Key Points
Question
What are the sociodemographic characteristics of adults who engage in high-frequency cannabis use?
Findings
In this survey study including 387 157 US adults residing in 21 states conducted in 2016 through 2019, young, male, Black, and Native American individuals and individuals with low educational attainment and income were more likely to engage in higher frequency cannabis use.
Meaning
Higher-frequency use among these populations may warrant more attention from policymakers and public health officials in the form of screening, risk stratification, and treatment given the known and emerging adverse health effects of cannabis.
This survey study of 21 US states and 2 US territories examines social and demographic characteristics associated with the frequency of cannabis use among adults.
Abstract
Importance
Cannabis use has increased, but there are few studies on frequent and daily cannabis use among US adults. Individuals who engage in higher frequency use may suffer more health consequences.
Objective
To examine frequency of cannabis use and associated factors among US adults.
Design, Setting, and Participants
This survey study included data from 21 US states and 2 US territories reported in the Behavioral Risk Factor Surveillance System surveys from 2016 to 2019. Cross-sectional data on US adults ages 18 years and older were used to estimate demographic, socioeconomic, and behavioral risk factors for cannabis use, taking into account the survey strata and sampling weights for the 4 years of combined data. Using a multivariable ordinal logistic analysis, the association of demographic, socioeconomic status, and behavioral risk factors with past month cannabis frequency were examined.
Exposures
Sociodemographic characteristic, ie, age, gender, race and ethnicity, educational attainment, employment status, and annual household income.
Main Outcomes and Measures
Ordinal categorization of number of days of cannabis use in the past 30 days in terms of nonuse, infrequent use (1-5 days), frequent use (6-29 days), and daily use.
Results
Among the 387 179 respondents, 58 009 (27.9%) were ages 18 to 34 years, 186 923 (50.3%) were ages 35 to 64 years, and 142 225 (21.8%) were age 65 years or older (mean [SD] age, 48.3 [0.1] years). The sample included 28 345 (9.8%) Black, 36 697 (22.6%) Hispanic, and 292 210 (57.3%) White respondents. Smoking was the most common form of cannabis use. The frequency of cannabis use varied significantly by age, gender, race, marital status, education, and employment. Higher frequency cannabis use was associated with younger age (ages 18-34 years: adjusted odds ratio [aOR], 4.12; 95% CI, 3.63-4.68; ages 35-64 years: aOR, 2.22; 95% CI, 1.98-2.49), Black (aOR, 1.46; 95% CI, 1.33-1.71) and Native American (aOR, 1.25; 95% CI, 1.04-1.52) race, and less educational attainment (high school or less: aOR, 1.09; 95% CI, 1.02-1.17; some college: aOR, 1.27; 95% CI, 1.19-1.35). Being married (aOR, 0.54; 95% CI, 0.51-0.58) or identifying as Asian (aOR, 0.60; 95% CI, 0.51-0.71) or Hispanic (aOR, 0.71; 95% CI, 0.65-0.77) was associated with lower-frequency cannabis use after accounting for other baseline factors.
Conclusions and Relevance
This nationally based study found that higher-frequency cannabis use is more common among young and racial minority populations, as well as respondents with low socioeconomic status. Given the known and emerging negative health effects of cannabis use, more attention may need to be paid to high-frequency use among underserved populations in the form of screening, risk stratification, and treatment.
Introduction
From 2002 to 2019, past-year prevalence of cannabis use increased from 10.4% to 18.0%, while daily or almost daily use (ie, 300 or more days per year) increased from 1.3% to 3.9% among US adults.1 Despite the dramatic rise in past-year cannabis use and daily or almost daily use, the distribution of use frequency (ie, days per month) and determinants of higher-frequency use have not been adequately described.
Evidence for the adverse mental and physical health effects of cannabis is emerging. While the existing evidence base is insufficient and includes few studies at low risk of bias, some studies have shown that cannabis use is associated with adverse effects including respiratory symptoms (cough and sputum production), tachycardia, and some forms of cancer.2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19 Long-term cannabis use is associated with deficits in memory among adults.20 Long-term cannabis use is associated with poor educational outcomes and increased risk of psychotic disorders, although some experts believe a causal link is not yet established.21,22,23,24,25 Cannabis use may negatively affect mental health treatment outcomes for patients with anxiety and depression, and use is associated with suicidal ideation.26,27,28,29,30,31,32,33,34 Finally, recent data suggests that that 1 out of 5 individuals who use cannabis have a cannabis use disorder.35
Studies that have examined the health effects of cannabis have used various measures of exposure (eg, ever use, past-year use, monthly use, daily and almost daily use); however, there is a wide spectrum of outcomes for use frequency within the past month.36 While daily use is likely to have the most effect, like alcohol, there may be a gradient of outcomes based on frequency of use.37
An annual cannabis module was added to the Centers for Disease Control and Prevention’s Behavioral Risk Factor Surveillance System (BRFSS) in 2016, which allows evaluation of cannabis use patterns among adults (ages 18 and older) in 23 states and territories.38 We examined the distribution of frequency of use and factors associated with higher frequency use using the BRFSS survey. Understanding prevalence of cannabis use and frequency of use in different populations will shed light on groups most likely to be affected by the health consequences of use.
Methods
Data Source
We combined 2016 through 2019 BRFSS data from 21 American states and 2 US territories participating in the cannabis module during at least 1 of these years (eTable 1 in the Supplement). BRFSS is a telephone-administered survey that collects data from a representative sample of US adult residents regarding health-related risk behaviors, chronic conditions, and health care access.38 This study is based on publicly available deidentified data and is exempt from institutional review board review and informed consent requirements.
This study followed the American Association for Public Opinion Research (AAPOR) reporting guideline; response rates for BRFSS data were calculated using standards set by AAPOR response rate formula 4.39 The response rate is the number of respondents who completed the survey as a proportion of all eligible and likely eligible people. The median (IQR) survey response rates for all states, territories and Washington, DC, in 2016, 2017, 2018, and 2019 were 46.7% (41.2%-54.5%), 44.9% (38.6%-51.5%), 49.8% (44.2%-55.0%), and 50% (44.1%-55.3%), respectively, and ranged from 30.6% to 73.1%. Response rates for states and territories included in this analysis had a median of 49.8% and ranged from 31.1% to 65.0%. For detailed information see the BRFSS Summary Data Quality Report.89
Analytic Sample
To assess cannabis use in the past month, we used the question, “During the past 30 days, on how many days did you use marijuana or hashish?” Response options included any number of days from 0 to 30, “Don’t know,” or refusing to answer the question. We excluded the 0.8% of respondents who answered “Don’t know” or refused to answer, leaving 387 157 respondents living in 21 states (ie, Alaska, California, Colorado, Florida, Georgia, Idaho, Illinois, Maryland, Minnesota, Mississippi, Montana, Nebraska, New Hampshire, North Dakota, Ohio, Oklahoma, South Carolina, Tennessee, Utah, West Virginia, Wyoming) and 2 territories (Guam, Puerto Rico) (unweighted sample sizes in Table 1). To assess the primary form of past-month cannabis use, we used the question, “During the past 30 days, which one of the following ways did you use marijuana the most often? Did you usually….” Response options included, smoke it, eat it, drink it, vaporize it (“in an e-cigarette-like vaporizer or other vaporizing device”), dab it (“using waxes or concentrates”), use it some other way, or “Don’t know/Not sure” or “Refused.” We used an answer of zero days to the question of past-month cannabis use to categorize nonuse. There were 6350 cannabis users within the past month who did not respond to the question on forms of use.
Table 1. Unweighted Number of Respondents by Past-Month Cannabis Use Frequency Categories Among Respondents of Behavioral Risk Factor Surveillance System Cannabis Module in Years 2016-2019.
| Characteristics | Respondents, No. (%) | ||||
|---|---|---|---|---|---|
| Cannabis use in past month | Frequency of past-month use among cannabis usersa | ||||
| Nonuse | Current use | Infrequent | Frequent | Daily | |
| Total | 361 847 | 25 310 | 9904 | 6951 | 8455 |
| Age, y | |||||
| 18-34 | 48 842 | 9167 | 3447 | 2641 | 3079 |
| 35-64 | 174 051 | 12 872 | 5052 | 3379 | 4441 |
| >65 | 138 954 | 3271 | 1405 | 931 | 935 |
| Sex | |||||
| Men | 156 023 | 15 348 | 5727 | 4303 | 5318 |
| Women | 205 696 | 9951 | 4176 | 2643 | 3132 |
| Race and ethnicity | |||||
| African American | 26 170 | 2175 | 847 | 489 | 839 |
| Asian, Native Hawaiian, or Pacific Islander | 8959 | 623 | 334 | 148 | 141 |
| Hispanic | 34 112 | 2585 | 1032 | 701 | 852 |
| Native American | 4916 | 693 | 207 | 172 | 314 |
| White | 274 435 | 17 775 | 6987 | 5049 | 5739 |
| Other | 7379 | 1022 | 349 | 274 | 399 |
| Marital status | |||||
| Not married | 164 301 | 16 852 | 6356 | 4636 | 5860 |
| Married | 195 508 | 8333 | 3508 | 2273 | 2552 |
| Education | |||||
| ≤High school degree | 125 669 | 9448 | 3229 | 2363 | 3856 |
| Some college | 101 287 | 8389 | 3203 | 2397 | 2789 |
| College degree | 133 840 | 7440 | 3461 | 2178 | 1801 |
| Employment | |||||
| Employed | 175 107 | 14 769 | 5899 | 4004 | 4866 |
| Unemployed | 37 706 | 4932 | 1622 | 1296 | 2014 |
| Student | 7809 | 1372 | 670 | 425 | 277 |
| Retiree | 118 416 | 3387 | 1396 | 979 | 1012 |
| Homemaker | 20 598 | 726 | 272 | 205 | 249 |
| Annual household income, $ | |||||
| <25 000 | 79 775 | 7478 | 2625 | 1966 | 2887 |
| 25 000 to <75 000 | 124 534 | 6469 | 3338 | 24,53 | 3131 |
| ≥75 000 | 102 364 | 6271 | 2909 | 1829 | 1533 |
| Legality of cannabis in state of residence | |||||
| Nonlegal | 137 605 | 6761 | 2742 | 1795 | 2224 |
| Legalized cannabis | |||||
| Medical | 185 194 | 12 721 | 4943 | 3436 | 4342 |
| Recreational | 39 048 | 5828 | 2219 | 1720 | 1889 |
| Smoker | |||||
| Current | 45 074 | 9416 | 2989 | 2515 | 3912 |
| Former | 101 291 | 7412 | 2808 | 2074 | 2530 |
| Never | 213 411 | 8364 | 4056 | 2328 | 1980 |
| e-Cigarette use | |||||
| Current | 6770 | 2327 | 718 | 671 | 938 |
| Former | 28 575 | 6919 | 2552 | 1945 | 2422 |
| Never | 222 086 | 7557 | 3433 | 1971 | 2153 |
| No e-cigarette questionb | 83 460 | 7373 | 2757 | 2078 | 2538 |
| Alcohol | |||||
| Any alcohol in past 30 d | 172 702 | 18 163 | 7637 | 5161 | 5365 |
| Any alcohol binges in past 30 d | 39 008 | 9294 | 3827 | 2791 | 2676 |
Infrequent use was defined as 1 to 5 days of cannabis use in the past month; frequent, as 6 to 29 days; and daily, as 30 days of use in the past month.
The 2019 survey did not include a question about e-cigarette use.
Independent Variables
Demographic variables were age, gender, marital status, and self-identified race and ethnicity. Race and ethnicity were coded mutually exclusively as Hispanic, non-Hispanic Asian and Pacific Islander, non-Hispanic Black, non-Hispanic Native American or Alaskan Native, non-Hispanic White, and other.
Socioeconomic status was represented by educational attainment, employment status, and annual household income. Educational attainment was categorized by combining 4 categories corresponding to high school degree or less, some college, and college degree. Employment status was divided into employed, unemployed, student, retired, and homemaker categories. The educational and employment categories were defined by BRFSS. Annual household income was divided into less than $25 000, $25 000 to $74 999, and $75 000 or higher categories corresponding to 2019 federal annual thresholds for family of 4 poverty and median income.40,41 Legality of cannabis in state of residence for an individual was determined by their year of response to the BRFSS survey and divided into 3 separate categories: nonlegal cannabis, legalized medical cannabis, and legalized recreational cannabis (eTable 1 in the Supplement). All states that had legalized recreational cannabis also had legalized medical cannabis.
We controlled for differences in the behavioral risk factor domain of current, former, and nonuse of cigarettes and e-cigarettes, current alcohol use, and current binge drinking by including these covariates in the model. People who engaged in past-month binge drinking were a subset of past-month users of alcohol, where binge drinking was defined as responding to the following question with any number greater than zero, “Considering all types of alcoholic beverages, how many times during the past 30 days did you have 5 or more drinks for men or 4 or more drinks for women on an occasion?”
Outcome
We first categorized persons who use cannabis into daily and nondaily use and nonuse. To create a more granular distribution of cannabis use frequency, we divided nondaily use into infrequent and frequent nondaily use based on the median number of days of nondaily use (5 days). Thus, we categorized frequency of cannabis use into 4 categories: nonuse, infrequent (1-5 days), frequent (6-29 days), and daily cannabis use in the past 30 days.
Statistical Analysis
Weighted estimates of demographic, socioeconomic, and behavioral risk factors were calculated using survey strata and sampling weights for the 4 years of combined data to obtain representative results for the combined states using the cannabis module.42 P values for bivariate analyses were calculated by the Rao-Scott corrected χ2 test.
We conducted a multivariable ordinal logistic analysis of the association of past-month cannabis use ordinal frequency category (nonuse, infrequent, frequent, and daily use) as a function of demographic, socioeconomic status, and behavioral risk factors, accounting for the complex survey design of BRFSS. The proportional odds ratio (OR) assumption of an ordinal regression assumes that the associations between the highest vs all lower categories of the outcome variable are the same as those that describe the associations between the next highest category and all lower categories.43 We statistically and graphically tested the proportional OR assumption and the assumption was met. An OR greater than 1 for a certain variable implied that this variable was associated with higher frequency of use than the reference category, while an OR less than 1 implied that this variable was associated with a lower frequency of cannabis use.
Income had the highest degree of missingness, with 14.9% of the variables used in the ordinal regression. Listwise deletion of all cases with any missing variables resulted in data loss of 22.6% of the sample, necessitating multiple imputation.44 The multivariable ordinal logistic analysis was conducted using 23 multiple imputations with chained equations using the R statistical software version 4.0 (R Project for Statistical Computing) amelia package.45 Statistics were performed using the R survey package.
We conducted 2 sensitivity analyses to examine the robustness of our findings: (1) multivariable ordinal logistic regression in the set of complete cases was used to examine whether findings of the analyses employing imputed data and complete cases were similar; (2) because the 2 US territories (Guam and Puerto Rico) might affect ordinal logistic regression estimates on race and ethnicity, we excluded respondents from the 2 territories.
Results
Among the 387 179 respondents to the cannabis module, the prevalence of cannabis nonuse was 90.0% (361 847 respondents), infrequent cannabis use (ie, 1 to 5 days; median [IQR] use, 2 [1-3] days) was 3.7% (9904 respondents), frequent use (6 to 29 days; median [IQR] use, 15 [10-20] days) was 2.8% (6951 respondents), and daily use was 3.5% (8455 respondents).
The mean (SD) age of the respondents was 48.3 (0.1) years. Approximately 27.9% of individuals were ages 18 to 34 years in our weighted sample estimate, 50.3% were ages 35 to 64 years, and 21.8% were over age 65 years. More than half (51.5%) were women and the majority of the respondents were White (57.3%), 7.6% Asian, 9.8% were Black, 22.6% Hispanic, 0.8% Native American, and 1.9% other. About 40.9% had a high school education or less, and 27.2% had a college degree. Most of the sample were never smokers (61.4%), 24.2% had formerly smoked tobacco, and 14.4% currently smoked tobacco. Similarly, 59.3% of respondents were persons who had never used e-cigarettes, 12.4% were persons who formerly used e-cigarettes, 3.2% currently used e-cigarettes, and 25.1% of the sample were not asked a question about e-cigarette use in 2019. Over half of the sample consumed at least 1 alcoholic beverage in the past 30 days, while 15.6% had engaged in binge drinking within the past month.
Variation in the Prevalence and Frequency of Cannabis Use Among Different Sociodemographic Groups
Among respondents, 10.1% (95% CI, 9.8%-10.2%) used cannabis in the past month, including 3.8% (95% CI, 3.6%-3.8%) with infrequent use, 2.8% (95% CI, 2.7%-2.9%) with frequent use, and 3.5% (95% CI, 3.4%-3.7%) with daily use (Table 2). Smoking was the most common form of cannabis use (5.5%), followed by vaping (0.9%) and edibles (0.8%) (eFigure 1 in the Supplement). Daily use was more common among individuals who used smoked cannabis, while infrequent use was more common among those using edible cannabis (eFigure 1 in the Supplement)
Table 2. Past-Month Cannabis Use Frequency Categories Among Respondents of Behavioral Risk Factor Surveillance System Cannabis Module Between Years 2016 and 2019a .
| Covariates | Respondents, weighted % (95% CI) | P valuec | ||||
|---|---|---|---|---|---|---|
| Past-month cannabis use | Frequency of past-month use among cannabis usersb | |||||
| Nonusers | Current users | Infrequent | Frequent | Daily | ||
| Total | 90.0 (89.8-90.2) | 10.0 (9.8-10.2) | 3.8 (3.6-3.8) | 2.8 (2.7-2.9) | 3.5 (3.4-3.7) | |
| Age, y | ||||||
| 18-34 | 25.3 (25.0-25.7) | 49.9 (48.7-51.1) | 48.3 (46.4-50.1) | 51.9 (49.7-54.1) | 50.1 (48.0-52.1) | <.001 |
| 35-64 | 51.1 (50.7-51.4) | 43.3 (42.1-44.4) | 44.1 (42.3-46.0) | 41.0 (38.8-43.1) | 44.2 (42.2-46.2) | |
| ≥65 | 23.6 (23.3-23.9) | 6.8 (6.3-7.3) | 7.6 (6.8-8.4) | 7.1 (6.2-8.1) | 5.7 (4.0-6.5) | |
| Sex | ||||||
| Men | 46.7 (46.4-47.1) | 61.6 (60.5-62.8) | 57.8 (56.0-59.7) | 62.2 (60.0-64.3) | 65.2 (63.3-67.2) | <.001 |
| Women | 53.3 (52.9-53.6) | 38.4 (37.2-39.5) | 42.2 (40.3-44.0) | 37.8 (35,7-40.0) | 34.8 (32.8-36.7) | |
| Race and ethnicity | ||||||
| African American | 11.2 (11.0-11.5) | 14.1 (13.1-15.0) | 12.5 (11.1-13.8) | 12.9 (11.1-14.7) | 16.8 (15.0-18.6) | <.001 |
| Asian, Native Hawaiian, or Pacific Islander | 6.1 (5.8-6.3) | 4.3 (3.7-4.9) | 6.0 (4.8-7.1) | 4.3 (3.2-5.3) | 2.7 (1.9-3.5) | |
| Hispanic | 20.4 (20.1-20.7) | 17.9 (16.9-18.8) | 19.0 (17.4-20.6) | 17.3 (15.6-19.0) | 17.2 (15.5-18.8) | |
| Native American | 0.8 (0.8-0.9) | 1.3 (1.1-1.5) | 1.0 (0.7-1.2) | 1.1 (0.8-1.4) | 1.8 (1.6-1.9) | |
| White | 59.8 (59.5-60.2) | 59.5 (58.4-60.8) | 59.0 (57.1-60.9) | 61.9 (59.6-64.1) | 58.4 (56.3-60.5) | |
| Other | 1.7 (1.6-1.7) | 2.8 (2.5-3.1) | 2.6 (2.2-3.1) | 2.5 (2.0-3.2) | 3.2 (2.7-3.7) | |
| Marital status | ||||||
| Not married | 46.9 (46.6-47.3) | 70.5 (69.5-71.6) | 68.8 (67.1-70.5) | 70.0 (68.0-72.1) | 72.7 (70.9-74.5) | <.001 |
| Married | 53.1 (52.7-53.4) | 29.5 (28.3-30.5) | 31.2 (29.5-32.3) | 30.0 (27.9-32.0) | 27.3 (25.5-29.1) | |
| Education | ||||||
| ≤High school degree | 41.1 (40.8-41.5) | 41.3 (40.1-42.5) | 35.8 (34.0-37.6) | 36.7 (34.6-38.9) | 50.7 (48.6-52.3) | <.001 |
| Some college | 31.0 (30.6-31.3) | 38.7 (37.6-39.9) | 39.1 (37.2-41.0) | 41.5 (39.3-43.8) | 36.2 (34.2-38.2) | |
| College degree | 27.9 (27.6-28.2) | 20.0 (10.2-20.7) | 25.1 (23.6-26.5) | 21.7 (20.2-23.2) | 13.2 (12.1-14.3) | |
| Employment | ||||||
| Employed | 55.7 (55.3-56.0) | 63.4 (62.6-64.8) | 63.2 (61.4-65.0) | 63.5 (61.4-65.6) | 64.3 (62.4-66.2) | <.001 |
| Unemployed | 11.5 (11.3-11.8) | 16.9 (16.1-17.7) | 14.3 (13.1-15.5) | 16.3 (14.7-17.9) | 20.1 (18.5-21.6) | |
| Student | 4.9 (4.7-5.1) | 8.8 (8.1-9.5) | 11.4 (10.1-12.7) | 9.2 (7.9-10.5) | 5.7 (4.6-6.9) | |
| Retiree | 20.8 (20.6-21.1) | 7.7 (7.2-8.3) | 8.0 (7.1-8.9) | 8.0 (7.1-9.0) | 7.2 (6.3-8.1) | |
| Homemaker | 7.0 (6.9-7.2) | 2.9 (2.5-3.3) | 3.1 (2.5-3.8) | 2.9 (2.2-3.6) | 2.7 (2.1-3.3) | |
| Annual household income, $ | ||||||
| <25 000 | 27.9 (27.6-28.3) | 30.4 (29.3-31.5) | 26.8 (25.2-28.5) | 29.1 (27.1-31.2) | 35.1 (33.1-37.2) | <.001 |
| 25 000 to <75 000 | 37.6 (37.2-37.9) | 37.3 (36.1-38.5) | 36.1 (34.2-38.0) | 36.3 (34.1-38.5) | 39.3 (37.1-41.4) | |
| ≥75 000 | 34.5 (34.2-34.9) | 32.3 (31.1-33.5) | 37.1 (35.1-39.0) | 34.5 (32.3-36.8) | 25.6 (23.5-27.6) | |
| Legality of cannabis in state of residence | ||||||
| Nonlegal | 32.5 (32.3-32.8) | 22.9 (22.0-23.9) | 22.9 (21.4-24.4) | 22.2 (20.3-24.1) | 23.6 (21.9-25.3) | <.001 |
| Legalized cannabis | ||||||
| Medical | 43.9 (43.7-44.2) | 41.7 (40.6-42.9) | 41.6 (39.8-43.5) | 40.1 (38.0-42.3) | 43.1 (41.0-45.1) | |
| Recreational | 23.5 (23.3-23.8) | 35.3 (34.6-36.4) | 35.4 (33.7-37.2) | 37.7 (35.6-39.8) | 33.3 (31.5-35.2) | |
| Smoker | ||||||
| Current | 13.0 (12.7-13.2) | 34.5 (33.3-35.6) | 26.5 (24.8-28.1) | 33.7 (31.6-35.8) | 43.5 (41.4-45.5) | <.001 |
| Former | 24.0 (23.7-24.3) | 26.1 (25.1-27.1) | 24.5 (23.0-26.1) | 26.6 (24.7-28.5) | 27.3 (25.5-29.0) | |
| Never | 63.0 (62.7-63.3) | 39.5 (38.3-40.6) | 49.0 (47.1-50.9) | 39.7 (37.6-41.9) | 29.3 (27.3-31.2) | |
| e-Cigarettes | ||||||
| Current | 2.5 (2.4-2.6) | 10.5 (9.7-11.2) | 8.5 (7.4-9.5) | 10.5 (9.1-12.0) | 12.6 (11.1-14.0) | <.001 |
| Former | 10.1 (9.9-10.3) | 30.3 (29.2-31.4) | 28.9 (27.1-30.6) | 31.5 (29.4-33.7) | 30.8 (28.9-32.6) | |
| Never | 61.3 (61.0-61.6) | 27.4 (26.4-28.4) | 32.4 (30.7-34.2) | 25.6 (23.7-27.4) | 23.5 (21.8-25.2) | |
| No e-cigarette questiond | 26.1 (25.9-26.4) | 31.9 (30.7-33.0) | 30.2 (28.5-32.0) | 32.4 (30.2-34.5) | 33.2 (31.1-35.3) | |
| Alcohol | ||||||
| Any alcohol in past 30 d | 48.5 (48.2-48.9) | 75.3 (74.3-76.3) | 78.5 (76.9-80.1) | 77.3 (75.4-79.2) | 70.4 (68.6-72.1) | <.001 |
| Any alcohol binges in past 30 d | 12.8 (12.5-13.0) | 39.7 (38.5-40.8) | 39.8 (37.9-41.6) | 43.9 (41.7-46.2) | 36.2 (34.1-38.3) | <.001 |
The cannabis module was administered in: Alaska, California, Colorado, Florida, Georgia, Idaho, Illinois, Maryland, Minnesota, Mississippi, Montana, North Dakota, Nebraska, New Hampshire, Ohio, Oklahoma, South Carolina, Tennessee, Utah, West Virginia, Wyoming, Guam, and Puerto Rico. Idaho, Minnesota, Tennessee, and Wyoming were the 4 states participating in the cannabis module across all 4 years of the combined 2016-2019 BRFSS data. See eTable 1 in the Supplement.
Infrequent use was defined as 1 to 5 days of cannabis use in the past month; frequent, as 6 to 29 days; and daily, as 30 days of use in the past month.
P value for the null hypothesis that cannabis use frequency does not vary by covariate of interest.
The 2019 survey did not include a question about e-cigarette use.
Cannabis use varied significantly by age, gender, race, marital status, education, employment, and income (Table 2). Infrequent (weighted percentage, 6.4%), frequent (5.2%), and daily use (6.3%) were more prevalent among the youngest age group (18 to 34 years old) compared with the oldest age group (≥65 years) (infrequent, 1.3%; frequent, 0.9%; daily, 0.9%) (eFigure 2 in the Supplement). Cannabis use was more prevalent among men (infrequent, 4.4%; frequent, 3.6%; daily, 4.8%) than women (infrequent, 3.0%; frequent, 2.0%; daily, 2.4%). There was significant variation among racial and ethnic groups. Black (5.1%) and Native American (7.2%) cannabis users were more likely to be daily users, while Asian cannabis consumers tended to be infrequent users.
Unmarried individuals engaged in higher frequency use (infrequent, 5.2%; frequent, 3.9%; daily, 5.2%) compared with married individuals (infrequent, 2.3%; frequent, 1.6%; daily, 1.9%) (eFigure 3 in the Supplement). Daily cannabis use was more common among individuals with high school education or less (infrequent, 3.2%; frequent, 2.5%; daily, 4.3%) compared with individuals with college degrees (infrequent, 3.4%; frequent, 2.2%; daily, 1.7%) (eFigure 4 in the Supplement). The prevalence of daily cannabis use was lower for those with higher annual income (<$25 000, 4.6%; $25 000-$74 999, 3.8%; ≥$75 000, 2.7%).
Dual Use of Cannabis With Tobacco and Alcohol
The prevalence of the dual use of cannabis and smoked tobacco was 3.4% (34.5% of cannabis users), while the prevalence of the dual use of cannabis and e-cigarettes was 1.4% (15.4% of persons who use cannabis) and the prevalence of the dual use of cannabis and binge drinking was 3.9% (39.7% of persons who use cannabis) (eFigure 5 in the Supplement). Over two-thirds of dual users of cannabis and tobacco (71.5%) or e-cigarettes (70.1%) were daily or frequent cannabis users. Over half (62.8%) of dual binge drinkers and cannabis users engaged in frequent and daily use.
Cannabis use was common among people that engaged in smoking tobacco (infrequent, 6.5%; frequent, 6.2%; daily, 10.1%) compared with persons that formerly smoked tobacco (infrequent, 3.8%; frequent, 3.0%; daily; 4.0%,) and never users of smoked tobacco (infrequent, 3.0%; frequent, 1.8%; daily; 1.7%) (eFigure 6 in the Supplement). Frequent and daily cannabis use was more prevalent among persons who currently (infrequent, 9.6%; frequent, 9.0%; daily, 13.6%) and formerly used e-cigarettes (infrequent, 8.9%; frequent, 7.3%; daily, 9.0%) compared with those who have never used e-cigarettes (infrequent, 2.1%; frequent, 1.2%; daily, 1.4%). Prevalence of infrequent, frequent, and daily use was higher among persons who engaged in binge drinking (infrequent, 9.5%; frequent, 7.9%; daily, 8.2%) than those who did not (infrequent, 2.6%; frequent, 1.8%; daily, 2.6%) (eFigure 7 in the Supplement)
Variation in Higher-Frequency Cannabis Use Among States With Different Legal Status
Prevalence of cannabis use differed significantly by state cannabis legality. Prevalence of infrequent (5.3%), frequent (4.2%), and daily use (4.7%) of cannabis was higher in those states with recreational legal cannabis than other states with nonlegal use (infrequent, 2.7%; frequent, 1.9%; daily, 2.6%) or medically legal use (infrequent, 3.5%; frequent, 2.5%; daily, 3.5%) (eFigure 8 in the Supplement).
Multivariate Ordinal Regression Determination of Factors Associated With Frequency of Cannabis Use
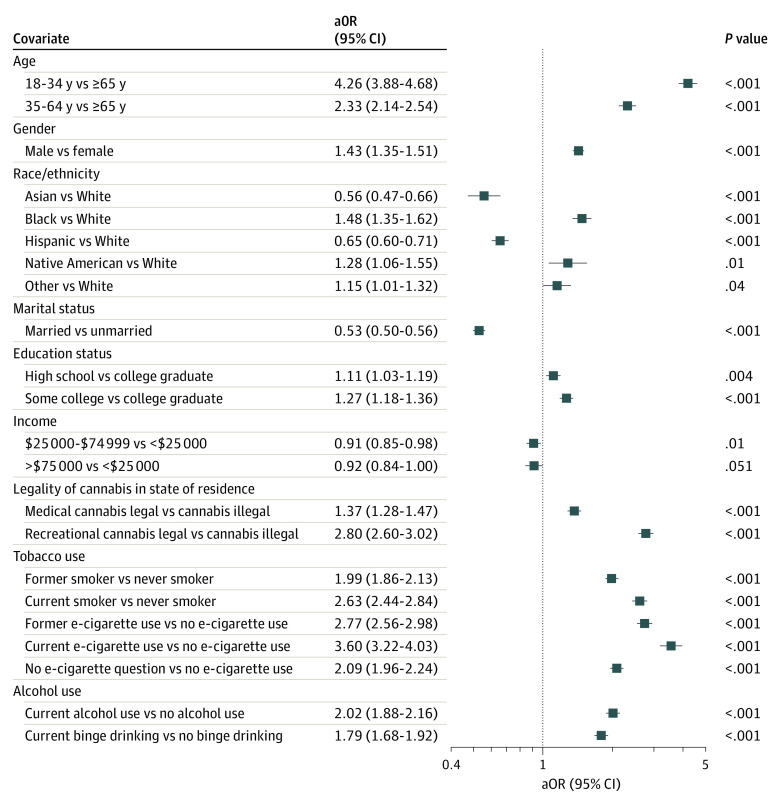
Compared with respondents ages 65 years or older, younger individuals were more likely to engage in higher-frequency cannabis use (ages 18-34 years: adjusted OR [aOR], 4.26; 95% CI, 3.88-4.68; ages 35-64 years: aOR, 2.33; 95% CI, 2.14-2.54) (Figure). Men were more likely to use cannabis at higher frequencies than women (aOR, 1.43; 95% CI, 1.35-1.51). Compared with White respondents, Black respondents (aOR, 1.48; 95% CI, 1.35-1.62) and Native American respondents (aOR, 1.28; 95% CI, 1.06-1.55) used cannabis at higher frequency, while Asian respondents (aOR, 0.56; 95% CI, 0.47-0.66) and Hispanic respondents (aOR, 0.65; 95% CI, 0.60-0.71) used cannabis with less frequency.
Figure. Adjusted ORs for Increased Cannabis Use Frequency Using Multiple Imputation Among Behavioral Risk Factor Surveillance System Respondents to the Cannabis Module, 2016-2019.
aOR indicates adjusted odds ratio.
Married respondents were less likely to use cannabis at higher frequencies compared with unmarried individuals (aOR, 0.53; 95% CI, 0.50-0.56). Compared with individuals with a college degree, having only a high school diploma or less (aOR, 1.11; 95% CI, 1.03-1.19) or some college experience (aOR, 1.27; 95% CI, 1.18-1.36) was associated with higher frequency cannabis use. Compared with the respondents with annual household incomes below $25 000, those with incomes between $25 000 and $74 999 (aOR, 0.91; 95% CI, 0.85-0.98) used cannabis with lower frequency, while those with incomes $75 000 and above were not significantly different (aOR, 0.92; 95% CI, 0.84-1.00).
Persons who currently (aOR, 2.63; 95% CI, 2.44-2.84) or formerly (aOR, 1.99; 95% CI, 1.86-2.13) smoked tobacco engaged in higher frequency cannabis use compared with never tobacco smokers. Current and former history of e-cigarette use was associated with higher frequency cannabis use (current: aOR, 3.60; 95% CI, 3.22-4.03; former: aOR, 2.77; 95% CI, 2.56-2.98) compared with nonuse of e-cigarettes. Alcohol use in the past 30 days (aOR, 2.02; 95% CI, 1.88-2.16) and binge drinking in the past 30 days (aOR, 1.79; 95% CI, 1.68-1.92) were associated with higher-frequency cannabis use. Compared with states where no cannabis use was legal, residence in a state with medically legal (aOR, 1.37; 95% CI, 1.28-1.47) or recreationally legal (aOR, 2.80; 95% CI, 2.60-3.02) cannabis use was associated with higher-frequency cannabis use.
Sensitivity Analyses
There were no substantial differences between the complete case analysis and that with multiple imputation except for the OR of high school education vs college degree, which was no longer significant. Excluding the 2 US territories from the analysis also resulted in no substantial change in the association between baseline factors and cannabis use frequency. We also compared the prevalence of model variables within sample (states during years where optional BRFSS cannabis module was given) and out of sample (states during years when optional cannabis module was not given) (eTable 2 in the Supplement). In-sample and out-of-sample covariates were distributed significantly differently at the 95% confidence level with the exceptions of differences for gender and marital status, which were not significantly different. Respondents to BRFSS in states that did not ask the cannabis module were younger and more likely to identify as White or Black, with a lower proportion of Hispanic individuals (eTable 2 in the Supplement). They also had greater prevalence of tobacco and alcohol use and less access to legalized recreational cannabis but greater access to medical cannabis. However, although there were statistically significant differences, most quantifiable differences between sample characteristics were quite small (eg, covariates for respondents aged 18-34 years: in sample, 27.9% vs out of sample, 29.7%; P < .001).
Discussion
Most research examining the association of cannabis use with demographic and behavioral factors have been studies with high risk of bias. Moreover, it has focused on past-month or past-year cannabis use, which does not inform our understanding of populations most likely to be affected by the health consequences of use. Some studies have looked at daily use, but these assume that nondaily users are homogeneous in risk, whereas they are likely heterogeneous given the potential spectrum of use frequency among nondaily users.46,47,48 We derived a data-driven categorization of past-month use based on the 5 days per month median of nondaily use. Infrequent use was more prevalent among students and married individuals. Both frequent and daily use were more common among younger individuals and men. Individuals who engaged in daily use were disproportionately Black or Native American and with lower socioeconomic status.
Legalization of cannabis has been partly driven by advocacy around the racial disparities in the legal system on possession and use of cannabis, with the goal of replacing a criminal justice approach to harm reduction.49 Our data demonstrates that higher-frequency cannabis use is more common among the same individuals that were the targets of the criminal justice system in terms of unfair sentencing (ie, young Black men).50 Higher-frequency cannabis use in these populations is especially a cause for concern, given the existing and emerging research that demonstrates the harms from use increase with frequency of use51,52,53
Our analysis also demonstrated that higher frequency cannabis use is concentrated among younger adults. The period between ages of 18 to 34 years are a crucial time for career development and higher education. Cannabis use, in particular use at least 4 days per week, is associated with neurocognitive deficits and poor educational and other social outcomes, especially in adolescents and young adults.51,54,55 The prevalence of cannabis use disorder is currently low in the US population (1.7%); however, it is underdiagnosed, and more cannabis use is associated with the development of cannabis use disorder.1,32,56 We found that over 6.4% of US (1 out of 16) adults engaged in frequent or daily use. These data suggest that young, Black, and Native American individuals may be more likely to be at risk for cannabis use disorder given that daily use is more common in this population. It is also possible that many young adults with higher frequency cannabis use are currently not being identified and screened for use disorders. Current guidelines only recommend screening for illicit drug use (including cannabis) in primary care when accurate diagnosis and treatment of substance use disorders are available in primary care or referral.57 However, there has been little research on how to practically diagnose and treat primary care patients with cannabis use disorders, and many primary care clinicians feel they lack the skills, time, and support necessary to diagnose and treat substance use disorders.58,59,60,61
Legalization of recreational cannabis has led to increased cannabis use.62 We found that higher frequency cannabis use was also more common among recreationally legal states. Because legalization has not prioritized public health, residents of US states with recreationally legal cannabis have higher exposure to cannabis advertising, media messages on benefits of cannabis, cannabis home delivery, and widespread dispensaries, which may perpetuate higher frequency of use.63,64,65,66,67,68,69,70,71,72,73 While state leaders have promoted the tax and criminal justice benefits of recreational legalization, the association of higher-frequency use with legalized recreational use may also eventually affect young adults from racial minority groups in those states (in the form of cannabis use disorders) and possibly the health systems (in the form of higher health care costs).74,75 While there are little data on the association of cannabis use with health care costs, emerging evidence indicates cannabis use is associated with motor vehicle accidents, increased poison control calls, and emergency department visits, suggesting that health system costs are possible.76,77,78,79,80,81,82,83
Cannabis use was also common among individuals with other adverse health behaviors, such as tobacco and alcohol use, suggesting that dual use with other legal substances may become an important public health consideration. Both cannabis and alcohol have psychoactive effects and are associated with impaired driving.84 In combination with alcohol, cannabis has a significantly enhanced impact on cognition, attention, and concentration and can potentiate the effects of impairment.85,86 Rates of driving under the influence of both alcohol and cannabis have risen in states with cannabis legalization.87 Given that high-frequency cannabis use is more common in recreationally legal states, more public health attention and campaigns on the dangers of combined cannabis and alcohol use in these states may be warranted. We also found that higher-frequency cannabis use was common among persons who use tobacco, including e-cigarettes. There is a limited literature examining the association of the dual use of cannabis and tobacco with health, but given that smoking is the most common form of cannabis use, the combination of tobacco use (either smoked or through e-cigarettes) and cannabis on cancer and cardiovascular and respiratory health is an important future direction for research.88 While our study has not examined any adverse or positive outcomes associated with cannabis use or high-frequency cannabis use, it suggests that with large enough samples, the association of high-frequency cannabis use and outcomes should be investigated.
Limitations
There are limitations to our study. Our sample may not be nationally representative because it only included the 21 states that were administered in the BRFSS cannabis module. While there were statistically significant differences among states that participated in the cannabis module and those that did not, most quantifiable differences between sample characteristics were small (eTable 2 in the Supplement). While respondents in states with legalized medical cannabis used cannabis on more days, we do not know to what extent, if any, this is the result of advice by health care professionals to do so. There were also no data on how many times per day respondents were using cannabis or the total amount of cannabis consumed. In the current study we were unable to measure the amount of use, patterns of use over time, or existing cannabis use disorder, and we did not examine other cannabis-associated problems.
Conclusions
This study of BRFSS data from 21 US states and 2 territories found that higher-frequency cannabis use was concentrated among younger and male adults, as well as adults who identified as Black or Native American or were from communities with low socioeconomic status. The decriminalization and legalization of cannabis was partly driven by social and racial justice concerns. Higher-frequency use among individuals in younger and racial minority populations is a cause for concern and may warrant attention from policymakers and public health officials. Furthermore, more attention may need to be paid to high frequency use in the form of screening, risk stratification, and treatment given the known and emerging negative health effects of cannabis.
eTable 1. Data Availability by State and Year, Color-Coded by Legality of Cannabis
eTable 2. Distribution of Covariates Within Sample (States During Years Where Optional Cannabis Module Was Given, n = 387 157) and Out of Sample (States During Years When Optional Cannabis Module Was Not Given, n = 1 404 866)
eFigure 1. Prevalence of Prominent Forms of Cannabis Use by Frequency of Use
eFigure 2. Prevalence of Cannabis Use Frequency by Age Group, Gender, and Race/Ethnicity
eFigure 3. Prevalence of Cannabis Use Frequency by Marital Status
eFigure 4. Prevalence of Cannabis Use Frequency by Educational Attainment, Employment Status, and Annual Income
eFigure 5. Prevalence of Dual Use of Cannabis and Smoked Tobacco, e-Cigarettes, and Binge Drinking by Frequency of Cannabis Use
eFigure 6. Prevalence of Cannabis Use Frequency by Tobacco Product Use
eFigure 7. Prevalence of Cannabis Use Frequency by Alcohol Use
eFigure 8. Prevalence of Cannabis Use Frequency by Legality of Cannabis in State of Residence
References
- 1.Center for Behavioral Health Statistics and Quality . 2019 National Survey on Drug Use and Health: Detailed Tables. Substance Abuse and Mental Health Services Administration . September 11, 2020. Accessed October 27, 2021. https://www.samhsa.gov/data/report/2019-nsduh-detailed-tables
- 2.Ghasemiesfe M, Ravi D, Vali M, et al. Marijuana use, respiratory symptoms, and pulmonary function: a systematic review and meta-analysis. Ann Intern Med. 2018;169(2):106-115. doi: 10.7326/M18-0522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ghasemiesfe M, Ravi D, Casino T, Korenstein D, Keyhani S. Acute cardiovascular effects of marijuana use. J Gen Intern Med. 2020;35(3):969-974. doi: 10.1007/s11606-019-05235-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ghasemiesfe M, Barrow B, Leonard S, Keyhani S, Korenstein D. Association between marijuana use and risk of cancer: a systematic review and meta-analysis. JAMA Netw Open. 2019;2(11):e1916318. doi: 10.1001/jamanetworkopen.2019.16318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morris MA, Jacobson SR, Kinney GL, et al. Marijuana use associations with pulmonary symptoms and function in tobacco smokers enrolled in the subpopulations and intermediate outcome measures in COPD study (SPIROMICS). Chronic Obstr Pulm Dis. 2018;5(1):46-56. doi: 10.15326/jcopdf.5.1.2017.0141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hancox RJ, Shin HH, Gray AR, Poulton R, Sears MR. Effects of quitting cannabis on respiratory symptoms. Eur Respir J. 2015;46(1):80-87. doi: 10.1183/09031936.00228914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Macleod J, Robertson R, Copeland L, McKenzie J, Elton R, Reid P. Cannabis, tobacco smoking, and lung function: a cross-sectional observational study in a general practice population. Br J Gen Pract. 2015;65(631):e89-e95. doi: 10.3399/bjgp15X683521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tashkin DP, Simmons MS, Tseng CH. Impact of changes in regular use of marijuana and/or tobacco on chronic bronchitis. COPD. 2012;9(4):367-374. doi: 10.3109/15412555.2012.671868 [DOI] [PubMed] [Google Scholar]
- 9.Aldington S, Williams M, Nowitz M, et al. Effects of cannabis on pulmonary structure, function and symptoms. Thorax. 2007;62(12):1058-1063. doi: 10.1136/thx.2006.077081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moore BA, Augustson EM, Moser RP, Budney AJ. Respiratory effects of marijuana and tobacco use in a US sample. J Gen Intern Med. 2005;20(1):33-37. doi: 10.1111/j.1525-1497.2004.40081.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sherrill DL, Krzyzanowski M, Bloom JW, Lebowitz MD. Respiratory effects of non-tobacco cigarettes: a longitudinal study in general population. Int J Epidemiol. 1991;20(1):132-137. doi: 10.1093/ije/20.1.132 [DOI] [PubMed] [Google Scholar]
- 12.Tashkin DP, Coulson AH, Clark VA, et al. Respiratory symptoms and lung function in habitual heavy smokers of marijuana alone, smokers of marijuana and tobacco, smokers of tobacco alone, and nonsmokers. Am Rev Respir Dis. 1987;135(1):209-216. [DOI] [PubMed] [Google Scholar]
- 13.Klumpers LE, Beumer TL, van Hasselt JG, et al. Novel Δ(9)-tetrahydrocannabinol formulation Namisol has beneficial pharmacokinetics and promising pharmacodynamic effects. Br J Clin Pharmacol. 2012;74(1):42-53. doi: 10.1111/j.1365-2125.2012.04164.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cooper ZD, Haney M. Comparison of subjective, pharmacokinetic, and physiological effects of marijuana smoked as joints and blunts. Drug Alcohol Depend. 2009;103(3):107-113. doi: 10.1016/j.drugalcdep.2009.01.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mittleman MA, Lewis RA, Maclure M, Sherwood JB, Muller JE. Triggering myocardial infarction by marijuana. Circulation. 2001;103(23):2805-2809. doi: 10.1161/01.CIR.103.23.2805 [DOI] [PubMed] [Google Scholar]
- 16.Callaghan RC, Allebeck P, Sidorchuk A. Marijuana use and risk of lung cancer: a 40-year cohort study. Cancer Causes Control. 2013;24(10):1811-1820. doi: 10.1007/s10552-013-0259-0 [DOI] [PubMed] [Google Scholar]
- 17.Aldington S, Harwood M, Cox B, et al. ; Cannabis and Respiratory Disease Research Group . Cannabis use and risk of lung cancer: a case-control study. Eur Respir J. 2008;31(2):280-286. doi: 10.1183/09031936.00065707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Berthiller J, Straif K, Boniol M, et al. Cannabis smoking and risk of lung cancer in men: a pooled analysis of three studies in Maghreb. J Thorac Oncol. 2008;3(12):1398-1403. doi: 10.1097/JTO.0b013e31818ddcde [DOI] [PubMed] [Google Scholar]
- 19.Voirin N, Berthiller J, Benhaïm-Luzon V, et al. Risk of lung cancer and past use of cannabis in Tunisia. J Thorac Oncol. 2006;1(6):577-579. doi: 10.1097/01243894-200607000-00013 [DOI] [PubMed] [Google Scholar]
- 20.Auer R, Vittinghoff E, Yaffe K, et al. Association between lifetime marijuana use and cognitive function in middle age: the Coronary Artery Risk Development in Young Adults (CARDIA) study. JAMA Intern Med. 2016;176(3):352-361. doi: 10.1001/jamainternmed.2015.7841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Volkow ND, Compton WM, Weiss SR. Adverse health effects of marijuana use. N Engl J Med. 2014;371(9):879. [DOI] [PubMed] [Google Scholar]
- 22.Moore TH, Zammit S, Lingford-Hughes A, et al. Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet. 2007;370(9584):319-328. doi: 10.1016/S0140-6736(07)61162-3 [DOI] [PubMed] [Google Scholar]
- 23.Large M, Sharma S, Compton MT, Slade T, Nielssen O. Cannabis use and earlier onset of psychosis: a systematic meta-analysis. Arch Gen Psychiatry. 2011;68(6):555-561. doi: 10.1001/archgenpsychiatry.2011.5 [DOI] [PubMed] [Google Scholar]
- 24.Marconi A, Di Forti M, Lewis CM, Murray RM, Vassos E. Meta-analysis of the association between the level of cannabis use and risk of psychosis. Schizophr Bull. 2016;42(5):1262-1269. doi: 10.1093/schbul/sbw003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Semple DM, McIntosh AM, Lawrie SM. Cannabis as a risk factor for psychosis: systematic review. J Psychopharmacol. 2005;19(2):187-194. doi: 10.1177/0269881105049040 [DOI] [PubMed] [Google Scholar]
- 26.Feingold D, Weinstein A. Cannabis and depression. Adv Exp Med Biol. 2021;1264:67-80. doi: 10.1007/978-3-030-57369-0_5 [DOI] [PubMed] [Google Scholar]
- 27.Walsh Z, Gonzalez R, Crosby K, S Thiessen M, Carroll C, Bonn-Miller MO. Medical cannabis and mental health: a guided systematic review. Clin Psychol Rev. 2017;51:15-29. doi: 10.1016/j.cpr.2016.10.002 [DOI] [PubMed] [Google Scholar]
- 28.Babson KA, Sottile J, Morabito D. Cannabis, cannabinoids, and sleep: a review of the literature. Curr Psychiatry Rep. 2017;19(4):23. doi: 10.1007/s11920-017-0775-9 [DOI] [PubMed] [Google Scholar]
- 29.Lev-Ran S, Roerecke M, Le Foll B, George TP, McKenzie K, Rehm J. The association between cannabis use and depression: a systematic review and meta-analysis of longitudinal studies. Psychol Med. 2014;44(4):797-810. doi: 10.1017/S0033291713001438 [DOI] [PubMed] [Google Scholar]
- 30.Mammen G, Rueda S, Roerecke M, Bonato S, Lev-Ran S, Rehm J. Association of cannabis with long-term clinical symptoms in anxiety and mood disorders: a systematic review of prospective studies. J Clin Psychiatry. 2018;79(4):17r11839. doi: 10.4088/JCP.17r11839 [DOI] [PubMed] [Google Scholar]
- 31.Bhagavan C, Kung S, Doppen M, et al. Cannabinoids in the treatment of insomnia disorder: a systematic review and meta-analysis. CNS Drugs. 2020;34(12):1217-1228. doi: 10.1007/s40263-020-00773-x [DOI] [PubMed] [Google Scholar]
- 32.Hasin DS. US epidemiology of cannabis use and associated problems. Neuropsychopharmacology. 2018;43(1):195-212. doi: 10.1038/npp.2017.198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bahorik AL, Campbell CI, Sterling SA, et al. Adverse impact of marijuana use on clinical outcomes among psychiatry patients with depression and alcohol use disorder. Psychiatry Res. 2018;259:316-322. doi: 10.1016/j.psychres.2017.10.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Metrik J, Stevens AK, Gunn RL, Borsari B, Jackson KM. Cannabis use and posttraumatic stress disorder: prospective evidence from a longitudinal study of veterans. Psychol Med. 2020;1-11. doi: 10.1017/S003329172000197X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Leung J, Chan GCK, Hides L, Hall WD. What is the prevalence and risk of cannabis use disorders among people who use cannabis? a systematic review and meta-analysis. Addict Behav. 2020;109:106479. doi: 10.1016/j.addbeh.2020.106479 [DOI] [PubMed] [Google Scholar]
- 36.Ravi D, Ghasemiesfe M, Korenstein D, Cascino T, Keyhani S. Associations between marijuana use and cardiovascular risk factors and outcomes: a systematic review. Ann Intern Med. 2018;168(3):187-194. doi: 10.7326/M17-1548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.O’Connor EA, Perdue LA, Senger CA, et al. Screening and Behavioral Counseling Interventions to Reduce Unhealthy Alcohol Use in Adolescents and Adults: An Updated Systematic Review for the US Preventive Services Task Force. Agency for Healthcare Research and Quality Publication No. 18-05242-EF-1. Published November 13, 2018. Accessed October 27, 2021. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/unhealthy-alcohol-use-in-adolescents-and-adults-screening-and-behavioral-counseling-interventions [PubMed]
- 38.Centers for Disease Control and Prevention . Behavioral Risk Factor Surveillance System. Updated August 31, 2020. Accessed November 4, 2020. https://www.cdc.gov/brfss/index.html
- 39.American Association for Public Opinion Research . Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys. Revised 2016. Accessed October 28, 2021. https://www.aapor.org/AAPOR_Main/media/publications/Standard-Definitions20169theditionfinal.pdf
- 40.US Census Bureau . Poverty thresholds by size of family and number of children. Revised October 8, 2021. Accessed October 27, 2021. https://www.census.gov/data/tables/time-series/demo/income-poverty/historical-poverty-thresholds.html
- 41.US Census Bureau . Income and Poverty in the United States: 2019. Report No. P60-270. September 15, 2020. Accessed October 27, 2021. https://www.census.gov/library/publications/2020/demo/p60-270.html
- 42.Centers for Disease Control and Prevention . Complex Sampling Weights and Preparing 2019 BRFSS Module Data for Analysis. Published July 2020. Accessed November 11, 2021. https://www.cdc.gov/brfss/annual_data/2019/pdf/Complex-Smple-Weights-Prep-Module-Data-Analysis-2019-508.pdf
- 43.Ananth CV, Kleinbaum DG. Regression models for ordinal responses: a review of methods and applications. Int J Epidemiol. 1997;26(6):1323-1333. doi: 10.1093/ije/26.6.1323 [DOI] [PubMed] [Google Scholar]
- 44.Graham JW, Olchowski AE, Gilreath TD. How many imputations are really needed? some practical clarifications of multiple imputation theory. Prev Sci. 2007;8(3):206-213. doi: 10.1007/s11121-007-0070-9 [DOI] [PubMed] [Google Scholar]
- 45.Honaker J, King G, Blackwell M. Amelia II: a program for missing data. Journal of Statistical Software. 2011;45(7):1-47. doi: 10.18637/jss.v045.i07 [DOI] [Google Scholar]
- 46.Brunet L, Moodie EE, Rollet K, et al. ; Canadian Co-infection Cohort Investigators . Marijuana smoking does not accelerate progression of liver disease in HIV-hepatitis C coinfection: a longitudinal cohort analysis. Clin Infect Dis. 2013;57(5):663-670. doi: 10.1093/cid/cit378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hézode C, Roudot-Thoraval F, Nguyen S, et al. Daily cannabis smoking as a risk factor for progression of fibrosis in chronic hepatitis C. Hepatology. 2005;42(1):63-71. doi: 10.1002/hep.20733 [DOI] [PubMed] [Google Scholar]
- 48.Di Forti M, Marconi A, Carra E, et al. Proportion of patients in south London with first-episode psychosis attributable to use of high potency cannabis: a case-control study. Lancet Psychiatry. 2015;2(3):233-238. doi: 10.1016/S2215-0366(14)00117-5 [DOI] [PubMed] [Google Scholar]
- 49.Firth CL, Maher JE, Dilley JA, Darnell A, Lovrich NP. Did marijuana legalization in Washington State reduce racial disparities in adult marijuana arrests? Subst Use Misuse. 2019;54(9):1582-1587. doi: 10.1080/10826084.2019.1593007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nguyen H, Reuter P.. How risky is marijuana possession? considering the role of age, race, and gender. Crime & Delinquency. 2012;58(6):879-910. doi: 10.1177/0011128712461122 [DOI] [Google Scholar]
- 51.National Academies of Sciences Engineering and Medicine . The Health Effects of Cannabis and Cannabinoids: Current State of Evidence and Recommendations for Research. National Academies of Science; 2017. [PubMed] [Google Scholar]
- 52.Page RL II, Allen LA, Kloner RA, et al. ; American Heart Association Clinical Pharmacology Committee and Heart Failure and Transplantation Committee of the Council on Clinical Cardiology; Council on Basic Cardiovascular Sciences; Council on Cardiovascular and Stroke Nursing; Council on Epidemiology and Prevention; Council on Lifestyle and Cardiometabolic Health; and Council on Quality of Care and Outcomes Research . Medical marijuana, recreational cannabis, and cardiovascular health: a scientific statement from the American Heart Association. Circulation. 2020;142(10):e131-e152. doi: 10.1161/CIR.0000000000000883 [DOI] [PubMed] [Google Scholar]
- 53.Tashkin DP, Roth MD. Pulmonary effects of inhaled cannabis smoke. Am J Drug Alcohol Abuse. 2019;45(6):596-609. doi: 10.1080/00952990.2019.1627366 [DOI] [PubMed] [Google Scholar]
- 54.Volkow ND, Baler RD, Compton WM, Weiss SR. Adverse health effects of marijuana use. N Engl J Med. 2014;370(23):2219-2227. doi: 10.1056/NEJMra1402309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Meier MH, Caspi A, Ambler A, et al. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proc Natl Acad Sci USA. 2012;109(40):e2657-e2664. doi: 10.1073/pnas.1206820109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Callaghan RC, Sanches M, Kish SJ. Quantity and frequency of cannabis use in relation to cannabis-use disorder and cannabis-related problems. Drug Alcohol Depend. 2020;217:108271. doi: 10.1016/j.drugalcdep.2020.108271 [DOI] [PubMed] [Google Scholar]
- 57.Krist AH, Davidson KW, Mangione CM, et al. ; US Preventive Services Task Force . Screening for unhealthy drug use: US Preventive Services Task Force recommendation statement. JAMA. 2020;323(22):2301-2309. doi: 10.1001/jama.2020.8020 [DOI] [PubMed] [Google Scholar]
- 58.Bradley KA, Lapham GT, Lee AK. Screening for drug use in primary care: practical implications of the new USPSTF recommendation. JAMA Intern Med. 2020;180(8):1050-1051. doi: 10.1001/jamainternmed.2019.7335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.McNeely J, Kumar PC, Rieckmann T, et al. Barriers and facilitators affecting the implementation of substance use screening in primary care clinics: a qualitative study of patients, providers, and staff. Addict Sci Clin Pract. 2018;13(1):8. doi: 10.1186/s13722-018-0110-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Saunders EC, Moore SK, Gardner T, et al. Screening for substance use in rural primary care: a qualitative study of providers and patients. J Gen Intern Med. 2019;34(12):2824-2832. doi: 10.1007/s11606-019-05232-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wakeman SE, Pham-Kanter G, Donelan K. Attitudes, practices, and preparedness to care for patients with substance use disorder: results from a survey of general internists. Subst Abus. 2016;37(4):635-641. doi: 10.1080/08897077.2016.1187240 [DOI] [PubMed] [Google Scholar]
- 62.Cerdá M, Mauro C, Hamilton A, et al. Association between recreational marijuana legalization in the United States and changes in marijuana use and cannabis use disorder from 2008 to 2016. JAMA Psychiatry. 2020;77(2):165-171. doi: 10.1001/jamapsychiatry.2019.3254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Barry RA, Glantz SA. Marijuana regulatory frameworks in four US states: an analysis against a public health standard. Am J Public Health. 2018;108(7):914-923. doi: 10.2105/AJPH.2018.304401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Orenstein DG, Glantz SA. Cannabis legalization in state legislatures: public health opportunity and risk. Marquette Law Rev. 2020;103(4):1313-1400. [PMC free article] [PubMed] [Google Scholar]
- 65.Bowling CM, Hafez AY, Glantz SA. Public health and medicine’s need to respond to cannabis commercialization in the United States: a commentary. J Psychoactive Drugs. 2020;52(4):377-382. doi: 10.1080/02791072.2020.1761040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zamengo L, Frison G, Zwitser G, Salomone A, Freeman TP. Cannabis knowledge and implications for health: considerations regarding the legalization of non-medical cannabis. Med Sci Law. 2020;60(4):309-314. doi: 10.1177/0025802420934255 [DOI] [PubMed] [Google Scholar]
- 67.Sznitman SR, Lewis N. Examining effects of medical cannabis narratives on beliefs, attitudes, and intentions related to recreational cannabis: a web-based randomized experiment. Drug Alcohol Depend. 2018;185:219-225. doi: 10.1016/j.drugalcdep.2017.11.028 [DOI] [PubMed] [Google Scholar]
- 68.Park SY, Holody KJ. Content, exposure, and effects of public discourses about marijuana: a systematic review. J Health Commun. 2018;23(12):1036-1043. doi: 10.1080/10810730.2018.1541369 [DOI] [PubMed] [Google Scholar]
- 69.Rup J, Goodman S, Hammond D. Cannabis advertising, promotion and branding: differences in consumer exposure between “legal” and “illegal” markets in Canada and the US. Prev Med. 2020;133:106013. doi: 10.1016/j.ypmed.2020.106013 [DOI] [PubMed] [Google Scholar]
- 70.Ishida JH, Zhang AJ, Steigerwald S, Cohen BE, Vali M, Keyhani S. Sources of information and beliefs about the health effects of marijuana. J Gen Intern Med. 2020;35(1):153-159. doi: 10.1007/s11606-019-05335-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Abraham A, Zhang AJ, Ahn R, Woodbridge A, Korenstein D, Keyhani S. Media content analysis of marijuana’s health effects in news coverage. J Gen Intern Med. 2018;33(9):1438-1440. doi: 10.1007/s11606-018-4492-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Cavazos-Rehg PA, Krauss MJ, Cahn E, et al. Marijuana promotion online: an investigation of dispensary practices. Prev Sci. 2019;20(2):280-290. doi: 10.1007/s11121-018-0889-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Silver LD, Naprawa AZ, Padon AA. Assessment of incorporation of lessons from tobacco control in city and county laws regulating legal marijuana in California. JAMA Netw Open. 2020;3(6):e208393. doi: 10.1001/jamanetworkopen.2020.8393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hammond D, Goodman S, Wadsworth E, Rynard V, Boudreau C, Hall W. Evaluating the impacts of cannabis legalization: the International Cannabis Policy study. Int J Drug Policy. 2020;77:102698. doi: 10.1016/j.drugpo.2020.102698 [DOI] [PubMed] [Google Scholar]
- 75.McGinty EE, Niederdeppe J, Heley K, Barry CL. Public perceptions of arguments supporting and opposing recreational marijuana legalization. Prev Med. 2017;99:80-86. doi: 10.1016/j.ypmed.2017.01.024 [DOI] [PubMed] [Google Scholar]
- 76.Ryan JL, Rosa VR. Healthcare cost associations of patients who use illicit drugs in Florida: a retrospective analysis. Subst Abuse Treat Prev Policy. 2020;15(1):73. doi: 10.1186/s13011-020-00313-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Gryczynski J, Schwartz RP, O’Grady KE, Restivo L, Mitchell SG, Jaffe JH. Understanding patterns of high-cost health care use across different substance user groups. Health Aff (Millwood). 2016;35(1):12-19. doi: 10.1377/hlthaff.2015.0618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Eichelberger AH. Marijuana use and driving in Washington State: risk perceptions and behaviors before and after implementation of retail sales. Traffic Inj Prev. 2019;20(1):23-29. doi: 10.1080/15389588.2018.1530769 [DOI] [PubMed] [Google Scholar]
- 79.Aydelotte JD, Brown LH, Luftman KM, et al. Crash fatality rates after recreational marijuana legalization in Washington and Colorado. Am J Public Health. 2017;107(8):1329-1331. doi: 10.2105/AJPH.2017.303848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wang GS, Le Lait MC, Deakyne SJ, Bronstein AC, Bajaj L, Roosevelt G. Unintentional pediatric exposures to marijuana in Colorado, 2009-2015. JAMA Pediatr. 2016;170(9):e160971. doi: 10.1001/jamapediatrics.2016.0971 [DOI] [PubMed] [Google Scholar]
- 81.Wang GS, Hall K, Vigil D, Banerji S, Monte A, VanDyke M. Marijuana and acute health care contacts in Colorado. Prev Med. 2017;104:24-30. doi: 10.1016/j.ypmed.2017.03.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Thomas AA, Von Derau K, Bradford MC, Moser E, Garrard A, Mazor S. Unintentional pediatric marijuana exposures prior to and after legalization and commercial availability of recreational marijuana in Washington State. J Emerg Med. 2019;56(4):398-404. doi: 10.1016/j.jemermed.2019.01.004 [DOI] [PubMed] [Google Scholar]
- 83.Hall KE, Monte AA, Chang T, et al. Mental health-related emergency department visits associated with cannabis in Colorado. Acad Emerg Med. 2018;25(5):526-537. doi: 10.1111/acem.13393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Asbridge M, Hayden JA, Cartwright JL. Acute cannabis consumption and motor vehicle collision risk: systematic review of observational studies and meta-analysis. BMJ. 2012;344:e536. doi: 10.1136/bmj.e536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Dubois S, Mullen N, Weaver B, Bédard M. The combined effects of alcohol and cannabis on driving: impact on crash risk. Forensic Sci Int. 2015;248:94-100. doi: 10.1016/j.forsciint.2014.12.018 [DOI] [PubMed] [Google Scholar]
- 86.Yurasek AM, Aston ER, Metrik J. Co-use of alcohol and cannabis: a review. Curr Addict Rep. 2017;4(2):184-193. doi: 10.1007/s40429-017-0149-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Salomonsen-Sautel S, Min SJ, Sakai JT, Thurstone C, Hopfer C. Trends in fatal motor vehicle crashes before and after marijuana commercialization in Colorado. Drug Alcohol Depend. 2014;140:137-144. doi: 10.1016/j.drugalcdep.2014.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Mayorga NA, Garey L, Nizio P, Buckner JD, Zvolensky MJ. The effects of cannabis use: a test among dual electronic and combustible cigarette users. Am J Addict. 2020;29(4):287-294. doi: 10.1111/ajad.13021 [DOI] [PubMed] [Google Scholar]
- 89.Centers for Disease Control and Prevention . Behavioral Risk Factor Surveillance System: 2019 Summary Data Quality Report. Published July 16, 2020. Accessed November 4, 2021. https://www.cdc.gov/brfss/annual_data/2019/pdf/2019-sdqr-508.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Data Availability by State and Year, Color-Coded by Legality of Cannabis
eTable 2. Distribution of Covariates Within Sample (States During Years Where Optional Cannabis Module Was Given, n = 387 157) and Out of Sample (States During Years When Optional Cannabis Module Was Not Given, n = 1 404 866)
eFigure 1. Prevalence of Prominent Forms of Cannabis Use by Frequency of Use
eFigure 2. Prevalence of Cannabis Use Frequency by Age Group, Gender, and Race/Ethnicity
eFigure 3. Prevalence of Cannabis Use Frequency by Marital Status
eFigure 4. Prevalence of Cannabis Use Frequency by Educational Attainment, Employment Status, and Annual Income
eFigure 5. Prevalence of Dual Use of Cannabis and Smoked Tobacco, e-Cigarettes, and Binge Drinking by Frequency of Cannabis Use
eFigure 6. Prevalence of Cannabis Use Frequency by Tobacco Product Use
eFigure 7. Prevalence of Cannabis Use Frequency by Alcohol Use
eFigure 8. Prevalence of Cannabis Use Frequency by Legality of Cannabis in State of Residence