs) who have recommended/prescribed a weight loss treatment (diet, exercise, medication, etc.) to patients in order to assist them in reducing the effects of the disease. HCPs were asked the following question: Have you recommended/prescribed a weight loss treatment (diet, exercise, medication, etc.) to patients with <disease> in order to assist them in reducing the effects of <disease>? n = 197, heart failure: n = 66, OA: n = 30, hypertension: n = 51, PCOS: n = 32, cirrhosis: n = 31, depression: n = 33, dyslipidemia: n = 40, OSA: n = 43, psoriasis: n = 34, female UI: n = 31, asthma: n = 28, CKD/ESRF: n = 29. OA, osteoarthritis; PCOS, polycystic ovarian syndrome; OSA, obstructive sleep apnea; UI, urinary incontinence; CKD, chronic kidney disease; ESRF, end‐stage renal failure
Among HCPs who have recommended a weight‐loss treatment to patients with any of the 12 diseases, lifestyle interventions such as patient education, nutritional counseling, exercise recommendations, and psychological or counseling (therapy, psychologist, etc.) were the most common recommendations (Table 2). In contrast, only between 17% (psoriasis) and 48% (OA and cirrhosis) of HCPs had previously prescribed or recommended anti‐obesity medications (AOMs), and between 30% (psoriasis) and 51% (OSA) had previously prescribed or recommended surgical treatment targeting weight loss (Table 2). AOMs were most commonly prescribed or recommended for OA, PCOS, and cirrhosis.
TABLE 2.
Percentage of HCPs who have recommended different weight‐loss treatments in relation to treating the 12 diseases
| Pharmacological treatment targeting weight loss | Surgical treatment targeting weight loss | Patient education regarding weight loss | Nutritional counseling | Exercise recommendations | Counseling (therapy, psychologist, etc.) | Other non‐pharmacological treatment | |
|---|---|---|---|---|---|---|---|
| Heart failure | 35% | 41% | 90% | 82% | 98% | 59% | 4% |
| OA | 48% | 37% | 100% | 96% | 100% | 52% | 4% |
| Hypertension | 38% | 36% | 98% | 93% | 95% | 57% | 5% |
| PCOS | 45% | 34% | 90% | 97% | 90% | 52% | 3% |
| Cirrhosis | 48% | 43% | 83% | 96% | 91% | 57% | 0% |
| Depression | 40% | 40% | 88% | 96% | 96% | 84% | 4% |
| Dyslipidemia | 43% | 37% | 91% | 97% | 97% | 34% | 3% |
| OSA | 23% | 51% | 95% | 95% | 97% | 59% | 8% |
| Psoriasis | 17% | 30% | 87% | 78% | 83% | 43% | 4% |
| Female UI | 32% | 41% | 77% | 86% | 91% | 55% | 14% |
| Asthma | 33% | 24% | 90% | 95% | 95% | 62% | 10% |
| CKD/ESRF | 38% | 43% | 95% | 100% | 95% | 43% | 5% |
Notes: HCPs were asked the following question: If you answered yes to having prescribed/recommended a weight loss treatment, which ones did you choose?
n = 358, heart failure: n = 51, osteoarthritis: n = 27, hypertension: n = 42, PCOS: n = 29, cirrhosis: n = 23, depression: n = 25, dyslipidemia: n = 35, obstructive sleep apnea: n = 39, psoriasis: n = 23, female UI: n = 22, asthma: n = 21, chronic kidney disease/end‐stage renal failure: n = 21.
Abbreviations: CKD, chronic kidney disease; ESRF, end‐stage renal failure; HCPs, healthcare providers; OA, osteoarthritis; OSA, obstructive sleep apnea; PCOS, polycystic ovarian syndrome; UI, urinary incontinence.
Although the frequency of prescribing AOMs was limited, between 71% (asthma) and 93% (OA) of HCPs stated that if medications were available and reimbursed, they would be likely to prescribe AOMs to a patient with a BMI > 35 who also had one of the 12 diseases (Figure 4).
FIGURE 4.
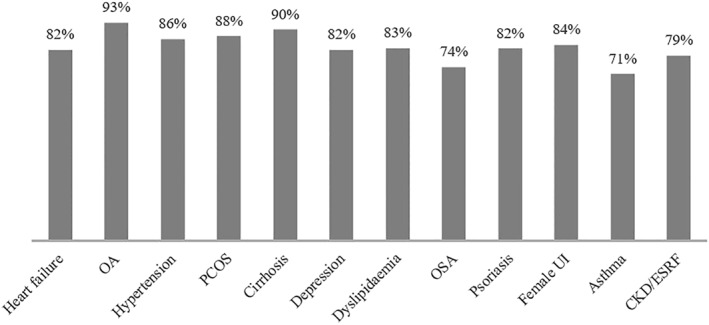
Percentage of healthcare providers (HCPs) who would likely or very likely prescribe pharmacological treatment targeting weight loss if it were available and reimbursed. HCPs were asked the following question: Imagine that you get a patient in your clinic with <disease> who has a body mass index of 38. How likely would you be to use pharmacological treatment targeting weight loss if it were available and reimbursed? n = 197, heart failure: n = 66, OA: n = 30, hypertension: n = 51, PCOS: n = 32, cirrhosis: n = 31, depression: n = 33, dyslipidemia: n = 40, OSA: n = 43, psoriasis: n = 34, female UI: n = 31, asthma: n = 28, CKD/ESRF: n = 29. OA, osteoarthritis; PCOS, polycystic ovarian syndrome; OSA, obstructive sleep apnea; UI, urinary incontinence; CKD, chronic kidney disease; ESRF, end‐stage renal failure
The survey indicated that one of the main barriers to using AOMs is that other weight‐loss modalities (such as diet and exercise) should be tried before other options are considered; this response accounted for 34% of comments regarding why the HCP was unlikely or very unlikely to prescribe AOM to patients with obesity. Moreover, many HCPs were not familiar with AOM options, did not see enough evidence of efficacy, and/or were concerned about potential safety issues (41% of comments). Some HCPs also mentioned that they thought AOMs should be prescribed by the patient's general practitioner or by a practitioner in another healthcare sector (12% of comments). Other reasons were mentioned in the remaining 13% of comments. Those included that HCPs were skeptical regarding the use of AOMs and that it is not a part of the routine to prescribe or recommend AOM.
4. DISCUSSION
The data suggest that many HCPs now acknowledge obesity as a disease and consider its treatment beneficial to patients' health outcomes. However, the data also suggest that a considerable gap in knowledge still exists about the amount of weight loss that is necessary to achieve control of obesity‐related diseases and the relative efficacy and indications of available evidence‐based treatments.
While the relationship between obesity and many other diseases is now well established, this knowledge has not yet translated into integrated clinical practice. Several studies have shown that as low as 5%–10% weight loss can reverse or delay the progression of several diseases that are associated with obesity. 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 Although the majority of HCPs in the current study recognized that weight loss is a means of delaying or reversing the progression of some of the 12 diseases considered in this study, they appeared to significantly overestimate the degree of weight loss that is necessary to do so. For example, for OA and OSA, past studies have found that a 5% 4 , 5 and an 8% 8 , 9 , 10 weight reduction, respectively, have a significant effect on the disease, whereas the HCPs in this study indicated that a 20% weight loss (median/mode) is needed to show a clinically meaningful or acceptable improvement. For all the investigated diseases except asthma and CKD/ESRF, there was a significant discrepancy between HCPs' perception and the results from published literature. This finding indicates a large knowledge gap in understanding the level of weight loss required to substantially improve the course of obesity‐related diseases. Moreover, a large difference in the association between the 12 diseases and obesity was found. For hypertension, dyslipidemia, and OSA, most HCPs agreed that those diseases were related to obesity, whereas for asthma, CKD/ESRF, psoriasis, and female UI, the results were more inconsistent. This finding also highlights the knowledge gap.
Furthermore, the study indicates a substantial knowledge gap in the relationship between weight management and disease progression and reversion for several diseases, especially asthma and psoriasis, for which obesity and weight loss can play a significant role in disease management. 19 Only 24%–30% of the HCPs in this survey believed that weight loss plays an important or a very important role in reversing or delaying progression for the above two obesity‐related conditions. Given the tight link between weight management and improvement of asthma and psoriasis symptoms in other studies, 19 there could be significant advantages for patients if HCPs had better knowledge about this relationship and hence begin advising patients on weight management in relation to those diseases.
The vast majority of respondents in this study signaled they see obesity as a disease that should be treated. However, most HCPs said to have recommended diet and exercise as weight‐loss strategies, and they indicated a belief that these options should be prioritized over evidence‐based methods for weight loss, such as bariatric surgery or AOMs. This finding suggests that many HCPs conceptualize treatment of obesity as a stepwise approach, whereby diet and exercise are used first while surgery or AOMs remain a “last resort” for patients who do not respond to lifestyle interventions. However, compared to the frequency of surgery and the use of AOMs in the included countries among people with obesity, the share of HCPs who have prescribed or recommended these weight‐loss options in this survey is high. Notably, most HCPs (71%–93%) stated that if AOMs were available and reimbursed, they would likely prescribe this to a person with BMI above 38 and with one of the included diseases. This result underscores the awareness of AOMs among HCPs and the willingness to recommend or prescribe AOM if it was available and reimbursed.
At the point of contact with the HCP, the chance of success with diet and exercise is most likely low, since many people with obesity have struggled with their weight for many years prior to having a weight management conversation with an HCP 13 and have already tried unsuccessfully to lose weight using diet and exercise. 20 The preference of HCPs for lifestyle interventions in this study is also at odds with the belief that improving or reversing obesity‐related diseases requires a level of weight loss well beyond what is achievable by non‐surgical and non‐pharmacological interventions. In fact, while lifestyle interventions such as diet and exercise can induce 3%–7% weight loss in the short term, 21 , 22 , 23 , 24 evidence shows that even a relatively modest degree of weight loss can rarely be maintained long term. 25 This paradox underscores the need for improving awareness of current scientific evidence about the relative efficacy of available weight loss treatments among HCPs.
Overestimation of the efficacy of lifestyle interventions, and, on the other one hand, widespread misperceptions about efficacy and safety of surgical and pharmacological anti‐obesity strategies which were found in this survey may explain the reluctance of HCPs in recommending the latter approaches.
Surgical options such as gastric banding, sleeve gastrectomy, and gastric bypass are associated with improvement or resolution of most obesity‐related illnesses and with weight‐loss outcomes ranging between 7%–23%, 26 13%–28%, 27 and 24%–38%, 26 respectively. Modern minimally invasive techniques have dramatically reduced morbidity of bariatric/metabolic surgery in recent decades—with complication rates that compare favorably with those of other commonly performed operations, such as appendectomy, hysterectomy, or knee replacement. 28 Yet, lack of knowledge about the efficacy of surgery and misperception (overestimate) of its risks continue to provide a significant barrier to access to surgical treatment. 29
Important safety issues associated with old weight‐loss drugs that have been eventually withdrawn from the market 30 , 31 may also contribute to misperceptions about the risks of modern AOMs among HCPs.
In fact, in this survey, HCPs attributed their reluctance in prescribing AOMs to potential safety issues and a lack of evidence regarding their efficacy. This is despite available clinical evidence documenting the safety and efficacy of modern AOMs, which can induce loss of up to 10% of body weight. 32 , 33 Several new drugs for the treatment of obesity are also under clinical development. With these new drugs in development, and given HCPs' increasing recognition that obesity is a disease entity requiring treatment, AOMs offer potential for vast expansion of obesity care; this could lead to a decrease in the far‐reaching, rapidly expanding burden of obesity on both patients and the healthcare sector throughout Europe. 34 AOMs can also be seen as an adjuvant treatment to enhance the efficacy of other options—a bridge toward a more consistent weight loss. 25
This study has several limitations that include a relatively low sample size per country/disease, its cross‐sectional and descriptive nature, and the fact that the HCPs were compensated for answering the survey, which may bias results. In addition, specialties and treatment experience were self‐reported. The HCPs from the chosen specialties, however, were selected at random from an online panel and were not briefed beforehand about the subject of the survey, thus mitigating selection bias. To our knowledge, this is also the first study to specifically aim at obtaining a snapshot of the current beliefs and attitudes toward the use of weight‐loss treatment strategies as part of the management of obesity‐related diseases among European HCPs.
The findings that most HCPs in Europe acknowledge obesity as a disease and consider obesity treatment beneficial to patients' health are consistent with the results of other studies in different regions of the world. 13 Given that many people with obesity are generally highly motivated to lose weight, HCPs' awareness of the importance of obesity should provide an opportunity for earlier adoption of weight loss options in the management of diseases that are known to be ameliorated by obesity reduction.
However, despite a large body of scientific evidence demonstrating the safety and efficacy of modern pharmacological and surgical interventions for obesity, most HCPs in this study appeared reluctant in recommending such approaches and overwhelmingly prefer lifestyle interventions such as diet and exercise, which have limited long‐term effectiveness. These findings underscore the need for improved education of HCPs about currently available, evidence‐based treatments of obesity and their beneficial effects on obesity‐related diseases.
CONFLICT OF INTEREST
Francesco Rubino has received research grants from Ethicon and Medtronic, consulting fees from Ethicon, Medtronic, and Novo Nordisk, and he is part of the scientific advisory board of GI Dynamics and Keyron.
Jennifer Logue has received research support from Slimming World and consulting fees from Novo Nordisk.
Ulrik Haagen Panton, Ana‐Paula Cancino, and Maria Høy are employees at Novo Nordisk A/S. Mette Bøgelund and Maria Elmegaard Madsen are employees at Incentive Denmark ApS, which is a paid vendor of Novo Nordisk A/S.
As employees of Novo Nordisk A/S, Ana‐Paula Cancino, Maria Høy, and Ulrik Haagen Panton are part of a Novo Nordisk A/S stock option program.
AUTHOR CONTRIBUTIONS
All authors contributed to the study design, the interpretation of the results, and the drafting of the manuscript. All authors have approved the final version of the manuscript to be published and agree to be accountable for all aspects of the work.
Supporting information
Supplementary Material
TABLE S1
ACKNOWLEDGMENT
This work was supported by Novo Nordisk North West Europe Pharmaceuticals A/S.
Rubino F, Logue J, Bøgelund M, et al. Attitudes about the treatment of obesity among healthcare providers involved in the care of obesity‐related diseases: a survey across medical specialties in multiple European countries. Obes Sci Pract. 2021;7(6):659‐668. 10.1002/osp4.518
REFERENCES
- 1. Pineda E, Sanchez‐Romero LM, Brown M, et al. Forecasting future trends in obesity across Europe: the value of improving surveillance. Obes Facts. 2018;11:360‐371. 10.1159/000492115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Yuen M, Earle RL, Kadambi N, et al. A Systematic Review and Evaluation of Current Evidence Reveals 236 Obesity‐Associated Disorders (ObAD). 2016. Poster T‐P‐3166 [Google Scholar]
- 3. World Obesity Day . Global Data on Numbers of Adults Affected. 2020. [Google Scholar]
- 4. Bliddal H, Leeds AR, Christensen R. Osteoarthritis, obesity and weight loss: evidence, hypotheses and horizons – a scoping review. Obes Rev. 2014;15:578‐586. 10.1111/obr.12173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Riddle DL, Stratford PW. Body weight changes and corresponding changes in pain and function in persons with symptomatic knee osteoarthritis: a cohort study. Arthritis Care Res. 2013;65:15‐22. 10.1002/acr.21692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Jamal M, Gunay Y, Capper A, Eid A, Heitshusen D, Samuel I. Roux‐en‐Y gastric bypass ameliorates polycystic ovary syndrome and dramatically improves conception rates: a 9‐year analysis. Surg Obes Relat Dis. 2012;8:440‐444. 10.1016/j.soard.2011.09.022 [DOI] [PubMed] [Google Scholar]
- 7. Legro RS, Dodson WC, Kris‐Etherton PM, et al. Randomized controlled trial of preconception interventions in infertile women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2015;100:4048‐4058. 10.1210/jc.2015-2778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Johansson K, Hemmingsson E, Harlid R, et al. Longer term effects of very low energy diet on obstructive sleep apnoea in cohort derived from randomised controlled trial: prospective observational follow‐up study. Br Med J. 2011;342:3017. 10.1136/bmj.d3017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tuomilehto HPI, Seppä JM, Partinen MM, et al. Lifestyle intervention with weight reduction. Am J Respir Crit Care Med. 2009;179:320‐327. 10.1164/rccm.200805-669OC [DOI] [PubMed] [Google Scholar]
- 10. Ashrafian H, Toma T, Rowland SP, et al. Bariatric surgery or non‐surgical weight loss for obstructive sleep apnoea? A systematic review and comparison of meta‐analyses. Obes Surg. 2015;25:1239‐1250. 10.1007/s11695-014-1533-2 [DOI] [PubMed] [Google Scholar]
- 11. Subak LL, Wing R, West DS, et al. Weight loss to treat urinary incontinence in overweight and obese women. N Engl J Med. 2009;360:481‐490. 10.1056/NEJMoa0806375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kaplan LM, Golden A, Jinnett K, et al. Perceptions of barriers to effective obesity care: results from the national ACTION study. Obesity. 2018;26:61‐69. 10.1002/oby.22054 [DOI] [PubMed] [Google Scholar]
- 13. Caterson ID, Alfadda AA, Auerbach P, et al. Gaps to bridge: misalignment between perception, reality and actions in obesity. Diabetes Obes Metab. 2019;21:1914‐1924. 10.1111/dom.13752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. International Diabetes Federation . About Diabetes. https://idf.org/aboutdiabetes/type‐2‐diabetes.html Accessed April 8, 2020 [Google Scholar]
- 15. Davies MJ, D’Alessio DA, Fradkin J, et al. Management of hyperglycaemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia. 2018;61:2461‐2498. [DOI] [PubMed] [Google Scholar]
- 16. Adler A, Bailey C, Chan J, et al. IDF Clinical Practice Recommendations for Managing Type 2 Diabetes in Primary Care. International Diabetes Federation; 2017. [Google Scholar]
- 17.Task Force for diabetes, pre‐diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) European Association for the Study of diabetes (EASD), Rydén L, et al. 2019 ESC guidelines on diabetes, pre‐diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020;41:255‐323. [DOI] [PubMed] [Google Scholar]
- 18. EphMRA . Code of Conduct 2019. 2019. https://www.ephmra.org/media/2811/ephmra‐2019‐code‐of‐conduct‐doc‐f.pdf. Accessed June 12, 2020. [Google Scholar]
- 19. Juel CT‐B, Ali Z, Nilas L, Ulrik CS. Asthma and obesity: does weight loss improve asthma control? a systematic review. J Asthma Allergy. 2012;5:21‐26. 10.2147/JAA.S32232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Santos I., Sniehotta F. F, Marques MM, Carraça EV, Teixeira PJ. Prevalence of personal weight control attempts in adults: a systematic review and meta‐analysis. Obes Rev. 2017;18:32‐50. 10.1111/obr.12466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Look AHEAD Research Group , Wing RR. Long‐term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes mellitus: four‐year results of the Look AHEAD trial. Arch Intern Med. 2010;170:1566‐1575. 10.1001/archinternmed.2010.334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wing RR. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care. 2011;34:1481‐1486. 10.2337/dc10-2415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lean MEJ, Leslie WS, Barnes AC, et al. Durability of a primary care‐led weight‐management intervention for remission of type 2 diabetes: 2‐year results of the DiRECT open‐label, cluster‐randomised trial. Lancet Diabetes Endocrinol. 2019;7:344‐355. 10.1016/S2213-8587(19)30068-3 [DOI] [PubMed] [Google Scholar]
- 24. Tsai AG, Wadden TA. The evolution of very‐low‐calorie diets: an update and meta‐analysis. Obes Silver Spring Md. 2006;14:1283‐1293. 10.1038/oby.2006.146 [DOI] [PubMed] [Google Scholar]
- 25. Wadden TA, Tronieri JS, Butryn ML. Lifestyle modification approaches for the treatment of obesity in adults. Am Psychol. 2020;75:235‐251. 10.1037/amp0000517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Courcoulas AP, Christian NJ, Belle SH, et al. Weight change and health outcomes at 3 years after bariatric surgery among individuals with severe obesity. J Am Med Assoc. 2013;310:2416‐2425. 10.1001/jama.2013.280928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Berry MA, Urrutia L, Lamoza P, et al. Sleeve gastrectomy outcomes in patients with BMI between 30 and 35 – 3 years of follow‐up. Obes Surg. 2018;28:649‐655. 10.1007/s11695-017-2897-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cefalu WT, Rubino F, Cummings DE. Metabolic surgery for type 2 diabetes: changing the landscape of diabetes care. Diabetes Care. 2016;39:857‐860. 10.2337/dc16-0686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Funk LM, Jolles S, Fischer LE, Voils CI. Patient and referring practitioner characteristics associated with the likelihood of undergoing bariatric surgery. JAMA Surg. 2015;150:999. 10.1001/jamasurg.2015.1250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Tak YJ, Lee SY. Anti‐obesity drugs: long‐term efficacy and safety: an updated review. World J Mens Health. 2021;39:208‐214. 10.5534/wjmh.200010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Onakpoya IJ, Heneghan CJ, Aronson JK. Post‐marketing withdrawal of anti‐obesity medicinal products because of adverse drug reactions: a systematic review. BMC Med. 2016;14:1‐11. 10.1186/s12916-016-0735-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wadden TA, Walsh OA, Berkowitz RI, et al. Intensive behavioral therapy for obesity combined with liraglutide 3.0 mg: a randomized controlled trial. Obesity. 2019;27:75‐86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Wadden TA, Foreyt JP, Foster GD, et al. Weight loss with naltrexone SR/bupropion SR combination therapy as an adjunct to behavior modification: the COR‐BMOD trial. Obes Silver Spring Md. 2011;19:110‐120. 10.1038/oby.2010.147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Srivastava G, Apovian C. Future pharmacotherapy for obesity: new anti‐obesity drugs on the horizon. Curr Obes Rep. 2018;7:147‐161. 10.1007/s13679-018-0300-4 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material
TABLE S1


